Endothelial Dysfunction May Link Interatrial Septal Abnormalities and MTHFR-Inherited Defects to Cryptogenic Stroke Predisposition
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Enrolment Criteria
2.2. Laboratory Test
2.3. Echocardiographic Imaging
2.4. Statistical Analysis
3. Results
3.1. Clinical and Laboratory Characteristics of Enrolled Patients
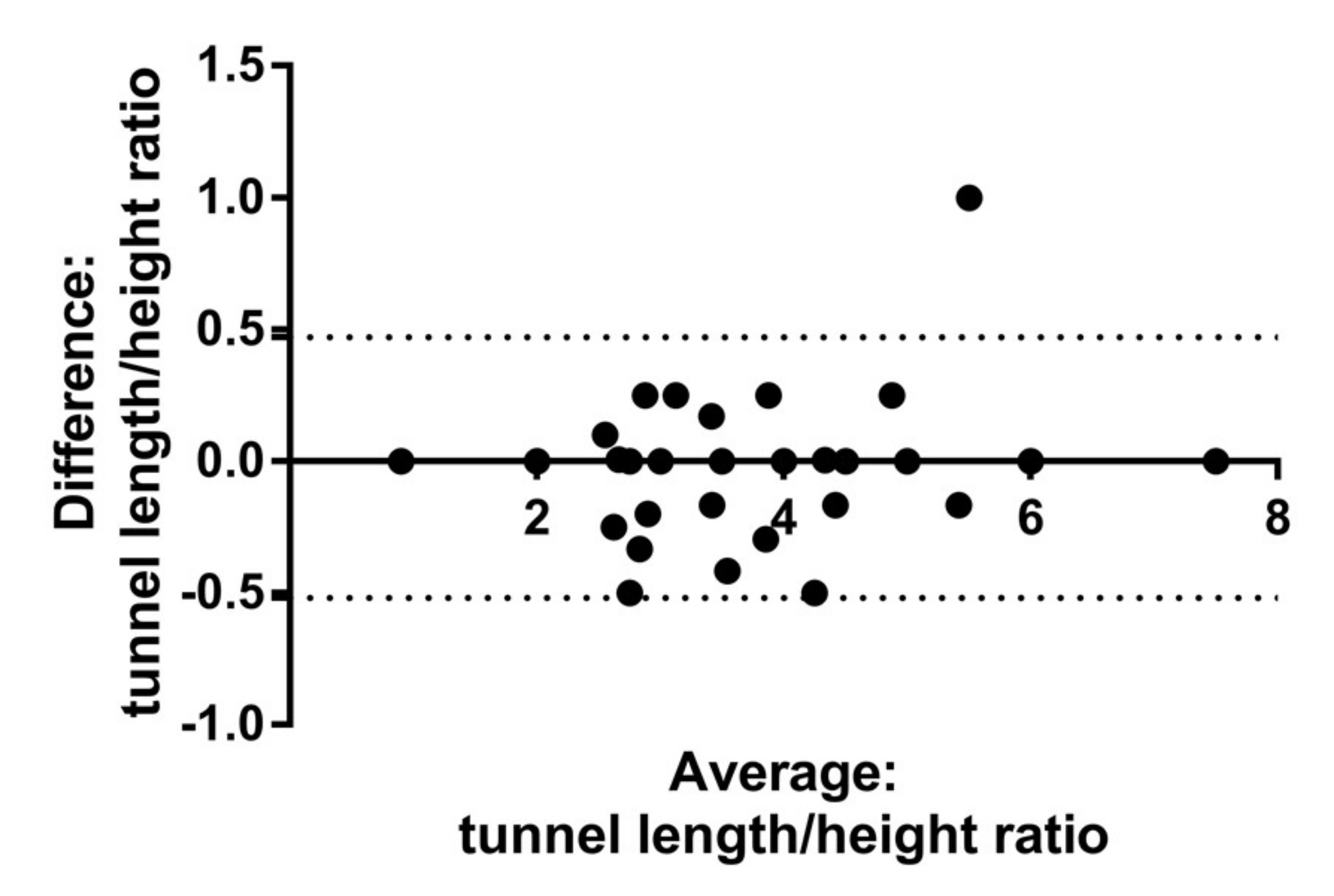
3.2. Morphologic Features of the IAS Defects and Folate-Related Metabolism
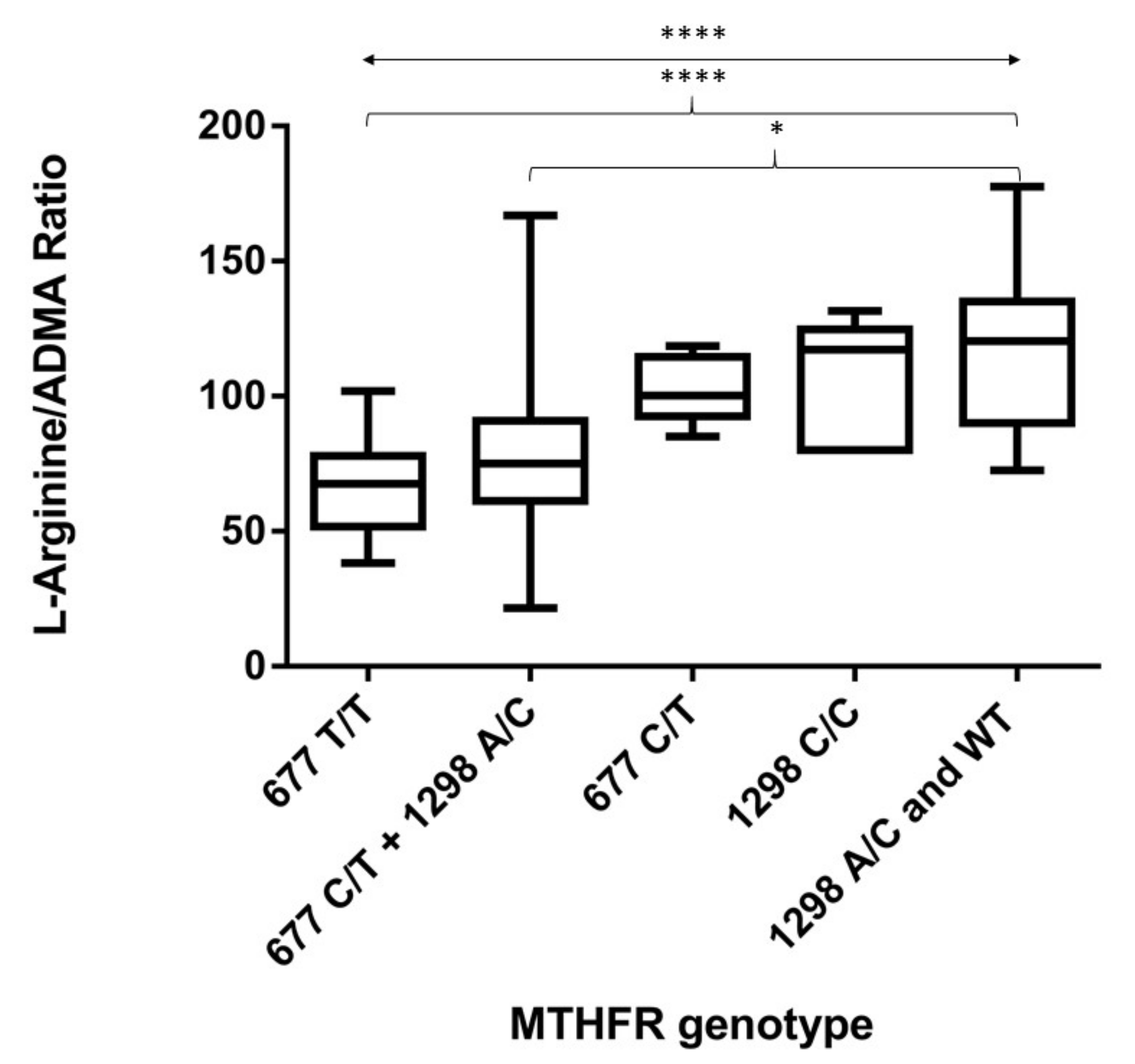
3.3. Distribution of MTHFR Genetic Variants and Folate-Related Metabolism
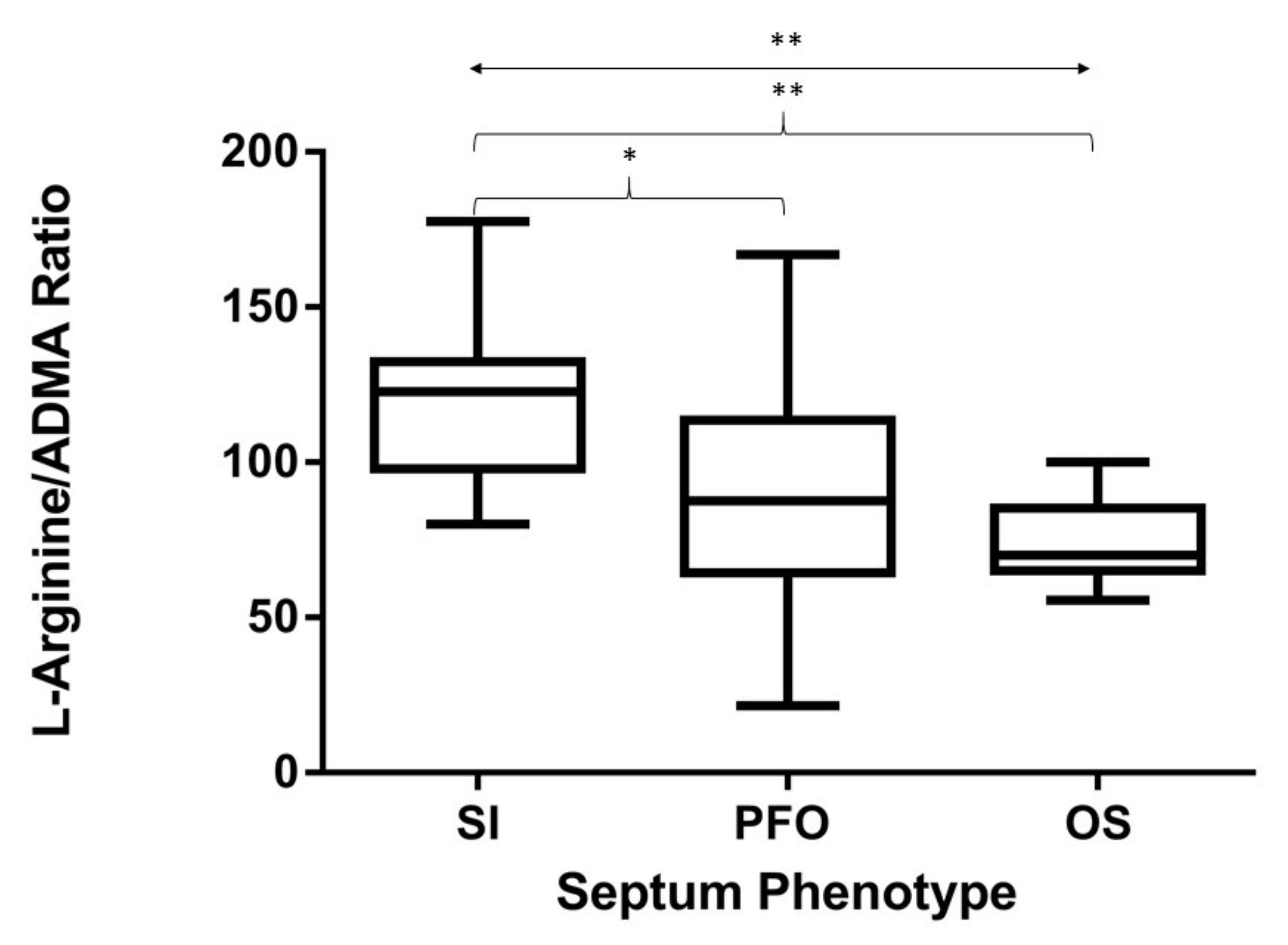
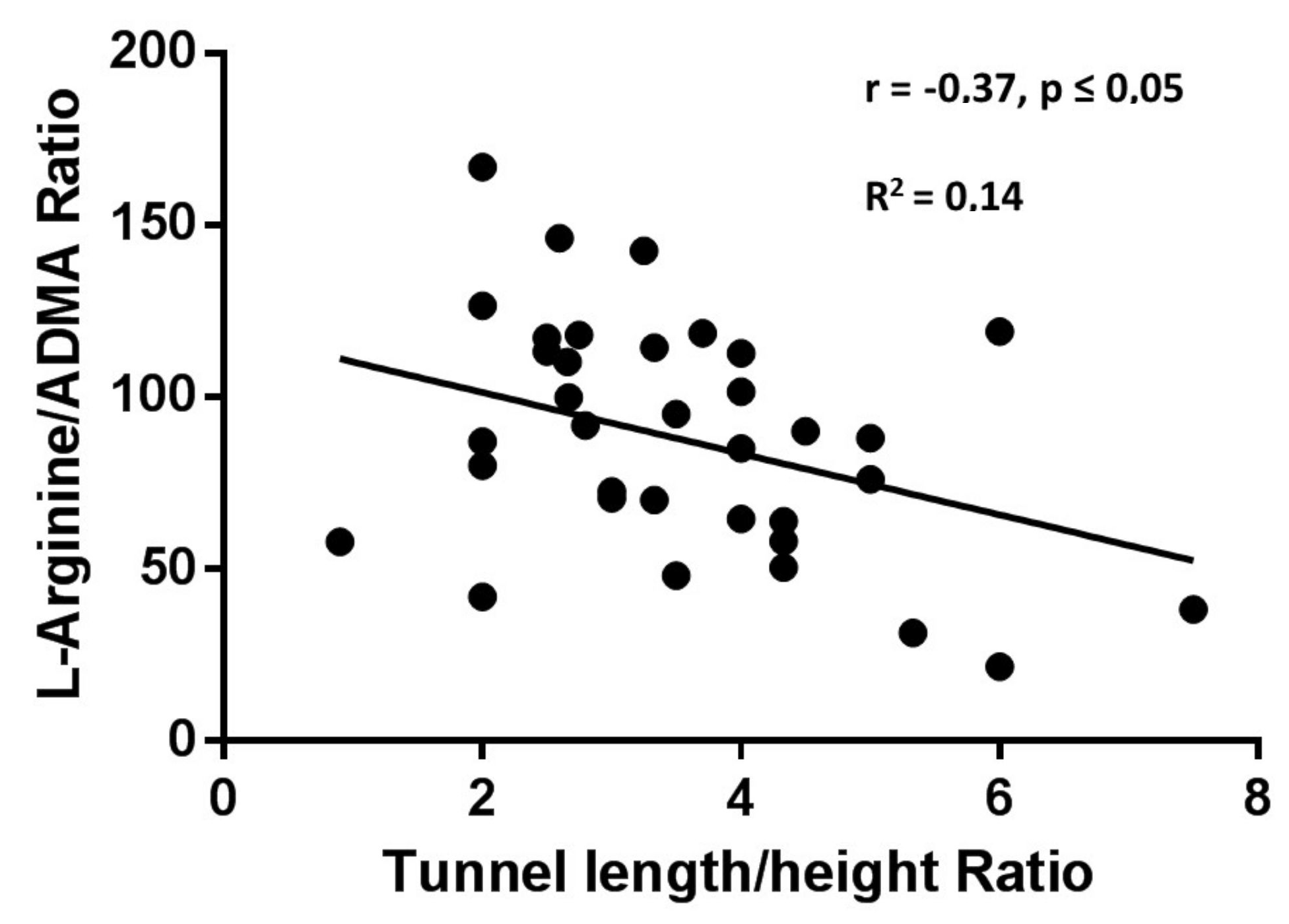
3.4. L-Arg/ADMA Ratio Related to IAS Phenotype and MTHFR Genotype
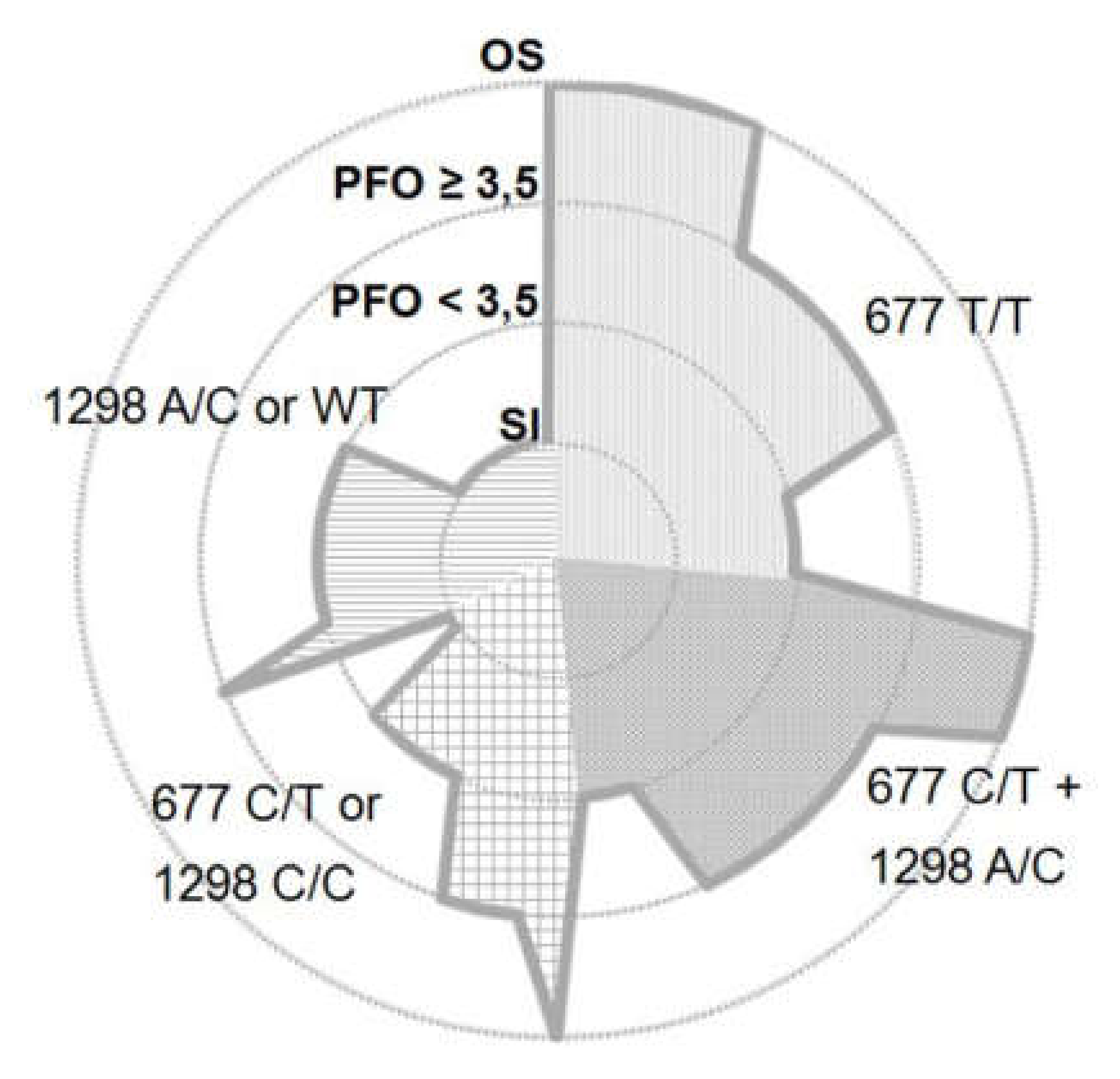
3.5. Distribution of MTHFR Genetic Variants and IAS Phenotype
4. Discussion
4.1. Correlation between the Severity of MTHFR Activity and the Degree of Endothelial Dysfunction
4.2. Correlation between the Degree of Endothelial Dysfunction and the IAS Phenotype
4.3. Relationship between the Severity of MTHFR Activity, the Characteristics of IAS Defects, and Cryptogenic Strokes
5. Limitations of the Study
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| MTHFR | methylene tetrahydrofolate reductase |
| PFO | patent foramen ovale |
| IAS | interatrial septum |
| OS | ostium secundum |
| ADMA | asymmetric dimethylarginine |
References
- Schulz, U.G.R.; Rothwell, P.M. Differences in Vascular Risk Factors between Etiological Subtypes of Ischemic Stroke. Stroke 2003, 34, 2050–2059. [Google Scholar] [CrossRef]
- Marelli, A.; Mackie, A.S.; Ionescu-Ittu, R.; Rahme, E.; Pilote, L. Congenital heart disease in the general population: Changing prevalence and age distribution. Circulation 2007, 115, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Homma, S.; Sacco, R.L. Patent foramen ovale and stroke. Circulation 2005, 112, 1063–1072. [Google Scholar] [CrossRef]
- Furlan, A.; Reisman, M.; Massaro, J.M.; Mauri, L.; Adams, H.; Albers, G.W.; Felberg, R.; Herrmann, H.; Kar, S.; Landzberg, M.; et al. Closure or Medical Therapy for Cryptogenic Stroke with Patent Foramen Ovale. N. Engl. J. Med. 2012, 366, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.D.; Saver, J.L.; Thaler, D.E.; Smalling, R.W.; Berry, S.; Macdonald, L.A.; Marks, D.S.; Tirschwell, D.L. Closure of Patent Foramen Ovale versus Medical Therapy after Cryptogenic Stroke. N. Engl. J. Med. 2013, 368, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Meier, B.; Kalesan, B.; Mattle, H.P.; Khattab, A.A.; Hildick-Smith, D.; Dudek, D.; Andersen, G.; Ibrahim, R.; Schuler, G.; Walton, A.S.; et al. Percutaneous Closure of Patent Foramen Ovale in Cryptogenic Embolism. N. Engl. J. Med. 2013, 368, 1083–1091. [Google Scholar] [CrossRef]
- Kent, D.; Dahabreh, I.J.; Ruthazer, R.; Furlan, A.J.; Reisman, M.; Carroll, J.D.; Saver, J.L.; Smalling, R.W.; Jüni, P.; Mattle, H.P.; et al. Device Closure of Patent Foramen Ovale After Stroke: Pooled Analysis of Completed Randomized Trials. J. Am. Coll. Cardiol. 2016, 67, 907–917. [Google Scholar] [CrossRef]
- Kitsios, G.D.; Thaler, D.E.; Kent, D. Potentially large yet uncertain benefits: A meta-analysis of patent foramen ovale closure trials. Stroke 2013, 44, 2640–2643. [Google Scholar] [CrossRef]
- Homma, S.; Sacco, R.; Tullio, M.; Sciacca, R.; Mohr, J. Effect of medical treatment in stroke patients with patent foramen ovale. patent foramen ovale in cryptogenic stroke study. ACC Curr. J. Rev. 2002, 11, 46. [Google Scholar] [CrossRef]
- Goel, S.S.; Tuzcu, E.M.; Shishehbor, M.H.; De Oliveira, E.I.; Borek, P.P.; Krasuski, R.A.; Rodriguez, L.L.; Kapadia, S.R. Morphology of the Patent Foramen Ovale in Asymptomatic Versus Symptomatic (Stroke or Transient Ischemic Attack) Patients. Am. J. Cardiol. 2009, 103, 124–129. [Google Scholar] [CrossRef]
- Wessler, B.S.; Thaler, D.E.; Ruthazer, R.; Weimar, C.; Di Tullio, M.R.; Elkind, M.S.V.; Homma, S.; Lutz, J.S.; Mas, J.-L.; Mattle, H.P.; et al. Response to letter regarding article, “Transesophageal echocardiography in cryptogenic stroke and patent foramen ovale analysis of putative high-risk features from the risk of paradoxical embolism database”. Circ. Cardiovasc. Imaging 2014, 7, 125–131. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Serena, J.; Marti-Fabregas, J.; Santamarina, E.; Rodriguez, J.J.; Perez-Ayuso, M.J.; Masjuan, J.; Segura, T.; Gallego, J.; Davalos, A. Recurrent stroke and massive right-to-left shunt: Results from the prospective Spanish multicenter (CODICIA) study. Stroke 2008, 39, 3131–3136. [Google Scholar] [CrossRef]
- Katsanos, A.H.; Spence, J.D.; Bogiatzi, C.; Parissis, J.; Giannopoulos, S.; Frogoudaki, A.; Safouris, A.; Voumvourakis, K.; Tsivgoulis, G. Recurrent Stroke and Patent Foramen Ovale. Stroke 2014, 45, 3352–3359. [Google Scholar] [CrossRef]
- Pristipino, C.; Anzola, G.P.; Ballerini, L.; Bartorelli, A.; Cecconi, M.; Chessa, M.; Donti, A.; Gaspardone, A.; Neri, G.; Onorato, E. Multidisciplinary position paper on the management of patent foramen ovale in the presence of cryptogenic cerebral ischemia—Italian version 2013. G. Ital. Cardiol. (Rome) 2013, 14, 699–712. [Google Scholar] [CrossRef]
- Giardini, A.; Donti, A.; Formigari, R.; Bronzetti, G.; Prandstraller, D.; Bonvicini, M.; Palareti, G.; Guidetti, D.; Gaddi, O.; Picchio, F.M. Comparison of results of percutaneous closure of patent foramen ovale for paradoxical embolism in patients with versus without thrombophilia. Am. J. Cardiol. 2004, 94, 1012–1016. [Google Scholar] [CrossRef] [PubMed]
- Pezzini, A.; Del Zotto, E.; Magoni, M.; Costa, A.B.; Archetti, S.; Grassi, M.; Akkawi, N.M.; Albertini, A.; Assanelli, D.; Vignolo, L.A.; et al. Inherited Thrombophilic Disorders in Young Adults With Ischemic Stroke and Patent Foramen Ovale. Stroke 2003, 34, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Karttunen, V.; Hiltunen, L.; Rasi, V.; Vahtera, E.; Hillbom, M. Factor V Leiden and prothrombin gene mutation may predispose to paradoxical embolism in subjects with patent foramen ovale. Blood Coagul. Fibrinolysis 2003, 14, 261–268. [Google Scholar] [CrossRef]
- Stover, P.J. Physiology of folate and vitamin B12 in health and disease. Nutr. Rev. 2004, 62, S3–S13. [Google Scholar] [CrossRef]
- Linnebank, M.; Homberger, A.; Nowak-Göttl, U.; Marquardt, T.; Harms, E.; Koch, H.G. Linkage disequilibrium of the common mutations 677C > T and 1298A > C of the human methylenetetrahydrofolate reductase gene as proven by the novel polymorphisms 129C > T, 1068C > T. Eur. J. Nucl. Med. Mol. Imaging 2000, 159, 472–473. [Google Scholar] [CrossRef]
- Moll, S.; Varga, E.A. Homocysteine and MTHFR Mutations. Circulation 2015, 132, e6–e9. [Google Scholar] [CrossRef] [PubMed]
- Feng, C.; Bai, X.; Xu, Y.; Hua, T.; Huang, J.; Liu, X.-Y. Hyperhomocysteinemia Associates with Small Vessel Disease More Closely Than Large Vessel Disease. Int. J. Med Sci. 2013, 10, 408–412. [Google Scholar] [CrossRef]
- Choi, B.; Kim, N.K.; Kang, M.; Lee, S.; Ahn, J.; Kim, O.; Oh, D.; Kim, S.; Kim, S. Homozygous C677T mutation in the MTHFR gene as an independent risk factor for multiple small-artery occlusions. Thromb. Res. 2003, 111, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Gerraty, R.P.; Parsons, M.W.; Barber, P.A.; Darby, D.G.; Desmond, P.M.; Tress, B.M.; Davis, S.M. Examining the lacunar hypothesis with diffusion and perfusion magnetic resonance imaging. Stroke 2002, 33, 2019–2024. [Google Scholar] [CrossRef] [PubMed]
- Wessels, T.; Rottger, C.; Jauss, M.; Kaps, M.; Traupe, H.; Stolz, E. Identification of Embolic Stroke Patterns by Diffusion-Weighted MRI in Clinically Defined Lacunar Stroke Syndromes. Stroke 2005, 36, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Cotlarciuc, I.; Malik, R.; Holliday, E.G.; Ahmadi, K.R.; Pare, G.; Psaty, B.M.; Fornage, M.; Hasan, N.; Rinne, P.E.; Ikram, M.A. Effect of genetic variants associated with plasma homocysteine levels on stroke risk. Stroke 2014, 45, 1920–1924. [Google Scholar] [CrossRef]
- Ozdemir, A.O.; Tamayo, A.; Muñoz, C.; Dias, B.; Spence, J.D. Cryptogenic stroke and patent foramen ovale: Clinical clues to paradoxical embolism. J. Neurol. Sci. 2008, 275, 121–127. [Google Scholar] [CrossRef]
- Hart, R.G.; Diener, H.-C.; Coutts, S.B.; Easton, J.D.; Granger, C.B.; O’Donnell, M.; Sacco, R.L.; Connolly, S.J. Embolic strokes of undetermined source: The case for a new clinical construct. Lancet Neurol. 2014, 13, 429–438. [Google Scholar] [CrossRef]
- Schwedhelm, E.; Maas, R.; Tan-Andresen, J.; Schulze, F.; Riederer, U.; Böger, R.H. High-throughput liquid chromatographic-tandem mass spectrometric determination of arginine and dimethylated arginine derivatives in human and mouse plasma. J. Chromatogr. B 2007, 851, 211–219. [Google Scholar] [CrossRef]
- Kayacelebi, A.A.; Langen, J.; Weigt-Usinger, K.; Chobanyan-Jürgens, K.; Mariotti, F.; Schneider, J.Y.; Rothmann, S.; Frölich, J.C.; Atzler, R.; Choe, C.-U.; et al. Biosynthesis of homoarginine (hArg) and asymmetric dimethylarginine (ADMA) from acutely and chronically administered free l-arginine in humans. Amino Acids 2015, 47, 1893–1908. [Google Scholar] [CrossRef]
- Chen, S.; Li, N.; Deb-Chatterji, M.; Dong, Q.; Kielstein, J.T.; Weissenborn, K.; Worthmann, H. Asymmetric Dimethyarginine as Marker and Mediator in Ischemic Stroke. Int. J. Mol. Sci. 2012, 13, 15983–16004. [Google Scholar] [CrossRef]
- Teerlink, T.; Luo, Z.; Palm, F.; Wilcox, C.S. Cellular ADMA: Regulation and action. Pharmacol. Res. 2009, 60, 448–460. [Google Scholar] [CrossRef] [PubMed]
- Stuhlinger, M.C.; Oka, R.K.; Graf, E.E.; Schmolzer, I.; Upson, B.M.; Kapoor, O.; Szuba, A.; Malinow, M.R.; Wascher, T.C.; Pachinger, O.; et al. Endothelial Dysfunction Induced by Hyperhomocyst(e)inemia. Circulation 2003, 108, 933–938. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Zeng, H.; Li, F.; Feng, J.; Liu, S.; Liu, J.; Yu, J.; Mao, J.; Hong, T.; Chen, A.F.; et al. Homocysteine impairs coronary artery endothelial function by inhibiting tetrahydrobiopterin in patients with hyperhomocysteinemia. Am. J. Physiol. Metab. 2010, 299, E1061–E1065. [Google Scholar] [CrossRef] [PubMed]
- Dimitroulas, T.; Sandoo, A.; Hodson, J.; Smith, J.; Douglas, K.; Kitas, G.; Kitas, G.D. Associations between asymmetric dimethylarginine, homocysteine, and the methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism (rs1801133) in rheumatoid arthritis. Scand. J. Rheumatol. 2016, 45, 267–273. [Google Scholar] [CrossRef]
- Sniezawska, A.; Dorszewska, J.; Różycka, A.; Przedpelska-Ober, E.; Lianeri, M.; Jagodzinski, P.P.; Kozubski, W. MTHFR, MTR, and MTHFD1 gene polymorphisms compared to homocysteine and asymmetric dimethylarginine concentrations and their metabolites in epileptic patients treated with antiepileptic drugs. Seizure 2011, 20, 533–540. [Google Scholar] [CrossRef]
- Scherbakov, N.; Sandek, A.; Martens-Lobenhoffer, J.; Kung, T.; Turhan, G.; Liman, T.; Ebinger, M.; Von Haehling, S.; Bode-Böger, S.; Endres, M.; et al. Endothelial Dysfunction of the Peripheral Vascular Bed in the Acute Phase after Ischemic Stroke. Cerebrovasc. Dis. 2012, 33, 37–46. [Google Scholar] [CrossRef]
- Böger, R.H.; Sullivan, L.; Schwedhelm, E.; Wang, T.J.; Maas, R.; Benjamin, E.J.; Schulze, F.; Xanthakis, V.; Benndorf, R.A.; Vasan, R.S. Plasma Asymmetric Dimethylarginine and Incidence of Cardiovascular Disease and Death in the Community. Circulation 2009, 119, 1592–1600. [Google Scholar] [CrossRef]
- Notsu, Y.; Nabika, T.; Bokura, H.; Suyama, Y.; Kobayashi, S.; Yamaguchi, S.; Masuda, J. Evaluation of Asymmetric Dimethylarginine and Homocysteine in Microangiopathy-Related Cerebral Damage. Am. J. Hypertens. 2009, 22, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Pikula, A.; Böger, R.H.; Beiser, A.; Maas, R.; DeCarli, C.; Schwedhelm, E.; Himali, J.J.; Schulze, F.; Au, R.; Kelly-Hayes, M.; et al. Association of plasma ADMA levels with MRI markers of vascular brain injury: Framingham offspring study. Stroke 2009, 40, 2959–2964. [Google Scholar] [CrossRef] [PubMed]
- Bode-Boger, S.M.; Boger, R.H.; Kienke, S.; Junker, W.; Frolich, J.C. Elevated L-arginine/dimethylarginine ratio contributes to enhanced systemic NO production by dietary L-arginine in hypercholesterolemic rabbits. Biochem. Biophys. Res. Commun. 1996, 219, 598–603. [Google Scholar] [CrossRef]
- Lepic, E.; Burger, D.; Lu, X.; Song, W.; Feng, Q. Lack of endothelial nitric oxide synthase decreases cardiomyocyte proliferation and delays cardiac maturation. Am. J. Physiol. Physiol. 2006, 291, C1240–C1246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Feng, Q.; Song, W.; Lu, X.; Hamilton, J.A.; Lei, M.; Peng, T.; Yee, S.-P. Development of heart failure and congenital septal defects in mice lacking endothelial nitric oxide synthase. Circulation 2002, 106, 873–879. [Google Scholar] [CrossRef]
- Virdis, A.; Iglarz, M.; Neves, M.F.; Amiri, F.; Touyz, R.M.; Rozen, R.; Schiffrin, E.L. Effect of Hyperhomocystinemia and Hypertension on Endothelial Function in Methylenetetrahydrofolate Reductase–Deficient Mice. Arter. Thromb. Vasc. Boil. 2003, 23, 1352–1357. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study. Lancet 1991, 338, 131–137. [CrossRef]
- Amorim, M.R.; Lima, M.A.; Castilla, E.E.; Orioli, I.M. Non-Latin European descent could be a requirement for association of NTDs andMTHFR variant 677C > T: A meta-analysis. Am. J. Med. Genet. Part A 2007, 143, 1726–1732. [Google Scholar] [CrossRef]
- Zhao, M.; Wu, G.; Li, Y.; Wang, X.; Hou, F.F.; Xu, X.; Qin, X.; Cai, Y.-F. Meta-analysis of folic acid efficacy trials in stroke prevention. Neurology 2017, 88, 1830–1838. [Google Scholar] [CrossRef]
- Zidan, H.E.; Rezk, N.A.; Mohammed, D. MTHFR C677T and A1298C gene polymorphisms and their relation to homocysteine level in Egyptian children with congenital heart diseases. Gene 2013, 529, 119–124. [Google Scholar] [CrossRef]
- Zhu, W.; Yong, L.; Yan, L.; Dao, J.; Li, S. Maternal and offspring MTHFR gene C677T polymorphism as predictors of congenital atrial septal defect and patent ductus arteriosus. Mol. Hum. Reprod. 2006, 12, 51–54. [Google Scholar] [CrossRef]
- Angeline, T.; Jeyaraj, N.; Granito, S.; Tsongalis, G.J. Prevalence of MTHFR gene polymorphisms (C677T and A1298C) among Tamilians. Exp. Mol. Pathol. 2004, 77, 85–88. [Google Scholar] [CrossRef]
- Meissner, I.; Whisnant, J.P.; Khandheria, B.K.; Spittell, P.C.; O’Fallon, W.M.; Pascoe, R.D.; Enriquez-Sarano, M.; Seward, J.B.; Covalt, J.L.; Sicks, J.D.; et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: The SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin. Proc. 1999, 74, 862–869. [Google Scholar] [CrossRef]
- Rodriguez, C.J.; Homma, S.; Sacco, R.L.; Di Tullio, M.R.; Sciacca, R.R.; Mohr, J. Race-Ethnic Differences in Patent Foramen Ovale, Atrial Septal Aneurysm, and Right Atrial Anatomy Among Ischemic Stroke Patients. Stroke 2003, 34, 2097–2102. [Google Scholar] [CrossRef] [PubMed]
- Daniel Leclerc, S.S.; Rozen, R. Molecular Biology of Methylenetetrahydrofolate Reductase (MTHFR) and Overview of Mutations/Polymorphisms; Database, M.C.B., Ed.; Landes Bioscience: Austin, TX, USA, 2013. [Google Scholar]
- Hagen, P.T.; Scholz, D.G.; Edwards, W.D. Incidence and Size of Patent Foramen Ovale During the First 10 Decades of Life: An Autopsy Study of 965 Normal Hearts. Mayo Clin. Proc. 1984, 59, 17–20. [Google Scholar] [CrossRef]
- Lemarié, C.A.; Shbat, L.; Marchesi, C.; Angulo, O.J.; Deschênes, M.-E.; Blostein, M.D.; Paradis, P.; Schiffrin, E.L. Mthfr deficiency induces endothelial progenitor cell senescence via uncoupling of eNOS and downregulation of SIRT1. Am. J. Physiol. Circ. Physiol. 2011, 300, H745–H753. [Google Scholar] [CrossRef]
- Martí-Fàbregas, J.; Crespo, J.; Delgado-Mederos, R.; Martínez-Ramírez, S.; Peña, E.; Marín, R.; Dinia, L.; Jiménez-Xarrié, E.; Fernández-Arcos, A.; Pérez-Pérez, J.; et al. Endothelial progenitor cells in acute ischemic stroke. Brain Behav. 2013, 3, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Erdélyi-Bótor, S.; Deli, G.; Trauninger, A.; Komáromy, H.; Kamson, D.O.; Kovács, N.; Perlaki, G.; Orsi, G.; Molnar, T.; Illes, Z.; et al. Serum L-arginine and dimethylarginine levels in migraine patients with brain white matter lesions. Cephalalgia 2016, 37, 571–580. [Google Scholar] [CrossRef]
- Sunbul, M.; Ozben, B.; Durmus, E.; Kepez, A.; Pehlivan, A.; Midi, I.; Mutlu, B. Endothelial dysfunction is an independent risk factor for stroke patients irrespective of the presence of patent foramen ovale. Herz 2013, 38, 671–676. [Google Scholar] [CrossRef]
- Qin, X.; Li, J.; Spence, J.D.; Zhang, Y.; Li, Y.; Wang, X.; Wang, B.; Sun, N.; Chen, F.; Guo, J. Folic Acid Therapy Reduces the First Stroke Risk Associated With Hypercholesterolemia Among Hypertensive Patients. Stroke 2016, 47, 2805–2812. [Google Scholar] [CrossRef]
| SEPTUM INTEGRUM | PATENT FORAMEN OVALE | OSTIUM SECUNDUM | |
|---|---|---|---|
| PATIENTS (N) | 10 | 38 | 9 |
| Age (year) | 37 ± 10 | 42 ± 11 | 40 ± 17 |
| Fibrinogen (mg/dL) | 264 ± 36 | 249 ± 41 | 239 ± 43 |
| D-dimers (ng/dL) | 488 ± 421 | 463 ± 370 | 387 ± 122 |
| P-Hcy (µmol(L) | 7.2 ± 3.6 | 12.1 ± 7.6 * | 12.7 ± 3.2 * |
| Folates (ng/mL) | 5.0 ± 4.2 | 7.7 ± 4.5 | 17.7 ± 9.9 * |
| B12 Vit (pg/mL) | 438.4 ± 82.3 | 417.9 ± 166.1 | 341 ± 104.3 |
| Creatinine (mg/dL) | 0.65 ± 0.13 | 0.75 ± 0.13 | 0.70 ± 0.19 |
| eGFR (mL/min) | 103 ± 15 | 102 ±13 | 108 ± 19 |
| Glucose (mg/dL) | 96 ± 13.5 | 88.6 ± 9.5 | 76 ± 11.2 |
| Cholesterol (mg/dL) | 209 ± 27 | 182 ± 26 | 201 ± 12 |
| HDL (mg/dL) | 53 ± 9 | 59 ± 14 | 55 ± 5 |
| LDL (mg/dL) | 125 ± 45 | 103 ± 21 | 116 ± 12 |
| Triglicerides (mg/dL) | 110 ± 34.5 | 75 ± 24.2 | 60 ± 18.2 |
| Systolic BP (mmHg) | 118 ± 5.2 | 121 ± 4.78 | 119 ± 12.2 |
| Diastolic BP (mmHg) | 74 ± 9.5 | 75 ± 3.3 | 70 ± 9.4 |
| 677 T/T | 677 C/T + 1298 A/C | 677 C/T | 1298 C/C | 1298 A/C + WT | |
|---|---|---|---|---|---|
| PATIENTS (N) | 16 | 14 | 6 | 5 | 16 |
| Age (year) | 39 ± 12 | 40 ± 9 | 46 ± 18 | 40 ± 16 | 42 ± 9 |
| Fibrinogen (mg/dL) | 225 ± 24 | 268 ± 39 | 260 ± 37 | 264 ± 65 | 263 ± 44 |
| D-dimers (ng/dL) | 356 ± 153 | 466 ± 438 | 462 ± 298 | 653 ± 585 | 349 ± 322 |
| P-Hcy (µmol/L) | 16.3 ± 5.8 * | 9.8 ± 2.9 | 8.0 ± 2.1 | 7.9 ± 1.1 | 9.1 ± 2.9 |
| Folates (ng/mL) | 10.6 ± 4.4 | 7.9 ± 2.7 | 7.9 ± 5.6 | 11.4 ± 4.1 | 6.6 ± 3.3 |
| B12 Vit. (pg/mL) | 383.8 ± 150.3 | 376.3 ± 88.9 | 385.5 ± 112.5 | 541 ± 202.5 | 440.9 ± 199.4 |
| Creatinine (mg/dL) | 0.60 ± 0.06 | 0.79 ± 0.18 | 0.73 ± 0.21 | 0.72 ± 0.09 | 0.77 ± 0.09 |
| eGFR (mL/min) | 110.5 ± 6.4 | 102 ± 2.8 | 92 ± 26.8 | 109.5 ± 10.6 | 101.75 ± 12.3 |
| Glucose (mg/dL) | 87 ± 8.04 | 107.5 ± 12.02 | 86 ± 4.24 | 93.5 ± 23.33 | 95 ± 10.61 |
| Cholesterol (mg/dL) | 181 ± 24.3 | 172 ± 45.9 | 195 ± 30.4 | 182 ± 17.7 | 188 ± 54.1 |
| HDL (mg/dL) | 56 ± 7.5 | 53 ± 2.8 | 83 ± 4.9 | 46 ± 5.6 | 51 ± 16.2 |
| LDL (mg/dL) | 110 ± 28.2 | 101 ± 38.9 | 101 ± 24.4 | 112 ± 7.8 | 113 ± 40.9 |
| Triglicerides (mg/dL) | 78 ± 27.5 | 91 ± 49.5 | 54 ± 8.5 | 83 ± 21.2 | 69 ± 16.3 |
| Systolic BP (mmHg) | 117 ± 6.2 | 120 ± 7.8 | 122 ± 2.2 | 118 ± 5.6 | 119 ± 8.1 |
| Diastolic BP (mmHg) | 76 ± 5.5 | 78 ± 4.3 | 79 +6.4 | 79 ± 2.5 | 76 ± 10.2 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sgarra, L.; Bortone, A.S.; Potenza, M.A.; Nacci, C.; De Salvia, M.A.; Acquaviva, T.; De Cillis, E.; Ciccone, M.M.; Grimaldi, M.; Montagnani, M. Endothelial Dysfunction May Link Interatrial Septal Abnormalities and MTHFR-Inherited Defects to Cryptogenic Stroke Predisposition. Biomolecules 2020, 10, 861. https://doi.org/10.3390/biom10060861
Sgarra L, Bortone AS, Potenza MA, Nacci C, De Salvia MA, Acquaviva T, De Cillis E, Ciccone MM, Grimaldi M, Montagnani M. Endothelial Dysfunction May Link Interatrial Septal Abnormalities and MTHFR-Inherited Defects to Cryptogenic Stroke Predisposition. Biomolecules. 2020; 10(6):861. https://doi.org/10.3390/biom10060861
Chicago/Turabian StyleSgarra, Luca, Alessandro Santo Bortone, Maria Assunta Potenza, Carmela Nacci, Maria Antonietta De Salvia, Tommaso Acquaviva, Emanuela De Cillis, Marco Matteo Ciccone, Massimo Grimaldi, and Monica Montagnani. 2020. "Endothelial Dysfunction May Link Interatrial Septal Abnormalities and MTHFR-Inherited Defects to Cryptogenic Stroke Predisposition" Biomolecules 10, no. 6: 861. https://doi.org/10.3390/biom10060861
APA StyleSgarra, L., Bortone, A. S., Potenza, M. A., Nacci, C., De Salvia, M. A., Acquaviva, T., De Cillis, E., Ciccone, M. M., Grimaldi, M., & Montagnani, M. (2020). Endothelial Dysfunction May Link Interatrial Septal Abnormalities and MTHFR-Inherited Defects to Cryptogenic Stroke Predisposition. Biomolecules, 10(6), 861. https://doi.org/10.3390/biom10060861







