The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review
Abstract
1. Introduction
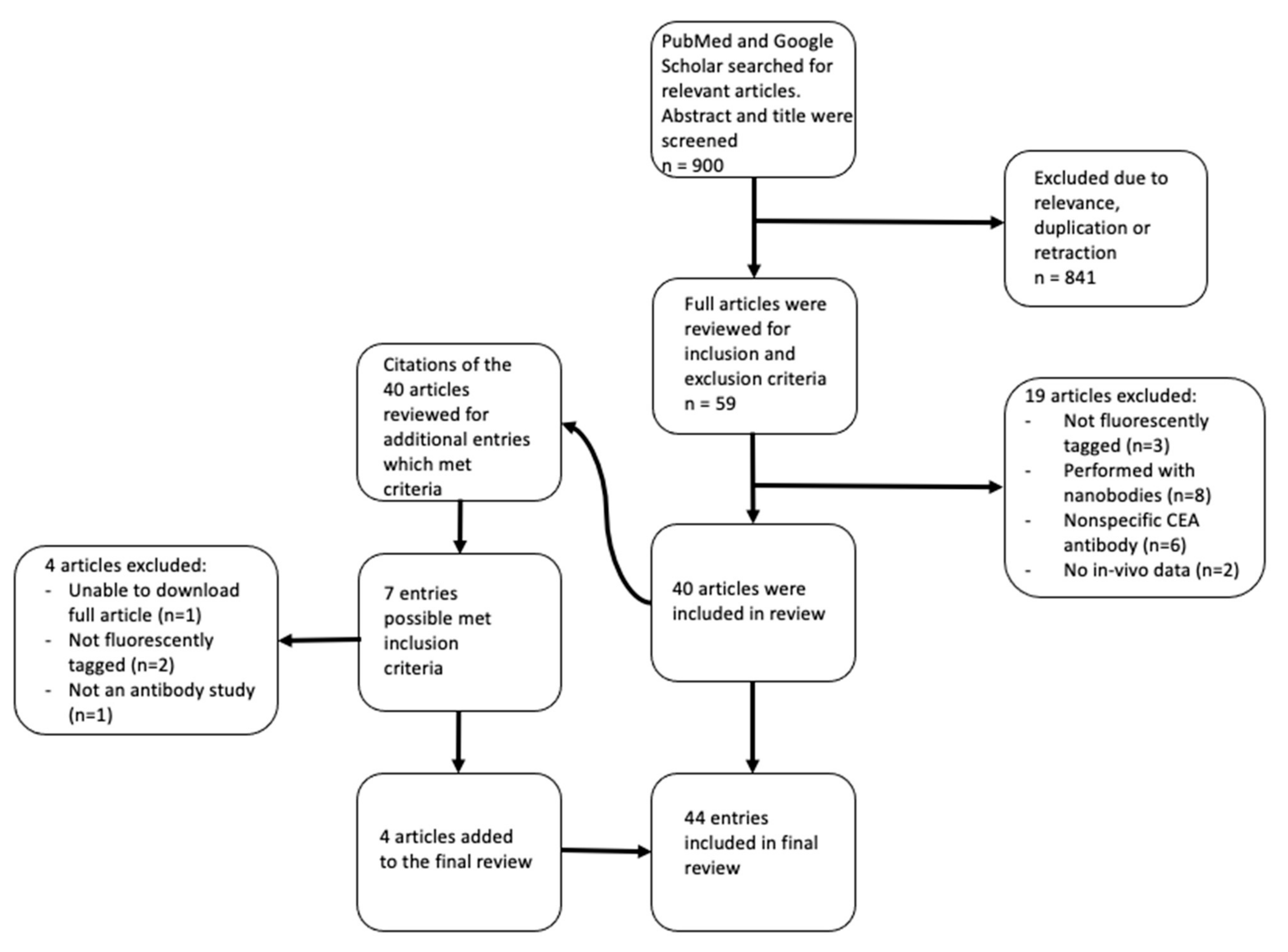
2. Materials and Methods
3. Results
3.1. Colorectal Cancer
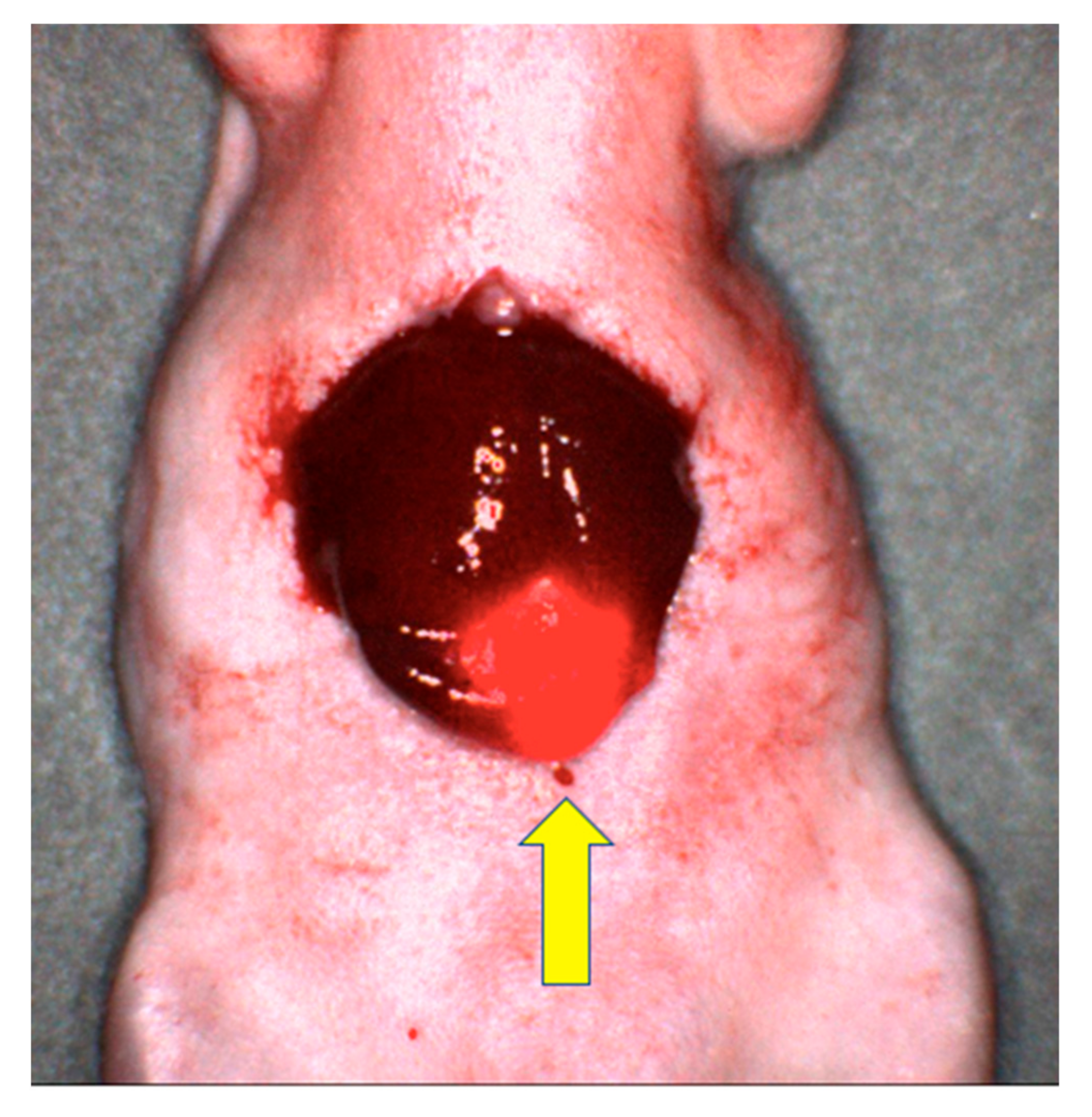
3.1.1. Subcutaneous Mouse Models
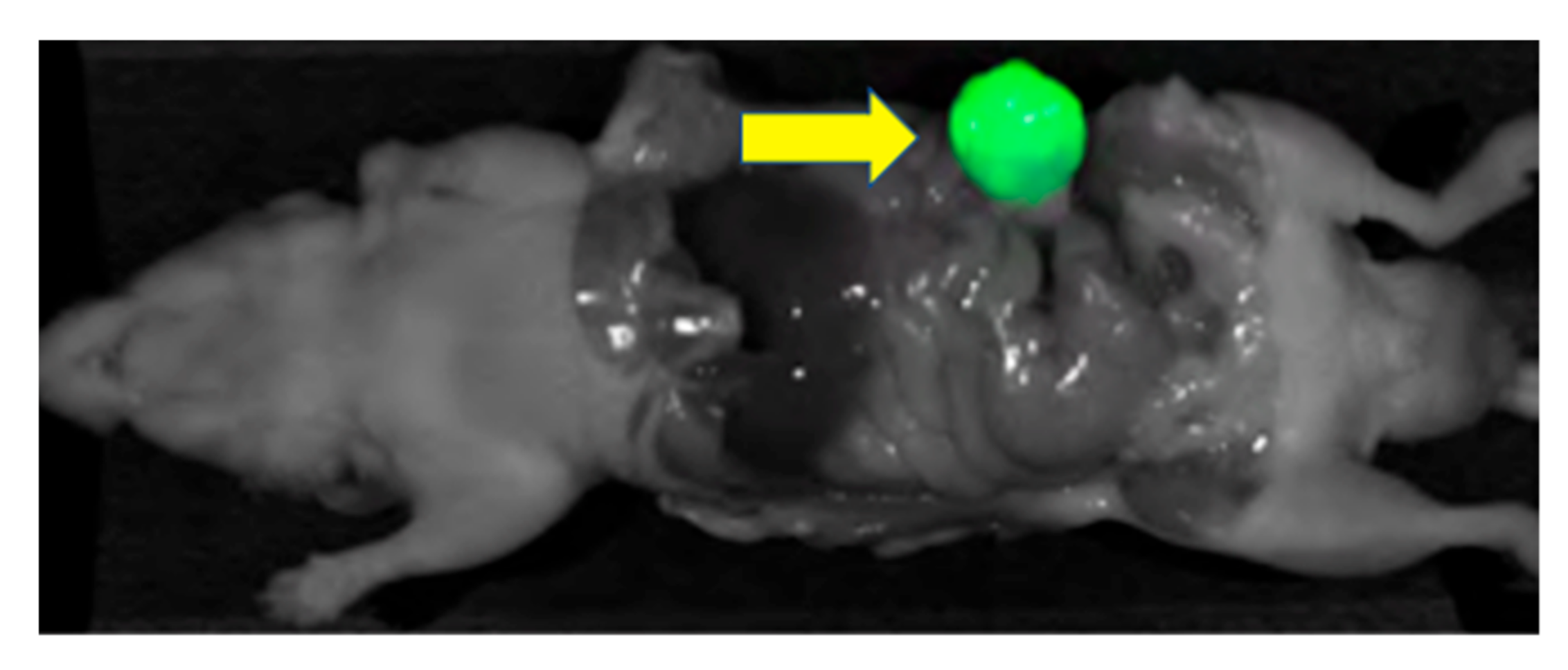
3.1.2. Orthotopic and Intraperitoneal Mouse Models
3.1.3. Clinical Trials
3.2. Pancreatic Cancer
3.2.1. Subcutaneous Mouse Models
3.2.2. Orthotopic and Intraperitoneal Mouse Models
3.2.3. Clinical Trials
3.3. Gastric and Other Cancers
3.3.1. Subcutaneous Mouse Models
3.3.2. Orthotopic and Intraperitoneal Mouse Models
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mieog, J.S.D.; Achterberg, F.B.; Zlitni, A.; Hutteman, M.; Burggraaf, J.; Rutger-Jan, S.; Gioux, S.; Vahrmeijer, A.L. Fundamentals and developments in fluorescence-guided cancer surgery. Nat. Rev. Clin. Oncol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Lwin, T.M.; Hoffman, R.M.; Bouvet, M. Unique Benefits of Tumor-Specific Nanobodies for Fluorescence Guided Surgery. Biomolecules 2021, 11, 311. [Google Scholar] [CrossRef]
- Bouvet, M.; Hoffman, R.M. Glowing Tumors Make for Better Detection and Resection. Sci. Transl. Med. 2011, 3, 110fs10. [Google Scholar] [CrossRef] [PubMed]
- Orosco, R.K.; Tapia, V.J.; Califano, J.A.; Clary, B.; Cohen, E.E.W.; Kane, C.; Lippman, S.M.; Messer, K.; Molinolo, A.; Murphy, J.D.; et al. Positive Surgical Margins in the 10 Most Common Solid Cancers. Sci. Rep. 2018, 8, 5686. [Google Scholar] [CrossRef]
- Hermanek, P.; Wittekind, C. The pathologist and the residual tumor (R) classification. Pathol. Res. Pract. 1994, 190, 115–123. [Google Scholar] [CrossRef]
- Kitai, T.; Inomoto, T.; Miwa, M.; Shikayama, T. Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer Tokyo Jpn. 2005, 12, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Kusano, M.; Tajima, Y.; Yamazaki, K.; Kato, M.; Watanabe, M.; Miwa, M. Sentinel node mapping guided by indocyanine green fluorescence imaging: A new method for sentinel node navigation surgery in gastrointestinal cancer. Dig. Surg. 2008, 25, 103–108. [Google Scholar] [CrossRef]
- Gotoh, K.; Yamada, T.; Ishikawa, O.; Takahasi, H.; Eguchi, H.; Yano, M.; Ohigashi, H.; Tomita, Y.; Miyamoto, Y.; Imaoka, S. A novel image-guided surgery of hepatocellular carcinoma by indocyanine green fluorescence imaging navigation. J. Surg. Oncol. 2009, 100, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, V.C.; Jaffe, S.; Rajasekaran, K.; Cannady, S.B.; Shanti, R.M.; Lee, J.Y.K.; Newman, J.G. Intraoperative Imaging with Second Window Indocyanine Green for Head and Neck Lesions and Regional Metastasis. Otolaryngol. Head Neck Surg. Off. J. Am. Acad. Otolaryngol. Head Neck Surg. 2019, 161, 539–542. [Google Scholar] [CrossRef]
- Zhao, S.; Wu, J.; Wang, C.; Liu, H.; Dong, X.; Shi, C.; Shi, C.; Liu, Y.; Teng, L.; Han, D.; et al. Intraoperative fluorescence-guided resection of high-grade malignant gliomas using 5-aminolevulinic acid-induced porphyrins: A systematic review and meta-analysis of prospective studies. PLoS ONE 2013, 8, e63682. [Google Scholar] [CrossRef]
- Broekx, S.; Weyns, F.; de Vleeschouwer, S. 5-Aminolevulinic acid for recurrent malignant gliomas: A systematic review. Clin. Neurol. Neurosurg. 2020, 195, 105913. [Google Scholar] [CrossRef] [PubMed]
- Tiernan, J.P.; Perry, S.L.; Verghese, E.T.; West, N.P.; Yeluri, S.; Jayne, D.G.; Hughes, T.A. Carcinoembryonic antigen is the preferred biomarker for in vivo colorectal cancer targeting. Br. J. Cancer 2013, 108, 662–667. [Google Scholar] [CrossRef]
- Hammarström, S. The carcinoembryonic antigen (CEA) family: Structures, suggested functions and expression in normal and malignant tissues. Semin. Cancer Biol. 1999, 9, 67–81. [Google Scholar] [CrossRef]
- Beauchemin, N.; Arabzadeh, A. Carcinoembryonic antigen-related cell adhesion molecules (CEACAMs) in cancer progression and metastasis. Cancer Metastasis Rev. 2013, 32, 643–671. [Google Scholar] [CrossRef]
- Pèlegrin, A.; Folli, S.; Buchegger, F.; Mach, J.-P.; Wagnières, G.; Bergh, H.V.D. Antibody–fluorescein conjugates for photoimmunodiagnosis of human colon carcinoma in nude mice. Cancer 1991, 67, 2529–2537. [Google Scholar] [CrossRef]
- Berk, D.A.; Yuan, F.; Leunig, M.; Jain, R.K. Direct in vivo measurement of targeted binding in a human tumor xenograft. Proc. Natl. Acad. Sci. USA 1997, 94, 1785–1790. [Google Scholar] [CrossRef] [PubMed]
- Lisy, M.-R.; Goermar, A.; Thomas, C.; Pauli, J.; Resch-Genger, U.; Kaiser, W.A.; Hilger, I. In Vivo Near-infrared Fluorescence Imaging of Carcinoembryonic Antigen–expressing Tumor Cells in Mice. Radiology 2008, 247, 779–787. [Google Scholar] [CrossRef]
- Kaushal, S.; McElroy, M.K.; Talamini, M.A.; Moossa, A.R.; Bouvet, M. Fluorophore-conjugated anti-CEA Antibody for the Intraoperative Imaging of Pancreatic and Colorectal Cancer. J. Gastrointest. Surg. 2008, 12, 1938–1950. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X. Near-Infrared Fluorescent Imaging of Pancreatic Cancer in Mice Using a Novel Antibody to CEACAM5. Ph.D. Thesis, Kiel University, Kiel, Germany, 2021. Available online: https://macau.uni-kiel.de/receive/macau_mods_00001232 (accessed on 29 August 2021).
- Lu, Z.; Pham, T.T.; Rajkumar, V.; Yu, Z.; Pedley, R.B.; Årstad, E.; Maher, J.; Yan, R. A Dual Reporter Iodinated Labeling Reagent for Cancer Positron Emission Tomography Imaging and Fluorescence-Guided Surgery. J. Med. Chem. 2018, 61, 1636–1645. [Google Scholar] [CrossRef]
- Metildi, C.A.; Kaushal, S.; Luiken, G.A.; Talamini, M.A.; Hoffman, R.M.; Bouvet, M. Fluorescently labeled chimeric anti-CEA antibody improves detection and resection of human colon cancer in a patient-derived orthotopic xenograft (PDOX) nude mouse model. J. Surg. Oncol. 2014, 109, 451–458. [Google Scholar] [CrossRef]
- Hiroshima, Y.; Maawy, A.; Metildi, C.A.; Zhang, Y.; Uehara, F.; Miwa, S.; Yano, S.; Sato, S.; Murakami, T.; Momiyama, M.; et al. Successful Fluorescence-Guided Surgery on Human Colon Cancer Patient-Derived Orthotopic Xenograft Mouse Models Using a Fluorophore-Conjugated Anti-CEA Antibody and a Portable Imaging System. J. Laparoendosc. Adv. Surg. Tech. 2014, 24, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, M.C.; Tolner, B.; Schaafsma, B.E.; Boogerd, L.S.F.; Prevoo, H.A.J.M.; Bhavsar, G.; Kuppen, P.J.K.; Sier, C.F.M.; Bonsing, B.A.; Frangioni, J.V.; et al. Preclinical evaluation of a novel CEA-targeting near-infrared fluorescent tracer delineating colorectal and pancreatic tumors. Int. J. Cancer 2015, 137, 1910–1920. [Google Scholar] [CrossRef] [PubMed]
- DeLong, J.C.; Murakami, T.; Yazaki, P.J.; Hoffman, R.M.; Bouvet, M. Near-infrared-conjugated humanized anti-carcinoembryonic antigen antibody targets colon cancer in an orthotopic nude-mouse model. J. Surg. Res. 2017, 218, 139–143. [Google Scholar] [CrossRef]
- Hiroshima, Y.; Lwin, T.M.; Murakami, T.; Maawy, A.A.; Kuniya, T.; Chishima, T.; Endo, I.; Clary, B.M.; Hoffman, R.; Bouvet, M. Effective fluorescence-guided surgery of liver metastasis using a fluorescent anti-CEA antibody. J. Surg. Oncol. 2016, 114, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Gutowski, M.; Carcenac, M.; Pourquier, D.; Larroque, C.; Saint-Aubert, B.; Rouanet, P.; Pèlegrin, A. Intraoperative immunophotodetection for radical resection of cancers: Evaluation in an experimental model. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2001, 7, 1142–1148. [Google Scholar]
- Rijpkema, M.; Oyen, W.J.; Bos, D.; Franssen, G.M.; Goldenberg, D.M.; Boerman, O.C. SPECT- and Fluorescence Image–Guided Surgery Using a Dual-Labeled Carcinoembryonic Antigen–Targeting Antibody. J. Nucl. Med. 2014, 55, 1519–1524. [Google Scholar] [CrossRef][Green Version]
- Hekman, M.C.H.; Rijpkema, M.; Bos, D.L.; Oosterwijk, E.; Goldenberg, D.M.; Mulders, P.F.A.; Boerman, O.C. Detection of Micrometastases Using SPECT/Fluorescence Dual-Modality Imaging in a CEA-Expressing Tumor Model. J. Nucl. Med. 2017, 58, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Maawy, A.A.; Hiroshima, Y.; Zhang, Y.; Luiken, G.A.; Hoffman, R.M.; Bouvet, M. Polyethylene glycol (PEG) linked to near infrared (NIR) dyes conjugated to chimeric anti-carcinoembryonic antigen (CEA) antibody enhances imaging of liver metastases in a nude-mouse model of human colon cancer. PLoS ONE 2014, 9, e97965. [Google Scholar] [CrossRef]
- Gutowski, M.; Framery, B.; Boonstra, M.C.; Garambois, V.; Quenet, F.; Dumas, K.; Scherninski, F.; Cailler, F.; Vahrmeijer, A.L.; Pèlegrin, A. SGM-101: An innovative near-infrared dye-antibody conjugate that targets CEA for fluorescence-guided surgery. Surg. Oncol. 2017, 26, 153–162. [Google Scholar] [CrossRef]
- Nishino, H.; Turner, M.A.; Amirfakhri, S.; Hollandsworth, H.M.; Lwin, T.M.; Yamamoto, J.; Framery, B.; Cailler, F.; Hoffman, R.M.; Bouvet, M. Spectrally Distinct Double Labeling of Colon-Cancer Liver Metastases and Adjacent Liver Segment with a Near-Infrared-labeled Anti-Carcinoembryonic Antigen (CEA) Antibody and Indocyanine Green in an Orthotopic Mouse Model | Elsevier Enhanced Reader. J. Am. Coll. Surg. 2021, 233, S154. [Google Scholar] [CrossRef]
- Mitsunaga, M.; Ogawa, M.; Kosaka, N.; Rosenblum, L.T.; Choyke, P.L.; Kobayashi, H. Cancer cell–selective in vivo near infrared photoimmunotherapy targeting specific membrane molecules. Nat. Med. 2011, 17, 1685–1691. [Google Scholar] [CrossRef] [PubMed]
- Shirasu, N.; Yamada, H.; Shibaguchi, H.; Kuroki, M.; Kuroki, M. Potent and specific antitumor effect of CEA-targeted photoimmunotherapy. Int. J. Cancer 2014, 135, 2697–2710. [Google Scholar] [CrossRef] [PubMed]
- Elekonawo, F.M.K.; Bos, D.L.; Goldenberg, D.M.; Boerman, O.C.; Rijpkema, M. Carcinoembryonic antigen-targeted photodynamic therapy in colorectal cancer models. EJNMMI Res. 2019, 9, 108. [Google Scholar] [CrossRef] [PubMed]
- Hollandsworth, H.M.; Amirfakhri, S.; Filemoni, F.; Molnar, J.; Hoffman, R.M.; Yazaki, P.J.; Bouvet, M. Near-infrared photoimmunotherapy is effective treatment for colorectal cancer in orthotopic nude-mouse models. PLoS ONE 2020, 15, e0234643. [Google Scholar] [CrossRef]
- Boogerd, L.S.F.; Hoogstins, C.E.S.; Schaap, D.P.; Kusters, M.; Handgraaf, H.J.M.; van der Valk, M.J.M.; Hilling, D.E.; Holman, F.A.; Peeters, K.C.M.J.; Mieog, J.S.D.; et al. Safety and effectiveness of SGM-101, a fluorescent antibody targeting carcinoembryonic antigen, for intraoperative detection of colorectal cancer: A dose-escalation pilot study. Lancet Gastroenterol. Hepatol. 2018, 3, 181–191. [Google Scholar] [CrossRef]
- De Valk, K.S.; Deken, M.M.; Schaap, D.P.; Meijer, R.P.; Boogerd, L.S.; Hoogstins, C.E.; van der Valk, M.J.; Kamerling, I.M.; Bhairosingh, S.S.; Framery, B.; et al. Dose-Finding Study of a CEA-Targeting Agent, SGM-101, for Intraoperative Fluorescence Imaging of Colorectal Cancer. Ann. Surg. Oncol. 2021, 28, 1832–1844. [Google Scholar] [CrossRef]
- Schaap, D.P.; de Valk, K.S.; Deken, M.M.; Meijer, R.P.J.; Burggraaf, J.; Vahrmeijer, A.L.; Kusters, M. Carcinoembryonic antigen-specific, fluorescent image-guided cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for metastatic colorectal cancer. Br. J. Surg. 2020, 107, 334–337. [Google Scholar] [CrossRef]
- Folli, S.; Wagnières, G.; Pèlegrin, A.; Calmes, J.M.; Braichotte, D.; Buchegger, F.; Chalandon, Y.; Hardman, N.; Heusser, C.; Givel, J.C.; et al. Immunophotodiagnosis of colon carcinomas in patients injected with fluoresceinated chimeric antibodies against carcinoembryonic antigen. Proc. Natl. Acad. Sci. USA 1992, 89, 7973–7977. [Google Scholar] [CrossRef] [PubMed]
- Keller, R.; Winde, G.; Terpe, H.J.; Foerster, E.C.; Domschke, W. Fluorescence Endoscopy Using a Fluorescein-Labeled Monoclonal Antibody Against Carcinoembryonic Antigen in Patients with Colorectal Carcinoma and Adenoma. Endoscopy 2002, 34, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Elekonawo, F.M.K.; de Gooyer, J.M.; Boerman, O.C.; Bremers, A.J.A.; Aarnntzen, E.; Nagtegaal, I.D.; Rijpkema, M.; de Wilt, J.H.W. Multimodal image-guided surgery of colorectal peritoneal carcinomatosis: A phase 1 clinical trial. In Improving the Surgical Treatment of Peritoneal Metastases of Colorectal Origin; Radbound University: Nijmegen, The Netherlands, 2020; pp. 184–201. [Google Scholar]
- Knutson, S.; Raja, E.; Bomgarden, R.; Nlend, M.; Chen, A.; Kalyanasundaram, R.; Desai, S. Development and Evaluation of a Fluorescent Antibody-Drug Conjugate for Molecular Imaging and Targeted Therapy of Pancreatic Cancer. PLoS ONE 2016, 11, e0157762. [Google Scholar] [CrossRef]
- Maawy, A.A.; Hiroshima, Y.; Zhang, Y.; Luiken, G.A.; Hoffman, R.M.; Bouvet, M. Specific tumor labeling enhanced by polyethylene glycol linkage of near infrared dyes conjugated to a chimeric anti-carcinoembryonic antigen antibody in a nude mouse model of human pancreatic cancer. J. Biomed. Opt. 2014, 19, 101504. [Google Scholar] [CrossRef] [PubMed]
- Maawy, A.A.; Hiroshima, Y.; Kaushal, S.; Luiken, G.A.; Hoffman, R.M.; Bouvet, M. Comparison of a chimeric anti-carcinoembryonic antigen antibody conjugated with visible or near-infrared fluorescent dyes for imaging pancreatic cancer in orthotopic nude mouse models. J. Biomed. Opt. 2013, 18, 126016. [Google Scholar] [CrossRef]
- Metildi, C.A.; Kaushal, S.; Lee, C.; Hardamon, C.R.; Synder, C.S.; Luiken, G.A.; Talamini, M.A.; Hoffman, R.M.; Bouvet, M. An LED light source and novel fluorophore combinations improve fluorescence laparoscopic detection of metastatic pancreatic cancer in orthotopic mouse models. J. Am. Coll. Surg. 2012, 214, 997–1007. [Google Scholar] [CrossRef]
- Tran Cao, H.S.; Kaushal, S.; Metildi, C.A.; Menen, R.S.; Lee, C.; Synder, C.S.; Messer, K.; Pu, M.; Luiken, G.A.; Talamini, M.A.; et al. Tumor-specific fluorescence antibody imaging enables accurate staging laparoscopy in an orthotopic model of pancreatic cancer. Hepatogastroenterology 2012, 59, 1994–1999. [Google Scholar] [CrossRef]
- Metildi, C.A.; Kaushal, S.; Luiken, G.A.; Hoffman, R.M.; Bouvet, M. Advantages of fluorescence-guided laparoscopic surgery of pancreatic cancer labeled with fluorescent anti-carcinoembryonic antigen antibodies in an orthotopic mouse model. J. Am. Coll. Surg. 2014, 219, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Metildi, C.A.; Kaushal, S.; Pu, M.; Messer, K.A.; Luiken, G.A.; Moossa, A.R.; Hoffman, R.M.; Bouvet, M. Fluorescence-guided Surgery with a Fluorophore-conjugated Antibody to Carcinoembryonic Antigen (CEA), that Highlights the Tumor, Improves Surgical Resection and Increases Survival in Orthotopic Mouse Models of Human Pancreatic Cancer. Ann. Surg. Oncol. 2014, 21, 1405–1411. [Google Scholar] [CrossRef]
- Lwin, T.M.; Murakami, T.; Miyake, K.; Yazaki, P.J.; Shively, J.E.; Hoffman, R.M.; Bouvet, M. Tumor-Specific Labeling of Pancreatic Cancer Using a Humanized Anti-CEA Antibody Conjugated to a Near-Infrared Fluorophore. Ann. Surg. Oncol. 2018, 25, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Yazaki, P.; Lwin, T.M.; Minnix, M.; Li, L.; Sherman, A.; Molnar, J.; Miller, A.; Frankel, P.; Chea, J.; Poku, E.; et al. Improved antibody-guided surgery with a near-infrared dye on a pegylated linker for CEA-positive tumors. J. Biomed. Opt. 2019, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hiroshima, Y.; Maawy, A.; Zhang, Y.; Murakami, T.; Momiyama, M.; Mori, R.; Matsuyama, R.; Katz, M.H.G.; Fleming, J.B.; Chishima, T.; et al. Metastatic Recurrence in a Pancreatic Cancer Patient Derived Orthotopic Xenograft (PDOX) Nude Mouse Model Is Inhibited by Neoadjuvant Chemotherapy in Combination with Fluorescence-Guided Surgery with an Anti-CA 19-9-Conjugated Fluorophore. PLoS ONE 2014, 9, e114310. [Google Scholar] [CrossRef]
- Hiroshima, Y.; Maawy, A.; Zhang, Y.; Murakami, T.; Momiyama, M.; Mori, R.; Matsuyama, R.; Chishima, T.; Tanaka, K.; Ichikawa, Y.; et al. Fluorescence-guided surgery, but not bright-light surgery, prevents local recurrence in a pancreatic cancer patient derived orthotopic xenograft (PDOX) model resistant to neoadjuvant chemotherapy (NAC). Pancreatol. Off. J. Int. Assoc. Pancreatol. IAP Al. 2015, 15, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Lwin, T.M.; Miyake, K.; Murakami, T.; DeLong, J.C.; Amirfakhri, S.; Filemoni, F.; Yoon, S.N.; Yazaki, P.J.; Shivley, J.E.; Datnow, B.; et al. Fluorescent humanized anti-CEA antibody specifically labels metastatic pancreatic cancer in a patient-derived orthotopic xenograft (PDOX) mouse model. Oncotarget 2018, 9, 37333–37342. [Google Scholar] [CrossRef]
- Maawy, A.A.; Hiroshima, Y.; Zhang, Y.; Heim, R.; Makings, L.; Garcia-Guzman, M.; Luiken, G.A.; Kobayshi, H.; Hoffman, R.M.; Bouvet, M. Near Infra-Red Photoimmunotherapy with Anti-CEA-IR700 Results in Extensive Tumor Lysis and a Significant Decrease in Tumor Burden in Orthotopic Mouse Models of Pancreatic Cancer. PLoS ONE 2015, 10, e0121989. [Google Scholar] [CrossRef] [PubMed]
- Hoogstins, C.E.S.; Boogerd, L.S.F.; Mulder, B.G.S.; Mieog, J.S.D.; Swijnenburg, R.J.; van de Velde, C.J.H.; Sarasueta, A.F.; Bonsing, B.A.; Framer, B.; Pèlegrin, A.; et al. Image-Guided Surgery in Patients with Pancreatic Cancer: First Results of a Clinical Trial Using SGM-101, a Novel Carcinoembryonic Antigen-Targeting, Near-Infrared Fluorescent Agent. Ann. Surg. Oncol. 2018, 25, 3350–3357. [Google Scholar] [CrossRef]
- Koga, S.; Oshima, Y.; Honkura, N.; Iimura, T.; Kameda, K.; Sato, K.; Yoshida, M.; Yamamoto, Y.; Watanabe, Y.; Hikita, A.; et al. In vivo subcellular imaging of tumors in mouse models using a fluorophore-conjugated anti-carcinoembryonic antigen antibody in two-photon excitation microscopy. Cancer Sci. 2014, 105, 1299–1306. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Ito, Y.; Matsushima, S.; Tsuchida, D.; Ogasawara, M.; Hasegawa, J.; Misawa, K.; Kondo, E.; Kaneda, N.; Nakanishi, H. New whole-body multimodality imaging of gastric cancer peritoneal metastasis combining fluorescence imaging with ICG-labeled antibody and MRI in mice. Gastric Cancer 2014, 17, 497–507. [Google Scholar] [CrossRef][Green Version]
- Hollandsworth, H.M.; Turner, M.A.; Hoffman, R.M.; Bouvet, M. A review of tumor-specific fluorescence-guided surgery for colorectal cancer. Surg. Oncol. 2021, 36, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, E.L.; Zinn, K.R. Putting Numbers to Fluorescent Guided Surgery. Mol. Imaging Biol. 2013, 15, 647–648. [Google Scholar] [CrossRef]
- Zanetti-Domingues, L.C.; Tynan, C.J.; Rolfe, D.J.; Clarke, D.T.; Martin-Fernandez, M. Hydrophobic fluorescent probes introduce artifacts into single molecule tracking experiments due to non-specific binding. PLoS ONE 2013, 8, e74200. [Google Scholar] [CrossRef]
- Hollandsworth, H.M.; Nishino, H.; Turner, M.; Amirfakhri, S.; Filemoni, F.; Hoffman, R.M.; Yazaki, P.J.; Bouvet, M. Humanized Fluorescent Tumor-associated Glycoprotein-72 Antibody Selectively Labels Colon-cancer Liver Metastases in Orthotopic Mouse Models. In Vivo 2020, 34, 2303–2307. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.A.; Amirfakhri, S.; Nishino, H.; Lwin, T.M.; Savides, T.J.; Reid, T.R.; Singer, B.B.; Hoffman, R.M.; Bouvet, M. A Patient-Derived Orthotopic Xenograft Model of Gastroesophageal-Junction Adenocarcinoma Translated to the Clinic by Tumor-Targeting Fluorescent Antibodies to Carcinoembryonic-Antigen-Related Cell-Adhesion Molecules. In Vivo 2021, 35, 1959–1963. [Google Scholar] [CrossRef] [PubMed]
- Harlaar, N.J.; Koller, M.; de Jongh, S.J.; van Leeuwen, B.L.; Hemmer, P.H.; Kruijff, S.; van Ginkel, R.J.; Been, L.B.; de Jong, J.S.; Kats-Ugurlu, G.; et al. Molecular fluorescence-guided surgery of peritoneal carcinomatosis of colorectal origin: A single-centre feasibility study. Lancet Gastroenterol. Hepatol. 2016, 1, 283–290. [Google Scholar] [CrossRef]
- Park, Y.; Ryu, Y.M.; Jung, Y.; Wang, T.; Baek, Y.; Yoon, Y.; Bae, S.M.; Park, J.; Hwang, S.; Kim, J.; et al. Spraying Quantum Dot Conjugates in the Colon of Live Animals Enabled Rapid and Multiplex Cancer Diagnosis Using Endoscopy. ACS Nano 2014, 8, 8896–8910. [Google Scholar] [CrossRef] [PubMed]
- Keating, J.J.; Runge, J.J.; Singhal, S.; Nims, S.; Venegas, O.; Durham, A.C.; Swain, G.; Nie, S.; Low, P.S.; Holt, D.E. Intraoperative near-infrared fluorescence imaging targeting folate receptors identifies lung cancer in a large-animal model. Cancer 2017, 123, 1051–1060. [Google Scholar] [CrossRef] [PubMed]
- Resch-Genger, U.; Grabolle, M.; Cavaliere-Jaricot, S.; Nitschke, R.; Nann, T. Quantum dots versus organic dyes as fluorescent labels. Nat. Methods 2008, 5, 763–775. [Google Scholar] [CrossRef] [PubMed]
| Title | Author | Year | Model | Antibody | Dye | Dose | Timing | Tumor |
|---|---|---|---|---|---|---|---|---|
| Antibody-fluorescein conjugates for photoimmunodiagnosis of human colon carcinoma in nude mice [15] | Pèlegrin, A. | 1991 | Mice | MoAB 35 (Murine) | Fluorescein | 20 μg | 6–96 h | T380 (human CRC) subcutaneous (SQ) |
| Immunophotodiagnosis of colon carcinomas in patients injected with fluoresceinated chimeric antibodies against carcinoembryonic antigen [39] | Folli, S. | 1992 | Human | CGP44290 (Murine) | Fluorescein isothyocyanate | 4.5 mg 9 mg | 24 h | known primary CRC |
| Direct in vivo measurement of targeted binding in a human tumor xenograft [16] | Berk, D.A. | 1997 | Mice | ZCE025 (Murine) | Fluorescein | 20–6000 μg | 10 m–24 h | LS174T SQ |
| Intraoperative immunophotodetection for radical resection of cancers [26] | Gutowski, M. | 2001 | Mice | 35A7 (Murine) | ICG | 10, 40, 100 μg | 48 h | LS174T IP cell injection |
| Fluorescence endoscopy using a fluorescein-labeled monoclonal antibody against carcinoembryonic antigen in patients with colorectal carcinoma and adenoma [40] | Keller, R. | 2002 | Human | Monoclonal (Murine) | FLOUS | 2–6 mL | 10 min | 27 patients with large colonic lesions |
| In vivo near-infrared fluorescence imaging of carcinoembryonic antigen-expressing tumor cells in mice [17] | Lisy, M. | 2008 | Mice | Arcitumomab (Chimeric) | DY-676 | 40 μg | 2–24 h | LS174T SQ |
| Fluorophore-conjugated anti-CEA antibody for the intraoperative imaging of pancreatic and colorectal cancer [18] | Kaushal, S. | 2008 | Mice | Monoclonal (Murine) | AlexaFluor 488 | 75 μg | 24 h | BxPC3 SQ Colo4104 (CRC) SQ and cecal orthotopic |
| An LED light source and novel fluorophore combinations improve fluorescence laparoscopic detection of metastatic pancreatic cancer in orthotopic mouse models [45] | Metildi, C. | 2012 | Mice | Monoclonal (Murine) | Alexa 448 Alexa 555 | 75 μg | 24 h | BxPC3 pancreatic orthotopic |
| Tumor-specific fluorescence antibody imaging enables accurate staging laparoscopy in an orthotopic model of pancreatic cancer [46] | Tran Cao, H.S. | 2012 | Mice | Monoclonal (Murine) | Alexa Fluor 488 | 75 μg | 24 h | BxPC3 pancreatic orthotopic BxPC3 IP cell injection |
| New whole-body multimodality imaging of gastric cancer peritoneal metastasis combining fluorescence imaging with ICG-labeled antibody and MRI in mice [57] | Ito, A. | 2013 | Mice | HB 8747 (Murine) | XenoLight CF750 | 0.05 mg | 10 m–7 d | MKN-28 (gastric cancer cell line), GCIY (gastric cancer cell line), GLM-1, GLM -2 (patient derived gastric cancer liver metastasis) IP models |
| Comparison of a chimeric anti-carcinoembryonic antigen antibody conjugated with visible or near-infrared fluorescent dyes for imaging pancreatic cancer in orthotopic nude mouse models [44] | Maawy, A. | 2013 | Mice | Monoclonal (Chimeric) | 488 nm, 550 nm, 650 nm, 750 nm | 50–75 μg (1.25 μmol of dye) | 24 h | BxPC3 pancreatic orthotopic |
| SPECT- and fluorescence image-guided surgery using a dual-labeled carcinoembryonic antigen-targeting antibody [27] | Rijpkema, M. | 2014 | Mice | MN-14 (Murine) | IRDye 800CW | 1–100 μg | 1–8 d | LS174T SQ cell injection LS174T IP cell injection |
| Fluorescently labeled chimeric anti-CEA antibody improves detection and resection of human colon cancer in a patient-derived orthotopic xenograft (PDOX) nude mouse model [21] | Metildi, C. | 2014 | Mice | Monoclonal (Chimeric) | Alexa Fluor 488 | 75 μg | 24 h | Patient derived (PD) CRC orthotopic |
| Successful fluorescence-guided surgery on human colon cancer patient-derived orthotopic xenograft mouse models using a fluorophore-conjugated anti-CEA antibody and a portable imaging system [22] | Hiroshima, Y. | 2014 | Mice | Monoclonal (Murine) | Alexa Fluor 488 | Unspecified | 24 h | PD CRC |
| Specific tumor labeling enhanced by polyethylene glycol linkage of near-infrared dyes conjugated to a chimeric anti-carcinoembryonic antigen antibody in a nude mouse model of human pancreatic cancer [43] | Maawy, A. | 2014 | Mice | Monoclonal (Chimeric) | DyLight 650/750 DyLight 650/750 PEG | 2.5 nmol | 5 m–24 h | BxPC3 SQ |
| Polyethylene glycol (PEG) linked to near-infrared (NIR) dyes conjugated to chimeric Anti-Carcinoembryonic Antigen (CEA) antibody enhances imaging of liver metastases in a nude-mouse model of human colon cancer [29] | Maawy, A. | 2014 | Mice | Monoclonal (Chimeric) | DyLight 650/750 DyLight 650/750 PEG | 2.5 nmol (94 μg) | 24 h | HT29 spleen injection |
| Advantages of fluorescence-guided laparoscopic surgery of pancreatic cancer labeled with fluorescent anti-carcinoembryonic antigen antibodies in an orthotopic mouse model [47] | Metildi, C. | 2014 | Mice | Monoclonal (Chimeric) | Alexa Fluor 488 | 75 μg | 24 h | BxPC3-RFP pancreatic orthotopic |
| Fluorescence-guided surgery with a fluorophore-conjugated antibody to carcinoembryonic antigen (CEA), that highlights the tumor, improves surgical resection and increases survival in orthotopic mouse models of human pancreatic cancer [48] | Metildi, C. | 2014 | Mice | Monoclonal (Chimeric) | Alexa Fluor 488 | 75 μg | 24 h | BxPC3-RFP pancreatic ortho |
| Potent and specific antitumor effect of CEA-targeted photoimmunotherapy [33] | Shirasu, N. | 2014 | Mice | C2-45 (Human) | IRDye 700DX NHS Ester | 100, 200 μg | 24 h | MKN-45-luc (gastric cancer) SQ cell injection |
| In vivo subcellular imaging of tumors in mouse models using a fluorophore-conjugated anti-carcinoembryonic antigen antibody in two-photon excitation microscopy [56] | Koga, S. | 2014 | Mice | CB30 (Murine) | Alexa 594 | 10, 50 μg | 24 h | HT1080 (human fibrosarcoma) SQ cell injection MKN45 (human gastric) SQ cell injection |
| Metastatic recurrence in a pancreatic cancer patient-derived orthotopic xenograft (PDOX) nude mouse model is inhibited by neoadjuvant chemotherapy in combination with fluorescence-guided surgery with an anti-CA 19-9-conjugated fluorophore. [51] | Hiroshima, Y. | 2014 | Mice | Monoclonal (Chimeric) | DyLight 650 | 50 μg | 24 h | PD pancreatic cancer patient-derived orthotopic xenograft (PDOX) |
| Fluorescence-guided surgery, but not bright-light surgery, prevents local recurrence in a pancreatic cancer patient-derived orthotopic xenograft (PDOX) model resistant to neoadjuvant chemotherapy (NAC) [52] | Hiroshima, Y. | 2015 | Mice | Monoclonal (Chimeric) | DyLight 650 | 50 μg | 24 h | PD pancreatic cancer PDOX |
| Near-infrared photoimmunotherapy with anti-CEA-IR700 results in extensive tumor lysis and a significant decrease in tumor burden in orthotopic mouse models of pancreatic cancer [54] | Maawy, A. | 2015 | Mice | Monoclonal (Chimeric) | IRDye 700DX NHS Ester | 100 μg | 24 h | BxPC3 pancreatic orthotopic |
| Preclinical evaluation of a novel CEA-targeting near-infrared fluorescent tracer delineating colorectal and pancreatic tumors [23] | Boonstra, M. | 2015 | Mice | ssSM3E (Humanized) | IRDye 800CW | 28 μg | 8–120 h | HT29 cecal orthotopic BxPC3 cell injection pancreatic ortho |
| Effective fluorescence-guided surgery of liver metastasis using a fluorescent anti-CEA antibody [25] | Hiroshima, Y. | 2016 | Mice | Monoclonal (Chimeric) | DyLight 650 | 50 μg | 24 h–72 h | HT29 liver orthotopic and liver metastasis spleen injection |
| Development and evaluation of a fluorescent antibody-drug conjugate for molecular imaging and targeted therapy of pancreatic cancer [42] | Knutson, S. | 2016 | Mice | Monoclonal (Murine) | DyLight-680-4xPEG | 100 μg | 24 h | BxPC3 SQ |
| Near-infrared-conjugated humanized anti-carcinoembryonic antigen antibody targets colon cancer in an orthotopic nude-mouse model [24] | DeLong, J. | 2017 | Mice | M5A (Humanized) | NHS-IRDye 800CW | 75 μg | 24–48 h | HT29 cecal orthotopic |
| Detection of micrometastases using SPECT/fluorescence dual-modality imaging in a CEA-expressing tumor model [28] | Hekman, M. | 2017 | Mice | Labetuzumab (Humanized) | IRDye 800CW | 10 μg | 3 d | GW-39 (human CRC) cell injection lung metastasis |
| SGM-101: An innovative near-infrared dye-antibody conjugate that targets CEA for fluorescence-guided surgery [30] | Gutowski, M. | 2017 | Mice | SGM-ch511 (Chimeric) | BM104 | 30 μg | 24 h–96 h | LS174T IP model HT29 cecal orthotopic LS174T liver metastasis via spleen BxPC3 pancreatic orthotopic |
| A Dual Reporter Iodinated Labeling Reagent for Cancer Positron Emission Tomography Imaging and Fluorescence-Guided Surgery [20] | Lu, Z. | 2018 | Mice | A5B7 (Murine) | I-Green | 44 μg | 72 h | SW1222 CRC SQ |
| Safety and effectiveness of SGM-101, a fluorescent antibody targeting carcinoembryonic antigen, for intraoperative detection of colorectal cancer: a dose-escalation pilot study [36] | Boogerd, L.S.F. | 2018 | Human | SGM-ch511 (Chimeric) | BM104 | 5–10 mg | 48 h–96 h | CRC |
| Image-guided surgery in patients with pancreatic cancer: First results of a clinical trial using SGM-101, a novel carcinoembryonic antigen-targeting, near-infrared fluorescent agent [55] | Hoogstins, C. | 2018 | Human | SGM-ch511 (Chimeric) | BM104 | 5, 7.5, 10 mg | 48 h, 96 h | PDAC |
| Fluorescent humanized anti-CEA antibody specifically labels metastatic pancreatic cancer in a patient-derived orthotopic xenograft (PDOX) mouse model [53] | Lwin, T.M. | 2018 | Mice | M5A (Humanized) | IRDye 800CW | 75 μg | 48 h | PD pancreatic PDOX |
| Tumor-specific labeling of pancreatic cancer using a humanized anti-CEA antibody conjugated to a near-infrared fluorophore [49] | Lwin, T.M. | 2018 | Mice | M5A (Humanized) | IRDye 800CW | 75 μg | 6–96 h | BxPC3 pancreatic orthotopic |
| Improved antibody-guided surgery with a near-infrared dye on a pegylated linker for CEA-positive tumors [50] | Yazaki, P.J. | 2019 | Mice | M5A (Humanized) | NHS-IRDye 800CW PEGylated | 75 μg | 24–96 h | BxPC3 pancreatic orthotopic |
| Carcinoembryonic antigen-targeted photodynamic therapy in colorectal cancer models [34] | Elekonawo, F. | 2019 | Mice | Labetuzumab (Humanized) | IRDye 700DX NHS Ester | 30 μg | LOVO SQ cell injection | |
| Near-infrared photoimmunotherapy is effective treatment for colorectal cancer in orthotopic nude-mouse models [35] | Hollandsworth, H.M. | 2020 | athymic nude mice | M5A (Humanized) | IRDye 700DX NHS Ester | 50 μg | 24 h | LS174T cecal orthotopic |
| Carcinoembryonic antigen-specific, fluorescent image-guided cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for metastatic colorectal cancer [38] | Schaap, D.P. | 2020 | Human | SGM-ch511 (Chimeric) | BM104 | 10–15 mg | 4–6 d | peritoneal metastatic CRC |
| Multimodal image-guided surgery of colorectal peritoneal carcinomatosis: a phase 1 clinical trial [41] | Elekonawo, F. | 2020 | Human | Labetuzumab (Humanized) | IRDye 800CW | 2 or 5 mg | 5–6 days | Colorectal peritoneal metastasis |
| Near-infrared fluorescent imaging of pancreatic cancer in mice using a novel antibody to CEACAM 5 [19] | Zhou, X. | 2021 | Mice | C1P83 | IRDye 800CW | 25 μg (SQ model) 25, 100 μg (ortho) | 24 h–6 d | C15A3 CRC SQ BxPC3 pancreatic orthotopic |
| Spectrally distinct double labeling of colon-cancer liver metastases and adjacent liver segment with a near-infrared-labeled anti-Carcinoembryonic antigen (CEA_ antibody and indocyanine green in an orthotopic mouse model. [31] | Nishino, H. | 2021 | Mice | SGM-ch511 (Chimeric) | BM104 | Unspecified | 48 h–96 h | LS174T liver orthotopic |
| Dose-finding study of a CEA-targeting agent, SGM-101, for intraoperative fluorescence imaging of colorectal cancer [37] | de Valk, K. | 2021 | Human | SGM-ch511 (Chimeric) | BM104 | 5–15 mg | 24 h–6 d | CRC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turner, M.A.; Lwin, T.M.; Amirfakhri, S.; Nishino, H.; Hoffman, R.M.; Yazaki, P.J.; Bouvet, M. The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review. Biomolecules 2021, 11, 1819. https://doi.org/10.3390/biom11121819
Turner MA, Lwin TM, Amirfakhri S, Nishino H, Hoffman RM, Yazaki PJ, Bouvet M. The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review. Biomolecules. 2021; 11(12):1819. https://doi.org/10.3390/biom11121819
Chicago/Turabian StyleTurner, Michael A., Thinzar M. Lwin, Siamak Amirfakhri, Hiroto Nishino, Robert M. Hoffman, Paul J. Yazaki, and Michael Bouvet. 2021. "The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review" Biomolecules 11, no. 12: 1819. https://doi.org/10.3390/biom11121819
APA StyleTurner, M. A., Lwin, T. M., Amirfakhri, S., Nishino, H., Hoffman, R. M., Yazaki, P. J., & Bouvet, M. (2021). The Use of Fluorescent Anti-CEA Antibodies to Label, Resect and Treat Cancers: A Review. Biomolecules, 11(12), 1819. https://doi.org/10.3390/biom11121819







