Update on Biomarkers Associated with Large-Artery Atherosclerosis Stroke
Abstract
:1. Introduction
2. Biomarkers and Their Usefulness in Stroke
- -
- Firstly, even though stenosis severity is the primarily used parameter for risk evaluation, being recommended by medical guidelines to decide treatment (medical vs. surgical), it is known that several high-grade stenoses are asymptomatic, with a low rate of symptomatic conversion. On the contrary, there appears to be a higher risk in low-grade stenosis, with a substantial proportion of symptomatic patients and a risk of recurrent ipsilateral stroke of up to 8% at three years [6]. Biomarkers can help to understand the real risk of symptomatic conversion of these patients and allow clinicians to act accordingly.
- -
- Secondly, LAA biomarkers may be useful to identify the stroke cause in patients classified as having an undetermined stroke etiology. The problem persists when patients have more than one possible cause for a stroke [5,7]. Having a biomarker that provides clues to a possible etiology may allow the clinician to better tailor preventive measures to the individual patient and plan their follow-up.
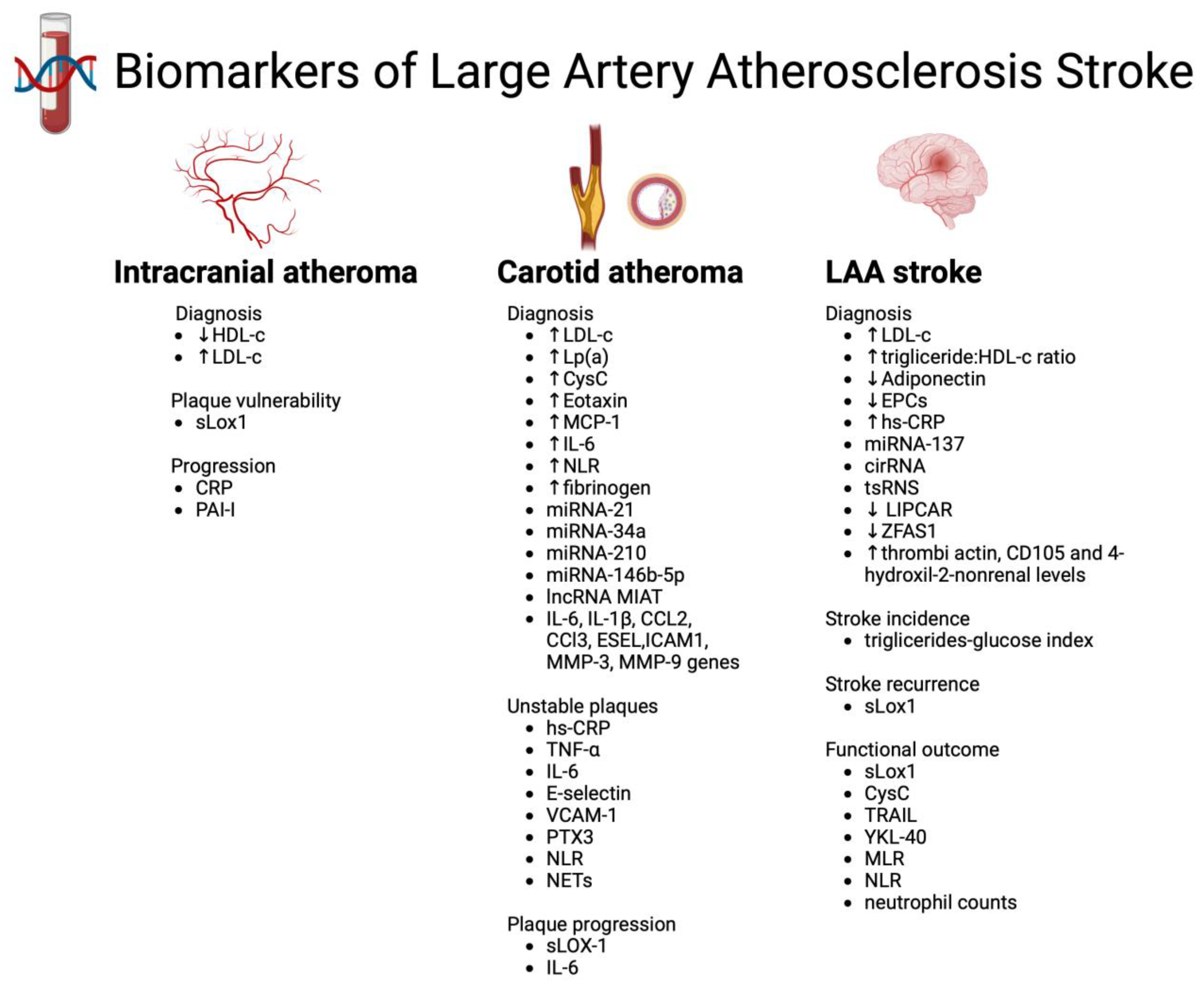
3. Biomarkers Associated with LAA Stroke
3.1. Chemical Biomarkers
3.2. Inflammatory Biomarkers
3.2.1. Proteins
3.2.2. White Blood Cells
3.3. Metabolomics
3.4. RNA Biomarkers
3.4.1. MicroRNAs
3.4.2. Circular RNA
3.4.3. Transfer-RNA-Derived Small RNAs
3.4.4. Long Noncoding RNA
3.5. Genetic Biomarkers
3.6. Biomarkers Found in Retrieved Thrombi
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cole, J.W. Large Artery Atherosclerotic Occlusive Disease. Continuum 2017, 23, 133–157. [Google Scholar] [CrossRef]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef]
- Maitrias, P.; Metzinger-Le Meuth, V.; Nader, J.; Reix, T.; Caus, T.; Metzinger, L. The involvement of miRNA in carotid-related stroke. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1608–1617. [Google Scholar] [CrossRef] [PubMed]
- Siniscalchi, A.; Murphy, S.; Gray, C.; De Sarro, G.; Gallelli, L. Biomarkers in Unstable Carotid Plaque: Physiopathology and Prediction. Cardiovasc. Hematol. Agents Med. Chem. 2022, 20, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Kamtchum-Tatuene, J.; Jickling, G.C. Blood biomarkers for stroke diagnosis and management. Neuromolecular Med. 2019, 21, 344–368. [Google Scholar] [CrossRef]
- Saba, L.; Moody, A.R.; Saam, T.; Kooi, M.E.; Wasserman, B.A.; Staub, D.; van der Lugt, A.; DeMarco, J.K.; Saloner, D.; Wintermark, M.; et al. Vessel wall-imaging biomarkers of carotid plaque vulnerability in stroke prevention trials: A viewpoint from the Carotid Imaging Consensus Group. JACC Cardiovasc. Imaging 2020, 13, 2445–2456. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, A.C.; Ferro, J.M. Cryptogenic stroke. Eur. J. Neurol. 2015, 22, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Kigka, V.I.; Potsika, V.; Mantzaris, M.; Tsakanikas, V.; Koncar, I.; Fotiadis, D.I. Serum biomarkers in carotid artery disease. Diagnostics 2021, 11, 2143. [Google Scholar] [CrossRef]
- Bang, O.Y.; Saver, J.L.; Liebesking, D.S.; Pineda, S.; Ovbiagele, B. Association of serum lipid indices with large artery atherosclerotic stroke. Neurology 2008, 70, 841–847. [Google Scholar] [CrossRef]
- Qian, Y.; Pu, Y.; Liu, L.; Wang, D.Z.; Zhao, X.; Wang, C.; Wang, Y.; Liu, G.; Pan, Y.; Wang, Y. Low HDL-C level is associated with the development of intracranial artery stenosis: Analysis from the Chinese IntraCranial AtheroSclerosis (CICAS) study. PLoS ONE 2013, 8, e64395. [Google Scholar] [CrossRef]
- Lin, L.; Deng, K.Q.; Chen, Z.; Lei, F.; Qin, J.J.; Huang, X.; Sun, T.; Zhang, X.; Hu, Y.; Zhang, P.; et al. Lipoprotein(a) distribution and its association with carotid arteriopathy in the Chinese population. Atherosclerosis 2023, 372, 1–9. [Google Scholar] [CrossRef]
- Ren, K.; Jiang, H.; Li, T.; Qian, C.; Zhu, L.; Wang, T. Correlation of sLOX-1 Levels and MR Characteristics of Culprit Plaques in Intracranial Arteries with Stroke Recurrence. Diagnostics 2023, 13, 804. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Li, Q.; Chen, X.; Lin, Y.; Xue, J.; Cai, Z.; Zhang, W.; Wang, H.; Jin, K.; Shao, B. Soluble lectin-like oxidized low-density lipoprotein receptor-1 as a novel biomarker for large-artery atherosclerotic stroke. Int. J. Neurosci. 2017, 127, 881–886. [Google Scholar] [CrossRef]
- Jiang, M.; Wu, H.; Zhang, H.; Su, F.; Cao, L.; Ren, X.; Tatenda, G.; Hu, J.; Cheng, M.; Wen, Y. Association between the triglyceride-glucose index and the risk of large artery atherosclerotic stroke. Int. J. Clin. Pract. 2022, 2022, 5191581. [Google Scholar] [CrossRef] [PubMed]
- Umemura, T.; Kawamura, T.; Mashita, S.; Kameyama, T.; Sobue, G. Higher Levels of Cystatin C Are Associated with Extracranial Carotid Artery Steno-Occlusive Disease in Patients with Noncardioembolic Ischemic Stroke. Cerebrovasc. Dis. Extra 2016, 6, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Pang, M.; Ma, A.; Wang, K.; Zhang, Z.; Zhong, Q.; Yang, S. Association of TRAIL and Its Receptors with Large-Artery Atherosclerotic Stroke. PLoS ONE 2015, 10, e0136414. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Huang, Z.; Xie, Y.; Chen, X.; Zhang, J.; Qiu, Z.; Ma, N.; Xu, G.; Liu, X. Lower levels of plasma adiponectin and endothelial progenitor cells are associated with large artery atherosclerotic stroke. Int. J. Neurosci. 2016, 126, 121–126. [Google Scholar] [CrossRef]
- Wei, L.K.; Quan, L.S. Biomarkers for ischaemic stroke subtypes: A protein-protein interaction analysis. Comput. Biol. Chem. 2019, 83, 107116. [Google Scholar] [CrossRef]
- Arenillas, J.F.; Alvarez-Sabín, J.; Molina, C.A.; Chacón, P.; Fernández-Cadenas, I.; Ribó, M.; Delgado, P.; Rubiera, M.; Penalba, A.; Rovira, A.; et al. Progression of symptomatic intracranial large artery atherosclerosis is associated with a proinflammatory state and impaired fibrinolysis. Stroke 2008, 39, 1456–1463. [Google Scholar] [CrossRef]
- Holmegaard, L.; Stanne, T.M.; Andreasson, U.; Zetterberg, H.; Blennow, K.; Blomstrand, C.; Jood, K.; Jern, C. Proinflammatory protein signatures in cryptogenic and large artery atherosclerosis stroke. Acta Neurol. Scand. 2021, 143, 303–312. [Google Scholar] [CrossRef]
- Shindo, A.; Tanemura, H.; Yata, K.; Hamada, K.; Shibata, M.; Umeda, Y.; Asakura, F.; Toma, N.; Sakaida, H.; Fujisawa, T.; et al. Inflammatory biomarkers in atherosclerosis: Pentraxin 3 can become a novel marker of plaque vulnerability. PLoS ONE 2014, 9, e100045. [Google Scholar] [CrossRef] [PubMed]
- Kamtchum-Tatuene, J.; Saba, L.; Heldner, M.R.; Poorthuis, M.H.; de Borst, G.J.; Rundek, T.; Kakkos, S.K.; Chaturvedi, S.; Topakian, R.; Polak, J.F.; et al. Interleukin-6 predicts carotid plaque severity, vulnerability, and progression. Cir. Res. 2022, 131, e22–e33. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, A.; Palaiopanos, K.; Björkbacka, H.; Peters, A.; de Lemos, J.A.; Seshadri, S.; Dichgans, M.; Georgakis, M.K. Circulating interleukin-6 levels and incident ischemic stroke: A systematic review and meta-analysis of prospective studies. Neurology 2022, 98, e1002–e1012. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.L.; Li, Q.; Huang, W.S.; Lin, Y.S.; Xue, J.; Wang, B.; Jin, K.L.; Shao, B. Serum YKL-40, a prognostic marker in patients with large-artery atherosclerotic stroke. Acta Neurol. Scand. 2017, 136, 97–102. [Google Scholar] [CrossRef]
- Wang, C.J.; Pang, C.Y.; Huan-Yu Cheng, Y.F.; Wang, H.; Deng, B.B.; Huang, H.J. Monocyte-to-lymphocyte ratio affects prognosis in LAA-type stroke patients. Heliyon 2022, 8, e10948. [Google Scholar] [CrossRef]
- Buonacera, A.; Stancanelli, B.; Colaci, M.; Malatino, L. Neutrophil to Lymphocyte Ratio: An Emerging Marker of the Relationships between the Immune System and Diseases. Int. J. Mol. Sci. 2022, 23, 3636. [Google Scholar] [CrossRef]
- Li, X.; Li, J.; Wu, G. Relationship of Neutrophil-to-Lymphocyte Ratio with Carotid Plaque Vulnerability and Occurrence of Vulnerable Carotid Plaque in Patients with Acute Ischemic Stroke. Biomed Res. Int. 2021, 2021, 6894623. [Google Scholar] [CrossRef]
- Corriere, T.; Di Marca, S.; Cataudella, E.; Pulvirenti, A.; Alaimo, S.; Stancanelli, B.; Malatino, L. Neutrophil-to-Lymphocyte Ratio is a strong predictor of atherosclerotic carotid plaques in older adults. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 23–27. [Google Scholar] [CrossRef]
- Tracey, K. Reflex control of immunity. Nat. Rev. Immunol. 2009, 9, 418–428. [Google Scholar] [CrossRef]
- Kadoya, M.; Koyama, H.; Kurajoh, M.; Kanzaki, A.; KakutaniHatayama, M.; Okazaki, H.; Shoji, T.; Moriwaki, Y.; Yamamoto, T.; Emoto, M.; et al. Sleep, cardiac autonomic function, and carotid atherosclerosis in patients with cardiovascular risks: HSCAA study. Atherosclerosis 2015, 238, 409–414. [Google Scholar] [CrossRef]
- Feng, X.; Yu, F.; Wei, M.; Luo, Y.; Zhao, T.; Liu, Z.; Huang, Q.; Tu, R.; Li, J.; Zhang, B.; et al. The association between neutrophil counts and neutrophil-to-lymphocyte ratio and stress hyperglycemia in patients with acute ischemic stroke according to stroke etiology. Front. Endocrinol. 2023, 14, 1117408. [Google Scholar] [CrossRef] [PubMed]
- Fest, J.; Ruiter, R.; Ikram, M.A.; Voortman, T.; Van Eijck CHJ:Stricker, B.H. Reference values for white blood-cell-based inflammatory markers in the Rotterdam Study: A population-based prospective cohort study. Sci. Rep. 2018, 8, 10566. [Google Scholar] [CrossRef] [PubMed]
- Shimonaga, K.; Matsushige, T.; Takahashi, H.; Hashimoto, Y.; Yoshiyama, M.; Ono, C.; Sakamoto, S. Peptidylarginine Deiminase 4 as a Possible Biomarker of Plaque Instability in Carotid Artery Stenosis. J. Stroke Cerebrovasc. Dis. 2021, 30, 105816. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, L.; Sun, W.; Pei, L.L.; Tian, M.; Liang, J.; Liu, X.; Zhang, R.; Fang, H.; Wu, J.; et al. Changes of Metabolites in Acute Ischemic Stroke and Its Subtypes. Front. Neurosci. 2021, 14, 580929. [Google Scholar] [CrossRef] [PubMed]
- Xuan, J.; Shang, M.; Li, X. Serum microRNA-137 serves as a novel biomarker for cerebral atherosclerosis diagnosis and cerebrovascular event prediction. J. Cardiovasc. Pharmacol. 2021, 78, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Badacz, R.; Przewłocki, T.; Legutko, J.; Żmudka, K.; Kabłak-Ziembicka, A. microRNAs Associated with Carotid Plaque Development and Vulnerability: The Clinician’s Perspective. Int. J. Mol. Sci. 2022, 23, 15645. [Google Scholar] [CrossRef] [PubMed]
- Ostolaza, A.; Blanco-Luquin, I.; Urdánoz-Casado, A.; Rubio, I.; Labarga, A.; Zandio, B.; Roldán, M.; Martínez-Cascales, J.; Mayor, S.; Herrera, M.; et al. Circular RNA expression profile in blood according to ischemic stroke etiology. Cell Biosci. 2020, 10, 34. [Google Scholar] [CrossRef]
- Liu, M.; Liu, X.; Zhou, M.; Guo, S.; Sun, K. Impact of CircRNAs on Ischemic Stroke. Aging Dis. 2022, 13, 329–339. [Google Scholar] [CrossRef]
- Yang, K.; Xiao, Q.; Wang, K.; Zhao, J.; Hou, R.; Pan, X.; Zhu, X. Circulating exosomal tsRNAs: Potential biomarkers for large artery atherosclerotic stroke superior to plasma tsRNAs. Clin. Transl. Med. 2023, 13, e1194. [Google Scholar] [CrossRef] [PubMed]
- Fasolo, F.; Jin, H.; Winski, G.; Chernogubova, E.; Pauli, J.; Winter, H.; Li, D.Y.; Glukha, N.; Bauer, S.; Metschl, S.; et al. Long Noncoding RNA MIAT Controls Advanced Atherosclerotic Lesion Formation and Plaque Destabilization. Circulation 2021, 144, 1567–1583. [Google Scholar] [CrossRef]
- Liu, Z.-Z.; Lin, W.-J.; Feng, Y.; Huang, C.-L.; Yan, Y.-F.; Guo, W.-Y.; Zhang, H.; Lei, Z.; Lu, Q.-L.; Liu, P.; et al. Plasma lncRNA LIPCAR Expression Levels Associated with Neurological Impairment and Stroke Subtypes in Patients with Acute Cerebral Infarction: A Prospective Observational Study with a Control Group. Neurol. Ther. 2023, 12, 1385–1398. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ruan, J.; Zhu, M.; Yang, J.; Du, S.; Xu, P.; Zhang, Z.; Wang, P.; Yang, W.; Yu, M. Predictive value of long noncoding RNA ZFAS1 in patients with ischemic stroke. Clin. Exp. Hypertens. 2019, 41, 615–621. [Google Scholar] [CrossRef]
- Ding, Y.; Xu, Z.; Pan, Y.; Meng, X.; Xiang, X.; Li, H.; Liu, L.; Wang, Y. Association between CST3 gene polymorphisms and large-artery atherosclerotic stroke. Front. Neurol. 2021, 12, 738148. [Google Scholar] [CrossRef]
- Shen, Y.; Peng, C.; Bai, Q.; Ding, Y.; Yi, X.; Du, H.; He, L.; Zhou, D.; Chen, X. Epigenome-wide association study indicates hypomethylation of MTRNR2L8 in large-artery atherosclerosis stroke. Stroke 2019, 50, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Biscetti, F.; Straface, G.; Bertoletti, G.; Vincenzoni, C.; Snider, F.; Arena, V.; Landolfi, R.; Flex, A. Identification of a potential proinflammatory genetic profile influencing carotid plaque vulnerability. J. Vasc. Surg. 2015, 61, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Wang, Z.; Jiang, L.; Gu, G.; Zheng, B.; Xian, L.; Zhang, Y.; Wang, J. High actin expression in thrombus of acute ischemic stroke can be a biomarker of atherothrombotic origin stroke. Front. Neurol. 2022, 13, 896428. [Google Scholar] [CrossRef] [PubMed]
- Osakada, Y.; Yamashita, T.; Morihara, R.; Matsumoto, N.; Sasaki, R.; Tadokoro, K.; Nomura, E.; Kawahara, Y.; Omote, Y.; Hishikawa, N.; et al. 4-Hydroxyl-2-Nonenal Localized Expression Pattern in Retrieved Clots is Associated with Large Artery Atherosclerosis in Stroke Patients. J. Stroke Cerebrovasc. Dis. 2021, 30, 105583. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosário, M.; Fonseca, A.C. Update on Biomarkers Associated with Large-Artery Atherosclerosis Stroke. Biomolecules 2023, 13, 1251. https://doi.org/10.3390/biom13081251
Rosário M, Fonseca AC. Update on Biomarkers Associated with Large-Artery Atherosclerosis Stroke. Biomolecules. 2023; 13(8):1251. https://doi.org/10.3390/biom13081251
Chicago/Turabian StyleRosário, Madalena, and Ana Catarina Fonseca. 2023. "Update on Biomarkers Associated with Large-Artery Atherosclerosis Stroke" Biomolecules 13, no. 8: 1251. https://doi.org/10.3390/biom13081251
APA StyleRosário, M., & Fonseca, A. C. (2023). Update on Biomarkers Associated with Large-Artery Atherosclerosis Stroke. Biomolecules, 13(8), 1251. https://doi.org/10.3390/biom13081251







