Abstract
The emergence of the COVID-19 pandemic has increased research outputs in telemedicine over the last couple of years. One solution to the COVID-19 pandemic as revealed in literature is to leverage telemedicine for accessing health care remotely. In this survey paper, we review several articles on eHealth and Telemedicine with emphasis on the articles’ focus area, including wireless technologies and architectures in eHealth, communications protocols, Quality of Service, and Experience Standards, among other considerations. In addition, we provide an overview of telemedicine for new readers. This survey reviews several telecommunications technologies currently being proposed along with their standards and challenges. In general, an encompassing survey on the developments in telemedicine technology, standards, and protocols is presented while acquainting researchers with several open issues. Special mention of the state-of-the-art specialist application areas are presented. We conclude the survey paper by presenting important research challenges and potential future directions as they pertain to telemedicine technology.
1. Introduction
The concept of telemedicine encompasses the use of information and telecommunication technology to render medical services irrespective of geographical separation between physicians and patients [1]. Telemedicine has been in practice as far back as the 1900s. It covers any form of electronic communication between health workers and patients from a remote location [1,2]. Recently, researchers have focused more on wireless communication technologies for telemedicine to provide effective and reliable health care service delivery from remote location especially during emergencies. Various communication technologies have been proposed and implemented for providing expert medical services to patients without the need for the conventional face-to-face encounters with patients. This has greatly reduced the cost of medical diagnosis and the need to travel long distances in search of professional consultations. Available studies on telemedicine implementations suggest the need for continuous research to address several issues and challenges [3,4]. There is a need to compare relevant studies in the field in order to provide a broad overview of available communication technologies suitable for modern designs as well as to identify the most viable means of practical implementation. This is not to say that telemedicine should completely replace the conventional practice of physical diagnostic and other medical processes, as certain services require physical face-to-face contact. Nonetheless, the deployment of telemedicine could greatly reduce congestion in hospitals, and consequently limit the spread of infectious diseases.
The advent of the COVID-19 pandemic has increased the need to leverage the benefits of telemedicine and eHealth. Telemedicine and eHealth research has seen an upsurge in recent works [5]. For instance, the authors of [6] examined variability in services between in-person and telemedicine. The method adopted involved analysis of 1104 patients. Comparing patients seen in-person to those seen by telemedicine revealed telemedicine to be an acceptable alternative to in-person evaluation for routine pediatric clinical genetics care. This result affirms similar conclusions in [7,8,9,10,11]. Several studies have encouraged the use of telemedicine in the post-COVID-19 era [12,13,14,15]; as such, there is a need for a review of telecommunication technologies towards the realization of fully functional telemedicine services.
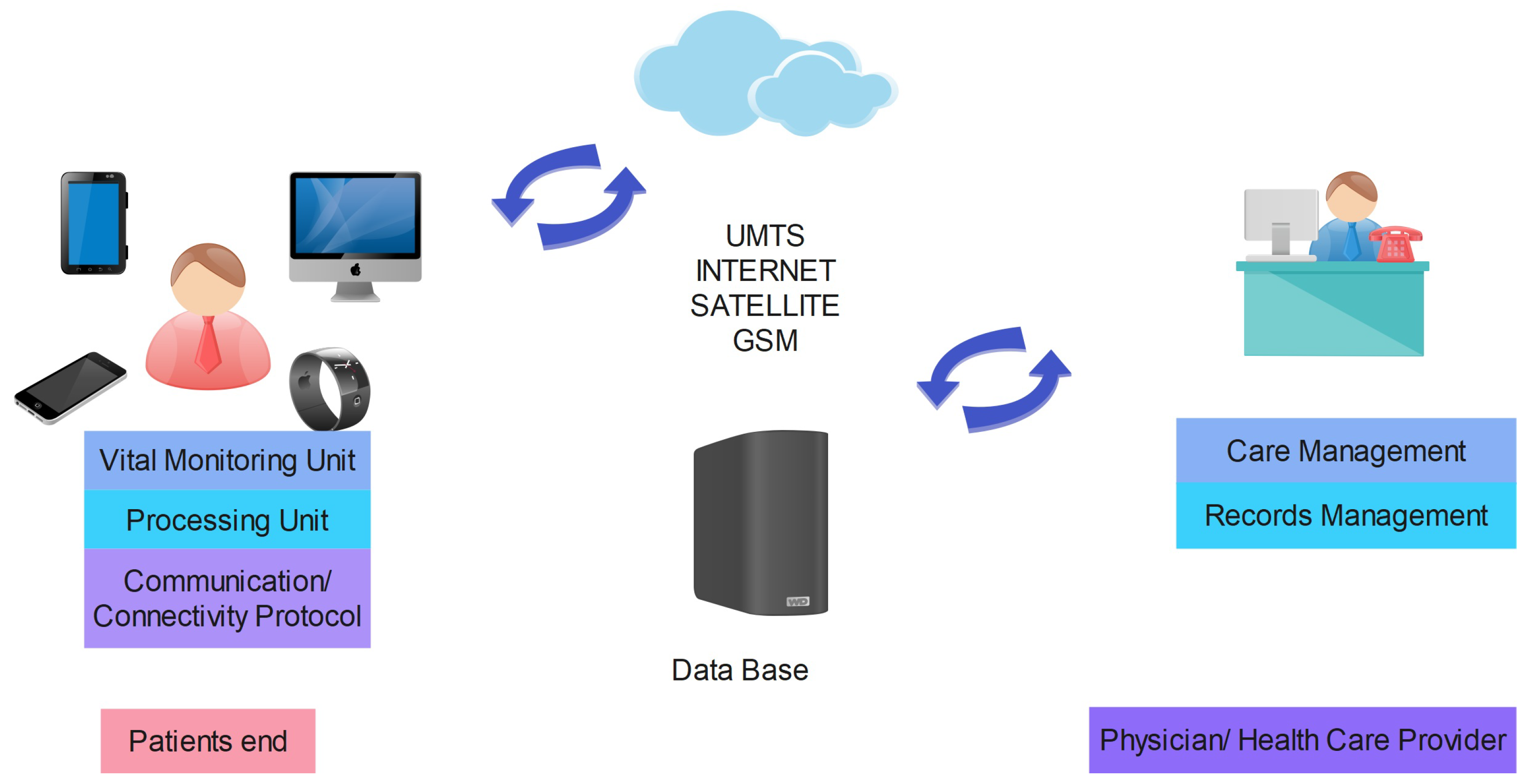
This survey work presents previous work carried out by other researchers with respect to the different communication technologies that have been deployed in telemedicine. Among these technologies are internet and wireless technologies for digital data transmission, mobile telemedicine, wireless design, WBAN, satellite-based communication, and cellular technologies, including the use of infrared links. A general overview of telemedicine systems is presented in Figure 1. For telemedicine applications, communications can be classified as follows:
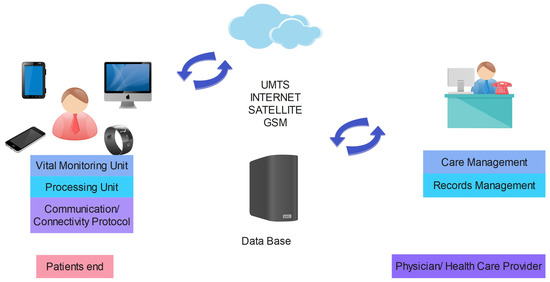
Figure 1.
Telemedicine Systems.
- Body Area Communication: communication between patients and telemedical devices such as the wearable sensors;
- Remote Communications: communication between the telemedical devices and remote servers, including satellite, internet, GSM, and WAN communications;
- Communication based on application area, including communication for emergency telemedicine, video conferencing, and transmission of medical images.
Connectivity protocols/standards required for communications technologies in telemedicine consist of ZigBee/IEEE 802.15.4, Bluetooth/IEEE 802.15.1, WiMAX/IEEE Broadband Wireless Access (BWA) 802.16, Wi-Fi/WLAN/IEEE 802.11, User Datagram Protocol (UDP), Real-Time Protocol (RTP), and Real-Time Transport Control Protocol (RTCP) and TCP/IP.
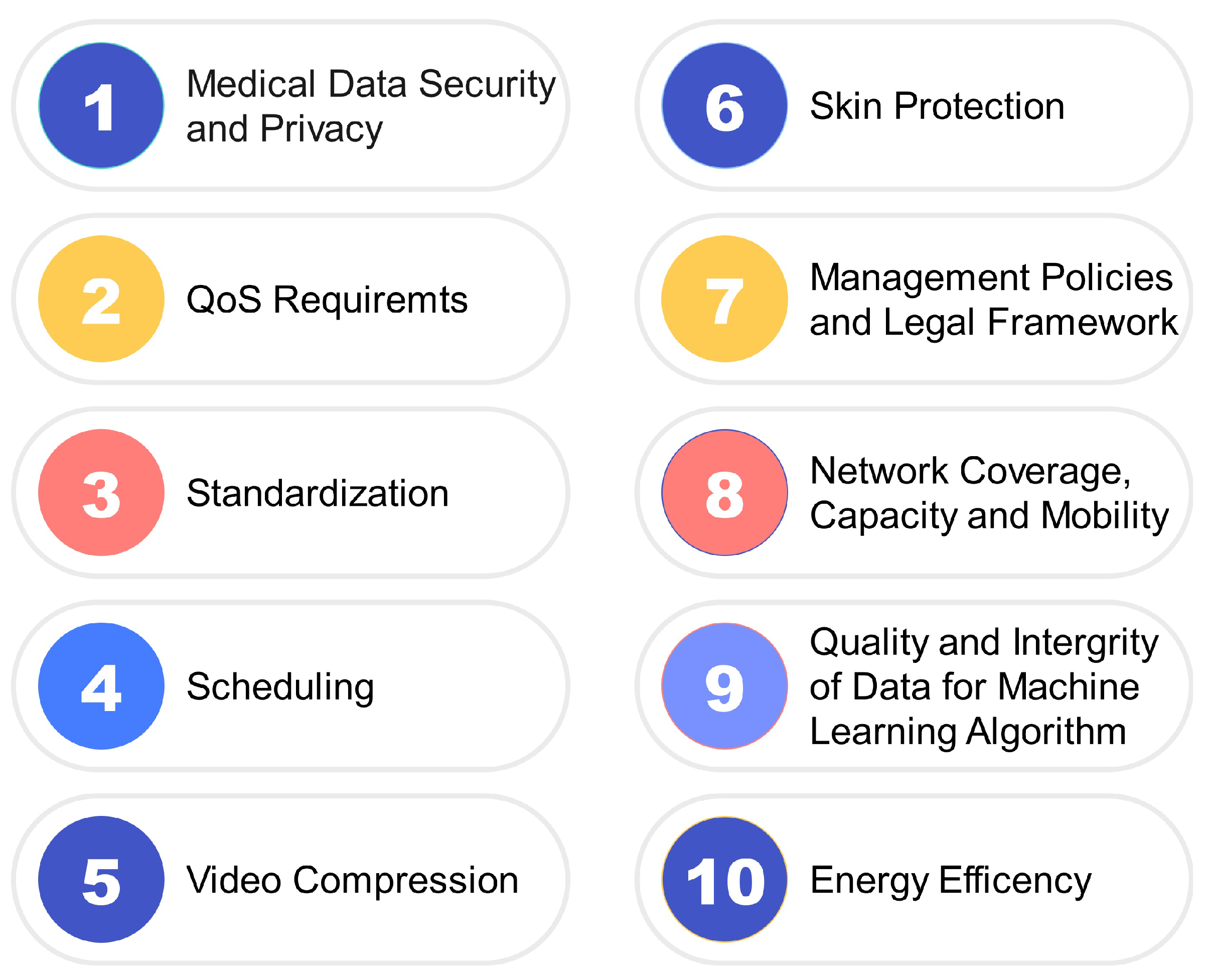
Again, this research work essentially focuses on reviewing communications technologies utilized in telemedicine implementations, issues and challenges associated with deployment, and standardization and future directions for further research. Despite several efforts by researchers in the existing literature, no standard format has been developed for medical data communication in telemedicine [16]. This issue of standardization and incompatible devices has greatly affected the smooth and speedy roll-out of newly invented telemedicine projects. Other challenges and research issues include data security and privacy, safety of patients in case of wearable devices, and QoS requirements. These are important areas that require attention by researchers to enhance the deployment of telemedicine in addressing the rising demand and cost of medication.
The specific contributions of this work include:
- An overview of telemedicine and the evolution of telecommunications technology;
- A review of the various standards and protocols present in telemedicine, with a focus on the current trends;
- Identification of several deployment challenges along with the state-of-the-art in this research area.
A general outline of the rest of this article is provided here. Section 2 presents a review of major research areas, with the aim of identifying state-of-the-art technologies along with existing implementation constraints. Section 3 provides an overview of telemedicine, while Section 4 introduces the evolution of communication technologies for telemedicine. Some use cases of telemedicine were presented in Section 5 also types of information transmitted in Section 6. Communications standards and protocols used in telemedicine are highlighted in Section 7. Finally, Section 8 outlines the current research challenges and future directions involved in harnessing robust, secure, efficient, and high-quality communications technologies for telemedicine systems, and we conclude the review in Section 9.
2. Related Work
Several studies and surveys have been conducted into e-health and telemedicine. In one survey paper, [17], the authors addressed a number of central issues, including upcoming applications of internet and wireless telemedicine systems, in particular the emergence of mobile IP and possible compatibility with Wireless Application Protocol (WAP) and GPRS-based phones for internet telemedicine. In a related article by [18], various applications and data transmission in e-health were discussed. In addition to the application of wireless telemedicine in real-time and digital data transmission currently in practice, the authors presented a broad overview and analysis of wireless technologies applied in telemedicine. In [19], the authors discussed IoT technologies and architecture, including the framework they can provide for use in telemedicine applications. In another related work [20], wireless technologies and their evolution for use in telemedice were detailed, bringing researchers up to speed on how ICT has enhanced telemedicine. Other radio technologies, such as the RFID-based devices, were discussed in the context of Healthcare delivery in [21].
In [22], the authors described the application of wireless communication technologies in telemedicine, and provided detailed architectural framework. A number of the major issues with mobile telemedicine were highlighted, along with a summary of the potential benefits of integrated wireless telemedicine systems. A related study by [23] presented telemedicine communications technologies and the challenges involved in deploying telemedicine services in Indonesia. The communications technologies discussed included the application of wireless LAN and satellite communication in telemedicine designs.
Another application of wireless communication and designs in telemedicine was discussed in [24], with particular emphasis on emerging technologies in telemedicine and ehealth applications. The author anticipated lower-cost wireless systems with improved data transfer rates and the use of intelligent agents in future designs of telemedicine systems. A similar overview of design analysis of mobile and wireless systems in telemedicine was presented in [25]. This article described three major aspects of mobile and wireless telemedicine designs, namely, mobile health systems, Wireless Body Area Network (WBAN), and intelligent wireless sensors.
A closely related system based on ICT applications and architectures in telemedicine was presented in [26]. This paper emphasized ICT development in telemedicine and classification of wireless networks for applications in telemedicine, and presented a detailed review of telemedicine architectures. While most review articles to date have focused on close-range communications technologies, Ref. [27] presented satellite-based projects for telemedicine applications. Their paper described various wireless communication technologies for telemedicine and a number of specific architectures for e-health systems via satellite communications technology. In [28], an overview of the basic components of an end-to-end wireless medical video telemedicine system was presented. The authors discussed a wireless medical video telemedicine system architecture for real-time applications. Four broad classifications of research in m-health systems were presented in their report.
Several factors problematizing the rapid deployment of telemedicine have been identified in research focused on telemedicine systems based on the internet in China [29]. In this study, the authors examined several telemedicine systems developed and adopted in China, including multicasting, teleconsultation, satellite-based communication, WLAN, SMS, Bluetooth, and wireless communication technologies. According to [3], most wireless telemedicine systems are associated with major issues, most prominently security, patient monitoring, scheduling, video compressing, and transmission media. In a similar survey, Ref. [30] highlighted several major issues in the implementation of wireless sensor network in telemedicine. In particular, issues related to ZigBee and Bluetooth transmission technologies used for communication between sensors and WSN were emphasized.
In their survey article, Ref. [31] specifically discussed mobile telemedicine systems using satellite-based communication and cellular technologies. In another article [16], the research was focused on wireless technologies and the challenges to e-health. Similarly, Ref. [32] provided useful insights on wireless technology and the challenges present in telemedicine. Their work presented more details on the application of wireless technologies in healthcare as well as challenges with wireless telemedicine, mobile phone telemedicine, and data transmission techniques. In [33], the authors presented an article on wireless telemedicine localized in Tanzania. The authors provided a description of different wireless technologies used in telemedicine.
Body Area Networks (BAN) for monitoring of patients in telemedicine were considered in [4]. This study posits that telemedicine can leverage the advancement of microelectronic technology for healthcare delivery. Specifically, their paper discusses the integration of BAN in telemedicine systems involving a Wide-Body Area Network (WBAN) framework. A review of devices used in telemedicine systems was showcased in [34]. Primarily, the authors showed the devices for obtaining the vital signs for telemedicine applications; more precisely, the integration of vital sign sensors and other wireless medical devices to telemedicine systems were highlighted. In [35], the authors showed how an ad hoc wireless sensor network system could be applied in the telemedicine sub-area of disaster survivor detection. Relay stations were deployed to transmit captured data to sink nodes, which then forwarded the data to either the base stations of a cellular network or to WIMAX-based antennas. In [31], the authors reported that mobile communication technologies for telemedicine must have operational parameters that meet the expected Quality of Service requirements of medical services, which can include clinical data measurement of images such as digital X-Rays and audio signals with high bit error rates.
The authors of [36] performed a thorough review of Quality of Service (QoS) and architectures in healthcare systems. Specifically, their paper presented the features of e-health applications along with QoS for the application of specific healthcare services in telemedicine and telemedicine architecture. In [37], the authors examined both QoS and Quality of Experience (QoE) in telemedicine systems. Wireless techniques in telemedicine were presented in [38], with a specific focus on the Vertical Handoff (VHO) technique in telemedicine. In the foregoing, several survey articles have been mentioned that looked at different areas involved in telemedicine. In the present article, the reader’s attention is drawn towards discussion of the communications technologies used in wearable sensor devices for vital sign monitoring in telemedicine applications. Table 1 presents an overview of previous survey articles and their respective areas of focus listed in chronological order based on the year of publication. From this table, it can be seen that early works in telemedicine focused on implementation-related issues and technologies, while recent works have focused more on policies related to standardization, QoS, and QoE.

Table 1.
Summary of Related Works.
3. Overview of Telemedicine
Telemedicine is a means of transmitting biomedical data between patient and care-giver at different locations without face-to-face contact. It saves cost and time in health care services by providing remote medication that eliminate the need to travel to see a medical expert [42]. In [18], the authors defined telemedicine as the delivery of health care and the sharing of medical knowledge over distance using telecommunication. Telemedicine provides expert-based medical care to any place where health care is needed without physical contact. It uses existing wired and wireless infrastructures for both prototype and real-time designs [33]. The use of telemedicine over wired communication technologies ha been implemented using plain old telephone systems (POTS) and integrated services digital networks (ISDN). In contemporary telemedicine, several wireless communication technologies have been deployed for various systems and designs [43]. These include ZigBee, Bluetooth, VSAT, WLAN, WiMAX, GPRS, and UMTS (3G and 4G). Telemedicine is a developing technology that could be implemented by combining telecommunication and information technologies towards the improvement of the medical profession. It is a new way of delivering health care facilities to patients, even those in extremely isolated areas [33].
In [16], telemedicine was viewed as the transmission of essential clinical information by means of modern ICT to deliver healthcare services to patients located at considerable distances, and was grouped into live telemedicine and store-and-forward telemedicine. In live telemedicine, audio-visual communications over high bandwidth and low latency connections involve the presence of both the patient and the doctor, while store-and-forward involves the acquisition of medical data, images, and video transmission by a medical expert for offline diagnosis. Telemedicine involves the use of ICT, especially two-way interactive audio/video communications, computers, and telemetry, to deliver health services to remote patients and facilitate information exchange between primary care physicians and specialists located at a distance from each other [26]. Alternatively, telemedicine can be seen as the use of advanced telecommunications technologies to exchange health information and provide healthcare services across geographic, time, social, and cultural barriers.
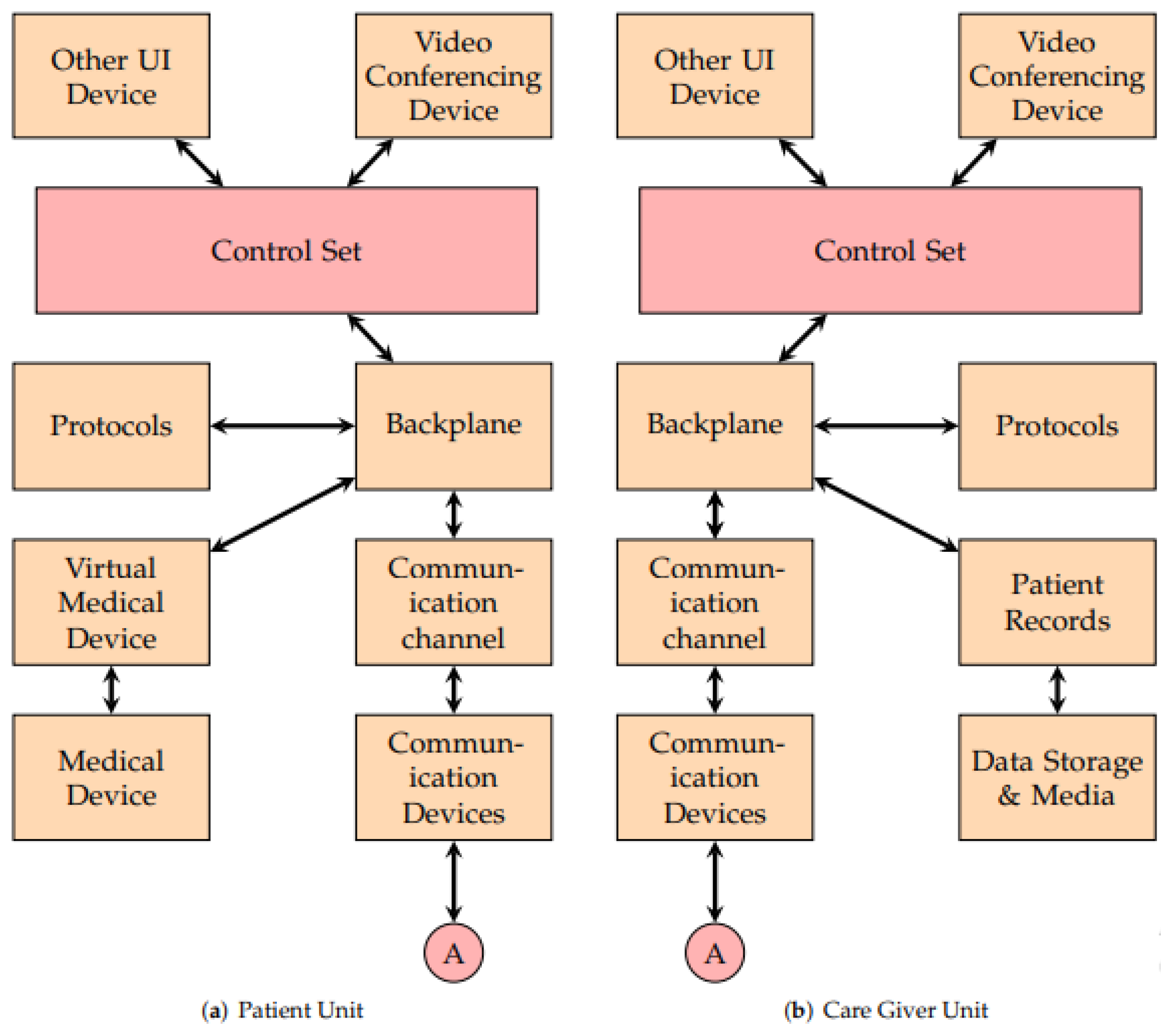
To appreciate the concept of telemedicine and how patients are connected to remote caregivers, Figure 2 provides a helpful illustration. The backplane is the main centre of connection to the other components, while the User Interface and the video conferencing device are linked by the control set to the backplane. Through the backplane, information is transmitted from the patient unit to the care giver unit over the communication channel of the communication device, as well as vice versa. The items represented by the block diagram describe the services, as follows [44]:
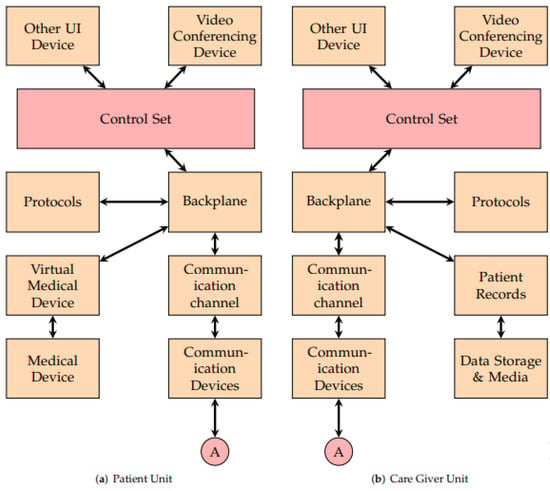
Figure 2.
Block Diagram of Telemedicine System.
- User Interface Device: this is the device that the patient or healthcare provider uses to access the telemedicine system; it could be a smartphone, tablet, computer, or any other device that has an internet connection.
- Communication Device: this device is responsible for establishing and maintaining the communication channel between the user interface device and the virtual medical device; it could be a modem, router, or any other networking device that can transmit data over the internet
- Communication Channel: this is the pathway through which data are transmitted between the user interface device and the virtual medical device; it could be a wired or wireless connection, depending on the type of communication device being used.
- Video Conferencing Device: this is a feature of the telemedicine system that enables live video and audio communication between the patient and healthcare provider; it allows for real-time interaction, examination, and diagnosis
- Control Set: this is a set of rules that governs the transmission of data over the communication channel; it ensures that the data is transmitted in a secure, reliable, and efficient manner.
- Protocol: This is a set of rules that govern the transmission of data over the communication channel. It ensures that that data are transmitted in a secure, reliable, and efficient manner.
- Backplane: this is the backbone of the telemedicine system that connects all the components together; it provides a high-speed and low-latency connection that enables real-time communication and data transfer. The backplane presents two kinds of interface to the system, namely, registry interface and object-supporting interface. The registry interface notes when parts join the system, change their inner state, or leave the system. Protocol components use registry data to find resources required for their activities. The object-supporting interface contains objects that aid local communications.
- Virtual Medical Device: this is a device that simulates the functions of a physical medical device; it could be a software program that runs on a computer or a specialized device that connects to the telemedicine system, and allows for remote examination, diagnosis, and treatment of the patient.
- Medical Device: this is a physical device that is used to examine, diagnose, or treat the patient; it could be a blood pressure monitor, stethoscope, or any other medical instrument that can be connected to the telemedicine system.
- EMR and Data Storage: these are electronic medical records (EMR) of patients stored in the telemedicine system; they include the patient’s medical history, diagnosis, treatment plan, and other relevant information. The data storage component ensures that the data are stored securely and can be accessed by authorized personnel.
3.1. Components of Telemedicine
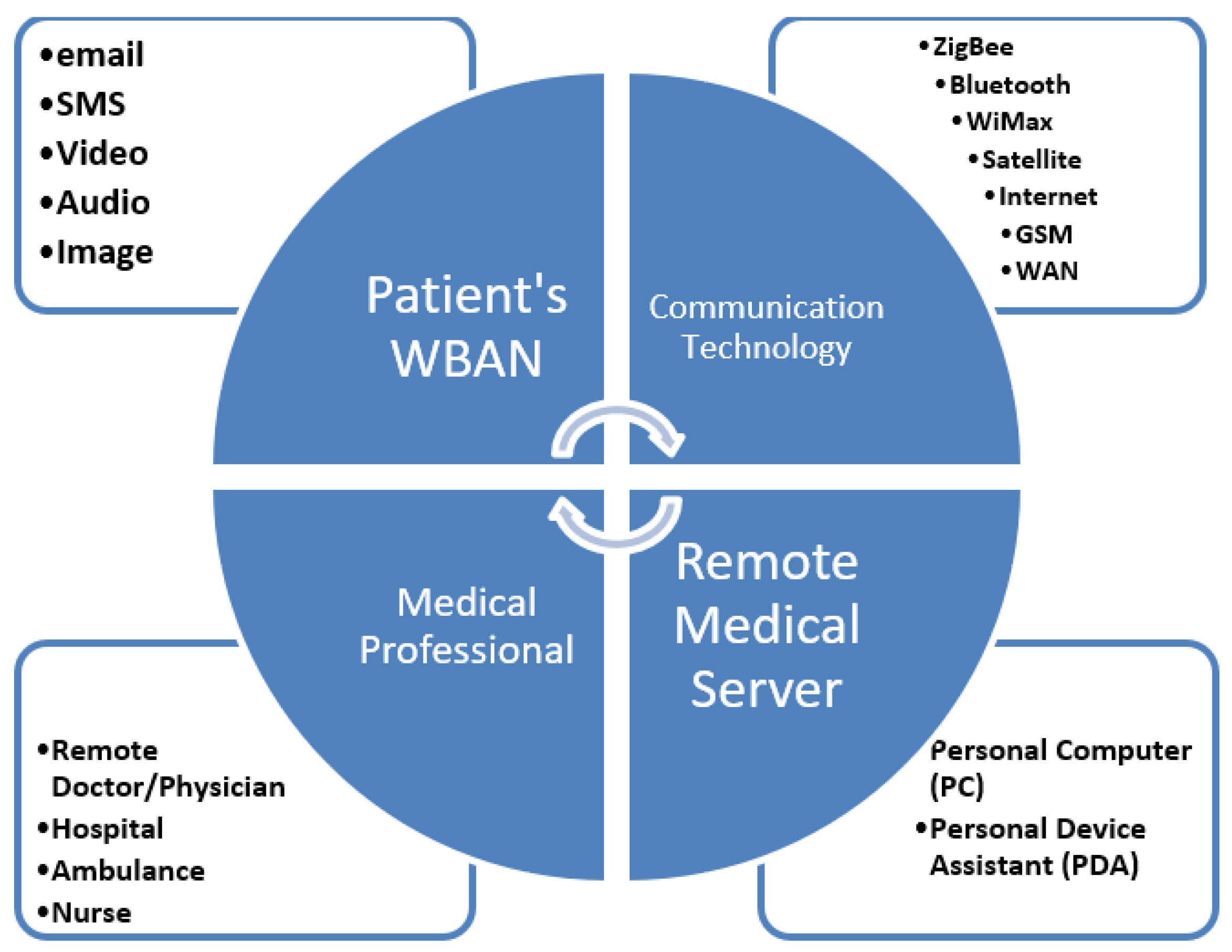
Figure 3 depicts the different parts that constitute a telemedicine system, its the activities and processes, consisting of the care seeker whose data is collected via sensors or through any other means, stored in an Electronic Health Record (EHR) or local server, and transmitted through the telecommunication network to the destination [45]. Among the wireless technologies used for short-range communication between wireless sensors are Bluetooth, ZigBee, and Wi-Fi. Transmission of patient data to a remote caregiver is carried out with long-range communication technologies such as LoRaWAN, internet, GSM, 3G, 4G, LTE, and 5G [19]. The connectivity between components is established by communication protocols during a medical procedure, such as taking the output of a test from a patient to the user interface control for display in a computer or other relevant display device [44]. Telemedicine systems consists of four basic units, which include the patient unit, a communications technology unit driven by one or more wireless communication technologies (such as ZigBee, Bluetooth, WIMax, etc.), the virtual or remote server unit, and the medical professional unit. Together, such systems can improve easy access to specialist health care delivery [46].
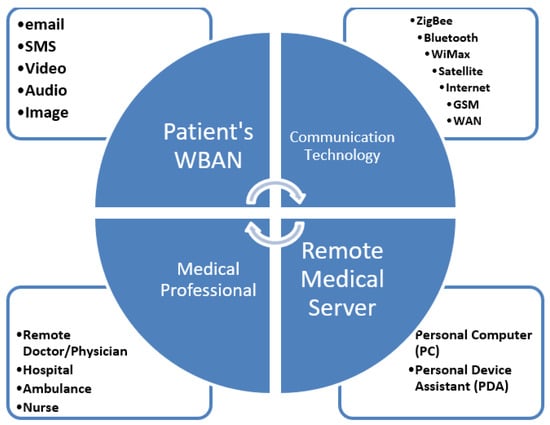
Figure 3.
Components of a Telemedicine System.
3.1.1. Patient’s WBAN Unit
The patient’s WBAN unit comprises the remote patient along with any biosensors, physiological sensors, or external sensors around the patient. These sensors are physical devices used for the collection of vital signs from the patient, and are processed for transmission through the communication unit. These devices have the ability to store and retrieve stored data and to interface with application programs to share acquired data. Sensors for telemedicine are usually of two categories, namely, physiological sensors and environmental sensors. Physiological sensors are wearable or embedded/implanted in the human body. These sensors are designed considering the need for ease of wearing, energy efficiency, data security, standardization, and skin protection. Environmental sensors are those sensors used to measure or collect environmental signals around the patient. Several sensors for collecting physiological signs and measurements of interest for medical prognosis have been identified in previous research, prominent among which are [47,48,49,50,51,52,53,54,55,56]:
- Electrocardiogram (ECG), which records the heart’s electrical signals.
- Pulse oximeter, which records the hemoglobin oxygen concentration in the blood.
- Pulse/heart rate.
- Blood pressure.
- Body temperature.
- Electroencephalogram (EEG), for measuring electrical activity in the human brain.
- Electromyography [57], for the assessment of nerve and muscle cells.
Other sensors used in telemedicine include, as in [19]:
- Photoplethysmography (PPG).
- Electrooculogram (EOG), for eye diagnosis.
- Diet sensors, for monitoring eating patterns and assessing Type II diabetes and coronary heart disease.
- Galvanic Skin Response (GSR).
Environmental sensors include thermometers, accelerometers, motion detectors, GPRS, humidity sensors, weight sensors, gyroscopes, and piezoelectric sensors. Very recently there have been a variety of nano-engineered electrochemical sensors used specifically for COVID-19 diagnosis and management, as discussed in [39], including:
- Field Effect Transistor-based (FET-based) sensors; these are ultrasensitive, and are used to detect Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) antigens.
- Laser-engraved graphene-based immunosensors, which are used o obtain a diagnosis from saliva.
- Nanomaterial-based hybrid sensors for exhaled breath analysis, which enable machine learning-assisted COVID-19 diagnosis.
With respect to WBAN, the provider should have a secure database to securely save patients’ data regardless of whether the telemedicine mode of operation is synchronous or asynchronous, and each user’s data should be uniquely assessed based on authorization and authentication. Such a database usually contains the EHR for proper follow-up, tracking of patients’ progress [58], and management of health issues.
3.1.2. Communications Technology Unit
The communications unit is responsible for providing the interface to the entire system, from transmission of information bits in the physical and datalink layer, to the application layer for connectivity requests, to remote devices, and finally requesting the links or protocol to be used in communication. This unit is central to telemedicine, representing a bridge without which care seekers and caregivers cannot interact. Particularly essential for communication are the short-range and long-range communication systems and the communication protocols.
Short-Range Communication
The vital signals collected by the sensors are transmitted via short-range wireless devices, such as Bluetooth, Wi-Fi, and ZigBee [59,60,61,62], to a local server. A Local Area Network (LAN) can be constructed for networked devices within nearby locations. It is highly desirable that the reach of such communications be spread over a wide locale. A Wide Area Network (WAN) can be established to make connection between a Care Seeker Unit (CSU) and Caregiver Unit (CGU) easier.
Long-Range Communication
Long-range communication is employed to transmit information from the CSU to the CGU. A number of relevant technologies have previously been outlined in the literature. With respect to the type of information intended to be transmitted, choices must be made as to which communications technology is most ideal. The size of the information, its bandwidth requirements, and the cost of execution may provide useful insights during the design of a telemedicine communication network. Long-range communication technologies that have been used in telemedicine include, but are not limited to, satellite, GSM, 3G, 4G, 5G, WAN, LoRaWAN, and internet technologies [29,63,64,65,66,67,68].
Communication Standards and Protocols
A set of rules and guidelines are necessary for consistency and universality in order for the successful transmission and reception of a message or information from the source to the sink for two or more communication devices. Communication protocols and standards include authentication, Error Detection and Correction (EDC), signaling, modulation, and demodulation techniques. Among the common communication protocols are:
- Bluetooth stack of protocols;
- Zigbee stack of protocols;
- Wireless Application Protocol (WAP);
- File Transfer Protocol (FTP);
- Hypertext Transfer Protocol (HTTP);
- TCP/IP;
- UDP.
3.1.3. Remote Medical Server Unit
This unit is where the expert physician or caregiver accesses the desired services remotely for the patient. The patient’s information from the Patient WBAN will have already been transmitted through the communication unit and made accessible to the caregiver. All the transmitted data or information must be received using the same transmission protocol. The information is received and stored in a database, and with the right authentication the physician can access the information for diagnosis. Videoconferencing is widely used in online consultations. Compatible cameras, microphones and other electronic devices and computers are used to assess patient EHRs.
3.1.4. Medical Professional Unit
This unit refers to the personnel that provide the medical or caregiving services remotely, who may include physicians, fospital facilities staff who carry out data interpretation, ambulance staff, nurses, and other healthcare professionals.
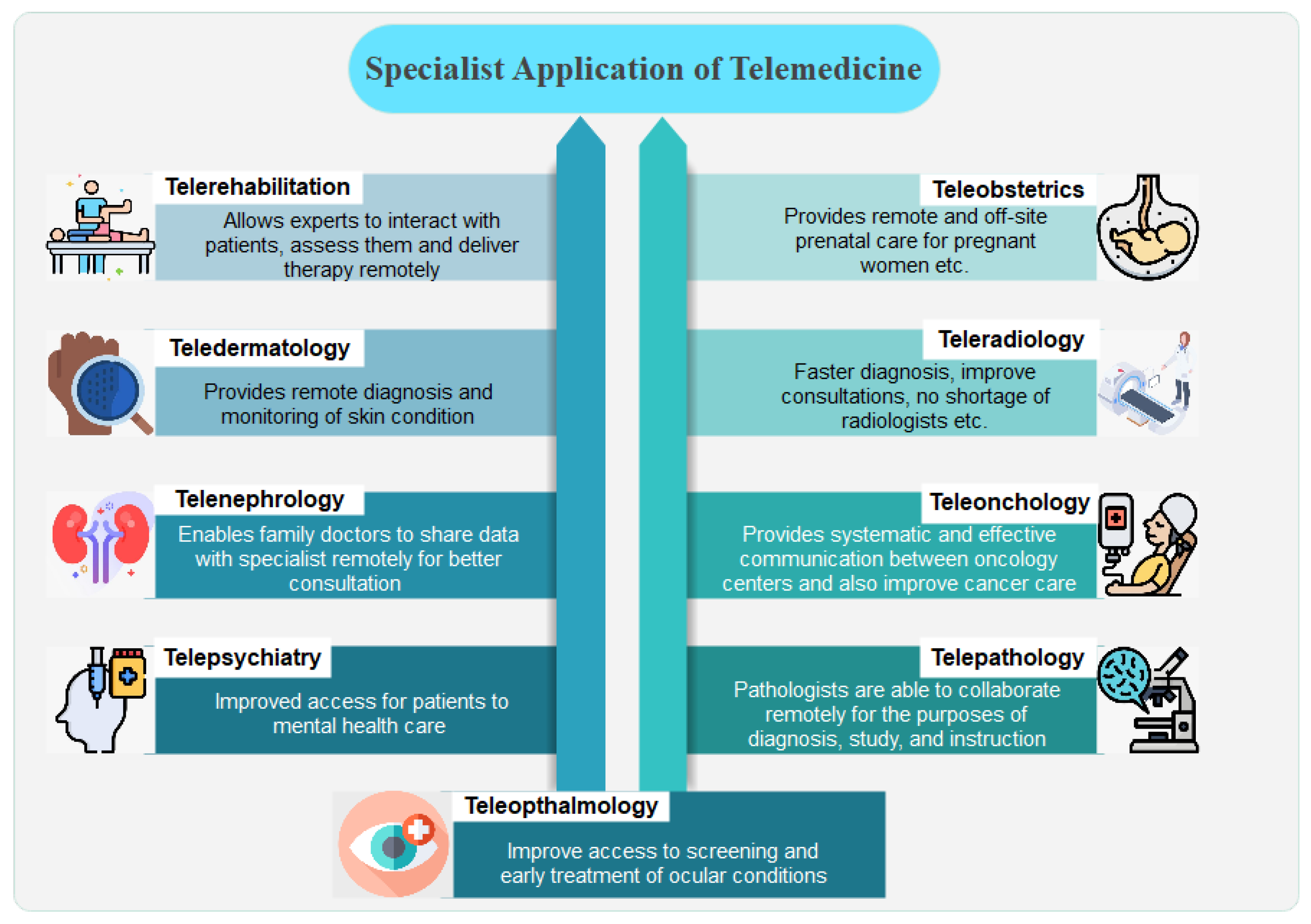
3.2. Specialist Application of Telemedicine
Telemedicine is increasingly being employed in both outpatient clinics and hospitals for a wide variety of medical procedures. Remote consultation with patients or other clinicians (often specialists) is useful in virtually all areas of medicine. Due to care provider shortages, restricted access to specialists, and patients in remote locations, telemedicine has proven to be an invaluable tool for healthcare providers. Early adopters in the field of medicine in certain sub-specialties have been essential in driving the research and development of telemedicine solutions tailored to their needs. This has led to the development of numerous sub-specialties within the field of telemedicine [18]. A number of common application areas of telemedicine solutions are presented in Figure 4 and discussed in the following.
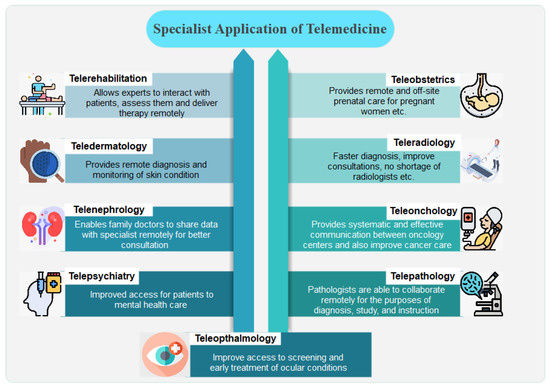
Figure 4.
Applications of Telemedicine.
- Teleradiology: in the field of telemedicine, teleradiology was one of the earliest subspecialties to emerge, having first been used in the 1960s [69]. In order to improve people’s access to radiologists, many teleradiology services have been created. It is quite possible that smaller hospitals around the globe may not always have a radiologist on staff, or may not have access to one at all hours of the day. This means that emergency room visitors, especially those who show up outside of normal business hours, have to wait for a diagnosis. Today, a skilled radiologist can be consulted remotely and quickly by sending a patient’s x-rays and documents to them through a secure teleradiology system [70].
- Telepsychiatry: using telepsychiatry, experienced psychiatrists can treat patients remotely, increasing patient access to mental health care. Psychiatrists are in short supply across many countries, and unlike other medical specialties psychiatry often does not necessitate extensive physical exams.
- Teledermatology: with the help of teledermatology technology, primary care physicians can remotely diagnose skin conditions such as rashes, moles, and other abnormalities. Primary care physicians and nurses are frequently the first in the medical field to recognize a problem and refer patients to specialists. Using teledermatology, high-resolution cameras can relate skin conditions to a remote primary care physicians, who can continue coordinating their patients’ care while providing prompt response as to whether or not a blood sample test examination is warranted.
- Teleophthalmology: using teleophthalmology technology, eye doctors can remotely monitor therapy progress and conduct examinations on patients.
- Telenephronology: telenephrology refers to the practice of remotely consulting a nephrologist; an example of an inter-professional application of telenephrology solutions is the case of a family doctor who requires a specialist opinion concerning a patient who has kidney disease.
- Teleobstetrics: through teleobstetrics, gynecologists can provide prenatal care to expectant mothers from afar; as an example, a doctor at one facility could film an ultrasound of a baby’s heart and send it to an obstetrician in another location for analysis.
- Teleonchology: with the goal of making cancer treatment more accessible, teleoncology has grown rapidly in recent years; among the different teleoncology technologies are store-and-forward mechanisms that transmit images for diagnosis and real-time video platforms that enable oncologists to consult with patients.
- Telepathology: through the use of telepathology technologies, pathologists are able to collaborate remotely on pathology cases for the purposes of diagnosis, study, and instruction; many telepathology solutions are “save and forward” systems that let pathologists send and receive high-resolution images and videos.
- Telerehabilitation: telemedicine allows healthcare providers to remotely provide rehabilitation treatments such as physical therapy to those who need them.
3.3. Benefits of Telemedicine
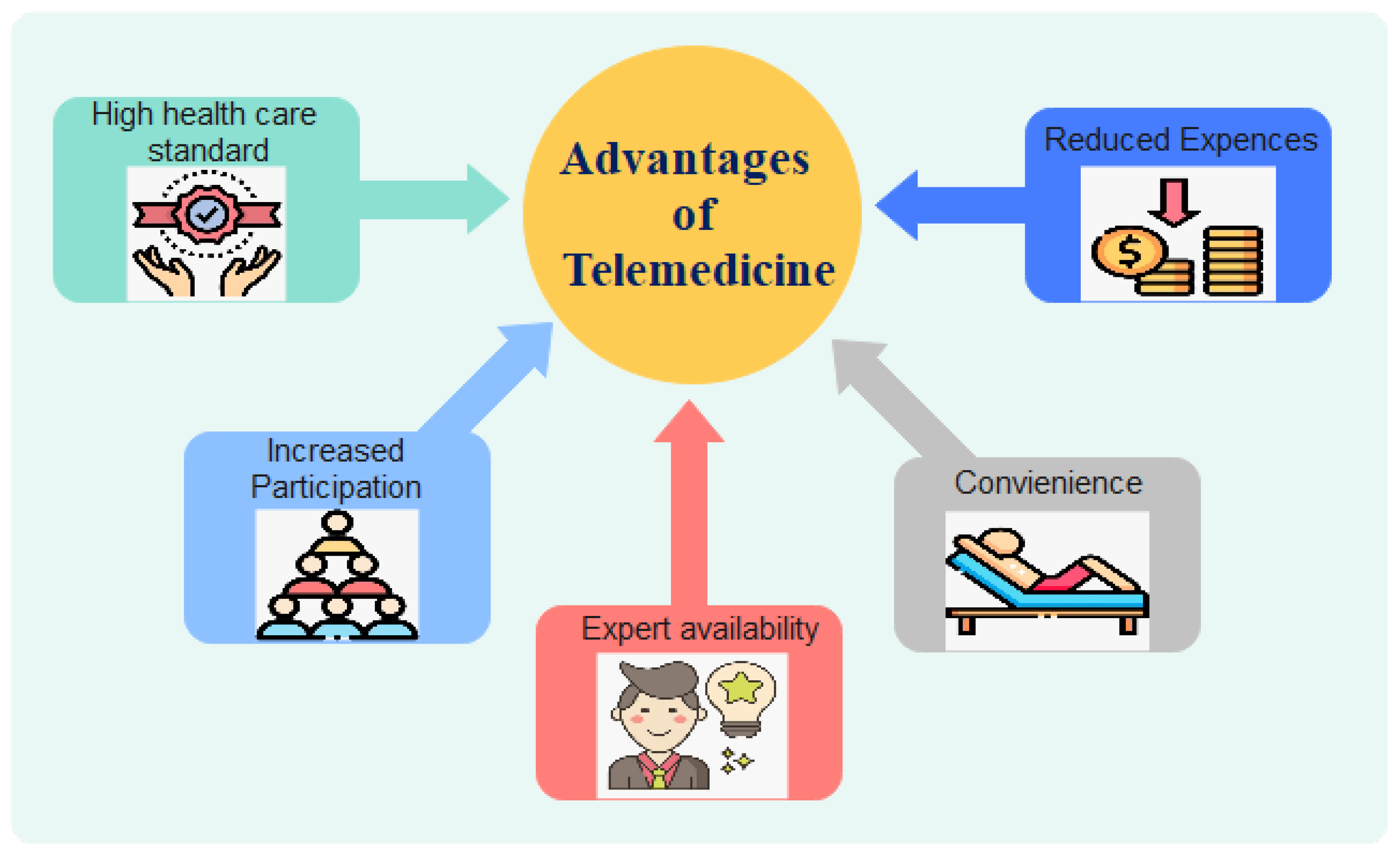
Telemedicine is anticipated to become pervasive within the very near future, and could lead to major advancements in the medical and engineering fields. Telemedicine creates new viable opportunities for efficient medical diagnoses, which will require drugs and equipment manufacturers to adopt new strategies to meet the resultant rising demand [71]. Telemedicine generally has positive outcomes. It enables more people, especially those who live in under-served or rural areas, to receive the high-quality medical treatment they deserve. Telemedicine is a method of interacting with the connected patients of today while reducing healthcare costs, and may lead to significant improvements in the current system of providing medical care. The near-future potential of telemedicine is discussed in this subsection and summarized in Figure 5.
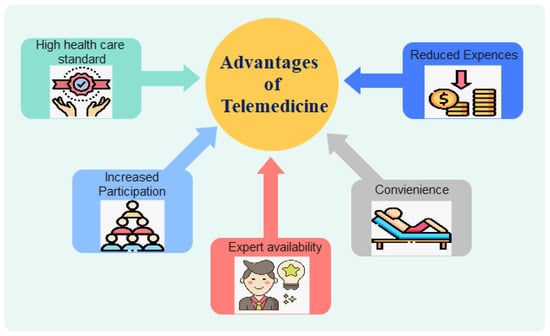
Figure 5.
Advantages of Telemedicine.
- Improved Patient Access and Convenience: the primary motivation behind the development of the telemedicine sphere is the desire to provide patients with easier access to high-quality medical care. The United States is widely credited as the birthplace of telemedicine, where it was established to fill the gap in medical care in under-served areas, particularly rural outposts [72]. Today, telemedicine is used all around the world, whether to provide primary care to residents of developing nations or to help an older patients with mobility challenges receive the medical attention they need without leaving the house. In addition to removing the restrictions that distance and time usually place on receipt of medical attention, telemedicine has the potential to streamline the entire healthcare delivery process for patients.
- Reduced Medical Expenses: every year, the United States spends more than any other developed country on healthcare, at nearly USD 2.9 trillion. [73]. Moreover, it is anticipated that almost USD 200 billion of these costs are wasteful and unnecessary expenditures. Because of its potential to improve the efficiency of regular healthcare appointments and reduce wasteful spending on items such as emergency room visits and drug refills, telemedicine has the potential to significantly reduce the national healthcare budget.
- Improving the Availability of Expert Advice: one of the most immediate benefits of implementing telemedicine into a medical facility or practice is the increased availability of subspecialists. This paves the way for primary care physicians to confer with medical specialists on a patient’s condition and for patients to see a required specialist regardless of their location. In addition, telemedicine allows X-Ray examinations to be outsourced, which is particularly useful for small hospitals that do not have a full staff of radiologists [72].
- Increasing Patient Participation: with the use of telemedicine, patients can maintain regular contact with their physician at their own convenience, which increases their level of involvement in their own care. In this way, the doctor–patient relationship is strengthened and patients have a greater sense of control over their health care.
- Higher Standard of Care for Patients: follow-up care is facilitated by telemedicine, as it allows doctors to check in with patients remotely to ensure their health and well-being. Better treatment outcomes are achieved through the use of telemedicine, whether through a more comprehensive remote patient monitoring system to check the patient’s heart or through a video chat that can answer queries about medication after hospital discharge.
3.4. Forms of Telemedicine
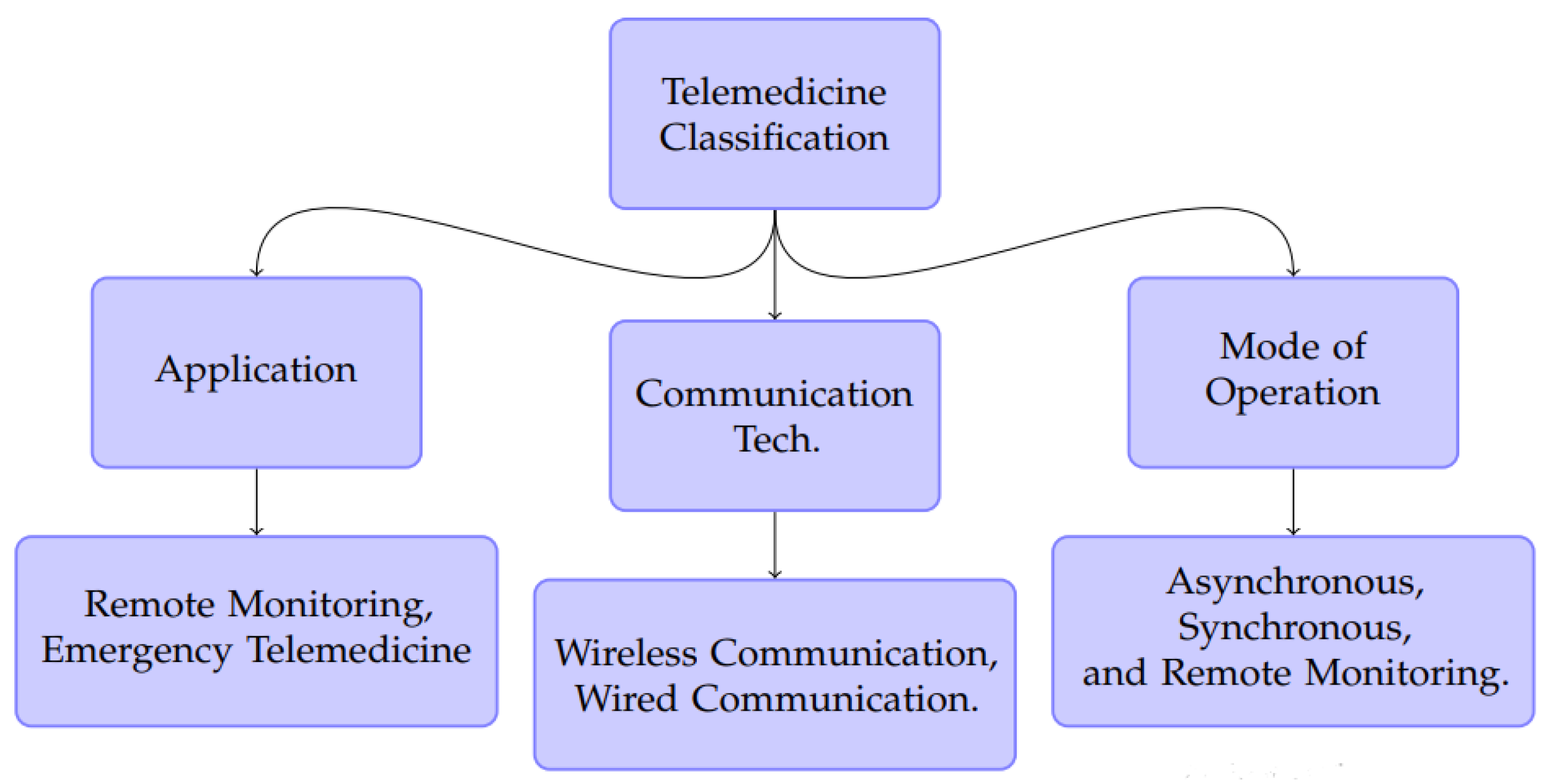
Telemedcine can be classified based on three considerations: the mode of operation, the communications technology employed, and the specific application area. Figure 6 shows the various classifications of telemedicine.
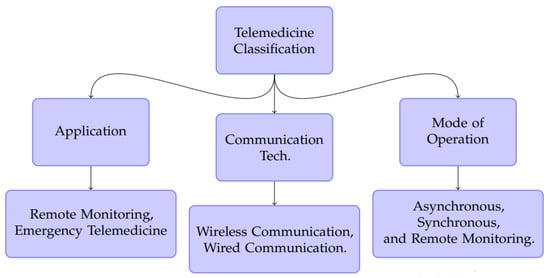
Figure 6.
General classification of Telemedicine.
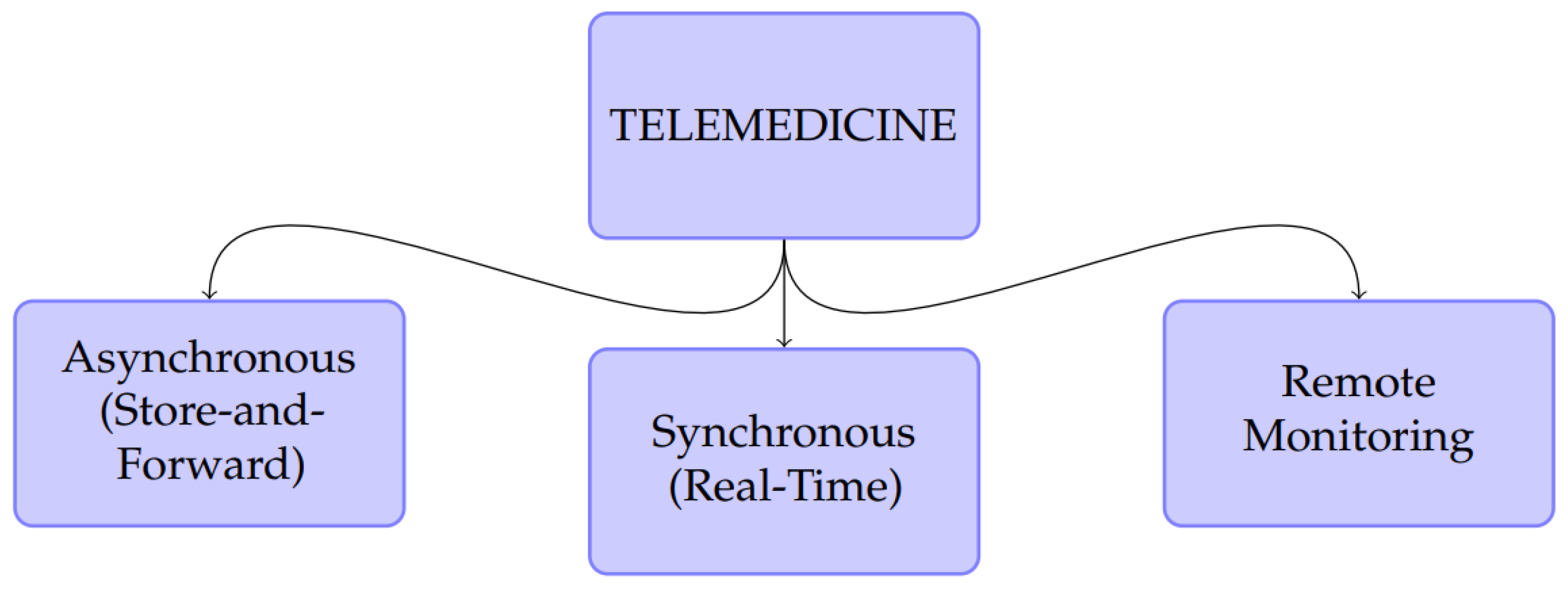
When considering mode of operation, researchers in the field of telemedicine have typically classified telemedicine into two main classes, namely, real-time and store-and-forward telemedicine [71,74,75,76,77]. In the research of [3,78], telemedicine was classified into two modes of operation, store-and-forward and two-way Interactive Television (IATV). Alternatively, [4,43,79,80,81] classified telemedicine into three classes: online/real-time, store-and-forward and remote health monitoring telemedicine. Adopting the three-class classification, Figure 7 depicts the forms or categorisation of telemedicine based on mode of operation.
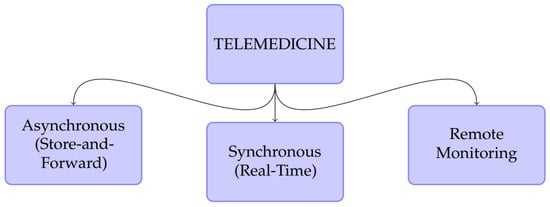
Figure 7.
Forms of Telemedicine Based on Mode of Operation.
3.4.1. Asynchronous Telemedicine
Asynchronous telemedicine, sometimes referred to as store-and-forward telemedicine, is a method in which physiological data captured from the patient are conveyed to medical experts based on a request for offline assessment [4,63,65,75,81,82,83,84,85]. It includes online storage and access of medical records by medical personnel. Because it uses low bandwidth, the cost of the process can be reduced. One major drawback of this method is the absence of any means of consultation between the patient and the doctor, which by implication may lead to wrong interpretation and diagnosis. Furthermore, it requires distribution of the patient’s medical history and data, which may incur security and privacy concerns. Dermatologists, radiologists, and pathologists most typically employ asynchronous telemedicine [43].
3.4.2. Remote Health Monitoring
Remote monitoring is a process of continuously monitoring patients with chronic diseases or specific conditions by means of various communication devices. This method is usually employed to monitor ailments such as heart disease, diabetes, and asthma. As it serves as an alternative to the intensive care unit (ICU), it can reduce post-operative costs [81]. This method enables real-time monitoring of patients outside of conventional medical facilities while they carry out their normal activities. This method is achieved by deploying wearable devices that monitor vital signs, acquire data, and transmit the data to a monitoring unit for remote diagnosis. This approach offers great advantages in terms of patient mobility and the ability to perform routine activities while monitoring patients for any health emergencies [43].
3.4.3. Synchronous Telemedicine
This method, sometimes known as interactive telemedicine services, consists of several contacts between patient and doctor, including phone calls, online diagnosis, and communications. It involves the collection and transmission of physiological and clinical data as well as medical images to a specialist for real-time online diagnosis [43]. Interactive telemedicine can be used to conduct physical examinations as well as psychiatric and ophthalmological assessments [81].
4. Evolution of Communications Technologies for Telemedicine
Communication technologies for telemedicine implement the transfer of captured data from sensors placed on the human body, and can be configured to form sensor network systems. The development of communications technologies has greatly aided the evolution of telemedicine. The invention of the electrical telegraph and Plain Old Telephone Service (POTS) has been linked with the beginning of modern telemedicine. With the electrical telegraph, medical information could be transmitted as text more easily and speedily than sending a letter by mail, which used to be the alternative means of communicating. The telegraph was first used in the medical context by the military, in teleconsultation, ordering of medical supplies, and as a means of transmitting other health information.
Communication technology further developed beyond the use of the POTS, which merely provided audio services. Over the years, communication in telemedicine has progressed from wired technology to wireless technology [86]. The introduction of Public Switched Telephone Network (PSTN), Integrated Services Digital Network (ISDN), and Voice over Internet Protocol (VoIP), all of which have the capabilities of transmitting data and voice over telephone lines, have enhanced telemedicine tremendously. Moreover, these technologies have very good transmission data rates; for instance, ISDN can provide a data rate of 128 kbps. The advent of the internet has led to a massive increase in information flow. The sudden rise in internet patronage in the 1990s provided a massive boost to telemedicine services and applications. The use of the internet has given rise to cloud computing, fast and reliable transmission of medical information, and videoconferencing.
4.1. Communication Network Links for Telemedicine
How exactly are telemedicine technologies made available to users, and what kinds of technological advancements make it possible to establish digital links between a healthcare physician at a large hospital and a patient residing in a remote rural home? Because of the proliferation of the internet, the manner in which telemedicine is provided has evolved in many ways. Patients who live in rural or otherwise inaccessible places can now take part in at least some forms of telemedicine thanks to the widespread availability of affordable high-speed internet connections. This subsection discusses the two communication network links that can be used to drive telemedicine, namely, point-to-point and point-to-multipoint communication links.
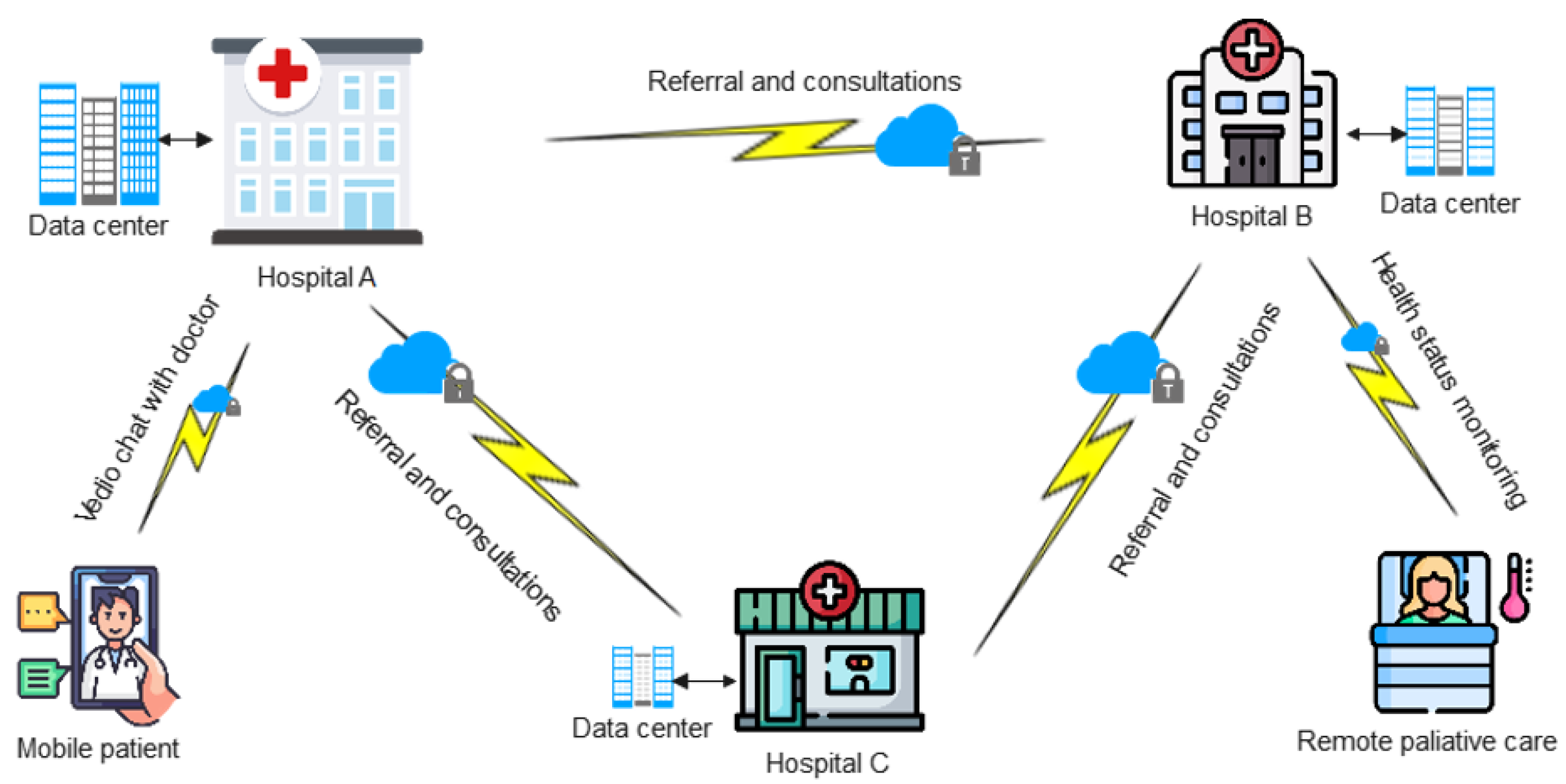
4.1.1. Point-to-Point Links
Through the use of point-to-point connections and high-speed internet, small remote health centers can be connected to larger health facilities. By utilizing this specific type of telemedicine link, medical care can be remotely outsourced to specialists located in other locations, and connected referrals can be made to these specialists. This is particularly useful for medical facilities that are either understaffed or have a smaller patient population. Mobile patients have the opportunity to establish contact with specialists for teleconsultations using this connection. Similarly, aged patients have the option of receiving palliative treatment in the comfort of their own homes while having their current health state remotely monitored. For telepsychiatry, teleradiology, and other urgent care services, point-to-point links are the norm. Figure 8 shows a typical network topology for point-to-point telemedicine connections.
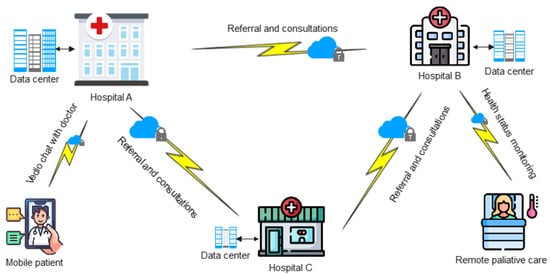
Figure 8.
Point-to-Point Links.
4.1.2. Point-to-Multipoint Links
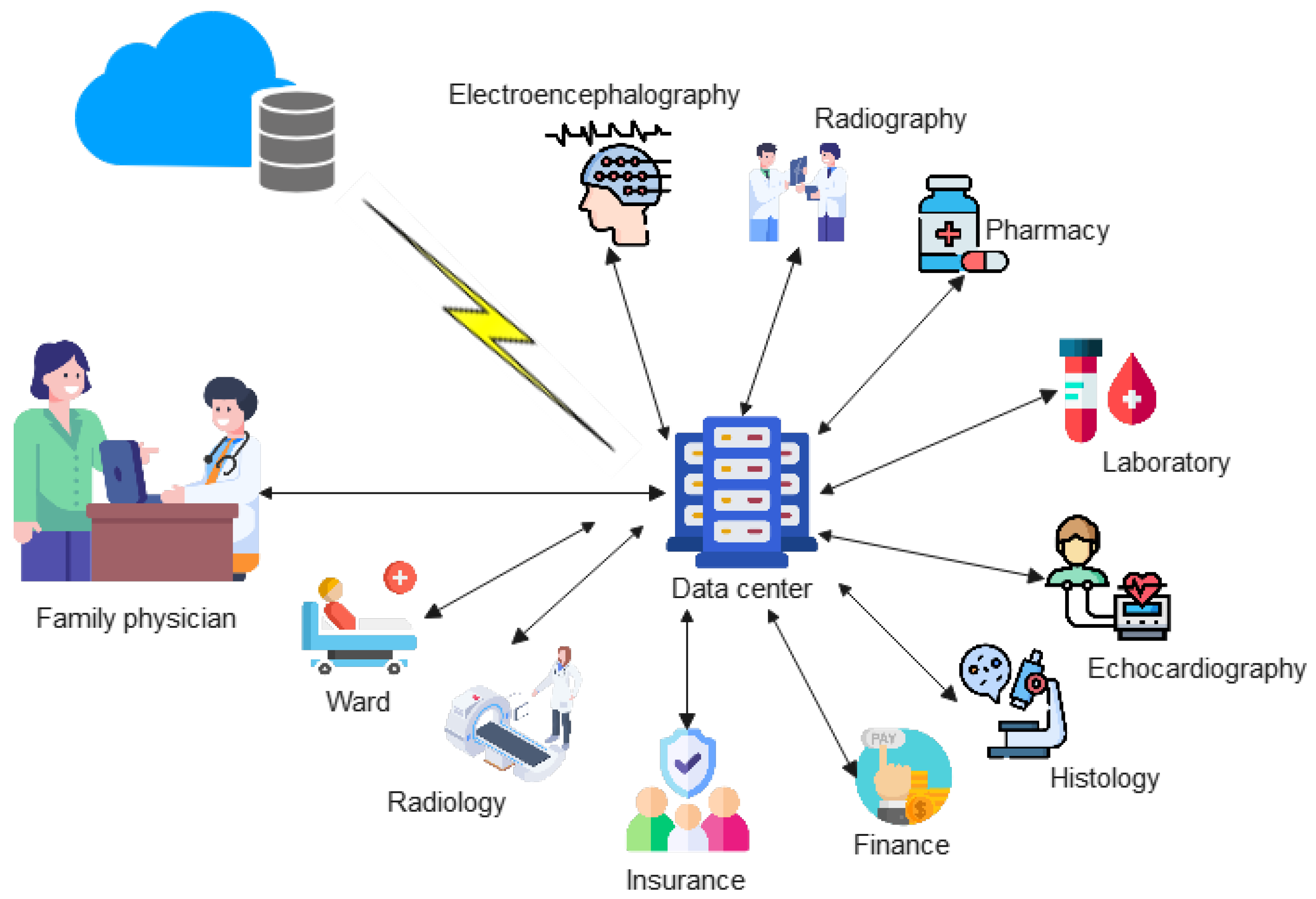
Point-to-multiploint links enable every department in a healthcare facility to be connected to a central hub (the datacentre) for seamless communication and healthcare service delivery (see Figure 9). By way of illustration, a primary care physician can utilize this link to initiate a test for a patient in the radiology department and obtain the result electronically. The same physician can provide authorization for the pharmacy to dispense drugs to a patient while at the same time the finance unit takes the necessary funds from the patient’s wallet for services rendered. In the same vein, telesurgery can be performed on a patient simultaneously by a number of surgeons from different locations via this link. This link can be implemented within a single health facility using an intranet connection for high speed and data security. However, in the event of telesurgery, which requires the participation of a specialist located at a distant healthcare center, a high-speed internet connection that is supported by a fiber optics network is helpful.
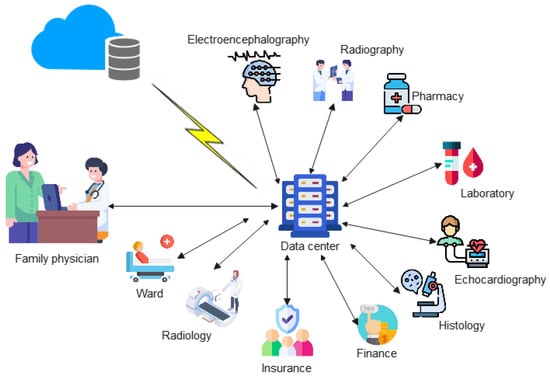
Figure 9.
Point-to-Multipoint Links.
4.2. Classification of Communication Technologies in Telemedicine
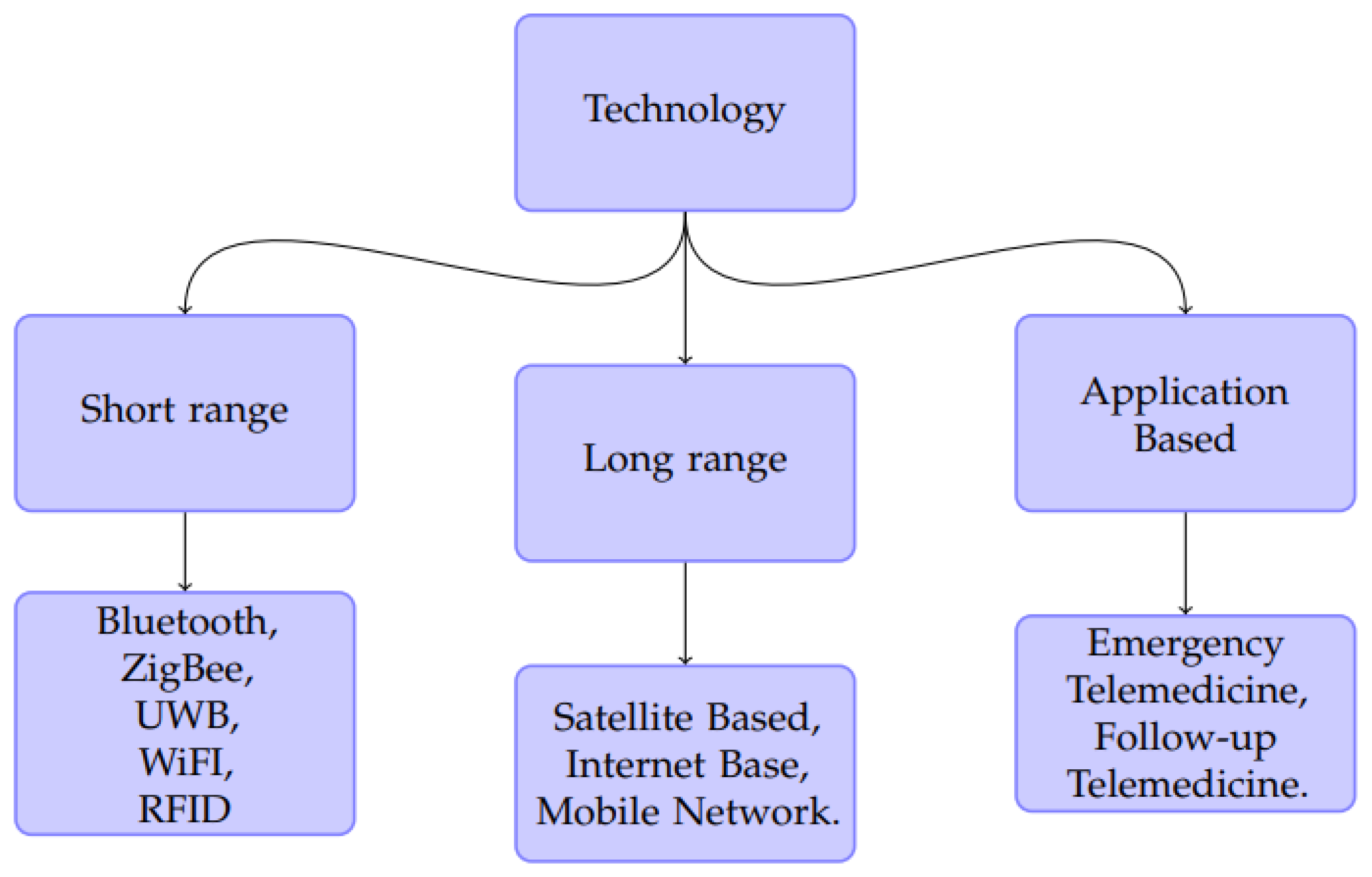
Communication technologies for telemedicine can be broadly classified into short-range communications such as Bluetooth, Wireless Fidelity (Wi-Fi), Zigbee, and Ultra-wideband (UWB), long-range communications such as satellite-based, internet-based, and mobile cellular network, and Wide Area Network (WAN), as shown in Figure 10.
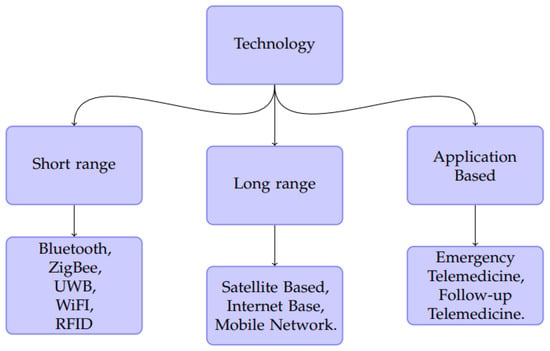
Figure 10.
Classification of Communications Technologies used in Telemedicine.
4.3. Short Range Communication Technologies
Telemedicine involves remote collection of human vital information; this can be carried out by establishing sensor network systems on the human body. This sensor network can be coupled with short-range communications technology to form a Body Area Network (BAN). A BAN is a network consisting of distributed nodes placed on the body to acquire physiological data [4].
The typical issues to consider in implementing wireless BANs (WBANs) include the sensor type, data management, routing method, quality of service expectation, communication path, standard/technology, security, and simulation environment [4]. The initial WBANs had low bandwidth requirements, with data rates between 10 kilobits per second (kbps) to 10 megabits per second (Mbps) [4]. The most popular short range communication technologies to achieve the telemedicine system are Bluetooth, Zigbee, Wi-Fi, and UWB. In [87], the implementation of a medical monitoring system comprising sensor communication technology was described. The communication protocols used for the communication aspect were Bluetooth and ANT/ANT+, while WebSocket technology was used to establish the connection between the mobile client and remote server. In [88], the authors presented a telemedicine system with a network that utilised an optical fibre backbone. WBANs were used for vital sign collection with the aid of the sensor nodes. The network was set up with nodes arranged in clusters, and each microcontroller in a cluster was connected to a sink which could predict the disaster parameters for a particular individual. The sensor network relayed the aggregated data remotely to doctors via the internet.
4.3.1. Bluetooth Low-Energy (BLE) Communication
Bluetooth is one of the most popular wireless technologies, enabling connectivity with other compactible devices for effective communication. It operates at the 2.4 GHz frequency in the ISM Frequency band. It is a low-cost and low-power device that supports wireless voice and data transmission to devices at different data rates, reaching up to 2 Mbps (BLE 5.0) depending on the version (whether fixed or mobile within a 10 m range for Bluetooth and over 240 m for Bluetooth 5.0 [89,90]). The communicating BLE devices are automatically set up in a network known as a piconet [65,82,89,91,92,93,94,95,96], where the maximum number of connected devices is eight; alternatively, a scatternet [65,82,94,96] can be used for more than eight connected devices. Bluetooth 4.x and Bluetooth 5.0 use star-bus and mesh network topologies, and can support an unlimited number of nodes [97]. Different versions of Bluetooth are currently available for use based on application requirements. Table 2 shows basic technical information on different Bluetooth versions and other related wireless communication technologies. BLE has been applied in telemedicine and reported in several studies. For instance, in [98] it was used in an ECG monitoring system. BLE 4.0 was used along with Wi-Fi and an IOS mobile application to display the results on a mobile phone in a telemedicine application. The ECG signal collection module of the biosensor acquired the ECG signal from the patient, the BLE 4.0 transmits the data to the mobile app in the mobile phone, and the Wi-Fi embedded in the mobile phone transmitted the data to the provider database for use by an authorized physician. In [89,99], the authors demonstrated the use of BLE in data transmission in a BAN. The work of [89] showed that BLE has a better energy consumption for data traffic in a BAN sensor compared to ZigBee.

Table 2.
Technical Comparison of Bluetooth versions and other Wireless technologies [99].
BLE continues to gain more acceptance in telemedicine applications. Among the reasons for this increasing acceptance are:
Merits:
- Frequency hopping: BLE uses adaptive frequency hopping (AFH) as a technique for media access. This means that BLE devices are sensitive to other nearby wireless networks and continuously change their channels to mitigate or reduce interference. Data transmission is hardly ever interrupted, as Bluetooth devices can determine which channels are occupied and use the available channels in the hop sequence.
- Number of nodes: Bluetooth devices can have unlimited active slave connections. Older versions of Bluetooth have a maximum of seven slave nodes, making for a maximum number of eight connections when the master is counted. As can be seen in Table 2, Bluetooth 4 and Bluetooth 5 can support unlimited nodes.
- Cost efficiency [100]: BLE is optimised for devices that use small batteries due to the reduction of the number of channels from 79 channels ay 1 MHz to 40 at 2 MHz.
- Low power consumption: BLE has been developed taking into consideration the minimisation of power requirements, especially when comparing newer Bluetooth versions to older ones.
- BLE is easy to integrate into networks.
- It has a relatively more secure connectivity than Wi-Fi connections.
Demerits:
The major downsides of Bluetooth technology lies in older versions, and have been appreciably addressed in BLE and Bluetooth 5.0. Issues with past versions include:
- High power consumption;
- Frequent connection or pairing loss;
- Non-automatic support of network formation.
Fortunately, these have been taken care of with the introduction of BLE.
4.3.2. ZigBee
ZigBee is another low-cost and low-energy consumption standard-based wireless short-range communication technology. It operates at 2.4 GHz within the ISM band (868 MHz in Europe and 902–928 MHz in North America). It uses the IEEE 802.15.4 standard, which uses 128-bit Advanced Encryption Standard (AES) for secure data transfer between ZigBee sensors and networks. The method of media access is CSMA/CA, and it uses mesh topology for networking. Zigbee has successfully been implemented in several research works, as seen in [49], where the authors used a ZigBee-based ECG monitoring system to acquire patient data for forward transmission to a remote base station for telemedical usage. Other articles on the use of ZigBee communication include [59,60,62,93,100,101,102]. The strengths of ZigBee technology include:
- Low latency;
- High data security;
- Collision avoidance and retransmission, ensuring more reliable data transmission;
- Support for multiple network topologies, such as point-to-point, star, and mesh topologies;
- Support for unlimited nodes in a network;
- Scalability;
- Low energy consumption;
- Ease of implementation;
- 128-bit AES encryption ensures data security.
4.3.3. Ultra-Wideband (UWB)
UWB is a short-range wireless technique for fast and reliable data transmission, and provides large bandwidth. It is based on the IEEE 802.15.3 standard. It operates in the unlicensed frequency band of 3.1 GHz–10.6 GHz [103] of the electromagnetic spectrum. It has good energy efficiency and throughput, which this makes it a choice technique for use in Wireless Body Area Networks (WBAN) for remote patient monitoring. A longer sensor operational life and even greater data transmission rate (up to 500 Mbps for 2 m range and 110 Mbps for 10 m range) are enhanced by the lower energy usage. Its use case was demonstrated in the design and implementation by [103] in a textile UWB wearable antenna. The Specific Absorption Rate (SAR) on the human skin was found to be 1.68 W/Kg, which is within safe limits to avoid radiation effects. Other works on UWB technique include in [26,92,100,104,105,106,107,108].
Types of UWB
- Multi-band (MB) Optical Frequency Division Multiplexing (OFDM) UWB.
- Impulse Radio (IR) UWB.
IR-UWB is suitable for WBAN, as it has low complexity, lower energy demand, and operates with a very short pulse duration, on the order of 2–3 ns. However, it has drawbacks due to the complexity of the front-end circuitry design.
4.3.4. Wi-Fi (IEEE 802.11)
This is a wireless communication technique is based on IEEE 802.11 standard. Similar to other short-range communication technologies discussed earlier, it uses the ISM band. The two frequencies most often used are 2.4 GHz and 5 GHz, depending on the required application. A new version of Wi-Fi, known as Wi-Fi 6, uses the 6 GHz frequency. In telemedicine applications, the Wi-Fi network usually comprises multiple access points, with medical sensor nodes moving freely within access points [107]. Wi-Fi or WLAN can be used along with WBAN to transmit biosignals to a nearby server and then to the internet.
The authors of [31] demonstrated a WLAN/IEEE 802.11n standard transmission scheme for wireless telemedicine applications. Their WLAN system transmits measured medical data using digital bits, ECG signals, case histories, and audio/video signals for telemedicine purposes.
Drawbacks:
A major drawback of Wi-Fi is the issue of data security, as data are broadcast wirelessly to nearby compatible devices. According to research, several security threats are associated with Wi-Fi networks due to their use of an open medium to transmit and receive data. Threats which can be detrimental in medical diagnosis contexts include denial of service, eavesdropping, and services theft [31].
4.3.5. Radio Frequency Identification (RFID)
RFID is a wireless technology that uses different frequency bands from both licensed and unlicensed (ISM band) bands. The different carrier frequencies used for RFID are:
- 125–135 KHz (Low Frequency)
- 23.56 MHz (High Frequency)
- 868–930 MHz (Ultra-High Frequency)
- 2.45 GHz (Microwave Frequency)
- 5.8 GHz (Microwave Frequency)
The two components that make up an RFID device are:
- A reader
- A tag
The reader has one or more antennas, which are used to emit radio waves, while the RFID tag is used to receive signals. RFID technology has been used for various applications, such as patient tracking and monitoring. The major drawbacks, as hinted at by [16,21], include the high cost of adoption, patient privacy and security issues, and Electromagnetic Interference (EMI) between RFID tags and other biomedical sensors.
4.4. Long-Range Communications
In all types of telemedicine approaches, whether in store-and-forward, remote monitoring, or real time telemedicine, patient information or data are usually transmitted to a physician or caregiver in a distant or remote location. Various technologies exist for remote communication, with varying capacities and ranges. One of the most widely used communication technologies in telemedicine is satellite communication, which has the major advantage of world-wide reach [87]. Other technologies include Global System for Mobile (GSM), internet, and the Wireless Area Network (WAN) communication.
4.4.1. Satellite Communication in Telemedicine
One of the most effective communication technologies in telemedicine is satellite communication. Satellite communication provides Broadcast Satellite Services (BSS), Fixed Satellite Services (FSS), and other telecommunication services, as well as Global Positioning System (GPS) services. It has the major advantage of world-wide reach. A useful benefit derived from satellite communication in telemedicine is access to broadband services in areas where other telecommunication services are inadequate or outright unavailable [87]. Satellite-based communication involves the transmission and reception of radio waves between a satellite launched into orbit and a base station on the ground. Geostationary Earth Orbit (GEO) satellites have near-global coverage, broadcast/multicast capability, and great capacity for use in telemedicine, especially in the rural areas where terrestrial communications are unavailable. However, this has a trade-off in terms of high end-to-end latency, between 1700 ms to 3000 ms for GEO satellites [109]. Communication from the base station uses an uplink frequency; the radio waves are transmitted to the transponder of the satellite, and communication occurs via uplink/downlink frequencies. Table 3 shows the uplink and downlink frequency bands for satellite communication. Each satellite frequency band has several transponders used for different applications.

Table 3.
Satellite Band Uplink and Downlink Frequencies.
In [2], the authors used satellite communication in a store-and-forward telemedicine system. A wireless internet protocol was used to transmit data through a Very Small Aperture Terminal (VSAT) satellite system. The C-band of the satellite communication was used in their work for both audio and video data transmission. In a review article [29], satellite communication was used in telemedicine communication. The Chinese military used satellite channels to establish telemedicine communication to two hospitals in different locations. In [87], the authors described useful benefits derivable from satellite communication in telemedicine, such as access to broadband services in areas where other telecommunication services are inadequate or wholly unavailable. In another article [38], satellite communication equipment was housed in a van and two-way online data transfer was used to transmit scanned patient information to specialist doctors for provision of telemedicine services.
Very Small Aperture Terminal (VSAT)
VSAT is a form of an earth station often used to communicate with satellites. In [2], a wireless internet protocol was used to transmit data through a VSAT satellite system in a store-and-forward telemedicine system. C-band satellite communication was used for both audio and video data transmission. Other bands that can be used include the Ku-band and Ka-band satellite communication frequencies. The uplink/downlink frequencies of a number of satellite frequency bands are summarized in Table 3.
In [29], the Chinese military used satellite channels to establish telemedicine communication between two hospitals in different locations. In a similar article [38], the authors highlighted satellite communication equipment housed in a van, with two-way online data transfer used to transmit scanned patient information to specialist doctors for telemedical services.
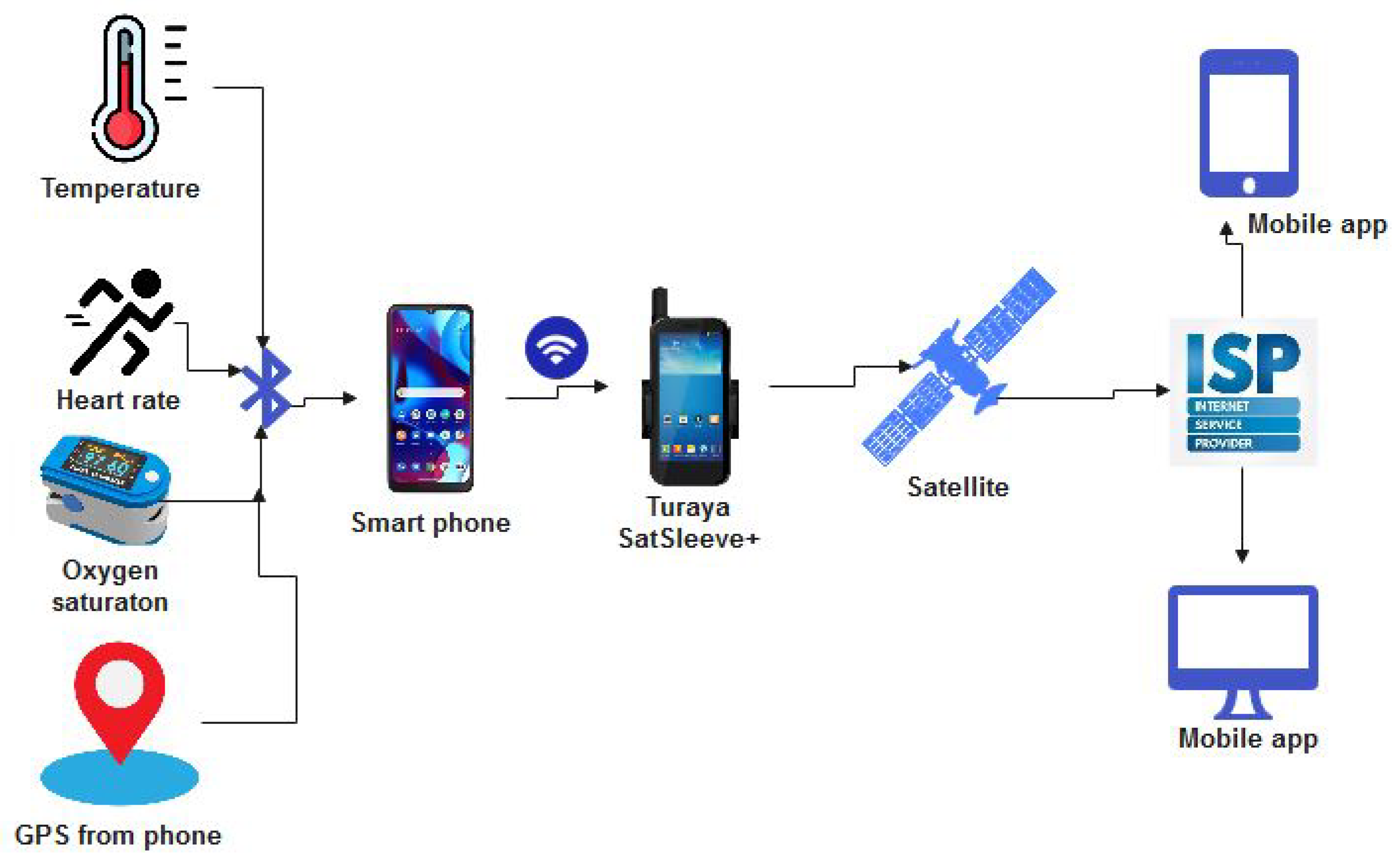
Thuraya Satellite Phone
The Thuraya satellite phone has been successfully utilised to break the communication barrier in certain unusual scenarios in which communication is otherwise impossible. The Thuraya phone is designed with the functionality of transmitting and receiving directly from a satellite. The phone has been made to integrate with terrestrial communication using a dual-SIM Thura phone. The first dual-SIM dual-mode Thuraya was the Thuraya XT-PRO DUAL, which used a satellite SIM card and a GSM SIM card to exploit communication services based on both technologies. Thuraya phones have been used in telemedicine systems, as reported in [109]; Figure 11 illustrates the use of the Thuraya phone for telemedicine.
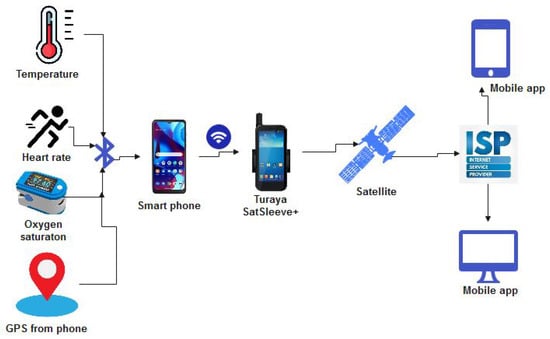
Figure 11.
Use of Thuraya Phone for Telemedicine.
4.4.2. Internet-Based Communication in Telemedicine
Internet-based communication in telemedicine has previously been presented in [29], comprising a teleconsultation system and an online medical information system. The network was used to connect medical specialists, devices, and data within various sites using the internet. The use of low bandwidth communication employed by the system was, however, noted to limit the high-volume transmission of medical data.
The authors of [81] developed a prototype internet-based telemedicine system that establishes an audio-visual connection as well as a data path from the client’s home to the care-giver through a web browser interface. The developed data path was able to provide other diagnosis functions as well, such as the use of an electrocardiogram, blood pressure, respiration, body temperature, and stethoscope.
In [110], a wireless IP network that provided voice communication as its basic service was reviewed. The internet-based system converts analogue voice signals into digital data, compresses and segments the data into packets, adds an IP address, and then enables distribution over the wireless IP network. Because the system is internet-based, normal PCs and other devices can easily be connected through the use of TCP/IP addresses. The system provides multimedia communication services such as data, audio, video, and imaging for telemedicine applications.
Although 3G and 4G communications are able to support video conferencing in telemedicine, medical image transmission has been shown to create nodal delay when using the internet [80]. To mitigate this effect, the authors designed a parabolic dish antenna that supports fast communication using the internet for telemedicine communication.
4.5. Mobile Networks
The advancement of mobile communications technology from the second generation (2G) to the fourth generation (4G) and beyond has brought about its widespread adoption of telemedicine. The authors of [111] opined that the evolution of 3G and mobile technologies will be the main propelling force for the future development of telemedicine. 2G mobile communication used Time Division Multiple Access (TDMA); next, General Packet Radio Service (GPRS) came online making possible a 115 kbps data rate [111]. In, [74], the authors proposed transmission of patients’s relevant physiological signs to a remote server using the GSM/GPRS network. As highlighted by [63], using GPRS may not be the best option for communication with a remote server; especially when high-bandwidth connectivity is the goal, using Universal Mobile Telecommunications System (UMTS) and Long-Term Evolution technology tends to provide much higher throughput. The work of [112] showed that the application of GSM/GPRS for communication in telemedicine can provide high reliability and performance in remote monitoring of patients by caregivers.
The mobile cellular networks used in communications technology have continued to evolve over time. The second-generation (2G) mobile network was based on the Global System for Mobile Communication (GSM). This has progressed to 3G, 4G, and 5G, with the next generation being 6G. Telemedicine has always leveraged the advancement and development of mobile networks. As such, the various communication techniques involved are discussed below and illustrated in Table 4. In certain scenarios, using all of the available mobile technologies may be required; as evidenced in [113].

Table 4.
The Evolution of Mobile Networks [20,114].
4.5.1. GSM
The GSM technology uses a frequency of 850/900/1800/1900 MHz [74] and the Time Division Multiple Access (TDMA) and Frequency Division Multiple Access techniques to provide audio and data services. The channel bandwidth needed for 2G transmission is 20–200 KHz, with digital modulation utilised to improve voice quality over 1G technology. The General Packet Radio Service (GPRS) was brought onboard after 2G, and the Enhanced Data rate for GSM Evolution (EDGE) followed suit after GPRS. Both GPRS and EDGE are advancements of GSM technology, and are often termed as 2.5G [28] and 2.75G [115], with improved data rates of 117 Kbps and 384 Kbps, respectively. GSM/GPRS/EDGE are often used to remotely communicate telemedicine information from the CSU to the CGU for real-time remote monitoring. In [28], the authors successfully used it alongside other mobile network technologies for real-time wireless communication of medical video on an open-source telemedicine platform.
4.5.2. 3G/WCDMA/UMTS
Third-generation technology (3G), often known as Universal Mobile Telecommunication Service, came onboard under the 3rd Generation Partnership Project (3GPP). It started with Code Division Multiple Access 2000 (CDMA 2000) and later Wideband Code Division Multiple Access (WCDMA), and provided high quality audio, video, Multimedia Services (MMS), and data. WCDMA was first launched commercially in 2001 in Japan. Another technology used in China for 3G wireless telecommunication is Time Division Synchronous Code Division Multiple Access (TD-SCDMA).
This technology advanced from 3G to 3.75G [115]. High-Speed Downlink Data Access (HSDPA) is commonly known as 3.5G, and can offer a data rate of 14.4 Mbps, while 3.75G refers to High Speed Uplink Data Access.
4.5.3. 4G/LTE/WiMAX
The dawn of 4G provided the internet with a major boost, as greatly improved data rates became ubiquitous. Throughput of well over 100 Mbps became achievable with 4G. 4G uses Long-Term Evolution (LTE) technology with the WiMAX protocol based on the IEEE 802.16 standard, which were developed to provide long-distance broadband wireless data connectivity. One major high point of 4G is the use of Orthogonal Frequency Division Multiple Access (OFDMA), which provides good spectral efficiency for more data rates, mitigation of frequency-selective fading, and narrow band interference. 4G uses Multicarrier CDMA (MC-CDMA) as an access technique. LTE, LTE-Advance (LTE-A), and the preceding generation (3G) have to a great extent improved spectral efficiency, throughput, coverage, and latency, with LTE and LTE-A superseding their respective predecessors. LTE technology has found many applications in telemedicine. The research work of [116] considered the handover mechanism between LTE and Wi-Fi and proposed a Vertical Hand-Over (VHO) algorithm between LTE and Wi-Fi wireless technologies.
Despite the numerous gains of 4G technologies in terms of throughput, coverage, and latency, there exist challenges that hamper the full benefits of its application, for example the high demands of IoT communications such as Machine-to-Machine (M2M) and real-time telemedicine applications. Among the challenges with 4G are [115]:
- Optimizing the allocation of spectrum resources;
- High energy consumption, leading to high CO2 emissions;
- The difficulty of significantly improving spectral efficiency.
4.5.4. 5G
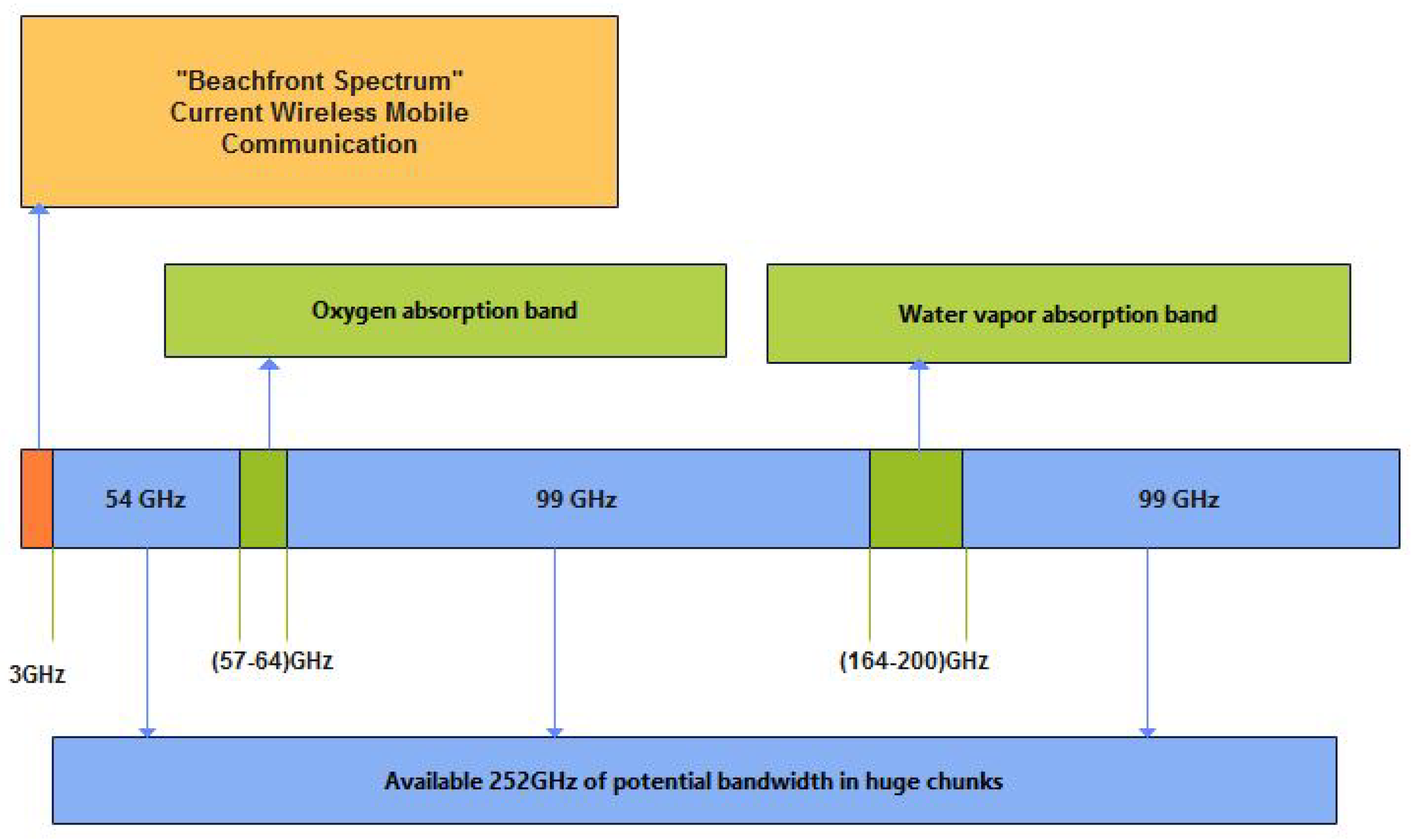
5G promises very high throughput, low latency, High Definition (HD) video, and unbounded connectivity. This is expected to provide smart healthcare with the use of connected smart wireless wearable sensor devices. 5G uses the mm-Wave. The mm-wave spectrum spans 3 GHz to 300 GHz in the electromagnetic spectrum. Within the mm-wave spectrum, only 57–64 GHz and 164–200 GHz are unsuitable for communication purposes, as shown in Figure 12 [117].
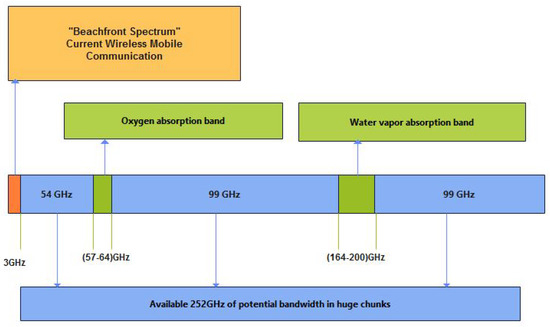
Figure 12.
Available mm-wave Communication Spectrum (3 GHz–300 GHz).
Media access techniques similar to those of 4G technology, such as Orthogonal Frequency Division Multiple Access (OFDMA), can be used with 5G. Advanced antenna systems such as massive Multiple Input Multiple Output (MIMO) in the physical layer improve capacity and bandwidth, which is highly required for 5G wireless communication. 5G is envisaged as possessing the following features: [20,40,114,117,118]:
- A high multi-peak data rate of 10Gbps;
- Ultra-low latency;
- Massive network capacity with high bandwidth;
- A very large number of connected devices; this is crucial for the vision of a breakthrough in IoT applications, which 5G can achieve using small cell sizes such as femtocell, picocell, and microcell;
- Availability of six “nines” (), that is, 5G networks should always be available to deliver as much capacity as possible;
- Maximum coverage;
- Low energy consumption;
- High user experience, with 5G expected to be user-centric rather than operator-centric.
4.5.5. Small Cells
Small cells are located within specific clusters, covering User Equipment (UEs) and sharing of resources with the base station. Small cells are located within close proximity to users, providing continuous connection to the user and supporting macrocells that have wider coverage. Small cell usage encourages better frequency reuse and management. Provision of small cells is a high point in 5G wireless technology at the mm-wave frequency. The various types of small cells and their coverage radii are shown in Table 5.

Table 5.
Types of Small Cells and their Coverage Radii [50].
Telemedicine has benefited from the offerings of 5G, especially in terms of high-speed medical information sharing in emergency cases, where physicians can use high-quality video for prompt and accurate decision-making. 5G networks provide massive M2M, D2D, IoT, and IoWT services with high reliability. Moreover, 5G can be used for more advanced applications such as Augmented Reality and Virtual reality [40] for eHealth systems [118]. Nonetheless, there are a number of challenges involved in the use of 5G for telemedicine, as listed in [40]:
- Scalability of devices in cases where there are many connected devices, meaning that device gateways and protocols need to be carefully designed;
- IoT connectivity;
- Resource optimisation;
- Interoperability;
- Energy requirements of connected devices;
- Data privacy, security, and trust;
- Enormous data computation.
5. Use Cases
There are various use cases in telemedicine systems, including the provision of diagnoses through video conferencing, transmission of still images, and simple phone conversation between patients and distant caregivers [119]. Communication in telemedicine can be viewed in terms of the relevant application, such as in emergency situations, or in terms of the type of information transmitted.
5.1. Emergency Telemedicine
In [87], an emergency telemedicine helicopter service was suggested to provide medical data and supply for life-saving services using the IEEE 802.11, 802.15, and 802.16 wireless standards. The proposed telemedicine system relied on satellite communication, thanks to its ability to provide instant access to broadband services in distant locations where medical services are inadequate or non-existent. Emergency telemedicine devices allow telediagnosis and teleconsultation through wireless communication networks such as GSM, GPRS, and satellite. The system collects and transmits vital biosignals and still images of the patient to a remote consultant during an emergency. Real-time transmission of data is strongly desirable for prompt response. Videoconferencing or a real-time two-way interactive TV system are often used. High-speed internet with high-capacity wireless transmission technologies such as LTE, 5G, and BLE, can be used with compatible devices. Emergency telemedicine for the resuscitation of new-borns was demonstrated in [120]. The Newborn Resuscitation Technology Program (NRTP) uses a wired telemedicine cart with a hardware CODEC, HD camera, and microphone–speaker arrangement for communication.
5.2. Follow-Up Telemedicine
Telemedicine is often employed in the progress monitoring and treatment of patients who are not in emergency or critical life-threatening condition, as in [11]. Patients who have initially received orthopedic or trauma surgery treatment in Germany received remote follow-up, and no substantial drawbacks were observed compared with face-to-face consultation. The communication technology used for this was telemonitoring with the aid of sensors to collect vital WBAN data for proper assessment and follow-up.
5.3. Avionics-Associated System
Telemedicine has been employed in aviation and domestic environments to ensure the safety and security of passengers and crew members. In [121], a sensor based telemedicine system for aviation was developed. The system relied on an optical cellular network using infrared wireless links. An infrared link was employed over cable or RF as the communications technology in order to limit interference. The design architecture of the avionics system was presented as well.
6. Types of Information Transmitted
Information and knowledge sharing between medical experts, medical students, and patients was carried out using ISDN and VoIP techniques for videoconferencing, video streaming, and podcasting in [45,122].
6.1. Video Conferencing
Advancements in information and communications technology has led to the increased use of video conferencing in telemedicine [123]. One such scenario was a telemedicine system designed for both rural and urban areas as a result of the dearth of medical personnel in rural areas of Iraq, called Mobile Field Hospital (MFH) [124]. In this scenario, intranet connections were established using GPRS devices (mobile phones) and personal computers. This allows a medical doctor in a remote hospital (MFH) to then perform a video conference with a specialist doctor in another location using GPRS within the network. In another example, telemedicine video conferencing was used at a mining station in Australia located about 1800 km away from the specialist clinic; the video conferencing unit was connected via an Integrated Services Digital Network (ISDN) and provided a data rate of 128 kbps [125].
In their design for a telemedicine framework, [34] used both Advanced Encryption Standard (AES) and the Rivest–Shamir–Adleman (RSA) algorithm for data encryption. The encrypted video and audio were transmitted using Real-time Transport Protocol (RTP) over User Datagram Protocol (UDP). In [2], video conferencing was achieved through Voice over Internet Protocol (VoIP) using the MPEG and MPEG2 file formats.
6.2. Transmission of Medical Images
Image transmission is another vital issue in telemedicine. For efficient medical diagnosis, relevant images transmitted from a patient to a remote physician need to have acceptable resolution and use standard file formats such as JPEG, TIFF, BMP, or Digital Imaging and Communications in Medicine (DICOM) [2]. The images are transmitted to the destination station via the File Transfer Protocol (FTP) or TCP/IP. Among the techniques used for capturing medical images are ultrasound, digital X-Rays, Magnetic Resonance Imaging (MRI), and Computed Tomography (CT) scanning. The work of [126] demonstrated that after using a wireless CT scan to obtain images of neurosurgical emergency cases, a neurosurgical consultant can reliably render telemedical services to the patient.
6.3. Video Streaming
This requires a high-speed internet connection such as UMTS or higher for viewing online content over the internet without the need to download media files. Such media content may include medical TV shows, healthcare educational content, and live event broadcasts. Communication protocols used in video streaming include HTTP Live Streaming protocol (HLS), Real-Time Messaging Protocol (RTMP), Real-Time Streaming Protocol (RTSP), and MPEG Dynamic Adaptive Streaming over HTTP (MPEG-DASH). A major challenge with live video streaming is transmission delay. The work of [127] proposed that the H.265 codec provides better quality and more efficient video compression and decompression techniques with reduced video transmission delay compared to the H.264 codec.
7. Communication Standards/Protocols in Telemedicine
Wireless communication technology plays a significant role in efficient healthcare delivery during medical emergency for patients and health care providers over a distance [38]. Two major connectivity techniques are used in telemedicine, namely, point-to-point and point-to-multipoint [43]. These technologies are used for effective communication between the wireless sensor nodes and the remote health care provider. Wireless Connectivity Protocols in Telemedicine include:
- ZigBee/IEEE 802.15.4: the ZigBee protocol is used for interfacing with data processing devices such as personal data assistants (PDA) and PCs that are directly connected to medical devices (point-to-point). Because of its simplicity, low power usage, and ability to cover large numbers of devices per network, ZigBee is projected to succeed in setting a leading standard for home control applications, which forms a vital component of telemedicine applications [60]. In [49], a ZigBee module was used to connect ECG data to a PC through a Universal Asynchronous Receiver–Transmitter (UART) connected to a USB transceiver device. Although the system supports only point-to-point connection, the end terminal can be any PC with a USB port and an operating system equipped with a USB-to-UART driver.
- Bluetooth/IEEE 802.15.1: Bluetooth is a short-range radio link intended to replace the cables connecting fixed electronic devices. It operates in the unlicensed Industrial Scientific Medicine (ISM) frequency band at 2.4 GHz [82]. A combination of ZigBee and Bluetooth was utilised in [93] to connect four different medical services. The system was interfaced through UART and an analog port, delivering data rates up to 42 kbps. Table 6 shows a comparison between the Bluetooth and Zigbee communication standards.
 Table 6. Key Features of Bluetooth and ZigBee Wireless Technologies [60,107].
Table 6. Key Features of Bluetooth and ZigBee Wireless Technologies [60,107]. - WiMAX/IEEE Broadband Wireless Access (BWA) 802.16: according to [128], WiMAX is a communication protocol based on the IEEE 802.16 standard. Developed to provide long distance broadband wireless data connectivity, it serves as an alternative to cable and DSL because of its high bandwidth and provision of BWA for up to 30 miles for fixed stations and 3–10 miles for mobile stations.With respect to telemedicine applications, [38] shows that WiMAX systems for wireless telemedicine provide high mobile connectivity for multimedia traffic with guaranteed QoS, representing advantages over 3G systems, which are designed for more basic data and voice transmission. A number of major communication challenges are addressed by WiMAX standards, including provision of high bandwidth, QoS support, integrated services, and security.
- WiFi/WLAN/IEEE 802.11: WiFi/WLAN is a wireless communication protocol based on the IEEE 802.11 standard. In telemedicine applications, WiFi networks usually comprise multiple access points, with medical sensor nodes moving freely among access points [107].A study by [108] demonstrated a WLAN/IEEE 802.11n standard transmission scheme for wireless telemedicine applications. The WLAN system could transmit measured medical data using digital bits, ECG signals, case histories, and audio/video signals for telemedical purposes. Similarly, medical signal accuracy in WiFi-based telemedicine schemes was presented in [107]. According to the authors, several security threats are associated with WiFi networks due to their use of open an medium to transmit and receive data. Threats which can be detrimental in medical contexts include: denial of service, eavesdropping, and services theft. Another issues is that the WiFi/802.11 protocol is limited to between 30–100 m, which is a disadvantage compared to the WiMAX protocol [128].
- User Datagram Protocol (UDP): protocols for media streaming are usually intended for communication between streaming servers and their users, and handle concerns around transport, session control, and network addressing. UDP is a transport protocol that is widely utilized for data streaming in telemedicine contexts [129]. UDP is the preferred transport protocol for streaming video over fading channels, and can be used in combination with other protocols to further benefit from their advantages. The UDP/IP protocol was utilized in [129]; refs. [130,131] recommend that UDP should be employed for delay-sensitive tasks with tolerance to minor loss of frame traffic, such as video streaming, in preference to TCP. In the work of [92], the UDP protocol was chosen instead of other protocols because of its swiftness and efficiency in real life applications, although [29] mention that video traffic or signals take the lowest priority in the UDP protocol. The UDP protocol uses a simple datagram without congestion control. This issue can be addressed by adopting a rate adjustment measure, as pointed out in [131,132]. While UDP may not be reliable for transmission of packet-based data, it is very good for networked games and streaming media [96].
- Real-Time Protocol (RTP) and Real-Time Transport Control Protocol (RTCP): the RTP and RTCP protocols are internet protocols belonging to the family of transport protocols for media streaming. For real-time applications, the RTP protocol provides an end-to-end transport function. RTCP is often used as a companion control protocol to the RTP protocol, where it helps to improve Quality of Service (QoS) feedback. The authors in [133] used RTP and RTCP protocols in their measurement of the QoS of video streams.
- TCP/IP: another wireless communication protocol utilised in telemedicine is the transmission control protocol (TCP)/internet protocol (IP). Due its low-cost and multiple functions, there has been significant rise in the use of IP-based networks in telemedicine applications [2]. A study by [84] presented an IP-based medical data transmission system that used the TCP/IP protocol to efficiently transmit data over the network, achieving a high bandwidth and low error rate. In their proposed design, data are transmitted between the server and the client in the form of packets using TCP.
8. Research Challenges and Future Directions
The application of wireless communication in telemedicine is driven by technological advancements, which are usually associated with several issues and challenges. As highlighted in [16], issues and challenges related to deployment of wireless communication technologies in telemedicine include interoperability and usability, co-existence and interference, and end-to-end QoS. The need for remote diagnosis and health care delivery is expected to eventually limit human involvement in telemedicine. Consequently, artificial intelligence and machine learning are quickly gaining traction in the field of telemedicine, posing a substantial range of challenges involving accuracy, interpretability, overfitting, and computational complexity.
Lack of a standard medical data communications protocol, interference from other wireless devices, and QoS in terms of high throughput and low delay are among the major issues affecting the full implementation of telemedicine systems; a number of these issues have to do with integration of heterogeneous wireless networks. Due to the significance of stable connectivity in WSNs for telemedicine, handover schemes are employed to maintain constant connectivity between the sensor nodes, gateway, and other wireless devices within the system. The process of connecting to the best access network is done through a Horizontal Handoff (HHO) mechanism, while Vertical Handoff (VHO) provides network access to the mobile nodes moving through heterogeneous access points [38].
8.1. Classification of Research Challenges in Telemedicine
Leading research challenges in wireless telemedicine implementations include: data security, scheduling, and video compression [3]; Quality of Service (QoS) and Quality of Experience (QoE) [37]; and privacy preservation and security [134]; energy efficiency, fault tolerance, and high bandwidth requirements for video streaming have been highlighted as well [101]. Figure 13 presents the research challenges mentioned above and discussed in the following subsections.
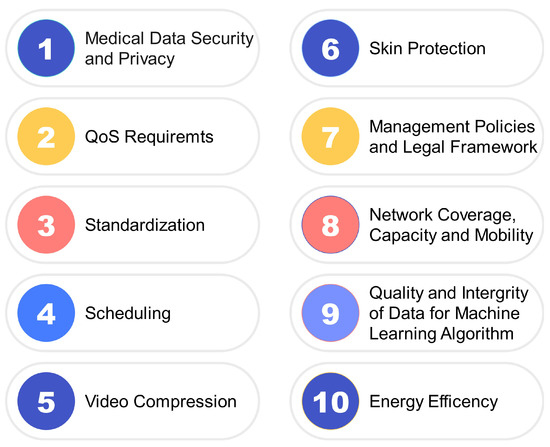
Figure 13.
Research Challenges in Telemedicine.
8.1.1. Medical Data Security and Privacy
Data security is very crucial in telemedicine designs in order to avoid incorrect diagnoses. The high proliferation of medical data on the cloud due to ease of access and telemedicine deployment has increased data vulnerability. Potential attacks such as information disclosure, Denial of Service attacks (DoS), cloud malware injection attacks, man-in-the middle cryptographic attacks, spoofing, and collusion attacks, as seen in [134], must be addressed in telemedicine deployment. This is a major barrier to the proper implementation of telemedicine, as noted by [135].
8.1.2. QoS Requirements
Another major research issue is the provision of QoS in transmitting telemedicine traffic. This is mainly due to the sensitive nature of medical data with respect to patients’ health. Therefore, provision of QoS is a key factor when transmitting data for telemedicine applications. Providing QoS in telemedicine networks is a major challenge, particularly in critical services such as live video streaming of surgeries and remote diagnosis tasks [37].
8.1.3. Standardization
Remote patient monitoring in telemedicine employs multiple monitoring and communication devices, potentially leading to compatibility issues. Because there are no specific technological standards in place, devices may not communicate effectively and it may not be easy to manage stored data from other devices or technologies that are not compatible [16]. There is a need to develop a standard format or protocol for medical data communication in order to mitigate this issue.
8.1.4. Scheduling
Scheduling is the process of making decision about resource allocation between a variable number of tasks [3]. Prioritizing data transmission and reception is a major issue in deploying telemedicine projects. Scheduling allows for a quick response in emergencies by ensuring preference to the most urgent needs of the patients in the network.
8.1.5. Video Compression
In order to transmit large volumes of medical data over a telemedicine network, there is a need to compress data for bandwidth optimization and effective management of data traffic. Due to the significance of this issue, researchers have attempted to develop a variety of video compression techniques, including lossless and lossy compression, as discussed in [3].
8.1.6. Skin Protection
One of the challenges raised in [4] is concern over skin protection. Wearable devices, which are in certain instances implanted into human body tissues, are prone to cause harm or other undesirable effects to the skin and other bodily systems. Researchers and other stakeholders need to take the absorption rate of radiation from wireless sensors into careful consideration during the conceptualization, design, prototyping, and deployment of WBAN devices in order to avoid causing more harm than good.
8.1.7. Cost of Deployment and Legal Framework
There are many benefits of employing telemedicine, including increased access to quality healthcare services and expert physicians, among others. These benefits are often out of reach, especially in the developing countries, due to the high cost of fully deploying communication infrastructures such as fiber optic links and satellite communications to remote areas. This has made it difficult to adequately meet the needs of remote communities. Even when deployed, the cost of services can be high, and this invariably translates to fewer services for the end users. Poor legal frameworks are another issue in this regard.
8.1.8. Network Coverage, Capacity and Mobility
Telemedicine applications require very good network coverage for smooth operation. As such, network providers must work to improve and sustain the transmission of medical information from local areas where patients require telemedical services to areas where doctors are based. This need is even more stringent if the medical services need to be provided in real time. As highlighted by [136], the issue of network coverage and mobility is crucial if telemedical services are to be guaranteed. Research on the improvement of network availability for more efficient telemedicine service delivery is an important area to be considered. Data transmission rates and capacity are not currently adequate for telemedicine operations in most deployment areas, and services such as telemedicine video conferencing require reliable 5G deployment.
8.1.9. Quality and Integrity of Data for ML Algorithms
The accessibility of quality datasets is essential for training ML algorithms. To obtain a reliable model that adapts to the domain of a particular research problem requires data with high integrity in order to extract the right features. As alluded by [135], this it is a herculean task that often requires the initiative of very big hospitals or health boards to collect patient medical records or data for research due to the need to ensure that patient data remains confidential. Even when such data are obtained, they may contain outliers that can adversely influence research outcomes if not properly handled.
8.1.10. Energy Efficiency
Most wearable devices demand enhanced power for measuring and communicating user data. Because wearable devices are often required to be small, the batteries are expected to be in miniature form, and need to be able to sustain the energy required for the task as well. The size and capacity of batteries is an important factor in the design of wearable telemedicine devices. For energy efficiency, devices should have low power demands and be capable of saving energy when not in operation.
8.2. Future Directions
Future research work needed in this area includes implementation of blockchain, mobile edge computing (MEC), and cloud computing technologies for secure data transmission. Resource allocation and stable all-the-time connectivity using vertical handoff techniques and efficient media compression methods is another viable research area in emergency telemedicine applications. Deployment of telemedicine designs must take into consideration the issues of availability, scalability, and standardization of communication technologies by studying available open standards and the use of gateways and open application programming interfaces (API). In addition, it is important to consider miniaturization of wearable devices by reducing design complexity and improving power efficiency through deployment of optimization techniques such as multi-cast energy-aware routing protocols and dynamic access scheduling techniques. The concept of RF energy harvesting is a development that could greatly help to address a number of energy problems involved in the future progression of telemedicine.
Prospective researchers might focus on combining existing telemedicine technologies highlighted in this study and incorporating emerging concepts such as the Internet of Medical Things (IoMT), Wearable Internet of Things (W-IoT), and Health Internet of things (H-IoT). This could improve rapid roll-out of remote health monitoring schemes and enhance the interoperability of devices and networks in telemedicine systems. Future surveys could explore areas such as medical data integration of conventional Electronic Health Records (EHRs) for wireless telemedicine and remote medical diagnosis, making the use of manual records and the usual face-to-face doctor-to-patient consultations less necessary. Future telemedicine research should concentrate on the advancement of telecommunication technologies, the integration of telemedicine with EHRs, and the development of new technologies such as artificial intelligence and wearable devices. Finally, researchers should concentrate on addressing challenges such as legal and regulatory issues, reimbursement, and access to technology. Researchers can help to ensure that telemedicine remains a safe, effective, and widely accepted method of healthcare delivery by addressing these challenges.
9. Conclusions
In this review article we have discussed the development of telemedicine systems, with a particular focus on the various communication technologies employed. Communication technologies such as BAN, remote communication with telemedical servers, and communication based on telemedical applications have been classified and reviewed. The use of internet, satellite, WAN and GSM communications, as mentioned and used by different researchers for the transmission of different types of data from a local point (patient) to a remote server (remote physician location) have been discussed in detail. The choice and use of any type depends on the availability of the infrastructure, type of application, and cost. The different connectivity protocols/standards used for communication were examined, with certain protocols noted to be better adapted to certain specific communication contexts based on the data type to be transmitted. The use of ML algorithms for telemedicine was considered. The overall purpose of this review is to provide a broad overview of the recent wireless communication technologies deployed in telemedicine systems, with a particular emphasis on implementation issues, challenges, and research gaps. Findings from the various articles reviewed here suggest the need to implement systems that combine multiple wireless networks in order to guarantee QoS and allow mobility for both clients/patients and remote care-givers. Despite the numerous studies conducted in this field, medical data transmission using a standard format that is universally compatible with other wireless devices remains lacking. Future telemedicine designs need to address issues such as scheduling, data security and privacy, and medical video streaming employing modern compression techniques. Another issue is that the design of wearable medical devices needs to take cognizance of energy efficiency, the absorption rate of radiation from wireless sensors, and the need for skin protection. Finally, the quality and integrity of data used for learning by ML algorithms is a crucial requirement for building reliable models to be used in telemedicine research and development.
Author Contributions
Authors C.O.A., H.O.O., A.O.A., A.J.O., E.E.O., A.I.B., S.A.O., E.K. and B.A. contributed equally to this work. Conceptualization, C.O.A., H.O.O., A.O.A., A.J.O.; methodology, H.O, A.J.O., A.O.A.; writing—original draft preparation, A.O.A., E.E.O., A.I.B., S.A.O.; writing—review and editing, C.O.A., A.J.O., H.O.O., A.O.A., E.K., A.I.B.; supervision, C.O.A., A.J.O., H.O.O., A.O.A.; funding acquisition, C.O.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the TETFund, Nigeria, with project number TETF/ES/DR& D-1674 CE/NRF2020/SET1/67/VOL.1.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Moore, M. The Evolution of Telemedicine. Future Gener. Comput. Syst. 1999, 15, 245–254. [Google Scholar] [CrossRef]
- Pandian, P.S.; Safeer, K.P.; Shakunthala, D.T.I.; Gopal, P.; Padaki, V.C. Store and Forward Applications in Telemedicine for Wireless IP Based Networks. J. Netw. 2007, 2, 58–65. [Google Scholar] [CrossRef]
- Devaraj, S.J.; Ezra, K. Current Trends and Future Challenges in Wireless Telemedicine System. In Proceedings of the 2011 3rd International Conference on Electronics Computer Technology, Kanyakumari, India, 8–10 April 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Chakraborty, C.; Gupta, B.; Ghosh, S.K. A Review on Telemedicine-Based WBAN Framework for Patient Monitoring. Telemed. e-Health 2013, 19, 619–626. [Google Scholar] [CrossRef]
- Alenoghena, C.O.; Onumanyi, A.J.; Ohize, H.O.O.; Adejo, A.O.; Oligbi, M.; Ali, S.; Okoh, S.A. eHealth: A Survey of Architectures, Developments in mHealth, Security Concerns and Solutions. Int. J. Environ. Res. Public Health 2022, 19, 13071. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.; Crowley, T.; Keena, B.; Donoghue, S.; McManus, M.; Zackai, E. The experience of one pediatric geneticist with telemedicine-based clinical diagnosis. Am. J. Med. Genet. 2023, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.G.; Watts, I.; Beales, E.; Maudhoo, A.; Hayward, J.; Sheridan, E.; Rafi, I. Videoconferencing to deliver genetics services: A systematic review of telegenetics in light of the COVID-19 pandemic. Am. J. Med. Genet. 2021, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Brenner, B.; Brancolini, S.; Eshraghi, Y.; Guirguis, M.; Durbhakula, S.; Provenzano, D.; Vorenkamp, K.; Shah, S.; Darden, M.; Kohan, L. Telemedicine Implementation in Pain Medicine: A Survey Evaluation of Pain Medicine Practices in Spring. Pain Physician 2022, 25, 387–390. [Google Scholar] [PubMed]
- Der-martirosian, C.; Shin, M.; Upham, M.L.; Douglas, J.H.; Zeliadt, S.B.; Taylor, S.L. Telehealth Complementary and Integrative Health Therapies During COVID-19 at the U.S. Department of Veterans Affairs. Telemed. e-Health 2022, 1–8. [Google Scholar] [CrossRef]
- Everard, K.M.; Schiel, K.A.; Xu, E.; Kulshreshtha, A. Use of Telemedicine in the Family Medicine Clerkship: A CERA Study. PRiMER 2022, 6, 25. [Google Scholar] [CrossRef]
- Muschol, J.; Heinrich, M.; Heiss, C.; Knapp, G.; Repp, H.; Schneider, H.; Thormann, U.; Uhlar, J.; Unzeitig, K.; Gissel, C. Assessing Telemedicine Efficiency in German Follow-up Care With Video Consultations for Patients in Orthopedic and Trauma Surgery: A Randomized Controlled Trial. J. Med. Internet Res. 2022, 24. [Google Scholar] [CrossRef]
- Yamin, M.A.Y.; Alyoubi, B.A. Adoption of telemedicine applications among Saudi citizens during COVID-19 pandemic: An alternative health delivery system. J. Infect. Public Health 2020, 13, 1845–1855. [Google Scholar] [CrossRef]
- Giansanti, D.; Morone, G.; Loreti, A.; Germanotta, M.; Aprile, I. A Narrative Review of the Launch and the Deployment of Telemedicine in Italy during the COVID-19 Pandemic. Healthcare 2022, 10, 415. [Google Scholar] [CrossRef]
- Bembinov, M.; Soenardi, N. An assessment of client and clinician satisfaction in veterinary teleconsultation compared to in-person consultations. Vet. Evid. 2023, 7, 1–17. [Google Scholar] [CrossRef]
- Arain, S.; Al, M.; Shabeer, S.; Thorakkattil, A.; Iqbal, S.; Fuad, M.; Ghamdi, A. Implementation of Pharmacist-led Telepsychiatry Services: Challenges and Opportunities in the Midst of COVID-19. J. Technol. Behav. Sci. 2022. [Google Scholar] [CrossRef]
- Khaddar, M.A.E.; Harroud, H.; Boulmalf, M.; Elkoutbi, M.; Habbani, A. Emerging Wireless Technologies in e-health Trends, Challenges, and Framework Design Issues. In Proceedings of the 2012 International Conference on Multimedia Computing and Systems, Tangiers, Morocco, 10–12 May 2012; IEEE: Piscataway, NJ, USA, 2012. [Google Scholar] [CrossRef]
- Laxminarayan, S.; Istepanian, R. UNWIRED E-MED: The Next Generation of Wireless and Internet Telemedicine Systems. IEEE Trans. Inf. Technol. Biomed. 2000, 4, 189–193. [Google Scholar] [CrossRef]
- Pattichis, C.; Kyriacou, E.; Voskarides, S.; Pattichis, M.; Istepanian, R.; Schizas, C. Wireless Telemedicine Systems: An Overview. IEEE Antennas Propag. Mag. 2002, 44, 143–153. [Google Scholar] [CrossRef]
- Albahri, A.S.; Alwan, J.K.; Taha, Z.K.; Ismail, S.F.; Hamid, R.A.; Zaidan, A.; Albahri, O.S.; Zaidan, B.; Alamoodi, A.H.; Alsalem, M. Iot-based Telemedicine for Disease Prevention and Health Promotion: State-of-the-Art. J. Netw. Comput. Appl. 2021, 173, 102873. [Google Scholar] [CrossRef]
- Amuomo, N.O. The Evolution of GSM Technologies into 5G and the Imminent Emergence of Transformative Telemedicine Applications: A Review. East Afr. J. Inf. Technol. 2020, 2, 8–17. [Google Scholar] [CrossRef]
- Haddara, M.; Staaby, A. RFID Applications and Adoptions in Healthcare: A Review on Patient Safety. Procedia Comput. Sci. 2018, 138, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Tachakra, S.; Wang, X.; Istepanian, R.S.; Song, Y. Mobile e-Health: The Unwired Evolution of Telemedicine. Telemed. J. e-Health 2003, 9, 247–257. [Google Scholar] [CrossRef]
- Suksmono, A.B.; Sastrokusumo, U.; Mengko, T.L.R.; Pramudito, J.T.; Oktowaty, S. Overview of Telemedicine Activities in Indonesia: Progress and Constraints. In Proceedings of the 6th International Workshop on Enterprise Networking and Computing in Healthcare Industry-Healthcom 2004 (IEEE Cat. No. 04EX842), Odawara, Japan, 29 June 2004; IEEE: Piscataway, NJ, USA, 2004; pp. 37–40. [Google Scholar]
- Ferrante, F.E. Evolving Telemedicine/eHealth Technology. Telemed. e-Health 2005, 11, 370–383. [Google Scholar] [CrossRef]
- Raskovic, D.; Milenkovic, A.; Groen, P.C.D.; Jovanov, E. FromTelemedicine to Ubiquitous M-health: The Evolution of e-health Systems. In Biomedical Information Technology; Elsevier: Amsterdam, The Netherlands, 2008; pp. 479–496. [Google Scholar]
- Rashvand, H.; Salcedo, V.T.; Sánchez, E.M.; Iliescu, D. Ubiquitous Wireless Telemedicine. IET Commun. 2008, 2, 237. [Google Scholar] [CrossRef]
- Cova, G.; Xiong, H.; Gao, Q.; Guerrero, E.; Ricardo, R.; Estevez, J. A Perspective of State-of-the-Art Wireless Technologies for e-health Applications. In Proceedings of the 2009 IEEE International Symposium on IT in Medicine & Education, Jinan, China, 14–16 August 2009; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Panayides, A.; Pattichis, M.; Pattichis, C.S.; Schizas, C.N.; Spanias, A.; Kyriacou, E. An Overview of Recent End-to-End Wireless Medical Video Telemedicine Systems Using 3G. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; IEEE: Piscataway, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Wang, Z.; Gu, H. A Review of Telemedicine in China. J. Telemed. Telecare 2009, 15, 23–27. [Google Scholar] [CrossRef]
- Zubiete, E.D.; Luque, L.F.; Rodriguez, A.V.M.; Gonzalez, I.G. Review of Wireless Sensors Networks in Health Applications. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Lin, C.F.; Hung, S.I.; Chiang, I.H. An 802.11n Wireless Local Area Network Transmission Scheme for Wireless Telemedicine Applications. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2010, 224, 1201–1208. [Google Scholar] [CrossRef]
- Clifford, G.D.; Clifton, D. Wireless Technology in Disease Management and Medicine. Annu. Rev. Med. 2012, 63, 479–492. [Google Scholar] [CrossRef]
- Kayange, D.S.; Massawe, E.A. The Potential for a Tanzania Wireless Telemedicine Network: An Overview. Res. J. Eng. Appl. Sci. 2013, 2, 171–175. [Google Scholar]
- Mahfouz, M.R.; Kuhn, M.J.; To, G. Wireless Medical Devices: A Review of Current Research and Commercial Systems. In Proceedings of the 2013 IEEE Topical Conference on Biomedical Wireless Technologies, Networks, and Sensing Systems, Austin, TX, USA, 20–23 January 2013; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Ahmad, N.; Riaz, N.; Hussain, M. Ad hoc Wireless SensorNnetwork Architecture for Disaster Survivor Detection. Int. J. Adv. Sci. Technol. 2011, 34, 16. [Google Scholar]
- Algaet, M.A.; Noh, Z.A.B.M.; Shibghatullah, A.S.; Milad, A.A.; Mustapha, A. Provisioning Quality of Service of Wireless Telemedicine for E-Health Services: A Review. Wirel. Pers. Commun. 2014, 78, 375–406. [Google Scholar] [CrossRef]
- de la Torre Díez, I.; Alonso, S.G.; Hamrioui, S.; López-Coronado, M.; Cruz, E.M. Systematic Review about QoS and QoE in Telemedicine and eHealth Services and Applications. J. Med. Syst. 2018, 42, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rani, B.K.S.; Bhat, S.; Mukhopadhyay, A. A Survey of Wireless Technologies and Vertical Handoff Techniques from the Perspective of Telemedicine Scenarios. In Proceedings of the 2017 International Conference on Communication and Signal Processing (ICCSP), Chennai, India, 6–8 April 2017; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Lukas, H.; Xu, C.; Yu, Y.; Gao, W. Emerging Telemedicine Tools for Remote COVID-19 Diagnosis, Monitoring, and Management. ACS Nano 2020, 14, 16180–16193. [Google Scholar] [CrossRef]
- Nawaz, N.A.; Abid, A.; Rasheed, S.; Farooq, M.S.; Shahzadi, A. Impact of telecommunication network on future of telemedicine in healthcare: A systematic literature review. Int. J. Adv. Appl. Sci. 2022, 9, 122–138. [Google Scholar] [CrossRef]
- Chatterjee, S.; Khan, A.M.; Rani, P.; Jayesh, S. A systematic review on tele dentistry in public oral health during COVID-19. NeuroQuantology 2022, 20, 1107–1117. [Google Scholar] [CrossRef]
- Woodward, B.; Rasid, M. Wireless Telemedicine: The Next Step. In Proceedings of the 4th International IEEE EMBS Special Topic Conference on Information Technology Applications in Biomedicine, Birmingham, UK, 24–26 April 2003. [Google Scholar] [CrossRef]
- Pandian, P.S. An Overview of Telemedicine Technologies for Healthcare Applications. Int. J. Biomed. Clin. Eng. 2016, 5, 29–52. [Google Scholar] [CrossRef]
- Craft, R.L.; Funkhouser, D.R.; Gallagher, L.K.; Garcia, R.J.; Parks, R.C.; Warren, S. High-Surety Telemedicine in a Distributed, ‘Plug-and-Play’ Environment; Technical Report; Sandia National Laboratories (SNL): Albuquerque, NM, USA, 1999.
- Portnoy, J.M.; Pandya, A.; Waller, M.; Elliott, T. Telemedicine and emerging technologies for health care in allergy/immunology. J. Allergy Clin. Immunol. 2020, 145, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.; Chang, M.C. Usefulness of an Online Preliminary Questionnaire under the COVID-19 Pandemic. Nat. Public Health Emerg. Collect. 2020, 44, 116. [Google Scholar] [CrossRef]
- Khoor, S.; Nieberl, K.; Fugedi, K.; Kail, E. Telemedicine ECG-Telemetry with Bluetooth Technology. In Proceedings of the Computers in Cardiology 2001. Vol.28 (Cat. No.01CH37287), Rotterdam, The Netherlands, 23–26 September 2001; pp. 585–588. [Google Scholar] [CrossRef]
- Orlov, O.I.; Drozdov, D.V.; Doarn, C.R.; Merrell, R.C. Wireless ECG monitoring by telephone. Telemed. J. e-Health 2001, 7, 33–38. [Google Scholar] [CrossRef]
- Auteri, V.; Roffia, L.; Cinotti, T.S. ZigBee-Based Wireless ECG Monitor. In Proceedings of the 2007 Computers in Cardiology, Durham, NC, USA, 30 September–3 October 2007; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Aboalseoud, A.; Youssry, A.; El-Nozahi, M.; El-Rafei, A.; Elbialy, A.; Ragaai, H.; Wahba, A. Wireless ECG Monitoring System for Telemedicine Application. In Proceedings of the 2019 IEEE 9th International Conference on Intelligent Computing and Information Systems, ICICIS 2019, Cairo, Egypt, 8–10 December 2019; pp. 300–305. [Google Scholar] [CrossRef]
- Lin, J.L.; Liu, H.C.; Tai, Y.T.; Wu, H.H.; Hsu, S.J.; Jaw, F.S.; Chen, Y.Y. The development of wireless sensor network for ECG monitoring. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 3513–3516. [Google Scholar] [CrossRef]
- D’Souza, M.; Ros, M.; Postula, A. Wireless medical information system network for patient ECG monitoring. In Proceedings of the 9th EUROMICRO Conference on Digital System Design: Architectures, Methods and Tools, DSD 2006, Cavtat, Croatia, 30 August–1 September 2006; pp. 617–624. [Google Scholar] [CrossRef]
- Jimeno, M.; De la Hoz, Y.; Wilches, J. Wireless ECG and PCG Portable Telemedicine Kit for Rural Areas of Colombia. Investig. Innovación en Ing. 2014, 2, 1–9. [Google Scholar] [CrossRef]
- Nopparat, V.; Keeratiwintakorn, P. The three-lead wireless ECG in sensor networks for mobile patients. In Proceedings of the 2008 SICE Annual Conference, Chofu, Japan, 20–22 August 2008; pp. 2308–2311. [Google Scholar] [CrossRef]
- Rashkovska, A.; Tomašić, I.; Trobec, R. A Telemedicine application: ECG data from wireless body sensors on a Smartphone. In Proceedings of the 2011 Proceedings of the 34th International Convention MIPRO, Opatija, Croatia, 23–27 May 2011; pp. 262–265. [Google Scholar]
- Zhang, Z.; Jung, T.P.; Makeig, S.; Rao, B.D. Compressed sensing for energy-efficient wireless telemonitoring of noninvasive fetal ECG via block sparse bayesian learning. IEEE Trans. Biomed. Eng. 2013, 60, 300–309. [Google Scholar] [CrossRef]
- Abdulbaqi, A.S.; Najim, S.A.M.; Mohammed, F.M.; Masunda, T.; Panessai, I.Y. Wireless EEG transmission and evaluation based on iCloud efficiency: Age of telemedicine. J. Eng. Sci. Technol. 2021, 16, 2416–2425. [Google Scholar]
- Kannampallil, T.; Ma, J. Digital Translucence: Adapting Telemedicine Delivery Post-COVID-19. Telemed. e-Health 2020, 26, 1120–1122. [Google Scholar] [CrossRef]
- Hu, X.; Wang, J.; Yu, Q.; Liu, W.; Qin, J. A wireless sensor network based on ZigBee for telemedicine monitoring system. In Proceedings of the 2nd International Conference on Bioinformatics and Biomedical Engineering, iCBBE 2008, Shanghai, China, 16–18 May 2008; pp. 1367–1370. [Google Scholar] [CrossRef]
- Sîrbu, A.N.; Maiorescu, V.A.V.D.; Cleju, I.I. A Zigbee Solution for Telemedicine Applications. ACTA Tech. Napoc. Electron. Telecommun. 2008, 49, 35–39. [Google Scholar]
- Supriyanto, E.; Satria, H.; Mulyadi, I.H.; Putra, E.H. A Novel Low Cost Telemedicine System Using Wireless Mesh Network. In Proceedings of the 3rd SEATUC Symposium, Johor Bahru, Malaysia, 25–26 February 2009; pp. 382–402. [Google Scholar]
- Oh, S.; Kwon, H.; Varadan, V.K. Wireless telemedicine systems for diagnosing sleep disorders with Zigbee star network topology. Nanosyst. Eng. Med. 2012, 8548, 85482L. [Google Scholar] [CrossRef]
- Wang, X. Wireless mesh networks. J. Telemed. Telecare 2008, 14, 401–403. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Wang, M. A Wireless PDA-based Electrocardiogram Transmission System for Telemedicine. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 1–4 September 2005; Volume 7, pp. 3807–3809. [Google Scholar] [CrossRef]
- Wang, D.; Lu, Y.; Zhang, H.; Zhang, J.; Han, Y. Body Piconet for the Telemedicine System Based on Home Networks. In Proceedings of the 2007 IEEE/ICME International Conference on Complex Medical Engineering, Beijing, China, 23–27 May 2007; IEEE: Piscataway, NJ, USA, 2007; pp. 1202–1205. [Google Scholar]
- Lin, C.F.; Chung, C.H.; Chen, Z.L.; Song, C.J.; Wang, Z.X. A chaos-based unequal encryption mechanism in wireless telemedicine with error decryption. WSEAS Trans. Syst. 2008, 7, 49–55. [Google Scholar]
- Kugean, C.; Krishnan, S.M.; Chutatape, O.; Swaminathan, S.; Srinivasan, N.; Wang, P. Design of a mobile telemedicine system with wireless LAN. In Proceedings of the Asia-Pacific Conference on Circuits and Systems, Denpasar, Indonesia, 28–31 October 2002; Volume 1, pp. 313–316. [Google Scholar] [CrossRef]
- Moshayedi, A.J.; Kolahdooz, A.; Roy, A.S.; Rostami, S.A.L.; Xie, X. Design and promotion of cost-effective IOT-based heart rate monitoring. In Proceedings of the International Conference on Cloud Computing, Internet of Things, and Computer Applications (CICA 2022), Luoyang, China, 22–24 April 2022; Powell, W., Tolba, A., Eds.; International Society for Optics and Photonics: Bellingham, WA, USA, 2022; Volume 12303, pp. 405–410. [Google Scholar] [CrossRef]
- Thrall, J.H.; Boland, G. Teleradiology. In PACS: A Guide to the Digital Revolution; Dreyer, K.J., Mehta, A., Thrall, J.H., Eds.; Springer: New York, NY, USA, 2002; pp. 315–348. [Google Scholar] [CrossRef]
- Latifi, R.; Doarn, C.R.; Merrell, R.C. Telemedicine, Telehealth and Telepresence; Springer International Publishing: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Lin, Y.H.; Jan, I.C.; Ko, P.I.; Chen, Y.Y.; Wong, J.M.; Jan, G.J. A Wireless PDA-BasedPhysiological Monitoring System for Patient Transport. IEEE Trans. Inf. Technol. Biomed. 2004, 8, 439–447. [Google Scholar]
- Takahashi, M. Contribution of teleradiology in Japanese medicine. Int. J. Comput. Assist. Radiol. Surg. 2006, 1, 455–456. [Google Scholar] [CrossRef]
- Committee for a Responsible Budget. American Health Care: Health Spending and the Federal Budget. Available online: https://jamanetwork.com/journals/jama/fullarticle/2594716/ (accessed on 12 December 2022).
- Abo-Zahhad, M.; Ahmed, S.M.; Elnahas, O. A Wireless Emergency Telemedicine System for Patients Monitoring and Diagnosis. Int. J. Telemed. Appl. 2014, 2014, 380787. [Google Scholar] [CrossRef]
- Hung, K.; Zhang, Y. Usage of Bluetooth/sup TM/in Wireless Sensors for Tele-Healthcare. In Proceedings of the Second Joint 24th Annual Conference and the Annual Fall Meeting of the Biomedical Engineering Society Engineering in Medicine and Biology, Houston, TX, USA, 23–26 October 2002; IEEE: Piscataway, NJ, USA, 2002; Volume 3, pp. 1881–1882. [Google Scholar]
- Yew, H.T.; Kheau, C.; Chin, R.; Chekima, A.; Satria, M.H. Improved-TOPSIS Based Handover Scheme for Telemedicine Service Using Heterogeneous Wireless Networks. In Proceedings of the 2017 IEEE 2nd International Conference on Automatic Control and Intelligent Systems (I2CACIS), Kota Kinabalu, Malaysia, 21 October 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 155–160. [Google Scholar]
- Sukanesh, R.; Rajan, S.P.; Vijayprasath, S.; Aishwarya, N.; Angela, P.G. Intelligent Wireless Mobile Patient Monitoring System. In Proceedings of the 2010 International Conference On Communication Control and Computing Technologies, Nagercoil, India, 7–9 October 2010; IEEE: Piscataway, NJ, USA, 2010; pp. 540–543. [Google Scholar]
- Choi, Y.B.; Krause, J.S.; Seo, H.; Capitan, K.E.; Chung, K. Telemedicine in the USA: Standardization Through Information Management and Technical Applications. IEEE Commun. Mag. 2006, 44, 41–48. [Google Scholar] [CrossRef]
- Yu, X.; Xia, X.; Chen, X. Design and Application of RuBee-Based Telemedicine Data Acquisition System. In Proceedings of the 2011 10th IEEE/ACIS International Conference on Computer and Information Science, Sanya, China, 16–18 May 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Saravanan, S.; Sudhakar, P. Telemedicine Technology Using Internet Communication. Int. J. Pure Appl. Math. 2017, 115, 147–156. [Google Scholar]
- Celik, N.; Baker, J.; Youn, H.; Iskander, M.F. An Internet Based Interactive Telemedicine System for Remote Healthcare. In Proceedings of the 2010 IEEE Antennas and Propagation Society International Symposium, Toronto, ON, Canada, 11–17 July 2010; IEEE: Piscataway, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Wang, D.; Lu, Y.; Zhang, H.; Shuliang, C.; Han, Y. A Wireless Sensor Network Based on Bluetooth for Telemedicine Monitoring System. In Proceedings of the 2005 IEEE International Symposium on Microwave, Antenna, Propagation and EMC Technologies for Wireless Communications, Beijing, China, 8–12 August 2005; IEEE: Piscataway, NJ, USA, 2005; Volume 2, pp. 1361–1364. [Google Scholar] [CrossRef]
- de Almeida, J.P.L.; Pinto, A.C.; Pereira, J.; Pinto, S.; de Carvalho, M. Implementation of a Wireless Device for Real-Time Telemedical Assistance of Home-Ventilated Amyotrophic Lateral Sclerosis Patients: A Feasibility Study. Telemed. e-Health 2010, 16, 883–888. [Google Scholar] [CrossRef]
- Pandian, P.; Safeer, K.; Shakunthala, D.; Gopal, P.; Padaki, V. Internet Protocol Based Store and Forward Wireless Telemedicine System for VSAT and Wireless Local Area Network. In Proceedings of the 2007 International Conference on Signal Processing, Communications and Networking, Chennai, India, 22–24 February 2007; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Pavlopoulos, S.; Kyriacou, E.; Berler, A.; Dembeyiotis, S.; Koutsouris, D. A Novel Emergency Telemedicine System Based on Wireless Communication Technology-AMBULANCE. IEEE Trans. Inf. Technol. Biomed. 1998, 2, 261–267. [Google Scholar] [CrossRef]
- Lin, C.F. An Advance Wireless Multimedia Communication Application: Mobile Telemedicine. WSEAS Trans. Commun. 2010, 9, 206–215. [Google Scholar]
- Serener, A.; Kavalcioglu, C. Wireless Telemedicine System in Eemergency Medicine Helicopter. In Proceedings of the 11th WSEAS International Conference on Automatic Control, Modelling and Simulation, Istanbul, Turkey, 30 May–1 June 2009. [Google Scholar]
- Ullah. A Telemedicine Network Model for Health Applications in Pakistan: Current Status and Future Prospects. Int. J. Digit. Content Technol. Its Appl. 2009, 3, 149–155. [Google Scholar] [CrossRef]
- Afonso, J.A.; Maio, A.J.F.; Simoes, R. Performance Evaluation of Bluetooth Low Energy for High Data Rate Body Area Networks. Wirel. Pers. Commun. 2016, 90, 121–141. [Google Scholar] [CrossRef]
- Xu, C.; Yang, Y.; Gao, W. Skin-Interfaced Sensors in Digital Medicine: From Materials to Applications. Matter 2020, 2, 1414–1445. [Google Scholar] [CrossRef]
- Krco, S.; Delic, V. Personal wireless sensor network for mobile health care monitoring. In Proceedings of the 6th International Conference on Telecommunications in Modern Satellite, Cable and Broadcasting Service, Nis, Yugoslavia, 1–3 October 2003; Volume 2, pp. 471–474. [Google Scholar] [CrossRef]
- Tarín, C.; Traver, L.; Cardona, N. Wireless Body Area Networks for Telemedicine Applications. Mag. Waves 2009, 1, 124–125. [Google Scholar]
- Mulyadi, I.H.; Supriyanto, E.; Safri, N.M.; Satria, M.H. Wireless Medical Interface Using ZigBee and Bluetooth Technology. In Proceedings of the 2009 Third Asia International Conference on Modelling & Simulation, Bundang, Indonesia, 25–29 May 2009; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Salamon, D.; Grigioni, M.; Gianni, M.; Liberti, M.; De Luca, S.; Bei, A.; D’Inzeo, G. Indoor telemedicine in hospital: A PDA-based flexible solution for wireless monitoring and database integration. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 17–18 January 2006; pp. 386–389. [Google Scholar] [CrossRef]
- Bai, V.T.; Srivatsa, S.K. Design of wearable cardiac telemedicine system. Int. J. Electron. Healthc. 2007, 3, 303. [Google Scholar] [CrossRef]
- Berggren, M. Wireless Communication in Telemedicine Using Bluetooth and IEEE 802.11b; Technology Report; Department of Information Technology Uppsala University: Uppsala, Sweden, 2001. [Google Scholar]
- Collotta, M.; Pau, G.; Talty, T.; Tonguz, O.K. Bluetooth 5: A Concrete Step Forward toward the IoT. IEEE Commun. Mag. 2018, 56, 125–131. [Google Scholar] [CrossRef]
- Yu, B.; Xu, L.; Li, Y. Bluetooth Low Energy (BLE) based mobile electrocardiogram monitoring system. In Proceedings of the 2012 IEEE International Conference on Information and Automation, Shenyang, China, 6–8 June 2012; pp. 763–767. [Google Scholar] [CrossRef]
- Donati, M.; Celli, A.; Ruiu, A.; Saponara, S.; Fanucci, L. A Telemedicine Service System Exploiting BT/BLE Wireless Sensors for Remote Management of Chronic Patients. Technologies 2019, 7, 13. [Google Scholar] [CrossRef]
- Pramanik, P.K.D.; Nayyar, A.; Pareek, G. WBAN: Driving e-healthcare Beyond Telemedicine to Remote Health Monitoring: Architecture and Protocols; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 89–119. [Google Scholar] [CrossRef]
- ImtiazBinHamid, N.; Twarik Harouna, M.; Salele, N.; Muhammad, R. Comparative Analysis of Various Wireless Multimedia Sensor Networks for Telemedicine. Int. J. Comput. Appl. 2013, 73, 39–44. [Google Scholar] [CrossRef]
- Camilo, T.; Oscar, R.; Carlos, L. Biomedical signal monitoring using wireless sensor networks. In Proceedings of the 2009 IEEE Latin-American Conference on Communications, Medellin, Colombia, 10–11 September 2009; pp. 1–6. [Google Scholar] [CrossRef]
- Yadav, A.; Singh, V.K.; Bhoi, A.K.; Marques, G.; Garcia-Zapirain, B.; Díez, I.d.l.T. Wireless body area networks: UWB wearable textile antenna for telemedicine and mobile health systems. Micromachines 2020, 11, 558. [Google Scholar] [CrossRef]
- Lin, C.F.; Ching, Y.L. A DS UWB transmission system for wireless telemedicine. WSEAS Trans. Syst. 2008, 7, 578–588. [Google Scholar]
- Taparugssanagorn, A.; Pomalaza-Ráez, C.; Isola, A.; Tesi, R.; Hämäläinen, M.; Iinatti, J. UWB channel modelling for wireless body area networks in a hospital. Int. J. Ultra Wideband Commun. Syst. 2010, 1, 226–236. [Google Scholar] [CrossRef]
- Lin, C.F.; Lee, H.W. Wireless Multimedia Communication toward Mobile Telemedicine. In Proceedings of the AIC ’09: Proceedings of the 9th Wseas International Conference on Applied Informatics and Communications, Moscow, Russia, 20–22 August 2009; pp. 232–237. [Google Scholar]
- Qu, H.; Cheng, J.; Cheng, Q.; Wang, L.Y. WiFi-Based Telemedicine System: Signal Accuracy and Security. In Proceedings of the 2009 International Conference on Computational Science and Engineering, Vancouver, BC, Canada, 29–31 August 2009; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Lin, C.F. Mobile Telemedicine: A Survey Study. J. Med. Syst. 2010, 36, 511–520. [Google Scholar] [CrossRef]
- Bisu, A.A.; Gallant, A.; Sun, H.; Brigham, K.; Purvis, A. Telemedicine via Satellite: Improving Access to Healthcare for Remote Rural Communities in Africa. In Proceedings of the 2018 IEEE Region 10 Humanitarian Technology Conference (R10-HTC), Malambe, Sri Lanka, 6–8 December 2018. [Google Scholar] [CrossRef]
- Zhao, Y.; Yagi, Y.; Juzoji, H.; Nakajima, I. A Study of Wireless IP for Telemedicine. In Proceedings of the Fourth International Symposium on Multimediam Communications (WPWC’01), Alborg, Denmark, 3–7 September 2001; Volume 3. [Google Scholar]
- Yamauchi, K.; Chen, W.; Wei, D. 3G Mobile Phone aAplications in Telemedicine—A Survey. In Proceedings of the Fifth International Conference on Computer and Information Technology (CIT’05), Shanghai, China, 21–23 September 2005; IEEE: Piscataway, NJ, USA, 2005. [Google Scholar] [CrossRef]
- Yousef, J.; Lars, A. Validation of a Real-Time Wireless Telemedicine System, Using Bluetooth Protocol and a Mobile Phone, for Remote Monitoring Patient in Medical Practice. Eur. J. Med. Res. 2005, 10, 254–262. [Google Scholar]
- Adarsh, A.; Pathak, S.; Kumar, B. Design and Analysis of a Reliable, Prioritized and Cognitive Radio-Controlled Telemedicine Network Architecture for Internet of Healthcare Things. Int. J. Comput. Netw. Appl. 2021, 8, 54–66. [Google Scholar] [CrossRef]
- Mehta, H.; Patel, D.; Joshi, B.; Modi, H. 0G to 5G Mobile Technology: A Survey. J. Basic Appl. Eng. Res. 2014, 1, 56–60. [Google Scholar]
- Kayyali, S. Resource Management and Quality of Service Provisioning in 5G Cellular Networks. arXiv 2020, arXiv:2008.09601. [Google Scholar]
- Mukhopadhyay, A.; Hegde, R.R.; Thomas, A.S. Handover Mechanisms in Wireless Heterogeneous Telemedicine Networks. In Proceedings of the 2019 3rd International Conference on Computing Methodologies and Communication (ICCMC), Erode, India, 27–29 March 2019; pp. 938–945. [Google Scholar] [CrossRef]
- Agiwal, M.; Roy, A.; Saxena, N. Next Generation 5GWireless Networks: A Comprehensive Survey. IEEE Commun. Surv. Tutorials 2016, 18, 1617–1655. [Google Scholar] [CrossRef]
- Noohani, M.S.; Magsi, K.U. A Review of 5G Technology: Architecture, Security and wide Applications. Int. Res. J. Eng. Technol. (IRJET) 2020, 7, 3440–3471. [Google Scholar] [CrossRef]
- Husni, E.; Heryadi, Y.; Woon, W.; Arifianto, M.; Viswacheda, D.; Barukang, L. Mobile Ad Hoc Network and Mobile IP for Future Mobile Telemedicine System. In Proceedings of the 2006 IFIP International Conference on Wireless and Optical Communications Networks, Bangalore, India, 11–13 April 2006; IEEE: Piscataway, NJ, USA, 2006; pp. 5–11. [Google Scholar]
- Beck, J.A.; Jensen, J.A.; Putzier, R.F.; Stubert, L.A.; Stuart, K.D.; Mohammed, H.; Kreofsky, B.L.; Boles, K.W.; Colby, C.E.; Fang, J.L. Developing a Newborn Resuscitation Telemedicine Program: A Comparison of Two Technologies. Telemed. e-Health 2018, 24, 481–488. [Google Scholar] [CrossRef]
- Vlissidis, N.; Leonidas, F.; Giovanis, C.; Marinos, D.; Aidinis, K.; Vassilopoulos, C.; Pagiatakis, G.; Schmitt, N.; Pistner, T.; Klaue, J. A sensor monitoring system for telemedicine, safety and security applications. Int. J. Electron. 2017, 104, 297–311. [Google Scholar] [CrossRef]
- Chand, R.D.; Kumar, A.; Kumar, A.; Tiwari, P.; Rajnish, R.; Mishra, S.K. Advanced Communication Technologies for Collaborative Learning in Telemedicine and Tele-care. In Proceedings of the 2019 9th International Conference on Cloud Computing, Data Science & Engineering (Confluence), Noida, India, 10–11 January 2019; pp. 601–605. [Google Scholar] [CrossRef]
- LeRouge, C.; Garfield, M.J.; Hevner, A.R. Quality Attributes in Telemedicine Video Conferencing. In Proceedings of the 35th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 10 January 2002; IEEE: Piscataway, NJ, USA, 2002; pp. 2050–2059. [Google Scholar]
- Aziz, J.S.; Hussein, O.A.; Naoom, A. Design of Telemedicine Systems for Rural and Urban Areas in Iraq. ARPN J. Eng. Appl. Sci. 2009, 4, 71. [Google Scholar]
- Bowater, M. The Experience of a Rural General Practitioner Using Videoconferencing for Telemedicine. J. Telemed. Telecare 2001, 7, 24–25. [Google Scholar] [CrossRef]
- Yamamoto, L.G.; Williams, D.R. A Demonstration of Instant Pocket Wireless CT Teleradiology to Facilitate Stat Neurosurgical Consultation and Future Telemedicine Implications. Am. J. Emerg. Med. 2000, 18, 423–426. [Google Scholar] [CrossRef]
- Suliman Munawar, H.; Ali Awan, A.; Khalid, U.; Munawar, S.; Maqsood, A. Revolutionizing Telemedicine by Instilling H.265. Int. J. Image Graph. Signal Process. 2017, 9, 20–27. [Google Scholar] [CrossRef]
- Chorbev, I.; Mihajlov, M. Building a Wireless Telemedicine Network within a WiMax Based Networking Infrastructure. In Proceedings of the 2009 IEEE International Workshop on Multimedia Signal Processing, Rio de Janeiro, Brazil, 5–7 October 2009; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Garawi, S.; Istepanian, R.; Abu-Rgheff, M. 3G Wireless Communications for Mobile Robotic Tele-Ultrasonography Systems. IEEE Commun. Mag. 2006, 44, 91–96. [Google Scholar] [CrossRef]
- Niyato, D.; Hossain, E.; Diamond, J. IEEE 802.16/WiMAX-Based Broadband Wireless Access and its Application for Telemedicine/e-Health Services. IEEE Wirel. Commun. 2007, 14, 72–83. [Google Scholar] [CrossRef]
- Chu, Y.; Ganz, A. Mobile Telemedicine Systems Using 3G Wireless Networks. Bus. Brief. US Healthc. Strateg. 2005, 20, 2007. [Google Scholar]
- Chu, Y.; Ganz, A. WISTA: A Wireless Telemedicine System for Disaster Patient Care. Mob. Netw. Appl. 2007, 12, 201–214. [Google Scholar] [CrossRef]
- Pedersen, P.C.; Dickson, B.W.; Chakareski, J. Telemedicine Applications of Mobile Ultrasound. In Proceedings of the 2009 IEEE International Workshop on Multimedia Signal Processing, Rio de Janeiro, Brazil, 5–7 October 2009; IEEE: Piscataway, NJ, USA, 2009; pp. 1–6. [Google Scholar]
- Chenthara, S.; Ahmed, K.; Wang, H.; Whittaker, F. Security and Privacy-Preserving Challenges of e-Health Solutions in Cloud Computing. IEEE Access 2019, 7, 74361–74382. [Google Scholar] [CrossRef]
- Ashu, A.; Sharma, S. Ashu, A.; Sharma, S. A Novel Approach of Telemedicine for Managing Fetal Condition Based on Machine Learning Technology from IoT-Based Wearable Medical Device. In Machine Learning and the Internet of Medical Things in Healthcare; Elsevier: Amsterdam, The Netherlands, 2021; pp. 113–134. [Google Scholar] [CrossRef]
- Yew, H.T.; Supriyanto, E.; Haikal, M.; Hau, Y.W. A Vertical Handover Management for Mobile Telemedicine System Using Heterogeneous Wireless Networks. Int. J. Adv. Comput. Sci. Appl. 2016, 7, 1–9. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).