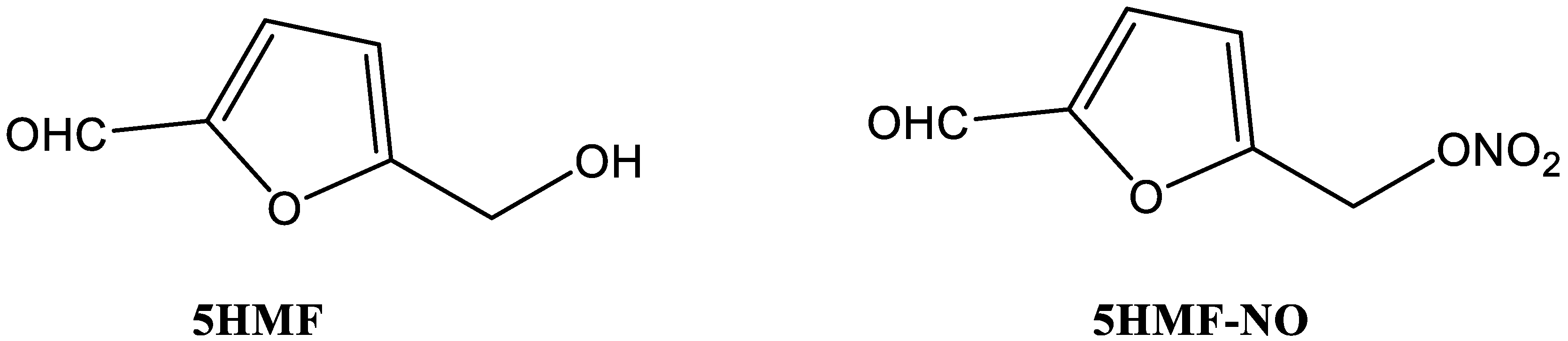
Design, Synthesis, and Antisickling Investigation of a Nitric Oxide-Releasing Prodrug of 5HMF for the Treatment of Sickle Cell Disease
Abstract
1. Introduction
2. Materials and Method
2.1. Study Approvals
2.2. Chemistry
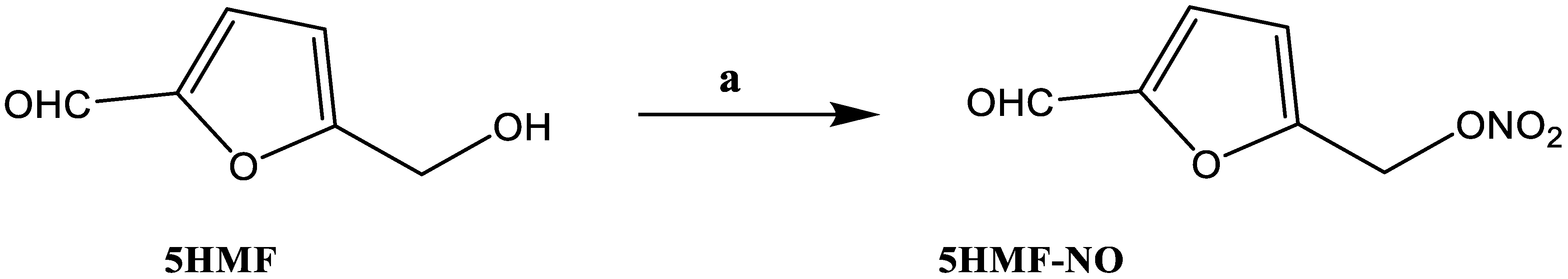
Synthesis of 5-Nitrooxymethyl Furfural (5HMF-NO)
2.3. Study of NO Release from 5HMF-NO in Whole Blood
2.4. In Vitro Hb Modification, Oxygen Equilibrium and Antisickling Studies Using Human Homozygous Sickle Cell (SS) Blood
2.5. Crystallographic Study of Hb Co-Crystallized with 5HMF-NO
3. Results and Discussion
3.1. Chemistry
3.2. 5HMF-NO Is Capable of Releasing NO
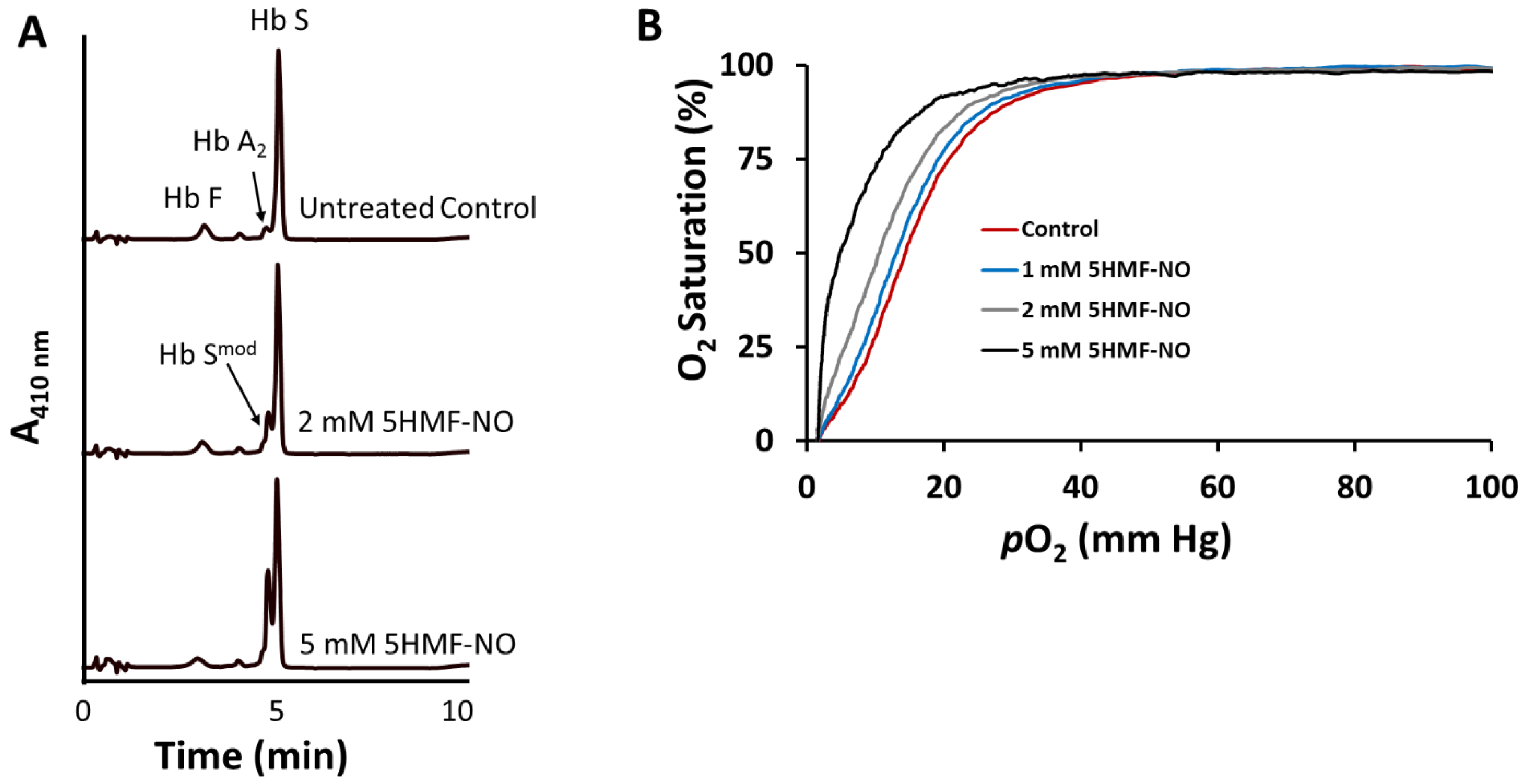
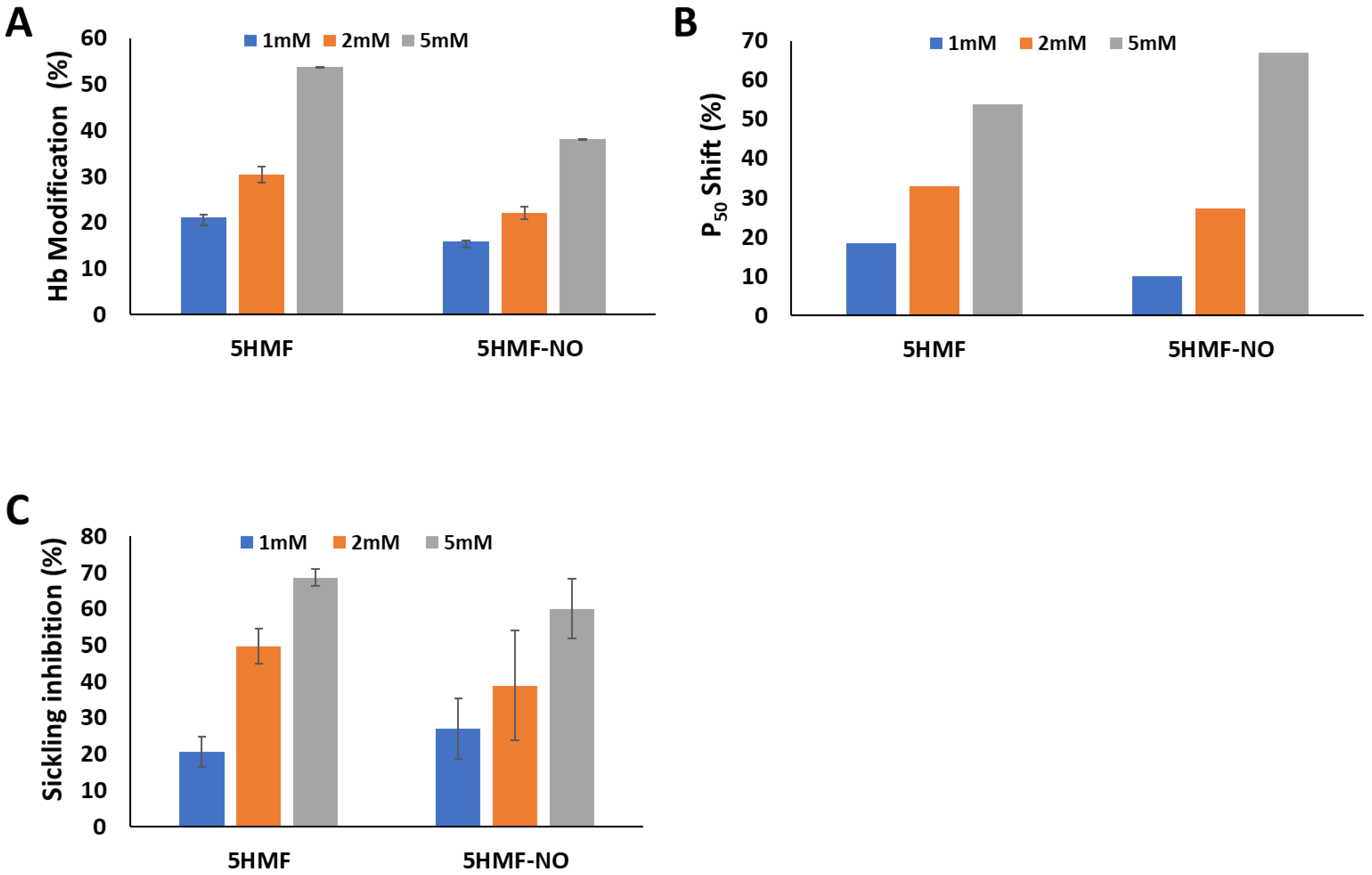
3.3. 5HMF-NO Forms Adduct with Hb to Increase the Affinity of Hb for Oxygen and Prevent Hypoxia-Induced RBC Sickling
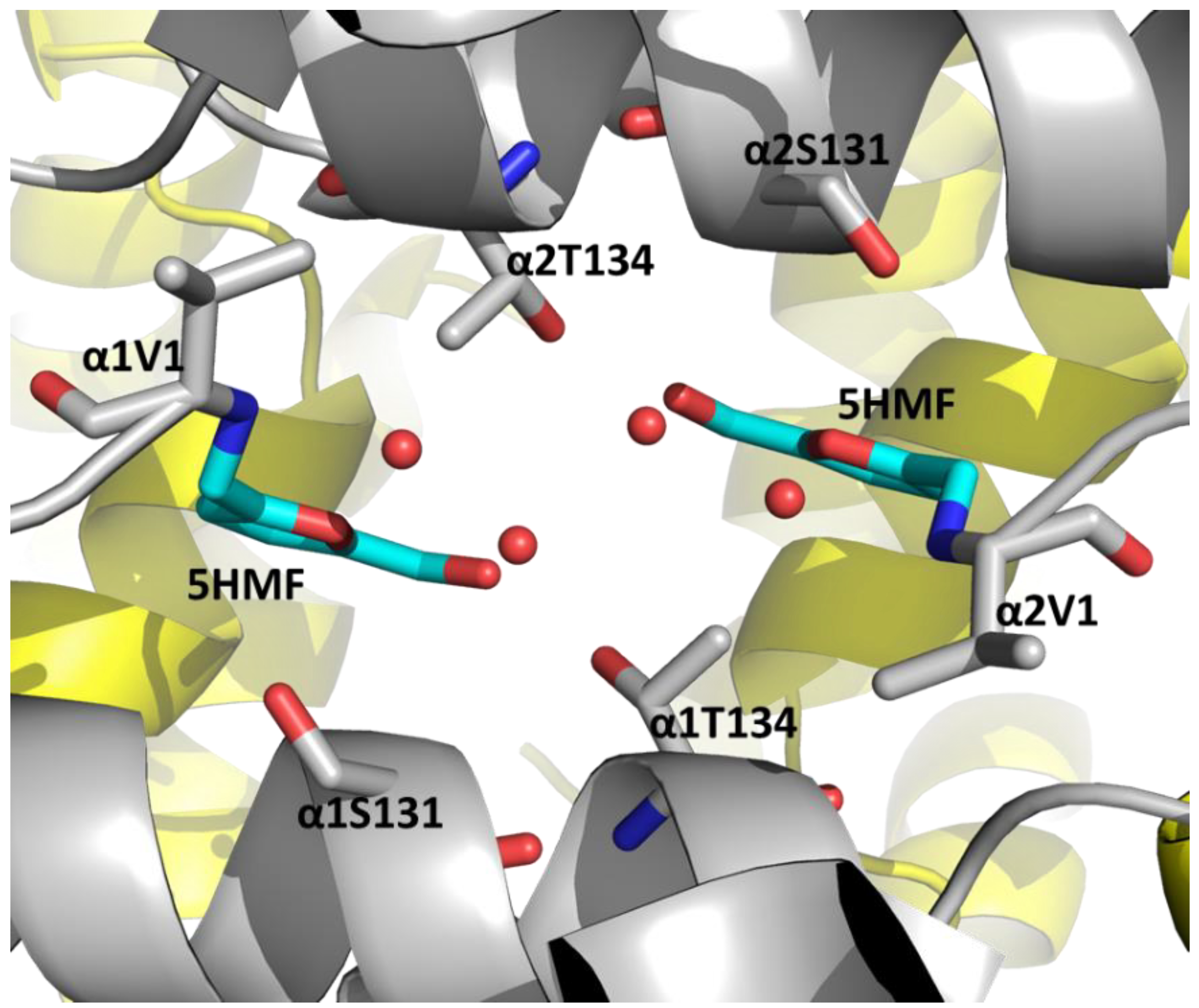
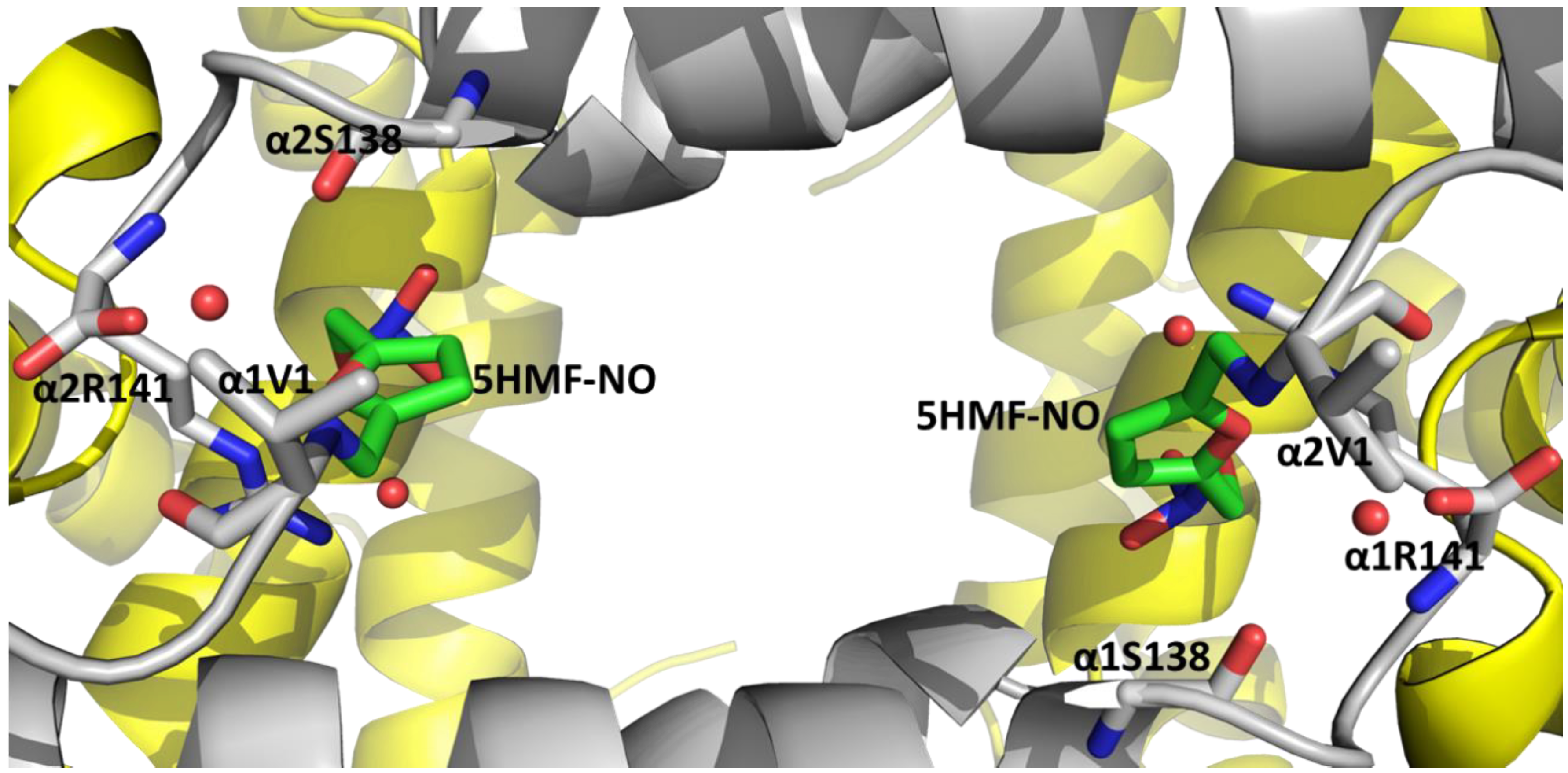
3.4. 5HMF-NO When Co-Crystallized with Hb Binds to the T-State as 5HMF-NO and R2-State Hb as 5HMF
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Pauling, L.; Itano, H.A.; Singer, S.J.; Wells, I.C. Sickle cell anemia, a molecular disease. Science 1949, 110, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Ghatge, M.S.; Ahmed, M.H.; Omar, A.S.M.; Pagare, P.P.; Rosef, S.; Kellogg, G.E.; Abdulmalik, O.; Safo, M.K. Crystal structure of carbonmonoxy sickle hemoglobin in R-state conformation. J. Struct. Biol. 2016, 194, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Cretegny, I.; Edelstein, S.J. Double strand packing in hemoglobin S fibers. J. Mol. Biol. 1993, 230, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Ferrone, F.A. Polymerization and sickle cell disease: A molecular view. Microcirculation 2004, 11, 115–128. [Google Scholar] [CrossRef]
- Thein, M.S.; Igbineweka, N.E.; Thein, S.L. Sickle cell disease in the older adult. Pathology 2017, 49, 1–9. [Google Scholar] [CrossRef]
- Chaturvedi, S.; DeBaun, M.R. Evolution of sickle cell disease from a life-threatening disease of children to a chronic disease of adults: The last 40 years. Am. J. Hematol. 2016, 91, 5–14. [Google Scholar] [CrossRef]
- Jin, R.C.; Loscalzo, J. Vascular nitric oxide: Formation and function. J. Blood Med. 2010, 1, 147. [Google Scholar]
- Mack, A.K.; Kato, G.J. Sickle cell disease and nitric oxide: A paradigm shift? Int. J. Biochem. Cell Biol. 2006, 38, 1237–1243. [Google Scholar] [CrossRef]
- Kassim, A.A.; DeBaun, M.R. Sickle cell disease, vasculopathy, and therapeutics. Annu. Rev. Med. 2013, 64, 451–466. [Google Scholar] [CrossRef]
- Head, C.A.; Brugnara, C.; Martinez-Ruiz, R.; Kacmarek, R.M.; Bridges, K.R.; Kuter, D.; Bloch, K.D.; Zapol, W.M. Low concentrations of nitric oxide increase oxygen affinity of sickle erythrocytes in vitro and in vivo. J. Clin. Investig. 1997, 100, 1193–1198. [Google Scholar] [CrossRef]
- Steppan, J.; Tran, H.T.; Bead, V.R.; Oh, Y.J.; Sikka, G.; Bivalacqua, T.J.; Burnett, A.L.; Berkowitz, D.E.; Santhanam, L. Arginase inhibition reverses endothelial dysfunction, pulmonary hypertension and vascular stiffness in transgenic sickle cell mice. Anesth. Analg. 2016, 123, 652. [Google Scholar] [CrossRef]
- Iyamu, E.W.; Cecil, R.; Parkin, L.; Woods, G.; Ohene-Frempong, K.; Asakura, T. Modulation of erythrocyte arginase activity in sickle cell disease patients during hydroxyurea therapy. Br. J. Haematol. 2005, 131, 389–394. [Google Scholar] [CrossRef]
- Kahn, M.J.; Maley, J.H.; Lasker, G.F.; Kadowitz, P.J. Updated role of nitric oxide in disorders of erythrocyte function. Cardiovasc. Haematol. Disord. Drug Targets 2013, 13, 83–87. [Google Scholar] [CrossRef][Green Version]
- Kim-Shapiro, D.B.; Gladwin, M.T. Nitric oxide pathology and therapeutics in sickle cell disease. Clin. Hemorheol. Microcirc. 2018, 68, 223–237. [Google Scholar] [CrossRef]
- Mvalo, T.; Topazian, H.; Kamthunzi, P.; Chen, J.; Kambalame, I.; Mafunga, P.; Mumba, N.; Chiume-Chiphaliwali, M.; Paseli, K.; Key, N. Increasing hydroxyurea use in children with sickle cell disease at Kamuzu Central Hospital, Malawi. Blood Adv. 2018, 2, 30. [Google Scholar] [CrossRef]
- Zhu, X.; Hu, T.; Ho, M.H.; Wang, Y.; Yu, M.; Patel, N.; Pi, W.; Choi, J.-H.; Xu, H.; Ganapathy, V. Hydroxyurea differentially modulates activator and repressors of γ-globin gene in erythroblasts of responsive and non-responsive patients with sickle cell disease in correlation with Index of Hydroxyurea Responsiveness. Haematologica 2017, 102, 1995. [Google Scholar] [CrossRef]
- L-glutamine (Endari) for sickle cell disease. Med. Lett. Drugs Ther. 2018, 60, 21–22.
- Ataga, K.I.; Kutlar, A.; Kanter, J.; Liles, D.; Cancado, R.; Friedrisch, J.; Guthrie, T.H.; Knight-Madden, J.; Alvarez, O.A.; Gordeuk, V.R. Crizanlizumab for the prevention of pain crises in sickle cell disease. N. Engl. J. Med. 2017, 376, 429–439. [Google Scholar] [CrossRef]
- Hutchaleelaha, A.; Patel, M.; Silva, A.; Oksenberg, D.; Metcalf, B. GBT440 demonstrates high specificity for red blood cells in nonclinical species. Blood 2015, 126, 2172. [Google Scholar] [CrossRef]
- Metcalf, B.; Chuang, C.; Dufu, K.; Patel, M.P.; Silva-Garcia, A.; Johnson, C.; Lu, Q.; Partridge, J.R.; Patskovska, L.; Patskovsky, Y. Discovery of GBT440, an orally bioavailable R-state stabilizer of sickle cell hemoglobin. ACS Med. Chem. Lett. 2017, 8, 321–326. [Google Scholar] [CrossRef]
- Oksenberg, D.; Dufu, K.; Patel, M.P.; Chuang, C.; Li, Z.; Xu, Q.; Silva-Garcia, A.; Zhou, C.; Hutchaleelaha, A.; Patskovska, L. GBT 440 increases haemoglobin oxygen affinity, reduces sickling and prolongs RBC half-life in a murine model of sickle cell disease. Br. J. Haematol. 2016, 175, 141–153. [Google Scholar] [CrossRef]
- Vichinsky, E.; Hoppe, C.C.; Ataga, K.I.; Ware, R.E.; Nduba, V.; El-Beshlawy, A.; Hassab, H.; Achebe, M.M.; Alkindi, S.; Brown, R.C.; et al. A Phase 3 Randomized Trial of Voxelotor in Sickle Cell Disease. N. Engl. J. Med. 2019, 381, 509–519. [Google Scholar] [CrossRef]
- Safo, M.K.; Ahmed, M.H.; Ghatge, M.S.; Boyiri, T. Hemoglobin–ligand binding: Understanding Hb function and allostery on atomic level. Biochim. Biophys. Acta 2011, 1814, 797–809. [Google Scholar] [CrossRef] [PubMed]
- Nnamani, I.N.; Joshi, G.S.; Danso-Danquah, R.; Abdulmalik, O.; Asakura, T.; Abraham, D.J.; Safo, M.K. Pyridyl derivatives of benzaldehyde as potential antisickling agents. Chem. Biodivers. 2008, 5, 1762–1769. [Google Scholar] [CrossRef]
- Oder, E.; Safo, M.K.; Abdulmalik, O.; Kato, G.J. New developments in anti-sickling agents: Can drugs directly prevent the polymerization of sickle haemoglobin in vivo? Br. J. Haematol. 2016, 175, 24–30. [Google Scholar] [CrossRef]
- Abdulmalik, O.; Safo, M.K.; Chen, Q.; Yang, J.; Brugnara, C.; Ohene-Frempong, K.; Abraham, D.J.; Asakura, T. 5-hydroxymethyl-2-furfural modifies intracellular sickle haemoglobin and inhibits sickling of red blood cells. Br. J. Haematol. 2005, 128, 552–561. [Google Scholar] [CrossRef]
- Safo, M.K.; Abdulmalik, O.; Danso-Danquah, R.; Burnett, J.C.; Nokuri, S.; Joshi, G.S.; Musayev, F.N.; Asakura, T.; Abraham, D.J. Structural basis for the potent antisickling effect of a novel class of five-membered heterocyclic aldehydic compounds. J. Med. Chem. 2004, 47, 4665–4676. [Google Scholar] [CrossRef]
- Abdulmalik, O.; Ghatge, M.S.; Musayev, F.N.; Parikh, A.; Chen, Q.; Yang, J.; Nnamani, I.; Danso-Danquah, R.; Eseonu, D.N.; Asakura, T. Crystallographic analysis of human hemoglobin elucidates the structural basis of the potent and dual antisickling activity of pyridyl derivatives of vanillin. Acta Crystallogr. D Biol. Crystallogr. 2011, 67, 920–928. [Google Scholar] [CrossRef]
- Abdulmalik, O.; Pagare, P.P.; Huang, B.; Xu, G.G.; Ghatge, M.S.; Xu, X.; Chen, Q.; Anabaraonye, N.; Musayev, F.N.; Omar, A.M.; et al. VZHE-039, a novel antisickling agent that prevents erythrocyte sickling under both hypoxic and anoxic conditions. Sci. Rep. 2020, 10, 20277. [Google Scholar] [CrossRef]
- Pagare, P.P.; Ghatge, M.S.; Musayev, F.N.; Deshpande, T.M.; Chen, Q.; Braxton, C.; Kim, S.; Venitz, J.; Zhang, Y.; Abdulmalik, O. Rational design of pyridyl derivatives of vanillin for the treatment of sickle cell disease. Bioorg. Med. Chem. 2018, 26, 2530–2538. [Google Scholar] [CrossRef]
- Stern, W.; Mathews, D.; McKew, J.; Shen, X.; Kato, G.J. A phase 1, first-in-man, dose–response study of Aes-103 (5-HMF), an anti-sickling, allosteric modifier of hemoglobin oxygen affinity in healthy normal volunteers. Blood 2012, 120, 3210. [Google Scholar] [CrossRef]
- Safo, M.K.; Aljahdali, A.; Burnett, J.; Abraham, D.J.; Abdulmalik, O. Therapeutic Strategies for the Treatment of Sickle Cell Disease. In Burger’s Medicinal Chemistry and Drug Discovery; John Wiley & Sons: Hoboken, NJ, USA, 2021; pp. 1–31. [Google Scholar]
- Wong, G.; Marsden, P. Nitric oxide synthases: Regulation in disease. Nephrol. Dial. Transplant. 1996, 11, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Lamas, S.; Pérez-Sala, D.; Moncada, S. Nitric oxide: From discovery to the clinic. Trends Pharmacol. Sci. 1998, 19, 436–438. [Google Scholar] [CrossRef]
- Ignarro, L.J. Nitric oxide: A unique endogenous signaling molecule in vascular biology. Biosci. Rep. 1999, 19, 51–71. [Google Scholar] [CrossRef]
- De Franceschi, L. Pathophisiology of sickle cell disease and new drugs for the treatment. Mediterr. J. Hematol. Infect. Dis. 2009, 1, e2009024. [Google Scholar] [CrossRef]
- Wallis, J. Nitric oxide and blood: A review. Trans. Med. 2005, 15, 1–11. [Google Scholar] [CrossRef]
- Liu, C.; Wajih, N.; Liu, X.; Basu, S.; Janes, J.; Marvel, M.; Keggi, C.; Helms, C.C.; Lee, A.N.; Belanger, A.M. Mechanisms of human erythrocytic bioactivation of nitrite. J. Biol. Chem. 2015, 290, 1281–1294. [Google Scholar] [CrossRef]
- Lundberg, J.O.; Weitzberg, E. NO generation from nitrite and its role in vascular control. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 915–922. [Google Scholar] [CrossRef]
- Maley, J.H.; Lasker, G.F.; Kadowitz, P.J. Nitric oxide and disorders of the erythrocyte: Emerging roles and therapeutic targets. Cardiovasc. Haematol. Disord. Drug Targets 2010, 10, 284–291. [Google Scholar] [CrossRef]
- Gladwin, M.T.; Kato, G.J.; Weiner, D.; Onyekwere, O.C.; Dampier, C.; Hsu, L.; Hagar, R.W.; Howard, T.; Nuss, R.; Okam, M.M. Nitric oxide for inhalation in the acute treatment of sickle cell pain crisis: A randomized controlled trial. JAMA 2011, 305, 893–902. [Google Scholar] [CrossRef]
- Martinez-Ruiz, R.; Montero-Huerta, P.; Hromi, J.; Head, C.A. Inhaled nitric oxide improves survival rates during hypoxia in a sickle cell (SAD) mouse model. J. Am. Soc. Anesthesiol. 2001, 94, 1113–1118. [Google Scholar] [CrossRef]
- Cabrales, P.; Han, G.; Nacharaju, P.; Friedman, A.J.; Friedman, J.M. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide. Am. J. Physiol.-Heart Circ. Physiol. 2011, 300, H49–H56. [Google Scholar] [CrossRef]
- Kaur, J.; Bhardwaj, A.; Huang, Z.; Narang, D.; Chen, T.-Y.; Plane, F.; Knaus, E.E. Synthesis and biological investigations of nitric oxide releasing nateglinide and meglitinide type II antidiabetic prodrugs: In-vivo antihyperglycemic activities and blood pressure lowering studies. J. Med. Chem. 2012, 55, 7883–7891. [Google Scholar] [CrossRef]
- Nachuraju, P.; Friedman, A.J.; Friedman, J.M.; Cabrales, P. Exogenous nitric oxide prevents cardiovascular collapse during hemorrhagic shock. Resuscitation 2011, 82, 607–613. [Google Scholar] [CrossRef]
- Velázquez, C.; Praveen Rao, P.; Knaus, E.E. Novel nonsteroidal antiinflammatory drugs possessing a nitric oxide donor diazen-1-ium-1, 2-diolate moiety: Design, synthesis, biological evaluation, and nitric oxide release studies. J. Med. Chem. 2005, 48, 4061–4067. [Google Scholar] [CrossRef]
- Napoli, C.; Ignarro, L.J. Nitric oxide–releasing drugs. Annu. Rev. Pharmacol. Toxicol. 2003, 43, 97–123. [Google Scholar] [CrossRef]
- Andrade, C.; Barros, L.; Lima, M.; Azero, E. Purification and characterization of human hemoglobin: Effect of the hemolysis conditions. Int. J. Biol. Macromol. 2004, 34, 233–240. [Google Scholar] [CrossRef]
- Safo, M.K.; Abraham, D.J. X-ray crystallography of hemoglobins. In Hemoglobin Disorders; Humana Press Inc: Totowa, NJ, USA, 2003; p. 1. [Google Scholar]
- Gavrila, A.; Andersen, L.; Skrydstrup, T. A convenient and simple procedure for the preparation of nitrate esters from alcohols employing LiNO3/(CF3CO)2O. Tetrahedron Lett. 2005, 46, 6205–6207. [Google Scholar] [CrossRef]
- Xu, G.G.; Deshpande, T.M.; Ghatge, M.S.; Mehta, A.Y.; Omar, A.S.M.; Ahmed, M.H.; Venitz, J.; Abdulmalik, O.; Zhang, Y.; Safo, M.K. Design, Synthesis, and Investigation of Novel Nitric Oxide (NO)-Releasing Prodrugs as Drug Candidates for the Treatment of Ischemic Disorders: Insights into NO-Releasing Prodrug Biotransformation and Hemoglobin–NO Biochemistry. Biochemistry 2015, 54, 7178–7192. [Google Scholar] [CrossRef]
- Winn, M.D.; Ballard, C.C.; Cowtan, K.D.; Dodson, E.J.; Emsley, P.; Evans, P.R.; Keegan, R.M.; Krissinel, E.B.; Leslie, A.G.; McCoy, A. Overview of the CCP4 suite and current developments. Acta Crystallogr. D Biol. Crystallogr. 2011, 67, 235–242. [Google Scholar] [CrossRef]
- Adams, P.D.; Afonine, P.V.; Bunkóczi, G.; Chen, V.B.; Echols, N.; Headd, J.J.; Hung, L.-W.; Jain, S.; Kapral, G.J.; Kunstleve, R.W.G. The Phenix software for automated determination of macromolecular structures. Methods 2011, 55, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Echols, N.; Grosse-Kunstleve, R.W.; Afonine, P.V.; Bunkóczi, G.; Chen, V.B.; Headd, J.J.; McCoy, A.J.; Moriarty, N.W.; Read, R.J.; Richardson, D.C. Graphical tools for macromolecular crystallography in PHENIX. J. Appl. Crystallogr. 2012, 45, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Brünger, A.T.; Adams, P.D.; Clore, G.M.; DeLano, W.L.; Gros, P.; Grosse-Kunstleve, R.W.; Jiang, J.-S.; Kuszewski, J.; Nilges, M.; Pannu, N.S. Crystallography & NMR system: A new software suite for macromolecular structure determination. Acta Crystallogr. D Biol. Crystallogr. 1998, 54, 905–921. [Google Scholar] [PubMed]
- Thatcher, G.R.; Nicolescu, A.C.; Bennett, B.M.; Toader, V. Nitrates and NO release: Contemporary aspects in biological and medicinal chemistry. Free Radic. Biol. Med. 2004, 37, 1122–1143. [Google Scholar] [CrossRef]
- Wang, E.Q.; Balthasar, J.P.; Fung, H.-L. Pharmacodynamics of in vivo nitroglycerin tolerance in normal conscious rats: Effects of dose and dosing protocol. Pharm. Res. 2004, 21, 114–120. [Google Scholar] [CrossRef]
- Ahmed, M.H.; Ghatge, M.S.; Safo, M.K. Hemoglobin: Structure, function and allostery. In Vertebrate and Invertebrate Respiratory Proteins, Lipoproteins and Other Body Fluid Proteins; Springer Nature: Cham, Switzerland, 2020; pp. 345–382. [Google Scholar]
- Silva, M.M.; Rogers, P.H.; Arnone, A. A third quaternary structure of human hemoglobin A at 1.7-A resolution. J. Biol. Chem. 1992, 267, 17248–17256. [Google Scholar] [CrossRef]
- Fermi, G.; Perutz, M.F.; Shaanan, B.; Fourme, R. The crystal structure of human deoxyhaemoglobin at 1.74 Å resolution. J. Mol. Bol. 1984, 175, 159–174. [Google Scholar] [CrossRef]
- Abraham, D.J.; Safo, M.K.; Boyiri, T.; Danso-Danquah, R.E.; Kister, J.; Poyart, C. How allosteric effectors can bind to the same protein residue and produce opposite shifts in the allosteric equilibrium. Biochemistry 1995, 34, 15006–15020. [Google Scholar] [CrossRef]
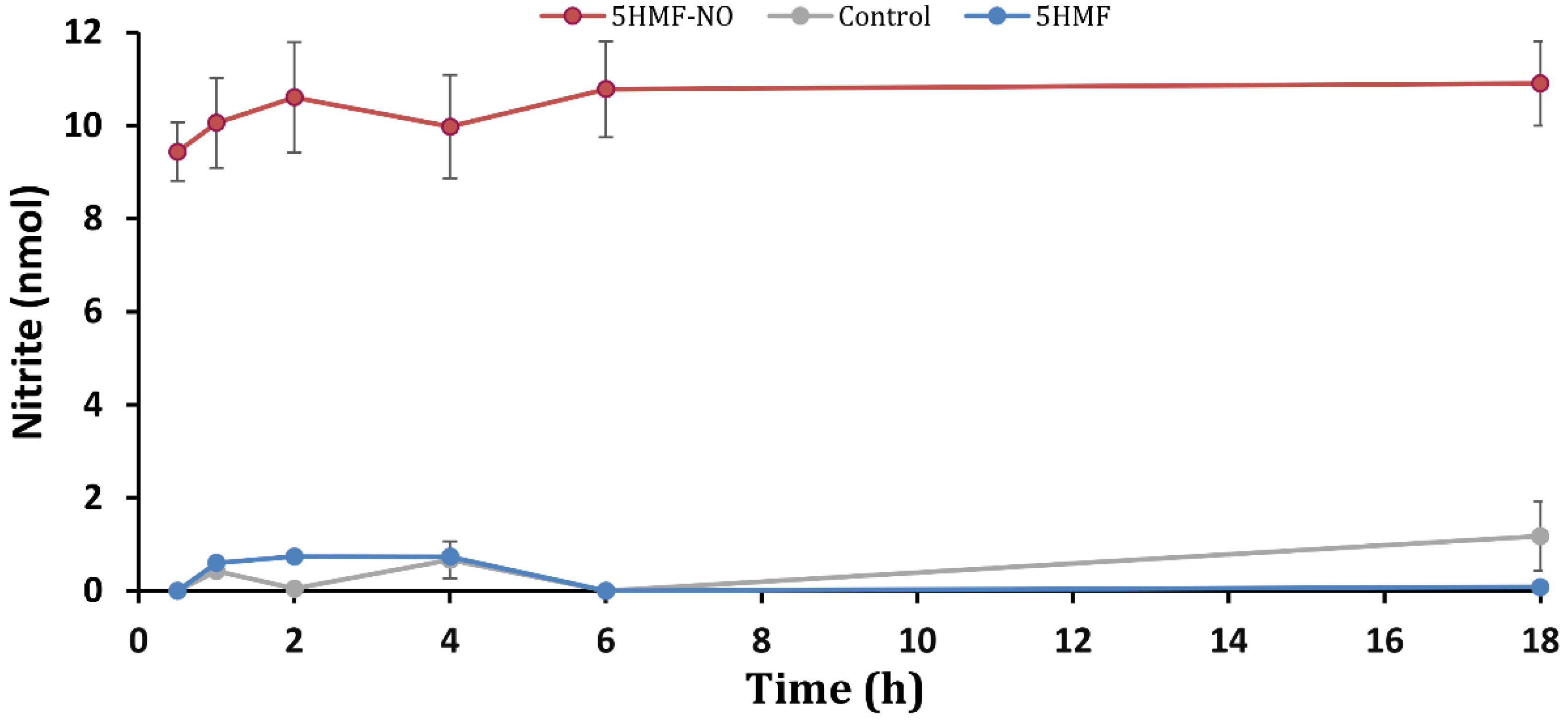
| NO2− Concentration (nmol) | ||||||
|---|---|---|---|---|---|---|
| Compound | 0.5 h | 1 h | 2 h | 4 h | 6 h | 18 h |
| 5HMF-NO | 9.44 ± 0.63 | 10.1 ± 0.97 | 10.6 ± 1.19 | 9.98 ± 1.11 | 10.8 ± 1.03 | 10.9 ± 0.91 |
| 5HMF | 0.00 ± 0.00 | 0.59 ± 0.01 | 0.73 ± 0.01 | 0.73 ± 0.01 | 0.30 ± 0.02 | 0.079 ± 0.00 |
| Control | 0.00 ± 0.04 | 0.42 ± 0.00 | 0.04 ± 0.28 | 0.66 ± 0.00 | 0.00 ± 0.52 | 1.18 ± 0.52 |
| Compound | % Functional/Biological Effect | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hb Modification | Sickling Inhibition | ΔP50 | |||||||
| 1 mM | 2 mM | 5 mM | 1 mM | 2 mM | 5 mM | 1 mM | 2 mM | 5 mM | |
| 5HMF-NO | 15.9 ± 0.2 | 20.7 ± 1.3 | 38.1 ± 0.6 | 27.0 ± 8.4 | 38.9 ± 15.1 | 59.9 ± 8.2 | 10.0 | 27.2 | 66.9 |
| 5HMF | 21.1 ± 0.6 | 30.9 ± 1.7 | 53.7 ± 0.1 | 20.6 ± 4.2 | 49.7 ± 4.8 | 68.5 ± 2.3 | 18.4 | 33.0 | 53.9 |
| Data Collection Statistics | 5HMF-NO (T-State) | Hydrolyzed 5HMF (R2-State) |
|---|---|---|
| PDB ID | 7UD7 | 7UD8 |
| Space group | P21 | P3221 |
| Cell dimensions (Ǻ) | 62.34, 82.03, 53.45; 99.49 | 92.23, 92.23, 144.07 |
| Tetramer/AU | 1 | 1 |
| Resolution (Ǻ) | 29.92–1.80 (1.86–1.80) | 28.39–1.80 (1.84–1.80) |
| Measured reflections | 18,7917 | 71,6379 (20,836) |
| Unique reflections | 46,300 (4367) | 66,309 (3896) |
| Redundancy | 4.06 (3.81) | 10.8 (5.3) |
| I/σI | 25.9 (10.8) | 28.8 (2.0) |
| Completeness (%) | 94.1 (89.4) | 100 (99.7) |
| Rmerge (%) a | 3.9 (8.2) | 5.5 (72.7) |
| Structure refinement | ||
| Resolution limit (Ǻ) | 26.36–1.80 (1.86–1.80) | 28.39–1.80 (1.86–1.80) |
| No. of reflections | 46,299 (4366) | 66,260 (6521) |
| Rwork (%) | 15.1 (18.9) | 18.6 (24.1) |
| Rfree (%) b | 19.1 (24.4) | 22.8 (26.9) |
| Rmsd geometry | ||
| Bond lengths (Ǻ) | 0.007 | 0.026 |
| Bond angles (°) | 1.37° | 2.01° |
| Dihedral angles (%) | ||
| Most favored regions | 98.2 | 98.1 |
| Allowed regions | 1.6 | 1.6 |
| Average B-factors (Å2) | ||
| All atoms | 15.6 | 27.3 |
| Protein alone | 13.84 | 26.2 |
| Ligands | 13.74 | 24.5 |
| Water | 26.18 | 35.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhashimi, R.T.; Ghatge, M.S.; Donkor, A.K.; Deshpande, T.M.; Anabaraonye, N.; Alramadhani, D.; Danso-Danquah, R.; Huang, B.; Zhang, Y.; Musayev, F.N.; et al. Design, Synthesis, and Antisickling Investigation of a Nitric Oxide-Releasing Prodrug of 5HMF for the Treatment of Sickle Cell Disease. Biomolecules 2022, 12, 696. https://doi.org/10.3390/biom12050696
Alhashimi RT, Ghatge MS, Donkor AK, Deshpande TM, Anabaraonye N, Alramadhani D, Danso-Danquah R, Huang B, Zhang Y, Musayev FN, et al. Design, Synthesis, and Antisickling Investigation of a Nitric Oxide-Releasing Prodrug of 5HMF for the Treatment of Sickle Cell Disease. Biomolecules. 2022; 12(5):696. https://doi.org/10.3390/biom12050696
Chicago/Turabian StyleAlhashimi, Rana T., Mohini S. Ghatge, Akua K. Donkor, Tanvi M. Deshpande, Nancy Anabaraonye, Dina Alramadhani, Richmond Danso-Danquah, Boshi Huang, Yan Zhang, Faik N. Musayev, and et al. 2022. "Design, Synthesis, and Antisickling Investigation of a Nitric Oxide-Releasing Prodrug of 5HMF for the Treatment of Sickle Cell Disease" Biomolecules 12, no. 5: 696. https://doi.org/10.3390/biom12050696
APA StyleAlhashimi, R. T., Ghatge, M. S., Donkor, A. K., Deshpande, T. M., Anabaraonye, N., Alramadhani, D., Danso-Danquah, R., Huang, B., Zhang, Y., Musayev, F. N., Abdulmalik, O., & Safo, M. K. (2022). Design, Synthesis, and Antisickling Investigation of a Nitric Oxide-Releasing Prodrug of 5HMF for the Treatment of Sickle Cell Disease. Biomolecules, 12(5), 696. https://doi.org/10.3390/biom12050696







