Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain
Abstract
1. Introduction
2. Causes of Post-Traumatic Trigeminal Neuropathic Pain (PTNP)
3. Clinical Considerations in PTNP
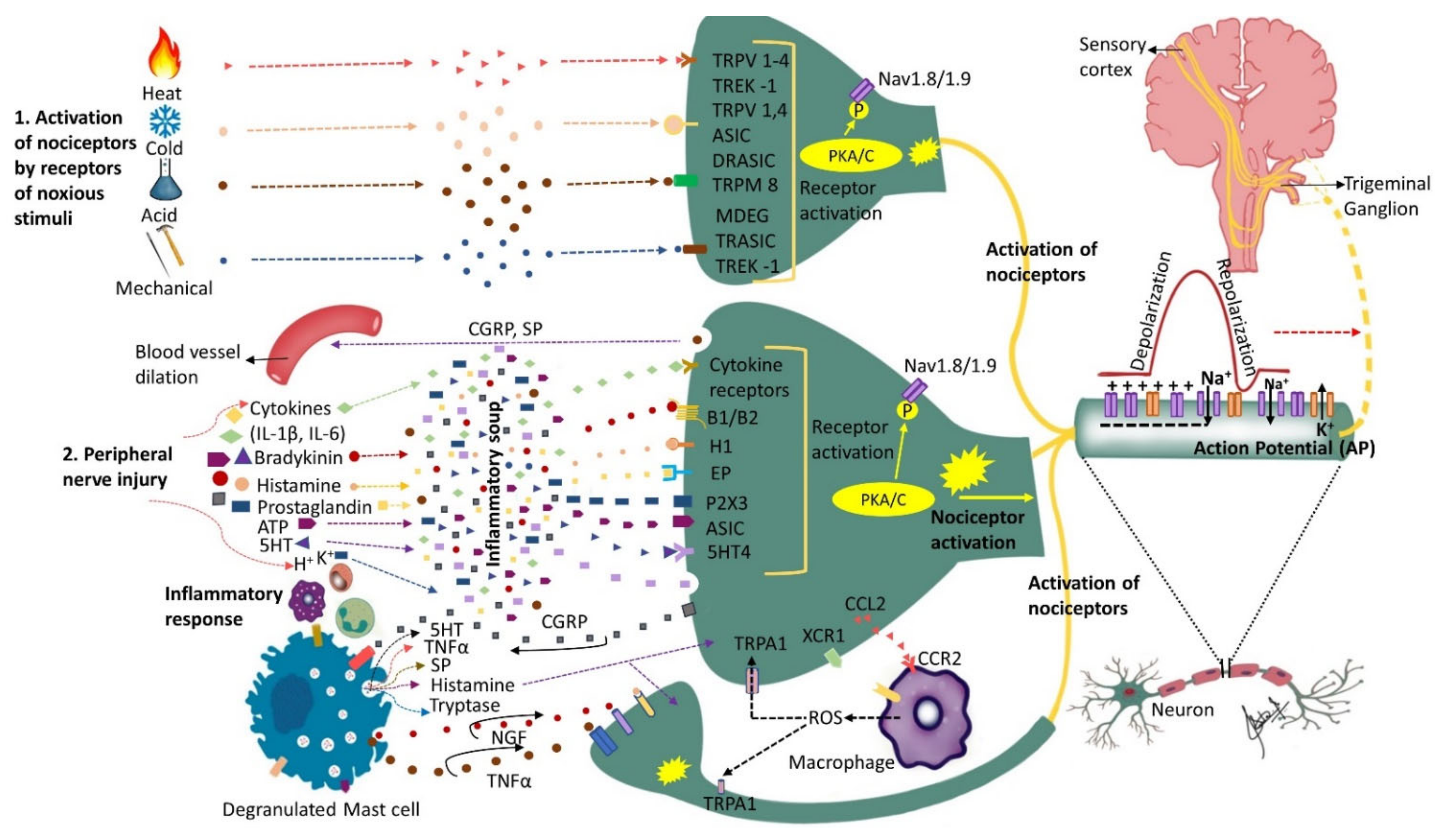
4. Peripheral Events in the Pathophysiology of PTNP
4.1. The Role of Receptors and Inflammatory Soup
4.2. The Role of Chemokines
4.3. Peripheral Sensitization
4.4. Spontaneous Neural Activity
4.5. SA in Different Nerve Fibers
4.6. Ion Channels Alterations
4.7. The Role of Neurovascular Interactions in Orofacial Neuropathic Pain
4.8. The Possible Role of Microorganisms in Peripheral Sensitization
4.9. The Role of Oxytocin in the Pathophysiology of PTNP
4.10. The Role of MicroRNAs in Pathophysiology of PTNP
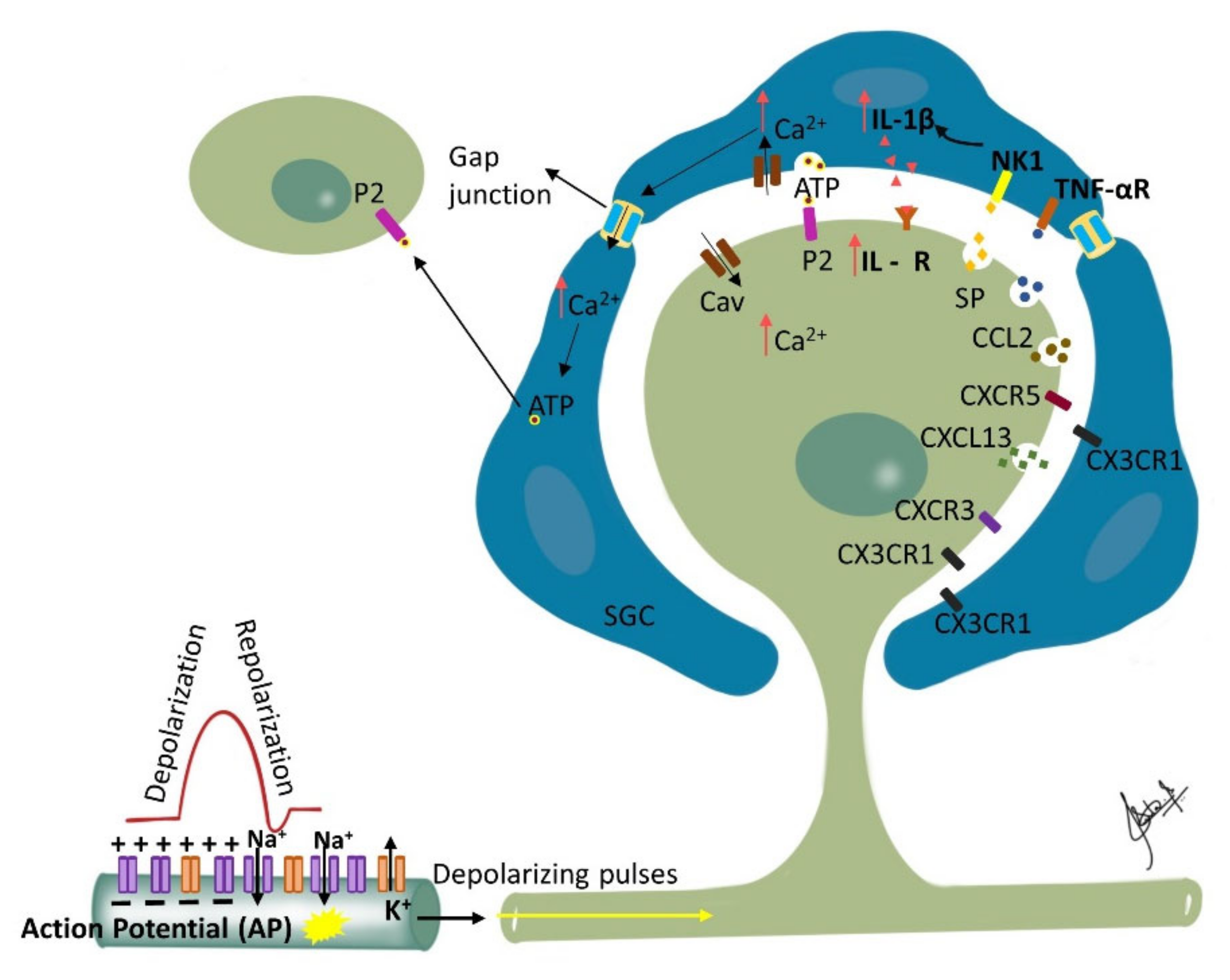
4.11. Ganglionic Sensitization and Phenotypic Changes
4.12. Phenotypic Changes and Allodynia
4.13. Response of the Injured Trigeminal System to Stress
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Haanpää, M.; Attal, N.; Backonja, M.; Baron, R.; Bennett, M.; Bouhassira, D.; Cruccu, G.; Hansson, P.; Haythornthwaite, J.A.; Iannetti, G.D.; et al. NeuPSIG guidelines on neuropathic pain assessment. Pain 2011, 152, 14–27. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [CrossRef] [PubMed]
- Benoliel, R.; Teich, S.; Eliav, E. Painful Traumatic Trigeminal Neuropathy. Oral Maxillofac. Surg. Clin. N. Am. 2016, 28, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Baad-Hansen, L.; Benoliel, R. Neuropathic orofacial pain: Facts and fiction. Cephalalgia 2017, 37, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.G.; Elias, L.A.; Yilmaz, Z.; Barker, S.; Shah, K.; Shah, S.; Renton, T. The psychosocial and affective burden of posttraumatic neuropathy following injuries to the trigeminal nerve. J. Orofac. Pain 2013, 27, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Pigg, M.; Svensson, P.; Drangsholt, M.; List, T. Seven-year follow-up of patients diagnosed with atypical odontalgia: A prospective study. J. Orofac. Pain 2013, 27, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Barron, R.P.; Benoliel, R.; Zeltser, R.; Eliav, E.; Nahlieli, O.; Gracely, R.H. Effect of dexamethasone and dipyrone on lingual and inferior alveolar nerve hypersensitivity following third molar extractions: Preliminary report. J. Orofac. Pain 2004, 18, 62–68. [Google Scholar]
- Valmaseda-Castellon, E.; Berini-Aytes, L.; Gay-Escoda, C. Inferior alveolar nerve damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral. Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 92, 377–383. [Google Scholar] [CrossRef]
- Gomes, A.C.; Vasconcelos, B.C.; de Oliveira e Silva, E.D.; da Silva, L.C. Lingual nerve damage after mandibular third molar surgery: A randomized clinical trial. J. Oral Maxillofac. Surg. 2005, 63, 1443–1446. [Google Scholar] [CrossRef]
- Queral-Godoy, E.; Figueiredo, R.; Valmaseda-Castellon, E.; Berini-Aytes, L.; Gay-Escoda, C. Frequency and evolution of lingual nerve lesions following lower third molar extraction. J. Oral Maxillofac. Surg. 2006, 64, 402–407. [Google Scholar] [CrossRef]
- Renton, T.; Adey-Viscuso, D.; Meechan, J.G.; Yilmaz, Z. Trigeminal nerve injuries in relation to the local anaesthesia in mandibular injections. Br. Dent. J. 2010, 209, E15. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Lee, S.J.; Kim, E.; Lee, C.Y. Hypoesthesia after IAN block anesthesia with lidocaine: Management of mild to moderate nerve injury. Restor. Dent. Endod. 2012, 37, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.H.; Lung, K.E. Nerve injuries after dental injection: A review of the literature. J. Can. Dent. Assoc. 2006, 72, 559–564. [Google Scholar] [PubMed]
- Nixdorf, D.R.; Moana-Filho, E.J.; Law, A.S.; McGuire, L.A.; Hodges, J.S.; John, M.T. Frequency of persistent tooth pain after root canal therapy: A systematic review and meta-analysis. J. Endod. 2010, 36, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Klasser, G.D.; Kugelmann, A.M.; Villines, D.; Johnson, B.R. The prevalence of persistent pain after nonsurgical root canal treatment. Quintessence Int. 2011, 42, 259–269. [Google Scholar] [PubMed]
- Gregg, J.M. Neuropathic complications of mandibular implant surgery: Review and case presentations. Ann. R. Australas. Coll. Dent. Surg. 2000, 15, 176–180. [Google Scholar]
- Benoliel, R.; Birenboim, R.; Regev, E.; Eliav, E. Neurosensory changes in the infraorbital nerve following zygomatic fractures. Oral. Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 657–665. [Google Scholar] [CrossRef]
- Benoliel, R.; Eliav, E.; Elishoov, H.; Sharav, Y. Diagnosis and treatment of persistent pain after trauma to the head and neck. J. Oral Maxillofac. Surg. 1994, 52, 1138–1147; discussion 1138–1147. [Google Scholar] [CrossRef]
- Berge, T.I. Incidence of chronic neuropathic pain subsequent to surgical removal of impacted third molars. Acta Odontol. Scand. 2002, 60, 108–112. [Google Scholar] [CrossRef]
- Arap, A.; Siqueira, S.R.; Silva, C.B.; Teixeira, M.J.; Siqueira, J.T. Trigeminal pain and quantitative sensory testing in painful peripheral diabetic neuropathy. Arch. Oral Biol. 2010, 55, 486–493. [Google Scholar] [CrossRef]
- Benoliel, R.; Eliav, E.; Tal, M. No sympathetic nerve sprouting in rat trigeminal ganglion following painful and non-painful infraorbital nerve neuropathy. Neurosci. Lett. 2001, 297, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Korczeniewska, O.A.; Katzmann Rider, G.; Gajra, S.; Narra, V.; Ramavajla, V.; Chang, Y.J.; Tao, Y.; Soteropoulos, P.; Husain, S.; Khan, J.; et al. Differential gene expression changes in the dorsal root versus trigeminal ganglia following peripheral nerve injury in rats. Eur. J. Pain 2020, 24, 967–982. [Google Scholar] [CrossRef] [PubMed]
- Latremoliere, A.; Mauborgne, A.; Masson, J.; Bourgoin, S.; Kayser, V.; Hamon, M.; Pohl, M. Differential implication of proinflammatory cytokine interleukin-6 in the development of cephalic versus extracephalic neuropathic pain in rats. J. Neurosci. 2008, 28, 8489–8501. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.L.; Parks, K.W.; Dodds, R.N. Chronic facial pain associated with endodontic therapy. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Lobb, W.K.; Zakariasen, K.L.; McGrath, P.J. Endodontic treatment outcomes: Do patients perceive problems? J. Am. Dent. Assoc. 1996, 127, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Marbach, J.J.; Hulbrock, J.; Hohn, C.; Segal, A.G. Incidence of phantom tooth pain: An atypical facial neuralgia. Oral Surg. Oral Med. Oral Pathol. 1982, 53, 190–193. [Google Scholar] [CrossRef]
- Polycarpou, N.; Ng, Y.L.; Canavan, D.; Moles, D.R.; Gulabivala, K. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int. Endod. J. 2005, 38, 169–178. [Google Scholar] [CrossRef]
- Kohli, D.; Katzmann, G.; Benoliel, R.; Korczeniewska, O.A. Diagnosis and management of persistent posttraumatic trigeminal neuropathic pain secondary to implant therapy: A review. J. Am. Dent. Assoc. 2021, 152, 483–490. [Google Scholar] [CrossRef]
- Kohli, D.; Falcon, C.; Katzmann, G.; Benoliel, R.; Khan, J.; Korczeniewska, O.A. Postendodontic pain: A practical approach to diagnosis and management. Quintessence Int. 2021, 52, 384–392. [Google Scholar] [CrossRef]
- Al-Sabbagh, M.; Okeson, J.P.; Khalaf, M.W.; Bhavsar, I. Persistent pain and neurosensory disturbance after dental implant surgery: Pathophysiology, etiology, and diagnosis. Dent. Clin. N. Am. 2015, 59, 131–142. [Google Scholar] [CrossRef]
- Steinberg, M.J.; Kelly, P.D. Implant-related nerve injuries. Dent. Clin. N. Am. 2015, 59, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Nixdorf, D.R.; Law, A.S.; John, M.T.; Sobieh, R.M.; Kohli, R.; Nguyen, R.H.; National Dental, P.C.G. Differential diagnoses for persistent pain after root canal treatment: A study in the National Dental Practice-based Research Network. J. Endod. 2015, 41, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Renton, T.; Yilmaz, Z. Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. J. Orofac. Pain 2011, 25, 333–344. [Google Scholar] [PubMed]
- Benoliel, R.; Zadik, Y.; Eliav, E.; Sharav, Y. Peripheral painful traumatic trigeminal neuropathy: Clinical features in 91 cases and proposal of novel diagnostic criteria. J. Orofac. Pain 2012, 26, 49–58. [Google Scholar] [PubMed]
- Penarrocha, M.A.; Penarrocha, D.; Bagan, J.V.; Penarrocha, M. Post-traumatic trigeminal neuropathy. A study of 63 cases. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e297–e300. [Google Scholar] [CrossRef][Green Version]
- Siqueira, S.R.; Siviero, M.; Alvarez, F.K.; Teixeira, M.J.; Siqueira, J.T. Quantitative sensory testing in trigeminal traumatic neuropathic pain and persistent idiopathic facial pain. Arq. Neuropsiquiatr. 2013, 71, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Eliav, E.; Benoliel, R.; Tal, M. Inflammation with no axonal damage of the rat saphenous nerve trunk induces ectopic discharge and mechanosensitivity in myelinated axons. Neurosci. Lett. 2001, 311, 49–52. [Google Scholar] [CrossRef]
- Dickie, A.C.; McCormick, B.; Lukito, V.; Wilson, K.L.; Torsney, C. Inflammatory Pain Reduces C Fiber Activity-Dependent Slowing in a Sex-Dependent Manner, Amplifying Nociceptive Input to the Spinal Cord. J. Neurosci. 2017, 37, 6488–6502. [Google Scholar] [CrossRef]
- Nitzan-Luques, A.; Devor, M.; Tal, M. Genotype-selective phenotypic switch in primary afferent neurons contributes to neuropathic pain. Pain 2011, 152, 2413–2426. [Google Scholar] [CrossRef]
- Nasri-Heir, C.; Khan, J.; Benoliel, R.; Feng, C.; Yarnitsky, D.; Kuo, F.; Hirschberg, C.; Hartwell, G.; Huang, C.Y.; Heir, G.; et al. Altered pain modulation in patients with persistent postendodontic pain. Pain 2015, 156, 2032–2041. [Google Scholar] [CrossRef]
- Von Hehn, C.A.; Baron, R.; Woolf, C.J. Deconstructing the neuropathic pain phenotype to reveal neural mechanisms. Neuron 2012, 73, 638–652. [Google Scholar] [CrossRef] [PubMed]
- Nitzan-Luques, A.; Minert, A.; Devor, M.; Tal, M. Dynamic genotype-selective “phenotypic switching” of CGRP expression contributes to differential neuropathic pain phenotype. Exp. Neurol. 2013, 250, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Kadoi, J.; Takeda, M.; Matsumoto, S. Prostaglandin E2 potentiates the excitability of small diameter trigeminal root ganglion neurons projecting onto the superficial layer of the cervical dorsal horn in rats. Exp. Brain Res. 2007, 176, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Takahashi, M.; Kitagawa, J.; Kanazawa, T.; Nasu, M.; Matsumoto, S. Brain-derived neurotrophic factor enhances the excitability of small-diameter trigeminal ganglion neurons projecting to the trigeminal nucleus interpolaris/caudalis transition zone following masseter muscle inflammation. Mol. Pain 2013, 9, 49. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Ikeda, M.; Takahashi, M.; Kanazawa, T.; Nasu, M.; Matsumoto, S. Suppression of ATP-induced excitability in rat small-diameter trigeminal ganglion neurons by activation of GABAB receptor. Brain Res. Bull. 2013, 98, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Beyak, M.J.; Vanner, S. Inflammation-induced hyperexcitability of nociceptive gastrointestinal DRG neurones: The role of voltage-gated ion channels. Neurogastroenterol. Motil. 2005, 17, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Bhave, G.; Gereau, R.W.t. Posttranslational mechanisms of peripheral sensitization. J. Neurobiol. 2004, 61, 88–106. [Google Scholar] [CrossRef]
- Chahine, M.; O’Leary, M.E. Regulation/modulation of sensory neuron sodium channels. Handb. Exp. Pharmacol. 2014, 221, 111–135. [Google Scholar] [CrossRef]
- Lampert, A.; Eberhardt, M.; Waxman, S.G. Altered sodium channel gating as molecular basis for pain: Contribution of activation, inactivation, and resurgent currents. Handb. Exp. Pharmacol. 2014, 221, 91–110. [Google Scholar] [CrossRef]
- Takeda, M.; Tsuboi, Y.; Kitagawa, J.; Nakagawa, K.; Iwata, K.; Matsumoto, S. Potassium channels as a potential therapeutic target for trigeminal neuropathic and inflammatory pain. Mol. Pain 2011, 7, 5. [Google Scholar] [CrossRef]
- Busserolles, J.; Tsantoulas, C.; Eschalier, A.; Lopez Garcia, J.A. Potassium channels in neuropathic pain: Advances, challenges, and emerging ideas. Pain 2016, 157 (Suppl. S1), S7–S14. [Google Scholar] [CrossRef] [PubMed]
- Montague, K.; Malcangio, M. The therapeutic potential of targeting chemokine signalling in the treatment of chronic pain. J. Neurochem. 2017, 141, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Solis-Castro, O.O.; Wong, N.; Boissonade, F.M. Chemokines and Pain in the Trigeminal System. Front. Pain Res. 2021, 2, 689314. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.J.; Dong, Y.L.; Lu, Y.; Cao, S.; Zhao, Z.Q.; Gao, Y.J. Chemokine CCL2 and its receptor CCR2 in the medullary dorsal horn are involved in trigeminal neuropathic pain. J. Neuroinflamm. 2012, 9, 136. [Google Scholar] [CrossRef]
- Lin, J.; Liu, F.; Zhang, Y.Y.; Song, N.; Liu, M.K.; Fang, X.Y.; Liao, D.Q.; Zhou, C.; Wang, H.; Shen, J.F. P2Y14 receptor is functionally expressed in satellite glial cells and mediates interleukin-1beta and chemokine CCL2 secretion. J. Cell. Physiol. 2019, 234, 21199–21210. [Google Scholar] [CrossRef]
- Dauvergne, C.; Molet, J.; Reaux-Le Goazigo, A.; Mauborgne, A.; Melik-Parsadaniantz, S.; Boucher, Y.; Pohl, M. Implication of the chemokine CCL2 in trigeminal nociception and traumatic neuropathic orofacial pain. Eur. J. Pain 2014, 18, 360–375. [Google Scholar] [CrossRef]
- Xie, W.; Strong, J.A.; Meij, J.T.A.; Zhang, J.M.; Yu, L. Neuropathic pain: Early spontaneous afferent activity is the trigger. Pain 2005, 116, 243–256. [Google Scholar] [CrossRef]
- Belkouch, M.; Dansereau, M.A.; Reaux-Le Goazigo, A.; Van Steenwinckel, J.; Beaudet, N.; Chraibi, A.; Melik-Parsadaniantz, S.; Sarret, P. The chemokine CCL2 increases Nav1.8 sodium channel activity in primary sensory neurons through a Gbetagamma-dependent mechanism. J. Neurosci. 2011, 31, 18381–18390. [Google Scholar] [CrossRef]
- Van Steenwinckel, J.; Auvynet, C.; Sapienza, A.; Reaux-Le Goazigo, A.; Combadiere, C.; Melik Parsadaniantz, S. Stromal cell-derived CCL2 drives neuropathic pain states through myeloid cell infiltration in injured nerve. Brain Behav. Immun. 2015, 45, 198–210. [Google Scholar] [CrossRef]
- Domoto, R.; Sekiguchi, F.; Tsubota, M.; Kawabata, A. Macrophage as a Peripheral Pain Regulator. Cells 2021, 10, 1881. [Google Scholar] [CrossRef]
- Chen, O.; Donnelly, C.R.; Ji, R.R. Regulation of pain by neuro-immune interactions between macrophages and nociceptor sensory neurons. Curr. Opin. Neurobiol. 2020, 62, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Cao, D.L.; Zhang, Z.J.; Jiang, B.C.; Gao, Y.J. Chemokine CXCL13 mediates orofacial neuropathic pain via CXCR5/ERK pathway in the trigeminal ganglion of mice. J. Neuroinflamm. 2016, 13, 183. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhu, M.D.; Cao, D.L.; Bai, X.Q.; Gao, Y.J.; Wu, X.B. Chemokine CXCL13 activates p38 MAPK in the trigeminal ganglion after infraorbital nerve injury. Inflammation 2017, 40, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, T.; Afroz, S.; Inoue, M.; Arakaki, R.; Oshima, M.; Raju, R.; Waskitho, A.; Inoue, M.; Baba, O.; Matsuka, Y. IL-10 and CXCL2 in trigeminal ganglia in neuropathic pain. Neurosci. Lett. 2019, 703, 132–138. [Google Scholar] [CrossRef]
- Ju, Y.Y.; Jiang, M.; Xu, F.; Wang, D.; Ding, B.; Ma, L.J.; Wu, H. CXCL10 and CXCR3 in the Trigeminal Ganglion Contribute to Trigeminal Neuropathic Pain in Mice. J. Pain Res. 2021, 14, 41–51. [Google Scholar] [CrossRef]
- Hucho, T.; Levine, J.D. Signaling pathways in sensitization: Toward a nociceptor cell biology. Neuron 2007, 55, 365–376. [Google Scholar] [CrossRef]
- Sessle, B.J. Chronic Orofacial Pain: Models, Mechanisms, and Genetic and Related Environmental Influences. Int. J. Mol. Sci. 2021, 22, 7112. [Google Scholar] [CrossRef]
- Sundt, D.; Gamper, N.; Jaffe, D.B. Spike propagation through the dorsal root ganglia in an unmyelinated sensory neuron: A modeling study. J. Neurophysiol. 2015, 114, 3140–3153. [Google Scholar] [CrossRef]
- Ma, C.; LaMotte, R.H. Multiple sites for generation of ectopic spontaneous activity in neurons of the chronically compressed dorsal root ganglion. J. Neurosci. 2007, 27, 14059–14068. [Google Scholar] [CrossRef]
- Wall, P.D.; Devor, M. Sensory afferent impulses originate from dorsal root ganglia as well as from the periphery in normal and nerve injured rats. Pain 1983, 17, 321–339. [Google Scholar] [CrossRef]
- Liu, C.N.; Wall, P.D.; Ben-Dor, E.; Michaelis, M.; Amir, R.; Devor, M. Tactile allodynia in the absence of C-fiber activation: Altered firing properties of DRG neurons following spinal nerve injury. Pain 2000, 85, 503–521. [Google Scholar] [CrossRef] [PubMed]
- Coggan, J.S.; Sejnowski, T.J.; Prescott, S.A. Cooperativity between remote sites of ectopic spiking allows afterdischarge to be initiated and maintained at different locations. J. Comput. Neurosci. 2015, 39, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Amir, R.; Liu, C.N.; Kocsis, J.D.; Devor, M. Oscillatory mechanism in primary sensory neurones. Brain 2002, 125, 421–435. [Google Scholar] [CrossRef]
- Amir, R.; Michaelis, M.; Devor, M. Burst discharge in primary sensory neurons: Triggered by subthreshold oscillations, maintained by depolarizing afterpotentials. J. Neurosci. 2002, 22, 1187–1198. [Google Scholar] [CrossRef] [PubMed]
- Velasco, E.; Alvarez, J.L.; Meseguer, V.M.; Gallar, J.; Talavera, K. Membrane potential instabilities in sensory neurons: Mechanisms and pathophysiological relevance. Pain 2022, 163, 64–74. [Google Scholar] [CrossRef]
- Benoliel, R.; Eliav, E.; Tal, M. Strain-dependent modification of neuropathic pain behaviour in the rat hindpaw by a priming painful trigeminal nerve injury. Pain 2002, 97, 203–212. [Google Scholar] [CrossRef]
- Chacur, M.; Milligan, E.D.; Gazda, L.S.; Armstrong, C.; Wang, H.; Tracey, K.J.; Maier, S.F.; Watkins, L.R. A new model of sciatic inflammatory neuritis (SIN): Induction of unilateral and bilateral mechanical allodynia following acute unilateral peri-sciatic immune activation in rats. Pain 2001, 94, 231–244. [Google Scholar] [CrossRef]
- Orstavik, K.; Jorum, E. Microneurographic findings of relevance to pain in patients with erythromelalgia and patients with diabetic neuropathy. Neurosci. Lett. 2010, 470, 180–184. [Google Scholar] [CrossRef]
- Campero, M.; Serra, J.; Marchettini, P.; Ochoa, J.L. Ectopic impulse generation and autoexcitation in single myelinated afferent fibers in patients with peripheral neuropathy and positive sensory symptoms. Muscle Nerve 1998, 21, 1661–1667. [Google Scholar] [CrossRef]
- Taha, O.; Opitz, T.; Mueller, M.; Pitsch, J.; Becker, A.; Evert, B.O.; Beck, H.; Jeub, M. Neuropathic pain in experimental autoimmune neuritis is associated with altered electrophysiological properties of nociceptive DRG neurons. Exp. Neurol. 2017, 297, 25–35. [Google Scholar] [CrossRef]
- Donadio, V.; Liguori, R. Microneurographic recording from unmyelinated nerve fibers in neurological disorders: An update. Clin. Neurophysiol. 2015, 126, 437–445. [Google Scholar] [CrossRef]
- North, R.Y.; Lazaro, T.T.; Dougherty, P.M. Ectopic Spontaneous Afferent Activity and Neuropathic Pain. Neurosurgery 2018, 65, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Devor, M. Ectopic discharge in Abeta afferents as a source of neuropathic pain. Exp. Brain Res. 2009, 196, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Molander, C.; Hongpaisan, J.; Persson, J.K. Distribution of c-fos expressing dorsal horn neurons after electrical stimulation of low threshold sensory fibers in the chronically injured sciatic nerve. Brain Res. 1994, 644, 74–82. [Google Scholar] [CrossRef]
- Day, A.S.; Lue, J.H.; Sun, W.Z.; Shieh, J.Y.; Wen, C.Y. A beta-fiber intensity stimulation of chronically constricted median nerve induces c-fos expression in thalamic projection neurons of the cuneate nucleus in rats with behavioral signs of neuropathic pain. Brain Res. 2001, 895, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Shortland, P.; Molander, C. The time-course of abeta-evoked c-fos expression in neurons of the dorsal horn and gracile nucleus after peripheral nerve injury. Brain Res. 1998, 810, 288–293. [Google Scholar] [CrossRef]
- Fujisawa, N.; Terayama, R.; Yamaguchi, D.; Omura, S.; Yamashiro, T.; Sugimoto, T. Fos protein-like immunoreactive neurons induced by electrical stimulation in the trigeminal sensory nuclear complex of rats with chronically injured peripheral nerve. Exp. Brain Res. 2012, 219, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Chaplan, S.R.; Guo, H.Q.; Lee, D.H.; Luo, L.; Liu, C.; Kuei, C.; Velumian, A.A.; Butler, M.P.; Brown, S.M.; Dubin, A.E. Neuronal hyperpolarization-activated pacemaker channels drive neuropathic pain. J. Neurosci. 2003, 23, 1169–1178. [Google Scholar] [CrossRef]
- Yao, H.; Donnelly, D.F.; Ma, C.; LaMotte, R.H. Upregulation of the hyperpolarization-activated cation current after chronic compression of the dorsal root ganglion. J. Neurosci. 2003, 23, 2069–2074. [Google Scholar] [CrossRef]
- Kitagawa, J.; Takeda, M.; Suzuki, I.; Kadoi, J.; Tsuboi, Y.; Honda, K.; Matsumoto, S.; Nakagawa, H.; Tanabe, A.; Iwata, K. Mechanisms involved in modulation of trigeminal primary afferent activity in rats with peripheral mononeuropathy. Eur. J. Neurosci. 2006, 24, 1976–1986. [Google Scholar] [CrossRef]
- Cho, H.J.; Staikopoulos, V.; Furness, J.B.; Jennings, E.A. Inflammation-induced increase in hyperpolarization-activated, cyclic nucleotide-gated channel protein in trigeminal ganglion neurons and the effect of buprenorphine. Neuroscience 2009, 162, 453–461. [Google Scholar] [CrossRef] [PubMed]
- He, J.T.; Li, X.Y.; Zhao, X.; Liu, X. Hyperpolarization-activated and cyclic nucleotide-gated channel proteins as emerging new targets in neuropathic pain. Rev. Neurosci. 2019, 30, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.S.; Kim, Y.S.; Moozhayil, S.J.; Yang, E.S.; Bae, Y.C. The expression of hyperpolarization-activated cyclic nucleotide-gated channel 1 (HCN1) and HCN2 in the rat trigeminal ganglion, sensory root, and dental pulp. Neuroscience 2015, 291, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Weng, X.; Smith, T.; Sathish, J.; Djouhri, L. Chronic inflammatory pain is associated with increased excitability and hyperpolarization-activated current (Ih) in C- but not Adelta-nociceptors. Pain 2012, 153, 900–914. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Chang, L.; Sorkin, L.S.; Chaplan, S.R. Hyperpolarization-activated, cation-nonselective, cyclic nucleotide-modulated channel blockade alleviates mechanical allodynia and suppresses ectopic discharge in spinal nerve ligated rats. J. Pain 2005, 6, 417–424. [Google Scholar] [CrossRef]
- Huang, D.; Liang, C.; Zhang, F.; Men, H.; Du, X.; Gamper, N.; Zhang, H. Inflammatory mediator bradykinin increases population of sensory neurons expressing functional T-type Ca(2+) channels. Biochem. Biophys. Res. Commun. 2016, 473, 396–402. [Google Scholar] [CrossRef]
- Marger, F.; Gelot, A.; Alloui, A.; Matricon, J.; Ferrer, J.F.; Barrere, C.; Pizzoccaro, A.; Muller, E.; Nargeot, J.; Snutch, T.P.; et al. T-type calcium channels contribute to colonic hypersensitivity in a rat model of irritable bowel syndrome. Proc. Natl. Acad. Sci. USA 2011, 108, 11268–11273. [Google Scholar] [CrossRef]
- Garcia-Caballero, A.; Gadotti, V.M.; Stemkowski, P.; Weiss, N.; Souza, I.A.; Hodgkinson, V.; Bladen, C.; Chen, L.; Hamid, J.; Pizzoccaro, A.; et al. The deubiquitinating enzyme USP5 modulates neuropathic and inflammatory pain by enhancing Cav3.2 channel activity. Neuron 2014, 83, 1144–1158. [Google Scholar] [CrossRef]
- Jagodic, M.M.; Pathirathna, S.; Joksovic, P.M.; Lee, W.; Nelson, M.T.; Naik, A.K.; Su, P.; Jevtovic-Todorovic, V.; Todorovic, S.M. Upregulation of the T-type calcium current in small rat sensory neurons after chronic constrictive injury of the sciatic nerve. J. Neurophysiol. 2008, 99, 3151–3156. [Google Scholar] [CrossRef]
- Jagodic, M.M.; Pathirathna, S.; Nelson, M.T.; Mancuso, S.; Joksovic, P.M.; Rosenberg, E.R.; Bayliss, D.A.; Jevtovic-Todorovic, V.; Todorovic, S.M. Cell-specific alterations of T-type calcium current in painful diabetic neuropathy enhance excitability of sensory neurons. J. Neurosci. 2007, 27, 3305–3316. [Google Scholar] [CrossRef]
- Kang, X.J.; Chi, Y.N.; Chen, W.; Liu, F.Y.; Cui, S.; Liao, F.F.; Cai, J.; Wan, Y. Increased expression of CaV3.2 T-type calcium channels in damaged DRG neurons contributes to neuropathic pain in rats with spared nerve injury. Mol. Pain 2018, 14, 1744806918765808. [Google Scholar] [CrossRef] [PubMed]
- Todorovic, S.M.; Jevtovic-Todorovic, V. Neuropathic pain: Role for presynaptic T-type channels in nociceptive signaling. Pflug. Arch. 2013, 465, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Messinger, R.B.; Naik, A.K.; Jagodic, M.M.; Nelson, M.T.; Lee, W.Y.; Choe, W.J.; Orestes, P.; Latham, J.R.; Todorovic, S.M.; Jevtovic-Todorovic, V. In vivo silencing of the Ca(V)3.2 T-type calcium channels in sensory neurons alleviates hyperalgesia in rats with streptozocin-induced diabetic neuropathy. Pain 2009, 145, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Todorovic, S.M.; Jevtovic-Todorovic, V.; Meyenburg, A.; Mennerick, S.; Perez-Reyes, E.; Romano, C.; Olney, J.W.; Zorumski, C.F. Redox modulation of T-type calcium channels in rat peripheral nociceptors. Neuron 2001, 31, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Latham, J.R.; Pathirathna, S.; Jagodic, M.M.; Choe, W.J.; Levin, M.E.; Nelson, M.T.; Lee, W.Y.; Krishnan, K.; Covey, D.F.; Todorovic, S.M.; et al. Selective T-type calcium channel blockade alleviates hyperalgesia in ob/ob mice. Diabetes 2009, 58, 2656–2665. [Google Scholar] [CrossRef] [PubMed]
- Todorovic, S.M.; Pathirathna, S.; Brimelow, B.C.; Jagodic, M.M.; Ko, S.H.; Jiang, X.; Nilsson, K.R.; Zorumski, C.F.; Covey, D.F.; Jevtovic-Todorovic, V. 5beta-reduced neuroactive steroids are novel voltage-dependent blockers of T-type Ca2+ channels in rat sensory neurons in vitro and potent peripheral analgesics in vivo. Mol. Pharmacol. 2004, 66, 1223–1235. [Google Scholar] [CrossRef] [PubMed]
- Cai, S.; Gomez, K.; Moutal, A.; Khanna, R. Targeting T-type/CaV3.2 channels for chronic pain. Transl. Res. 2021, 234, 20–30. [Google Scholar] [CrossRef]
- Montera, M.; Goins, A.; Cmarko, L.; Weiss, N.; Westlund, K.N.; Alles, S.R.A. Trigeminal neuropathic pain is alleviated by inhibition of Cav3.3 T-type calcium channels in mice. Channels 2021, 15, 31–37. [Google Scholar] [CrossRef]
- Stanimirovic, D.B.; Friedman, A. Pathophysiology of the neurovascular unit: Disease cause or consequence? J. Cereb. Blood Flow Metab. 2012, 32, 1207–1221. [Google Scholar] [CrossRef]
- Echeverry, S.; Shi, X.Q.; Rivest, S.; Zhang, J. Peripheral nerve injury alters blood-spinal cord barrier functional and molecular integrity through a selective inflammatory pathway. J. Neurosci. 2011, 31, 10819–10828. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.K.Y.; Shi, X.Q.; Martin, H.C.; Huang, H.; Luheshi, G.; Rivest, S.; Zhang, J. Blood-nerve barrier dysfunction contributes to the generation of neuropathic pain and allows targeting of injured nerves for pain relief. Pain 2014, 155, 954–967. [Google Scholar] [CrossRef] [PubMed]
- Jurga, A.M.; Rojewska, E.; Piotrowska, A.; Makuch, W.; Pilat, D.; Przewlocka, B.; Mika, J. Blockade of Toll-Like Receptors (TLR2, TLR4) Attenuates Pain and Potentiates Buprenorphine Analgesia in a Rat Neuropathic Pain Model. Neural Plast. 2016, 2016, 5238730. [Google Scholar] [CrossRef] [PubMed]
- Moreau, N.; Dieb, W.; Mauborgne, A.; Bourgoin, S.; Villanueva, L.; Pohl, M.; Boucher, Y. Hedgehog Pathway-Mediated Vascular Alterations Following Trigeminal Nerve Injury. J. Dent. Res. 2017, 96, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Nocera, G.; Jacob, C. Mechanisms of Schwann cell plasticity involved in peripheral nerve repair after injury. Cell. Mol. Life Sci. 2020, 77, 3977–3989. [Google Scholar] [CrossRef] [PubMed]
- Moreau, N.; Mauborgne, A.; Bourgoin, S.; Couraud, P.O.; Romero, I.A.; Weksler, B.B.; Villanueva, L.; Pohl, M.; Boucher, Y. Early alterations of Hedgehog signaling pathway in vascular endothelial cells after peripheral nerve injury elicit blood-nerve barrier disruption, nerve inflammation, and neuropathic pain development. Pain 2016, 157, 827–839. [Google Scholar] [CrossRef] [PubMed]
- Moreau, N.; Mauborgne, A.; Couraud, P.O.; Romero, I.A.; Weksler, B.B.; Villanueva, L.; Pohl, M.; Boucher, Y. Could an endoneurial endothelial crosstalk between Wnt/beta-catenin and Sonic Hedgehog pathways underlie the early disruption of the infra-orbital blood-nerve barrier following chronic constriction injury? Mol. Pain 2017, 13, 1744806917727625. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.R.; Chamessian, A.; Zhang, Y.Q. Pain regulation by non-neuronal cells and inflammation. Science 2016, 354, 572–577. [Google Scholar] [CrossRef]
- Yang, N.J.; Chiu, I.M. Bacterial Signaling to the Nervous System through Toxins and Metabolites. J. Mol. Biol. 2017, 429, 587–605. [Google Scholar] [CrossRef]
- Talbot, S.; Foster, S.L.; Woolf, C.J. Neuroimmunity: Physiology and Pathology. Annu. Rev. Immunol. 2016, 34, 421–447. [Google Scholar] [CrossRef]
- Boucher, Y.; Moreau, N.; Mauborgne, A.; Dieb, W. Lipopolysaccharide-mediated inflammatory priming potentiates painful post-traumatic trigeminal neuropathy. Physiol. Behav. 2018, 194, 497–504. [Google Scholar] [CrossRef]
- Lu, Y.C.; Yeh, W.C.; Ohashi, P.S. LPS/TLR4 signal transduction pathway. Cytokine 2008, 42, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Hendrich, J.; Alvarez, P.; Joseph, E.K.; Chen, X.; Bogen, O.; Levine, J.D. Electrophysiological correlates of hyperalgesic priming in vitro and in vivo. Pain 2013, 154, 2207–2215. [Google Scholar] [CrossRef] [PubMed]
- Aley, K.O.; Levine, J.D. Different peripheral mechanisms mediate enhanced nociception in metabolic/toxic and traumatic painful peripheral neuropathies in the rat. Neuroscience 2002, 111, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Meacham, K.; Shepherd, A.; Mohapatra, D.P.; Haroutounian, S. Neuropathic Pain: Central vs. Peripheral Mechanisms. Curr Pain Headache Rep. 2017, 21, 28. [Google Scholar] [CrossRef]
- Dieb, W.; Moreau, N.; Chemla, I.; Descroix, V.; Boucher, Y. Neuropathic pain in the orofacial region: The role of pain history. A retrospective study. J. Stomatol. Oral Maxillofac. Surg. 2017, 118, 147–150. [Google Scholar] [CrossRef]
- Khan, J.; Puchimada, B.; Kadouri, D.; Zusman, T.; Javed, F.; Eliav, E. The anti-nociceptive effects of Porphyromonas gingivalis lipopolysaccharide. Arch. Oral Biol. 2019, 102, 193–198. [Google Scholar] [CrossRef]
- Liu, R.; Desta, T.; Raptis, M.; Darveau, R.P.; Graves, D.T.P. gingivalis and E. coli lipopolysaccharides exhibit different systemic but similar local induction of inflammatory markers. J. Periodontol. 2008, 79, 1241–1247. [Google Scholar] [CrossRef]
- Amir, R.; Kocsis, J.D.; Devor, M. Multiple interacting sites of ectopic spike electrogenesis in primary sensory neurons. J. Neurosci. 2005, 25, 2576–2585. [Google Scholar] [CrossRef]
- Mika, J.; Zychowska, M.; Popiolek-Barczyk, K.; Rojewska, E.; Przewlocka, B. Importance of glial activation in neuropathic pain. Eur. J. Pharmacol. 2013, 716, 106–119. [Google Scholar] [CrossRef]
- Scholz, J.; Woolf, C.J. The neuropathic pain triad: Neurons, immune cells and glia. Nat. Neurosci. 2007, 10, 1361–1368. [Google Scholar] [CrossRef]
- Vallejo, R.; Tilley, D.M.; Vogel, L.; Benyamin, R. The role of glia and the immune system in the development and maintenance of neuropathic pain. Pain Pract. 2010, 10, 167–184. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, C.R.; Andriessen, A.S.; Chen, G.; Wang, K.; Jiang, C.; Maixner, W.; Ji, R.R. Central Nervous System Targets: Glial Cell Mechanisms in Chronic Pain. Neurotherapeutics 2020, 17, 846–860. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Green, C.R.; Rupenthal, I.D.; Moalem-Taylor, G. Role of gap junctions in chronic pain. J. Neurosci. Res. 2012, 90, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.R.; Strichartz, G. Cell signaling and the genesis of neuropathic pain. Sci. STKE 2004, 2004, reE14. [Google Scholar] [CrossRef]
- Hanani, M. Intercellular communication in sensory ganglia by purinergic receptors and gap junctions: Implications for chronic pain. Brain Res. 2012, 1487, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Kubo, A.; Shinoda, M.; Katagiri, A.; Takeda, M.; Suzuki, T.; Asaka, J.; Yeomans, D.C.; Iwata, K. Oxytocin alleviates orofacial mechanical hypersensitivity associated with infraorbital nerve injury through vasopressin-1A receptors of the rat trigeminal ganglia. Pain 2017, 158, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Ando, M.; Hayashi, Y.; Hitomi, S.; Shibuta, I.; Furukawa, A.; Oto, T.; Inada, T.; Matsui, T.; Fukaya, C.; Noma, N.; et al. Oxytocin-Dependent Regulation of TRPs Expression in Trigeminal Ganglion Neurons Attenuates Orofacial Neuropathic Pain Following Infraorbital Nerve Injury in Rats. Int. J. Mol. Sci. 2020, 21, 9173. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.L.; Liu, F.; Zhang, Y.Y.; Lin, J.; Fu, M.; Li, Y.L.; Zhou, C.; Li, C.J.; Shen, J.F. Activation of oxytocin receptor in the trigeminal ganglion attenuates orofacial ectopic pain attributed to inferior alveolar nerve injury. J. Neurophysiol. 2021, 125, 223–231. [Google Scholar] [CrossRef]
- Tufekci, K.U.; Meuwissen, R.L.; Genc, S. The role of microRNAs in biological processes. Methods Mol. Biol. 2014, 1107, 15–31. [Google Scholar] [CrossRef]
- Kress, M.; Huttenhofer, A.; Landry, M.; Kuner, R.; Favereaux, A.; Greenberg, D.; Bednarik, J.; Heppenstall, P.; Kronenberg, F.; Malcangio, M.; et al. microRNAs in nociceptive circuits as predictors of future clinical applications. Front. Mol. Neurosci. 2013, 6, 33. [Google Scholar] [CrossRef]
- Li, X.; Wang, D.; Zhou, J.; Yan, Y.; Chen, L. Evaluation of circulating microRNA expression in patients with trigeminal neuralgia: An observational study. Medicine 2020, 99, e22972. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.L.; Lin, K.; Lin, S.K. NLRP3 inflammasome signaling as an early molecular response is negatively controlled by miR-186 in CFA-induced prosopalgia mice. Braz. J. Med. Biol. Res. 2018, 51, e7602. [Google Scholar] [CrossRef] [PubMed]
- Qi, R.; Cao, J.; Sun, Y.; Li, Y.; Huang, Z.; Jiang, D.; Jiang, X.H.; Snutch, T.P.; Zhang, Y.; Tao, J. Histone methylation-mediated microRNA-32-5p down-regulation in sensory neurons regulates pain behaviors via targeting Cav3.2 channels. Proc. Natl. Acad. Sci. USA 2022, 119, e2117209119. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, H.; Zhang, T.; He, M.; Liang, H.; Wang, H.; Xu, L.; Chen, S.; Xu, M. Inhibition of MicroRNA-195 Alleviates Neuropathic Pain by Targeting Patched1 and Inhibiting SHH Signaling Pathway Activation. Neurochem. Res. 2019, 44, 1690–1702. [Google Scholar] [CrossRef] [PubMed]
- Reinhold, A.K.; Krug, S.M.; Salvador, E.; Sauer, R.S.; Karl-Scholler, F.; Malcangio, M.; Sommer, C.; Rittner, H.L. MicroRNA-21-5p functions via RECK/MMP9 as a proalgesic regulator of the blood nerve barrier in nerve injury. Ann. N. Y. Acad. Sci. 2022, 1515, 184–195. [Google Scholar] [CrossRef]
- Huang, B.; Guo, S.; Zhang, Y.; Lin, P.; Lin, C.; Chen, M.; Zhu, S.; Huang, L.; He, J.; Zhang, L.; et al. MiR-223-3p alleviates trigeminal neuropathic pain in the male mouse by targeting MKNK2 and MAPK/ERK signaling. Brain Behav. 2022, 12, e2634. [Google Scholar] [CrossRef]
- Jasmin, L.; Vit, J.P.; Bhargava, A.; Ohara, P.T. Can satellite glial cells be therapeutic targets for pain control? Neuron Glia Biol. 2010, 6, 63–71. [Google Scholar] [CrossRef]
- Goto, T.; Oh, S.B.; Takeda, M.; Shinoda, M.; Sato, T.; Gunjikake, K.K.; Iwata, K. Recent advances in basic research on the trigeminal ganglion. J. Physiol. Sci. 2016, 66, 381–386. [Google Scholar] [CrossRef]
- Takeda, M.; Tanimoto, T.; Kadoi, J.; Nasu, M.; Takahashi, M.; Kitagawa, J.; Matsumoto, S. Enhanced excitability of nociceptive trigeminal ganglion neurons by satellite glial cytokine following peripheral inflammation. Pain 2007, 129, 155–166. [Google Scholar] [CrossRef]
- Takeda, M.; Kitagawa, J.; Takahashi, M.; Matsumoto, S. Activation of interleukin-1beta receptor suppresses the voltage-gated potassium currents in the small-diameter trigeminal ganglion neurons following peripheral inflammation. Pain 2008, 139, 594–602. [Google Scholar] [CrossRef]
- Takeda, M.; Takahashi, M.; Matsumoto, S. Contribution of the activation of satellite glia in sensory ganglia to pathological pain. Neurosci. Biobehav. Rev. 2009, 33, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Wang, D.; Xu, J.; Zhang, H.; Yu, W. New Insights on the Role of Satellite Glial Cells. Stem Cell Rev. Rep. 2022. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Takahashi, M.; Matsumoto, S. Contribution of activated interleukin receptors in trigeminal ganglion neurons to hyperalgesia via satellite glial interleukin-1beta paracrine mechanism. Brain Behav. Immun. 2008, 22, 1016–1023. [Google Scholar] [CrossRef] [PubMed]
- Donegan, M.; Kernisant, M.; Cua, C.; Jasmin, L.; Ohara, P.T. Satellite glial cell proliferation in the trigeminal ganglia after chronic constriction injury of the infraorbital nerve. Glia 2013, 61, 2000–2008. [Google Scholar] [CrossRef] [PubMed]
- Kung, L.H.; Gong, K.; Adedoyin, M.; Ng, J.; Bhargava, A.; Ohara, P.T.; Jasmin, L. Evidence for glutamate as a neuroglial transmitter within sensory ganglia. PLoS ONE 2013, 8, e68312. [Google Scholar] [CrossRef] [PubMed]
- Suadicani, S.O.; Cherkas, P.S.; Zuckerman, J.; Smith, D.N.; Spray, D.C.; Hanani, M. Bidirectional calcium signaling between satellite glial cells and neurons in cultured mouse trigeminal ganglia. Neuron Glia Biol. 2010, 6, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Y.; Gu, Y.; Chen, Y. Communication between neuronal somata and satellite glial cells in sensory ganglia. Glia 2013, 61, 1571–1581. [Google Scholar] [CrossRef]
- Fan, W.; Zhu, X.; He, Y.; Zhu, M.; Wu, Z.; Huang, F.; He, H. The role of satellite glial cells in orofacial pain. J. Neurosci. Res. 2019, 97, 393–401. [Google Scholar] [CrossRef]
- Matsuka, Y.; Afroz, S.; Dalanon, J.C.; Iwasa, T.; Waskitho, A.; Oshima, M. The role of chemical transmitters in neuron-glia interaction and pain in sensory ganglion. Neurosci. Biobehav. Rev. 2020, 108, 393–399. [Google Scholar] [CrossRef]
- Neumann, S.; Doubell, T.P.; Leslie, T.; Woolf, C.J. Inflammatory pain hypersensitivity mediated by phenotypic switch in myelinated primary sensory neurons. Nature 1996, 384, 360–364. [Google Scholar] [CrossRef]
- Takeda, M.; Tanimoto, T.; Ikeda, M.; Nasu, M.; Kadoi, J.; Shima, Y.; Ohta, H.; Matsumoto, S. Temporomandibular joint inflammation potentiates the excitability of trigeminal root ganglion neurons innervating the facial skin in rats. J. Neurophysiol. 2005, 93, 2723–2738. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Takahashi, M.; Hara, N.; Matsumoto, S. Glial cell line-derived neurotrophic factor modulates the excitability of nociceptive trigeminal ganglion neurons via a paracrine mechanism following inflammation. Brain Behav. Immun. 2013, 28, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.Y.; Huang, L.Y. Peripheral inflammation sensitizes P2X receptor-mediated responses in rat dorsal root ganglion neurons. J. Neurosci. 2002, 22, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Lolignier, S.; Eijkelkamp, N.; Wood, J.N. Mechanical allodynia. Pflug. Arch. 2015, 467, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Bongenhielm, U.; Boissonade, F.M.; Westermark, A.; Robinson, P.P.; Fried, K. Sympathetic nerve sprouting fails to occur in the trigeminal ganglion after peripheral nerve injury in the rat. Pain 1999, 82, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.; Chung, J.M. Sympathetic sprouting in the dorsal root ganglion after spinal nerve ligation: Evidence of regenerative collateral sprouting. Brain Res. 2001, 895, 204–212. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korczeniewska, O.A.; Kohli, D.; Benoliel, R.; Baddireddy, S.M.; Eliav, E. Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain. Biomolecules 2022, 12, 1753. https://doi.org/10.3390/biom12121753
Korczeniewska OA, Kohli D, Benoliel R, Baddireddy SM, Eliav E. Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain. Biomolecules. 2022; 12(12):1753. https://doi.org/10.3390/biom12121753
Chicago/Turabian StyleKorczeniewska, Olga A., Divya Kohli, Rafael Benoliel, Sita Mahalakshmi Baddireddy, and Eli Eliav. 2022. "Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain" Biomolecules 12, no. 12: 1753. https://doi.org/10.3390/biom12121753
APA StyleKorczeniewska, O. A., Kohli, D., Benoliel, R., Baddireddy, S. M., & Eliav, E. (2022). Pathophysiology of Post-Traumatic Trigeminal Neuropathic Pain. Biomolecules, 12(12), 1753. https://doi.org/10.3390/biom12121753




