The Effects and Mechanisms of PBM Therapy in Accelerating Orthodontic Tooth Movement
Abstract
1. Introduction
2. The Efficacy of PBM Therapy on OTM in Cell and Animal Experiments
3. The Chromophores of PBM Therapy
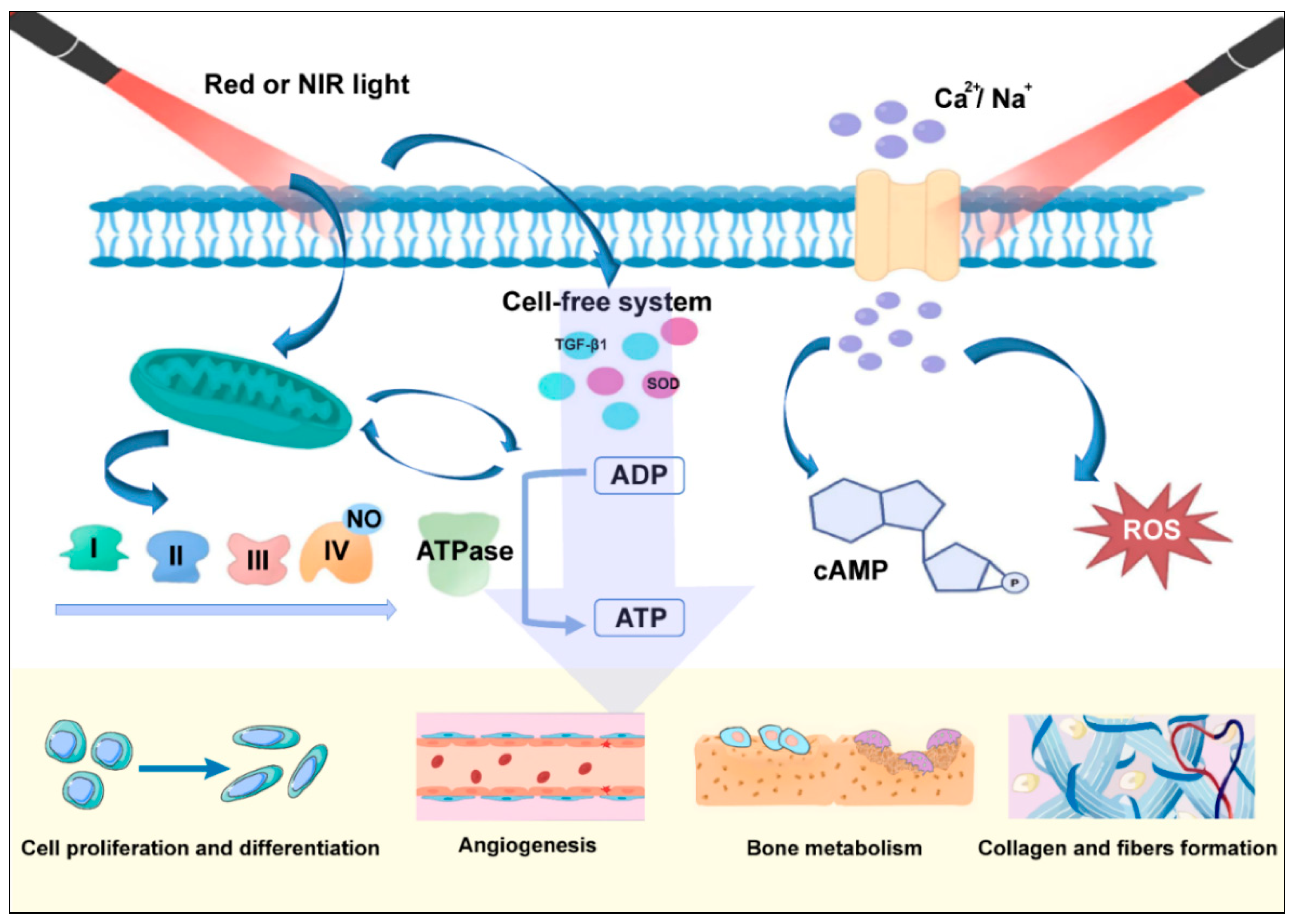
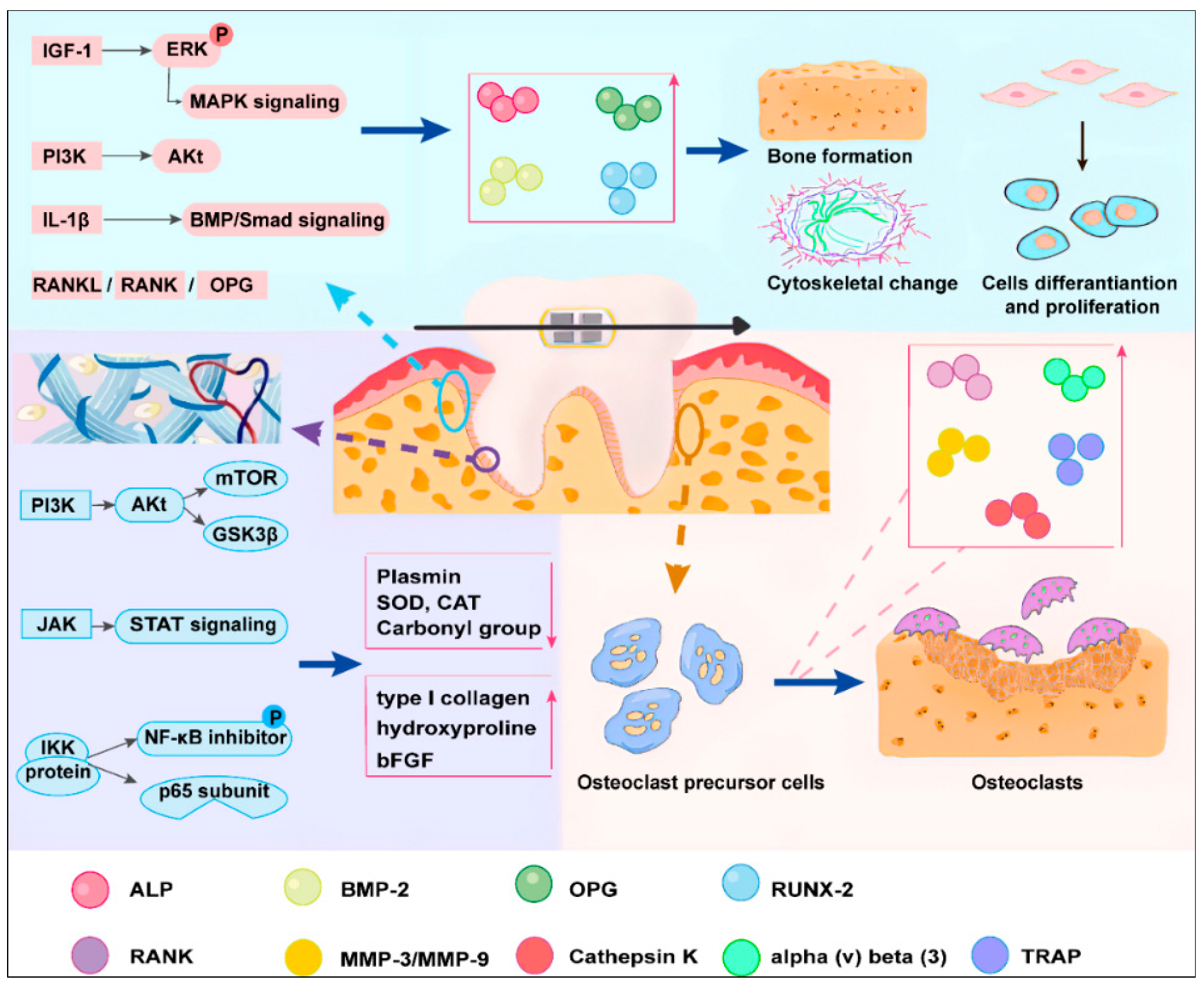
4. PBM-Therapy-Related Cytokines and Signaling in Orthodontic Treatment
4.1. Blood Vessels
4.2. Inflammatory Response
4.3. Collagen and Fibers
4.4. Mineralized Tissues
5. Clinical Trials and Applications
6. Cooperative Effects of PBM Therapy and Clinical Translations
7. Comparison between PBM and the Other Methods in OTM
8. Discussion and Perspectives
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [PubMed]
- Barlow, M.; Kula, K. Factors influencing efficiency of sliding mechanics to close extraction space: A systematic review. Orthod. Craniofac. Res. 2008, 11, 65–73. [Google Scholar] [CrossRef]
- Seifi, M.; Matini, N.S. Laser Surgery of Soft Tissue in Orthodontics: Review of the Clinical Trials. J. Lasers Med. Sci. 2017, 8 (Suppl. 1), S1–S6. [Google Scholar] [CrossRef] [PubMed]
- Moon, K.S.; Bae, J.M.; Park, Y.B.; Choi, E.J.; Oh, S.H. Photobiomodulation-Based Synergic Effects of Pt-Coated TiO(2) Nanotubes and 850 nm Near-Infrared Irradiation on the Osseointegration Enhancement: In Vitro and In Vivo Evaluation. Nanomaterial 2023, 13, 1377. [Google Scholar] [CrossRef]
- Austin, E.; Geisler, A.N.; Nguyen, J.; Kohli, I.; Hamzavi, I.; Lim, H.W.; Jagdeo, J. Visible light. Part I: Properties and cutaneous effects of visible light. J. Am. Acad. Dermatol. 2021, 84, 1219–1231. [Google Scholar] [CrossRef]
- Finlayson, L.; Barnard, I.R.M.; McMillan, L.; Ibbotson, S.H.; Brown, C.T.A.; Eadie, E.; Wood, K. Depth Penetration of Light into Skin as a Function of Wavelength from 200 to 1000 nm. Photochem. Photobiol. 2022, 98, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Chen, Z.; Li, X.; Yang, M.; Lv, J.; Li, H.; Yuan, Z. Chemiluminescence in Combination with Organic Photosensitizers: Beyond the Light Penetration Depth Limit of Photodynamic Therapy. Int. J. Mol. Sci. 2022, 23, 12556. [Google Scholar] [CrossRef] [PubMed]
- Thilwind, R.E.; ’t Hooft, G.; Uzunbajakava, N.E. Improved depth resolution in near-infrared diffuse reflectance spectroscopy using obliquely oriented fibers. J. Biomed. Opt. 2009, 14, 024026. [Google Scholar] [CrossRef]
- Fan, W.; Huang, P.; Chen, X. Overcoming the Achilles’ heel of photodynamic therapy. Chem. Soc. Rev. 2016, 45, 6488–6519. [Google Scholar] [CrossRef]
- Hamblin, M.R. Photobiomodulation for the management of alopecia: Mechanisms of action, patient selection and perspectives. Clin. Cosmet Investig. Dermatol. 2019, 12, 669–678. [Google Scholar] [CrossRef]
- Mester, E.; Szende, B.; Spiry, T.; Scher, A. Stimulation of wound healing by laser rays. Acta Chir. Acad. Sci. Hung. 1972, 13, 315–324. [Google Scholar]
- Jin, H.; Zou, Z.; Chang, H.; Shen, Q.; Liu, L.; Xing, D. Photobiomodulation therapy for hair regeneration: A synergetic activation of β-CATENIN in hair follicle stem cells by ROS and paracrine WNTs. Stem Cell Rep. 2021, 16, 1568–1583. [Google Scholar] [CrossRef]
- Jun, I.; Han, S.J.; Shin, H.S.; Kim, J.; Kim, E.K.; Kim, T.I.; Yoon, S.C.; Seo, K.Y. Comparison of ophthalmic toxicity of light-emitting diode and organic light-emitting diode light sources. Sci. Rep. 2020, 10, 11582. [Google Scholar] [CrossRef] [PubMed]
- Lapchak, P.A.; Wei, J.; Zivin, J.A. Transcranial infrared laser therapy improves clinical rating scores after embolic strokes in rabbits. Stroke 2004, 35, 1985–1988. [Google Scholar] [CrossRef] [PubMed]
- Tucker, L.D.; Lu, Y.; Dong, Y.; Yang, L.; Li, Y.; Zhao, N.; Zhang, Q. Photobiomodulation Therapy Attenuates Hypoxic-Ischemic Injury in a Neonatal Rat Model. J. Mol. Neurosci. 2018, 65, 514–526. [Google Scholar] [CrossRef]
- Trelles, M.A.; Mayayo, E. Bone fracture consolidates faster with low-power laser. Lasers Surg. Med. 1987, 7, 36–45. [Google Scholar] [CrossRef]
- Pick, R.M.; Pecaro, B.C.; Silberman, C.J. The laser gingivectomy. The use of the CO2 laser for the removal of phenytoin hyperplasia. J. Periodontol. 1985, 56, 492–496. [Google Scholar] [CrossRef]
- Arany, P.R. Craniofacial Wound Healing with Photobiomodulation Therapy: New Insights and Current Challenges. J. Dent. Res. 2016, 95, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Sgolastra, F.; Petrucci, A.; Severino, M.; Gatto, R.; Monaco, A. Lasers for the treatment of dentin hypersensitivity: A meta-analysis. J. Dent. Res. 2013, 92, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Peralta-Mamani, M.; da Silva, B.M.; da Silva Pinto, A.C.; Rubira-Bullen, I.R.F.; Honório, H.M.; Rubira, C.M.F.; da Silva Santos, P.S. Low-level laser therapy dosimetry most used for oral mucositis due to radiotherapy for head and neck cancer: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2019, 138, 14–23. [Google Scholar] [CrossRef]
- Fazlyab, M.; Esmaeili Shahmirzadi, S.; Esnaashari, E.; Azizi, A.; Moshari, A.A. Effect of low-level laser therapy on postoperative pain after single-visit root canal retreatment of mandibular molars: A randomized controlled clinical trial. Int. Endod. J. 2021, 54, 2006–2015. [Google Scholar] [CrossRef]
- Wu, S.; Chen, Y.; Zhang, J.; Chen, W.; Shao, S.; Shen, H.; Zhu, L.; Ye, P.; Svensson, P.; Wang, K. Effect of low-level laser therapy on tooth-related pain and somatosensory function evoked by orthodontic treatment. Int. J. Oral Sci. 2018, 10, 22. [Google Scholar] [CrossRef]
- Bjordal, J.M.; Johnson, M.I.; Iversen, V.; Aimbire, F.; Lopes-Martins, R.A. Low-level laser therapy in acute pain: A systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed. Laser Surg. 2006, 24, 158–168. [Google Scholar] [CrossRef]
- Kawasaki, K.; Shimizu, N. Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg. Med. 2000, 26, 282–291. [Google Scholar] [CrossRef]
- Wan, Z.; Zhang, P.; Lv, L.; Zhou, Y. NIR light-assisted phototherapies for bone-related diseases and bone tissue regeneration: A systematic review. Theranostics 2020, 10, 11837–11861. [Google Scholar] [CrossRef]
- Yang, H.; Liu, J.; Yang, K. Comparative Study of 660 and 830 nm Photobiomodulation in Promoting Orthodontic Tooth Movement. Photobiomodul. Photomed. Laser Surg. 2019, 37, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.P.; Tadinada, A.; Dutra, E.H.; Utreja, A.; Uribe, F.; Reichenberger, E.J. Dental Anomalies Associated with Craniometaphyseal Dysplasia. J. Dent. Res. 2014, 93, 553–558. [Google Scholar] [CrossRef]
- Olek, M.; Machorowska-Pieniążek, A.; Stós, W.; Kalukin, J.; Bartusik-Aebisher, D.; Aebisher, D.; Cieślar, G.; Kawczyk-Krupka, A. Photodynamic Therapy in Orthodontics: A Literature Review. Pharmaceutics 2021, 13, 720. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Wang, Y.; Jian, F.; Liao, L.N.; Yang, X.; Lai, W.L. Current advances in orthodontic pain. Int. J. Oral. Sci. 2016, 8, 67–75. [Google Scholar] [CrossRef]
- Glass, G.E. Photobiomodulation: The Clinical Applications of Low-Level Light Therapy. Aesthet. Surg. J. 2021, 41, 723–738. [Google Scholar] [CrossRef] [PubMed]
- Dompe, C.; Moncrieff, L.; Matys, J.; Grzech-Leśniak, K.; Kocherova, I.; Bryja, A.; Bruska, M.; Dominiak, M.; Mozdziak, P.; Skiba, T.H.I.; et al. Photobiomodulation-Underlying Mechanism and Clinical Applications. J. Clin. Med. 2020, 9, 1724. [Google Scholar] [CrossRef] [PubMed]
- Nimeri, G.; Kau, C.H.; Abou-Kheir, N.S.; Corona, R. Acceleration of tooth movement during orthodontic treatment--a frontier in orthodontics. Prog. Orthod. 2013, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.D.; Milward, M.R.; Cooper, P.R.; Hadis, M.; Palin, W.M. Developments in low level light therapy (LLLT) for dentistry. Dent. Mater. 2014, 30, 465–475. [Google Scholar] [CrossRef]
- Li, W.; Zheng, J.; Xu, Y.; Niu, W.; Guo, D.; Cui, J.; Bian, W.; Wang, X.; Niu, J. Remodeling of the periodontal ligament and alveolar bone during axial tooth movement in mice with type 1 diabetes. Front. Endocrinol. 2023, 14, 1098702. [Google Scholar] [CrossRef]
- Meikle, M.C. The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur. J. Orthod. 2006, 28, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Sokos, D.; Everts, V.; de Vries, T.J. Role of periodontal ligament fibroblasts in osteoclastogenesis: A review. J. Periodontal Res. 2015, 50, 152–159. [Google Scholar] [CrossRef]
- Craveiro, R.B.; Florea, A.; Niederau, C.; Brenji, S.; Kiessling, F.; Sahnoun, S.E.M.; Morgenroth, A.; Mottaghy, F.M.; Wolf, M. [(68)Ga]Ga-Pentixafor and Sodium [(18)F]Fluoride PET Can Non-Invasively Identify and Monitor the Dynamics of Orthodontic Tooth Movement in Mouse Model. Cells 2022, 11, 2949. [Google Scholar] [CrossRef]
- Yan, T.; Xie, Y.; He, H.; Fan, W.; Huang, F. Role of nitric oxide in orthodontic tooth movement (Review). Int. J. Mol. Med. 2021, 48, 168. [Google Scholar] [CrossRef]
- Suzuki, S.S.; Garcez, A.S.; Suzuki, H.; Ervolino, E.; Moon, W.; Ribeiro, M.S. Low-level laser therapy stimulates bone metabolism and inhibits root resorption during tooth movement in a rodent model. J. Biophotonics 2016, 9, 1222–1235. [Google Scholar] [CrossRef]
- Altan, A.B.; Bicakci, A.A.; Mutaf, H.I.; Ozkut, M.; Inan, V.S. The effects of low-level laser therapy on orthodontically induced root resorption. Lasers Med. Sci. 2015, 30, 2067–2076. [Google Scholar] [CrossRef]
- Higashi, D.T.; Andrello, A.C.; Tondelli, P.M.; de Oliveira Toginho Filho, D.; de Paula Ramos, S. Three consecutive days of application of LED therapy is necessary to inhibit experimentally induced root resorption in rats: A microtomographic study. Lasers Med. Sci. 2017, 32, 181–187. [Google Scholar] [CrossRef]
- Baser Keklikci, H.; Yagci, A.; Yay, A.H.; Goktepe, O. Effects of 405-, 532-, 650-, and 940-nm wavelengths of low-level laser therapies on orthodontic tooth movement in rats. Prog. Orthod. 2020, 21, 43. [Google Scholar] [CrossRef] [PubMed]
- Kushibiki, T.; Hirasawa, T.; Okawa, S.; Ishihara, M. Blue laser irradiation generates intracellular reactive oxygen species in various types of cells. Photomed. Laser Surg. 2013, 31, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Baser Keklikci, H.; Yagci, A. Effects of different wavelengths of low-level laser therapy on orthodontically induced inflammatory root resorption in rats investigated with micro-computerized tomography. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e245–e251. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, Y.Y.; Wang, Y.; Lyu, P.; Hamblin, M.R. Photobiomodulation (blue and green light) encourages osteoblastic-differentiation of human adipose-derived stem cells: Role of intracellular calcium and light-gated ion channels. Sci. Rep. 2016, 6, 33719. [Google Scholar] [CrossRef]
- Jawad, M.M.; Husein, A.; Azlina, A.; Alam, M.K.; Hassan, R.; Shaari, R. Effect of 940 nm low-level laser therapy on osteogenesis in vitro. J. Biomed. Opt. 2013, 18, 128001. [Google Scholar] [CrossRef] [PubMed]
- Fujita, S.; Yamaguchi, M.; Utsunomiya, T.; Yamamoto, H.; Kasai, K. Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod. Craniofac. Res. 2008, 11, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Cifter, M.; Celikel, A.D.G.; Cifter, E.D.; Tagrikulu, B.; Olgaç, V.; Erdem, M.A.; Cankaya, A.B. Comparison of the efficiency of alveolar decortication and low level laser therapy on orthodontic tooth movement and alveolar metabolism in rats. J. Dent. Sci. 2019, 14, 401–407. [Google Scholar] [CrossRef]
- Maia, L.G.; Alves, A.V.; Bastos, T.S.; Moromizato, L.S.; Lima-Verde, I.B.; Ribeiro, M.A.; Gandini Júnior, L.G.; de Albuquerque-Júnior, R.L. Histological analysis of the periodontal ligament and alveolar bone during dental movement in diabetic rats subjected to low-level laser therapy. J. Photochem. Photobiol. B 2014, 135, 65–74. [Google Scholar] [CrossRef]
- Suzuki, S.S.; Garcez, A.S.; Reese, P.O.; Suzuki, H.; Ribeiro, M.S.; Moon, W. Effects of corticopuncture (CP) and low-level laser therapy (LLLT) on the rate of tooth movement and root resorption in rats using micro-CT evaluation. Lasers Med. Sci. 2018, 33, 811–821. [Google Scholar] [CrossRef]
- Alazzawi, M.M.J.; Husein, A.; Alam, M.K.; Hassan, R.; Shaari, R.; Azlina, A.; Salzihan, M.S. Effect of low level laser and low intensity pulsed ultrasound therapy on bone remodeling during orthodontic tooth movement in rats. Prog. Orthod. 2018, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Na, S.; TruongVo, T.; Jiang, F.; Joll, J.E.; Guo, Y.; Utreja, A.; Chen, J. Dose analysis of photobiomodulation therapy on osteoblast, osteoclast, and osteocyte. J. Biomed. Opt. 2018, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, C.; Wu, F. Low-level laser irradiation enhances the proliferation and osteogenic differentiation of PDLSCs via BMP signaling. Lasers Med. Sci. 2022, 37, 941–948. [Google Scholar] [CrossRef]
- Wang, L.; Liu, C.; Song, Y.; Wu, F. The effect of low-level laser irradiation on the proliferation, osteogenesis, inflammatory reaction, and oxidative stress of human periodontal ligament stem cells under inflammatory conditions. Lasers Med. Sci. 2022, 37, 3591–3599. [Google Scholar] [CrossRef]
- Houreld, N.N.; Abrahamse, H. Laser light influences cellular viability and proliferation in diabetic-wounded fibroblast cells in a dose- and wavelength-dependent manner. Lasers Med. Sci. 2008, 23, 11–18. [Google Scholar] [CrossRef]
- Huang, Y.Y.; Chen, A.C.; Carroll, J.D.; Hamblin, M.R. Biphasic dose response in low level light therapy. Dose Response 2009, 7, 358–383. [Google Scholar] [CrossRef]
- Karu, T. Photobiology of low-power laser effects. Health Phys. 1989, 56, 691–704. [Google Scholar] [CrossRef] [PubMed]
- Pires Oliveira, D.A.; de Oliveira, R.F.; Zangaro, R.A.; Soares, C.P. Evaluation of low-level laser therapy of osteoblastic cells. Photomed. Laser Surg. 2008, 26, 401–404. [Google Scholar] [CrossRef]
- Pastore, D.; Greco, M.; Passarella, S. Specific helium-neon laser sensitivity of the purified cytochrome c oxidase. Int. J. Radiat. Biol. 2000, 76, 863–870. [Google Scholar] [CrossRef]
- Masha, R.T.; Houreld, N.N.; Abrahamse, H. Low-intensity laser irradiation at 660 nm stimulates transcription of genes involved in the electron transport chain. Photomed. Laser Surg. 2013, 31, 47–53. [Google Scholar] [CrossRef]
- Houreld, N.N.; Masha, R.T.; Abrahamse, H. Low-intensity laser irradiation at 660 nm stimulates cytochrome c oxidase in stressed fibroblast cells. Lasers Surg. Med. 2012, 44, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Huang, M.; Chen, X.; Chen, J.; Zou, Z.; Li, L.; Ji, K.; Nie, Z.; Yang, B.; Wei, Z.; et al. The role of S-nitrosylation of PFKM in regulation of glycolysis in ovarian cancer cells. Cell Death Dis. 2021, 12, 408. [Google Scholar] [CrossRef]
- Lane, N. Cell biology: Power games. Nature 2006, 443, 901–903. [Google Scholar] [CrossRef]
- de Freitas, L.F.; Hamblin, M.R. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE J. Sel. Top. Quantum Electron. 2016, 22, 7000417. [Google Scholar] [CrossRef] [PubMed]
- Karu, T.I. Mitochondrial signaling in mammalian cells activated by red and near-IR radiation. Photochem. Photobiol. 2008, 84, 1091–1099. [Google Scholar] [CrossRef]
- Chellini, F.; Sassoli, C.; Nosi, D.; Deledda, C.; Tonelli, P.; Zecchi-Orlandini, S.; Formigli, L.; Giannelli, M. Low pulse energy Nd:YAG laser irradiation exerts a biostimulative effect on different cells of the oral microenvironment: “An in vitro study”. Lasers Surg. Med. 2010, 42, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Tani, A.; Chellini, F.; Giannelli, M.; Nosi, D.; Zecchi-Orlandini, S.; Sassoli, C. Red (635 nm), Near-Infrared (808 nm) and Violet-Blue (405 nm) Photobiomodulation Potentiality on Human Osteoblasts and Mesenchymal Stromal Cells: A Morphological and Molecular In Vitro Study. Int. J. Mol. Sci. 2018, 19, 1946. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, D.; Schwarz, W. TRPV Channels in Mast Cells as a Target for Low-Level-Laser Therapy. Cells 2014, 3, 662–673. [Google Scholar] [CrossRef]
- Yuan, J.; Liu, H.; Zhang, H.; Wang, T.; Zheng, Q.; Li, Z. Controlled Activation of TRPV1 Channels on Microglia to Boost Their Autophagy for Clearance of Alpha-Synuclein and Enhance Therapy of Parkinson’s Disease. Adv. Mater. 2022, 34, e2108435. [Google Scholar] [CrossRef]
- Peng, J.; Zhao, J.; Tang, Q.; Wang, J.; Song, W.; Lu, X.; Huang, X.; Chen, G.; Zheng, W.; Zhang, L.; et al. Low intensity near-infrared light promotes bone regeneration via circadian clock protein cryptochrome 1. Int. J. Oral Sci. 2022, 14, 53. [Google Scholar] [CrossRef]
- Arany, P.R.; Cho, A.; Hunt, T.D.; Sidhu, G.; Shin, K.; Hahm, E.; Huang, G.X.; Weaver, J.; Chen, A.C.; Padwa, B.L.; et al. Photoactivation of endogenous latent transforming growth factor-β1 directs dental stem cell differentiation for regeneration. Sci. Transl. Med. 2014, 6, 238ra69. [Google Scholar] [CrossRef]
- Vladimirov, Y.A.; Gorbatenkova, E.A.; Paramonov, N.V.; Azizova, O.A. Photoreactivation of superoxide dismutase by intensive red (laser) light. Free Radic. Biol. Med. 1988, 5, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Davidovitch, Z.; Nicolay, O.F.; Ngan, P.W.; Shanfeld, J.L. Neurotransmitters, cytokines, and the control of alveolar bone remodeling in orthodontics. Dent. Clin. N. Am. 1988, 32, 411–435. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhan, Q.; Bao, M.; Yi, J.; Li, Y. Biomechanical and biological responses of periodontium in orthodontic tooth movement: Up-date in a new decade. Int. J. Oral Sci. 2021, 13, 20. [Google Scholar] [CrossRef]
- Domínguez, A.; Velásquez, S.A. Acceleration of Dental Movement by Photobiomodulation: How Does It Happen? Photobiomodul. Photomed. Laser Surg. 2021, 39, 379–380. [Google Scholar] [CrossRef] [PubMed]
- Altan, B.A.; Sokucu, O.; Ozkut, M.M.; Inan, S. Metrical and histological investigation of the effects of low-level laser therapy on orthodontic tooth movement. Lasers Med. Sci. 2012, 27, 131–140. [Google Scholar] [CrossRef]
- Hsu, L.F.; Tsai, M.H.; Shih, A.H.; Chen, Y.C.; Chang, B.E.; Chen, Y.J.; Yao, C.J. 970 nm low-level laser affects bone metabolism in orthodontic tooth movement. J. Photochem. Photobiol. B 2018, 186, 41–50. [Google Scholar] [CrossRef]
- Tim, C.R.; Bossini, P.S.; Kido, H.W.; Malavazi, I.; von Zeska Kress, M.R.; Carazzolle, M.F.; Parizotto, N.A.; Rennó, A.C. Effects of low level laser therapy on inflammatory and angiogenic gene expression during the process of bone healing: A microarray analysis. J. Photochem. Photobiol. B 2016, 154, 8–15. [Google Scholar] [CrossRef]
- Hayashi, H.; Terao, A.; Kunimatsu, R.; Kawata, T. Effects of a low level laser on periodontal tissue in hypofunctional teeth. PLoS ONE 2014, 9, e100066. [Google Scholar] [CrossRef]
- Wang, Q.; Chang, H.; Shen, Q.; Li, Y.; Xing, D. Photobiomodulation therapy for thrombocytopenia by upregulating thrombopoietin expression via the ROS-dependent Src/ERK/STAT3 signaling pathway. J. Thromb. Haemost. 2021, 19, 2029–2043. [Google Scholar] [CrossRef]
- Abi-Ramia, L.B.; Stuani, A.S.; Stuani, A.S.; Stuani, M.B.; Mendes Ade, M. Effects of low-level laser therapy and orthodontic tooth movement on dental pulps in rats. Angle Orthod. 2010, 80, 116–122. [Google Scholar] [CrossRef]
- Pansani, T.N.; Basso, F.G.; Turrioni, A.P.; Soares, D.G.; Hebling, J.; de Souza Costa, C.A. Effects of low-level laser therapy and epidermal growth factor on the activities of gingival fibroblasts obtained from young or elderly individuals. Lasers Med. Sci. 2017, 32, 45–52. [Google Scholar] [CrossRef]
- Wang, X.; Tian, F.; Soni, S.S.; Gonzalez-Lima, F.; Liu, H. Interplay between up-regulation of cytochrome-c-oxidase and hemoglobin oxygenation induced by near-infrared laser. Sci. Rep. 2016, 6, 30540. [Google Scholar] [CrossRef] [PubMed]
- Rupel, K.; Zupin, L.; Colliva, A.; Kamada, A.; Poropat, A.; Ottaviani, G.; Gobbo, M.; Fanfoni, L.; Gratton, R.; Santoro, M.; et al. Photobiomodulation at Multiple Wavelengths Differentially Modulates Oxidative Stress In Vitro and In Vivo. Oxid. Med. Cell Longev. 2018, 2018, 6510159. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, N.; Yamaguchi, M.; Goseki, T.; Shibata, Y.; Takiguchi, H.; Iwasawa, T.; Abiko, Y. Inhibition of prostaglandin E2 and interleukin 1-beta production by low-power laser irradiation in stretched human periodontal ligament cells. J. Dent. Res. 1995, 74, 1382–1388. [Google Scholar] [CrossRef]
- Varella, A.M.; Revankar, A.V.; Patil, A.K. Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 535–544.e535. [Google Scholar] [CrossRef] [PubMed]
- Üretürk, S.E.; Saraç, M.; Fıratlı, S.; Can, Ş.B.; Güven, Y.; Fıratlı, E. The effect of low-level laser therapy on tooth movement during canine distalization. Lasers Med. Sci. 2017, 32, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Eid, F.Y.; El-Kenany, W.A.; Mowafy, M.I.; El-Kalza, A.R.; Guindi, M.A. A randomized controlled trial evaluating the effect of two low-level laser irradiation protocols on the rate of canine retraction. Sci. Rep. 2022, 12, 10074. [Google Scholar] [CrossRef]
- Kaya, Y.; Alkan, Ö.; Kömüroglu, A.U.; Keskin, S. Effects of ibuprofen and low-level laser therapy on orthodontic pain by means of the analysis of interleukin 1-beta and substance P levels in the gingival crevicular fluid. J. Orofac. Orthop. 2021, 82, 143–152. [Google Scholar] [CrossRef]
- Bicakci, A.A.; Kocoglu-Altan, B.; Toker, H.; Mutaf, I.; Sumer, Z. Efficiency of low-level laser therapy in reducing pain induced by orthodontic forces. Photomed. Laser Surg. 2012, 30, 460–465. [Google Scholar] [CrossRef]
- Pourzarandian, A.; Watanabe, H.; Ruwanpura, S.M.; Aoki, A.; Noguchi, K.; Ishikawa, I. Er:YAG laser irradiation increases prostaglandin E production via the induction of cyclooxygenase-2 mRNA in human gingival fibroblasts. J. Periodontal Res. 2005, 40, 182–186. [Google Scholar] [CrossRef]
- Sakurai, Y.; Yamaguchi, M.; Abiko, Y. Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur. J. Oral Sci. 2000, 108, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Pallotta, R.C.; Bjordal, J.M.; Frigo, L.; Leal Junior, E.C.; Teixeira, S.; Marcos, R.L.; Ramos, L.; Messias Fde, M.; Lopes-Martins, R.A. Infrared (810-nm) low-level laser therapy on rat experimental knee inflammation. Lasers Med. Sci. 2012, 27, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, Y.; Shimizu, N.; Abiko, Y. Low-energy diode laser irradiation reduced plasminogen activator activity in human periodontal ligament cells. Lasers Surg. Med. 1997, 21, 456–463. [Google Scholar] [CrossRef]
- Silveira, P.C.; Silva, L.A.; Freitas, T.P.; Latini, A.; Pinho, R.A. Effects of low-power laser irradiation (LPLI) at different wavelengths and doses on oxidative stress and fibrogenesis parameters in an animal model of wound healing. Lasers Med. Sci. 2011, 26, 125–131. [Google Scholar] [CrossRef]
- Milligan, M.; Arudchelvan, Y.; Gong, S.G. Effects of two wattages of low-level laser therapy on orthodontic tooth movement. Arch. Oral Biol. 2017, 80, 62–68. [Google Scholar] [CrossRef]
- Kim, Y.D.; Kim, S.S.; Kim, S.J.; Kwon, D.W.; Jeon, E.S.; Son, W.S. Low-level laser irradiation facilitates fibronectin and collagen type I turnover during tooth movement in rats. Lasers Med. Sci. 2010, 25, 25–31. [Google Scholar] [CrossRef]
- Chen, A.C.; Arany, P.R.; Huang, Y.Y.; Tomkinson, E.M.; Sharma, S.K.; Kharkwal, G.B.; Saleem, T.; Mooney, D.; Yull, F.E.; Blackwell, T.S.; et al. Low-level laser therapy activates NF-kB via generation of reactive oxygen species in mouse embryonic fibroblasts. PLoS ONE 2011, 6, e22453. [Google Scholar] [CrossRef]
- Shingyochi, Y.; Kanazawa, S.; Tajima, S.; Tanaka, R.; Mizuno, H.; Tobita, M. A Low-Level Carbon Dioxide Laser Promotes Fibroblast Proliferation and Migration through Activation of Akt, ERK, and JNK. PLoS ONE 2017, 12, e0168937. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, F.A.; Matos, A.A.; Matsuda, S.S.; Buzalaf, M.A.; Bagnato, V.S.; Machado, M.A.; Damante, C.A.; Oliveira, R.C.; Peres-Buzalaf, C. Low level laser therapy modulates viability, alkaline phosphatase and matrix metalloproteinase-2 activities of osteoblasts. J. Photochem. Photobiol. B 2017, 169, 35–40. [Google Scholar] [CrossRef]
- Aihara, N.; Yamaguchi, M.; Kasai, K. Low-energy irradiation stimulates formation of osteoclast-like cells via RANK expression in vitro. Lasers Med. Sci. 2006, 21, 24–33. [Google Scholar] [CrossRef]
- Ninomiya, T.; Hosoya, A.; Nakamura, H.; Sano, K.; Nishisaka, T.; Ozawa, H. Increase of bone volume by a nanosecond pulsed laser irradiation is caused by a decreased osteoclast number and an activated osteoblasts. Bone 2007, 40, 140–148. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Hayashi, M.; Fujita, S.; Yoshida, T.; Utsunomiya, T.; Yamamoto, H.; Kasai, K. Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta(3) integrin in rats. Eur. J. Orthod. 2010, 32, 131–139. [Google Scholar] [CrossRef]
- Gomes, M.F.; da Graças Vilela Goulart, M.; Giannasi, L.C.; Hiraoka, C.M.; de Fátima Santana Melo, G.; de Sousa, A.G.V.; Nóbrega, C.J.P.; Zangaro, R.A.; Salgado, M.A.C. Effects of the GaAlAs diode laser (780 nm) on the periodontal tissues during orthodontic tooth movement in diabetes rats: Histomorphological and immunohistochemical analysis. Lasers Med. Sci. 2017, 32, 1479–1487. [Google Scholar] [CrossRef]
- Kiyosaki, T.; Mitsui, N.; Suzuki, N.; Shimizu, N. Low-level laser therapy stimulates mineralization via increased Runx2 expression and ERK phosphorylation in osteoblasts. Photomed. Laser Surg. 2010, 28 (Suppl. 1), S167–S172. [Google Scholar] [CrossRef]
- Oliveira, F.A.; Matos, A.A.; Santesso, M.R.; Tokuhara, C.K.; Leite, A.L.; Bagnato, V.S.; Machado, M.A.; Peres-Buzalaf, C.; Oliveira, R.C. Low intensity lasers differently induce primary human osteoblast proliferation and differentiation. J. Photochem. Photobiol. B 2016, 163, 14–21. [Google Scholar] [CrossRef]
- Wu, Y.H.; Wang, J.; Gong, D.X.; Gu, H.Y.; Hu, S.S.; Zhang, H. Effects of low-level laser irradiation on mesenchymal stem cell proliferation: A microarray analysis. Lasers Med. Sci. 2012, 27, 509–519. [Google Scholar] [CrossRef]
- Zheng, J.; Yang, K. Clinical research: Low-level laser therapy in accelerating orthodontic tooth movement. BMC Oral Health 2021, 21, 324. [Google Scholar] [CrossRef] [PubMed]
- Tidball, J.G.; Villalta, S.A. Regulatory interactions between muscle and the immune system during muscle regeneration. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 298, R1173–R1187. [Google Scholar] [CrossRef] [PubMed]
- Souza, N.H.; Ferrari, R.A.; Silva, D.F.; Nunes, F.D.; Bussadori, S.K.; Fernandes, K.P. Effect of low-level laser therapy on the modulation of the mitochondrial activity of macrophages. Braz. J. Phys. Ther. 2014, 18, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Fujikado, N.; Manaka, H.; Yasuda, H.; Iwakura, Y. IL-1 plays an important role in the bone metabolism under physiological conditions. Int. Immunol. 2010, 22, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, P.; Kharbanda, O.P.; Monga, N.; Miglani, R.; Kapila, S. Effect of orthodontic forces on cytokine and receptor levels in gingival crevicular fluid: A systematic review. Prog. Orthod. 2014, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- d’Apuzzo, F.; Cappabianca, S.; Ciavarella, D.; Monsurrò, A.; Silvestrini-Biavati, A.; Perillo, L. Biomarkers of periodontal tissue remodeling during orthodontic tooth movement in mice and men: Overview and clinical relevance. Sci. World J. 2013, 2013, 105873. [Google Scholar] [CrossRef]
- Sanchez, T.; Moreno, J.J. Role of EP(1) and EP(4) PGE(2) subtype receptors in serum-induced 3T6 fibroblast cycle progression and proliferation. Am. J. Physiol. Cell Physiol. 2002, 282, C280–C288. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V. Orthodontic pain: From causes to management--a review. Eur. J. Orthod. 2007, 29, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Avellán, N.L.; Sorsa, T.; Tervahartiala, T.; Forster, C.; Kemppainen, P. Experimental tooth pain elevates substance P and matrix metalloproteinase-8 levels in human gingival crevice fluid. Acta Odontol. Scand. 2008, 66, 18–22. [Google Scholar] [CrossRef]
- Zecha, J.A.; Raber-Durlacher, J.E.; Nair, R.G.; Epstein, J.B.; Sonis, S.T.; Elad, S.; Hamblin, M.R.; Barasch, A.; Migliorati, C.A.; Milstein, D.M.; et al. Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: Part 1: Mechanisms of action, dosimetric, and safety considerations. Support. Care Cancer 2016, 24, 2781–2792. [Google Scholar] [CrossRef]
- Jere, S.W.; Abrahamse, H.; Houreld, N.N. The JAK/STAT signaling pathway and photobiomodulation in chronic wound healing. Cytokine Growth Factor Rev. 2017, 38, 73–79. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, Y.; Sun, X. [A study on expression of basic fibroblast growth factors in periodontal tissue following orthodontic tooth movement associated with low power laser irradiation]. Hua Xi Kou Qiang Yi Xue Za Zhi 2002, 20, 166–168. [Google Scholar]
- Tsuka, Y.; Kunimatsu, R.; Gunji, H.; Nakajima, K.; Kimura, A.; Hiraki, T.; Nakatani, A.; Tanimoto, K. Effects of Nd:YAG low-level laser irradiation on cultured human osteoblasts migration and ATP production: In vitro study. Lasers Med. Sci. 2019, 34, 55–60. [Google Scholar] [CrossRef]
- Ozawa, Y.; Shimizu, N.; Kariya, G.; Abiko, Y. Low-energy laser irradiation stimulates bone nodule formation at early stages of cell culture in rat calvarial cells. Bone 1998, 22, 347–354. [Google Scholar] [CrossRef]
- Jettar, V.; Napimoga, M.H.; Freitas, F.; Clemente-Napimoga, J.T.; Suzuki, S.S.; Montalli, V.A.; Garcez, A.S. Effects of Photobiomodulation on SOFAT, A T-cell-derived Cytokine, May Explain Accelerated Orthodontic Tooth Movement. Photochem. Photobiol. 2018, 94, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Mao, C.Y.; Wang, Y.G.; Zhang, X.; Zheng, X.Y.; Tang, T.T.; Lu, E.Y. Double-edged-sword effect of IL-1β on the osteogenesis of periodontal ligament stem cells via crosstalk between the NF-κB, MAPK and BMP/Smad signaling pathways. Cell Death Dis. 2016, 7, e2296. [Google Scholar] [CrossRef]
- Kushibiki, T.; Awazu, K. Blue laser irradiation enhances extracellular calcification of primary mesenchymal stem cells. Photomed. Laser Surg. 2009, 27, 493–498. [Google Scholar] [CrossRef]
- Domínguez, A.; Gómez, C.; Palma, J.C. Effects of low-level laser therapy on orthodontics: Rate of tooth movement, pain, and release of RANKL and OPG in GCF. Lasers Med. Sci. 2015, 30, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Domínguez Camacho, A.; Montoya Guzmán, D.; Velásquez Cujar, S.A. Effective Wavelength Range in Photobiomodulation for Tooth Movement Acceleration in Orthodontics: A Systematic Review. Photobiomodul. Photomed. Laser Surg. 2020, 38, 581–590. [Google Scholar] [CrossRef] [PubMed]
- AlSayed Hasan, M.M.A.; Sultan, K.; Hamadah, O. Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: A randomized controlled clinical trial. Angle Orthod. 2017, 87, 499–504. [Google Scholar] [CrossRef]
- Doshi-Mehta, G.; Bhad-Patil, W.A. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: A clinical investigation. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 289–297. [Google Scholar] [CrossRef]
- Genc, G.; Kocadereli, I.; Tasar, F.; Kilinc, K.; El, S.; Sarkarati, B. Effect of low-level laser therapy (LLLT) on orthodontic tooth movement. Lasers Med. Sci. 2013, 28, 41–47. [Google Scholar] [CrossRef]
- Pérignon, B.; Bandiaky, O.N.; Fromont-Colson, C.; Renaudin, S.; Peré, M.; Badran, Z.; Cuny-Houchmand, M.; Soueidan, A. Effect of 970 nm low-level laser therapy on orthodontic tooth movement during Class II intermaxillary elastics treatment: A RCT. Sci. Rep. 2021, 11, 23226. [Google Scholar] [CrossRef]
- Mistry, D.; Dalci, O.; Papageorgiou, S.N.; Darendeliler, M.A.; Papadopoulou, A.K. The effects of a clinically feasible application of low-level laser therapy on the rate of orthodontic tooth movement: A triple-blind, split-mouth, randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Al-Dboush, R.; Esfahani, A.N.; El-Bialy, T. Impact of photobiomodulation and low-intensity pulsed ultrasound adjunctive interventions on orthodontic treatment duration during clear aligner therapy. Angle Orthod. 2021, 91, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Caccianiga, G.; Crestale, C.; Cozzani, M.; Piras, A.; Mutinelli, S.; Lo Giudice, A.; Cordasco, G. Low-level laser therapy and invisible removal aligners. J. Biol. Regul. Homeost Agents 2016, 30, 107–113. [Google Scholar] [PubMed]
- Costa, A.C.F.; Maia, T.A.C.; de Barros Silva, P.G.; Abreu, L.G.; Gondim, D.V.; Santos, P.C.F. Effects of low-level laser therapy on the orthodontic mini-implants stability: A systematic review and meta-analysis. Prog. Orthod. 2021, 22, 6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Huang, X.; Huo, S.; Zhang, C.; Cen, X.; Zhao, Z. Effect of photobiomodulation therapy on mini-implant stability: A systematic review and meta-analysis. Lasers Med. Sci. 2021, 36, 1557–1566. [Google Scholar] [CrossRef]
- Michelogiannakis, D.; Jabr, L.; Barmak, A.B.; Rossouw, P.E.; Kotsailidi, E.A.; Javed, F. Influence of low-level-laser therapy on the stability of orthodontic mini-screw implants. A systematic review and meta-analysis. Eur. J. Orthod. 2022, 44, 11–21. [Google Scholar] [CrossRef]
- Ng, D.; Chan, A.K.; Papadopoulou, A.K.; Dalci, O.; Petocz, P.; Darendeliler, M.A. The effect of low-level laser therapy on orthodontically induced root resorption: A pilot double blind randomized controlled trial. Eur. J. Orthod. 2018, 40, 317–325. [Google Scholar] [CrossRef]
- Eid, F.Y.; El-Kenany, W.A.; Mowafy, M.I.; El-Kalza, A.R. The influence of two photobiomodulation protocols on orthodontically induced inflammatory root resorption (a randomized controlled clinical trial). BMC Oral Health 2022, 22, 221. [Google Scholar] [CrossRef]
- Goymen, M.; Gulec, A. Effect of photobiomodulation therapies on the root resorption associated with orthodontic forces: A pilot study using micro computed tomography. Clin. Oral Investig. 2020, 24, 1431–1438. [Google Scholar] [CrossRef]
- Impellizzeri, A.; Horodynski, M.; Fusco, R.; Palaia, G.; Polimeni, A.; Romeo, U.; Barbato, E.; Galluccio, G. Photobiomodulation Therapy on Orthodontic Movement: Analysis of Preliminary Studies with a New Protocol. Int. J. Environ. Res. Public Health 2020, 17, 3547. [Google Scholar] [CrossRef]
- Spadari, G.S.; Zaniboni, E.; Vedovello, S.A.; Santamaria, M.P.; do Amaral, M.E.; Dos Santos, G.M.; Esquisatto, M.A.; Mendonca, F.A.; Santamaria, M., Jr. Electrical stimulation enhances tissue reorganization during orthodontic tooth movement in rats. Clin. Oral Investig. 2017, 21, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Wilcko, W.M.; Wilcko, T.; Bouquot, J.E.; Ferguson, D.J. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int. J. Periodontics Restor. Dent. 2001, 21, 9–19. [Google Scholar]
- Zaniboni, E.; Bagne, L.; Camargo, T.; do Amaral, M.E.C.; Felonato, M.; de Andrade, T.A.M.; Dos Santos, G.M.T.; Caetano, G.F.; Esquisatto, M.A.M.; Santamaria, M., Jr.; et al. Do electrical current and laser therapies improve bone remodeling during an orthodontic treatment with corticotomy? Clin. Oral Investig. 2019, 23, 4083–4097. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, N.R.; DiBiase, A.T.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Donaldson, A.N.; Cobourne, M.T. Supplemental vibrational force during orthodontic alignment: A randomized trial. J. Dent. Res. 2015, 94, 682–689. [Google Scholar] [CrossRef] [PubMed]
- Reiss, S.; Chouinard, M.C.; Frias Landa, D.; Nanda, R.; Chandhoke, T.; Sobue, T.; Allareddy, V.; Kuo, C.L.; Mu, J.; Uribe, F. Biomarkers of orthodontic tooth movement with fixed appliances and vibration appliance therapy: A pilot study. Eur. J. Orthod. 2020, 42, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Sekhavat, A.R.; Mousavizadeh, K.; Pakshir, H.R.; Aslani, F.S. Effect of misoprostol, a prostaglandin E1 analog, on orthodontic tooth movement in rats. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 542–547. [Google Scholar] [CrossRef]
- Kehoe, M.J.; Cohen, S.M.; Zarrinnia, K.; Cowan, A. The effect of acetaminophen, ibuprofen, and misoprostol on prostaglandin E2 synthesis and the degree and rate of orthodontic tooth movement. Angle Orthod. 1996, 66, 339–349. [Google Scholar]
- Yi, J.; Xiao, J.; Li, H.; Li, Y.; Li, X.; Zhao, Z. Effectiveness of adjunctive interventions for accelerating orthodontic tooth movement: A systematic review of systematic reviews. J. Oral Rehabil. 2017, 44, 636–654. [Google Scholar] [CrossRef]
- Stark, T.M.; Sinclair, P.M. Effect of pulsed electromagnetic fields on orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Gracco, A.; Finotti, M.; Bruno, G.; de Stefani, A. Corticotomy-assisted orthodontic camouflage in a class III adult patient with a severe transverse discrepancy. Int. Orthod. 2018, 16, 268–280. [Google Scholar] [CrossRef]
- Jindarojanakul, C.; Samruajbenjakun, B. Influence of ibuprofen combined with corticotomy on tooth movement and alveolar bone remodeling in rats. Angle Orthod. 2022, 92, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Alqadasi, B.; Xia, H.Y.; Alhammadi, M.S.; Hasan, H.; Aldhorae, K.; Halboub, E. Three-dimensional assessment of accelerating orthodontic tooth movement-micro-osteoperforations vs piezocision: A randomized, parallel-group and split-mouth controlled clinical trial. Orthod. Craniofac. Res. 2021, 24, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Gibreal, O.; Hajeer, M.Y.; Brad, B. Evaluation of the levels of pain and discomfort of piezocision-assisted flapless corticotomy when treating severely crowded lower anterior teeth: A single-center, randomized controlled clinical trial. BMC Oral. Health 2019, 19, 57. [Google Scholar] [CrossRef]
- Bicknell, B.; Liebert, A.; McLachlan, C.S.; Kiat, H. Microbiome Changes in Humans with Parkinson’s Disease after Photobiomodulation Therapy: A Retrospective Study. J. Pers. Med. 2022, 12, 49. [Google Scholar] [CrossRef]
- Liebert, A.; Bicknell, B.; Laakso, E.L.; Heller, G.; Jalilitabaei, P.; Tilley, S.; Mitrofanis, J.; Kiat, H. Improvements in clinical signs of Parkinson’s disease using photobiomodulation: A prospective proof-of-concept study. BMC Neurol. 2021, 21, 256. [Google Scholar] [CrossRef]
- Naeser, M.A.; Martin, P.I.; Ho, M.D.; Krengel, M.H.; Bogdanova, Y.; Knight, J.A.; Hamblin, M.R.; Fedoruk, A.E.; Poole, L.G.; Cheng, C.; et al. Transcranial Photobiomodulation Treatment: Significant Improvements in Four Ex-Football Players with Possible Chronic Traumatic Encephalopathy. J. Alzheimers Dis. Rep. 2023, 7, 77–105. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Tang, E.; Arany, P. Molecular pathway of near-infrared laser phototoxicity involves ATF-4 orchestrated ER stress. Sci. Rep. 2015, 5, 10581. [Google Scholar] [CrossRef]
- Moro, C.; Torres, N.; Arvanitakis, K.; Cullen, K.; Chabrol, C.; Agay, D.; Darlot, F.; Benabid, A.L.; Mitrofanis, J. No evidence for toxicity after long-term photobiomodulation in normal non-human primates. Exp. Brain Res. 2017, 235, 3081–3092. [Google Scholar] [CrossRef]
- Cassano, P.; Caldieraro, M.A.; Norton, R.; Mischoulon, D.; Trinh, N.H.; Nyer, M.; Dording, C.; Hamblin, M.R.; Campbell, B.; Iosifescu, D.V. Reported Side Effects, Weight and Blood Pressure, After Repeated Sessions of Transcranial Photobiomodulation. Photobiomodul. Photomed. Laser Surg. 2019, 37, 651–656. [Google Scholar] [CrossRef]
- Mostafavinia, A.; Bidram, M.; Gomi Avili, A.; Mahmanzar, M.; Karimifard, S.A.; Sajadi, E.; Amini, A.; Hadipour Jahromy, M.; Ghoreishi, S.K.; Chien, S.; et al. An improvement in acute wound healing in rats by the synergistic effect of photobiomodulation and arginine. Lab. Anim. Res. 2019, 35, 28. [Google Scholar] [CrossRef]

| Rad Emission Mode | Model | Wavelength (nm) | Power (mW/cm2) | Energy Density (J/cm2) | Frequency/Time | Effects | Mechanism/Evidences | Study |
|---|---|---|---|---|---|---|---|---|
| Continuous | In rats | 405 | 100 | 54 | Starting from the 1st day, with 48 h intervals for 3 min, 7 replicates | Osteogenesis (+), the least bone formation, no obvious root absorption | The increased intracellular free radicals [43], and inadequate depth penetration | [42,44] |
| 532 | 100 | 54 | Osteogenesis (++), root absorption reduction | The increased RUNX-2 expression [45] | ||||
| 650 | 100 | 54 | Osteogenesis (+++), the maximum distance of OTM, root absorption reduction | Less light energy loss, decreased intracellular free radicals [43], and increased expression of CRY1 | ||||
| 940 | 100 | 54 | Osteogenesis (+++), root absorption reduction | The increased ALP activity, the stimulation of osteoblasts [46], and the CCO of ETC | ||||
| Not specified | In rats | 810 | 100 mW | 75 | Starting from the 1st day, with 48 h intervals for 15 s, 7 replicates | 31–46% increase in the OTM rate, 25–70% reduction in hyalinization areas | Micro-CT analysis, increased RANKL expression and TRAP-positive cells at the compression side, and increased OPG expression at the tension side | [39] |
| Continuous | In rats | 660 | 50 mW | 5 | Irradiation on days 0, 1, 2, 3, 4, 5, and 7 for 50 s | Increased OTM rate (+), bone remodeling (+), osteoclastic activity (++) (More side effects) | 660 nm light increased RANKL, IL-1β expression, and number of TRAP-positive cells than 830 nm | [26] |
| 830 | 50 mW | 5 | The increase in OTM rate (+) and bone remodeling (+) osteoclastic activity (+) | |||||
| Continuous | In rats | 820 | 50 mW | 4.8 | Irradiation with 48 h intervals in 11 days for 12 s (SL) or a further 14 days after appliance removal (LL) | More preventive than preventive effect of PBM therapy on OIIRR | The increased number of osteoblasts, osteoclasts, fibroblasts, and capillary and the lowest RANKL/OPG activity in LL group | [40] |
| Incoherent | In rats | 940 | 16.6 | 4 | Irradiation on days 0, 1, and 2, once daily | OIIRR reduced from 100% to 12.5% at day 7 | The increased expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta (3) integrin | [41] |
| Continuous | In rats | 810 | 100 mW | Not specified | Starting from the 1st day, with 24h intervals in 8 days for 9 min | A 1.5-fold increase in the OTM rate at day 7 | RANK/RANKL expression increase | [47] |
| Incoherent | In rats | 850 | 75 mW | Not specified | Starting from the 1st day, with 24 h intervals in 8 days for 12 min | No obvious difference | Not specified | |
| Continuous | In rats | 830 | 100 mW | 11.8 W/cm2 | Starting from the 1st day, with 24 h intervals in 13 days for 9 min | A 1.3-fold increase in the OTM rate at day 12 | The increased number of TRAP-positive and PCNA-positive cells, the analysis of calcein double staining | [24] |
| Continuous | In rats | 830 | 100 mW | Not specified | Starting from the 1st day, with 24 h intervals in 7 or 14 days for 3 min | A 1.6-fold and a 1.4-fold increase in the OTM rate at day 6 and 14, respectively | The increased OPG, RANKL expression, and account of osteoclasts | [48] |
| Continuous | In diabetic rats | 780 | 70 mW | 35 | Starting from the 1st day, with 48 h intervals for 60 s, 7 replicates | The periodontal damages were reversed partially | The increased number of osteoblasts, osteoclasts, capillary, and collagenization rate | [49] |
| Continuous | In rats | 810 | 100 mW | 75 | Starting from the 1st day, with 48 h intervals for 30 s, 6 replicates | A 1.3-fold increase in the OTM rate at day 14 | Micro-CT and hyalinized tissue in histology analysis | [50] |
| Continuous | In rats | 940 | 100 mW | 45.85 | Starting from the 1st day, with 24 h intervals in 8 days for 6 min | The increase in OTM rate | The stimulation of cell mitochondria and energy cell cycle to increase the expression of RANK, RANKL OPG, RUNX2 | [51] |
| Cells Type | Wavelength (nm) | Power Densities (mW/cm2) | Energy Density (J/cm2) | Time of Laser Applications | Results | Reasons | Study |
|---|---|---|---|---|---|---|---|
| MC3T3-E1 MLOA5 RANKL-treated RAW264.7 | 940 | 1.67 | 1 | 10 min | Enhancing osteoblast proliferation, osteoclast differentiation, and osteoclastic bone resorption activity | High energy density could regulate different cell proliferation and differentiation-related signaling pathways and result in decreased osteocyte and osteoclast activity | [52] |
| 8.33 | 5 | Decreasing viability of osteocytes and osteoclasts | |||||
| 12.5 | 7.5 | Osteoblast viability was negatively impacted | |||||
| hPDLSCs | 1064 | 0.25 W | 2 | Every other day for 20 s | Promoting the proliferation and osteogenesis | The promotion of BMP/Smad signaling | [53] |
| 4 | |||||||
| 6 | |||||||
| 8 | Suppressing osteogenic differentiation | Biphasic dose response | |||||
| hPDLSCs/pPDLSCs | 1064 | 270 | 4 | 15 s | Promoting oxidative stress (hPDLSCs) | CCO photon absorption or the simulation of light/temperature-gated calcium ion channels to increase ATP production | [54] |
| 8 | 30 s | Modulating the osteogenic potential of hPDLSCs, decreasing inflammatory cytokines and ROS levels (pPDLSCs), promoting oxidative stress(hPDLSCs) | |||||
| 16 | 60 s | Suppressing proliferation and osteogenic differentiation, promoting inflammatory cytokines and ROS levels | High energy density could damage cells through heating effects | ||||
| Diabetic-induced wounded fibroblasts | 632.8 | Not Specified | 5 | Every 72 h | Complete wound closure, increased cell viability, and bFGF expression | Not Specified | [55] |
| 830 | 5 | Incomplete wound closure, increased bFGF expression | |||||
| 1064 | 5 | Incomplete closure and increased apoptosis | |||||
| 632.8 | 16 | Incomplete wound closure, increased apoptosis, decreased bFGF expression | |||||
| 830 | 16 | ||||||
| 1064 | 16 |
| Stages | Rad Emission Mode | Model | Wavelength (nm) | Results | Study |
|---|---|---|---|---|---|
| Blood vessels | Continuous/Incoherent | In rats | 820/970 | An increased neovascularization, angiogenic genes, VEGF, and bFGF expression were observed. | [76,77,78,79] |
| Continuous | In rats and hHCC | 635 | The up-regulation of the Src/ERK/STAT3 signaling and thrombopoietin level could be observed. | [80] | |
| Continuous | In rats | 830 | Faster repair of the pulpal tissue could be observed. | [81] | |
| Continuous | In human | 780/1064 | The up-regulation of VEGF expression and a positive linear correlation between the CCO and HbO concentration could be found. | [82,83] | |
| Inflammatory response | Continuous | In hPMN granulocytes and hHCC and hPDLSCs | 635/660/970 | An increased level of ROS, TGF-β, oxidative stress, PGE2, and IL-1β expression could be observed. | [54,80,84,85] |
| Continuous | In human | 810/820/940/980 | An increased IL-1β and decreased PGE2 expression could be observed. | [86,87,88,89,90] | |
| Incoherent | In human gingival fibroblasts | 830/2940 | The COX-2 and PGE2 expression could be elevated in normal cells, while could be inhibited in an inflammatory context. | [91,92] | |
| Continuous | In rats | 810/830 | An increased IL-1, IL-6, COX-2, and PGE2 could be found. | [78,93] | |
| Collagen and fibers | Continuous | In stretched hPDLCs | 830 | PBM therapy could inhibit PA activity to prevent tissue damage. | [94] |
| Continuous | In rats | 660/808/810 | PBM therapy could increase hydroxyproline content, and diminish the activities of the antioxidant enzymes SOD, catalase CAT, lipid, and protein oxidation (carbonyl groups). The up-regulation of RANKL, MMP-13, type I collagen, and elastin expression could also be observed. | [95,96,97] | |
| Incoherent | In H-end endothelial cells and NIH/3T3 fibroblasts | 1064 | The up-regulation of vinculin and type I collagen could be found in endothelial cells and fibroblasts, respectively. | [66] | |
| Continuous | In mouse embryonic fibroblasts and in human dermal fibroblasts | 810/10,600 | NF-κB, Akt, ERK, and JNK signaling were stimulated to up-regulate the expression of the fibrogenic-related gene. | [98,99] | |
| Mineralized tissues | Continuous/Incoherent | In MC3T3-E1 pre-osteoblasts and in Sao-2 | 660/780/1064 | The up-regulation of cell activities, ALP, MMP-2, and BMP-2 expression could be observed. | [100] |
| Continuous | In rats’ osteoclast precursor cells | 810 | An increased expression of RANK and the number of TRAP-positive cells could be observed. | [101] | |
| Continuous | In human Osteoblasts and Mesenchymal Stromal Cells | 808 | Cytoskeletal changes could be induced by PBM therapy to increase osteoblastic mineralization. | [67] | |
| Continuous/Incoherent | In rats | 830/1064 | Granulation, new bone formation, increased bone volume, trabecular thickness, and mineral apposition rate could be observed. | [78,102] | |
| Continuous | In rats | 660/810/830 | An increased expression of IL-1β, RANKL, OPG, MMP-9, MMP-13, alpha (v) beta (3), and TRAP-positive cells could be observed. | [26,47,96,103] | |
| Continuous | In diabetic rats | 780 | A reduced number of osteoclasts and osteoblasts could be partially reversed by PBM therapy and the enhancement of bone remodeling could be found. | [49,104] | |
| Incoherent | In MC3T3-E1 cells | 830 | The expression of IGF-I could be up-regulated by PBM therapy to affect ERK phosphorylation. | [105] | |
| Continuous | In human primary osteoblasts | 660/780 | The phosphorylation of ERK1/2 could be stimulated. | [106] | |
| In rats’ mesenchymal stem cells | 635 | An increased PI3K could regulate Akt signaling after PBM therapy. | [107] | ||
| Continuous | hPDLSCs | 1064 | The BMP/Smad signaling could be stimulated. | [53] | |
| Continuous | In BMSCs | 810 | A decreased CRY1 expression could be found. | [70] | |
| Continuous | In human | 810 | An increased expression of OPG, IL-1β, and RANKL in GCF were observed. | [108] |
| Study | Study Design | Purpose | Irradiation Parameters | Malocclusion Type | Treatment Type | Main Findings |
|---|---|---|---|---|---|---|
| Camacho et al. (2020) [126] | Systematic review | To determine the optimal range of LLLT wavelengths for accelerating orthodontic tooth movement in clinical practice | 780–830 nm | - | - | 780–830 nm wavelengths could shorten orthodontic treatment time by 24% |
| Hasan et al. (2017) [127] | RCT | To assess the efficacy of LLLT in accelerating the orthodontic tooth movement of maxillary incisors with crowding | 830 nm, 8 J/teeth, repeated on days 3, 7, and 14, and then every 15 days starting from the second month | crowded maxillary incisors | Fixed aligners | Lessening the treatment time by 26% |
| Zheng et al. (2021) [108] | RCT | To examine the impact of LLLT on orthodontic tooth movement as well as changes in related cytokines | 810 nm wavelength, 100 mW power output, 6.29 2 J/cm2 energy density | canine retraction | Fixed aligners | The mean retraction velocity increased by 35% |
| Doshi-Mehta et al. (2012) [128] | RCT | To assess the effectiveness of LLLT in reducing the duration of orthodontic treatment and alleviating pain | 810 nm, repeated on days 3, 7, and 14, and then every 15 days starting from the second month | canine retraction | Fixed aligners | Accelerated tooth movement by 30% and significant pain relief |
| Genc et al. (2013) [129] | RCT | To evaluate the effects of LLLT on the rate of orthodontic tooth movement and the concentration of nitric oxide in GCF during orthodontic treatment | Output power of 20 mW and a dose of 0.71 2 J/cm2, applied on day 0, and on the 3rd, 7th, 14th, 21st, and 28th days (10 points per tooth) | canine retraction | Fixed aligners | Significant acceleration of tooth movement |
| Üretürk et al. (2017) [87] | RCT | To investigate the impact of LLLT on tooth movement during canine distalization by assessing the levels of IL-1β and TGF-β1 in GCF | 820 nm, 20 mW, applied on day 0, and on the 3rd, 7th, 14th, 21th, 30th, 33rd, 37th, 60th, 63th, and 67th days | Angle Class II | Brackets and the maxillary molar bands | Nearly 40% acceleration in the speed of orthodontic tooth movement |
| Pérignon et al. (2021) [130] | RCT | To assess the impact of LLLT on tooth movement | 970 nm, 2 s at a power of 0.5 Watts and with an energy of 30 J/cm2. Each exposure point received 0.9 J (three points per tooth, three teeth on one side) | Angle Class II | Brackets and Class II elastics | Significant acceleration in tooth movement |
| Mistry et al. (2020) [131] | RCT | To examine the impact of LLLT on the degree of maxillary canine distalization when administered at 4-week intervals over a period of 12 weeks | 808 nm, treatment carried out on day 0, 28, and 56, with 80 s per tooth | canine retraction | Fixed aligners | No group differences were observed |
| Al-Dboush et al. (2021) [132] | Retrospective study | To evaluate the effectiveness of LIPUS and PBM interventions in accelerating orthodontic tooth movement | 850 nm and intensity of 60 mW/cm2, 10 min per day | Angle Class I, II and III | Invisible removal aligners | PBM therapy showed a 26.6% reduction in treatment duration |
| Caccianiga et al. (2016) [133] | Controlled Clinical Trial | To assess the impact of LLLT on orthodontic treatment utilizing removable clear aligners | Every second week | - | Invisible removal aligners | Reduced wearing time from 20–22 h/day to 12 h/day |
| Costa et al. (2021) [134] | Systematic review and meta-analysis | To evaluate the impact of PBM therapy on the stability of OMI | - | - | Mini-screws | LLLT demonstrates favorable effects on the stability of OMI |
| Zhang et al. (2021) [135] | Systematic review and meta-analysis | To evaluate the impact of PBM therapy on the stability of OMI | - | - | Mini-screws | LLLT demonstrates favorable effects on the stability of OMI |
| Michelogiannakis et al. (2022) [136] | Systematic review and meta-analysis | To evaluate the impact of PBM therapy on the stability of OM | - | - | Mini-screws | The influence of PBM therapy on mini-implant stability remains controversial |
| Ng et al. (2018) [137] | RCT | To examine the impact of LLLT on OIIRR | 808 nm wavelength, 0.18 W power, 1.6 J per point, and duration of 9 s for continuous mode and 4.5 s for pulsed mode. Laser applied on days 0, 1, 2, 3, 7, 14, and 21 | - | OIIRR | Reduced root resorption by nearly 23% |
| Eid et al. (2022) [138] | RCT | To assess the impact of high and low frequencies of LLLT on root resorption | Group A: 980 nm, 100 mW, 8 s, 8 2 J/cm2, applied on days 0, 3, 7, and 14, and every 2 weeks thereafter; Group B: 980 nm, 100 mW, 8 s, 8 J/cm2, applied every 3 weeks | - | OIIRR | PBM therapy does not affect root resorption |
| Goymen et al. (2020) [139] | RCT | To examine the impact of PBM therapy on root resorption | 810 nm, applied at 0, 3, 7, 14, 21, and 28 days to 2 J/cm2 | - | OIIRR | PBM therapy does not affect root resorption |
| Wu et al. (2018) [22] | RCT | To assess the impact of LLLT on pain and somatosensory sensitization induced by orthodontic treatmen | 810 nm, 400 mW, 2 J/cm2, applied at 0 h, 2 h, 24 h, 4 days, and 7 days after treatment | - | Pain relief | PBM therapy exhibits significant analgesic effects |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Liu, Q.; Peng, J.; Song, W.; Zhao, J.; Chen, L. The Effects and Mechanisms of PBM Therapy in Accelerating Orthodontic Tooth Movement. Biomolecules 2023, 13, 1140. https://doi.org/10.3390/biom13071140
Wang X, Liu Q, Peng J, Song W, Zhao J, Chen L. The Effects and Mechanisms of PBM Therapy in Accelerating Orthodontic Tooth Movement. Biomolecules. 2023; 13(7):1140. https://doi.org/10.3390/biom13071140
Chicago/Turabian StyleWang, Xinyuan, Qian Liu, Jinfeng Peng, Wencheng Song, Jiajia Zhao, and Lili Chen. 2023. "The Effects and Mechanisms of PBM Therapy in Accelerating Orthodontic Tooth Movement" Biomolecules 13, no. 7: 1140. https://doi.org/10.3390/biom13071140
APA StyleWang, X., Liu, Q., Peng, J., Song, W., Zhao, J., & Chen, L. (2023). The Effects and Mechanisms of PBM Therapy in Accelerating Orthodontic Tooth Movement. Biomolecules, 13(7), 1140. https://doi.org/10.3390/biom13071140





