Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews
Abstract
1. Introduction
1.1. Virtual Reality’s Transformative Role in Healthcare: An Introduction
1.2. Virtual Reality and Radiology: Exploring Related Studies to Formulate Hypotheses and Research Directions
1.2.1. Radiology Meets Digital Health: A Seamless Blend
1.2.2. Digital Radiology Meets Virtual Reality: Proposing Hypotheses and Research Avenues
1.2.3. Virtual Reality in Radiology: Technological Components, Integration towards Extended Reality, and the Contribution of COVID-19 to Research Expansion
Technological Components and Integration towards Extended Reality
The Contribution of COVID-19 to Research Expansion
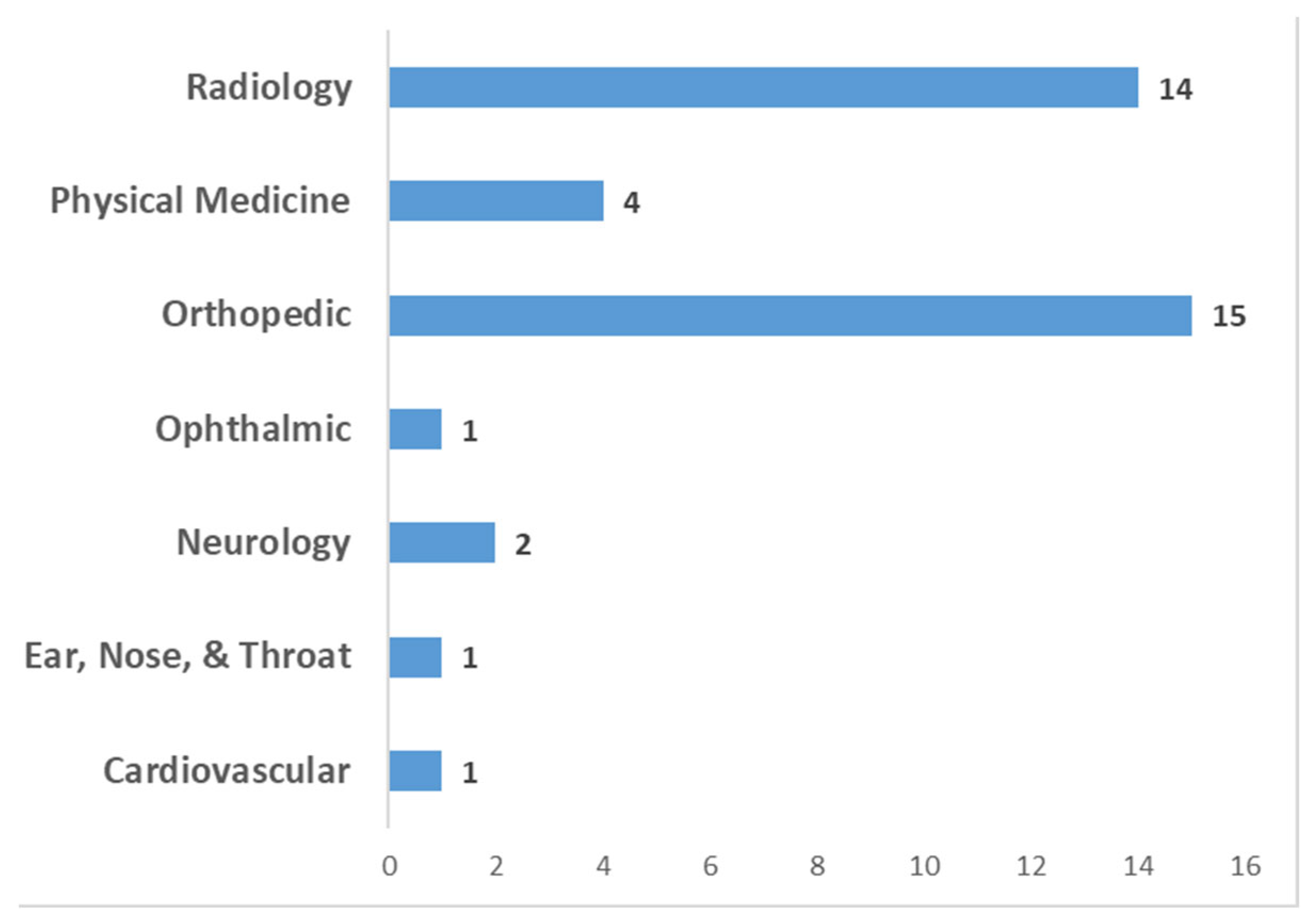
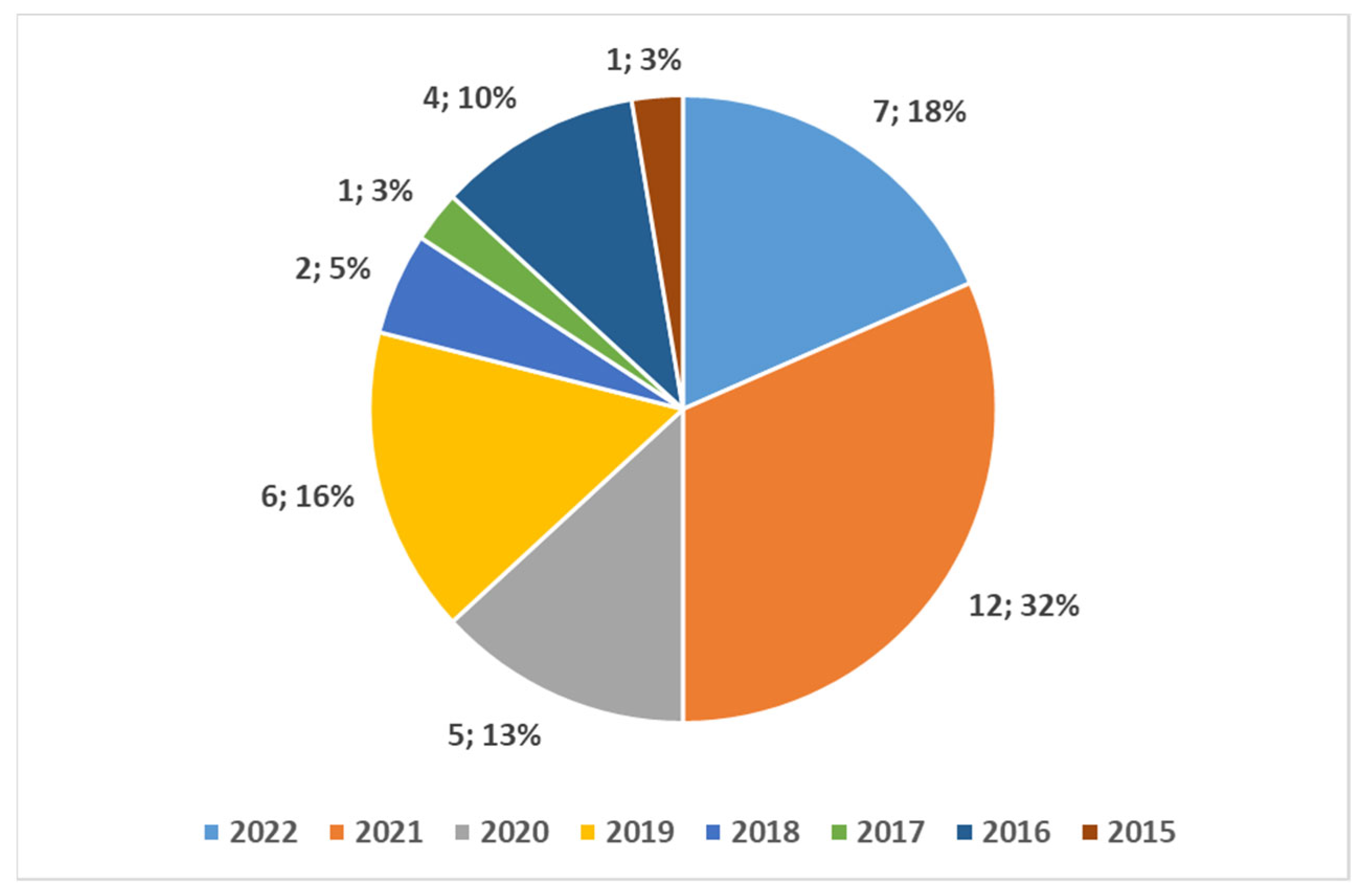
- FDA approval initiatives for VR (and AR) tools as Medical Devices, started in 2015, have gradually accelerated from 2020 (until 2022) [7] (see also: Table 2, based on an Excel dump from the public register; and the graphical presentation in Figure 2 and Figure 3) with 63% of approval in the years 2020–2022.
- The COVID-19 Pandemic’s momentum since 2020 has acted as a catalyst for numerous innovative technologies in the medical field.
Standardization of VR in the Health Domain with a Focus on Radiology
- The transition towards this European directive from the previous one [70] will conclude by May 2024 with adoption across all member states.
- A delay in adopting technological innovations such as VR is highlighted, along with an invitation for more concrete actions. According to the authors, it must be clearly understood how a VR software for medical application [71,72] differs from a general exergame [73], considering the various medical areas in which VR [74] can be applied.
1.3. The Rationale for a Narrative Review Study in This Field
- What do scholars mean by Virtual Reality in radiology applications, and how do they perceive it?
- How has the integration of Virtual Reality in radiology evolved over time, and what significant advancements and challenges have shaped this intersection, and what are the emerging themes/patterns?
- How has virtual reality been integrated in the radiology domain with other innovative technologies (e.g., robotics, Artificial Intelligence, and Augmented Reality)?
- In what ways has Virtual Reality demonstrated its potential to enhance diagnostic capabilities, improve medical training, or transform patient care within the field of radiology, and what are the current obstacles to overcome?
1.4. Purpose of the Study
2. Materials and Methods
- Clarity of study rationale in the Introduction.
- Appropriateness of work’s design.
- Clarity in describing methods.
- Clear presentation of results.
- Justification and alignment of conclusions with results.
- Adequate disclosure of conflicts of interest by authors.
- -
- Each of the first five parameters must obtain a minimum score of 3.
- -
- The last parameter must be marked as “Yes” for conflict disclosure.
3. Results
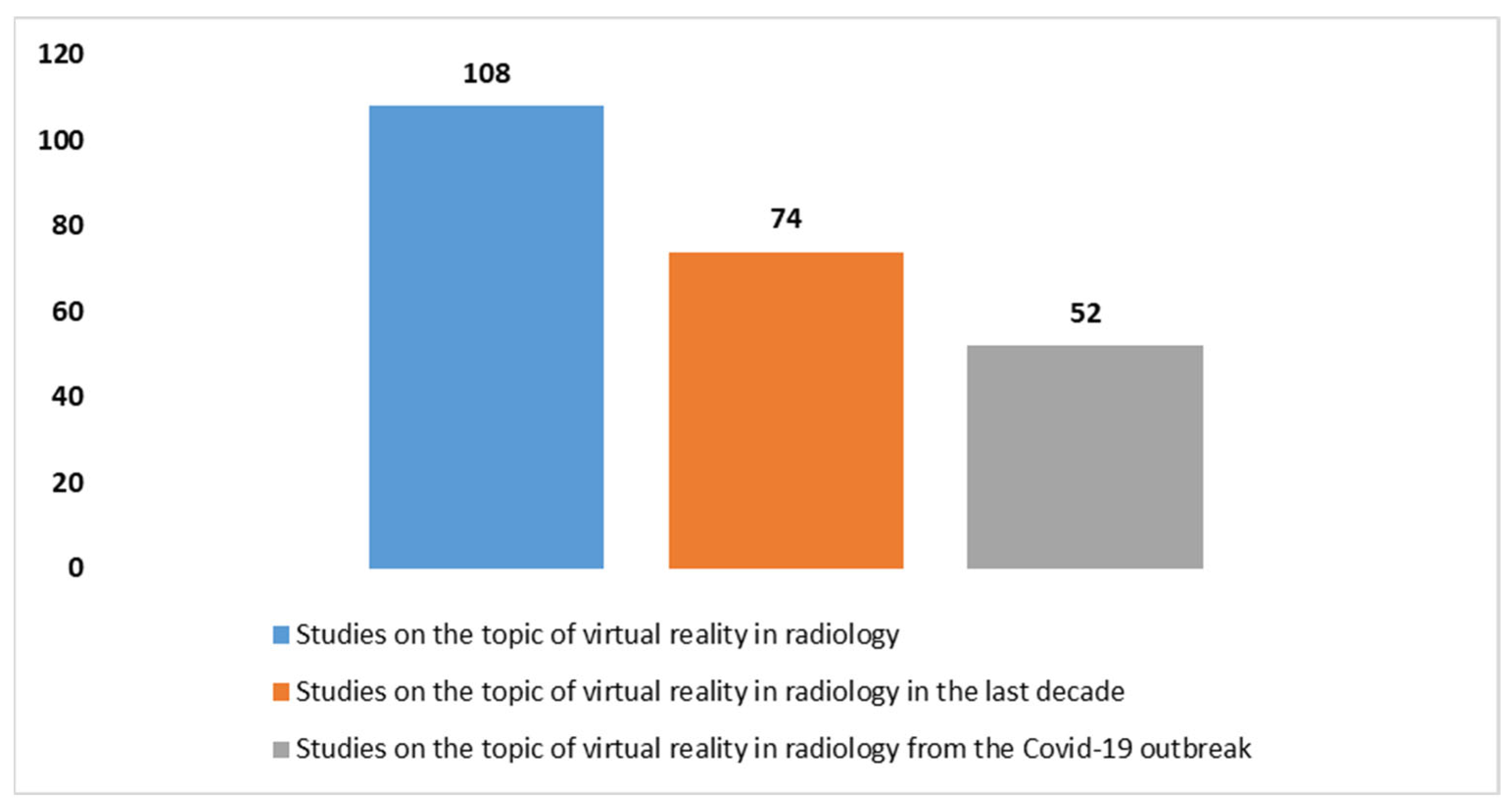
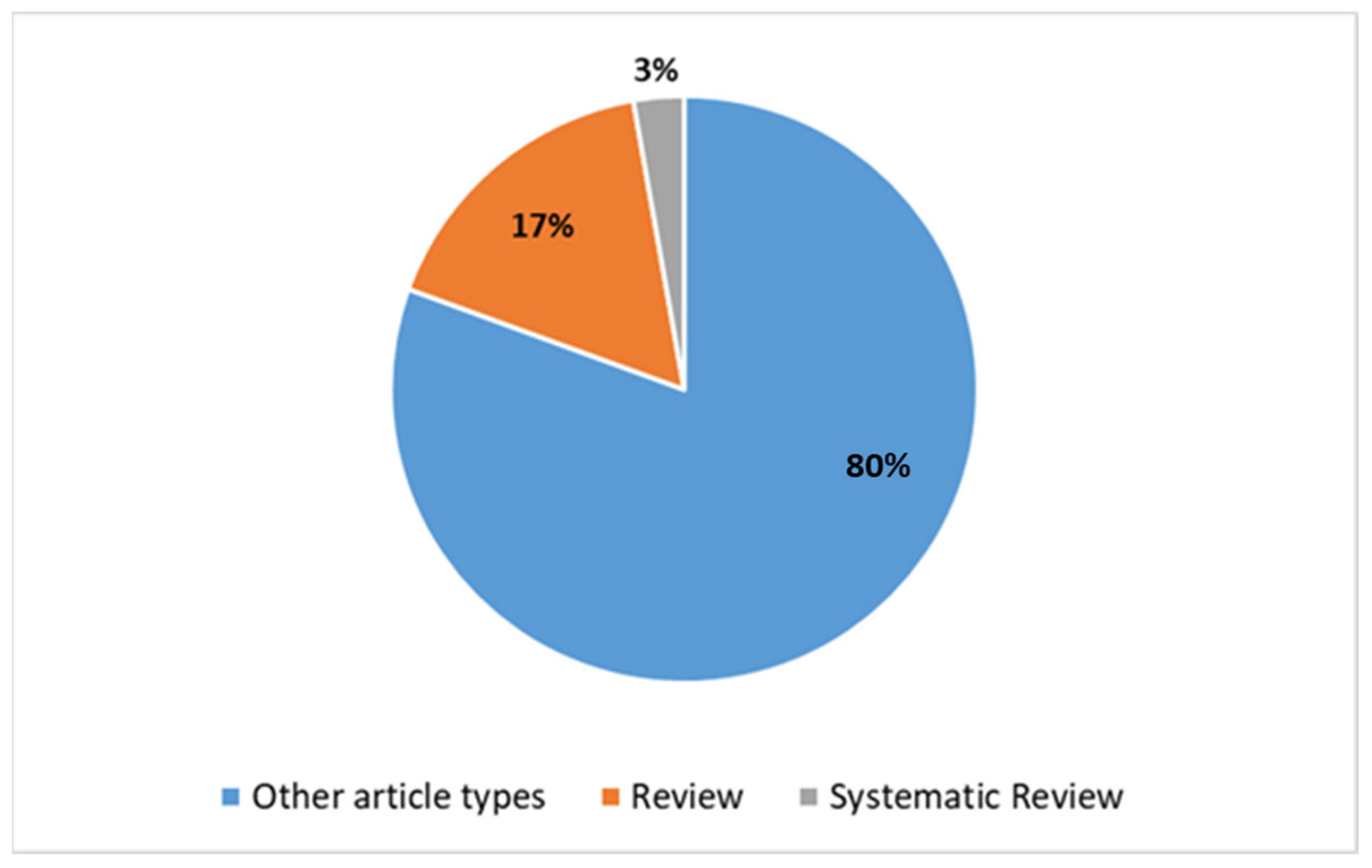
3.1. The Trends in the Studies on Virtual Reality in the Field of Radiology
| (virtual reality[Title/Abstract]) AND (radiology[Title/Abstract]) |
| (Virtual Reality[Title/Abstract]) AND (Radiology[Title/Abstract]) AND (applications[Title/Abstract]) |
| (virtual reality[Title/Abstract]) AND (radiology[Title/Abstract]) AND (robotics) |
3.2. Key Findings: Common Emerging Message and Emerging Themes/Patterns
3.2.1. Common Emerging Message
- Firstly, the phenomenon of “cyber sickness” is a notable concern. This refers to discomfort experienced by users, including symptoms like nausea and dizziness, which can occur when using VR and AR applications. The underlying cause is often attributed to a mismatch between the visual perception of motion and the input from the vestibular system. To mitigate this, developers are exploring various strategies such as synchronizing movement with the user’s head motion and improving tracking accuracy.
- Secondly, in the realm of the VR and AR, ensuring accurate localization of virtual reconstructions over real-world anatomy is essential during image-guided procedures. Challenges include overcoming respiratory motion and organ deformation while maintaining smooth and accurate image movement. Moreover, the AR device must seamlessly integrate with the operator’s senses and be lightweight and comfortable for prolonged use.
- Furthermore, while VR and AR have the potential to simulate reality, achieving high levels of realism requires substantial resources and expertise. Hence, prioritizing simpler simulations for tasks like training may offer more immediate value.
- Caution is warranted in the adoption of VR and AR technologies in radiology and generally in the health domain. Regulatory approvals aside, rigorous research is needed to ascertain their efficacy in improving medical workflows and patient outcomes. Additionally, ethical concerns arise regarding the potential for inaccurate simulations to impact training quality and patient care. Collaborative oversight involving medical professionals, developers, and regulatory bodies is essential to ensure responsible integration.
3.2.2. Emerging Themes/Patterns
- Integration of VR and AR in radiology
- Integration of VR with AI and impact on Radiology
- Educational Applications of VR integrated with AR in radiologyGelmini et al. [83], Chytas et al. [86], and McBain et al. [95] explore the effectiveness of VR and AR in medical education, particularly in radiology and anatomy, based on digital radiology imaging. The positive reception and effectiveness of these technologies in enhancing learning and skills acquisition are highlighted.
- User Interface (UI) Evolution with VR in RadiologyIannessi et al. [97] delve into the evolution of user interfaces in radiology, emphasizing the need for radiologist-specific UIs for better acceptance and usability. The study discusses alternatives such as touchscreens, kinetic sensors, and augmented/virtual reality for two- and three-dimensional imaging.
- SBME and Training with VR in radiologyReviews by Rooney et al. [99], Dankelman et al. [89], and Alvarez-Lopez et al. [100] focus on the importance of SBME and training, especially in radiation oncology, interventional radiology, and surgery. The effectiveness of VR and other technologies in providing realistic and cost-effective training solutions is highlighted.
- Advances in Imaging Technology and VR in radiologyRavindran [92], Dammann [97], ter Haar Romeny et al. [98], and Zhao et al. [94] discuss technological advances of VR integration with the digital radiology. The reviews emphasize improvements in image quality, 3D visualization, and the application of novel technologies, such as the 3D printing [92], both in diagnostic and interventional radiology.
- Application of VR integration into radiology in Advanced Technology integration in DentistrySinghal et al. [96] specifically highlight the potential impact of VR, AR, and 3D printing in dentistry based on digital radiology imaging, covering aspects such as diagnosis, surgery, and patient care.
- Shift in radiology education and Personalized LearningGuimarães et al. [93] discuss the evolving trends in medical education, emphasizing a shift towards integrating basic and clinical sciences using technologies like 3D modeling and digital imaging. The potential role of AI and VR in personalized learning processes is highlighted.
- Integration of VR into Extended Reality (ER) in Diagnostic radiology ImagingKukla et al. [90] focus on the use of ER in diagnostic radiology imaging, emphasizing its positive impact on patient positioning, medical education, and reduction of anesthesia use.
- VR and Advancements in Difficult Airway ManagementRavindran [92] outlines advancements in managing difficult airways, including both the role of the digital radiology and 3D printing, suggesting opportunities in this field.
3.2.3. The Focus on the Role of the Radiology and on the Virtual Reality in the Overviewed Studies
4. Discussion
4.1. Interpretation of Results of the Narrative Review, Opportunities, Limitations, and Suggestions for a Broader Investigation
4.1.1. Emerging Opportunities
4.1.2. Emerging Limitations and Areas Needing Broader Investigation
4.2. Assessing Initial Assumptions: A Reflective Perspective and Comparative Analysis
4.3. Advancements in Robotic Integration and Further Considerations
4.3.1. Highlights and Deepening from the Overview of Reviews
4.3.2. A Complementary Review
4.3.3. Further Considerations on the Integrations with the Robotics
4.4. Synoptic Diagram
4.5. Takeaway Message
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
List of Acronyms
| VR | Virtual Reality |
| AR | Augmented Reality |
| FDA | Food and Drug administration |
| DICOM | Digital Information and Communication |
| PACS | Picture Archiving and Communication System |
| RIS | Radiology Information System |
| CT | Computed Tomography |
| MRI | Magnetic Resonance Imaging |
| VAR | Virtual and Augmented Reality |
| ER | Extended Reality (1st definition) |
| XR | Extended Reality (2nd definition) |
| MR | Mixed Reality |
| HMD | Head Mounted Device |
| CAVE | Cave Automatic Virtual Environment |
| AI | Artificial Intelligence |
| SBME | Simulation-based medical education |
| UI | Unit Interface |
| IR | Interventional Radiology |
| COTS | Commercial off-the-shelf |
| MK | Microsoft Kinect |
| LMC | Leap Motion Controller |
References
- Kouijzer, M.M.T.E.; Kip, H.; Bouman, Y.H.A.; Kelders, S.M. Implementation of virtual reality in healthcare: A scoping review on the implementation process of virtual reality in various healthcare settings. Implement. Sci. Commun. 2023, 4, 67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Erdilek, D.; Gümüştaş, B.; Efes, B.G. Digitalization era of dental education: A systematic review. Dent. Med. Probl. 2023, 60, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Foronda, C.L.P.; Gonzalez, L.P.; Meese, M.M.M.; Slamon, N.; Baluyot, M.; Lee, J.M.; Aebersold, M.P. A Comparison of Virtual Reality to Traditional Simulation in Health Professions Education. Simul. Health J. Soc. Simul. Health 2023, 19, S90–S97. [Google Scholar] [CrossRef] [PubMed]
- Said, R.R.; Bin Heyat, B.; Song, K.; Tian, C.; Wu, Z. A Systematic Review of Virtual Reality and Robot Therapy as Recent Rehabilitation Technologies Using EEG-Brain–Computer Interface Based on Movement-Related Cortical Potentials. Biosensors 2022, 12, 1134. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kanschik, D.; Bruno, R.R.; Wolff, G.; Kelm, M.; Jung, C. Virtual and augmented reality in intensive care medicine: A systematic review. Ann. Intensiv. Care 2023, 13, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Osservatorio Terapie Avanzate. IL PORTALE ITALIANO DEDICATO ALL’INFORMAZIONE E ALLA DIVULGAZIONE SULLE TERAPIE AVANZATE. Available online: https://www.osservatorioterapieavanzate.it/innovazioni-tecnologiche/digital-health/realta-virtuale-tecnologie-dirompenti-al-servizio-della-medicina (accessed on 15 April 2024).
- Available online: https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices?utm_medium=email&utm_source=govdelivery&utm_source=STAT+Newsletters&utm_campaign=1f31ee8897-health_tech_COPY_01&utm_medium=email&utm_term=0_8cab1d7961-1f31ee8897-151808433 (accessed on 15 April 2024).
- Žiak, P.; Holm, A.; Halička, J.; Mojžiš, P.; Piñero, D.P. Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: Preliminary results. BMC Ophthalmol. 2017, 17, 105. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.dicomstandard.org/ (accessed on 15 April 2024).
- Pirrera, A.; Giansanti, D. Human–Machine Collaboration in Diagnostics: Exploring the Synergy in Clinical Imaging with Artificial Intelligence. Diagnostics 2023, 13, 2162. [Google Scholar] [CrossRef] [PubMed]
- DICOM Whole Slide Imaging (WSI). NEMA. Available online: http://dicom.nema.org/Dicom/DICOMWSI/ (accessed on 15 April 2024).
- Giansanti, D.; Grigioni, M.; D’Avenio, G.; Morelli, S.; Maccioni, G.; Bondi, A.; Giovagnoli, M.R. Virtual microscopy and digital cytology: State of the art. Ann. Ist. Super. Sanità 2010, 46, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Kahn, C.E.; Carrino, J.A.; Flynn, M.J.; Peck, D.J.; Horii, S.C. DICOM and Radiology: Past, Present, and Future. J. Am. Coll. Radiol. 2007, 4, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Hu, G.; Yan, J.; Li, D. Analysis of DICOM and its application in teleradiology. J. Biomed. Eng. 2003, 20, 171–174. (In Chinese) [Google Scholar] [PubMed]
- Valenzuela, T.F.; Iaizzo, P.A. Post-procedure micro-CT analyses of coronary artery stenting in left main vessels of reanimated and perfusion-fixed human hearts. Biomed. Eng. Online 2023, 22, 27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=%28Virtual+Reality%5BTitle%2FAbstract%5D%29+AND+%28Radiology%5BTitle%2FAbstract%5D%29&sort=date&size=200 (accessed on 15 April 2024).
- Javaid, M.; Haleem, A.; Singh, R.P.; Khan, S. Understanding roles of virtual reality in radiology. Internet Things Cyber-Phys. Syst. 2022, 2, 91–98. [Google Scholar] [CrossRef]
- Abramson, Z.; Thompson, D.; Goode, C.; Morin, C.E.; Daniels, S.; Choudhri, A.F.; Davidoff, A.M. Current and emerging 3D visualization technologies in radiology. Pediatr. Radiol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, A.R.; Moloudi, F.; Balasalle, E.; Lang, M.; Uppot, R.N. Virtual Reading Room for Diagnostic Radiology. Curr. Probl. Diagn. Radiol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://dictionary.cambridge.org/it/dizionario/inglese/virtual-reality (accessed on 15 April 2024).
- Available online: https://www.collinsdictionary.com/it/dizionario/inglese/virtual-reality (accessed on 15 April 2024).
- Available online: https://www.merriam-webster.com/dictionary/virtual%20reality (accessed on 15 April 2024).
- Yadav, S. Transformative Frontiers: A Comprehensive Review of Emerging Technologies in Modern Healthcare. Cureus 2024, 16, e56538. [Google Scholar] [CrossRef] [PubMed]
- Ammanuel, S.; Brown, I.; Uribe, J.; Rehani, B. Creating 3D models from Radiologic Images for Virtual Reality Medical Education Modules. J. Med. Syst. 2019, 43, 166. [Google Scholar] [CrossRef] [PubMed]
- Uppot, R.N.; Laguna, B.; McCarthy, C.J.; De Novi, G.; Phelps, A.; Siegel, E.; Courtier, J. Implementing Virtual and Augmented Reality Tools for Radiology Education and Training, Communication, and Clinical Care. Radiology 2019, 291, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Mandalika, V.B.H.; Chernoglazov, A.I.; Billinghurst, M.; Bartneck, C.; Hurrell, M.A.; Ruiter, N.; Butler, A.P.H.; Butler, P.H. A Hybrid 2D/3D User Interface for Radiological Diagnosis. J. Digit. Imaging 2018, 31, 56–73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Douglas, D.B.; Venets, D.; Wilke, C.; Gibson, D.; Liotta, L.; Petricoin, E.; Beck, B.; Douglas, R. Augmented Reality and Virtual Reality: Initial Successes in Diagnostic Radiology. In State of the Art Virtual Reality and Augmented Reality Knowhow; IntechOpen: London, UK, 2018. [Google Scholar]
- Hopper, K.D.; Iyriboz, A.T.; Wise, S.W.; Neuman, J.D.; Mauger, D.T.; Kasales, C.J. Mucosal Detail at CT Virtual Reality: Surface versus Volume Rendering. Radiology 2000, 214, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.S.M.; Evers, V.; Zudilova, E.V.; Sloot, P.M.A. Context analysis to support development of virtual reality applications. Virtual Real. 2004, 7, 177–186. [Google Scholar] [CrossRef]
- King, F.; Jayender, J.; Bhagavatula, S.K.; Shyn, P.B.; Pieper, S.; Kapur, T.; Lasso, A.; Fichtinger, G. An Immersive Virtual Reality Environment for Diagnostic Imaging. J. Med. Robot. Res. 2016, 1, 1640003. [Google Scholar] [CrossRef]
- Ong, C.S.; Deib, G.; Yesantharao, P.; Qiao, Y.; Pakpoor, J.; Hibino, N.; Hui, F.; Garcia, J.R. Virtual Reality in Neurointervention. J. Vasc. Intervent. Neurol. 2018, 10, 17–22. [Google Scholar]
- Xin, M.; Lei, Z.; Volkau, I.; Weili, Z.; Aziz, A.; Ang, M.; Nowinski, W. A Virtual Reality Simulator for Remote Interventional Radiology: Concept and Prototype Design. IEEE Trans. Biomed. Eng. 2006, 53, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Garg, T.; Loya, M.F.; Shrigiriwar, A. Virtual Reality and Its Applications in Interventional Radiology. Acad. Radiol. 2020, 27, 1495. [Google Scholar] [CrossRef] [PubMed]
- Venson, J.; Berni, J.A.; da Silva Maia, C.E.; da Silva, A.M.; d’Ornellas, M.C.; Maciel, A. A case-based study with radiologists performing diagnosis tasks in virtual reality. In MEDINFO 2017: Precision Healthcare through Informatics: Proceedings of the 16th World Congress on Medical and Health Informatics; IOS Press: Amsterdam, The Netherlands, 2018; Volume 245, p. 244. [Google Scholar]
- Javaid, M.; Haleem, A.; Khan, I.H. Virtual reality (VR) applications in dentistry: An innovative technology to embrace. Indian J. Dent. Res. 2020, 31, 666–667. [Google Scholar] [CrossRef] [PubMed]
- Goha, K.Y. Virtual reality applications in neurosurgery. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 17–18 January 2006; IEEE: New York, NY, USA, 2006; pp. 4171–4173. [Google Scholar]
- Noguera Aguilar, J.F. Digital imaging, virtual and augmented reality. Cir. Esp. 2024; in press. [Google Scholar] [CrossRef] [PubMed]
- Nakata, N.; Suzuki, N.; Hattori, A.; Hirai, N.; Miyamoto, Y.; Fukuda, K. Informatics in Radiology: Intuitive User Interface for 3D Image Manipulation Using Augmented Reality and a Smartphone as a Remote Control. RadioGraphics 2012, 32, E169–E174. [Google Scholar] [CrossRef]
- Available online: https://www.merriam-webster.com/dictionary/augmented%20reality (accessed on 15 April 2024).
- Spiegel, B.M.R.; Rizzo, A.; Persky, S.; Liran, O.; Wiederhold, B.; Woods, S.; Donovan, K.; Sarkar, K.; Xiang, H.; Joo, S.; et al. What Is Medical Extended Reality? A Taxonomy Defining the Current Breadth and Depth of an Evolving Field. J. Med. Ext. Real. 2024, 1, 4–12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Solbiati, L.A. Augmented Reality: Thrilling Future for Interventional Oncology? Cardiovasc. Interv. Radiol. 2021, 44, 782–783. [Google Scholar] [CrossRef] [PubMed]
- Goo, H.W.; Park, S.J.; Yoo, S.-J. Advanced Medical Use of Three-Dimensional Imaging in Congenital Heart Disease: Augmented Reality, Mixed Reality, Virtual Reality, and Three-Dimensional Printing. Korean J. Radiol. 2020, 21, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Takata, T.; Nakabayashi, S.; Kondo, H.; Yamamoto, M.; Furui, S.; Shiraishi, K.; Kobayashi, T.; Oba, H.; Okamoto, T.; Kotoku, J. Mixed Reality Visualization of Radiation Dose for Health Professionals and Patients in Interventional Radiology. J. Med. Syst. 2021, 45, 38. [Google Scholar] [CrossRef] [PubMed]
- Werner, H.; Dos Santos, J.R.L.; Ribeiro, G.; Júnior, E.A. Prenatal Phenotype of Down Syndrome Using 3-D Virtual Reality. J. Obstet. Gynaecol. Can. 2017, 39, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.sciencedirect.com/topics/engineering/head-mounted-device (accessed on 15 April 2024).
- Available online: https://www.techtarget.com/whatis/definition/CAVE-Cave-Automatic-Virtual-Environment (accessed on 15 April 2024).
- Jung, A.R.; Park, E.A. The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery. Int. J. Environ. Res. Public Health 2022, 19, 4823. [Google Scholar] [CrossRef] [PubMed]
- Combe, T.; Chardonnet, J.R.; Merienne, F.; Ovtcharova, J. CAVE and HMD: Distance perception comparative study. Virtual Real. 2023, 27, 2003–2013. [Google Scholar] [CrossRef] [PubMed]
- López-Ojeda, W.; Hurley, R.A. Extended-Reality Technologies: An Overview of Emerging Applications in Medical Education and Clinical Care. J. Neuropsychiatry 2021, 33, A4–A177. [Google Scholar] [CrossRef]
- Kang, S.L.; Shkumat, N.; Dragulescu, A.; Guerra, V.; Padfield, N.; Krutikov, K.; Chiasson, D.A.; Chaturvedi, R.R.; Yoo, S.J.; Benson, L.N. Mixed-reality view of cardiac specimens: A new approach to understanding complex intracardiac congenital lesions. Pediatr. Radiol. 2020, 50, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Mehraeen, E.; SeyedAlinaghi, S.; Heydari, M.; Karimi, A.; Mahdavi, A.; Mashoufi, M.; Sarmad, A.; Mirghaderi, P.; Shamsabadi, A.; Qaderi, K.; et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review. Health Inform. J. 2023, 29, 14604582231167431. [Google Scholar] [CrossRef] [PubMed]
- Hayre, C.M.; Kilgour, A. Diagnostic radiography education amidst the COVID-19 pandemic: Current and future use of virtual reality (VR). J. Med. Imaging Radiat. Sci. 2021, 52, S20–S23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oulefki, A.; Agaian, S.; Trongtirakul, T.; Benbelkacem, S.; Aouam, D.; Zenati-Henda, N.; Abdelli, M.-L. Virtual Reality visualization for computerized COVID-19 lesion segmentation and interpretation. Biomed. Signal Process. Control 2021, 73, 103371. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yeung, A.W.K.; Parvanov, E.D.; Hribersek, M.; Eibensteiner, F.; Klager, E.; Kletecka-Pulker, M.; Rössler, B.; Schebesta, K.; Willschke, H.; Atanasov, A.G.; et al. Digital Teaching in Medical Education: Scientific Literature Landscape Review. JMIR Med. Educ. 2022, 8, e32747. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, J.; Lyu, L.; Chai, S.; Huang, H.; Wang, F.; Tateyama, T.; Lin, L.; Chen, Y. Augmented Reality Visualization and Quantification of COVID-19 Infections in the Lungs. Electronics 2024, 13, 1158. [Google Scholar] [CrossRef]
- Amara, K.; Aouf, A.; Kerdjidj, O.; Kennouche, H.; Djekoune, O.; Guerroudji, M.A.; Zenati, N.; Aouam, D. Augmented Reality for COVID-19 Aid Diagnosis: Ct-Scan segmentation based Deep Learning. In Proceedings of the 2022 7th International Conference on Image and Signal Processing and their Applications (ISPA), Mostaganem, Algeria, 8–9 May 2022. [Google Scholar]
- Benbelkacem, S.; Oulefki, A.; Agaian, S.; Zenati-Henda, N.; Trongtirakul, T.; Aouam, D.; Masmoudi, M.; Zemmouri, M. COVI3D: Automatic COVID-19 CT Image-Based Classification and Visualization Platform Utilizing Virtual and Augmented Reality Technologies. Diagnostics 2022, 12, 649. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhugaonkar, K.; Bhugaonkar, R.; Masne, N. The Trend of Metaverse and Augmented & Virtual Reality Extending to the Healthcare System. Cureus 2022, 14, e29071. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsai, T.Y.; Onuma, Y.; Złahoda-Huzior, A.; Kageyama, S.; Dudek, D.; Wang, Q.; Lim, R.P.; Garg, S.; Poon, E.K.W.; Puskas, J.; et al. Merging virtual and physical experiences: Extended realities in cardiovascular medicine. Eur. Heart J. 2023, 44, 3311–3322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ong, T.; Wilczewski, H.; Paige, S.R.; Soni, H.; Welch, B.M.; Bunnell, B.E. Extended Reality for Enhanced Telehealth during and Beyond COVID-19. JMIR Serious Games 2021, 9, e26520. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.fda.gov/media/176814/download (accessed on 15 April 2024).
- Available online: https://www.fda.gov/media/176815/download (accessed on 15 April 2024).
- Available online: https://www.statista.com/statistics/1410751/vr-and-ar-medical-devices-approved-in-the-us-by-area/ (accessed on 15 April 2024).
- Available online: https://www.dicomdirector.com/recent-fda-device-reclassifications/ (accessed on 15 April 2024).
- Available online: https://www.dicomdirector.com/category/intravision-xr/ (accessed on 15 April 2024).
- Available online: https://www.fda.gov/media/160086/download (accessed on 15 April 2024).
- Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32017R0745 (accessed on 15 April 2024).
- Available online: https://health.ec.europa.eu/system/files/2023-10/md_mdcg_2023-4_software_en.pdf (accessed on 15 April 2024).
- Bini, F.; Franzò, M.; Maccaro, A.; Piaggio, D.; Pecchia, L.; Marinozzi, F. Is medical device regulatory compliance growing as fast as extended reality to avoid misunderstandings in the future? Health Technol. 2023, 13, 831–842. [Google Scholar] [CrossRef]
- The European Parliament and the Council of the Euroepan Union. Council Directive 93/42/EEC of 14 June 1993 Concerning Medical Devices. 1993. Available online: http://data.europa.eu/eli/dir/1993/42/oj (accessed on 15 April 2024).
- Baxter, C.; Carroll, J.A.; Keogh, B.; Vandelanotte, C. Seeking inspiration: Examining the validity and reliability of a new smartphone respiratory therapy exergame app. Sensors 2021, 21, 6472. [Google Scholar] [CrossRef] [PubMed]
- Franzò, M.; Pica, A.; Pascucci, S.; Serrao, M.; Marinozzi, F.; Bini, F. A Proof of Concept Combined Using Mixed Reality for Personalized Neurorehabilitation of Cerebellar Ataxic Patients. Sensors 2023, 23, 1680. [Google Scholar] [CrossRef]
- Williams, T.; Kennedy-malone, L.; Thompson, J.; Monge, E.C. The effect of an exergame on physical activity among olderadults residing in a long-term care facility: A pilot study. Geriatr. Nurs. 2022, 44, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Pensieri, C.; Pennacchini, M. Overview: Virtual Reality in Medicine. J. Virtual Worlds Res. 2014, 7. [Google Scholar] [CrossRef]
- Available online: https://www.canhealth.com/2021/07/28/vr-radiology-platform-approved-by-health-canada/ (accessed on 15 April 2024).
- Denyer, D.; Tranfield, D. Producing a Systematic Review. In The Sage Handbook of Organizational Research Methods; Sage Publications Ltd.: New York, NY, USA, 2009. [Google Scholar]
- Sukhera, J. Narrative Reviews: Flexible, Rigorous, and Practical. J. Grad. Med. Educ. 2022, 14, 414–417. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- ANDJ Checklist. Available online: https://www.elsevier.com/__data/promis_misc/ANDJ%20Narrative%20Review%20Checklist.pdf (accessed on 3 June 2023).
- Giansanti, D. An Umbrella Review of the Fusion of fMRI and AI in Autism. Diagnostics 2023, 13, 3552. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=%28Virtual+Reality%5BTitle%2FAbstract%5D%29+AND+%28Radiology%5BTitle%2FAbstract%5D%29&filter=pubt.meta-analysis&filter=pubt.review&filter=pubt.systematicreview&sort=date&size=200 (accessed on 15 April 2024).
- Sutherland, J.; Belec, J.; Sheikh, A.; Chepelev, L.; Althobaity, W.; Chow, B.J.W.; Mitsouras, D.; Christensen, A.; Rybicki, F.J.; La Russa, D.J. Applying Modern Virtual and Augmented Reality Technologies to Medical Images and Models. J. Digit. Imaging 2018, 32, 38–53. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elsayed, M.; Kadom, N.; Ghobadi, C.; Strauss, B.; Al Dandan, O.; Aggarwal, A.; Anzai, Y.; Griffith, B.; Lazarow, F.; Straus, C.M.; et al. Virtual and augmented reality: Potential applications in radiology. Acta Radiol. 2020, 61, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Gelmini, Y.P.; Duarte, M.L.; de Assis, A.M.; Junior, J.B.G.; Carnevale, F.C. Virtual reality in interventional radiology education: A systematic review. Radiol. Bras. 2021, 54, 254–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- von Ende, E.; Ryan, S.; Crain, M.A.; Makary, M.S. Artificial Intelligence, Augmented Reality, and Virtual Reality Advances and Applications in Interventional Radiology. Diagnostics 2023, 13, 892. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gamba, I.A.; Hartery, A. The Virtual Reality Radiology Workstation: Current Technology and Future Applications. Can. Assoc. Radiol. J. 2024. [Google Scholar] [CrossRef] [PubMed]
- Chytas, D.; Salmas, M.; Demesticha, T.; Noussios, G.; Paraskevas, G.; Chrysanthou, C.; Asouhidou, I.; Katsourakis, A.; Fiska, A. A Review of the Use of Virtual Reality for Teaching Radiology in Conjunction with Anatomy. Cureus 2021, 13, e20174. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iannessi, A.; Marcy, P.-Y.; Clatz, O.; Bertrand, A.-S.; Sugimoto, M. A review of existing and potential computer user interfaces for modern radiology. Insights Imaging 2018, 9, 599–609. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gurgitano, M.; Angileri, S.A.; Rodà, G.M.; Liguori, A.; Pandolfi, M.; Ierardi, A.M.; Wood, B.J.; Carrafiello, G. Interventional Radiology ex-machina: Impact of Artificial Intelligence on practice. Radiol. Med. 2021, 126, 998–1006. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dankelman, J.; Wentink, M.; Grimbergen, C.A.; Stassen, H.; Reekers, J. Does Virtual Reality Training Make Sense in Interventional Radiology? Training Skill-, Rule- and Knowledge-Based Behavior. Cardiovasc. Interv. Radiol. 2004, 27, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Kukla, P.; Maciejewska, K.; Strojna, I.; Zapał, M.; Zwierzchowski, G.; Bąk, B. Extended Reality in Diagnostic Imaging—A Literature Review. Tomography 2023, 9, 1071–1082. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, T.Y.; Bedi, H.S.; Deitte, L.A.; Lewis, P.J.; Marx, M.V.; Jordan, S.G. Brave New World: Challenges and Opportunities in the COVID-19 Virtual Interview Season. Acad. Radiol. 2020, 27, 1456–1460. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ravindran, B. Innovations in the Management of the Difficult Airway: A Narrative Review. Cureus 2023, 15, e35117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guimarães, B.; Tsisar, S.; Diniz, J.M.; Madeira, M.D.; Ferreira, M.A. Rethinking Anatomy: How to Overcome Challenges of Medical Education’s Evolution. Acta Med. Port. 2017, 30, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Ma, Y.; Mushtaq, A.; Radhakrishnan, V.; Hu, Y.; Ren, H.; Song, W.; Tse, Z.T.H. Engineering functional and anthropomorphic models for surgical training in interventional radiology: A state-of-the-art review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2022, 237, 3–17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McBain, K.A.; Habib, R.; Laggis, G.; Quaiattini, A.; Ventura, N.M.; Noel, G.P.J.C. Scoping review: The use of augmented reality in clinical anatomical education and its assessment tools. Anat. Sci. Educ. 2021, 15, 765–796. [Google Scholar] [CrossRef] [PubMed]
- Singhal, I.; Kaur, G.; Neefs, D.; Pathak, A.; Singhal, D. A Literature Review of the Future of Oral Medicine and Radiology, Oral Pathology, and Oral Surgery in the Hands of Technology. Cureus 2023, 15, e45804. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dammann, F. Bildverarbeitung in der Radiologie. Rofo 2002, 174, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Romeny, B.M.T.H.; Zuiderveld, K.J.; Van Waes, P.F.G.M.; Van Walsum, T.; Van Der Weijden, R.; Weickert, J.; Stokking, R.; Wink, O.; Kalitzin, S.; Maintz, T.; et al. Advances in three-dimensional diagnostic radiology. J. Anat. 1998, 193, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Rooney, M.K.; Zhu, F.; Gillespie, E.F.; Gunther, J.R.; McKillip, R.P.; Lineberry, M.; Tekian, A.; Golden, D.W. Simulation as More Than a Treatment-Planning Tool: A Systematic Review of the Literature on Radiation Oncology Simulation-Based Medical Education. Int. J. Radiat. Oncol. 2018, 102, 257–283. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alvarez-Lopez, F.; Maina, M.F.; Saigí-Rubió, F. Use of Commercial Off-The-Shelf Devices for the Detection of Manual Gestures in Surgery: Systematic Literature Review. J. Med. Internet Res. 2019, 21, e11925. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://eumdr.com/ (accessed on 15 April 2024).
- Shi, C.; Ishihara, H. Performance Evaluation of a Vascular Interventional Surgery Robotic System with Visual-Based Force Feedback. Machines 2023, 11, 727. [Google Scholar] [CrossRef]
- Marescaux, J.; Diana, M. Next step in minimally invasive surgery: Hybrid image-guided surgery. J. Pediatr. Surg. 2015, 50, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Ni, D. A virtual reality simulator for ultrasound-guided biopsy training. IEEE Comput. Graph. Appl. 2011, 31, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Moix, T.; Ilic, D.; Fracheboud, B.; Zoethout, J.; Bleuler, H. A real-time haptic interface for interventional radiology procedures. Stud. Health Technol. Inform. 2005, 111, 329–333. [Google Scholar] [PubMed]
- Moix, T.; Ilic, D.; Bleuler, H.; Zoethout, J. A haptic device for guide wire in interventional radiology procedures. Med. Meets Virtual Real. 14 2006, 119, 388–392. [Google Scholar]
- Benabid, A.L.; Hoffmann, D.; Ashraf, A.; Koudsie, A.; Esteve, F.; Le-Bas, J.F. La robotisation de la neurochirurgie: État actuel et perspectives d’avenir: The robotization of neurosurgery: State of the art and future outlook. Bull. Acad. Natl. Med. 1997, 181, 1625–1636. [Google Scholar] [PubMed]
- Benabid, A.L.; Hoffmann, D.; Ashraf, A.; Koudsie, A.; Esteve, F.; Le Bas, J.F. La robotisation de la neurochirurgie: État actuel et perspectives d’avenir: Robotics in neurosurgery: Current status and future prospects. Chirurgie 1998, 123, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Liu, Q.; Duan, J.; Qin, J. Research on Teleoperated Virtual Reality Human–Robot Five-Dimensional Collaboration System. Biomimetics 2023, 8, 605. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rudiman, R.; Mirbagheri, A.; Candrawinata, V.S. Assessment of robotic telesurgery system among surgeons: A single-center study. J. Robot. Surg. 2023, 17, 2757–2761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kazemzadeh, K.; Akhlaghdoust, M.; Zali, A. Advances in artificial intelligence, robotics, augmented and virtual reality in neurosurgery. Front. Surg. 2023, 10, 1241923. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://health.ec.europa.eu/system/files/2020-09/md_mdcg_2019_11_guidance_qualification_classification_software_en_0.pdf (accessed on 15 April 2024).




| Topic | Examples |
|---|---|
| Advancing Radiologist Expertise | Acts as a mentorship tool for students, enhancing training and learning. Provides immersive virtual simulations for diagnostic experience. Facilitates knowledge acquisition of innovative procedures, improving preclinical skills for patient safety. |
| Promoting Disease Awareness | Utilizes VR to help illustrating to a patient a medical problem/disease. Offers a comprehensive view for enhanced training and surgical planning. Enables virtual surgical planning for deeper understanding. Enhances patient interaction by sharing information from each visit. Drives awareness of emerging diseases through technology. |
| Enhancing Patient Relaxation | VR serves as a therapeutic solution for patient relaxation in medical scenarios. Expedites physical therapy, contributing to effective recovery. Alleviates stress through immersive VR experiences. Customizable virtual environments reduce stress during treatment. |
| Streamlining Healthcare Expenditure | Reduces overall treatment costs and shortens hospital stays. Lowers expenses in designing medical products. Provides a secure environment for medical professionals, reducing management costs. |
| Innovating Medical Imaging Inspection | VR enables thorough inspection of medical images, expediting analysis. Introduces innovative methods for reviewing and analyzing imaging data. Offers insights for clinical research, creating a conducive learning environment. |
| Improve the Access to Patient Images | Radiologist have the opportunity to interact with images presented in a 3D format. Enhances understanding of patient anatomy. Visualizes complex structures, aiding in accurate diagnoses. |
| Crystal Clear Visualization of Blood Vessels | Provides a 3D representation of blood vessels with an interactive opportunity to interact (rotate/zoom/pan, etc.) Inspects heart vessels, contributing to improved surgeries. VR simulation enhances learning opportunities. |
| Telemonitoring for Remote Healthcare | VR is crucial for remotely monitoring patients. Digitally visualizes real-time information for daily medical procedures. Enables remote-assisted treatment, establishing virtual therapy. |
| Strategic Preoperative Planning | VR plays a crucial role in preoperative planning. Regular patient screenings aid in early identification of potential causes. Utilized for precise planning of surgeries, contributing to improved patient care. |
| Identifying Patient Abnormalities | VR has the potential to provide information in a complimentary format that would be useful to be integrated with the other ones used for the diagnosis. Enhanced imaging capabilities enable preliminary analysis. Contributes to identifying symptoms of mental health disorders. |
| Tumor Analysis for Informed Treatment | VR assists in analyzing tumor size, providing insights for effective chemotherapy. Delivers precise information regarding tumor levels. Beneficial for successful clinical trials, allowing for detailed analysis. |
| Facilitating Informed Decision-Making | VR presents patient information in 3D, aiding well-informed decisions. Enhances comfort for both doctors and patients. Improves patient understanding of procedures and treatment processes. |
| Optimizing Interventional Radiology (IR) Treatments | VR enhances the efficiency of interventional radiology treatments. Applied in invasive procedures for various cancer treatments, reducing pain and recovery time. Guides medical treatment with minimum risk through real-time virtual video. |
| Date of Final Decision | Submission Number | Device | Company | Panel (Lead) |
|---|---|---|---|---|
| 09/29/2022 | K213034 | SpineAR SNAP | Surgical Theater, Inc. | Orthopedic |
| 09/01/2022 | K220104 | Knee+ | Pixee Medical | Orthopedic |
| 07/29/2022 | K220733 | OptiVu ROSA MxR | Orthosoft, Inc. (d/b/a Zimmer CAS) | Orthopedic |
| 06/15/2022 | K213684 | SurgiCase Viewer | Materialise NV | Radiology |
| 05/27/2022 | K220146 | VisAR | Novarad Corporation | Orthopedic |
| 03/10/2022 | K213751 | NextAR TKA Platform My Knee PPS | Medacta International S.A. | Orthopedic |
| 01/14/2022 | K211254 | ARAI Surgical Navigation System | Surgalign Spine Technologies | Orthopedic |
| 11/16/2021 | DEN210014 | EaseVRx | AppliedVR, Inc. | Physical Medicine |
| 11/10/2021 | K210344 | inVisionOS | PrecisionOS Technology Inc. | Radiology |
| 11/05/2021 | K210859 | NextAR Spine Platform | Medacta International, SA | Orthopedic |
| 10/20/2021 | DEN210005 | Luminopia One | Luminopia, Inc. | Ophthalmic |
| 10/02/2021 | K202927 | EYE-SYNC | SyncThink, Inc. | Neurology |
| 09/29/2021 | K210726 | Immersive Touch | ImmersiveTouch Inc. | Radiology |
| 07/19/2021 | K211188 | xvision Spine system (XVS) | Augmedics Ltd. | Orthopedic |
| 07/14/2021 | K203115 | ARVIS Surgical Navigation System | Insight Medical Systems Inc. | Orthopedic |
| 05/14/2021 | K210072 | HOLOSCOPE-i | Real View Imaging Ltd. | Radiology |
| 05/12/2021 | K210153 | NextAR RSA Platform | Medacta International SA | Orthopedic |
| 04/21/2021 | K202750 | Knee+ | Pixee Medical | Orthopedic |
| 01/28/2021 | K200384 | HipXpert 3D Display and Anchoring Application | Surgical Planning Associates, Inc. | Orthopedic |
| 10/27/2020 | K202152 | NextAR TKA Platform | Medacta International SA | Orthopedic |
| 09/18/2020 | K192890 | SentEP | SentiAR, Inc. | Cardiovascular |
| 07/17/2020 | K201465 | SuRgical Planner (SRP) BrainStorm | Surgical Theater, Inc. | Radiology |
| 07/10/2020 | K193559 | NextAR TKA Platform | Medacta Inernational SA | Orthopedic |
| 01/23/2020 | K191014 | Elements Viewer | Brainlab AG | Radiology |
| 12/20/2019 | K190929 | xvision Spine system (XVS) | Augmedics Ltd. | Orthopedic |
| 11/29/2019 | K192186 | I-Portal Neuro Otologic Test Center, I-Portal Video Nystagmo | Neurolign USA LLC | Ear, Nose, & Throat |
| 08/29/2019 | K183489 | D2P | 3D Systems, Inc. | Radiology |
| 05/13/2019 | K190764 | SurgicalAR | MEDIVIS, Inc. | Radiology |
| 03/18/2019 | K183296 | REAL Immersive System | Penumbra, Inc. | Physical Medicine |
| 02/22/2019 | K182643 | IRIS 1.0 System | Intuitive Surgical | Radiology |
| 09/21/2018 | K172418 | OpenSight | Novarad Corporation | Radiology |
| 02/12/2018 | K170793 | SuRgical Planner (SRP) | Surgical Theater, LLC | Radiology |
| 04/24/2017 | K162748 | MindMotionPRO | MindMaze SA | Physical Medicine |
| 06/28/2016 | K160584 | Surgical Navigation Advanced Platform (SNAP) | SURGICAL THEATER, LLC | Radiology |
| 02/12/2016 | K153004 | Clear Guide SCENERGY | CLEAR GUIDE MEDICAL | Radiology |
| 02/05/2016 | K151955 | YuGo System | BIOGAMING LTD. | Physical Medicine |
| 01/29/2016 | K152915 | EYE-SYNC | SyncThink Inc. | Neurology |
| 01/21/2015 | K142107 | ECHO TRUE 3D VIEWER | ECHO PIXEL INC. | Radiology |
| Review Study | Key Points | Focus on Radiology | Focus on VR Integration |
|---|---|---|---|
| Sutherland et al. (2019) [81] | This study explores VR (also integrated with AR) growth in the radiology field, addressing technology limitations and proposing a framework for medical image processing in VR/AR, suggesting its integration into radiological workflows and various clinical settings. | Discusses considerations for placing these methods directly into a radiology-based workflow and details on how it can be applied to a variety of clinical scenarios. | A comprehensive conceptual framework has been introduced to understand the various VR experiences also integrated with AR, categorized by technological sophistication. This framework assists in integrating VR technologies directly into radiology workflows, offering new perspectives on medical imaging interpretation and utilization. |
| Elsayed et al. (2020) [82] | This review provide an overview of VR (also integrated with AR) technologies, their current applications in radiology, future developments, and the challenges to their wider adoption in digital imaging. | Potential applications in diagnosis, surgical planning, interventional procedures, image interpretation, medical education, and 3D printing. | A comparison between 3D printing and VR/AR is reported. VR/AR offer interactive visual simulations with real-time render customizability, contrasting with the pre-printing limitations of 3D printing. While both require software, VR/AR systems are accessible via head-mounted displays (HMDs) without the need for a 3D printer or printing materials. Additionally, VR/AR typically have quicker turnaround times and varying ease of use, with potential side effects like cyber sickness, unlike 3D printing which lacks such effects. |
| Gelmini et al. (2021) [83] | This systematic review compares VR simulations to traditional teaching in interventional radiology, analyzing five trials using the Kirkpatrick model with mixed outcomes. Findings suggest VR enhances learning effectively, yet underlines the need for standardized VR integration and further research in this field. | Assesses the efficacy of VR as an educational tool in interventional radiology, particularly in enhancing skill transfer and reducing medical errors. Studies indicate that VR-based teaching facilitates skill acquisition among residents and novice physicians, potentially shortening the learning curve and improving patient outcomes. Additionally, VR-based simulation training shows promise in reducing morbidity, mortality, and healthcare costs associated with interventional radiology procedures, although further research is needed to evaluate its effectiveness across different populations and procedures. | VR is used in interventional radiology education by providing immersive simulations of procedural techniques, allowing trainees to practice in a virtual environment before performing procedures on patients. This method enables learners to acquire skills safely and effectively, leading to reduced procedural times, fewer technical errors, and ultimately better patient outcomes. |
| von Ende et al. (2023) [84] | Focuses on VR’s role in medicine, especially in diagnostic radiology, and points to its emerging potential in interventional radiology. The review discusses VR’s promise in enhancing radiological diagnosis and treatment through AR, AI, and radio genomics, despite current obstacles limiting clinical acceptance. It emphasizes the need for overcoming challenges to foster AI’s broader clinical adoption in interventional radiology. | The applications of VR integrated with AI and AR in interventional radiology is discussed. It spans across pre-procedural, intra-procedural, and post-procedural phases. Pre-procedural uses involve patient selection, radiogenomics, AR, and VR. Intra-procedural applications encompass procedural guidance and management of radiation exposure. Post-procedural applications focus on evaluating procedural outcomes and facilitating follow-up care. | The potential roles of VR, AR, and AI are discussed in the pre-procedural, intra-procedural applications, and post-procedural applications. |
| Gamba et al. (2024) [85] | This study explores the impact of VR also integrated with AR on digital imaging in radiology, highlighting the transformation of workspaces into interactive environments. Despite the infancy of research on VR-simulated radiology stations, the review stresses the need for further studies to understand their benefits and address adoption barriers, underscoring the technology’s potential to innovate radiological practices. | The focus is on exploring the potential applications of VR and Augmented Reality technology, particularly in redesigning the traditional radiology workstation (reading room) to enhance diagnostic interpretation. | Specifically within radiology, VR technology, also integrated with AR, is being explored to redesign traditional workstations, such as reading rooms, to improve diagnostic interpretation. Despite its promising potential, further research is needed to understand the full scope of benefits and address barriers to adoption. |
| Chytas et al. (2021) [86] | This review examines the benefits of VR in radiology and anatomy education, showing, through seven studies, that VR is well received and effective in enhancing anatomy knowledge. The findings advocate for VR’s integration in teaching, suggesting significant improvements in radiology education within anatomy courses. | The focus is on radiology in conjunction with anatomy education involving VR and AR. Studies have shown positive outcomes when radiology is taught alongside anatomy using VR and AR, with improvements observed in students’ academic performance and perception of the educational intervention. | Integration of VR and AR into anatomy education alongside radiology holds promise for enhancing learning experiences, and may encourage educators to adopt such approaches. Different VR and AR solutions are discussed. |
| Iannessi et al. (2018) [87] | This review navigates the evolution and future of UIs in radiology, noting the dominance of mouse and keyboard while evaluating alternatives like touchscreens and VR/AR for 2D and 3D imaging applications. The study stresses designing radiologist-specific UIs for better acceptance and usability, indicating a move towards UIs tailored to radiology’s unique needs. | The focus on radiology is on improving user interfaces (UI) for radiologists, especially with the evolution of digitalization and the increasing use of teleradiology. Designing specific UI tailored to radiologists’ needs, both in terms of hardware and software, is crucial for enhancing efficiency and productivity. | Advances in technology, such as touch technology and VR/AR, show promise in optimizing UI the design and facilitation of tasks like 3D image display and manipulation, particularly in interventional radiology units where contactless interfaces are preferred. |
| Gurgitano et al. (2021) [88] | This study explores AI’s role in radiology since the 1950s, enhancing diagnostic precision and treatment through machine and deep learning. Highlighting AI’s synergy with AR and VR in minimally invasive treatments, the study anticipates AI’s broad impact on IR, from patient screening to education, signaling a future where AI substantially boosts radiology and patient care. | The focus is the diagnostic and interventional radiology and the potential of integration of VR, AI, and AR. | The potential opportunities of AR/VRA/AI to streamline workflows, improve diagnostic accuracy, and enhance procedural planning and execution are discussed. |
| Dankelman et al. (2004) [89] | This review explores VR’s potential in interventional radiologist training, offering a realistic and cost-effective solution amidst the challenges of traditional and alternative methods, while advocating for further research and a thoughtful development approach based on Rasmussen’s model. | The focus on radiology revolves around exploring the potential of VR in training interventional radiologists to address the increasing procedural complexity and the limitations of traditional training methods. | VR emerges as a promising solution offering a realistic and cost-effective training environment, although its effectiveness in interventional radiology (IR) training requires further research. The study proposes using Rasmussen’s model of human behavior to evaluate VR training’s potential for IR education and to guide the development of future training methods. |
| Kukla et al. (2023) [90] | This review describes the decade-long application of ER (including the VR) in diagnostic imaging in digital radiology, noting its benefits in patient positioning, medical education, and reducing anesthesia use, while calling for more research to address clinical integration challenges and fully realize ER’s healthcare potential. | The focus in radiology is the medical education and diagnostic imaging. | Discusses specific applications such as the DIVA system for facial trauma diagnosis and the Magic Mirror system for projecting 3D anatomy images onto the body. Despite their potential benefits, challenges such as cost-effectiveness, standardization, and addressing cybersickness need to be addressed. Further research and standardization efforts are necessary to fully realize these benefits and ensure their effectiveness in clinical practice. |
| Patel et al. (2020) [91] | This review explores the transition to virtual interviews in residency programs due to COVID-19, discussing challenges, opportunities, and strategies for effective presentation and assessment, emphasizing preparation, technology, and adaptation in the selection process. | The focus is on the transition to virtual readiness in the residency recruitment process, particularly in the field of radiology. | It emphasizes the importance of preparing both applicants and programs for virtual interviews, updating online resources, and investing in online platforms for effective communication between applicants and program personnel. VR is recalled as a potential technology with which people are becoming familiar. |
| Ravindran (2023) [92] | This study emphasizes radiological advances like ultrasound, MRI, CT scans, and virtual endoscopy in managing difficult airways, noting their role in improving clinical standards and patient safety through enhanced diagnostics and training. | The focus is on advancements and innovations in managing the difficult airway within the field of radiology. It discusses various diagnostic techniques such as airway and neck Ultrasonography, MRI, and CT. | Discusses predictive tools like Virtual Endoscopy (VE) and 3D printing are discussed. Additionally, the study explores developments in airway devices, adjuncts, guidelines from organizations like the Difficult Airway Society and the American Society of Anesthesiologists, and emerging technologies such as VR for training and patient counsel. |
| Guimarães et al. (2017) [93] | This review discusses the shift in medical education in radiology towards integrating basic and clinical sciences with new technologies like 3D modelling and digital imaging, highlighting the future role of AI and VR in personalizing learning, essential for addressing medical education’s complexity. | In the context of medical education and anatomy education specifically, radiology plays a crucial role in providing complementary imaging modalities for studying anatomy. Traditional methods like cadaveric dissection are being supplemented or even replaced by newer technologies such as radiological imaging (e.g., X-rays, CT scans, and MRI scans). These imaging techniques offer detailed visualizations of anatomical structures in living organisms without the need for invasive procedures. | In the context of VR in Medical Education and Anatomy Education, the focus lies on enhancing the learning experience through immersive and interactive simulations of anatomical structures. VR technology allows students to explore the human body in three dimensions, providing a highly realistic and engaging learning environment. With VR, students can visualize complex anatomical structures from various angles and perspectives, offering a deeper understanding of spatial relationships and anatomical details. They can interact with virtual models, manipulate anatomical components, and simulate procedures in a risk-free setting. |
| Zhao et al. (2023) [94] | This study explore the shift in IR training to using anatomical phantom models made possible by material technology advances, highlighting gel-based and 3D printing methods’ role in this safer cost-effective alternative, amid current challenges and future research directions. | The focus is on the development of anatomical phantoms for medical training, particularly in the field of interventional radiology. | Researchers and physicians explore methods such as gel-based and 3D printing-based approaches to create these phantoms, aiming to provide safe and efficient training alternatives to traditional methods on real patients. Despite advancements, challenges such as time-consuming processes and the need for low-cost materials that accurately simulate tissues and organs remain to be addressed for widespread application. |
| McBain et al. (2022) [95] | This scoping review focused on anatomical education across training levels, and evaluated its modalities, urging further research on AR’s effects on skills, cognitive load, and performance with robust designs and validated tools. | The review aims to identify different AR applications specifically within the context of radiology education, highlighting the role of AR technology in improving the understanding and visualization of anatomical structures relevant to radiological practice. | The focus of this review is on identifying and evaluating different augmented reality modalities used in teaching anatomy to students, health professional trainees, and surgeons. It examines the assessment tools utilized to evaluate the performance of these AR modalities, highlighting variables such as usability, feasibility, acceptability, visuospatial ability, cognitive load, time on tasks, and academic achievement outcomes for further exploration and understanding of AR’s role in anatomical education. |
| Singhal et al. (2023) [96] | This literature review highlights how the technological advances like AI, VR, AR, and 3D printing have the potential to contribute to dentistry across diagnosis, surgery, and patient care, using radiology images, underscoring the need to understand their benefits and limitations for successful integration. | The focus is on oral radiology, a specialized field of dentistry dedicated to diagnosing and treating oral diseases using various imaging methods. The primary objective of oral radiology is to identify pathologies such as cysts, tumors, and infections in the oral cavity. The study also highlights the wide array of imaging techniques employed in oral radiology, including radiographs, CT scans, MRI, PET scans, and ultrasound, each serving specific diagnostic purposes related to dental and oral health. | The focus is on the integration of VR AR and MR technologies in oral surgery. The study highlights the potential benefits such as providing detailed anatomical information, facilitating surgical planning, enhancing dental anesthesia administration training, and assisting in various oral and maxillofacial surgeries. Additionally, the study highlights the potential of the AI integration in oral surgery, particularly in interpreting diagnostic imaging and optimizing treatment planning for conditions like impacted third molars and orofacial deformities. |
| Dammann (2002) [97] | Focusing on significant progress in radiology image processing, this study highlighted improvements in image quality, 3D visualization, and automated clinical applications like treatment planning and intervention guidance. It emphasizes the growing necessity for specialized skills in image handling and suggests evolving roles within radiology specialties due to these technological advances. | The focus is on the potential advancements in medical imaging processing and analysis methods in radiology, based on various techniques such as preprocessing algorithms, three-dimensional visualization, registration, segmentation, and automated quantification analysis. | The focus on VR in this piece is primarily on its integration into various aspects of medical imaging processing and analysis. VR technologies are highlighted as part of three-dimensional visualization techniques, such as volume rendering and virtual endoscopy, to evaluate sectional imaging data sets. Additionally, VR is mentioned in the context of three-dimensional therapy planning, simulation, and intervention guidance, alongside other technologies like medical modeling, surgical robots, and navigation systems. The article emphasizes the increasing use of VR in clinical applications and underscores the need for specialized skills in utilizing VR for the production and postprocessing of radiological imaging data. These methods have practical implications for radiologists in their daily work, and pave the way for future developments in medical imaging technology and its applications. |
| Romeny et al. (1998) [98] | This review describes advancements in diagnostic 3D radiology, emphasizing the impact of 3D rendering software and computer vision on improving imaging and anatomy visualization through processes like segmentation and ray casting. The paper highlights the role of modern workstations in facilitating the integration of multimodal data and interactive 3D image processing, significantly benefiting radiology practices and anatomical training. | The focus of this study in radiology is on the impact of computer-assisted techniques in various aspects of diagnostic radiology. It highlights the essential tasks in radiology, such as providing patient management information, navigation for minimally invasive therapy and surgery, and assessing effectiveness. The study discusses how computers aid in these tasks, particularly through advanced visualization techniques like 3D volume rendering and surface rendering, which allow for a better understanding of complex anatomical structures. Additionally, computer-assisted techniques are crucial in tasks like multiplanar reformatting, maximum intensity projection of CT and MRI angiography, and comparisons of different functional imaging modalities. Furthermore, the study delves into the challenges faced in radiology, such as noise reduction in images, and discusses advanced techniques like nonlinear diffusion filtering to address these challenges effectively. It also explores the importance of accurate registration of multiple imaging modalities for integrated visualization and analysis. Overall, the study emphasizes the significant role of computer-assisted techniques in enhancing various aspects of diagnostic radiology, from image processing and analysis to treatment planning and intervention guidance. | While the study primarily focuses on computer-assisted techniques in diagnostic radiology, it does not extensively discuss VR specifically. However, it does mention the use of modern workstations in operating rooms for guidance and even robotic assistance, which can potentially involve VR technologies. Additionally, it briefly touches upon the concept of interactive volume visualization, which aligns with some aspects of VR where users can manipulate datasets in real-time for optimal understanding and exploration. |
| Rooney et al. (2018) [99] | This systematic review evaluates SBME in radiation oncology, demonstrating its effectiveness in enhancing competencies like clinical decision-making and treatment planning through 54 studies. They advocate for SBME’s integration into training programs, noting the need for better reporting standards and centralized resource utilization for broader adoption. | This study focuses on SBME in radiation oncology. The study emphasizes the need to recognize SBME as a valuable component of radiation oncology education and advocates for its diversification beyond contouring skills. It suggests including a broader range of skill sets and targeting a wider variety of learners, including non-physician members of the oncology team. Ultimately, the study underscores the importance of establishing a framework for SBME in radiation oncology education to ensure its widespread acceptance and integration into training methodologies. | The study provides an overview of SBME interventions used in radiation oncology education. Among the SBME interventions identified, VR/haptic systems were mentioned, accounting for 13% of the total interventions. This indicates that VR technology is being utilized to some extent in radiation oncology education, alongside other simulation-based approaches. While the study does not delve into details about the use of VR specifically, it suggests that SBME interventions, including those utilizing VR, have shown effectiveness in teaching various radiation oncology competencies. It also hints at the potential for VR to be employed in teaching procedural skills, such as brachytherapy, and in simulating patient encounters to enhance communication and support skills. |
| Alvarez-Lopez et al. (2019) [100] | This systematic literature review analyses the application of devices like Microsoft Kinect and Leap Motion Controller in radiology and surgery for gesture-based image manipulation, showing promise for affordable, portable simulators in minimally invasive surgery training. This study indicates these technologies could transform raining and preparation, although their application in sterile surgical environments remains under-explored. | The study primarily focuses on the use and integration into radiology of commercial off-the-shelf (COTS) devices, such as the Microsoft Kinect (MK), the Leap Motion Controller (LMC), and the Myo armband, in various medical applications, particularly in surgery, robotic surgery, and training simulations. The fields of applications are the following: Application in Surgery; Application in Robotic Surgery; and Application in Training and Simulation. | COTS devices, particularly, motion-sensing technologies like the MK and the Leap Motion Controller LMC, in medical settings, specifically surgery and training have been investigated. These devices enable contactless interaction with medical images and data in environments such as operating rooms, addressing the need for real-time manipulation of medical images without compromising sterility protocols. Key points highlighted in the text include: Evaluation of Individual Devices: The study discusses the performance and characteristics of MK and LMC, both of which use infrared cameras. It compares their features, such as accuracy, interaction range, and device dimensions. Advantages and Limitations: It outlines the advantages of these devices, such as their low cost, portability, ease of use, and high gesture recognition rates. However, it also identifies limitations, such as latency issues, limited gesture recognition, and interference in small environments for MK, and performance alterations due to environmental factors and occlusion phenomena for LMC. Application in Robotic Surgery: The study discusses the application of gesture-based COTS devices in robot-assisted surgery, highlighting challenges related to cost, accuracy, and robustness. While some studies suggest potential applications for workflow monitoring and training purposes, others indicate limitations in controlling surgical robots using these devices. Training and Simulation: It explores the use of COTS devices in surgical education and simulation, particularly in teaching anatomy, bronchoscopy, colonoscopy, and minimally invasive surgery skills. The study discusses the development of VR simulators based on these devices and their potential in training for robotic surgery. |
| Associated Studies | Opportunities | Description |
|---|---|---|
| Gelmini et al. (2021) [83] Chytas et al. (2021) [86] | Enhanced Medical Education | The integration of VR and AR offers unprecedented opportunities to enhance medical education. Realistic simulations and interactive environments improve learning experiences, particularly in radiology and anatomy education. |
| Gurgitano et al. (2021) [88] | Improved Diagnostic Precision | AI, in conjunction with technologies like AR and VR, has the potential to significantly improve diagnostic precision in radiology. This not only enhances accuracy, but also aids in personalized treatment planning. |
| Singhal et al. (2023) [96] | Transformative Impact on Dentistry | Advances in technologies such as AI, VR, AR, and 3D printing present opportunities for a substantial impact on dentistry. From diagnosis to surgery, these innovations promise improved patient care and shorter treatment times. |
| Dankelman et al. (2004) [89] Rooney et al. (2018) [99] | SBME | VR, particularly in the form of SBME, provides a realistic and cost-effective solution for training healthcare professionals. This opportunity addresses challenges in traditional training methods, offering immersive environments for skill acquisition. |
| Sutherland et al. (2019) [81] von Ende et al. (2023) [84] | Technological Integration in Clinical Workflows | The integration of VR and AR into clinical workflows, including diagnostic radiology and interventional procedures, presents opportunities for increased efficiency and accuracy in patient care. |
| Guimarães et al. (2017) [93] | Personalized Learning in Medical Education | The shift towards integrating basic and clinical sciences, supported by technologies like AI, VR, and learning analytics, opens opportunities for personalized learning processes in real time, addressing the complexity of medical education. |
| Ravindran (2023) [92] | Application in Difficult Airway Management | Technological advancements, including ultrasound, MRI, CT scans, virtual endoscopy, and 3D printing, offer opportunities to improve standards in difficult airway management. This includes enhanced diagnostics, training, and patient counseling. |
| Iannessi et al. (2018) [87] | Evolution of User Interfaces | The evolution of user interfaces, encompassing touchscreens, kinetic sensors, and augmented/virtual reality, presents opportunities for designing interfaces specifically tailored to radiologists. This addresses usability concerns and ensures better acceptance. |
| Kukla et al. (2023) [90] | ER in Diagnostic Imaging | ER, as explored in diagnostic imaging, offers opportunities to improve patient positioning, medical education, and potentially reduce the need for anesthesia. The interactive benefits of ER in anatomy and patient positioning are recognized. |
| Zhao et al. (2023) [94] | Advancements in Surgical Training Models | The development of anatomical phantom models using gel-based and 3D printing methods for surgical training in interventional radiology presents opportunities for safer, cost-effective alternatives. This allows for realistic simulations of multi-layer tissue structures. |
| Patel et al. (2020) [91] | Shift to Virtual Interviews | The shift to virtual interviews in residency programs due to the COVID-19 pandemic presents opportunities for optimizing interview processes, leveraging technology for effective presentation and assessment, and exploring new formats for interaction in the selection process. |
| Dammann (2002) [97] ter Haar Romenyet al. (1998) [98] | Improvements in Image Processing | Advancements in image processing, including pre-processing algorithms, 3D visualization, and segmentation methods, offer opportunities for automated quantification, treatment planning, and intervention guidance in radiology. |
| Alvarez-Lopez et al. (2019) [100] | Application COTS Devices | The application of COTS devices, such as Microsoft Kinect and Leap Motion Controller, in radiology and surgery for gesture-based image manipulation offers opportunities for affordable portable simulators in minimally invasive surgery training. |
| Limitations/Areas of Improvements | Description | Associated Studies |
|---|---|---|
| Technology Limitations in Clinical Application VR and AR | Face challenges in clinical application due to insufficient quality and technological constraints, hindering their broader adoption in medical settings. | [81] |
| Challenges to AI Acceptance in Interventional Radiology | Despite AI’s potential in enhancing radiological diagnosis through VR, AR, and radio genomics, clinical acceptance in interventional radiology is hindered by obstacles that must be overcome for broader adoption. | [84] |
| Lack of Standardization in VR Education | While VR enhances learning in interventional radiology, the lack of research on standardizing its use across procedures underscores the need for further study and standardization in VR education. | [83] |
| Obstacles to AI Integration in Radiology | AI integration in radiology faces technical challenges and limitations, restricting its clinical acceptance. Overcoming these obstacles is crucial for broader adoption in radiological practices. | [88] |
| Infancy of Research on VR-Simulated Radiology Stations | Research on VR-simulated radiology stations is in its infancy, with limited studies on potential applications. Further research is essential to understand benefits and overcome adoption barriers. | [85] |
| Usability Challenges in UIs | Despite advancements, the dominance of mouse and keyboard in radiology UIs poses challenges. Designing UIs specific to radiologists is crucial for better acceptance and usability. | [87] |
| Cost and Ethical Concerns in VR Training | VR training faces challenges related to costs and ethical considerations. Investigating cost-effectiveness and ethical implications is necessary for informed adoption. | [89] |
| Clinical Integration Challenges of ER | ER’s positive impact on diagnostic procedures encounters challenges in clinical integration. Addressing cost-effectiveness and integration challenges requires further research. | [90] |
| Challenges in Virtual Interviews | The shift to virtual interviews in residency programs presents challenges in technology adaptation and assessment. Developing strategies is crucial to overcome these challenges. | [91] |
| Adoption Challenges in Difficult Airway Management | Despite advancements, challenges persist in the widespread adoption of technologies in difficult airway management. Addressing guideline compliance and technology application in clinical settings is imperative. | [92] |
| Transition from Traditional Training to VR in Surgery | The transition to VR in surgery faces challenges such as ethical concerns and high costs. Further research and thoughtful development approaches are needed for effective integration. | [89] |
| Challenges in SBME Reporting Standards | While SBME is effective, improved reporting standards and centralized resource utilization are needed for broader adoption in radiation oncology training programs. | [99] |
| Exploratory Nature of COTS Devices in Surgery | The application of COTS devices in surgery, especially in sterile environments, remains exploratory. Further exploration is required to realize their potential in contributing to training and preparation. | [100] |
| Associated Studies | Key Emerging Themes | Details |
|---|---|---|
| Benabid et al. [107,108] | Neurosurgery as a Platform for Robotics | These studies highlighted neurosurgery’s role in developing robotic applications, utilizing multimodal image guidance. Motorized tools were employed in stereotaxy and conventional neurosurgery, with a forecast of integration with AR/VR. |
| Shi et al. [102] | Endovascular Robotic Systems in Interventional Surgery | This study focused on endovascular robotic systems in interventional surgery. They introduced a VR interventional training system, enhancing surgical safety. The study included innovative catheterization modeling, and demonstrated effectiveness through validation. |
| Marescaux and Diana [103] | Hybrid Image-Guided Minimally Invasive Therapies | This study discussed the convergence of surgery, endoscopy, and interventional radiology into hybrid image-guided minimally invasive therapies. Integration of robotics and computer sciences was proposed to advance minimally invasive approaches. |
| Ni et al. [104] | VR Simulation for Ultrasound-Guided Biopsy Training | This study introduced a VR simulation system for ultrasound-guided biopsy training. The system featured 3D anatomical model reconstruction, data fusion, realistic rendering, interactive navigation, and haptic feedback, enhancing radiologist and physician training. |
| Moix et al. [105] | Quality Training Environment for Interventional Radiology | This study proposed a quality training environment for interventional radiology with a VR simulation linked to a robotic interface. The focus was on addressing limitations of existing systems and designing a haptic interface tailored for guide wires. |
| Moix et al. [106] | This study further discussed a computer-assisted training environment for interventional radiology, integrating VR simulation and a robotic interface with a specific focus on catheters. The paper detailed the design and prototyping of a haptic interface. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lastrucci, A.; Giansanti, D. Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews. Robotics 2024, 13, 69. https://doi.org/10.3390/robotics13050069
Lastrucci A, Giansanti D. Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews. Robotics. 2024; 13(5):69. https://doi.org/10.3390/robotics13050069
Chicago/Turabian StyleLastrucci, Andrea, and Daniele Giansanti. 2024. "Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews" Robotics 13, no. 5: 69. https://doi.org/10.3390/robotics13050069
APA StyleLastrucci, A., & Giansanti, D. (2024). Radiological Crossroads: Navigating the Intersection of Virtual Reality and Digital Radiology through a Comprehensive Narrative Review of Reviews. Robotics, 13(5), 69. https://doi.org/10.3390/robotics13050069







