Development of ssDNA Aptamers for Diagnosis and Inhibition of the Highly Pathogenic Avian Influenza Virus Subtype H5N1
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Random ssDNA Library
2.3. SELEX Using the Membrane Filtration Column Method
2.4. Analysis of Aptamer Sequences and Secondary Structures
2.5. Optimization of the Reduced Graphene Oxide (rGO)-Based Aptamer Characterization Test
2.6. Aptamer Binding Assay by Fluorescence Recovery Analysis
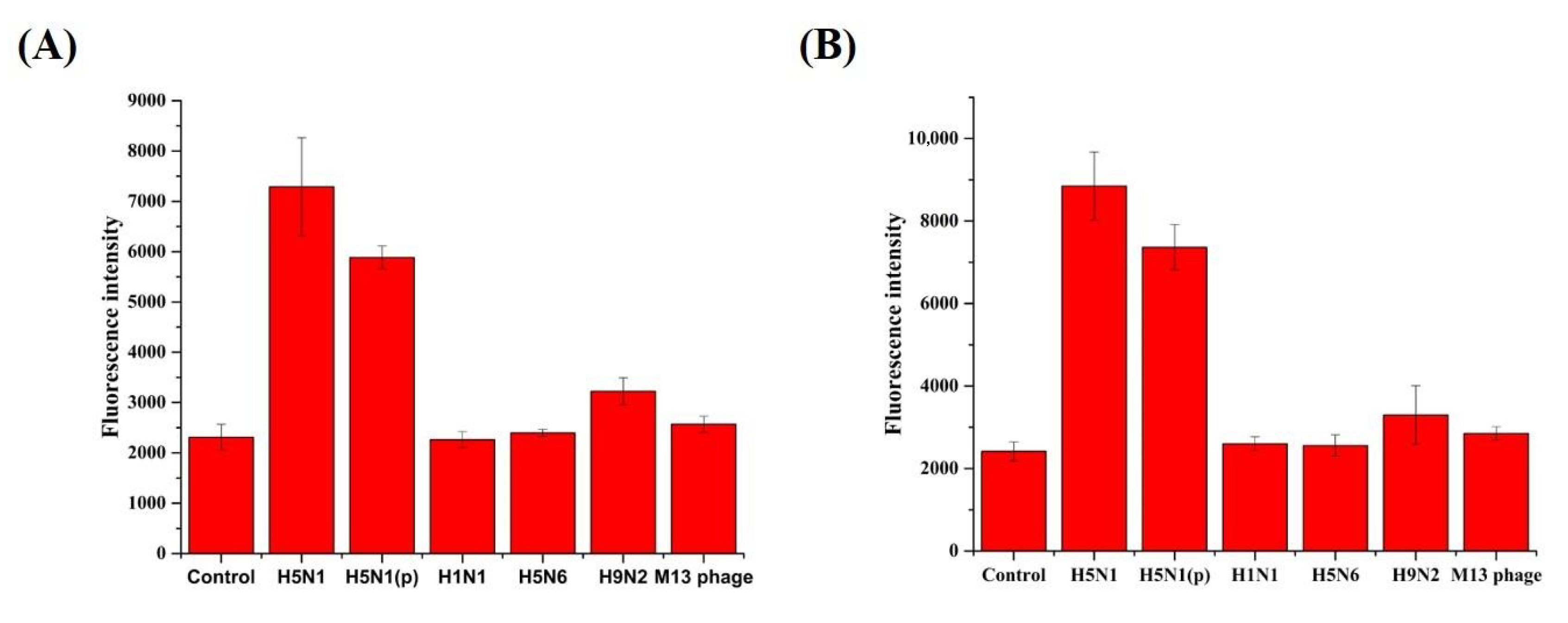
2.7. Aptamer Specificity Test Against Virus Subtypes
2.8. Estimation of the Detection Limit
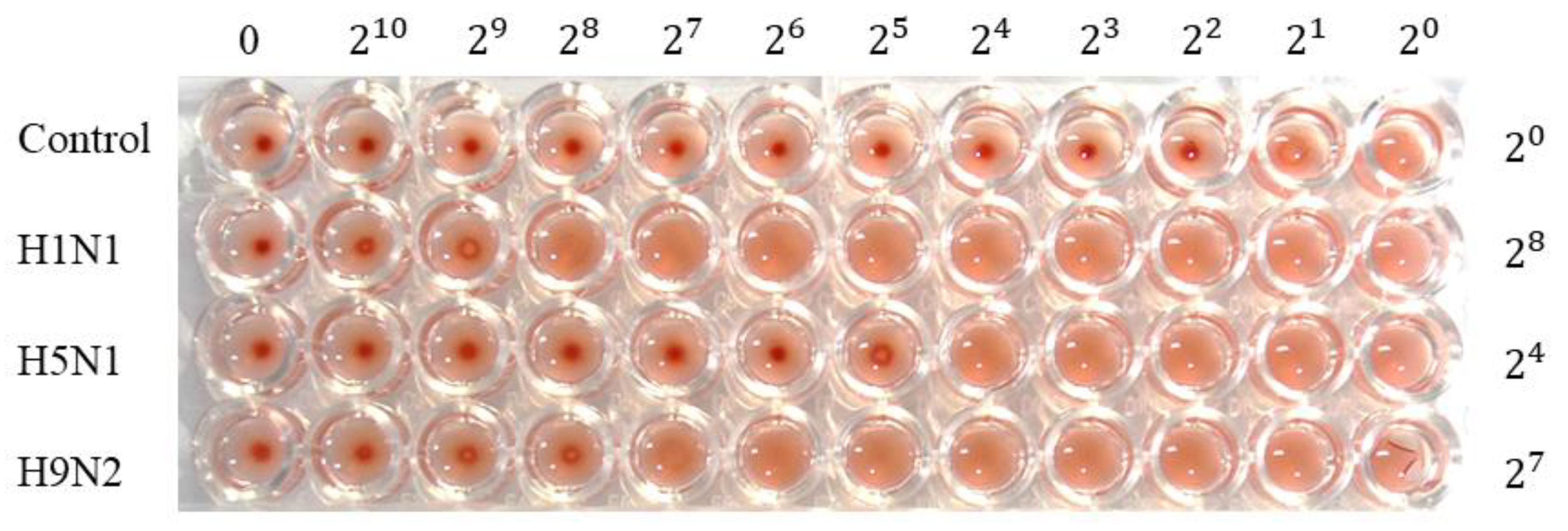
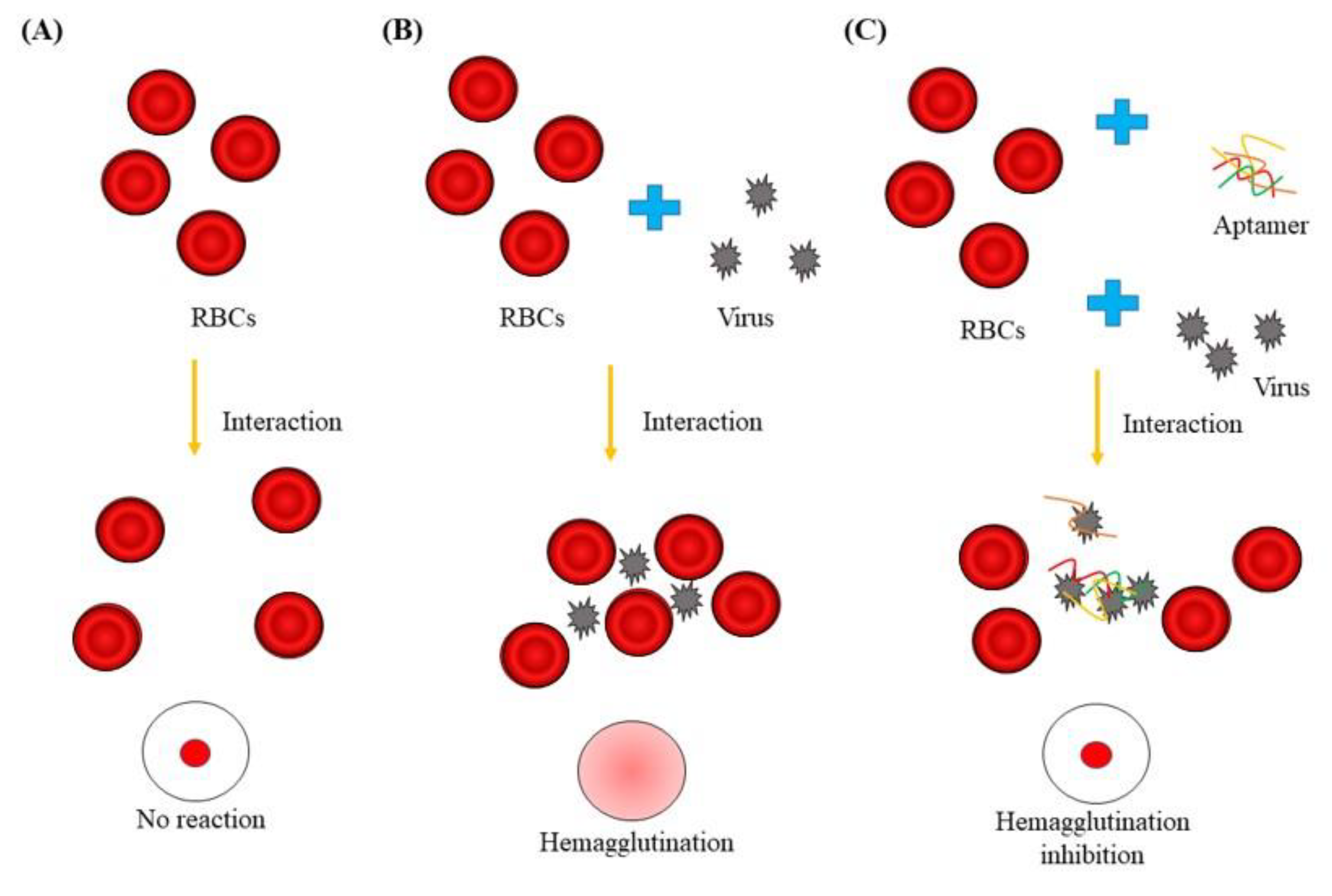
2.9. Hemagglutination Assay
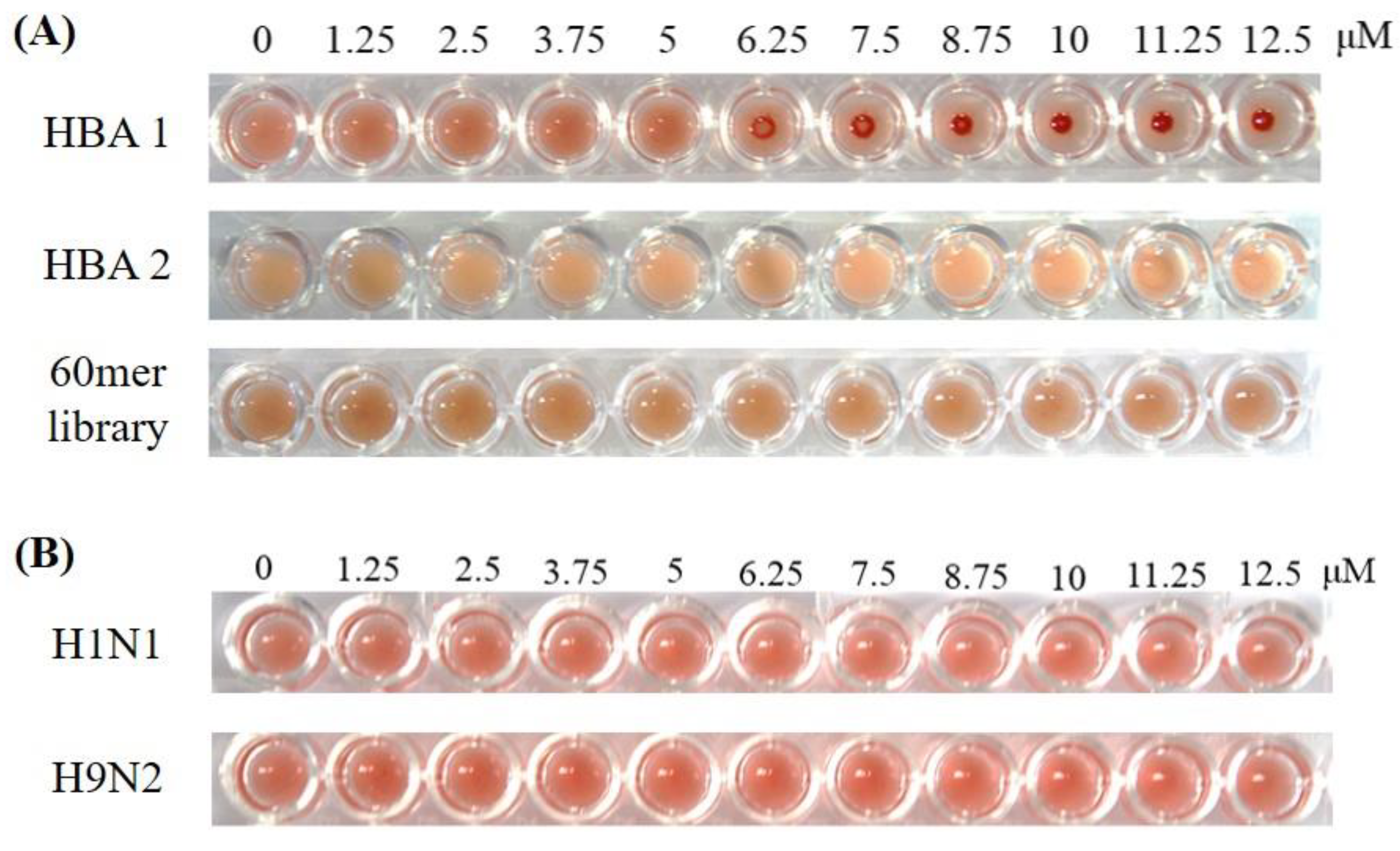
2.10. Hemagglutination Inhibition Assay
2.11. Statistical Analyses
3. Results
3.1. Identification and Structural Analysis of H5N1-Binding Aptamers (HBAs)
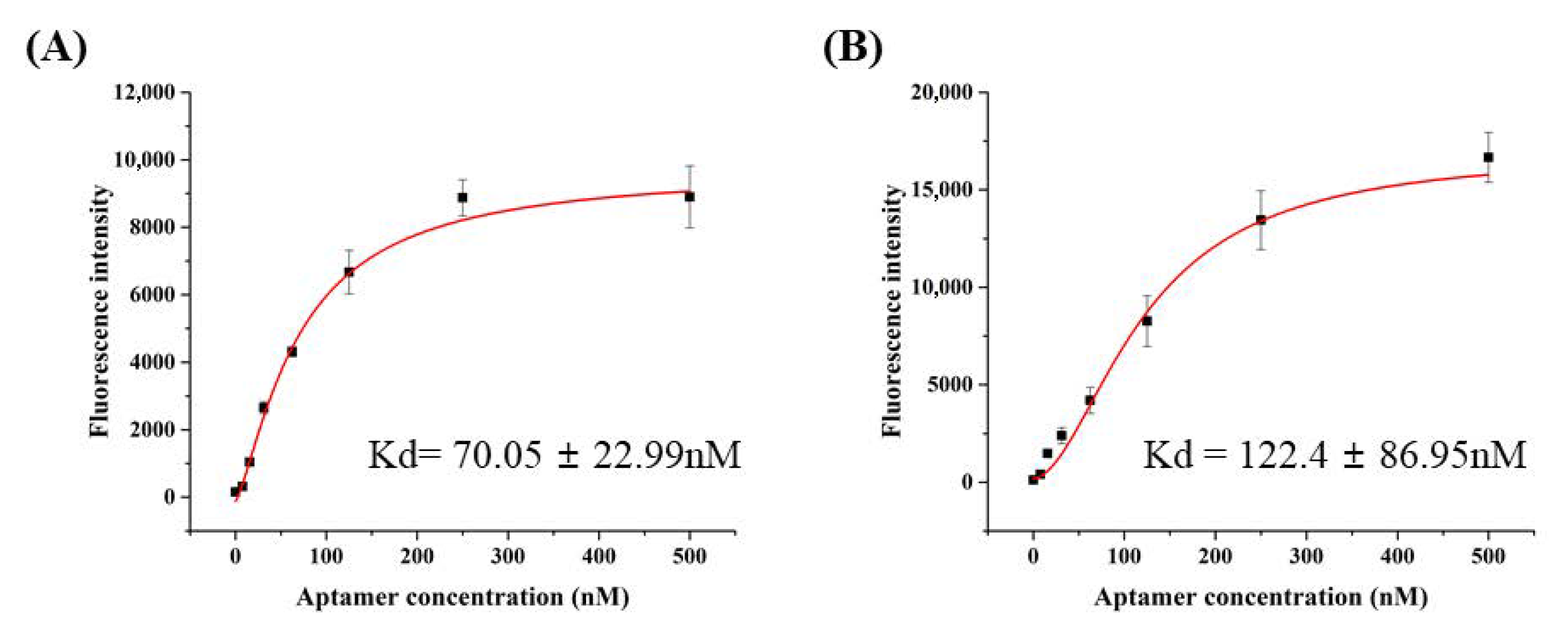
3.2. Characterization of H5N1-Binding Aptamers
3.3. Detection Limit for HBA1 and HBA2
3.4. Hemagglutination Inhibition Assay
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Avian Influenza in Birds. Available online: http://www.cdc.gov/flu/avianflu (accessed on 1 September 2018).
- Guinat, C.; Artois, J.; Bronner, A.; Guérin, J.L.; Gilbert, M.; Paul, M.C. Duck production systems and highly pathogenic avian influenza H5N8 in France 2016–2017. Sci. Rep. 2019, 9, 6177. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Influenza (Avian and other Zoonotic). Available online: http://www.who.int/news-room/fact-sheets/detail/influenza (accessed on 13 November 2018).
- Nuradji, H.; Payne, J.; Harper, J.; Lowther, S.; Wibawa, H.; Long, N.T.; Meers, J.; Bingham, J. Highly Pathogenic Avian Influenza (H5N1) Virus in Feathers. Vet. Pathol. 2016, 54, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Suenaga, E.; Kumar, P.K. An aptamer that binds efficiently to the hemagglutinins of highly pathogenic avian influenza viruses (H5N1 and H7N7) and inhibits hemagglutinin–glycan interactions. Acta Biomater. 2014, 10, 1314–1323. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Sun, L.; Xiong, J.; Wang, C.; Chen, L.; Yang, P.; Yu, H.; Yan, Q.; Cheng, Y.; Jiang, L.; et al. Semiaquatic mammals might be intermediate hosts to spread avian influenza viruses from avian to human. Sci. Rep. 2019, 9, 11641. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Avian Influenza A Virus Infections in Humans. Available online: https://www.cdc.gov/flu/avianflu/avian-in-humans.htm (accessed on 18 April 2017).
- Nagy, A.; Jiřinec, T.; Jiřincová, H.; Černíková, L.; Havlíčková, M. In silico re-assessment of a diagnostic RT-qPCR assay for universal detection of Influenza A viruses. Sci. Rep. 2019, 9, 1630. [Google Scholar] [CrossRef]
- Lee, M.H.; Song, K.-Y.; Hwang, H.J.; Kim, J.H.; Hwang, I. Development of fast and sensitive protocols for the detection of viral pathogens using a small portable convection PCR platform. Mol. Biol. Rep. 2019, 46, 5073–5077. [Google Scholar] [CrossRef]
- Al-Attar, M.Y.; Danial, F.A.; Al-Baroodi, S.Y. Detection of Antibodies Against Avian Influenza Virus in Wild Pigeons and Starlings. J. Anim. Vet. Adv. 2008, 7, 448–449. [Google Scholar]
- El Zowalaty, M.E.; Bustin, S.A.; Husseiny, M.I.; Ashour, H.M. Avian influenza: Virology, diagnosis and surveillance. Future Microbiol. 2013, 8, 1209–1227. [Google Scholar] [CrossRef]
- Govorkova, E.A.; Baranovich, T.; Seiler, P.; Armstrong, J.; Burnham, A.; Guan, Y.; Peiris, M.; Webby, R.J.; Webster, R.G. Antiviral resistance among highly pathogenic influenza A (H5N1) viruses isolated worldwide in 2002–2012 shows need for continued monitoring. Antivir. Res. 2013, 98, 297–304. [Google Scholar] [CrossRef]
- Le, Q.M.; Kiso, M.; Someya, K.; Sakai, Y.T.; Nguyen, T.H.; Nguyen, K.H.L.; Pham, N.D.; Hgyen, H.H.; Yamada, S.; Muramoto, Y.; et al. Avian Flu: Isolation of Drug-Resistant H5N1. Nature 2005, 437, 1108. [Google Scholar] [CrossRef]
- Ilgu, M.; Nilsen-Hamilton, M. Aptamers in analytics. Analyst 2016, 141, 1551–1568. [Google Scholar] [CrossRef] [PubMed]
- Blind, M.; Blank, M. Aptamer Selection Technology and Recent Advances. Mol. Ther. Nucleic Acids 2016, 4, e223. [Google Scholar] [CrossRef]
- Stoltenburg, R.; Reinemann, C.; Strehlitz, B. SELEX—A (r)evolutionary method to generate high-affinity nucleic acid ligands. Biomol. Eng. 2007, 24, 381–403. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Q.; Luo, Y.; Gao, T.; Zhao, Y.; Pei, R. In vitro selection of ssDNA aptamers that can specifically recognize and differentiate riboflavin and its derivative FAD. Talanta 2019, 204, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, X.; Zhang, Q.; Zhang, C.; Liu, Y.; Tu, K.; Tu, J. Selection of DNA aptamers that bind to four organophosphorus pesticides. Biotechnol. Lett. 2012, 34, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Song, K.-M.; Lee, S.; Ban, C. Aptamers and Their Biological Applications. Sensors 2012, 12, 612–631. [Google Scholar] [CrossRef]
- Kim, A.-R.; Ha, N.-R.; Jung, I.-P.; Kim, S.-H.; Yoon, M.-Y. Development of a ssDNA aptamer system with reduced graphene oxide (rGO) to detect nonylphenol ethoxylate in domestic detergent. J. Mol. Recognit. 2018, 32, e2764. [Google Scholar] [CrossRef]
- Choi, J.S.; Kim, S.G.; LaHousse, M.; Park, H.-Y.; Park, H.-C.; Jeong, B.; Kim, J.; Kim, S.-K.; Yoon, M.-Y. Screening and Characterization of High-Affinity ssDNA Aptamers against Anthrax Protective Antigen. J. Biomol. Screen. 2011, 16, 266–271. [Google Scholar] [CrossRef]
- Ha, N.-R.; Lee, S.-C.; Hyun, J.-W.; Yoon, M.-Y. Development of inhibitory ssDNA aptamers for the FtsZ cell division protein from citrus canker phytopathogen. Process. Biochem. 2016, 51, 24–33. [Google Scholar] [CrossRef]
- Chen, Z.; Ruffner, D.E. Modified Crush-and-Soak Method for Recovering Oligodeoxynucleotides from Polyacrylamide Gel. Biotechniques 1996, 21, 820–822. [Google Scholar] [CrossRef]
- Fregel, R.; Gonzalez, A.; Cabrera, V.M. Improved ethanol precipitation of DNA. Electrophororesis 2010, 31, 1350–1352. [Google Scholar] [CrossRef]
- Zuker, M. On finding all suboptimal foldings of an RNA molecule. Science 1989, 244, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Zuker, M. Mfold web serber for nucleic acid folding and hybridization prediction. Nucleic Acids Res. 2003, 31, 3406–3415. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Chao, J.; Li, Z.; Xing, S.; Su, S.; Li, X.; Song, S.; Zuo, X.; Fan, C.; Liu, B.; et al. Graphene Oxide-Assisted Nucleic Acids Assays Using Conjugated Polyelectrolytes-Based Fluorescent Signal Transduction. Anal. Chem. 2015, 87, 3877–3883. [Google Scholar] [CrossRef]
- Eisfeld, A.J.; Neumann, G.; Kawaoka, Y. Influenza A virus isolation, culture and identification. Nat. Protoc. 2014, 9, 2663–2681. [Google Scholar] [CrossRef] [PubMed]
- Ruscito, A.; DeRosa, M.C. Small-Molecule Binding Aptamers: Selection Strategies, Characterization, and Applications. Front. Chem. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Ozer, A.; White, B.S.; Lis, J.T.; Shalloway, D. Density-dependent cooperative non-specific binding in solid-phase SELEX affinity selection. Nucleic Acids Res. 2013, 41, 7167–7175. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gu, H.; Duan, N.; Wu, S.; Hao, L.; Xia, Y.; Ma, X.; Wang, Z. Graphene oxide-assisted non-immobilized SELEX of okdaic acid aptamer and the analytical application of aptasensor. Sci. Rep. 2016, 6, 21665. [Google Scholar] [CrossRef]
- Yang, K.-A.; Pei, R.; Stojanovic, M.N. In Vitro selection and amplification protocols for isolation of aptameric sensors for small molecules. Methods 2016, 106, 58–65. [Google Scholar] [CrossRef]
- Hasegawa, H.; Savory, N.; Abe, K.; Ikebukuro, K. Methods for Improving Aptamer Binding Affinity. Molecules 2016, 21, 421. [Google Scholar] [CrossRef]
- Xi, G.; Wang, X.; Chen, T. A reduced graphene oxide-based fluorescence resonance energy transfer sensor for highly sensitive detection of matrix metalloproteinase 2. Int. J. Nanomed. 2016, 11, 1537–1547. [Google Scholar] [CrossRef]
- Park, J.-W.; Tatavarty, R.; Kim, D.W.; Jung, H.-T.; Gu, M.B. Immobilization-free screening of aptamers assisted by graphene oxide. Chem. Commun. 2012, 48, 2071–2073. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; He, B.; Li, C.; Zhang, X.; Wu, W.; Yin, X.; Fan, B.; Fan, X.; Wang, J. Real-time RT-PCR for H5N1 avian influenza A virus detection. J. Med. Microbiol. 2007, 56, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhu, Y.; Xue, F.; Mei, Z.; Yao, L.; Wang, X.; Zheng, L.; Liu, J.; Liu, G.; Peng, C.; et al. Recent trends in SELEX technique and its application to food safety monitoring. Microchim. Acta 2014, 181, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Kanagarajan, S.; Tolf, C.; Lundgren, A.; Waldenström, J.; Brodelius, P.E. Transient Expression of Hemagglutinin Antigen from Low Pathogenic Avian Influenza A (H7N7) in Nicotiana benthamiana. PLoS ONE 2012, 7, e33010. [Google Scholar] [CrossRef]
- Shen, X.; Zhang, X.; Liu, S. Novel hemagglutinin-based influenza virus inhibitors. J. Thorac. Dis. 2013, 5, S149–S159. [Google Scholar]
- Truelove, S.; Zhu, H.; Lessler, J.; Riley, S.; Read, J.M.; Wang, S.; Kwok, K.O.; Guan, Y.; Jiang, C.Q.; Cummings, D.A.T. A comparison of hemagglutination inhibition and neutralization assays for characterizing immunity to seasonal influenza A. Influ. Other Respir. Viruses 2016, 10, 518–524. [Google Scholar] [CrossRef]
- Trombetta, C.M.; Remarque, E.J.; Mortier, D.; Montomoli, E. Comparison of hemagglutination inhibition, single radial hemolysis, virus neutralization assays, and ELISA to detect antibody levels against seasonal influenza viruses. Influ. Other Respir. Viruses 2018, 12, 675–686. [Google Scholar] [CrossRef]

| No. | F-Random Sequence-R | Frequency |
|---|---|---|
| 1 | GCGACCGTGTCAGCGGGGACTAGCGGTGTA | 13/41 |
| 2 | GGGTCTGAGGAGTGCGCGGTGCCAGTGAGT | 9/41 |
| 3 | GGGGGCTTGGACCGAGCGGTGTACGGCGCG | 3/41 |
| 4 | CGATCCACGAGAGTGCGCCCTGCATCCGAC | 2/41 |
| 5 | CGACGGCAGAGAGGCGCGGCGTCCCTTCGGTCC | 2/41 |
| 6 | GCCGTCAAGGGGTCAGTCACGGAAGCAAAG | 2/41 |
| 7 | GGTGTGGTTACACAGCCCGGACCGCCATGC | 1/41 |
| 8 | TCCCGGAGCAGCGGCAGCGTCCGGCTCT | 1/41 |
| 9 | GCATCGCAGTCACGCATGCGGAGTACGCCT | 1/41 |
| 10 | CCAGTGGATGGGGCGTGGGTTAGCTGCCGGAGG | 1/41 |
| 11 | TAGTCAGCAAGGTTCGCGGACCGGCGGGGT | 1/41 |
| 12 | GACGAAACGGAGGTGCGGCCCCTGCTGCC | 1/41 |
| 13 | GCGACCGTGTCAGCGGGGACTAGCGGTGTA | 1/41 |
| 14 | ACGTGAGCTTGTGCTGGACCTTGGCCACCC | 1/41 |
| 15 | GATGGGCGGCGTTCGCAGGGATCTGGCTGT | 1/41 |
| 16 | CAGGCACGACGTCGGGTCATCTGCAGCTCG | 1/41 |
| F(5′-ATGCGGATCCCGCGC-3′) R(5′-GCGCGAAGCTTGCGC-3′) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-H.; Choi, J.-W.; Kim, A.-R.; Lee, S.-C.; Yoon, M.-Y. Development of ssDNA Aptamers for Diagnosis and Inhibition of the Highly Pathogenic Avian Influenza Virus Subtype H5N1. Biomolecules 2020, 10, 1116. https://doi.org/10.3390/biom10081116
Kim S-H, Choi J-W, Kim A-R, Lee S-C, Yoon M-Y. Development of ssDNA Aptamers for Diagnosis and Inhibition of the Highly Pathogenic Avian Influenza Virus Subtype H5N1. Biomolecules. 2020; 10(8):1116. https://doi.org/10.3390/biom10081116
Chicago/Turabian StyleKim, Sang-Heon, Jae-Woo Choi, A-Ru Kim, Sang-Choon Lee, and Moon-Young Yoon. 2020. "Development of ssDNA Aptamers for Diagnosis and Inhibition of the Highly Pathogenic Avian Influenza Virus Subtype H5N1" Biomolecules 10, no. 8: 1116. https://doi.org/10.3390/biom10081116
APA StyleKim, S.-H., Choi, J.-W., Kim, A.-R., Lee, S.-C., & Yoon, M.-Y. (2020). Development of ssDNA Aptamers for Diagnosis and Inhibition of the Highly Pathogenic Avian Influenza Virus Subtype H5N1. Biomolecules, 10(8), 1116. https://doi.org/10.3390/biom10081116





