The Preventive and Therapeutic Effects of Acute and Severe Inflammatory Disorders with Heparin and Heparinoid
Abstract
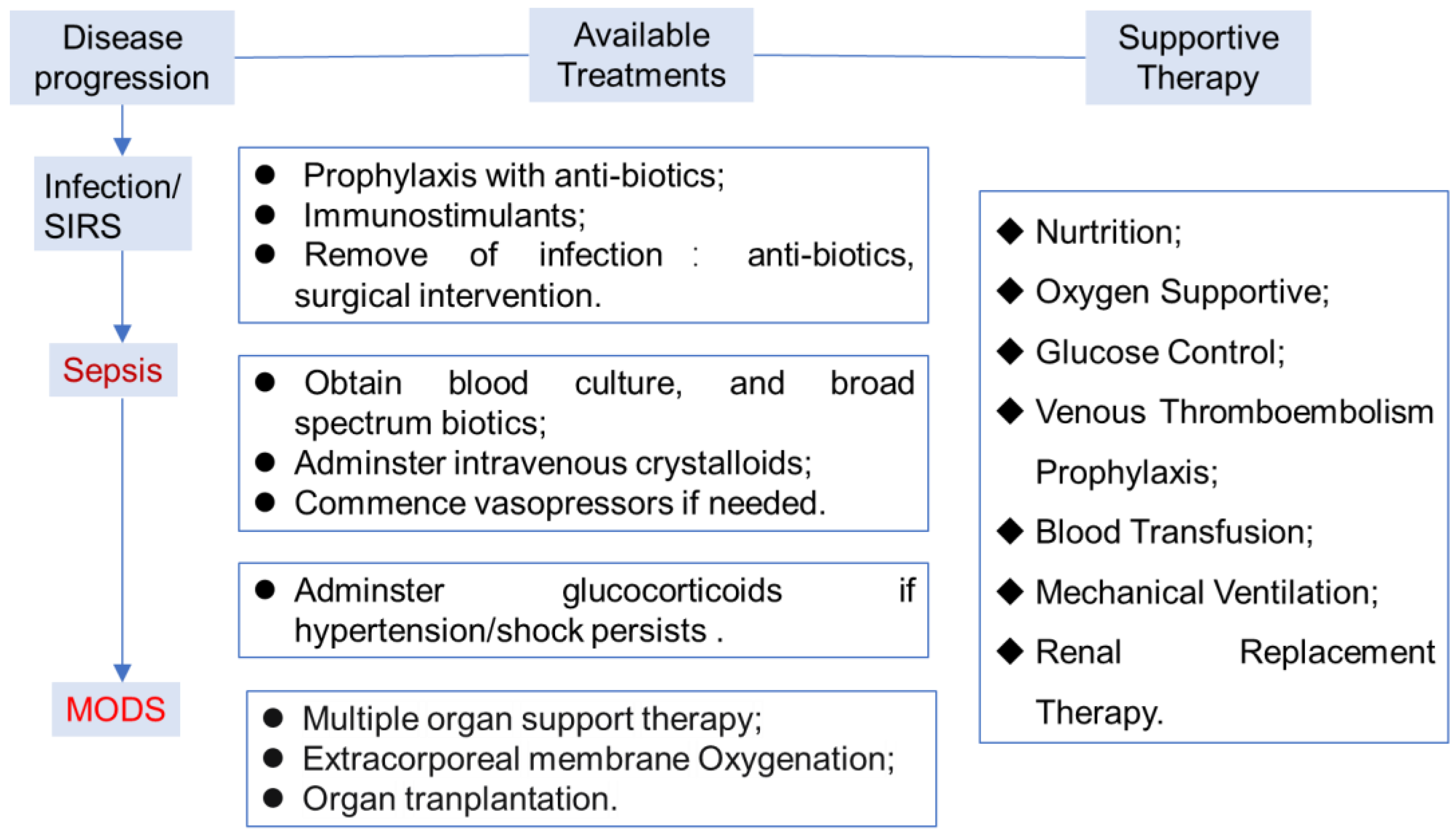
1. Introduction
2. Recent Innovations of the Molecular Mechanism Research
2.1. Inhibition of HMGB-1-Driven Inflammation Reactions
2.2. Inhibition of Histone Toxicity
2.3. Thrombo-Inflammatory Response Control
2.3.1. Protect the Structure Integrity of the Endothelial Cells
2.3.2. Disrupt the NET Formation
2.3.3. The Emerging New Mechanisms
2.4. The Mechanisms for Heparin Defenses against COVID-19
3. The Prophylaxis and Treatment of Sepsis with Heparin in Clinical Trials
3.1. Comparison between the Different Types of Heparins
3.2. Severe Acute Pancreatitis (SAP) Therapy
4. Discussions and Perspectives
| Disease | Mechanism of the Effects | Clinical Progress | Notes |
|---|---|---|---|
| Sepsis/acute lung injury |
|
| |
| The experiment design does not consider the proper time and patients for heparin therapy. | ||
| COVID-19 |
|
| |
| Heparin might intervene with the inflammatory reaction in the early stage of sepsis that initiates the coagulation cascade. | ||
| Acute kidney injury | Reduces H4 (histone) levels and the release of pro-inflammatory cytokine in HK-2 cells (human renal tubular epithelial cells). | ||
| Acute severe pancreatitis |
|
| |
| Acute liver injury | By targeting the HMGB-1 /RAGE axis, the chemotaxis of neutrophils is inhibited, the anti-inflammatory effect on the damaged liver is enhanced and the efficacy is significantly improved. |
|
Author Contributions
Funding
Conflicts of Interest
References
- Hotchkiss, R.S.; Karl, I.E. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 2003, 348, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Kaukonen, K.M.; Bailey, M.; Pilcher, D.; Cooper, D.J.; Bellomo, R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N. Engl. J. Med. 2015, 372, 1629–1638. [Google Scholar] [CrossRef] [PubMed]
- van der Poll, T.; Shankar-Hari, M.; Wiersinga, W.J. The immunology of sepsis. Immunity 2021, 54, 2450–2464. [Google Scholar] [CrossRef]
- Vincent, J.-L. Current sepsis therapeutics. EBioMedicine 2022, 86, 104318. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Wang, G.; Xie, J. Immune dysregulation in sepsis: Experiences, lessons and perspectives. Cell Death Discov. 2023, 9, 465. [Google Scholar] [CrossRef]
- Russell, J.A. Management of sepsis. New Engl. J. Med. 2006, 355, 1699–1713. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Aschenbrenner, A.C.; Bauer, M.; Bock, C.; Calandra, T.; Gat-Viks, I.; Kyriazopoulou, E.; Lupse, M.; Monneret, G.; Pickkers, P.; et al. The pathophysiology of sepsis and precision-medicine-based immunotherapy. Nat. Immunol. 2024, 25, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Lonsdale, D.O.; Shah, R.V.; Lipman, J. Infection, Sepsis and the Inflammatory Response: Mechanisms and Therapy. Front. Med. 2020, 7, 588863. [Google Scholar] [CrossRef]
- Thompson, K.; Venkatesh, B.; Finfer, S. Sepsis and septic shock: Current approaches to management. Intern. Med. J. 2019, 49, 160–170. [Google Scholar] [CrossRef]
- Hotchkiss, R.S.; Moldawer, L.L.; Opal, S.M.; Reinhart, K.; Turnbull, I.R.; Vincent, J.L. Sepsis and septic shock. Nat. Rev. Dis. Primers 2016, 2, 16045. [Google Scholar] [CrossRef]
- Papafilippou, L.; Claxton, A.; Dark, P.; Kostarelos, K.; Hadjidemetriou, M. Nanotools for Sepsis Diagnosis and Treatment. Adv. Healthc. Mater. 2021, 10, e2001378. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Beni, S.; Limtiaco, J.F.; Langeslay, D.J.; Larive, C.K. Heparin characterization: Challenges and solutions. Annu. Rev. Anal. Chem. 2011, 4, 439–465. [Google Scholar] [CrossRef] [PubMed]
- Lever, R.; Page, C.P. Novel drug development opportunities for heparin. Nat. Rev. Drug Discov. 2002, 1, 140–148. [Google Scholar] [CrossRef]
- Fu, S.; Yu, S.; Wang, L.; Ma, X.; Li, X. Unfractionated heparin improves the clinical efficacy in adult sepsis patients: A systematic review and meta-analysis. BMC Anesthesiol. 2022, 22, 28. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chi, C.; Guo, L.; Wang, X.; Guo, L.; Sun, J.; Sun, B.; Liu, S.; Chang, X.; Li, E. Heparin therapy reduces 28-day mortality in adult severe sepsis patients: A systematic review and meta-analysis. Crit. Care 2014, 18, 563. [Google Scholar] [CrossRef]
- Zou, Z.Y.; Huang, J.J.; Luan, Y.Y.; Yang, Z.J.; Zhou, Z.P.; Zhang, J.J.; Yao, Y.M.; Wu, M. Early prophylactic anticoagulation with heparin alleviates mortality in critically ill patients with sepsis: A retrospective analysis from the MIMIC-IV database. Burns Trauma. 2022, 10, tkac029. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Costanzo, S.; Antinori, A.; Berselli, N.; Blandi, L.; Bonaccio, M.; Cauda, R.; Guaraldi, G.; Menicanti, L.; Mennuni, M.; et al. Heparin in COVID-19 Patients Is Associated with Reduced In-Hospital Mortality: The Multicenter Italian CORIST Study. Thromb. Haemost. 2021, 121, 1054–1065. [Google Scholar] [CrossRef]
- Jaimes, F.; De La Rosa, G.; Morales, C.; Fortich, F.; Arango, C.; Aguirre, D.; Muñoz, A. Unfractioned heparin for treatment of sepsis: A randomized clinical trial (The HETRASE Study). Crit. Care Med. 2009, 37, 1185–1196. [Google Scholar] [CrossRef] [PubMed]
- Kienast, J.; Juers, M.; Wiedermann, C.J.; Hoffmann, J.N.; Ostermann, H.; Strauss, R.; Keinecke, H.O.; Warren, B.L.; Opal, S.M. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J. Thromb. Haemost. 2006, 4, 90–97. [Google Scholar] [CrossRef]
- Lawler, P.R.; Goligher, E.C.; Berger, J.S.; Neal, M.D.; McVerry, B.J.; Nicolau, J.C.; Gong, M.N.; Carrier, M.; Rosenson, R.S.; Reynolds, H.R.; et al. Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 790–802. [Google Scholar] [CrossRef]
- Goligher, E.C.; Bradbury, C.A.; McVerry, B.J.; Lawler, P.R.; Berger, J.S.; Gong, M.N.; Carrier, M.; Reynolds, H.R.; Kumar, A.; Turgeon, A.F.; et al. Therapeutic Anticoagulation with Heparin in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 777–789. [Google Scholar] [CrossRef]
- Zang, L.; Zhu, H.; Wang, K.; Liu, Y.; Yu, F.; Zhao, W. Not Just Anticoagulation-New and Old Applications of Heparin. Molecules 2022, 27, 6968. [Google Scholar] [CrossRef] [PubMed]
- Litov, L.; Petkov, P.; Rangelov, M.; Ilieva, N.; Lilkova, E.; Todorova, N.; Krachmarova, E.; Malinova, K.; Gospodinov, A.; Hristova, R.; et al. Molecular Mechanism of the Anti-Inflammatory Action of Heparin. Int. J. Mol. Sci. 2021, 22, 730. [Google Scholar] [CrossRef]
- Chen, D. Heparin beyond anti-coagulation. Curr. Res. Transl. Med. 2021, 69, 103300. [Google Scholar] [CrossRef]
- Capila, I.; Linhardt, R.J. Heparin-protein interactions. Angew. Chem. Int. Ed. Engl. 2002, 41, 391–412. [Google Scholar] [CrossRef] [PubMed]
- Arnold, K.; Liao, Y.E.; Liu, J. Potential Use of Anti-Inflammatory Synthetic Heparan Sulfate to Attenuate Liver Damage. Biomedicines 2020, 8, 503. [Google Scholar] [CrossRef]
- Pan, Q.; Zhang, C.; Wu, X.; Chen, Y. Identification of a heparosan heptasaccharide as an effective anti-inflammatory agent by partial desulfation of low molecular weight heparin. Carbohydr. Polym. 2020, 227, 115312. [Google Scholar] [CrossRef]
- Xu, D.; Esko, J.D. Demystifying heparan sulfate-protein interactions. Annu. Rev. Biochem. 2014, 83, 129–157. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, U.; Akhtar, F.; Xue, J.; Wan, X.; Zhang, T.; He, S. Review: Inhibitory potential of low molecular weight Heparin in cell adhesion; emphasis on tumor metastasis. Eur. J. Pharmacol. 2021, 892, 173778. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Kang, R.; Tang, D. The mechanism of HMGB1 secretion and release. Exp. Mol. Med. 2022, 54, 91–102. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Zeh, H.J.; Lotze, M.T. The multifunctional protein HMGB1: 50 years of discovery. Nat. Rev. Immunol. 2023, 23, 824–841. [Google Scholar] [CrossRef] [PubMed]
- Idoudi, S.; Bedhiafi, T.; Pedersen, S.; Elahtem, M.; Alremawi, I.; Akhtar, S.; Dermime, S.; Merhi, M.; Uddin, S. Role of HMGB1 and its associated signaling pathways in human malignancies. Cell Signal. 2023, 112, 110904. [Google Scholar] [CrossRef]
- Griffin, K.L.; Fischer, B.M.; Kummarapurugu, A.B.; Zheng, S.; Kennedy, T.P.; Rao, N.V.; Foster, W.M.; Voynow, J.A. 2-O, 3-O-desulfated heparin inhibits neutrophil elastase-induced HMGB-1 secretion and airway inflammation. Am. J. Respir. Cell Mol. Biol. 2014, 50, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Kummarapurugu, A.B.; Afosah, D.K.; Sankaranarayanan, N.V.; Boothello, R.S.; Desai, U.R.; Kennedy, T.; Voynow, J.A. 2-O, 3-O Desulfated Heparin Blocks High Mobility Group Box 1 Release by Inhibition of p300 Acetyltransferase Activity. Am. J. Respir. Cell Mol. Biol. 2017, 56, 90–98. [Google Scholar] [CrossRef]
- Wang, M.; Gauthier, A.G.; Kennedy, T.P.; Wang, H.; Velagapudi, U.K.; Talele, T.T.; Lin, M.; Wu, J.; Daley, L.; Yang, X.; et al. 2-O, 3-O desulfated heparin (ODSH) increases bacterial clearance and attenuates lung injury in cystic fibrosis by restoring HMGB1-compromised macrophage function. Mol. Med. 2021, 27, 79. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Ling, Y.; Huang, M.; Yin, T.; Gou, S.M.; Zhan, N.Y.; Xiong, J.X.; Wu, H.S.; Yang, Z.Y.; Wang, C.Y. Heparin inhibits the inflammatory response induced by LPS and HMGB1 by blocking the binding of HMGB1 to the surface of macrophages. Cytokine 2015, 72, 36–42. [Google Scholar] [CrossRef]
- Tang, Y.; Wang, X.; Li, Z.; He, Z.; Yang, X.; Cheng, X.; Peng, Y.; Xue, Q.; Bai, Y.; Zhang, R.; et al. Heparin prevents caspase-11-dependent septic lethality independent of anticoagulant properties. Immunity 2021, 54, 454–467.e456. [Google Scholar] [CrossRef]
- Arnold, K.; Xu, Y.; Sparkenbaugh, E.M.; Li, M.; Han, X.; Zhang, X.; Xia, K.; Piegore, M.; Zhang, F.; Zhang, X.; et al. Design of anti-inflammatory heparan sulfate to protect against acetaminophen-induced acute liver failure. Sci. Transl. Med. 2020, 12, eaav8075. [Google Scholar] [CrossRef]
- Chen, R.; Kang, R.; Fan, X.G.; Tang, D. Release and activity of histone in diseases. Cell Death Dis. 2014, 5, e1370. [Google Scholar] [CrossRef]
- Szatmary, P.; Huang, W.; Criddle, D.; Tepikin, A.; Sutton, R. Biology, role and therapeutic potential of circulating histones in acute inflammatory disorders. J. Cell Mol. Med. 2018, 22, 4617–4629. [Google Scholar] [CrossRef]
- Li, X.; Ye, Y.; Peng, K.; Zeng, Z.; Chen, L.; Zeng, Y. Histones: The critical players in innate immunity. Front. Immunol. 2022, 13, 1030610. [Google Scholar] [CrossRef]
- Marsman, G.; Zeerleder, S.; Luken, B.M. Extracellular histones, cell-free DNA, or nucleosomes: Differences in immunostimulation. Cell Death Dis. 2016, 7, e2518. [Google Scholar] [CrossRef] [PubMed]
- Wildhagen, K.C.; García de Frutos, P.; Reutelingsperger, C.P.; Schrijver, R.; Aresté, C.; Ortega-Gómez, A.; Deckers, N.M.; Hemker, H.C.; Soehnlein, O.; Nicolaes, G.A. Nonanticoagulant heparin prevents histone-mediated cytotoxicity in vitro and improves survival in sepsis. Blood 2014, 123, 1098–1101. [Google Scholar] [CrossRef] [PubMed]
- Reutelingsperger, C.P.M.; Gijbels, M.J.; Spronk, H.; Van Oerle, R.; Schrijver, R.; Ekhart, P.; de Kimpe, S.; Nicolaes, G.A.F. M6229 Protects against Extracellular-Histone-Induced Liver Injury, Kidney Dysfunction, and Mortality in a Rat Model of Acute Hyperinflammation. Int. J. Mol. Sci. 2024, 25, 1376. [Google Scholar] [CrossRef] [PubMed]
- Nagano, F.; Mizuno, T.; Mizumoto, S.; Yoshioka, K.; Takahashi, K.; Tsuboi, N.; Maruyama, S.; Yamada, S.; Nagamatsu, T. Chondroitin sulfate protects vascular endothelial cells from toxicities of extracellular histones. Eur. J. Pharmacol. 2018, 826, 48–55. [Google Scholar] [CrossRef]
- Sharma, N.; Haggstrom, L.; Sohrabipour, S.; Dwivedi, D.J.; Liaw, P.C. Investigations of the effectiveness of heparin variants as inhibitors of histones. J. Thromb. Haemost. 2022, 20, 1485–1495. [Google Scholar] [CrossRef]
- Iba, T.; Levy, J.H. Inflammation and thrombosis: Roles of neutrophils, platelets and endothelial cells and their interactions in thrombus formation during sepsis. J. Thromb. Haemost. 2018, 16, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.P.; Darbousset, R.; Schoenwaelder, S.M. Thromboinflammation: Challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood 2019, 133, 906–918. [Google Scholar] [CrossRef]
- Liu, L.; Yu, H.; Wang, L.; Zhou, D.; Duan, X.; Zhang, X.; Yin, J.; Luan, S.; Shi, H. Heparin-network-mediated long-lasting coatings on intravascular catheters for adaptive antithrombosis and antibacterial infection. Nat. Commun. 2024, 15, 107. [Google Scholar] [CrossRef]
- Han, J.; Ding, R.; Zhao, D.; Zhang, Z.; Ma, X. Unfractionated heparin attenuates lung vascular leak in a mouse model of sepsis: Role of RhoA/Rho kinase pathway. Thromb. Res. 2013, 132, e42–e47. [Google Scholar] [CrossRef]
- Liu, Y.; Mu, S.; Li, X.; Liang, Y.; Wang, L.; Ma, X. Unfractionated Heparin Alleviates Sepsis-Induced Acute Lung Injury by Protecting Tight Junctions. J. Surg. Res. 2019, 238, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Han, S.; Liu, X.; Wang, T.; Xu, H.; Xia, B.; Kong, G.; Li, J.; Zhu, W.; Hu, H.; et al. Both UFH and NAH alleviate shedding of endothelial glycocalyx and coagulopathy in LPS-induced sepsis. Exp. Ther. Med. 2020, 19, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhu, J.; Liu, K.; Hu, Y.; Huang, K.; Pan, S. Heparin ameliorates cerebral edema and improves outcomes following status epilepticus by protecting endothelial glycocalyx in mice. Exp. Neurol. 2020, 330, 113320. [Google Scholar] [CrossRef]
- Yang, R.; Chen, M.; Zheng, J.; Li, X.; Zhang, X. The Role of Heparin and Glycocalyx in Blood-Brain Barrier Dysfunction. Front. Immunol. 2021, 12, 754141. [Google Scholar] [CrossRef] [PubMed]
- Masola, V.; Greco, N.; Gambaro, G.; Franchi, M.; Onisto, M. Heparanase as active player in endothelial glycocalyx remodeling. Matrix Biol. Plus 2022, 13, 100097. [Google Scholar] [CrossRef]
- Iba, T.; Maier, C.L.; Helms, J.; Ferrer, R.; Thachil, J.; Levy, J.H. Managing sepsis and septic shock in an endothelial glycocalyx-friendly way: From the viewpoint of surviving sepsis campaign guidelines. Ann. Intensive Care 2024, 14, 64. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Bai, J. Protective effects of heparin on endothelial cells in sepsis. Int. J. Clin. Exp. Med. 2015, 8, 5547–5552. [Google Scholar]
- Li, X.; Zheng, Z.; Li, X.; Ma, X. Unfractionated heparin inhibits lipopolysaccharide-induced inflammatory response through blocking p38 MAPK and NF-κB activation on endothelial cell. Cytokine 2012, 60, 114–121. [Google Scholar] [CrossRef]
- Dauth, A.; Bręborowicz, A.; Ruan, Y.; Tang, Q.; Zadeh, J.K.; Böhm, E.W.; Pfeiffer, N.; Khedkar, P.H.; Patzak, A.; Vujacic-Mirski, K.; et al. Sulodexide Prevents Hyperglycemia-Induced Endothelial Dysfunction and Oxidative Stress in Porcine Retinal Arterioles. Antioxidants 2023, 12, 388. [Google Scholar] [CrossRef]
- Ying, J.; Zhang, C.; Wang, Y.; Liu, T.; Yu, Z.; Wang, K.; Chen, W.; Zhou, Y.; Lu, G. Sulodexide improves vascular permeability via glycocalyx remodelling in endothelial cells during sepsis. Front. Immunol. 2023, 14, 1172892. [Google Scholar] [CrossRef] [PubMed]
- Shen, D.; Chen, R.; Zhang, L.; Rao, Z.; Ruan, Y.; Li, L.; Chu, M.; Zhang, Y. Sulodexide attenuates endoplasmic reticulum stress induced by myocardial ischaemia/reperfusion by activating the PI3K/Akt pathway. J. Cell. Mol. Med. 2019, 23, 5063–5075. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, K.; Liu, Q.; Liu, M.; Zhang, G.; Feng, K.; Wang, K.; Ding, X.; Zhu, H.; Yang, S.; et al. A Novel Drug Candidate for Sepsis Targeting Heparanase by Inhibiting Cytokine Storm. Adv. Sci. 2024, 11, e2403337. [Google Scholar] [CrossRef]
- Mu, S.; Liu, Y.; Jiang, J.; Ding, R.; Li, X.; Li, X.; Ma, X. Unfractionated heparin ameliorates pulmonary microvascular endothelial barrier dysfunction via microtubule stabilization in acute lung injury. Respir. Res. 2018, 19, 220. [Google Scholar] [CrossRef]
- Eshun-Wilson, L.; Zhang, R.; Portran, D.; Nachury, M.V.; Toso, D.B.; Löhr, T.; Vendruscolo, M.; Bonomi, M.; Fraser, J.S.; Nogales, E. Effects of α-tubulin acetylation on microtubule structure and stability. Proc. Natl. Acad. Sci. USA 2019, 116, 10366–10371. [Google Scholar] [CrossRef]
- Meara, C.H.O.; Coupland, L.A.; Kordbacheh, F.; Quah, B.J.C.; Chang, C.W.; Simon Davis, D.A.; Bezos, A.; Browne, A.M.; Freeman, C.; Hammill, D.J.; et al. Neutralizing the pathological effects of extracellular histones with small polyanions. Nat. Commun. 2020, 11, 6408. [Google Scholar] [CrossRef]
- Li, X.; Ma, X. The role of heparin in sepsis: Much more than just an anticoagulant. Br. J. Haematol. 2017, 179, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Colicchia, M.; Perrella, G.; Gant, P.; Rayes, J. Novel mechanisms of thrombo-inflammation during infection: Spotlight on neutrophil extracellular trap-mediated platelet activation. Res. Pract. Thromb. Haemost. 2023, 7, 100116. [Google Scholar] [CrossRef]
- Zhan, Y.; Ling, Y.; Deng, Q.; Qiu, Y.; Shen, J.; Lai, H.; Chen, Z.; Huang, C.; Liang, L.; Li, X.; et al. HMGB1-Mediated Neutrophil Extracellular Trap Formation Exacerbates Intestinal Ischemia/Reperfusion-Induced Acute Lung Injury. J. Immunol. 2022, 208, 968–978. [Google Scholar] [CrossRef]
- Manfredi, A.A.; Rovere-Querini, P.; D’Angelo, A.; Maugeri, N. Low molecular weight heparins prevent the induction of autophagy of activated neutrophils and the formation of neutrophil extracellular traps. Pharmacol. Res. 2017, 123, 146–156. [Google Scholar] [CrossRef]
- An, S.; Raju, I.; Surenkhuu, B.; Kwon, J.E.; Gulati, S.; Karaman, M.; Pradeep, A.; Sinha, S.; Mun, C.; Jain, S. Neutrophil extracellular traps (NETs) contribute to pathological changes of ocular graft-vs.-host disease (oGVHD) dry eye: Implications for novel biomarkers and therapeutic strategies. Ocul. Surf. 2019, 17, 589–614. [Google Scholar] [CrossRef]
- Liao, Y.E.; Xu, Y.; Arnold, K.; Zhang, F.; Li, J.; Sellers, R.; Yin, C.; Pagadala, V.; Inman, A.M.; Linhardt, R.J.; et al. Using heparan sulfate octadecasaccharide (18-mer) as a multi-target agent to protect against sepsis. Proc. Natl. Acad. Sci. USA 2023, 120, e2209528120. [Google Scholar] [CrossRef] [PubMed]
- Roncato, R.; Angelini, J.; Pani, A.; Talotta, R. Lipid rafts as viral entry routes and immune platforms: A double-edged sword in SARS-CoV-2 infection? Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2022, 1867, 159140. [Google Scholar] [CrossRef]
- Wang, L.; Liu, Z.; Dong, Z.; Pan, J.; Ma, X. Azurocidin-induced inhibition of oxygen metabolism in mitochondria is antagonized by heparin. Exp. Ther. Med. 2014, 8, 1473–1478. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ji, Y.; Wang, Y.; Zeng, W.; Mei, X.; Du, S.; Yan, Y.; Hao, J.; Zhang, Z.; Lu, Y.; Zhang, C.; et al. A heparin derivatives library constructed by chemical modification and enzymatic depolymerization for exploitation of non-anticoagulant functions. Carbohydr. Polym. 2020, 249, 116824. [Google Scholar] [CrossRef]
- Connors, J.M.; Levy, J.H. Thromboinflammation and the hypercoagulability of COVID-19. J. Thromb. Haemost. 2020, 18, 1559–1561. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.W.; Ilyas, I.; Weng, J.P. Endothelial dysfunction in COVID-19: An overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol. Sin. 2023, 44, 695–709. [Google Scholar] [CrossRef] [PubMed]
- Kelliher, S.; Weiss, L.; Cullivan, S.; O’Rourke, E.; Murphy, C.A.; Toolan, S.; Lennon, Á.; Szklanna, P.B.; Comer, S.P.; Macleod, H.; et al. Non-severe COVID-19 is associated with endothelial damage and hypercoagulability despite pharmacological thromboprophylaxis. J. Thromb. Haemost. 2022, 20, 1008–1014. [Google Scholar] [CrossRef]
- Potje, S.R.; Costa, T.J.; Fraga-Silva, T.F.C.; Martins, R.B.; Benatti, M.N.; Almado, C.E.L.; de Sá, K.S.G.; Bonato, V.L.D.; Arruda, E.; Louzada-Junior, P.; et al. Heparin prevents in vitro glycocalyx shedding induced by plasma from COVID-19 patients. Life Sci. 2021, 276, 119376. [Google Scholar] [CrossRef]
- Clausen, T.M.; Sandoval, D.R.; Spliid, C.B.; Pihl, J.; Perrett, H.R.; Painter, C.D.; Narayanan, A.; Majowicz, S.A.; Kwong, E.M.; McVicar, R.N.; et al. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell 2020, 183, 1043–1057. [Google Scholar] [CrossRef]
- Kalra, R.S.; Kandimalla, R. Engaging the spikes: Heparan sulfate facilitates SARS-CoV-2 spike protein binding to ACE2 and potentiates viral infection. Signal Transduct. Target. Ther. 2021, 6, 39. [Google Scholar] [CrossRef]
- Zhang, Q.; Tang, W.; Stancanelli, E.; Jung, E.; Syed, Z.; Pagadala, V.; Saidi, L.; Chen, C.Z.; Gao, P.; Xu, M.; et al. Host heparan sulfate promotes ACE2 super-cluster assembly and enhances SARS-CoV-2-associated syncytium formation. Nat. Commun. 2023, 14, 5777. [Google Scholar] [CrossRef]
- Guimond, S.E.; Mycroft-West, C.J.; Gandhi, N.S.; Tree, J.A.; Le, T.T.; Spalluto, C.M.; Humbert, M.V.; Buttigieg, K.R.; Coombes, N.; Elmore, M.J.; et al. Synthetic Heparan Sulfate Mimetic Pixatimod (PG545) Potently Inhibits SARS-CoV-2 by Disrupting the Spike-ACE2 Interaction. ACS Cent. Sci. 2022, 8, 527–545. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Tingting, W.; Li, J.P.; Sullivan, M.A.; Wang, C.; Wang, H.; Deng, B.; Zhang, Y. Comprehensive Landscape of Heparin Therapy for COVID-19. Carbohydr. Polym. 2021, 254, 117232. [Google Scholar] [CrossRef] [PubMed]
- Goligher, E.C.; Lawler, P.R.; Jensen, T.P.; Talisa, V.; Berry, L.R.; Lorenzi, E.; McVerry, B.J.; Chang, C.H.; Leifer, E.; Bradbury, C.; et al. Heterogeneous Treatment Effects of Therapeutic-Dose Heparin in Patients Hospitalized for COVID-19. Jama 2023, 329, 1066–1077. [Google Scholar] [CrossRef] [PubMed]
- Tuinman, P.R.; Dixon, B.; Levi, M.; Juffermans, N.P.; Schultz, M.J. Nebulized anticoagulants for acute lung injury—A systematic review of preclinical and clinical investigations. Crit. Care 2012, 16, R70. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Helms, J.; Totoki, T.; Levy, J.H. Heparins May Not Be the Optimal Anticoagulants for Sepsis and Sepsis-Associated Disseminated Intravascular Coagulation. Semin. Thromb. Hemost. 2024. [Google Scholar] [CrossRef]
- Cools, F.; Virdone, S.; Sawhney, J.; Lopes, R.D.; Jacobson, B.; Arcelus, J.I.; Hobbs, F.D.R.; Gibbs, H.; Himmelreich, J.C.L.; MacCallum, P.; et al. Thromboprophylactic low-molecular-weight heparin versus standard of care in unvaccinated, at-risk outpatients with COVID-19 (ETHIC): An open-label, multicentre, randomised, controlled, phase 3b trial. Lancet Haematol. 2022, 9, e594–e604. [Google Scholar] [CrossRef]
- Rodman, C.; Ali, A.; Lannon, L.; Yusuf, E.; Bansal, V.; Lal, A.; Garces, J.P.D.; Kashyap, R. Association of early heparin use among patients with COVID-19 and sepsis and hospital outcomes. Crit. Care Med. 2023, 51, 110. [Google Scholar] [CrossRef]
- Gonzalez-Ochoa, A.J.; Raffetto, J.D.; Hernandez, A.G.; Zavala, N.; Gutierrez, O.; Vargas, A.; Loustaunau, J. Sulodexide in the treatment of patients with early stages of COVID-19: A randomized controlled trial. Thromb. Haemost. 2021, 121, 944–954. [Google Scholar] [CrossRef]
- Schulman, S.; Harenberg, J. Anticoagulant Treatment of COVID-19 as Early as Possible—Sulodexide and Perspectives. Thromb. Haemost. 2021, 121, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Ten Cate, H. Surviving COVID-19 with Heparin? N. Engl. J. Med. 2021, 385, 845–846. [Google Scholar] [CrossRef]
- Elsharnouby, N.M.; Eid, H.E.; Abou Elezz, N.F.; Aboelatta, Y.A. Heparin/N-acetylcysteine: An adjuvant in the management of burn inhalation injury: A study of different doses. J. Crit. Care 2014, 29, e181–e184. [Google Scholar] [CrossRef]
- Stattin, K.; Lipcsey, M.; Andersson, H.; Pontén, E.; Bülow Anderberg, S.; Gradin, A.; Larsson, A.; Lubenow, N.; von Seth, M.; Rubertsson, S.; et al. Inadequate prophylactic effect of low-molecular weight heparin in critically ill COVID-19 patients. J. Crit. Care 2020, 60, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Fragkou, P.C.; Palaiodimou, L.; Stefanou, M.I.; Katsanos, A.H.; Lambadiari, V.; Paraskevis, D.; Andreadou, E.; Dimopoulou, D.; Zompola, C.; Ferentinos, P.; et al. Effects of low molecular weight heparin and fondaparinux on mortality, hemorrhagic and thrombotic complications in COVID-19 patients. Ther. Adv. Neurol. Disord. 2022, 15, 17562864221099472. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Alés, G.; Domingo-Relloso, A.; Quintana-Díaz, M.; Fernández-Capitán, C.; Hernán, M.A. Thromboprophylaxis with standard-dose vs. flexible-dose heparin for hospitalized COVID-19 patients: A target trial emulation. J. Clin. Epidemiol. 2022, 151, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Shute, J.K. Heparin, Low Molecular Weight Heparin, and Non-Anticoagulant Derivatives for the Treatment of Inflammatory Lung Disease. Pharmaceuticals 2023, 16, 584. [Google Scholar] [CrossRef]
- Dixon, B.; Smith, R.J.; Campbell, D.J.; Moran, J.L.; Doig, G.S.; Rechnitzer, T.; MacIsaac, C.M.; Simpson, N.; van Haren, F.M.P.; Ghosh, A.N.; et al. Nebulised heparin for patients with or at risk of acute respiratory distress syndrome: A multicentre, randomised, double-blind, placebo-controlled phase 3 trial. Lancet Respir. Med. 2021, 9, 360–372. [Google Scholar] [CrossRef]
- Erelel, M.; Kaskal, M.; Akbal-Dagistan, O.; Issever, H.; Dagistanli, A.S.; Balkanci, H.; Oguz, M.S.; Qarayeva, A.; Culha, M.; Erturk, A.; et al. Early Effects of Low Molecular Weight Heparin Therapy with Soft-Mist Inhaler for COVID-19-Induced Hypoxemia: A Phase IIb Trial. Pharmaceutics 2021, 13, 1768. [Google Scholar] [CrossRef]
- Douen, A.; Basit, A.; Panetti, R.; Farag, P.; Mbolu, G.; Popilevsky, F.; Apergis, G. Old medicine for new problems: Potential role of a novel treatment using nebulized heparin in COVID-19 ards. Chest 2021, 160, 943A–944A. [Google Scholar] [CrossRef]
- Hursitoglu, M.; Eroz, E.; Ozgul, M.A. Nebulized Heparin for Post-COVID-19-Related Hypoxia. TH Open 2021, 5, e312–e314. [Google Scholar] [CrossRef] [PubMed]
- van Haren, F.M.P.; van Loon, L.M.; Steins, A.; Smoot, T.L.; Sas, C.; Staas, S.; Vilaseca, A.B.; Barbera, R.A.; Vidmar, G.; Beccari, H.; et al. Inhaled nebulised unfractionated heparin for the treatment of hospitalised patients with COVID-19: A multicentre case series of 98 patients. Br. J. Clin. Pharmacol. 2022, 88, 2802–2813. [Google Scholar] [CrossRef] [PubMed]
- DeNucci, G.; Wilkinson, T.; Sverdloff, C.; Babadopulos, T.; Woodcock, A.; Shute, J.; Renato Guazelli, P.; Gerbase, L.F.; Mourão, P.A.S.; Singh, D.; et al. Inhaled nebulised unfractionated heparin (UFH) for the treatment of hospitalised patients with COVID-19: A randomised controlled pilot study. Pulm. Pharmacol. Ther. 2023, 80, 102212. [Google Scholar] [CrossRef] [PubMed]
- van Haren, F.M.P.; Page, C.; Laffey, J.G.; Artigas, A.; Camprubi-Rimblas, M.; Nunes, Q.; Smith, R.; Shute, J.; Carroll, M.; Tree, J.; et al. Nebulised heparin as a treatment for COVID-19: Scientific rationale and a call for randomised evidence. Crit. Care 2020, 24, 454. [Google Scholar] [CrossRef]
- Buijsers, B.; Yanginlar, C.; Maciej-Hulme, M.L.; de Mast, Q.; van der Vlag, J. Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients. EBioMedicine 2020, 59, 102969. [Google Scholar] [CrossRef]
- Oliynyk, O.; Barg, W.; Slifirczyk, A.; Oliynyk, Y.; Dubrov, S.; Gurianov, V.; Rorat, M. Comparison of the Effect of Unfractionated Heparin and Enoxaparin Sodium at Different Doses on the Course of COVID-19-Associated Coagulopathy. Life 2021, 11, 1032. [Google Scholar] [CrossRef]
- Al Sulaiman, K.; Aljuhani, O.; Korayem, G.B.; Hafiz, A.; Alalawi, M.; Badreldin, H.A.; Altebainawi, A.F.; Vishwakarma, R.; Alissa, A.; Alghamdi, A.; et al. Standard dosing of enoxaparin versus unfractionated heparin in critically ill patient with COVID-19: A multicenter propensity-score matched study. Thromb. J. 2022, 20, 74. [Google Scholar] [CrossRef] [PubMed]
- Volteas, P.; Drakos, P.; Alkadaa, L.N.; Cleri, N.A.; Asencio, A.A.; Oganov, A.; Giannopoulos, S.; Saadon, J.R.; Mikell, C.B., 3rd; Rubano, J.A.; et al. Low-molecular-weight heparin compared with unfractionated heparin in critically ill COVID-19 patients. J. Vasc. Surg. Venous Lymphat. Disord. 2022, 10, 1128–1136. [Google Scholar] [CrossRef]
- Wang, Z.; Li, F.; Liu, J.; Luo, Y.; Guo, H.; Yang, Q.; Xu, C.; Ma, S.; Chen, H. Intestinal Microbiota—An Unmissable Bridge to Severe Acute Pancreatitis-Associated Acute Lung Injury. Front. Immunol. 2022, 13, 913178. [Google Scholar] [CrossRef]
- Antkowiak, R.; Bialecki, J.; Chabowski, M.; Domoslawski, P. Treatment of Microcirculatory Disturbances in Acute Pancreatitis: Where Are We Now? Pancreas 2022, 51, 415–421. [Google Scholar] [CrossRef]
- Yang, J.; Tang, X.; Wu, Q.; Ren, P.; Yan, Y.; Liu, W.; Pan, C. Heparin Protects Severe Acute Pancreatitis by Inhibiting HMGB-1 Active Secretion from Macrophages. Polymers 2022, 14, 2470. [Google Scholar] [CrossRef] [PubMed]
- Patil, B.; Meena, L.N.; Sharma, D.C.; Agarwal, G.; Dadhich, Y.; Gupta, G. Impact of low-molecular-weight heparin in the treatment of moderately severe and severe acute pancreatitis; a randomized, single blind, phase 3 control trial. Int. J. Surg. 2022, 101, 106621. [Google Scholar] [CrossRef]
- Rojaramani, K.; Sobharani, B.; Hari Babu Mekala, A.; Venkat Vineeth, A. Study of role of low molecular weight heparin in conjunction with conventional therapy in severe acute pancreatitis. Asian J. Med. Sci. 2022, 13, 109–116. [Google Scholar] [CrossRef]
- Lu, X.S.; Qiu, F.; Li, J.Q.; Fan, Q.Q.; Zhou, R.G.; Ai, Y.H.; Zhang, K.C.; Li, Y.X. Low molecular weight heparin in the treatment of severe acute pancreatitis: A multiple centre prospective clinical study. Asian J. Surg. 2009, 32, 89–94. [Google Scholar] [CrossRef]
- Qian, D.; Luan, X.; Zhang, Y. Effect of low molecular weight heparin and ulinastatin as a combined therapy on soluble myeloid cell expression and intestinal mucosal function in patients with severe pancreatitis. Trop. J. Pharm. Res. 2022, 21, 1515–1521. [Google Scholar] [CrossRef]
- Lu, X.-S.; Qiu, F.; Li, Y.-X.; Li, J.-Q.; Fan, Q.-Q.; Zhou, R.-G. Effect of Lower-Molecular Weight Heparin in the Prevention of Pancreatic Encephalopathy in the Patient With Severe Acute Pancreatitis. Pancreas 2010, 39, 516–519. [Google Scholar] [CrossRef] [PubMed]
- Gui, M.; Zhao, B.; Huang, J.; Chen, E.; Qu, H.; Mao, E. Pathogenesis and Therapy of Coagulation Disorders in Severe Acute Pancreatitis. J. Inflamm. Res. 2023, 16, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Du, J.D.; Zheng, X.; Huang, Z.Q.; Cai, S.W.; Tan, J.W.; Li, Z.L.; Yao, Y.M.; Jiao, H.B.; Yin, H.N.; Zhu, Z.M. Effects of intensive insulin therapy combined with low molecular weight heparin anticoagulant therapy on severe pancreatitis. Exp. Ther. Med. 2014, 8, 141–146. [Google Scholar] [CrossRef][Green Version]
- Ahmed, S.F.; Qadir, P.H.; Ahmed, S.M.; Salih, K.M.; Abdulla, B.A.; Mohammed, H.R.; Salih, A.M.; Kakamad, F.H. Recurrent seasonal severe hypertriglyceridemia-induced acute pancreatitis; a case report. Ann. Med. Surg. 2022, 75, 103406. [Google Scholar] [CrossRef]
- Ghizlane, E.A.; Manal, M.; Salma, T.; Abderrahim, E.K.; Mohammed, M.; Ikram, Z.; Fatem-Zahra, A.; Sanae, E.M.; Houssam, B.; Brahim, H. Hypertriglyceridemia revealing acute pancreatitis: A case report. Ann. Med. Surg. 2021, 70, 102914. [Google Scholar] [CrossRef]
- Ackermann, M.; Anders, H.J.; Bilyy, R.; Bowlin, G.L.; Daniel, C.; De Lorenzo, R.; Egeblad, M.; Henneck, T.; Hidalgo, A.; Hoffmann, M.; et al. Patients with COVID-19: In the dark-NETs of neutrophils. Cell Death Differ. 2021, 28, 3125–3139. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Al-Hussaniy, H.A.; Al-Harcan, N.A.H.; Alexiou, A.; Batiha, G.E. Neutrophil Extracellular Traps (NETs) and COVID-19: A new frontiers for therapeutic modality. Int. Immunopharmacol. 2022, 104, 108516. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Chen, C.; Zhang, X.; Wang, S.; Zhu, R.; Zhou, A.; Chen, S.; Feng, J. Heparin improves alveolarization and vascular development in hyperoxia-induced bronchopulmonary dysplasia by inhibiting neutrophil extracellular traps. Biochem. Biophys. Res. Commun. 2020, 522, 33–39. [Google Scholar] [CrossRef]
- Melkumyants, A.; Buryachkovskaya, L.; Lomakin, N.; Antonova, O.; Docenko, J.; Ermishkin, V.; Serebruany, V. Effect of Sulodexide on Circulating Blood Cells in Patients with Mild COVID-19. J. Clin. Med. 2022, 11, 1995. [Google Scholar] [CrossRef]
- Niu, C.; Du, Y.; Kaltashov, I.A. Towards better understanding of the heparin role in NETosis: Feasibility of using native mass spectrometry to monitor interactions of neutrophil elastase with heparin oligomers. Int. J. Mass. Spectrom. 2021, 463, 116550. [Google Scholar] [CrossRef]
- Lelliott, P.M.; Momota, M.; Shibahara, T.; Lee, M.S.J.; Smith, N.I.; Ishii, K.J.; Coban, C. Heparin induces neutrophil elastase-dependent vital and lytic NET formation. Int. Immunol. 2020, 32, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Chi, L.; Zhang, Z.; Zhao, H.; Zhang, F.; Linhardt, R.J. Heparin: An old drug for new clinical applications. Carbohydr. Polym. 2022, 295, 119818. [Google Scholar] [CrossRef]
- Shaikh, N.; Chanda, A.H.; Rahman, M.A.; Nainthramveetil, M.M.; Kumar, A.; Mathias, R.M.; Nashwan, A.J. Inhalational injury and use of heparin & N-acetylcysteine nebulization: A case report. Respir. Med. Case Rep. 2022, 37, 101640. [Google Scholar] [CrossRef]
- Ushio, N.; Yamakawa, K.; Mochizuki, K.; Hisamune, R.; Umemura, Y.; Takasu, A. Efficacy of unfractionated heparin in patients with moderate sepsis-induced coagulopathy: An observational study. Thromb. Res. 2024, 241, 109095. [Google Scholar] [CrossRef]
- Smilowitz, N.R.; Hade, E.M.; Kornblith, L.Z.; Castellucci, L.A.; Cushman, M.; Farkouh, M.; Gong, M.N.; Heath, A.; Hunt, B.J.; Kim, K.S.; et al. Effect of therapeutic-dose heparin on severe acute kidney injury and death in noncritically ill patients hospitalized for COVID-19: A prespecified secondary analysis of the ACTIV4a and ATTACC randomized trial. Res. Pract. Thromb. Haemost. 2023, 7, 102167. [Google Scholar] [CrossRef]
- Charfeddine, S.; Ibnhadjamor, H.; Jdidi, J.; Torjmen, S.; Kraiem, S.; Bahloul, A.; Makni, A.; Kallel, N.; Moussa, N.; Boudaya, M.; et al. Sulodexide Significantly Improves Endothelial Dysfunction and Alleviates Chest Pain and Palpitations in Patients With Long-COVID-19: Insights From TUN-EndCOV Study. Front. Cardiovasc. Med. 2022, 9, 866113. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.Y.; Peng, M.; Fan, M.M.; Zou, Q.F.; Li, Y.R.; Jiang, D. Heparin is an effective treatment for preventing liver failure after hepatectomy. World J. Gastroenterol. 2024, 30, 2881–2892. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, Y.; Wu, Y.; Ding, F.; Li, S.; Shen, Y.; Yang, B.; Tang, X.; Ren, L.; Deng, L.; Jin, X.; et al. The Preventive and Therapeutic Effects of Acute and Severe Inflammatory Disorders with Heparin and Heparinoid. Biomolecules 2024, 14, 1078. https://doi.org/10.3390/biom14091078
Song Y, Wu Y, Ding F, Li S, Shen Y, Yang B, Tang X, Ren L, Deng L, Jin X, et al. The Preventive and Therapeutic Effects of Acute and Severe Inflammatory Disorders with Heparin and Heparinoid. Biomolecules. 2024; 14(9):1078. https://doi.org/10.3390/biom14091078
Chicago/Turabian StyleSong, Ying, Yuxiang Wu, Fangfang Ding, Shuo Li, Yaojia Shen, Bingyan Yang, Xinran Tang, Lige Ren, Lirong Deng, Xuewen Jin, and et al. 2024. "The Preventive and Therapeutic Effects of Acute and Severe Inflammatory Disorders with Heparin and Heparinoid" Biomolecules 14, no. 9: 1078. https://doi.org/10.3390/biom14091078
APA StyleSong, Y., Wu, Y., Ding, F., Li, S., Shen, Y., Yang, B., Tang, X., Ren, L., Deng, L., Jin, X., & Yan, Y. (2024). The Preventive and Therapeutic Effects of Acute and Severe Inflammatory Disorders with Heparin and Heparinoid. Biomolecules, 14(9), 1078. https://doi.org/10.3390/biom14091078





