Assessing Heatwave-Related Deaths among Older Adults by Diagnosis and Urban/Rural Areas from 1999 to 2020 in Slovenia
Abstract
1. Introduction
2. Methods
2.1. Study Area
2.2. Time Period
2.3. Number of Deaths Source
2.4. Definition of Heatwave, Heatwave Deaths, and Reference Periods Deaths
2.5. Definitions of Subgroups
2.6. Statistical Analysis: Relative Risks, 95% Confidence Interval and Excess Deaths
3. Results
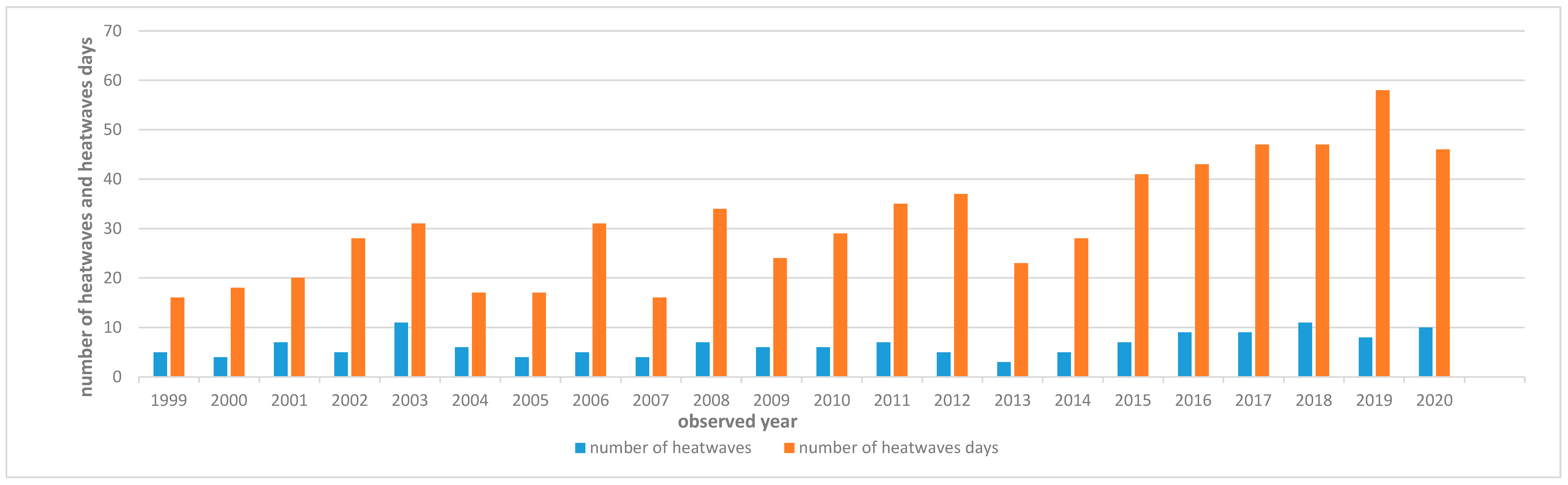
3.1. Analysis of Number of Deaths during Heatwaves for Each Year from 1999 to 2020
- For the general population, heatwaves were associated with an increase in deaths due to all causes: 10% (95% CI: 0–21%) more in 2006; 26% more in both 2007 (95% CI: 12–42%) and 2014 (95% CI: 14–40%).
- For those aged 75 and older, heatwaves were associated with an increase in deaths due to all causes: 22% more (95% CI: 4–44%) in 2007, 27% more (95% CI: 12–43%) in 2014, and 28% more (95% CI: 15–41%) in 2015.
- For those aged 75 and older, heatwaves were associated with an increase in deaths due to circulatory system diseases: 25% more (95% CI: 5–48%) in 2006, 33% more (95% CI: 6–67%) in 2007, 30% more (95% CI: 1–55%) in 2014, and 27% more (95% CI: 1–48%) in 2015.
3.2. Reports for Air Pollution in Slovenia for the Observed Years (2006, 2007, 2014, 2015)
4. Discussion
Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perkins-Kirkpatrick, S.E.; Lewis, S.C. Increasing trends in regional heatwaves. Nat. Commun. 2020, 11, 3357. [Google Scholar] [CrossRef] [PubMed]
- IPCC. Climate Change 2021: The Physical Science Basis; Masson-Delmotte, V., Zhai, P., Pirani, A., Connors, S.L., Péan, C., Chen, Y., Goldfarb, L., Gomis, M.I., Matthews, J.B.R., Berger, S., et al., Eds.; Cambridge University Press: Cambridge, UK, 2021. [Google Scholar]
- Berkeley Earth. Available online: https://berkeleyearth.org/ (accessed on 29 October 2023).
- Martínez-Solanas, È.; Quijal-Zamorano, M.; Achebak, H.; Petrova, D.; Robine, J.M.; Herrmann, F.R.; Rodó, X.; Ballester, J. Projections of temperature-attributable mortality in Europe: A time series analysis of 147 contiguous regions in 16 countries. Lancet Planet Health 2021, 5, e446–e454. [Google Scholar] [CrossRef] [PubMed]
- Ocena Podnebnih Sprememb v Sloveniji do Konca 21. Stoletja. Available online: https://meteo.arso.gov.si/uploads/probase/www/climate/text/sl/publications/OPS21_Porocilo.pdf (accessed on 23 October 2023).
- European Environment Agency. Climate Change, Impacts and Vulnerability in Europe 2012; EEA Report No 12/2012; EEA: Kebnhaven, Denmark, 2012.
- Fouillet, A.; Rey, G.; Wagner, V.; Laaidi, K.; Empereur-Bissonnet, P.; Le Tertre, A.; Frayssinet, P.; Bessemoulin, P.; Laurent, F.; De Crouy-Chanel, P.; et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol. 2008, 37, 309–317. [Google Scholar] [CrossRef]
- Casanueva, A.; Burgstall, A.; Kotlarski, S.; Messeri, A.; Morabito, M.; Flouris, A.D.; Nybo, L.; Spirig, C.; Schwierz, C. Overview of Existing Heat-Health Warning Systems in Europe. Int. J. Environ. Res. Public Health 2019, 16, 2657. [Google Scholar] [CrossRef] [PubMed]
- Åström, D.O.; Forsberg, B.; Rocklöv, J. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef]
- Kenney, W.L.; Munce, T.A. Invited review: Aging and human temperature regulation. J. Appl. Physiol. (1985) 2003, 95, 2598–2603. [Google Scholar] [CrossRef]
- Sommet, A.; Durrieu, G.; Lapeyre-Mestre, M.; Montastruc, J.L.; Association of French PharmacoVigilance Centres. A comparative study of adverse drug reactions during two heat waves that occurred in France in 2003 and 2006. Pharmacoepidemiol. Drug Saf. 2012, 21, 285–288. [Google Scholar] [CrossRef]
- United Nation. World Population Ageing 2013 ST/ESA/SER.A/348; Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2013. [Google Scholar]
- Statistical Office of the Republic of Slovenia. EUROPOP2023 Population Projections-Demographic Balances and Selected Indicators, Slovenia, 2022–2100. Available online: https://pxweb.stat.si/SiStatData/pxweb/sl/Data/Data/05U3019S.px/ (accessed on 27 October 2023).
- Linares, C.; Mirón, I.J.; Montero, J.C.; Criado-Álvarez, J.J.; Tobías, A.; Díaz, J. The time trend temperature-mortality as a factor of uncertainty analysis of impacts of future heat waves. Environ. Health Perspect. 2014, 122, A118. [Google Scholar] [CrossRef]
- Martinez, G.S.; Baccini, M.; De Ridder, K.; Hooyberghs, H.; Lefebvre, W.; Kendrovski, V.; Scott, K.; Spasenovska, M. Projected heat-related mortality under climate change in the metropolitan area of Skopje. BMC Public Health 2016, 16, 407. [Google Scholar] [CrossRef]
- Wu, J.; Zhou, Y.; Gao, Y.; Fu, J.S.; Johnson, B.A.; Huang, C.; Kim, Y.M.; Liu, Y. Estimation and uncertainty analysis of impacts of future heat waves on mortality in the eastern United States. Environ. Health Perspect. 2014, 122, 10–16. [Google Scholar] [CrossRef]
- Peng, R.D.; Bobb, J.F.; Tebaldi, C.; McDaniel, L.; Bell, M.L.; Dominici, F. Toward a quantitative estimate of future heat wave mortality under global climate change. Environ. Health Perspect. 2011, 119, 701–706. [Google Scholar] [CrossRef]
- Roldán, E.; Gómez, M.; Pino, M.R.; Pórtoles, J.; Linares, C.; Díaz, J. The effect of climate-change-related heat waves on mortality in Spain: Uncertainties in health on a local scale. Stoch. Environ. Res. Risk A 2016, 30, 831–839. [Google Scholar] [CrossRef]
- Bobb, J.F.; Peng, R.D.; Bell, M.L.; Dominici, F. Heat-related mortality and adaptation to heat in the United States. Environ. Health Perspect. 2014, 122, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Díaz, J.; Carmona, R.; Mirón, I.J.; Ortiz, C.; Linares, C. Comparison of the effects of extreme temperatures on daily mortality in Madrid (Spain), by age group: The need for a cold wave prevention plan. Environ. Res. 2015, 143 Pt A, 186–191. [Google Scholar] [CrossRef]
- Ng, C.F.S.; Boeckmann, M.; Ueda, K.; Zeeb, H.; Nitta, H.; Watanabe, C.; Honda, Y. Heat-related mortality: Effect modification and adaptation in Japan from 1972 to 2010. Glob. Environ. Change 2014, 9, 234–243. [Google Scholar] [CrossRef]
- Perčič, S.; Kukec, A.; Cegnar, T.; Hojs, A. Number of Heat Wave Deaths by Diagnosis, Sex, Age Groups, and Area, in Slovenia, 2015 vs. 2003. Int. J. Environ. Res. Public Health 2018, 15, 173. [Google Scholar] [CrossRef]
- Republic of Slovenia Statistical Office. Population of Slovenia. Available online: https://www.google.com/search?sxsrf=ACYBGNTJ6IA1Lb1L92EqTGYAVmhU2HdxgA%3A1571495426941&source=hp&ei=Ah6rXar6NuuXmwXdxYS4AQ&q=prebivalstvo+slovenije&oq=prebivastvo&gs_l=psy-ab.1.0.0i13l10.2340055.2346463.2348400...0.0..0.304.1473.8j2j1j1......0....1..gws-wiz.....10..35i362i39j35i39j0j0i10j0i203.XYQvALUynys#spf=1571497774642 (accessed on 18 October 2023).
- Slovenian Environment Agency (ARSO). National Meteorological Service of Slovenia. Available online: http://meteo.arso.gov.si/met/en/climate/ (accessed on 23 October 2023).
- Michelozzi, P.; Kirchmayer, U.; Katsouyanni, K.; Biggeri, A.; McGregor, G.; Menne, B.; Kassomenos, P.; Anderson, H.R.; Baccini, M.; Accetta, G.; et al. Assessment and prevention of acute health effects of weather conditions in Europe, the PHEWE project: Background, objectives, design. Environ. Health 2007, 6, 12. [Google Scholar] [CrossRef]
- Vida, M. Medicinska Meteorologija; Medicinska Fakulteta: Ljubljana, Slovenia, 1990. [Google Scholar]
- Joe, L.; Hoshiko, S.; Dobraca, D.; Jackson, R.; Smorodinsky, S.; Smith, D.; Harnly, M. Mortality during a Large-Scale Heat Wave by Place, Demographic Group, Internal and External Causes of Death, and Building Climate Zone. Int. J. Environ. Res. Public Health 2016, 13, 299. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.G.; Bell, M.L. Weather-related mortality: How heat, cold, and heat waves affect mortality in the United States. Epidemiology 2009, 20, 205–213. [Google Scholar] [CrossRef]
- Bao, J.; Wang, Z.; Yu, C.; Li, X. The influence of temperature on mortality and its Lag effect: A study in four Chinese cities with different latitudes. BMC Public Health 2016, 16, 375. [Google Scholar] [CrossRef]
- Baccini, M.; Kosatsky, T.; Analitis, A.; Anderson, H.R.; D’Ovidio, M.; Menne, B.; Michelozzi, P.; Biggeri, A.; PHEWE Collaborative Group. Impact of heat on mortality in 15 European cities: Attributable deaths under different weather scenarios. J. Epidemiol. Community Health 2011, 65, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Slovenian Environment Agency. Air Qality–Yearly Reports. Available online: http://rte.arso.gov.si/zrak/kakovost%20zraka/poro%C4%8Dila%20in%20publikacije/kakovost_letna.html (accessed on 9 September 2024).
- Van Someren, E.J. More than a marker: Interaction between the circadian regulation of temperature and sleep, age-related changes, and treatment possibilities. Chronobiol. Int. 2000, 17, 313–354. [Google Scholar] [CrossRef]
- Son, J.; Liu, J.C.; Bell, M.L. Temperature-related mortality: A systematic review and investigation of effect modifiers. Environ. Res. Lett. 2019, 14, 073004. [Google Scholar] [CrossRef]
- Sherina, M.S.; Rampal, L.; Mustaqim, A. Factors associated with chronic illness among the elderly in a rural community in Malaysia. Asia Pac. J. Public Health 2004, 16, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Franklin, R.C.; Mason, H.M.; King, J.C.; Peden, A.E.; Nairn, J.; Miller, L.; Watt, K.; FitzGerald, G. Heatwaves and mortality in Queensland 2010–2019: Implications for a homogenous state-wide approach. Int. J. Biometeorol. 2023, 67, 503–515. [Google Scholar] [CrossRef]
- Aghababaeian, H.; Ostadtaghizadeh, A.; Ardalan, A.; Asgary, A.; Akbary, M.; Yekaninejad, M.S.; Sharafkhani, R.; Stephens, C. Mortality Risk Related to Heatwaves in Dezful City, Southwest of Iran. Environ. Health Insights 2023, 17, 11786302231151538. [Google Scholar] [CrossRef]
- Xi, D.; Liu, L.; Zhang, M.; Huang, C.; Burkart, K.G.; Ebi, K.; Zeng, Y.; Ji, J.S. Risk factors associated with heatwave mortality in Chinese adults over 65 years. Nat. Med. 2024, 30, 1489–1498. [Google Scholar] [CrossRef]
- Liu, J.; Varghese, B.M.; Hansen, A.; Zhang, Y.; Driscoll, T.; Morgan, G.; Dear, K.; Gourley, M.; Capon, A.; Bi, P. Heat exposure and cardiovascular health outcomes: A systematic review and meta-analysis. Lancet Planet Health 2022, 6, e484–e495. [Google Scholar] [CrossRef]
- Thompson, R.; Landeg, O.; Kar-Purkayastha, I.; Hajat, S.; Kovats, S.; O’Connell, E. Heatwave Mortality in Summer 2020 in England: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 6123. [Google Scholar] [CrossRef]
- Chen, K.; Bi, J.; Chen, J.; Chen, X.; Huang, L.; Zhou, L. Influence of heat wave definitions to the added effect of heat waves on daily mortality in Nanjing, China. Sci. Total Environ. 2015, 506–507, 18–25. [Google Scholar] [CrossRef]
- Kim, E.J.; Kim, H. Effect modification of individual- and regional-scale characteristics on heat wave-related mortality rates between 2009 and 2012 in Seoul, South Korea. Sci. Total Environ. 2017, 595, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Zeng, W.; Zhou, M.; Wang, L.; Rutherford, S.; Lin, H.; Liu, T.; Zhang, Y.; Xiao, J.; Zhang, Y.; et al. The short-term effect of heat waves on mortality and its modifiers in China: An analysis from 66 communities. Environ. Int. 2015, 75, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, K.M.; Endlicher, W.R. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environ. Pollut. 2011, 159, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Burkart, K.; Schneider, A.; Breitner, S.; Khan, M.H.; Krämer, A.; Endlicher, W. The effect of atmospheric thermal conditions and urban thermal pollution on all-cause and cardiovascular mortality in Bangladesh. Environ. Pollut. 2011, 159, 2035–2043. [Google Scholar] [CrossRef] [PubMed]
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar] [CrossRef]
- Kovats, R.S.; Hajat, S. Heat stress and public health: A critical review. Annu. Rev. Public Health 2008, 29, 41–55. [Google Scholar] [CrossRef]
- Hu, K.; Guo, Y.; Hochrainer-Stigler, S.; Liu, W.; See, L.; Yang, X.; Zhong, J.; Fei, F.; Chen, F.; Zhang, Y.; et al. Evidence for Urban-Rural Disparity in Temperature-Mortality Relationships in Zhejiang Province, China. Environ. Health Perspect. 2019, 127, 37001. [Google Scholar] [CrossRef]
- Zeng, W.; Lao, X.; Rutherford, S.; Xu, Y.; Xu, X.; Lin, H.; Liu, T.; Luo, Y.; Xiao, J.; Hu, M.; et al. The effect of heat waves on mortality and effect modifiers in four communities of Guangdong Province, China. Sci. Total Environ. 2014, 482–483, 214–221. [Google Scholar] [CrossRef]
- Chen, K.; Zhou, L.; Chen, X.; Ma, Z.; Liu, Y.; Huang, L.; Bi, J.; Kinney, P.L. Urbanization Level and Vulnerability to Heat-Related Mortality in Jiangsu Province, China. Environ. Health Perspect. 2016, 124, 1863–1869. [Google Scholar] [CrossRef]
- D’Ippoliti, D.; Michelozzi, P.; Marino, C.; de’Donato, F.; Menne, B.; Katsouyanni, K.; Kirchmayer, U.; Analitis, A.; Medina-Ramón, M.; Paldy, A.; et al. The impact of heat waves on mortality in 9 European cities: Results from the EuroHEAT project. Environ. Health 2010, 9, 37. [Google Scholar] [CrossRef]
- Conti, S.; Masocco, M.; Meli, P.; Minelli, G.; Palummeri, E.; Solimini, R.; Toccaceli, V.; Vichi, M. General and specific mortality among the elderly during the 2003 heat wave in Genoa (Italy). Environ. Res. 2007, 103, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Health in Slovenia. Available online: https://nijz.si/wp-content/uploads/2022/07/zdravje_v_sloveniji_eng_e-verzija.pdf (accessed on 18 October 2023).
- American Heart Association. Available online: https://www.heart.org/en/health-topics/cholesterol/about-cholesterol/atherosclerosis (accessed on 18 October 2023).
- Folkow, B. Physiological aspects of primary hypertension. Physiol. Rev. 1982, 62, 347–504. [Google Scholar] [CrossRef]
- Greene, A.S.; Tonellato, P.J.; Lui, J.; Lombard, J.H.; Cowley, A.W., Jr. Microvascular rarefaction and tissue vascular resistance in hypertension. Am. J. Physiol. 1989, 256 Pt 2, H126–H231. [Google Scholar] [CrossRef]
- Carberry, P.A.; Shepherd, A.M.; Johnson, J.M. Resting and maximal forearm skin blood flows are reduced in hypertension. Hypertension 1992, 20, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.; Segal-Gidan, G. Heat-related illness in the elderly. Clin. Geriatr. 2007, 15, 37–45. [Google Scholar]
- Kenney, W.L.; Craighead, D.H.; Alexander, L.M. Heat waves, aging, and human cardiovascular health. Med. Sci. Sports Exerc. 2014, 46, 1891–1899. [Google Scholar] [CrossRef]
- Cui, J.; Arbab-Zadeh, A.; Prasad, A.; Durand, S.; Levine, B.D.; Crandall, C.G. Effects of heat stress on thermoregulatory responses in congestive heart failure patients. Circulation 2005, 112, 2286–2292. [Google Scholar] [CrossRef]
- Schols, J.M.; De Groot, C.P.; van der Cammen, T.J.; Olde Rikkert, M.G. Preventing and treating dehydration in the elderly during periods of illness and warm weather. J. Nutr. Health Aging 2009, 13, 150–157. [Google Scholar] [CrossRef]
- Watso, J.C.; Farquhar, W.B. Hydration Status and Cardiovascular Function. Nutrients 2019, 11, 1866. [Google Scholar] [CrossRef]
- Keatinge, W.R.; Coleshaw, S.R.; Easton, J.C.; Cotter, F.; Mattock, M.B.; Chelliah, R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am. J. Med. 1986, 81, 795–800. [Google Scholar] [CrossRef]
- Knochel, J.P. Heat stroke and related heat stress disorders. Dis. Mon. 1989, 35, 301–377. [Google Scholar] [PubMed]
- Glazer, J.L. Management of heatstroke and heat exhaustion. Am. Fam. Physician 2005, 71, 2133–2140. [Google Scholar] [PubMed]
- Wang, L.; Green, F.H.; Smiley-Jewell, S.M.; Pinkerton, K.E. Susceptibility of the aging lung to environmental injury. Semin. Respir. Crit. Care Med. 2010, 31, 539–553. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, D.; Berry, P.; Bouchet, V.; Charron, D.; Clarke, K.L.; Doyon, B.; Fleury, M.; Furgal, C.; Gosselin, P.; Lamy, S.; et al. Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity; Séguin, J., Ed.; Health Canada: Ottawa, ON, Canada, 2008. Available online: www.sindark.com/NonBlog/Articles/hc-cc-report/CCandHealth.pdf (accessed on 19 October 2019).
- Bevan, G.H.; Al-Kindi, S.G.; Brook, R.; Rajagopalan, S. Ambient Air Pollution and Atherosclerosis: Recent Updates. Curr. Atheroscler. Rep. 2021, 23, 63. [Google Scholar] [CrossRef]
- Robertson, S.; Miller, M.R. Ambient air pollution and thrombosis. Part. Fibre Toxicol. 2018, 15, 1. [Google Scholar] [CrossRef]
- Mazzoli-Rocha, F.; Fernandes, S.; Einicker-Lamas, M.; Zin, W.A. Roles of oxidative stress in signaling and inflammation induced by particulate matter. Cell Biol. Toxicol. 2010, 26, 481–498. [Google Scholar] [CrossRef]
- Šuškovič, S.; Camlek, T.; Gril, M.; Hudoklin, I.; Klobučar, A.; Koren, I.; Koterle, M.; Terzin, K.; Mežnar, B.; Silič, A. Prevalenca astme pri odraslih v Sloveniji. Zdrav. Vestn. 2011, 80, 451–457. [Google Scholar]
- Blanco, I.; Diego, I.; Bueno, P.; Fernández, E.; Casas-Maldonado, F.; Esquinas, C.; Soriano, J.B.; Miravitlles, M. Geographical distribution of COPD prevalence in Europe, estimated by an inverse distance weighting interpolation technique. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 13, 57–67. [Google Scholar] [CrossRef]
- Nairn, J.R.; Fawcett, R. Defining Heatwaves: Heatwave Defined as a Heat-Impact Event Servicing all Community and Business Sectors in Australia; Technical Report 060; Centre for Australian Weather and Climate Research (CAWCR): Kent Town, SA, Australia, 2013; 84p.

| 1999 | 2000 | 2001 | 2002 | 2003 | |
| Underlying Cause of Death (ICD-10 code) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| ALL, all causes (A00-T98) | 0.96 (0.85–1.08) | 1.06 (0.94–1.19) | 1.09 (0.97–1.21) | 1.04 (0.95–1.14) | 1.03 (0.94–1.12) |
| ALL, all causes, age group 75+ years (A00-T98) | 0.91 (0.76–1.09) | 1.14 (0.96–1.36) | 1.09 (0.93–1.28) | 1.04 (0.94–1.18) | 1.02 (0.92–1.16) |
| ALL, circulatory diseases, age group 75+ years (I00-I99) | 0.8 (0.63–1.02) | 1.17 (0.92–1.49) | 1.19 (0.94–1.51) | 1.09 (0.9–1.32) | 0.89 (0.47–1.06) |
| ALL, respiratory diseases, age group 75+ years (J00-J99) | 1.2 (0.69–2.3) | 1.03 (0.54–1.96) | 0.90 (0.53–1.53) | 1.05 (0.66–1.69) | 0.98 (0.65–1.48) |
| ALL, urban area, age group 75+ years (A00-T98) | 1.04 (0.63–1.74) | 1.04 (0.72–1.49) | 1.18 (0.85–1.65) | 1.08 (0.82–1.42) | 1.11 (0.86–1.43) |
| ALL, rural area, age group 75+ years (A00-T98) | 0.85 (0.71–1.03) | 1.16 (0.95–1.41) | 1.07 (0.89–1.28) | 1.03 (0.89–1.19) | 1.00 (0.87–1.15) |
| 2004 | 2005 | 2006 | 2007 | 2008 | |
| Underlying Cause of Death (ICD-10 code) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| ALL, all causes (A00-T98) | 1.03 (0.91–1.16) | 1.01 (0.9–1.14) | 1.10 (1.00–1.21) | 1.26 (1.12–1.42) | 1.02 (0.93–1.11) |
| ALL, all causes, age group 75+ years (A00-T98) | 1.01 (0.86–1.19) | 0.98 (0.84–1.15) | 1.07 (0.95–1.21) | 1.22 (1.04–1.44) | 1.01 (0.90–1.13) |
| ALL, circulatory diseases, age group 75+ years (I00-I99) | 1.05 (0.81–1.33) | 1.08 (0.85–1.35) | 1.25 (1.05–1.48) | 1.33 (1.06–1.67) | 0.99 (0.84–1.16) |
| ALL, respiratory diseases, age group 75+ years (J00-J99) | 1.10 (0.64–1.88) | 1.29 (0.71–2.31) | 1.13 (0.79–1.69) | 1 (0.52–2.07) | 0.95 (0.65–1.38) |
| ALL, urban area, age group 75+ years (A00-T98) | 1.18 (0.84–1.66) | 1.06 (0.77–1.47) | 1.33 (1.02–1.72) | 1.07 (0.77–1.49) | 0.98 (0.78–1.23) |
| ALL, rural area, age group 75+ years (A00-T98) | 0.94 (0.78–1.13) | 0.94 (0.79–1.13) | 1.09 (0.95–1.26) | 1.29 (1.13–1.47) | 1.02 (0.90–1.16) |
| 2009 | 2010 | 2011 | 2012 | 2013 | |
| Underlying Cause of Death (ICD-10 code) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| ALL, all causes (A00-T98) | 1.01 (0.91–1.11) | 1.05 (0.96–1.14) | 1.01 (0.93–1.09) | 1.03 (0.95–1.11) | |
| ALL, all causes, age group 75+ years (A00-T98) | 0.96 (0.84–1.1) | 1.03 (0.91–1.15) | 1.03 (0.93–1.15) | 1.07 (0.96–1.19) | 0.96 (0.86–1.09) |
| ALL, circulatory diseases, age group 75+ years (I00-I99) | 1.04 (0.85–1.26) | 0.97 (0.87–1.15) | 1.01 (0.87–1.18) | 1.07 (0.92–1.24) | 0.99 (0.83–1.17) |
| ALL, respiratory diseases, age group 75+ years (J00-J99) | 0.86 (0.52–1.40) | 1.27 (0.84–1.93) | 0.84 (0.57–1.23) | 0.81 (0.56–1.17) | 1.23 (0.79–1.91) |
| ALL, urban area, age group 75+ years (A00-T98) | 1.17 (0.89–1.53) | 1.25 (0.98–1.60) | 1.02 (0.82–1.28) | 1.26 (1.01–1.57) | 1.04 (0.84–1.27) |
| ALL, rural area, age group 75+ years (A00-T98) | 0.90 (0.77–1.05) | 0.96 (0.84–1.1) | 1.03 (0.92–1.16) | 1.02 (0.9–1.14) | 0.93 (0.8–1.07) |
| 2014 | 2015 | 2016 | 2017 | 2018 | |
| Underlying Cause of Death (ICD-10 code) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| ALL, all causes (A00-T98) | 1.26 (1.14–1.40) | 1.07 (0.99–1.16) | 0.99 (0.91–1.06) | 1.01 (0.94–1.09) | 1.01 (0.92–1.08) |
| ALL, all causes, age group 75+ years (A00-T98) | 1.27 (1.12–1.43) | 1.28 (1.15–1.41) | 1.07 (9.96–1.19) | 0.98 (0.90–1.06) | 0.99 (0.89–1.09) |
| ALL, circulatory diseases, age group 75+ years (I00-I99) | 1.3 (1.1–1.55) | 1.27 (1.1–1.48) | 1.02 (0.87–1.18) | 0.97 (0.86–1.11) | 1.02 (0.85–1.21) |
| ALL, respiratory diseases, age group 75+ years (J00-J99) | 1.03 (0.65–1.63) | 1.08 (0.75–1.55) | 0.83 (0.55–1.23) | 0.98 (0.67–1.44) | 0.97 (0.58–1.63) |
| ALL, urban area, age group 75+ years (A00-T98) | 1.29 (0.99–1.68) | 1.17 (0.95–1.45) | 1.14 (0.92–1.43) | 0.98 (0.87–1.11) | 1.10 (0.90–1.36) |
| ALL, rural area, age group 75+ years (A00-T98) | 1.26 (1.09–1.45) | 1.31 (1.16–1.47) | 1.05 (0.93–1.18) | 0.97 (0.86–1.1) | 1.05 (0.90–1.23) |
| 2019 | 2020 | ||||
| Underlying Cause of Death (ICD-10 code) | RR (95% CI) | RR (95% CI) | |||
| ALL, all causes (A00-T98) | 1 (0.94–1.06) | 1.06 (0.99–1.13) | |||
| ALL, all causes, age group 75+ years (A00-T98) | 0.96 (0.87–1.03) | 1.03 (0.95–1.12) | |||
| ALL, circulatory diseases, age group 75+ years (I00-I99) | 0.89 (0.80–1.00) | 1.05 (0.93–1.2) | |||
| ALL, respiratory diseases, age group 75+ years (J00-J99) | 0.88 (0.79–1.01) | 1.02 (0.68–1.55) | |||
| ALL, urban area, age group 75+ years (A00-T98) | 1.08 (0.92–1.28) | 0.98 (0.83–1.17) | |||
| ALL, rural area, age group 75+ years (A00-T98) | 1.03 (0.92–1.16) | 1.04 (0.95–1.15) |
 —statistically significant association.
—statistically significant association.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perčič, S.; Bitenc, K.; Pohar, M.; Uršič, A.; Cegnar, T.; Hojs, A. Assessing Heatwave-Related Deaths among Older Adults by Diagnosis and Urban/Rural Areas from 1999 to 2020 in Slovenia. Climate 2024, 12, 148. https://doi.org/10.3390/cli12090148
Perčič S, Bitenc K, Pohar M, Uršič A, Cegnar T, Hojs A. Assessing Heatwave-Related Deaths among Older Adults by Diagnosis and Urban/Rural Areas from 1999 to 2020 in Slovenia. Climate. 2024; 12(9):148. https://doi.org/10.3390/cli12090148
Chicago/Turabian StylePerčič, Simona, Katarina Bitenc, Majda Pohar, Anka Uršič, Tanja Cegnar, and Ana Hojs. 2024. "Assessing Heatwave-Related Deaths among Older Adults by Diagnosis and Urban/Rural Areas from 1999 to 2020 in Slovenia" Climate 12, no. 9: 148. https://doi.org/10.3390/cli12090148
APA StylePerčič, S., Bitenc, K., Pohar, M., Uršič, A., Cegnar, T., & Hojs, A. (2024). Assessing Heatwave-Related Deaths among Older Adults by Diagnosis and Urban/Rural Areas from 1999 to 2020 in Slovenia. Climate, 12(9), 148. https://doi.org/10.3390/cli12090148









