Abstract
The prevalence of patients with hyperuricemia or gout is increasing worldwide. Hyperuricemia and gout are primarily attributed to genetic factors, along with lifestyle factors like consuming a purine-rich diet, alcohol and/or fructose intake, and physical activity. While numerous studies have reported various comorbidities linked to hyperuricemia or gout, the range of these associations is extensive. This review article focuses on the relationship between uric acid and thirteen specific domains: transporters, genetic factors, diet, lifestyle, gout, diabetes mellitus, metabolic syndrome, atherosclerosis, hypertension, kidney diseases, cardiovascular diseases, neurological diseases, and malignancies. The present article provides a comprehensive review of recent developments in these areas, compiled by experts from the Young Committee of the Japanese Society of Gout and Uric and Nucleic Acids. The consolidated summary serves to enhance the global comprehension of uric acid-related matters.
1. Introduction
The worldwide prevalence of patients with hyperuricemia or gout is increasing [1,2,3]. Genetic factors are recognized as contributors to hyperuricemia and gout, along with lifestyle factors such as consuming a purine-rich diet, alcohol and/or fructose intake, and physical activity. Hyperuricemia is a well-established causative risk factor for gout flares. Additionally, gout flare is associated with a higher risk of cerebrocardiovascular diseases [4,5]. Therefore, lifestyle modifications are recommended for every individual with hyperuricemia or gout.
The activity of uricase, an enzyme catalyzing the conversion of uric acid to allantoin, was lost about 8–20 million years ago, and therefore, uric acid is the end product of purine metabolism in humans. [6] In addition, the renal tubules reabsorb most uric acid filtered in the glomeruli, resulting in 5 to 10 times higher concentrations of serum uric acid in humans than those in other mammalians. These findings suggest that uric acid was necessary for human evolution. Experimental studies have shown that uric acid is a powerful antioxidant. [7] Uric acid may exert its beneficial effects by protecting cells from oxidative damage by maintaining superoxide dismutase, scavenging radical species, and chelating transition metals. [8,9] However, the worldwide prevalence of patients with hyperuricemia or gout is increasing.
While medical treatment for patients with a history of gout and hyperuricemia is recommended, the landscape for treating asymptomatic hyperuricemia remains intricate and variable, with recommendations differing across countries due to insufficient evidence [10,11,12,13]. Although a standardized international consensus for treating asymptomatic hyperuricemia has not been established yet, a wealth of studies has revealed various comorbidities intertwined with hyperuricemia or gout. This review article focuses on the intricate relationship between uric acid and thirteen specific domains: transporters, genetic factors, diet, lifestyle, gout, diabetes mellitus, metabolic syndrome, atherosclerosis, hypertension, kidney diseases, cardiovascular diseases (CVD), neurological diseases, and malignancies. An overview of this review is shown in Figure 1.
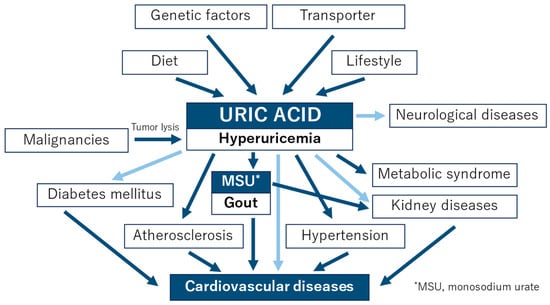
Figure 1.
An overview of this review.
The blue lines indicate a high degree of established relationship, while the light blue lines suggest that the relationship has not yet been clearly established.
A comprehensive review of recent developments in each of these domains has been meticulously compiled by the professional members of the Young Committee of the Japanese Society of Gout and Uric and Nucleic Acids. This summary of evidence will prove instrumental in shaping forthcoming discussions and fostering a deeper understanding of this intricate landscape.
2. Transporters
Because of its lipophobicity, uric acid cannot passively permeate the lipid bilayer. Therefore, it is reasonable to assume that membrane transporters play a pivotal role in regulating serum uric acid levels. Since identifying uric acid transporter-1 (URAT1) as the first transporter involved in uric acid reuptake from urine in 2002 [14], researchers have made great efforts to find transporters regulating uric acid homeostasis. Owing to these efforts, glucose transporter 9 (GLUT9) and ATP-binding cassette transporter G2 (ABCG2) were discovered as physiologically important uric acid reuptake and efflux transporters, respectively. However, these membrane proteins are not enough to explain the whole picture of uric acid regulation in our body; thus, scientists continue their studies to clarify the unknown factors. Considering that URAT1 is the molecular target of uricosuric agents such as benzbromarone and dotinurad, the discovery of novel transporters could lead to the development of a therapeutic strategy for abnormal uric acid homeostasis. This section focuses on recent advances in the attempts to identify novel uric acid transporters (Figure 2).
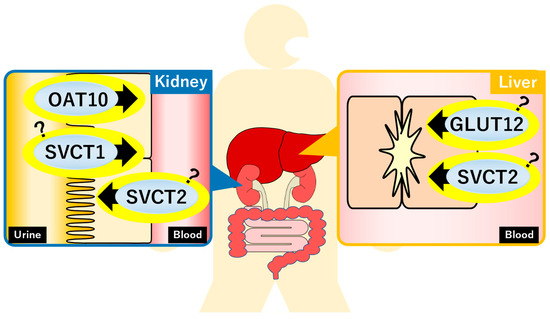
Figure 2.
Recently identified uric acid transporters and their estimated functions. GLUT, glucose transporter; OAT, organic anion transporter; SVCT, sodium-dependent vitamin C transporter.
2.1. Glucose Transporter 12 (GLUT12)
GLUT12 is a member of the glucose transporter family and has been shown to have glucose transport activity in vitro [15]. The relationship between GLUT12 and uric acid was first identified in a genome-wide association study (GWAS) that focused on serum uric acid levels [16]. Based on this GWAS report, Toyoda et al. examined the uric acid transport activity of GLUT12 using in vitro transient overexpression cell systems and confirmed that GLUT12 functions as a uric acid transporter [17]. Furthermore, this study investigated the physiological importance of Glut12 in uric acid homeostasis using a knockout (KO) mouse model. Since mice can metabolize uric acid to allantoin by uricase (Uox), a uric acid metabolizing enzyme, double KO (DKO) mice of Glut12 and Uox genes (Glut12-Uox DKO mice) were established and analyzed. As a result, plasma uric acid levels of Glut12-Uox DKO mice were significantly higher than those of Uox single KO mice. On the other hand, liver uric acid levels and the ratio of liver to plasma uric acid levels were lower in Glut12-Uox DKO mice, suggesting the role of Glut12 in transporting uric acid from plasma to the liver. Given that GLUT12 was identified in a GWAS of serum uric acid levels, it appears that GLUT12 would also be a physiologically important uric acid transporter in humans.
2.2. Organic Anion Transporter 10 (OAT10)
OATs are involved in the transmembrane transport of organic anions and belong to a wide range of transporter families, including organic cation transporters and organic cation/carnitine transporters, alongside the well-known uric acid transporter URAT1. Although the uric acid transport activities of OAT10 were reported in in vitro studies [18], its physiological importance in uric acid homeostasis had not been reported for a decade. This was mainly because mutations in the OAT10 gene were rare in individuals other than Japanese, preventing the detection of this gene in GWAS. Recently, to clarify the roles of OAT10 in uric acid homeostasis, comprehensive exon sequencing analyses were conducted in Japanese gout patients and healthy controls [19]. This study revealed that the allele frequency of missense mutation in the OAT10 gene, 1129C > T, which induces the amino acid substitution Arg377Cys (R377C), was lower in gout patients. In vitro functional analyses demonstrated that the OAT10 R377C mutant had no uric acid transport activity. A subsequent study revealed that the fractional excretion of uric acid to urine (FEUA) was significantly high in people with the OAT10 R377C mutation [20]. Combining the genetic and in vitro analyses, OAT10 was identified as a uric acid reabsorption transporter from urine. Interestingly, some uricosuric agents inhibited the uric acid transport activity of OAT10 in vitro, suggesting the potential of OAT10 as a molecular target of hyperuricemia [20].
2.3. Sodium-Dependent Vitamin C Transporter 1/2 (SVCT1/SVCT2)
SVCTs are human homologs of the nucleobase–ascorbate transporter (NAT) family. It is well known that SVCT1/SVCT2 transport vitamin C (VC) in a sodium-dependent manner. Analyses of Svct1 KO mice revealed the involvement of Svct1 in the reuptake of VC from urine and the regulation of plasma VC levels [21]. In contrast, Svct2 is considered to regulate VC levels in various tissues, such as the liver and kidney, although Svct2 KO mice die soon after birth [22]. Based on a report demonstrating that the bacterial NAT family transporter YgfU transported uric acid, investigations into the uric acid transport activities of SVCT1/SVCT2 were conducted using in vitro transient overexpression cell systems [23,24]. As a result, it was clarified that both SVCT1 and SVCT2 transport not only VC but also uric acid in a sodium-dependent manner. In mouse models, Svct1 was suggested to regulate serum uric acid levels as a uric acid reabsorption transporter from urine [23]. However, due to lethality, there are no reports investigating changes in uric acid homeostasis in Svct2 KO mice. Future studies are needed to reveal the physiological importance of SVCT1/SVCT2 in uric acid homeostasis in humans.
3. Genetic Factors
Mendelian randomization analyses have provided evidence that genes responsible for hyperuricemia are not independently associated with hypertension, ischemic heart disease, type 2 diabetes, cerebrovascular disease, or heart failure [25,26,27]. These findings suggest that the genes responsible for uric acid regulation, specifically those encoding uric acid transporters, may not directly act as independent risk factors for these health issues. However, it is worth emphasizing that not all genetic factors related to hyperuricemia exert the same influence. Some studies have indicated a positive association between the xanthine oxidoreductase (XOR) gene and blood pressure, hinting at the possible involvement of XOR and oxidative stress in influencing blood pressure levels [28,29]. Additionally, evidence shows a connection between serum uric acid levels and a genetic risk score based on eight uric acid-regulating single nucleotide polymorphisms associated with cardiovascular death and sudden cardiac death [30]. Moreover, Mendelian randomization research using data from UK Biobank and clinical trials has suggested that higher serum uric acid levels may indeed contribute to increased blood pressure, potentially mediating an increased risk of CVD [31].
Uric acid levels are regulated by both uric acid transporters and XOR, which play roles in its accumulation and production. Importantly, while most studies of the uric acid transporter gene were negative, most studies exploring gene regulation of XOR have been positive. In addition, it is crucial to recognize that hyperuricemia is influenced not only by genetic predisposition but also by lifestyle factors, including diet, alcohol and fructose intake, and physical activity. Dietary habits have rapidly changed in the last 100 years, and these acquired factors possibly affect CVD [32]. Therefore, when assessing the risk of CVD related to uric acid levels, we must consider both genetic and acquired factors, taking a comprehensive approach to understand their interplay.
4. Diet
Hyperuricemia is a lifestyle-related disease; hence, advising patients to modify their lifestyle is important, regardless of pharmacotherapy. A healthy diet tailored to each individual according to lifestyle and coexisting diseases must be chosen rather than relying solely on a low-purine diet alone. Long-term adherence is important for improving overall health, managing metabolic comorbidities, and preventing and managing conditions such as hyperuricemia or gout.
Healthy diets, such as dietary approaches to stop hypertension (DASH) and Mediterranean diets, have been reported to reduce serum uric acid levels and gout incidences [33]. Studies suggest that a healthy diet combined with weight loss in overweight or obese individuals significantly reduces cardiometabolic risk factors, including blood pressure, cholesterol profile, triglycerides, and insulin resistance, and improves gout outcomes. Consumption of certain dietary risk factors (e.g., alcohol, sugar-sweetened beverages, and red meat) and adherence to a healthy diet are associated with serum uric acid levels and the prevalence of gout; however, it has been shown that these have minimal effects compared to genetic variation [34,35]. Only recently was the interaction between DASH diet adherence and gout risk in women found to have a significant additive gene–diet interaction [36]. Shirai et al. reported that habitual coffee consumption reduced gout risk without altering serum uric acid levels [37] like anti-inflammatory therapy. Similarly, a healthy diet may also have anti-inflammatory effects.
Conversely, the impact of short-term dietary factors such as consuming purine-rich foods and alcohol on gout flare-ups must be heeded. However, the idea of restricting protein consumption to reduce purine load is not accurate. Kaneko et al. reported on purines in foodstuffs [38]; based on the reported values obtained by calculating the optimal energy intake (1800 kcal) and macronutrient energy distribution for 28 days in a hospital diet, the purine quantity is approximately 190–600 mg/day, with a confirmed average value of approximately 380 mg/day. However, it is slightly high at 600 mg/day for a menu including fish such as cutlass [39]. Significant deviation from the recommended quantities is unlikely during energy intake optimization, even if high-purine foods are incorporated throughout a daily diet.
Purine nucleotides are also umami components. Using nucleotide umami substances, such as guanosine 5’-monophosphate and inosine 5’-monophosphate, in combination with monosodium glutamate, has been reported to reduce salt intake without impairing taste [40]. Furthermore, the intestinal epithelium has a high demand for nucleotides for energy acquisition, proliferation, and innate immunity, and the significant increase in nucleotide substrate requirement during injury, infection, and wound healing is well known. It has been recently reported that gut microbiota can utilize multiple purines, including uric acid, as carbon and energy sources and can act as the major source of purines used for nucleotide production by the intestinal mucosa [41]. Various lactic acid strains and other bacteria have been proven to lower serum uric acid levels and improve gout flare-ups in human trials [42]. Gut microbiota changes associated with dietary changes may improve host uric acid metabolism; hence, future research on these aspects is awaited.
5. Lifestyle (Children and Adults)
Hyperuricemia is associated with obesity and lifestyle diseases in adults. Gout, the most common presentation of hyperuricemia in adults, is rare in children, and most children with gout have some underlying disease such as Down syndrome, renal hypoplasia, atrial septal defect, glycogen storage disease, leukemia, and methylmalonic acidemia [43]. Therefore, abnormal serum uric acid concentration in children is considered a biochemical disorder with no clinical significance. However, recent evidence has suggested that hyperuricemia in children is an important lifestyle-related clinical problem [44,45,46,47,48]. Some recent topics of uric acid research related to lifestyle are introduced below.
Hyperuricemia in children is associated with obesity, metabolic syndrome, and its components of metabolic syndrome [43]. Because serum uric acid concentrations change with growth in children, with differences between males and females appearing around 10 years of age [44], it is important to establish age- and sex-specific pediatric reference values when defining hyperuricemia in children. In a recent large-scale population-based study of Japanese children aged 9–10, hyperuricemia was found to be associated with obesity, high hemoglobin A1c (HbA1c) levels, dyslipidemia (hypertriglyceridemia and hypo high-density lipoprotein (HDL)-cholesterolemia), and liver damage [44]. In this study, factors associated with hyperuricemia in children were more accurately assessed by focusing on a limited age group. Non-alcoholic fatty liver disease (NAFLD) [45] and non-alcoholic steatohepatitis [46], the main causes of liver injury in children, are associated with elevated uric acid levels. Longitudinal studies have shown that hyperuricemia is a risk factor for the future development of hypertension [47] and chronic kidney disease (CKD) [48].
Because younger patients have fewer complications, studies in those patients with hyperuricemia are reasonable. Further, longitudinal studies are needed to determine the long-term prognosis of patients with hyperuricemia and the effectiveness of interventions.
In adults, lifestyle habits that prevent hyperuricemia include exercise, smoking cessation, and work participation. According to the 2021EULAR guidelines [49], people with rheumatic and musculoskeletal diseases that include hyperuricemia should avoid physical inactivity; they should engage in regular exercise according to their abilities. People with hyperuricemia should be encouraged to stop smoking and be informed that smoking is detrimental to symptoms, function, disease activity, disease progression, and the occurrence of comorbidities. Work participation may have beneficial effects on health outcomes of people with hyperuricemia. However, the relationship between exercise habits and hyperuricemia disappeared when the body mass index (BMI) was adjusted in the model, indicating that the exercise effect was entirely mediated through BMI [35,50]. Conversely, in two population-based cross-sectional studies [51,52], levels of physical activity and sedentary behavior were significantly associated with hyperuricemia status, even with adjustment for BMI. The important thing to remember is that lifestyle improvements complement medical treatment and do not replace it, and their effects cannot be expected without correcting obesity.
Additionally, a recent topic is the relationship between taste (umami) and hyperuricemia. Umami is one of the five basic tastes and is the sense that detects whether a food contains protein. Foods rich in purines often present an umami taste. Monosodium glutamate (MSG), one of the umami flavors, may directly induce obesity and metabolic syndrome through the formation of uric acid as well as fructose metabolism [53]. Thus, further research is needed to determine how purine-rich umami foods affect hyperuricemia [54].
6. Gout
Gout, distinguished by acute episodes of joint inflammation, occurs when there is an increase in serum uric acid levels of more than 7 mg/dL (420 µmol/L), contributing to the formation of deposits of monosodium urate (MSU), a tiny needle-shaped crystalline formation of uric acid [55]. Mendelian randomization studies suggest convincing evidence of an association with hyperuricemia exists for gout [56].
Gout can be a risk factor for CVD. A study showed that the risk for myocardial infarction and stroke in patients with gout was elevated 1.82 and 1.71 times, respectively, compared to those without gout [57]. Some studies have reported that CVD risk increases within 120 days, especially during the first 30 days following an acute gout flare [58,59]. Therefore, preventive medicine and gout management could be effective for both acute gout flare and CVD prevention.
Regarding the guidelines for gout management, they vary depending on the country. The 2020 American College of Rheumatology Guideline for the Management of Gout (ACR2020) recommends pharmacological treatment of hyperuricemia, uric acid-lowering treatment (ULT), for all patients with tophaceous gout or frequent gout flares with serum uric acid target levels of ≤5.0 mg/dL. It does not recommend treatment for patients without gout, even those with CVD risks [11]. In contrast, the Japanese Guideline on Management of Hyperuricemia and Gout (JGMHG) recommends lowering serum uric acid levels to ≤6 mg/dL and recommends pharmacological treatment for hyperuricemic patients (serum uric acid levels ≥ 8 mg/dL) with CKD and CVD risk and for hyperuricemic patients (serum uric acid levels ≥ 9 mg/dL) without CKD and CVD risk [12,60]. A recent retrospective cohort study using the JMDC Claims Database showed that occurrences of gout flare for both gout and asymptomatic hyperuricemia in patients who achieved serum uric acid levels ≤ 6.0 mg/dL with ULT decreased compared to patients whose serum uric acid levels remained >6.0 mg/dL or who were not receiving ULT [61]. Additionally, based on a meta-analysis of studies, a longer duration of ULT with achieving serum uric acid levels < 6 mg/dL was associated with reduced gout flares [62]. These studies provide evidence of serum uric acid levels ≤ 5.0 or 6.0 mg/dL as a treatment target for patients with gout and asymptomatic hyperuricemia.
From another perspective, MSU can be a better surrogate marker of gout flares. As a pathophysiology of gout flare, a previous prospective observational study found that an increase in MSU volume measured with dual-energy computed tomography was associated with a higher risk for gout flares [63]. In a prospective study examining the impact of ULT on MSU deposits in gout patients, the burden of MSU deposits significantly decreased over an average of 18 months of follow-up in patients undergoing lifestyle intervention and treated with allopurinol or febuxostat [64]. A change in MSU volume was significantly but weakly associated with a change in serum uric acid levels. No significant decline in MSU deposits was observed in patients who discontinued treatment. Recent research has shown that over a third of gout patients stop taking their ULT [65]. Allopurinol interrupters and discontinuers had indicators of more severe gout over time compared to adherers. These data indicate that the crucial aspects of gout management are continuing ULT and monitoring MSU deposits as a possible surrogate marker. Further research focusing on MSU deposits is required.
7. Diabetes Mellitus (Glucose Metabolism)
Serum uric acid levels are known to be influenced by the presence of diabetes mellitus and other lifestyle-related diseases. Epidemiological evidence to date indicates that type 2 diabetes mellitus is associated with gout [66]. On the other hand, it is also known that serum uric acid levels are not high in hyperglycemic conditions. According to past papers, both uric acid levels and the rate of hyperuricemia increase with increasing HbA1c levels but conversely decrease when HbA1c exceeds 6.0 to 6.9, indicating a bell-shaped relation due to the uricosuric effect of glucosuria [67]. The association between diabetes mellitus and serum uric acid levels is one of the most interesting topics.
Recently, Lee KW and Shin D reported that elevated serum uric acid levels may exacerbate the development of risk of type 2 diabetes mellitus in the Korean Genome and Epidemiology Study [68]. A total of 4152 Korean adults aged 45–76 years without type 2 diabetes mellitus, cancer, or gout at baseline in 2007–2008 were followed up until 2016. In this study, they reported that high levels of serum uric acid and high-sensitivity C-reactive protein (hsCRP) in combination were also associated with an increased incidence of type 2 diabetes mellitus compared to low levels of serum uric acid and hsCRP.
Jiahao Zhu et al. investigated bidirectional associations of type 2 diabetes mellitus and glycemic traits with plasma serum uric acid levels using a Mendelian randomization approach [69]. The associations of type 2 diabetes mellitus and fasting insulin with serum uric acid levels were shown. In addition, Xueting Hu et al. investigated the association between elevated plasma uric acid levels and a higher risk of insulin resistance in newly diagnosed type 2 diabetes through Mendelian randomization analysis. However, there was no strong association between uric acid and insulin resistance in this study [70].
On the other hand, the relationship between serum uric acid level and sodium–glucose cotransporter-2 (SGLT-2) inhibitors has also been attracting attention. Regardless of its precise mechanism, it has been known for a while that SGLT-2 inhibitors could significantly reduce serum uric acid levels in patients with type 2 diabetes mellitus6. Recently, Banerjee M et al. reported that SGLT2 inhibitors significantly reduced the risk of gout in individuals with type 2 diabetes mellitus and/or heart failure (HF) using data from five randomized controlled trials (RCTs) [71].
8. Metabolic Syndrome
Hyperuricemia is known to be associated with metabolic syndromes such as obesity, insulin resistance, and dyslipidemia. However, the causal relationship between uric acid and these metabolic syndromes remains unclear. The following studies have recently been reported and are expected to clarify the causal relationship between uric acid and metabolic syndrome in the future.
The relationship between hyperuricemia and dyslipidemia has long been recognized [72]. A recent longitudinal cohort study showed that triglyceride and HDL cholesterol levels and dyslipidemia were significantly associated with the development of hyperuricemia [73]. On the other hand, hyperuricemia is known to be associated with dyslipidemia [74], although a meta-analysis reported that treatment with allopurinol for 4 to 24 weeks did not significantly reduce serum triglyceride and low-density lipoprotein cholesterol levels [75]. Further studies, including long-term intervention trials, are needed to clarify the causal relationship between uric acid and dyslipidemia.
Although hyperuricemia is associated with the risk of NAFLD in a systematic review and meta-analysis [76], it remains unclear whether there is a bidirectional or temporal relationship between it and NAFLD. Using logistic regression and cross-lagged panel analysis, Zhimin Ma and colleagues showed a unidirectional relationship from hyperuricemia to NAFLD incidence [77]. This study suggests that hyperuricemia plays a fundamental role in the development of NAFLD. However, the effect of ULT on NAFLD has not been fully investigated [78]. Whether hyperuricemia is a therapeutic target for preventing the onset and progression of NAFLD needs to be investigated.
A meta-analysis of bariatric surgery showed that serum uric acid levels decreased from three months after surgery and persisted until the third year after surgery, as well as a reduction in the incidence of gout attacks. However, serum uric acid levels increased one month after surgery [79]. In addition, weight loss after bariatric surgery is associated with reduced serum uric acid levels. Bariatric surgery may be an important treatment option in preventing and managing hyperuricemia or gout.
An association between metabolism and XOR, a rate-limiting enzyme involved in the production of not only uric acid but also reactive oxygen species (ROS), has been reported [80]. Plasma XOR activity, determined via liquid chromatography/triple quadrupole mass spectrometry using radio-labeled xanthine, is associated with insulin resistance and glycemic control status [81]. Since plasma XOR activity has been reported to be associated with serum uric acid levels [82], the involvement of XOR activity should also be taken into account when considering uric acid and metabolic syndrome.
In experimental and clinical studies, the administration of benzbromarone, a non-selective inhibitor of URAT1, has been reported to increase adiponectin levels and improve insulin resistance [83,84]. Dotinurad, a URAT1 selective inhibitor, has been shown to ameliorate insulin resistance by attenuating hepatic steatosis and promoting brown adipose tissue re-browning in mice [85]. Further studies in humans are needed to clarify the effects of dotinurad on metabolism, including insulin resistance.
9. Atherosclerosis
Serum uric acid levels tend to be elevated by the presence of hypertension, CKD, and metabolic syndrome, all of which are established risk factors for atherosclerosis. Therefore, serum uric acid levels can be used as a useful biomarker for atherosclerosis. However, it remains a matter of debate whether hyperuricemia per se is an independent causal risk factor for atherosclerosis, such as endothelial dysfunction and arterial stiffening. Experimental studies have shown that hyperuricemia causes oxidative stress, inflammation, and dephosphorylation of endothelial nitric oxide synthase, which can lead to the progression of atherosclerosis and vascular dysfunction [86]. Indeed, observational clinical studies have shown that hyperuricemia is independently associated with the progression of atherosclerosis [87,88]. These findings indicate the possibility that hyperuricemia could be a causal risk factor for atherosclerosis. However, it has not been determined whether ULT inhibits the progression of atherosclerosis and deterioration of vascular function.
Allopurinol reduced the carotid intima-media thickness (CIMT) in hyperuricemic patients with type 2 diabetes [89] and recent ischemic stroke [90]. Meanwhile, in the recent PRIZE (program of vascular evaluation under uric acid control by xanthine oxidase inhibitor, febuxostat: multicenter, randomized controlled) study [91], 24 months of febuxostat, compared to non-pharmacological lifestyle modification care for hyperuricemia, did not delay the progression of CIMT in Japanese patients with asymptomatic hyperuricemia. Interestingly, in a sub-analysis of the PRIZE study, a greater reduction in serum uric acid was associated with an attenuation of CIMT progression, although no optimal target serum uric acid level to delay CIMT progression was observed [92].
Regarding the effects on vascular functional parameters, febuxostat did not change endothelial function as assessed by flow-mediated vasodilation [93], while the therapy modestly improved arterial stiffness markers involving pulse wave velocity (PWV) and the cardio-ankle vascular index (CAVI) [94]. A meta-analysis demonstrated that allopurinol did not affect arterial stiffness as assessed by PWV [95]. In addition, neither febuxostat nor topiroxostat had any obvious effects on arterial stiffness markers (PWV and CAVI) in patients with hypertension and treated hypertension [96]. Whether these conflicts about the effects of XOR inhibitors on atherosclerosis and vascular functional markers depend on the differences in the study design, population, or drug remains uncertain. Finally, since little clinical evidence on the effects of uricosuric agents, such as benzbromarone, on those markers is currently available, further research is required to assess this issue.
10. Hypertension
Epidemiological studies have suggested a significant association between elevated serum uric acid levels and hypertension. In several RCTs, uric acid-lowering medicine, including XOR inhibitors, showed a beneficial effect on blood pressure (BP), although some intervention studies reported no effect on BP. Therefore, some recent topics of uric acid research would be helpful to understand the relationship of serum uric acid with hypertension better, as follows.
First, numerous epidemiological studies have shown that higher serum uric acid levels predicted incident hypertension [97]. Serum XOR level was also associated with higher BP through generating ROS in cross-sectional studies [98]. Second, Feig DI et al. suggested that allopurinol reduced BP by both lowering systemic vascular resistance and plasma renin activity compared to placebo as the first intervention study of the effect of XOR inhibitor on BP [99]. A recent systematic review also suggested that allopurinol revealed a greater reduction of both systolic BP and diastolic BP [100]. Conversely, the FEATHER study (Febuxostat Versus Placebo Randomized Controlled Trial Regarding Reduced Renal Function in Patients with Hyperuricemia Complicated by Chronic Kidney Disease Stage 3) showed that febuxostat decreased BP, but there was no difference in BP reduction compared to placebo [101].
There are some points to be discussed in serum uric acid-hypertension association, which can explain the inconsistent study results of the above studies. First, a vast number of metabolic confounders are involved in uric acid research. For example, the serum uric acid-hypertension association varies depending on age, and it was stronger in children with few confounders [102]. Moreover, recent cross-lagged and mediation analyses revealed the role of BP on the association of serum uric acid with other diseases. Tian X et al. suggested that serum uric acid can elevate both systolic and diastolic BP, which partially facilitated the effect of serum uric acid on incident CVD (mediation effect: 57.6% for systolic BP and 46.3% for diastolic BP) [103]. Mendelian randomization mediation analysis in UK Biobank also supports the idea that higher BP mediates approximately one-third of the effect of serum uric acid on CVD risk [31]. These results may help us to elucidate the complicated network of serum uric acid and other confounders and estimate the effect of lowering BP on CVD prevention. Second, uric acid extracellularly acts as a strong antioxidant but intracellularly shows pro-inflammatory effects [104]. Intracellular uric acid, which is influenced by food very much, is more important in terms of an increased risk for vascular disease; however, it remains to be elucidated how uric acid-lowering medicines, including XOR inhibitors, affect extracellular and intracellular uric acid levels, respectively. Third, serum uric acid levels are also regulated by uric acid excretion. A retrospective study of 84 patients (mean age: 64 ± 16 years) suggested that systolic BP significantly decreased at 3 months after the start of dotinurad compared to baseline. The authors concluded that dotinurad could reduce systolic BP by possibly a relative inhibition of glucose transporter 9 (GLUT9) [105]. On the other hand, pegloticase, a recombinant uricase, significantly reduced mean arterial pressure for 6 months in patients with chronic gout, independent of changes in renal function [106]. The beneficial effect of uric acid-lowering medicines on BP may depend on how they work in the process of uric acid regulation.
Many epidemiological studies support the significant relationship between serum uric acid and hypertension. However, further RCTs are needed to clarify how its association varies depending on age, confounders or mediators, uric acid distribution, and regulation for an appropriate strategy to manage CVD risk.
Hypertensive Disorders of Pregnancy
Hypertensive disorders of pregnancy (HDP) are defined as hypertension in pregnant women, which is classified according to the timing of hypertension diagnosis and the presence or absence of clinical findings such as proteinuria and organ damage as follows: chronic hypertension; white coat hypertension; masked hypertension; gestational hypertension; and pre-eclampsia (de novo and superimposed on chronic hypertension) [107]. It is very important to distinguish pre-eclampsia from other types of HDP in clinical practice despite all types of HDP being high-risk pregnancies [108].
Previous studies have indicated an association between uric acid and pre-eclampsia [109], and measurement of serum uric acid is recommended in patients with HDP by European and American guidelines [110,111]: Elevated uric acid levels occur in pregnancies with pre-eclampsia compared to normal pregnancies [112,113]. Several mechanisms of elevated uric acid levels in pre-eclampsia have been reported [109]. Firstly, vasoconstrictors such as angiotensin II reduce renal blood flow, leading to decreased uric acid excretion. Secondly, hypoxia associated with placental insufficiency increases ROS and oxidative stress, resulting in increased uric acid production and decreased uric acid excretion. In contrast, some studies have reported that elevated serum uric acid levels indicate the severity of the disease process in pre-eclampsia [109], and the ratio of serum uric acid to creatinine is associated with the development of pre-eclampsia and adverse pregnancy outcomes [114]. Furthermore, an observational cohort study revealed that the development of pre-eclampsia is associated with elevated serum uric acid levels before 20 weeks of gestation, especially during the early 8–12 weeks, and the effect diminishes with increasing gestational weeks, suggesting that elevated serum uric acid in early pregnancy may be a potential causative role in pre-eclampsia [115]. However, it is not yet clear whether uric acid is merely a risk marker or a cause that contributes to the progression of pre-eclampsia pathology, and future investigation is needed.
Women who have experienced HDP suffer higher rates of CVD events, including heart failure, coronary artery disease, and stroke [116]. Additionally, the offspring of women with hypertensive pregnancy are more likely to suffer from CVD [117]. Uric acid may play an important role in the link between HDP and the subsequent development of CVD in both mother and child.
11. Kidney Diseases
The kidney plays a crucial role in regulating serum uric acid levels, accounting for 60–70% of uric acid excretion. Normally, the kidney reabsorbs approximately 90% of the uric acid filtered by the glomerulus in the proximal tubules [118]. Gout is present in one-third of patients with CKD, and a “gouty nephropathy” resulting from MSU deposits could be a significant cause of CKD [119]. A study reported that patients with gout are 29 percent more likely to suffer from advanced CKD and more than 200 percent more likely to have kidney failure [120]. Additionally, another study noted that patients with severe gout exhibited a diffuse hyperechoic kidney medulla pattern [121]. Therefore, gout serves as a warning sign for CKD or indicates a higher risk for kidney disease. However, the precise role of uric acid in CKD has not been completely determined. Hyperuricemia is associated with hypertension and aging and with renal atherosclerosis in patients with CKD, according to a cross-sectional analysis [122]. Although many epidemiologic studies have reported that elevated serum uric acid is a predictor of the development of CKD, the causal relationship remains controversial. The relationship between hyperuricemia and kidney disease was described by the International Kidney Disease (KDIGO) in its 2012 “CKD Guidelines” [123]. Although the guidelines indicate the importance of managing hyperuricemia in CKD, the evidence for the use of uric acid-lowering agents for renal protection in CKD without gout is insufficient and not recommended. In 2015, an RCT of patients with CKD stage G3–4 and asymptomatic hyperuricemia showed that 6 months of febuxostat treatment reduced renal dysfunction compared to placebo [124]. In 2018, the results of two RCTs of febuxostat and topiroxostat for hyperuricemia were reported [101,125]. In the FEATHER study of CKD stage G3 patients with asymptomatic hyperuricemia, febuxostat treatment in the setting of adequate CKD treatment showed no significant effect in preventing renal dysfunction [101]. However, a post-hoc analysis of the FEATHER study reported a significantly higher mean estimated glomerular filtration rate (eGFR) slope in the febuxostat group than in the placebo group in CKD patients without proteinuria [126]. In the UPWARD study of diabetic nephropathy patients with hyperuricemia (with/without gout), ULT with topiroxostat significantly reduced eGFR decline compared to placebo, although there was no significant difference in albuminuria [125]. In 2019, the FREED (Febuxostat for Cerebral and CaRdiorenovascular Events PrEvEntion StuDy) showed a significant reduction in renal dysfunction, including proteinuria, in the febuxostat treatment group [127]. The PERL (Preventing Early Renal Loss in Diabetes) study and CKD-FIX (Controlled Trial of Slowing of Kidney Disease Progression from the Inhibition of Xanthine Oxidase) showed that allopurinol-assisted ULT did not slow the decline in eGFR compared with placebo [128,129]. However, it is important to note that both the PERL and CKD-FIX included a large number of participants with normal uric acid levels. In this regard, it is important to note that lowering uric acid levels in normouricemic patients should not be included in clinical trials investigating the effects of hyperuricemia in CKD, as normouricemia is not associated with CKD progression. A meta-analysis including these RCTs was reported in 2020 and found that ULT did not reduce renal failure events (such as a 30% decline in eGFR during follow-up, doubling of serum creatinine levels, and renal failure) but reduced GFR decline (weighted mean difference, 1.18 mL/min/1.73 m2/year; 95% confidence interval, 0.44–1.91) [130]. Taken together, these results suggest that ULT is probably not indicated for all patients with CKD and that future clinical trials should be conducted in specific subgroups, such as younger patients and those with nephrosclerosis and hyperuricemia.
12. Cardiovascular Diseases (CVD)
Uric acid is an end-product of purine metabolism in humans that is mainly regulated through the XOR pathway [131]. The activation of the XOR pathway generates oxidative stress and uric acid, causing vascular inflammation, which may play a role in developing CVD (Figure 3) [132]. Ample evidence has suggested that there is a plausible link between hyperuricemia and/or gout and worsening prognosis in patients with overt CVD [132]. This chapter will summarize the recent studies that have highlighted the clinical significance of hyperuricemia/gout, particularly in the fields of HF, ischemic heart disease (IHD), and arrhythmia.
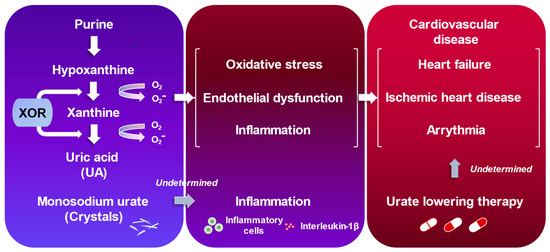
Figure 3.
Uric acid and cardiovascular diseases.
12.1. Heart Failure
HF patients are more likely to associate hyperuricemia [133]. Additionally, there has been evidence that hyperuricemia is associated with an increased risk of incident HF and adverse outcomes [134]. However, the guidelines currently do not recommend ULT to improve the prognosis in patients with hyperuricemia and HF. As shown before, although it is possible that XOR inhibition may have clinical benefits in patients with symptomatic HF [132], previous prospective interventional studies with XOR inhibitors have not yet reported an improvement in HF outcomes. For instance, one of the XOR inhibitors, oxypurinol, did not improve clinical outcomes in unselected patients with moderate-to-severe HF in the OPT-CHF (The Efficacy and Safety Study of Oxypurinol Added to Standard Therapy in the Patients With New York Heart Association Class III-IV Congestive Heart Failure) study [135]. Contrary to the result, post-hoc analysis revealed that high serum uric acid (≥9.5 mg/dL) received improvement in clinical status by taking oxypurinol compared with placebo [135]. Another XOR inhibitor, allopurinol, failed to improve clinical status in patients with HF with reduced ejection fraction (≤40%) and elevated serum uric acid levels (≥9.5 mg/dL) in the EXACT-HF (the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients) trial [136]. A systematic review and meta-analysis regarding the effect of ULT on patients with HF did not reveal any improvement in ejection fraction, B-type natriuretic peptide, 6 min walk test, all-cause mortality, and CVD death with ULT compared with placebo [137].
Thus, the efficacy of ULT in HF patients has not been previously determined, although the results of the FAST (Febuxostat versus Allopurinol Streamlined Trial) showed the possibility that febuxostat could have favorable effects for HF compared to allopurinol [138]. The LEAF-CHF (Effect of Urate-LowEring Agent Febuxostat in Chronic Heart Failure Patients with Hyperuricemia) study, which evaluates the improvement of plasma B-type natriuretic peptide using febuxostat in chronic HF patients with reduced ejection fraction and hyperuricemia, is currently in progress [139]. Clinical evidence needs to be established.
12.2. Ischemic Heart Disease
Albeit with the excellent predictive value of hyperuricemia for patients with IHD [140], whether or not ULT allows CVD risk reduction for this population remains an open question. It has been reported that high-dose allopurinol (600 mg/day) exerts beneficial effects on exercise tolerance in patients with stable chronic angina pectoris [141]. Indeed, allopurinol significantly increased total exercise time and the time to chest pain from a baseline when compared to placebo [141]. Most recently, the ALL-HEART study was conducted to determine whether ULT with allopurinol improves major CVD outcomes in patients with IHD [142]. The ALL-HEART study enrolled 5721 patients aged 60 years or older with IHD, irrespective of serum uric acid levels. While allopurinol (600 mg/day) profoundly decreased serum uric acid levels (from 0.34 mmol/L to 0.18 mmol/L), there was no difference in major CVD outcomes between the allopurinol group and the usual care group [142]. One of the major criticisms was that the ALL-HEART study did not include patients with a history of gout. In this regard, a retrospective observational study has underlined that preceding gout flare was more prevalent in patients who experienced a CVD event as compared with those who did not experience it [58].
MSU is frequently observed in synovial fluid of gout patients. MSU exacerbates gout-associated inflammation through inflammasome activation and interleukin-1β secretion (Figure 2) [143]. A recent study reported that dual-energy computed tomography makes it possible to identify MSU depositions in human aorta and coronary arteries in vivo [144]. Future studies with a novel imaging approach can be encompassed to explore the role of MSU in living patients.
12.3. Arrhythmia
In 2010, the first association between hyperuricemia and atrial fibrillation (AF), one of the most common and clinically important arrhythmias, was reported [145]. Subsequent studies have consistently validated this association, particularly in the incidence of new-onset AF [146,147,148]. A recent comprehensive meta-analysis involving 608,810 participants from 11 studies confirmed the increased risk of incident AF in individuals with hyperuricemia (risk ratio, 2.42; 95% confidence interval (CI), 1.24–3.03) across countries [149]. Moreover, serum uric acid concentrations also serve as a valuable marker for AF recurrence following AF catheter ablation [150]. Another meta-analysis involving 2046 patients from 14 studies demonstrated that individuals who experienced AF recurrence had a higher serum uric acid level compared to those who did not experience it (weighted mean difference, 0.69 mg/dL; 95% CI, 0.46–0.91) [151]. Furthermore, elevated serum uric acid was significantly associated with a higher AF recurrence rate after AF catheter ablation (odds ratio, 2.21; 95% CI, 1.73–2.83) [151]. These collective findings highlight the potential of elevated serum uric acid as a useful tool for stratifying risk in both new-onset AF and AF recurrence post-catheter ablation.
While investigations remain limited, some studies have reported associations between serum uric acid and other types of arrhythmic disorders, including ventricular arrhythmias [152] and atrioventricular block [153]. Such associations necessitate more robust and extensive validation through further research. A recent Mendelian randomization study supports the causal relationship between elevated serum uric acid and increased risk of CVD death, especially sudden cardiac death [30]. This finding is congruent with several prior studies examining patients with different backgrounds [152].
Despite these connections, it is critical to acknowledge the existence of conflicting evidence surrounding the potential benefits of ULT in the reduction of arrhythmias [154,155]. Further research is imperative to ascertain the effectiveness and usefulness of ULT definitively. In summary, while serum uric acid has been recognized as a significant indicator for AF and other arrhythmias, the therapeutic potential of ULT warrants further and detailed exploration.
13. Neurological Diseases
The effects of uric acid in neurological diseases are likely to vary greatly between stroke, a vascular disease, and Parkinson’s and Alzheimer’s diseases, which are neurodegenerative diseases [156]. A systematic review of umbrella reviews revealed a significant association of high serum uric acid levels with a decreased risk of several neurological diseases (i.e., Parkinson’s disease, Alzheimer’s disease, dementia, multiple sclerosis, neuromyelitis optica, and amyotrophic lateral sclerosis) [157]. Several recent studies that focused on the relationship between uric acid and varying neurological diseases are summarized below.
13.1. Stroke
There seems to be no doubt about the relationship between serum uric acid and stroke [158,159]. The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a case-cohort study with large data sets, concluded that hyperuricemia may be a risk factor for stroke [160]. A meta-umbrella review showed class I evidence that high uric acid levels were associated with risk for stroke mortality [157]. However, some epidemiological studies reported inconsistent findings on the relationship between serum uric acid levels and stroke [161,162]. In addition, Jiaqi et al. conducted a prospective cohort study in Japan and showed that elevated serum uric acid levels are an independent predictor of total and ischemic stroke in women only [163]. Therefore, the causality remains controversial.
A retrospective cohort study conducted using the Taiwanese population-based National Health Insurance Research Database showed that gout patients treated with ULT had a lower risk of hospitalized stroke and all-cause mortality compared to those without ULT. In addition, the effect of uricosuric agents on reducing the risk of hospitalization due to stroke showed a dose-response relationship [164]. The ALL-HEART did not differ in the outcome of nonfatal stroke between participants assigned to allopurinol therapy and those assigned to usual care [142]. Thus, there is still little clear evidence of stroke prevention by ULT.
13.2. Parkinson’s Disease
Parkinson’s disease is the second most common neurodegenerative disease after Alzheimer’s disease. Serum uric acid levels are known to be low in Parkinson’s disease. Furthermore, lower serum uric acid levels have been associated with the risk of developing Parkinson’s disease, severity, nonmotor symptoms, and slow disease progression [165,166]. This mechanism is thought to be due to low uric acid levels, which inhibit oxidative stress that predisposes to dopaminergic neuron degeneration in Parkinson’s disease [167]. To demonstrate this mechanism, a clinical trial was conducted in early Parkinson’s disease patients receiving inosine to increase serum uric acid levels. However, no difference in the rate of clinical disease progression in Parkinson’s disease was observed compared to placebo [168].
13.3. Alzheimer’s Disease and Dementia
The relationship between uric acid and dementia, especially neurodegenerative diseases such as Alzheimer’s, has been studied. Higher serum uric acid levels were associated with better cognitive function and appeared to be neuroprotective. A prospective cohort study conducted in Sweden involving women only over a 44-year period showed an association between higher serum uric acid levels and a lower risk of dementia. This study supports the hypothesis that serum uric acid levels play a protective role in the development of dementia, regardless of dementia subtype [169]. A cross-sectional study obtained from the ReGAl 2.0 project in Italy also showed that serum uric acid levels were lower in patients with Alzheimer’s disease [170]. In contrast, the Atherosclerosis Risk in Communities (ARIC) cohort showed no association between serum uric acid levels and incident dementia [171]. Since evidence from observational studies is susceptible to numerous biases, the effects of gender, age, and dementia subtypes must also be considered. To date, few clinical interventional studies have investigated the potential of inosine therapy in patients with Alzheimer’s disease. However, basic evidence suggests that inosine might be a promising therapeutic strategy for Alzheimer’s disease thanks to its ability to modulate different brain mechanisms involved in neuroprotection [172].
13.4. Multiple Sclerosis and Neuromyelitis Optica
Multiple sclerosis and neuromyelitis optica are autoimmune central nervous system diseases; a meta-analysis of 10 case-control studies found that patients with multiple sclerosis and neuromyelitis optica had lower serum uric acid levels compared to healthy controls [173]. In a 12-month randomized, placebo-controlled trial following patients after inosine administration, it was determined that inosine did not possess neuroprotective effects, thus proving ineffective for relapsing–remitting multiple sclerosis. Nevertheless, a comprehensive evaluation of the efficacy of inosine for multiple sclerosis is needed, involving an extended follow-up period of over one year [174].
13.5. Amyotrophic Lateral Sclerosis
A national database of South Korea study found that the prevalence of amyotrophic lateral sclerosis (ALS) in gout patients was substantially lower than in the general population [175]. A cross-sectional study was conducted to determine the relationship between serum uric acid levels and cognitive impairment in patients with ALS in China. The results showed that a low serum uric acid level was an independent risk factor for cognitive impairment in patients with amyotrophic lateral sclerosis [176]. Furthermore, a longitudinal cohort study in China found an inverse association between serum uric acid levels and risk of death, particularly pronounced in male patients with ALS [177].
14. Malignancies
The relationship between malignancy and hyperuricemia requires multifaceted references to antioxidant effects and etiology. Although it has long been proposed that uric acid, particularly as an endogenous antioxidant, may exert anticarcinogenic properties [7,178], recently, some studies have been conducted on cancer risk of hyperuricemia and inflammation caused by gout, or oxidative stress involved in ROS, in the etiology of malignant tumors [179].
The association between uric acid levels and prognosis has also been examined in several papers on hematologic malignancies and solid tumors. It has been suggested that high uric acid levels are a poor prognostic factor in acute myeloid leukemia [180]. In diffuse large B-cell lymphoma, a high uric acid level is a shorter progression-free and overall survival [181].
Tumor lysis syndrome (TLS) is a life-threatening complication that is caused by the sudden and massive death of cancer cells upon chemotherapy [182,183,184] (Figure 4). According to the Japanese Adverse Drug Event Report database, the incidence of TLS has increased 7.5 times from 2003 to 2019, with a total of 620 cases reported. The mortality rate due to TLS is reported to be 15–30%, making it one of the oncologic emergencies for which preventive treatment is recommended in the guidelines. Intracellular metabolites, which include proteins, potassium, phosphorus, and nucleic acids, are rapidly released from lysed cells to circulating blood. This may result in hyperkalemia, hyperphosphatemia, and hyperuricemia, thereby inducing renal insufficiency, cardiac arrhythmias, seizures, neurological disorders, and ultimately death. As far as TLS treatment, the use of rasburicase and febuxostat has led to a breakthrough in ULT, guidelines have been developed, and a consensus has been reached.
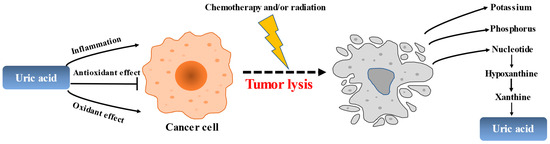
Figure 4.
The role of uric acid in the pathogenesis of tumors and tumor lysis.
In the past, TLS was mainly concerned with acute lymphocytic leukemia, aggressive lymphomas in advanced stages, and acute myeloid leukemia with high tumor volume. In recent years, however, caution has been exercised in cases of TLS in chronic lymphocytic leukemia and acute myeloid leukemia in the elderly with the advent of B-cell lymphoma-2 (BCL2) inhibitors, and in multiple myeloma, where multidrug combination therapy has become the mainstay with the advent of proteasome inhibition, immunomodulatory agents, and antibody drugs. While the risk of TLS in these cases has not been systematically examined, Howard et al. identified published Phase I–III clinical trials of monoclonal antibodies [185]. According to the paper, the incidence of TLS with alvocidib was 4.2% in recurrent treatment-resistant ALL, 13.2% in mantle cell lymphoma, indolent B-cell lymphoma, and chronic lymphocytic leukemia (CLL), and 42.2% in acute myeloid leukemia.
The relationship between uric acid and malignancies is uncertain. Therefore, it is necessary to continue to investigate the mechanism of how hyperuricemia is associated with the development of malignancy and to continue to manage TLS that may develop following chemotherapy. We must remember to evaluate and control TLS as a side effect prior to the use of new anticancer drugs.
Since there is no uniformity in the selection and use of uric acid-lowering medicine for TLS prophylaxis in clinical studies, adequate TLS management should also be evaluated when assessing the frequency of each TLS incidence.
15. Conclusions
Taking into account recent research on uric acid, it is important to acknowledge that while numerous studies have identified associations between uric acid and various diseases, establishing a definitive causal relationship remains challenging in numerous instances. Given the intricate and multifaceted nature of uric acid’s involvement across many diseases, there is a clear need for conducting additional comprehensive investigations into uric acid. One proposed solution to address these challenges is the implementation of high-quality prospective RCTs while considering their intricate interactions and potential implications. Such research endeavors are essential, as they hold the key to unraveling the complexities surrounding uric acid and revealing its potential role in disease pathogenesis.
Author Contributions
Conceptualization, M.K. (Masanari Kuwabara); methodology, M.K. (Masanari Kuwabara), M.K. (Masafumi Kurajoh) and K.A.; software, M.K. (Masanari Kuwabara); validation, M.K. (Masanari Kuwabara) and K.A.; investigation, all authors; resources, all authors; data curation, M.K. (Masanari Kuwabara); writing—original draft preparation, M.K. (Masanari Kuwabara), T.F., Y.A., E.M., M.O., M.K. (Masafumi Kurajoh), T.M., A.T., N.M., K.N., N.A., Y.T, N.O., M.M., H.M. and T.T.; writing—review and editing, all authors; visualization, M.K. (Masanari Kuwabara), T.F., A.T., K.N., N.A, Y.T., M.M., H.M., T.T. and K.A.; supervision, M.K. (Masanari Kuwabara), T.T., H.T., K.O., K.I. and I.H.; project administration, all authors; funding acquisition, M.K. (Masanari Kuwabara). All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by JSPS KAKENHI Grant (20K17168 and 23K07493) and Toranomon Hospital Grant (M.Kuwa.); JSPS KAKENHI Grant (21K11581) (T.F.); JSPS KAKENHI Grant (22K06701) (N.O.); and JSPS KAKENHI Grant (22K15507) (M.M.).
Conflicts of Interest
N.O. declares having received grants from Sato Pharmaceutical Co., Ltd. T.T. declares having re-ceived fees for advisory boards and speaking fees from Mochida Pharmaceutical company and Fuji Yakuhin Co., Ltd. I.H. declares having received grants and fees for advisory boards and speaking fees from Fuji Yakuhin Co., Ltd, Mochida Pharmaceutical company, and Meiji Co., Ltd. K.A. de-clares having received grants and honoraria from Mochida Pharmaceutical company. The other authors have no competing interests to declare.
References
- Elfishawi, M.M.; Zleik, N.; Kvrgic, Z.; Michet, C.J., Jr.; Crowson, C.S.; Matteson, E.L.; Bongartz, T. The Rising Incidence of Gout and the Increasing Burden of Comorbidities: A Population-based Study over 20 Years. J. Rheumatol. 2018, 45, 574–579. [Google Scholar] [CrossRef]
- Dehlin, M.; Jacobsson, L.; Roddy, E. Global epidemiology of gout: Prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 2020, 16, 380–390. [Google Scholar] [CrossRef] [PubMed]
- She, D.; Wang, Y.; Liu, J.; Luo, N.; Feng, S.; Li, Y.; Xu, J.; Xie, S.; Zhu, Y.; Xue, Y.; et al. Changes in the prevalence of hyperuricemia in clients of health examination in Eastern China, 2009 to 2019. BMC Endocr. Disord. 2022, 22, 202. [Google Scholar] [CrossRef] [PubMed]
- Barazani, S.H.; Chi, W.W.; Pyzik, R.; Chang, H.; Jacobi, A.; O’Donnell, T.; Fayad, Z.A.; Ali, Y.; Mani, V. Quantification of uric acid in vasculature of patients with gout using dual-energy computed tomography. World J. Radiol. 2020, 12, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Curhan, G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation 2007, 116, 894–900. [Google Scholar] [CrossRef]
- Oda, M.; Satta, Y.; Takenaka, O.; Takahata, N. Loss of urate oxidase activity in hominoids and its evolutionary implications. Mol. Biol. Evol. 2002, 19, 640–653. [Google Scholar] [CrossRef]
- Ames, B.N.; Cathcart, R.; Schwiers, E.; Hochstein, P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: A hypothesis. Proc. Natl. Acad. Sci. USA 1981, 78, 6858–6862. [Google Scholar] [CrossRef]
- Hink, H.U.; Santanam, N.; Dikalov, S.; McCann, L.; Nguyen, A.D.; Parthasarathy, S.; Harrison, D.G.; Fukai, T. Peroxidase properties of extracellular superoxide dismutase: Role of uric acid in modulating in vivo activity. Arterioscler. Thromb. Vasc. Biol. 2002, 22, 1402–1408. [Google Scholar] [CrossRef]
- Davies, K.J.; Sevanian, A.; Muakkassah-Kelly, S.F.; Hochstein, P. Uric acid-iron ion complexes. A new aspect of the antioxidant functions of uric acid. Biochem. J. 1986, 235, 747–754. [Google Scholar] [CrossRef]
- Hui, M.; Carr, A.; Cameron, S.; Davenport, G.; Doherty, M.; Forrester, H.; Jenkins, W.; Jordan, K.M.; Mallen, C.D.; McDonald, T.M.; et al. The British Society for Rheumatology Guideline for the Management of Gout. Rheumatology 2017, 56, e1–e20. [Google Scholar] [CrossRef]
- FitzGerald, J.D.; Dalbeth, N.; Mikuls, T.; Brignardello-Petersen, R.; Guyatt, G.; Abeles, A.M.; Gelber, A.C.; Harrold, L.R.; Khanna, D.; King, C.; et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res. 2020, 72, 744–760. [Google Scholar] [CrossRef] [PubMed]
- Yamanaka, H. Japanese guideline for the management of hyperuricemia and gout: Second edition. Nucleosides Nucleotides Nucleic Acids 2011, 30, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- Hisatome, I.; Ichida, K.; Mineo, I.; Ohtahara, A.; Ogino, K.; Kuwabara, M.; Ishizaka, N.; Uchida, S.; Kurajoh, M.; Kohagura, K.; et al. Japanese Society of gout and uric & nucleic acids 2019 guidelines for management of hyperuricemia and gout 3rd edition. Gout Uric Nucleic Acids 2020, 44, 1–40. [Google Scholar]
- Enomoto, A.; Kimura, H.; Chairoungdua, A.; Shigeta, Y.; Jutabha, P.; Cha, S.H.; Hosoyamada, M.; Takeda, M.; Sekine, T.; Igarashi, T.; et al. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 2002, 417, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.; Chandler, J.D.; Clarke, A.L.; Petrou, S.; Best, J.D. Glucose transporter GLUT12-functional characterization in Xenopus laevis oocytes. Biochem. Biophys. Res. Commun. 2003, 308, 422–426. [Google Scholar] [CrossRef]
- Tin, A.; Woodward, O.M.; Kao, W.H.; Liu, C.T.; Lu, X.; Nalls, M.A.; Shriner, D.; Semmo, M.; Akylbekova, E.L.; Wyatt, S.B.; et al. Genome-wide association study for serum urate concentrations and gout among African Americans identifies genomic risk loci and a novel URAT1 loss-of-function allele. Hum. Mol. Genet. 2011, 20, 4056–4068. [Google Scholar] [CrossRef]
- Toyoda, Y.; Takada, T.; Miyata, H.; Matsuo, H.; Kassai, H.; Nakao, K.; Nakatochi, M.; Kawamura, Y.; Shimizu, S.; Shinomiya, N.; et al. Identification of GLUT12/SLC2A12 as a urate transporter that regulates the blood urate level in hyperuricemia model mice. Proc. Natl. Acad. Sci. USA 2020, 117, 18175–18177. [Google Scholar] [CrossRef]
- Bahn, A.; Hagos, Y.; Reuter, S.; Balen, D.; Brzica, H.; Krick, W.; Burckhardt, B.C.; Sabolic, I.; Burckhardt, G. Identification of a new urate and high affinity nicotinate transporter, hOAT10 (SLC22A13). J. Biol. Chem. 2008, 283, 16332–16341. [Google Scholar] [CrossRef]
- Higashino, T.; Morimoto, K.; Nakaoka, H.; Toyoda, Y.; Kawamura, Y.; Shimizu, S.; Nakamura, T.; Hosomichi, K.; Nakayama, A.; Ooyama, K.; et al. Dysfunctional missense variant of OAT10/SLC22A13 decreases gout risk and serum uric acid levels. Ann. Rheum. Dis. 2020, 79, 164–166. [Google Scholar] [CrossRef]
- Toyoda, Y.; Kawamura, Y.; Nakayama, A.; Morimoto, K.; Shimizu, S.; Tanahashi, Y.; Tamura, T.; Kondo, T.; Kato, Y.; Ichida, K.; et al. OAT10/SLC22A13 Acts as a Renal Urate Re-Absorber: Clinico-Genetic and Functional Analyses with Pharmacological Impacts. Front. Pharmacol. 2022, 13, 842717. [Google Scholar] [CrossRef]
- Corpe, C.P.; Tu, H.; Eck, P.; Wang, J.; Faulhaber-Walter, R.; Schnermann, J.; Margolis, S.; Padayatty, S.; Sun, H.; Wang, Y.; et al. Vitamin C transporter Slc23a1 links renal reabsorption, vitamin C tissue accumulation, and perinatal survival in mice. J. Clin. Investig. 2010, 120, 1069–1083. [Google Scholar] [CrossRef] [PubMed]
- Sotiriou, S.; Gispert, S.; Cheng, J.; Wang, Y.; Chen, A.; Hoogstraten-Miller, S.; Miller, G.F.; Kwon, O.; Levine, M.; Guttentag, S.H.; et al. Ascorbic-acid transporter Slc23a1 is essential for vitamin C transport into the brain and for perinatal survival. Nat. Med. 2002, 8, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, Y.; Miyata, H.; Uchida, N.; Morimoto, K.; Shigesawa, R.; Kassai, H.; Nakao, K.; Tomioka, N.H.; Matsuo, H.; Ichida, K.; et al. Vitamin C transporter SVCT1 serves a physiological role as a urate importer: Functional analyses and in vivo investigations. Pflugers Arch. 2023, 475, 489–504. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, Y.; Miyata, H.; Shigesawa, R.; Matsuo, H.; Suzuki, H.; Takada, T. SVCT2/SLC23A2 is a sodium-dependent urate transporter: Functional properties and practical application. J. Biol. Chem. 2023, 299, 104976. [Google Scholar] [CrossRef]
- Keenan, T.; Zhao, W.; Rasheed, A.; Ho, W.K.; Malik, R.; Felix, J.F.; Young, R.; Shah, N.; Samuel, M.; Sheikh, N.; et al. Causal Assessment of Serum Urate Levels in Cardiometabolic Diseases through a Mendelian Randomization Study. J. Am. Coll. Cardiol. 2016, 67, 407–416. [Google Scholar] [CrossRef]
- Palmer, T.M.; Nordestgaard, B.G.; Benn, M.; Tybjaerg-Hansen, A.; Davey Smith, G.; Lawlor, D.A.; Timpson, N.J. Association of plasma uric acid with ischaemic heart disease and blood pressure: Mendelian randomisation analysis of two large cohorts. BMJ 2013, 347, f4262. [Google Scholar] [CrossRef]
- Sedaghat, S.; Pazoki, R.; Uitterlinden, A.G.; Hofman, A.; Stricker, B.H.; Ikram, M.A.; Franco, O.H.; Dehghan, A. Association of uric acid genetic risk score with blood pressure: The Rotterdam study. Hypertension 2014, 64, 1061–1066. [Google Scholar] [CrossRef]
- Chaves, F.J.; Corella, D.; Blesa, S.; Mansego, M.L.; Marin, P.; Portoles, O.; Sorli, J.V.; Gonzalez-Albert, V.; Tormos, M.C.; Garcia-Garcia, A.B.; et al. Xanthine oxidoreductase polymorphisms: Influence in blood pressure and oxidative stress levels. Pharmacogenet Genom. 2007, 17, 589–596. [Google Scholar] [CrossRef]
- Wu, B.; Hao, Y.; Shi, J.; Geng, N.; Li, T.; Chen, Y.; Sun, Z.; Zheng, L.; Li, H.; Li, N.; et al. Association between xanthine dehydrogenase tag single nucleotide polymorphisms and essential hypertension. Mol. Med. Rep. 2015, 12, 5685–5690. [Google Scholar] [CrossRef][Green Version]
- Kleber, M.E.; Delgado, G.; Grammer, T.B.; Silbernagel, G.; Huang, J.; Kramer, B.K.; Ritz, E.; Marz, W. Uric Acid and Cardiovascular Events: A Mendelian Randomization Study. J. Am. Soc. Nephrol. 2015, 26, 2831–2838. [Google Scholar] [CrossRef]
- Gill, D.; Cameron, A.C.; Burgess, S.; Li, X.; Doherty, D.J.; Karhunen, V.; Abdul-Rahim, A.H.; Taylor-Rowan, M.; Zuber, V.; Tsao, P.S.; et al. Urate, Blood Pressure, and Cardiovascular Disease: Evidence from Mendelian Randomization and Meta-Analysis of Clinical Trials. Hypertension 2021, 77, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.J.; Segal, M.S.; Sautin, Y.; Nakagawa, T.; Feig, D.I.; Kang, D.H.; Gersch, M.S.; Benner, S.; Sanchez-Lozada, L.G. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am. J. Clin. Nutr. 2007, 86, 899–906. [Google Scholar] [PubMed]
- Yokose, C.; McCormick, N.; Choi, H.K. The role of diet in hyperuricemia and gout. Curr. Opin. Rheumatol. 2021, 33, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Topless, R.K.G.; Major, T.J.; Florez, J.C.; Hirschhorn, J.N.; Cadzow, M.; Dalbeth, N.; Stamp, L.K.; Wilcox, P.L.; Reynolds, R.J.; Cole, J.B.; et al. The comparative effect of exposure to various risk factors on the risk of hyperuricaemia: Diet has a weak causal effect. Arthritis Res. Ther. 2021, 23, 75. [Google Scholar] [CrossRef] [PubMed]
- McCormick, N.; Rai, S.K.; Lu, N.; Yokose, C.; Curhan, G.C.; Choi, H.K. Estimation of Primary Prevention of Gout in Men through Modification of Obesity and Other Key Lifestyle Factors. JAMA Netw. Open 2020, 3, e2027421. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; McCormick, N.; Yokose, C.; Joshi, A.D.; Lu, N.; Curhan, G.C.; Merriman, T.R.; Saag, K.G.; Ridker, P.M.; Buring, J.E.; et al. Interactions Between Genetic Risk and Diet Influencing Risk of Incident Female Gout: Discovery and Replication Analysis of Four Prospective Cohorts. Arthritis Rheumatol. 2023, 75, 1028–1038. [Google Scholar] [CrossRef]
- Shirai, Y.; Nakayama, A.; Kawamura, Y.; Toyoda, Y.; Nakatochi, M.; Shimizu, S.; Shinomiya, N.; Okada, Y.; Matsuo, H.; Japan Gout Genomics, C. Coffee Consumption Reduces Gout Risk Independently of Serum Uric Acid Levels: Mendelian Randomization Analyses Across Ancestry Populations. ACR Open Rheumatol. 2022, 4, 534–539. [Google Scholar] [CrossRef]
- Kaneko, K.; Aoyagi, Y.; Fukuuchi, T.; Inazawa, K.; Yamaoka, N. Total purine and purine base content of common foodstuffs for facilitating nutritional therapy for gout and hyperuricemia. Biol. Pharm. Bull. 2014, 37, 709–721. [Google Scholar] [CrossRef]
- Takayanagi, F.; Uchino, T.; Motoki, N.; Uchida, K.; Asakura, H.; Uno-Eder, K.; Nomura, T.; Tsukamoto, K.; Fukuuchi, T.; Yamaoka, N.; et al. Purine content of hospital meals and its effect on serum uric acid, urine pH, and urinary uric acid excretion. Nucleosides Nucleotides Nucleic Acids 2022, 41, 1296–1304. [Google Scholar] [CrossRef]
- Nakamura, H.; Kawashima, T.; Yamasaki, L.; Lwin, K.S.; Eguchi, A.; Hayabuchi, H.; Tanoe, Y.; Tanaka, S.; Yoneoka, D.; Ghaznavi, C.; et al. Reducing salt intake with umami: A secondary analysis of data in the UK National Diet and Nutrition Survey. Food Sci. Nutr. 2023, 11, 872–882. [Google Scholar] [CrossRef]
- Kasahara, K.; Kerby, R.L.; Zhang, Q.; Pradhan, M.; Mehrabian, M.; Lusis, A.J.; Bergstrom, G.; Backhed, F.; Rey, F.E. Gut bacterial metabolism contributes to host global purine homeostasis. Cell Host Microbe 2023, 31, 1038–1053.e1010. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.M.; Garranzo, M.; Segura, J.; Orgaz, B.; Arroyo, R.; Alba, C.; Beltran, D.; Fernandez, L. A randomized pilot trial assessing the reduction of gout episodes in hyperuricemic patients by oral administration of Ligilactobacillus salivarius CECT 30632, a strain with the ability to degrade purines. Front. Microbiol. 2023, 14, 1111652. [Google Scholar] [CrossRef] [PubMed]
- Kubota, M. Hyperuricemia in Children and Adolescents: Present Knowledge and Future Directions. J. Nutr. Metab. 2019, 2019, 3480718. [Google Scholar] [CrossRef] [PubMed]
- Aoki, Y.; Sofue, T.; Kawakami, R.; Ozaki, T.; Manabe, M.; Kanda, K.; Yoda, T.; Kusaka, T.; Hirao, T.; Minamino, T. Prevalence and factors related to hypouricemia and hyperuricemia in schoolchildren: Results of a large-scale cross-sectional population-based study conducted in Japan. Sci. Rep. 2022, 12, 17848. [Google Scholar] [CrossRef]
- Sirota, J.C.; McFann, K.; Targher, G.; Johnson, R.J.; Chonchol, M.; Jalal, D.I. Elevated serum uric acid levels are associated with non-alcoholic fatty liver disease independently of metabolic syndrome features in the United States: Liver ultrasound data from the National Health and Nutrition Examination Survey. Metabolism 2013, 62, 392–399. [Google Scholar] [CrossRef]
- Mosca, A.; Nobili, V.; De Vito, R.; Crudele, A.; Scorletti, E.; Villani, A.; Alisi, A.; Byrne, C.D. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J. Hepatol. 2017, 66, 1031–1036. [Google Scholar] [CrossRef]
- Alper, A.B., Jr.; Chen, W.; Yau, L.; Srinivasan, S.R.; Berenson, G.S.; Hamm, L.L. Childhood uric acid predicts adult blood pressure: The Bogalusa Heart Study. Hypertension 2005, 45, 34–38. [Google Scholar] [CrossRef]
- Rodenbach, K.E.; Schneider, M.F.; Furth, S.L.; Moxey-Mims, M.M.; Mitsnefes, M.M.; Weaver, D.J.; Warady, B.A.; Schwartz, G.J. Hyperuricemia and Progression of CKD in Children and Adolescents: The Chronic Kidney Disease in Children (CKiD) Cohort Study. Am. J. Kidney Dis. 2015, 66, 984–992. [Google Scholar] [CrossRef]
- Gwinnutt, J.M.; Wieczorek, M.; Balanescu, A.; Bischoff-Ferrari, H.A.; Boonen, A.; Cavalli, G.; de Souza, S.; de Thurah, A.; Dorner, T.E.; Moe, R.H.; et al. 2021 EULAR recommendations regarding lifestyle behaviours and work participation to prevent progression of rheumatic and musculoskeletal diseases. Ann. Rheum. Dis. 2023, 82, 48–56. [Google Scholar] [CrossRef]
- Williams, P.T. Effects of diet, physical activity and performance, and body weight on incident gout in ostensibly healthy, vigorously active men. Am. J. Clin. Nutr. 2008, 87, 1480–1487. [Google Scholar] [CrossRef]
- Park, D.Y.; Kim, Y.S.; Ryu, S.H.; Jin, Y.S. The association between sedentary behavior, physical activity and hyperuricemia. Vasc. Health Risk Manag. 2019, 15, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Li, Y.; Zhang, L.; Liu, X.; Tu, R.; Wang, Y.; Li, R.; Li, L.; Hou, J.; Mao, Z.; et al. Independent and interactive effect of sitting time and physical activity on prevalence of hyperuricemia: The Henan Rural Cohort Study. Arthritis Res. Ther. 2021, 23, 7. [Google Scholar] [CrossRef] [PubMed]
- Andres-Hernando, A.; Cicerchi, C.; Kuwabara, M.; Orlicky, D.J.; Sanchez-Lozada, L.G.; Nakagawa, T.; Johnson, R.J.; Lanaspa, M.A. Umami-induced obesity and metabolic syndrome is mediated by nucleotide degradation and uric acid generation. Nat. Metab. 2021, 3, 1189–1201. [Google Scholar] [CrossRef] [PubMed]
- Yokose, C.; McCormick, N.; Choi, H.K. Dietary and Lifestyle-Centered Approach in Gout Care and Prevention. Curr. Rheumatol. Rep. 2021, 23, 51. [Google Scholar] [CrossRef] [PubMed]
- So, A.K.; Martinon, F. Inflammation in gout: Mechanisms and therapeutic targets. Nat. Rev. Rheumatol. 2017, 13, 639–647. [Google Scholar] [CrossRef]
- Li, X.; Meng, X.; Timofeeva, M.; Tzoulaki, I.; Tsilidis, K.K.; Ioannidis, J.P.; Campbell, H.; Theodoratou, E. Serum uric acid levels and multiple health outcomes: Umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ 2017, 357, j2376. [Google Scholar] [CrossRef]
- Seminog, O.O.; Goldacre, M.J. Gout as a risk factor for myocardial infarction and stroke in England: Evidence from record linkage studies. Rheumatology 2013, 52, 2251–2259. [Google Scholar] [CrossRef]
- Cipolletta, E.; Tata, L.J.; Nakafero, G.; Avery, A.J.; Mamas, M.A.; Abhishek, A. Association Between Gout Flare and Subsequent Cardiovascular Events Among Patients with Gout. JAMA 2022, 328, 440–450. [Google Scholar] [CrossRef]
- Lopez, D.; Dwivedi, G.; Nossent, J.; Preen, D.B.; Murray, K.; Raymond, W.; Inderjeeth, C.; Keen, H.I. Risk of Major Adverse Cardiovascular Event Following Incident Hospitalization for Acute Gout: A Western Australian Population-Level Linked Data Study. ACR Open Rheumatol. 2023, 5, 298–304. [Google Scholar] [CrossRef]
- Hisatome, I.; Li, P.; Miake, J.; Taufiq, F.; Mahati, E.; Maharani, N.; Utami, S.B.; Kuwabara, M.; Bahrudin, U.; Ninomiya, H. Uric Acid as a Risk Factor for Chronic Kidney Disease and Cardiovascular Disease—Japanese Guideline on the Management of Asymptomatic Hyperuricemia. Circ. J. 2021, 85, 130–138. [Google Scholar] [CrossRef]
- Koto, R.; Nakajima, A.; Horiuchi, H.; Yamanaka, H. Serum uric acid control for prevention of gout flare in patients with asymptomatic hyperuricaemia: A retrospective cohort study of health insurance claims and medical check-up data in Japan. Ann. Rheum. Dis. 2021, 80, 1483–1490. [Google Scholar] [CrossRef] [PubMed]
- Stamp, L.; Morillon, M.B.; Taylor, W.J.; Dalbeth, N.; Singh, J.A.; Lassere, M.; Christensen, R. Serum urate as surrogate endpoint for flares in people with gout: A systematic review and meta-regression analysis. Semin. Arthritis Rheum. 2018, 48, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Pascart, T.; Grandjean, A.; Capon, B.; Legrand, J.; Namane, N.; Ducoulombier, V.; Motte, M.; Vandecandelaere, M.; Luraschi, H.; Godart, C.; et al. Monosodium urate burden assessed with dual-energy computed tomography predicts the risk of flares in gout: A 12-month observational study: MSU burden and risk of gout flare. Arthritis Res. Ther. 2018, 20, 210. [Google Scholar] [CrossRef] [PubMed]
- Ellmann, H.; Bayat, S.; Araujo, E.; Manger, B.; Kleyer, A.; Cavallaro, A.; Lell, M.; Schenker, H.; Simon, D.; Tascilar, K.; et al. Effects of Conventional Uric Acid-Lowering Therapy on Monosodium Urate Crystal Deposits. Arthritis Rheumatol. 2020, 72, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.; Tomlinson, G.A.; Lipscombe, L.L.; Perkins, B.A.; Hawker, G.A. Allopurinol adherence, persistence and patterns of use in individuals with diabetes and gout: A retrospective, population-based cohort analysis. Semin. Arthritis Rheum. 2021, 51, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Rho, Y.H.; Lu, N.; Peloquin, C.E.; Man, A.; Zhu, Y.; Zhang, Y.; Choi, H.K. Independent impact of gout on the risk of diabetes mellitus among women and men: A population-based, BMI-matched cohort study. Ann. Rheum. Dis. 2016, 75, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Ford, E.S. Haemoglobin A1c, fasting glucose, serum C-peptide and insulin resistance in relation to serum uric acid levels—The Third National Health and Nutrition Examination Survey. Rheumatology 2008, 47, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Shin, D. Concurrent presence of high serum uric acid and inflammation is associated with increased incidence of type 2 diabetes mellitus in Korean adult population. Sci. Rep. 2022, 12, 11000. [Google Scholar] [CrossRef]
- Zhu, J.; Sun, L.; Yang, J.; Fan, J.; Tse, L.A.; Li, Y. Genetic Predisposition to Type 2 Diabetes and Insulin Levels Is Positively Associated with Serum Urate Levels. J. Clin. Endocrinol. Metab. 2021, 106, e2547–e2556. [Google Scholar] [CrossRef]
- Hu, X.; Rong, S.; Wang, Q.; Sun, T.; Bao, W.; Chen, L.; Liu, L. Association between plasma uric acid and insulin resistance in type 2 diabetes: A Mendelian randomization analysis. Diabetes Res. Clin. Pract. 2021, 171, 108542. [Google Scholar] [CrossRef]
- Banerjee, M.; Pal, R.; Maisnam, I.; Chowdhury, S.; Mukhopadhyay, S. Serum uric acid lowering and effects of sodium-glucose cotransporter-2 inhibitors on gout: A meta-analysis and meta-regression of randomized controlled trials. Diabetes Obes. Metab. 2023, 25, 2697–2703. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, D. Blood Lipid and Uric Acid Interrelationships. JAMA 1964, 190, 856–858. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Dong, H.; Zhang, B.; Zhang, J.; Ma, Q.; Sun, H. Association between dyslipidaemia and the risk of hyperuricaemia: A six-year longitudinal cohort study of elderly individuals in China. Ann. Med. 2022, 54, 2402–2410. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, M.; Borghi, C.; Cicero, A.F.G.; Hisatome, I.; Niwa, K.; Ohno, M.; Johnson, R.J.; Lanaspa, M.A. Elevated serum uric acid increases risks for developing high LDL cholesterol and hypertriglyceridemia: A five-year cohort study in Japan. Int. J. Cardiol. 2018, 261, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Castro, V.M.F.; Melo, A.C.; Belo, V.S.; Chaves, V.E. Effect of allopurinol and uric acid normalization on serum lipids hyperuricemic subjects: A systematic review with meta-analysis. Clin. Biochem. 2017, 50, 1289–1297. [Google Scholar] [CrossRef]
- Jaruvongvanich, V.; Ahuja, W.; Wirunsawanya, K.; Wijarnpreecha, K.; Ungprasert, P. Hyperuricemia is associated with nonalcoholic fatty liver disease activity score in patients with nonalcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1031–1035. [Google Scholar] [CrossRef]
- Ma, Z.; Zhang, J.; Kang, X.; Xu, C.; Sun, C.; Tao, L.; Zheng, D.; Han, Y.; Li, Q.; Guo, X.; et al. Hyperuricemia precedes non-alcoholic fatty liver disease with abdominal obesity moderating this unidirectional relationship: Three longitudinal analyses. Atherosclerosis 2020, 311, 44–51. [Google Scholar] [CrossRef]
- Paschos, P.; Athyros, V.G.; Tsimperidis, A.; Katsoula, A.; Grammatikos, N.; Giouleme, O. Can Serum Uric Acid Lowering Therapy Contribute to the Prevention or Treatment of Nonalcoholic Fatty Liver Disease? Curr. Vasc. Pharmacol. 2018, 16, 269–275. [Google Scholar] [CrossRef]
- Yeo, C.; Kaushal, S.; Lim, B.; Syn, N.; Oo, A.M.; Rao, J.; Koura, A.; Yeo, D. Impact of bariatric surgery on serum uric acid levels and the incidence of gout-A meta-analysis. Obes. Rev. 2019, 20, 1759–1770. [Google Scholar] [CrossRef]
- Bortolotti, M.; Polito, L.; Battelli, M.G.; Bolognesi, A. Xanthine oxidoreductase: One enzyme for multiple physiological tasks. Redox Biol. 2021, 41, 101882. [Google Scholar] [CrossRef]
- Kurajoh, M.; Fukumoto, S.; Murase, T.; Nakamura, T.; Ishihara, T.; Go, H.; Yamamoto, K.; Nakatani, S.; Tsuda, A.; Morioka, T.; et al. Insulin Resistance Associated with Plasma Xanthine Oxidoreductase Activity Independent of Visceral Adiposity and Adiponectin Level: MedCity21 Health Examination Registry. Int. J. Endocrinol. 2019, 2019, 1762161. [Google Scholar] [CrossRef] [PubMed]
- Kurajoh, M.; Fukumoto, S.; Emoto, M.; Murase, T.; Nakamura, T.; Ishihara, T.; Go, H.; Yamamoto, K.; Nakatani, S.; Tsuda, A.; et al. Independent association of plasma xanthine oxidoreductase activity with serum uric acid level based on stable isotope-labeled xanthine and liquid chromatography/triple quadrupole mass spectrometry: MedCity21 health examination registry. Clin. Chem. Lab. Med. 2020, 58, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, W.; McRae, S.; Marek, G.; Wymer, D.; Pannu, V.; Baylis, C.; Johnson, R.J.; Sautin, Y.Y. Hyperuricemia as a mediator of the proinflammatory endocrine imbalance in the adipose tissue in a murine model of the metabolic syndrome. Diabetes 2011, 60, 1258–1269. [Google Scholar] [CrossRef]
- Ogino, K.; Kato, M.; Furuse, Y.; Kinugasa, Y.; Ishida, K.; Osaki, S.; Kinugawa, T.; Igawa, O.; Hisatome, I.; Shigemasa, C.; et al. Uric acid-lowering treatment with benzbromarone in patients with heart failure: A double-blind placebo-controlled crossover preliminary study. Circ. Heart Fail. 2010, 3, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Nagoshi, T.; Takahashi, H.; Oi, Y.; Yoshii, A.; Kimura, H.; Ito, K.; Kashiwagi, Y.; Tanaka, T.D.; Yoshimura, M. URAT1-selective inhibition ameliorates insulin resistance by attenuating diet-induced hepatic steatosis and brown adipose tissue whitening in mice. Mol. Metab. 2022, 55, 101411. [Google Scholar] [CrossRef] [PubMed]
- Maruhashi, T.; Hisatome, I.; Kihara, Y.; Higashi, Y. Hyperuricemia and endothelial function: From molecular background to clinical perspectives. Atherosclerosis 2018, 278, 226–231. [Google Scholar] [CrossRef]
- Tanaka, A.; Kawaguchi, A.; Tomiyama, H.; Ishizu, T.; Matsumoto, C.; Higashi, Y.; Takase, B.; Suzuki, T.; Ueda, S.; Yamazaki, T.; et al. Cross-sectional and longitudinal associations between serum uric acid and endothelial function in subjects with treated hypertension. Int. J. Cardiol. 2018, 272, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Canepa, M.; Viazzi, F.; Strait, J.B.; Ameri, P.; Pontremoli, R.; Brunelli, C.; Studenski, S.; Ferrucci, L.; Lakatta, E.G.; AlGhatrif, M. Longitudinal Association between Serum Uric Acid and Arterial Stiffness: Results from the Baltimore Longitudinal Study of Aging. Hypertension 2017, 69, 228–235. [Google Scholar] [CrossRef]
- Liu, P.; Wang, H.; Zhang, F.; Chen, Y.; Wang, D.; Wang, Y. The Effects of Allopurinol on the Carotid Intima-media Thickness in Patients with Type 2 Diabetes and Asymptomatic Hyperuricemia: A Three-year Randomized Parallel-controlled Study. Intern. Med. 2015, 54, 2129–2137. [Google Scholar] [CrossRef]
- Higgins, P.; Walters, M.R.; Murray, H.M.; McArthur, K.; McConnachie, A.; Lees, K.R.; Dawson, J. Allopurinol reduces brachial and central blood pressure, and carotid intima-media thickness progression after ischaemic stroke and transient ischaemic attack: A randomised controlled trial. Heart 2014, 100, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Taguchi, I.; Teragawa, H.; Ishizaka, N.; Kanzaki, Y.; Tomiyama, H.; Sata, M.; Sezai, A.; Eguchi, K.; Kato, T.; et al. Febuxostat does not delay progression of carotid atherosclerosis in patients with asymptomatic hyperuricemia: A randomized, controlled trial. PLoS Med. 2020, 17, e1003095. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Toyoda, S.; Kato, T.; Yoshida, H.; Hamasaki, S.; Watarai, M.; Ishizu, T.; Ueda, S.; Inoue, T.; Node, K. Association between serum urate level and carotid atherosclerosis: An insight from a post hoc analysis of the PRIZE randomised clinical trial. RMD Open 2022, 8, e002226. [Google Scholar] [CrossRef] [PubMed]
- Maruhashi, T.; Higashi, Y.; Yoshida, H.; Tanaka, A.; Eguchi, K.; Tomiyama, H.; Kario, K.; Kato, T.; Oda, N.; Tahara, N.; et al. Long-Term Effect of Febuxostat on Endothelial Function in Patients with Asymptomatic Hyperuricemia: A Sub-Analysis of the PRIZE Study. Front. Cardiovasc. Med. 2022, 9, 882821. [Google Scholar] [CrossRef] [PubMed]
- Shiina, K.; Tomiyama, H.; Tanaka, A.; Yoshida, H.; Eguchi, K.; Kario, K.; Kato, T.; Teragawa, H.; Toyoda, S.; Ohishi, M.; et al. Differential effect of a xanthine oxidase inhibitor on arterial stiffness and carotid atherosclerosis: A subanalysis of the PRIZE study. Hypertens. Res. 2022, 45, 602–611. [Google Scholar] [CrossRef]
- Deng, G.; Qiu, Z.; Li, D.; Fang, Y.; Zhang, S. Effects of Allopurinol on Arterial Stiffness: A Meta-Analysis of Randomized Controlled Trials. Med. Sci. Monit. 2016, 22, 1389–1397. [Google Scholar] [CrossRef]
- Kario, K.; Nishizawa, M.; Kiuchi, M.; Kiyosue, A.; Tomita, F.; Ohtani, H.; Abe, Y.; Kuga, H.; Miyazaki, S.; Kasai, T.; et al. Comparative effects of topiroxostat and febuxostat on arterial properties in hypertensive patients with hyperuricemia. J. Clin. Hypertens. 2021, 23, 334–344. [Google Scholar] [CrossRef]
- Kuwabara, M.; Niwa, K.; Hisatome, I.; Nakagawa, T.; Roncal-Jimenez, C.A.; Andres-Hernando, A.; Bjornstad, P.; Jensen, T.; Sato, Y.; Milagres, T.; et al. Asymptomatic Hyperuricemia without Comorbidities Predicts Cardiometabolic Diseases: Five-Year Japanese Cohort Study. Hypertension 2017, 69, 1036–1044. [Google Scholar] [CrossRef]
- Miah, R.; Fariha, K.A.; Sony, S.A.; Ahmed, S.; Hasan, M.; Mou, A.D.; Barman, Z.; Hasan, A.; Mohanto, N.C.; Ali, N. Association of serum xanthine oxidase levels with hypertension: A study on Bangladeshi adults. Sci. Rep. 2022, 12, 21727. [Google Scholar] [CrossRef]
- Feig, D.I.; Soletsky, B.; Johnson, R.J. Effect of allopurinol on blood pressure of adolescents with newly diagnosed essential hypertension: A randomized trial. JAMA 2008, 300, 924–932. [Google Scholar] [CrossRef]
- Qu, L.H.; Jiang, H.; Chen, J.H. Effect of uric acid-lowering therapy on blood pressure: Systematic review and meta-analysis. Ann. Med. 2017, 49, 142–156. [Google Scholar] [CrossRef]
- Kimura, K.; Hosoya, T.; Uchida, S.; Inaba, M.; Makino, H.; Maruyama, S.; Ito, S.; Yamamoto, T.; Tomino, Y.; Ohno, I.; et al. Febuxostat Therapy for Patients with Stage 3 CKD and Asymptomatic Hyperuricemia: A Randomized Trial. Am. J. Kidney Dis. 2018, 72, 798–810. [Google Scholar] [CrossRef] [PubMed]
- Azegami, T.; Uchida, K.; Arima, F.; Sato, Y.; Awazu, M.; Inokuchi, M.; Murai-Takeda, A.; Itoh, H.; Tokumura, M.; Mori, M. Association of childhood anthropometric measurements and laboratory parameters with high blood pressure in young adults. Hypertens. Res. 2021, 44, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.; Chen, S.; Wang, P.; Xu, Q.; Zhang, Y.; Zhang, X.; Wu, S.; Luo, Y.; Wang, A. Temporal relationship between hyperuricemia and hypertension and its impact on future risk of cardiovascular disease. Eur. J. Intern. Med. 2023, 111, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Lozada, L.G.; Rodriguez-Iturbe, B.; Kelley, E.E.; Nakagawa, T.; Madero, M.; Feig, D.I.; Borghi, C.; Piani, F.; Cara-Fuentes, G.; Bjornstad, P.; et al. Uric Acid and Hypertension: An Update with Recommendations. Am. J. Hypertens. 2020, 33, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Yanai, H.; Katsuyama, H.; Hakoshima, M.; Adachi, H. Urate Transporter 1 Can Be a Therapeutic Target Molecule for Chronic Kidney Disease and Diabetic Kidney Disease: A Retrospective Longitudinal Study. Biomedicines 2023, 11, 567. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.J.; Choi, H.K.; Yeo, A.E.; Lipsky, P.E. Pegloticase Treatment Significantly Decreases Blood Pressure in Patients with Chronic Gout. Hypertension 2019, 74, 95–101. [Google Scholar] [CrossRef]
- Magee, L.A.; Brown, M.A.; Hall, D.R.; Gupte, S.; Hennessy, A.; Karumanchi, S.A.; Kenny, L.C.; McCarthy, F.; Myers, J.; Poon, L.C.; et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022, 27, 148–169. [Google Scholar] [CrossRef]
- Wu, P.; Green, M.; Myers, J.E. Hypertensive disorders of pregnancy. BMJ 2023, 381, e071653. [Google Scholar] [CrossRef]
- Khaliq, O.P.; Konoshita, T.; Moodley, J.; Naicker, T. The Role of Uric Acid in Preeclampsia: Is Uric Acid a Causative Factor or a Sign of Preeclampsia? Curr. Hypertens. Rep. 2018, 20, 80. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Roos-Hesselink, J.W.; Bauersachs, J.; Blomström-Lundqvist, C.; Cífková, R.; De Bonis, M.; Iung, B.; Johnson, M.R.; Kintscher, U.; Kranke, P.; et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur. Heart J. 2018, 39, 3165–3241. [Google Scholar] [CrossRef]
- Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet. Gynecol. 2020, 135, e237–e260. [CrossRef] [PubMed]
- Colmenares-Mejia, C.C.; Quintero-Lesmes, D.C.; Bautista-Niño, P.K.; Guío, E.; Paez, M.C.; Beltrán, M.; Williams, D.; Gray, K.J.; Casas, J.P.; Serrano, N.C. Uric acid and risk of pre-eclampsia: Results from a large case-control study and meta-analysis of prospective studies. Sci. Rep. 2023, 13, 3018. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Savitha, C. Estimation of Serum Uric Acid as an Indicator of Severity of Preeclampsia and Perinatal Outcome. J. Obstet. Gynaecol. India 2017, 67, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Piani, F.; Agnoletti, D.; Baracchi, A.; Scarduelli, S.; Verde, C.; Tossetta, G.; Montaguti, E.; Simonazzi, G.; Degli Esposti, D.; Borghi, C. Serum uric acid to creatinine ratio and risk of preeclampsia and adverse pregnancy outcomes. J. Hypertens. 2023, 41, 1333–1338. [Google Scholar] [CrossRef]
- Yue, C.; Ying, C.; Li, X. Association of first trimester serum uric acid with preeclampsia: An observational cohort study with propensity score matching. Hypertens. Res. 2023, 46, 377–385. [Google Scholar] [CrossRef]
- Khosla, K.; Heimberger, S.; Nieman, K.M.; Tung, A.; Shahul, S.; Staff, A.C.; Rana, S. Long-Term Cardiovascular Disease Risk in Women after Hypertensive Disorders of Pregnancy: Recent Advances in Hypertension. Hypertension 2021, 78, 927–935. [Google Scholar] [CrossRef]
- Goffin, S.M.; Derraik, J.G.B.; Groom, K.M.; Cutfield, W.S. Maternal pre-eclampsia and long-term offspring health: Is there a shadow cast? Pregnancy Hypertens. 2018, 12, 11–15. [Google Scholar] [CrossRef]
- Bobulescu, I.A.; Moe, O.W. Renal transport of uric acid: Evolving concepts and uncertainties. Adv. Chronic Kidney Dis. 2012, 19, 358–371. [Google Scholar] [CrossRef]
- Piani, F.; Johnson, R.J. Does gouty nephropathy exist, and is it more common than we think? Kidney Int. 2021, 99, 31–33. [Google Scholar] [CrossRef]
- Stack, A.G.; Johnson, M.E.; Blak, B.; Klein, A.; Carpenter, L.; Morlock, R.; Maguire, A.R.; Parsons, V.L. Gout and the risk of advanced chronic kidney disease in the UK health system: A national cohort study. BMJ Open 2019, 9, e031550. [Google Scholar] [CrossRef]
- Bardin, T.; Nguyen, Q.D.; Tran, K.M.; Le, N.H.; Do, M.D.; Richette, P.; Letavernier, E.; Correas, J.M.; Resche-Rigon, M. A cross-sectional study of 502 patients found a diffuse hyperechoic kidney medulla pattern in patients with severe gout. Kidney Int. 2021, 99, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Kohagura, K.; Kochi, M.; Miyagi, T.; Kinjyo, T.; Maehara, Y.; Nagahama, K.; Sakima, A.; Iseki, K.; Ohya, Y. An association between uric acid levels and renal arteriolopathy in chronic kidney disease: A biopsy-based study. Hypertens. Res. 2013, 36, 43–49. [Google Scholar] [CrossRef] [PubMed]
- CKD Work Group. Chapter 3: Management of progression and complications of CKD. Kidney Int. Suppl. 2013, 3, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Sircar, D.; Chatterjee, S.; Waikhom, R.; Golay, V.; Raychaudhury, A.; Chatterjee, S.; Pandey, R. Efficacy of Febuxostat for Slowing the GFR Decline in Patients with CKD and Asymptomatic Hyperuricemia: A 6-Month, Double-Blind, Randomized, Placebo-Controlled Trial. Am. J. Kidney Dis. 2015, 66, 945–950. [Google Scholar] [CrossRef]
- Wada, T.; Hosoya, T.; Honda, D.; Sakamoto, R.; Narita, K.; Sasaki, T.; Okui, D.; Kimura, K. Uric acid-lowering and renoprotective effects of topiroxostat, a selective xanthine oxidoreductase inhibitor, in patients with diabetic nephropathy and hyperuricemia: A randomized, double-blind, placebo-controlled, parallel-group study (UPWARD study). Clin. Exp. Nephrol. 2018, 22, 860–870. [Google Scholar] [CrossRef]
- Kataoka, H.; Mochizuki, T.; Ohara, M.; Tsuruta, Y.; Iwasa, N.; Yoshida, R.; Tsuchiya, K.; Nitta, K.; Kimura, K.; Hosoya, T.; et al. Urate-lowering therapy for CKD patients with asymptomatic hyperuricemia without proteinuria elucidated by attribute-based research in the FEATHER Study. Sci. Rep. 2022, 12, 3784. [Google Scholar] [CrossRef]
- Kojima, S.; Matsui, K.; Hiramitsu, S.; Hisatome, I.; Waki, M.; Uchiyama, K.; Yokota, N.; Tokutake, E.; Wakasa, Y.; Jinnouchi, H.; et al. Febuxostat for Cerebral and CaRdiorenovascular Events PrEvEntion StuDy. Eur. Heart J. 2019, 40, 1778–1786. [Google Scholar] [CrossRef]
- Doria, A.; Galecki, A.T.; Spino, C.; Pop-Busui, R.; Cherney, D.Z.; Lingvay, I.; Parsa, A.; Rossing, P.; Sigal, R.J.; Afkarian, M.; et al. Serum Urate Lowering with Allopurinol and Kidney Function in Type 1 Diabetes. N. Engl. J. Med. 2020, 382, 2493–2503. [Google Scholar] [CrossRef]
- Badve, S.V.; Pascoe, E.M.; Tiku, A.; Boudville, N.; Brown, F.G.; Cass, A.; Clarke, P.; Dalbeth, N.; Day, R.O.; de Zoysa, J.R.; et al. Effects of Allopurinol on the Progression of Chronic Kidney Disease. N. Engl. J. Med. 2020, 382, 2504–2513. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, Z.; Zhou, J.; Chen, Z.; Li, Y.; Li, S.; Zhao, H.; Badve, S.V.; Lv, J. Effect of Urate-Lowering Therapy on Cardiovascular and Kidney Outcomes: A Systematic Review and Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2020, 15, 1576–1586. [Google Scholar] [CrossRef]
- Hare, J.M.; Johnson, R.J. Uric acid predicts clinical outcomes in heart failure: Insights regarding the role of xanthine oxidase and uric acid in disease pathophysiology. Circulation 2003, 107, 1951–1953. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Tanaka, A.; Node, K.; Kobayashi, Y. Uric acid and cardiovascular disease: A clinical review. J. Cardiol. 2021, 78, 51–57. [Google Scholar] [CrossRef]
- Stone, M.L.; Richardson, M.R.; Guevara, L.; Rand, B.G.; Churilla, J.R. Elevated Serum Uric Acid and Self-Reported Heart Failure in US Adults: 2007–2016 National Health and Nutrition Examination Survey. Cardiorenal Med. 2019, 9, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Akashi, N.; Kuwabara, M.; Matoba, T.; Kohro, T.; Oba, Y.; Kabutoya, T.; Imai, Y.; Kario, K.; Kiyosue, A.; Mizuno, Y.; et al. Hyperuricemia predicts increased cardiovascular events in patients with chronic coronary syndrome after percutaneous coronary intervention: A nationwide cohort study from Japan. Front. Cardiovasc. Med. 2022, 9, 1062894. [Google Scholar] [CrossRef] [PubMed]
- Hare, J.M.; Mangal, B.; Brown, J.; Fisher, C., Jr.; Freudenberger, R.; Colucci, W.S.; Mann, D.L.; Liu, P.; Givertz, M.M.; Schwarz, R.P.; et al. Impact of oxypurinol in patients with symptomatic heart failure. Results of the OPT-CHF study. J. Am. Coll. Cardiol. 2008, 51, 2301–2309. [Google Scholar] [CrossRef]
- Givertz, M.M.; Anstrom, K.J.; Redfield, M.M.; Deswal, A.; Haddad, H.; Butler, J.; Tang, W.H.; Dunlap, M.E.; LeWinter, M.M.; Mann, D.L.; et al. Effects of Xanthine Oxidase Inhibition in Hyperuricemic Heart Failure Patients: The Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) Study. Circulation 2015, 131, 1763–1771. [Google Scholar] [CrossRef]
- Xu, H.; Liu, Y.; Meng, L.; Wang, L.; Liu, D. Effect of Uric Acid-Lowering Agents on Patients with Heart Failure: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Front. Cardiovasc. Med. 2021, 8, 639392. [Google Scholar] [CrossRef]
- Mackenzie, I.S.; Ford, I.; Nuki, G.; Hallas, J.; Hawkey, C.J.; Webster, J.; Ralston, S.H.; Walters, M.; Robertson, M.; De Caterina, R.; et al. Long-term cardiovascular safety of febuxostat compared with allopurinol in patients with gout (FAST): A multicentre, prospective, randomised, open-label, non-inferiority trial. Lancet 2020, 396, 1745–1757. [Google Scholar] [CrossRef]
- Yokota, T.; Fukushima, A.; Kinugawa, S.; Okumura, T.; Murohara, T.; Tsutsui, H. Randomized Trial of Effect of Urate-Lowering Agent Febuxostat in Chronic Heart Failure Patients with Hyperuricemia (LEAF-CHF). Int. Heart J. 2018, 59, 976–982. [Google Scholar] [CrossRef]
- Kojima, S.; Sakamoto, T.; Ishihara, M.; Kimura, K.; Miyazaki, S.; Yamagishi, M.; Tei, C.; Hiraoka, H.; Sonoda, M.; Tsuchihashi, K.; et al. Prognostic usefulness of serum uric acid after acute myocardial infarction (the Japanese Acute Coronary Syndrome Study). Am. J. Cardiol. 2005, 96, 489–495. [Google Scholar] [CrossRef]
- Noman, A.; Ang, D.S.; Ogston, S.; Lang, C.C.; Struthers, A.D. Effect of high-dose allopurinol on exercise in patients with chronic stable angina: A randomised, placebo controlled crossover trial. Lancet 2010, 375, 2161–2167. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, I.S.; Hawkey, C.J.; Ford, I.; Greenlaw, N.; Pigazzani, F.; Rogers, A.; Struthers, A.D.; Begg, A.G.; Wei, L.; Avery, A.J.; et al. Allopurinol versus usual care in UK patients with ischaemic heart disease (ALL-HEART): A multicentre, prospective, randomised, open-label, blinded-endpoint trial. Lancet 2022, 400, 1195–1205. [Google Scholar] [CrossRef]
- Martinon, F.; Petrilli, V.; Mayor, A.; Tardivel, A.; Tschopp, J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 2006, 440, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Klauser, A.S.; Halpern, E.J.; Strobl, S.; Gruber, J.; Feuchtner, G.; Bellmann-Weiler, R.; Weiss, G.; Stofferin, H.; Jaschke, W. Dual-Energy Computed Tomography Detection of Cardiovascular Monosodium Urate Deposits in Patients with Gout. JAMA Cardiol. 2019, 4, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Letsas, K.P.; Korantzopoulos, P.; Filippatos, G.S.; Mihas, C.C.; Markou, V.; Gavrielatos, G.; Efremidis, M.; Sideris, A.; Kardaras, F. Uric acid elevation in atrial fibrillation. Hellenic J. Cardiol. 2010, 51, 209–213. [Google Scholar] [PubMed]
- Kawasoe, S.; Kubozono, T.; Yoshifuku, S.; Ojima, S.; Miyata, M.; Miyahara, H.; Maenohara, S.; Ohishi, M. Uric Acid Level and New-Onset Atrial Fibrillation in the Japanese General Population—Longitudinal Study. Circ. J. 2018, 83, 156–163. [Google Scholar] [CrossRef]
- Hong, M.; Park, J.W.; Yang, P.S.; Hwang, I.; Kim, T.H.; Yu, H.T.; Uhm, J.S.; Joung, B.; Lee, M.H.; Jee, S.H.; et al. A mendelian randomization analysis: The causal association between serum uric acid and atrial fibrillation. Eur. J. Clin. Investig. 2020, 50, e13300. [Google Scholar] [CrossRef]
- Tamariz, L.; Agarwal, S.; Soliman, E.Z.; Chamberlain, A.M.; Prineas, R.; Folsom, A.R.; Ambrose, M.; Alonso, A. Association of serum uric acid with incident atrial fibrillation (from the Atherosclerosis Risk in Communities [ARIC] study). Am. J. Cardiol. 2011, 108, 1272–1276. [Google Scholar] [CrossRef]
- Gao, Z.; Shi, H.; Xu, W.; Guan, Z.; Su, X.; Guo, N.; Ma, H. Hyperuricemia Increases the Risk of Atrial Fibrillation: A Systematic Review and Meta-Analysis. Int. J. Endocrinol. 2022, 2022, 8172639. [Google Scholar] [CrossRef]
- Canpolat, U.; Aytemir, K.; Yorgun, H.; Sahiner, L.; Kaya, E.B.; Cay, S.; Topaloglu, S.; Aras, D.; Oto, A. Usefulness of serum uric acid level to predict atrial fibrillation recurrence after cryoballoon-based catheter ablation. Europace 2014, 16, 1731–1737. [Google Scholar] [CrossRef]
- Chen, Y.; Wu, Y.; Chu, X.; Wang, M. Meta-analysis of the correlation between recurrence of atrial fibrillation and serum uric acid level after radiofrequency ablation. Am. J. Transl. Res. 2022, 14, 8793–8799. [Google Scholar] [PubMed]
- Nodera, M.; Suzuki, H.; Matsumoto, Y.; Kamioka, M.; Kaneshiro, T.; Yoshihisa, A.; Ohira, T.; Takeishi, Y. Association between Serum Uric Acid Level and Ventricular Tachyarrhythmia in Heart Failure Patients with Implantable Cardioverter-Defibrillator. Cardiology 2018, 140, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Rigolon, R.; Pichiri, I.; Morani, G.; Bonapace, S.; Dugo, C.; Zoppini, G.; Bonora, E.; Targher, G. Relation of elevated serum uric acid levels to first-degree heart block and other cardiac conduction defects in hospitalized patients with type 2 diabetes. J. Diabetes Complicat. 2017, 31, 1691–1697. [Google Scholar] [CrossRef]
- Singh, J.A.; Yu, S. Allopurinol and the risk of atrial fibrillation in the elderly: A study using Medicare data. Ann. Rheum. Dis. 2017, 76, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Cleveland, J.D. Comparative effectiveness of allopurinol and febuxostat for the risk of atrial fibrillation in the elderly: A propensity-matched analysis of Medicare claims data. Eur. Heart J. 2019, 40, 3046–3054. [Google Scholar] [CrossRef] [PubMed]
- Otani, N.; Hoshiyama, E.; Ouchi, M.; Takekawa, H.; Suzuki, K. Uric acid and neurological disease: A narrative review. Front. Neurol. 2023, 14, 1164756. [Google Scholar] [CrossRef]
- Mentis, A.A.; Dardiotis, E.; Efthymiou, V.; Chrousos, G.P. Non-genetic risk and protective factors and biomarkers for neurological disorders: A meta-umbrella systematic review of umbrella reviews. BMC Med. 2021, 19, 6. [Google Scholar] [CrossRef]
- Dong, Y.; Shi, H.; Chen, X.; Fu, K.; Li, J.; Chen, H.; Teng, W.; Tian, L. Serum uric acid and risk of stroke: A dose-response meta-analysis. J. Clin. Biochem. Nutr. 2021, 68, 221–227. [Google Scholar] [CrossRef]
- Zheng, S.; Luo, Y.; Miao, Q.; Cheng, Z.; Liu, Y.; Lv, K.; Zhang, D.; Yin, C.; Wang, M.; Bai, Y. Serum Uric Acid Levels and Their Changes and Risk of Stroke: A 7-Year Prospective Cohort Study in Northwest China. Cerebrovasc. Dis. 2022, 51, 225–234. [Google Scholar] [CrossRef]
- Chaudhary, N.S.; Bridges, S.L., Jr.; Saag, K.G.; Rahn, E.J.; Curtis, J.R.; Gaffo, A.; Limdi, N.A.; Levitan, E.B.; Singh, J.A.; Colantonio, L.D.; et al. Severity of Hypertension Mediates the Association of Hyperuricemia with Stroke in the REGARDS Case Cohort Study. Hypertension 2020, 75, 246–256. [Google Scholar] [CrossRef]
- Kamei, K.; Konta, T.; Hirayama, A.; Ichikawa, K.; Kubota, I.; Fujimoto, S.; Iseki, K.; Moriyama, T.; Yamagata, K.; Tsuruya, K.; et al. Associations between serum uric acid levels and the incidence of nonfatal stroke: A nationwide community-based cohort study. Clin. Exp. Nephrol. 2017, 21, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wang, Y.; Wang, K.; Yin, R.; Pan, X.; Ma, A. Association between uric acid and the prognosis of acute ischemic stroke: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3016–3023. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Muraki, I.; Imano, H.; Cui, R.; Yamagishi, K.; Umesawa, M.; Hayama-Terada, M.; Ohira, T.; Kiyama, M.; Okada, T.; et al. Serum uric acid and risk of stroke and its types: The Circulatory Risk in Communities Study (CIRCS). Hypertens. Res. 2020, 43, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Yen, F.S.; Hsu, C.C.; Li, H.L.; Wei, J.C.; Hwu, C.M. Urate-lowering therapy may mitigate the risks of hospitalized stroke and mortality in patients with gout. PLoS ONE 2020, 15, e0234909. [Google Scholar] [CrossRef]
- Wen, M.; Zhou, B.; Chen, Y.H.; Ma, Z.L.; Gou, Y.; Zhang, C.L.; Yu, W.F.; Jiao, L. Serum uric acid levels in patients with Parkinson’s disease: A meta-analysis. PLoS ONE 2017, 12, e0173731. [Google Scholar] [CrossRef] [PubMed]
- van Wamelen, D.J.; Taddei, R.N.; Calvano, A.; Titova, N.; Leta, V.; Shtuchniy, I.; Jenner, P.; Martinez-Martin, P.; Katunina, E.; Chaudhuri, K.R. Serum Uric Acid Levels and Non-Motor Symptoms in Parkinson’s Disease. J. Park. Dis. 2020, 10, 1003–1010. [Google Scholar] [CrossRef]
- Seifar, F.; Dinasarapu, A.R.; Jinnah, H.A. Uric Acid in Parkinson’s Disease: What Is the Connection? Mov. Disord. 2022, 37, 2173–2183. [Google Scholar] [CrossRef]
- Parkinson Study Group, S.-P.D.I.; Schwarzschild, M.A.; Ascherio, A.; Casaceli, C.; Curhan, G.C.; Fitzgerald, R.; Kamp, C.; Lungu, C.; Macklin, E.A.; Marek, K.; et al. Effect of Urate-Elevating Inosine on Early Parkinson Disease Progression: The SURE-PD3 Randomized Clinical Trial. JAMA 2021, 326, 926–939. [Google Scholar] [CrossRef]
- Scheepers, L.; Jacobsson, L.T.H.; Kern, S.; Johansson, L.; Dehlin, M.; Skoog, I. Urate and risk of Alzheimer’s disease and vascular dementia: A population-based study. Alzheimers Dement. 2019, 15, 754–763. [Google Scholar] [CrossRef]
- Boccardi, V.; Carino, S.; Marinelli, E.; Lapenna, M.; Caironi, G.; Bianco, A.R.; Cecchetti, R.; Ruggiero, C.; Mecocci, P.; Re, G.S.G. Uric acid and late-onset Alzheimer’s disease: Results from the ReGAl 2.0 project. Aging Clin. Exp. Res. 2021, 33, 361–366. [Google Scholar] [CrossRef]
- Alam, A.B.; Wu, A.; Power, M.C.; West, N.A.; Alonso, A. Associations of serum uric acid with incident dementia and cognitive decline in the ARIC-NCS cohort. J. Neurol. Sci. 2020, 414, 116866. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, F.C.; Soares, M.S.P.; Blodorn, E.B.; Domingues, W.B.; Reichert, K.P.; Zago, A.M.; Carvalho, F.B.; Gutierres, J.M.; Goncales, R.A.; da Cruz Fernandes, M.; et al. Investigating the Effect of Inosine on Brain Purinergic Receptors and Neurotrophic and Neuroinflammatory Parameters in an Experimental Model of Alzheimer’s Disease. Mol. Neurobiol. 2022, 59, 841–855. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Hu, W.; Wang, J.; Qian, W.; Xiao, H. Low serum uric acid levels in patients with multiple sclerosis and neuromyelitis optica: An updated meta-analysis. Mult. Scler. Relat. Disord. 2016, 9, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Munoz Garcia, D.; Midaglia, L.; Martinez Vilela, J.; Marin Sanchez, M.; Lopez Gonzalez, F.J.; Arias Gomez, M.; Dapena Bolano, D.; Iglesias Castanon, A.; Alonso Alonso, M.; Romero Lopez, J. Associated Inosine to interferon: Results of a clinical trial in multiple sclerosis. Acta Neurol. Scand. 2015, 131, 405–410. [Google Scholar] [CrossRef]
- Kwon, H.S.; Park, Y.; Kim, J.H.; Kim, S.H.; Jun, J.B.; Park, S.; Kang, D.R.; Choi, H. Prevalence of motor neuron diseases in gout patients: A nationwide population-based cohort study. Neurol. Sci. 2023, 44, 593–600. [Google Scholar] [CrossRef]
- Tang, J.; Yang, Y.; Gong, Z.; Li, Z.; Huang, L.; Ding, F.; Liu, M.; Zhang, M. Plasma Uric Acid Helps Predict Cognitive Impairment in Patients with Amyotrophic Lateral Sclerosis. Front. Neurol. 2021, 12, 789840. [Google Scholar] [CrossRef]
- Xu, L.Q.; Hu, W.; Guo, Q.F.; Xu, G.R.; Wang, N.; Zhang, Q.J. Serum Uric Acid Levels Predict Mortality Risk in Male Amyotrophic Lateral Sclerosis Patients. Front. Neurol. 2021, 12, 602663. [Google Scholar] [CrossRef]
- Ko, W.F.; Helzlsouer, K.J.; Comstock, G.W. Serum albumin, bilirubin, and uric acid and the anatomic site-specific incidence of colon cancer. J. Natl. Cancer Inst. 1994, 86, 1874–1875. [Google Scholar] [CrossRef]
- Kuhn, T.; Sookthai, D.; Graf, M.E.; Schubel, R.; Freisling, H.; Johnson, T.; Katzke, V.; Kaaks, R. Albumin, bilirubin, uric acid and cancer risk: Results from a prospective population-based study. Br. J. Cancer 2017, 117, 1572–1579. [Google Scholar] [CrossRef]
- Yamauchi, T.; Negoro, E.; Lee, S.; Takai, M.; Matsuda, Y.; Takagi, K.; Kishi, S.; Tai, K.; Hosono, N.; Tasaki, T.; et al. A high serum uric acid level is associated with poor prognosis in patients with acute myeloid leukemia. Anticancer. Res. 2013, 33, 3947–3951. [Google Scholar]
- Li, Y.; Shi, P.; Xie, Y.; Qian, S. Serum uric acid level is a prognostic indicator and improves the predictive ability of the IPI score in diffuse large B-cell lymphoma. Int. J. Clin. Exp. Med. 2018, 11, 2223–2231. [Google Scholar]
- Cairo, M.S.; Bishop, M. Tumour lysis syndrome: New therapeutic strategies and classification. Br. J. Haematol. 2004, 127, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Coiffier, B.; Altman, A.; Pui, C.H.; Younes, A.; Cairo, M.S. Guidelines for the management of pediatric and adult tumor lysis syndrome: An evidence-based review. J. Clin. Oncol. 2008, 26, 2767–2778. [Google Scholar] [CrossRef] [PubMed]
- Cairo, M.S.; Coiffier, B.; Reiter, A.; Younes, A.; Panel, T.L.S.E. Recommendations for the evaluation of risk and prophylaxis of tumour lysis syndrome (TLS) in adults and children with malignant diseases: An expert TLS panel consensus. Br. J. Haematol. 2010, 149, 578–586. [Google Scholar] [CrossRef]
- Howard, S.C.; Trifilio, S.; Gregory, T.K.; Baxter, N.; McBride, A. Tumor lysis syndrome in the era of novel and targeted agents in patients with hematologic malignancies: A systematic review. Ann. Hematol. 2016, 95, 563–573. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).