Relationship between Metabolomics Profile of Perilymph in Cochlear-Implanted Patients and Duration of Hearing Loss
Abstract
:1. Introduction
2. Results
2.1. Metabolites Analysis
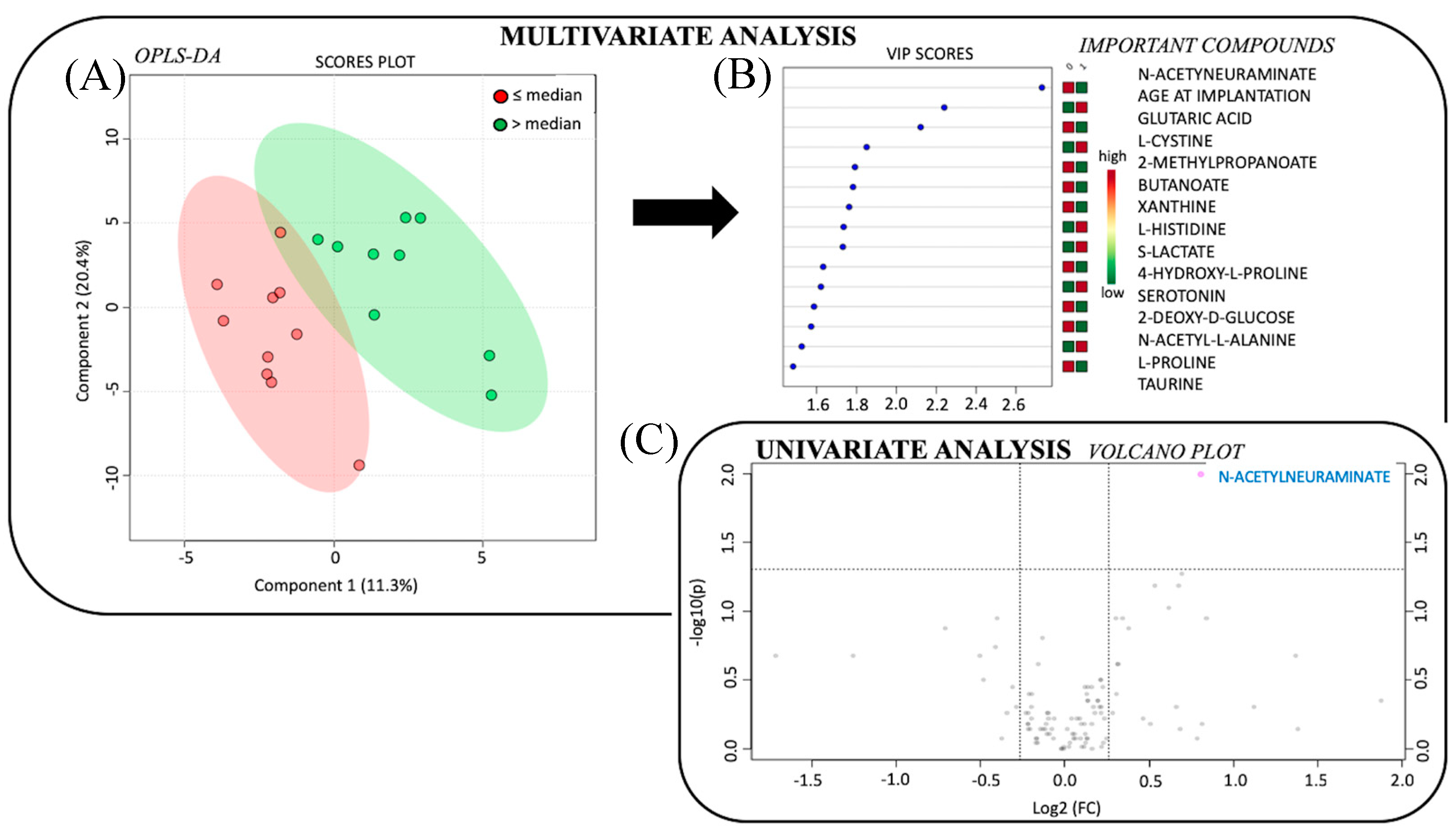
2.2. Significant Metabolic Profile for Duration of Hearing Loss
3. Discussion
3.1. Innovative Exploration of Perilymph Content
3.2. Perilymph Metabolome Discriminates Patients According to Hearing Loss Duration
3.3. Metabolites and Associated Metabolic Pathways Involved in Hearing Loss Duration
3.4. Perspectives of Perilymph Metabolome
4. Materials and Methods
4.1. Patients
4.2. Sample Collection
4.3. Liquid Chromatography−High-Resolution Mass Spectrometry
4.4. Univariate Analysis
4.5. Multivariate Analysis
5. Conclusions
Supplementary Materials
Ethical Approval
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kral, A.; O’Donoghue, G.M. Profound deafness in childhood. N. Engl. J. Med. 2010, 363, 1438–1450. [Google Scholar] [CrossRef] [PubMed]
- WHO. Available online: http://www.who.int/mediacentre/factsheets/fs300/fr/ (accessed on 5 March 2019).
- Davis, A. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int. J. Epidemiol. 1989, 18, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.H.; Walsh, P.G.; Sanchez, L.; Davis, A.C.; Taylor, A.W.; Tucker, G.; Meagher, I. The epidemiology of hearing impairment in an Australian adult population. Int. J. Epidemiol. 1999, 28, 247–522. [Google Scholar] [CrossRef] [PubMed]
- Petit, C.; Levilliers, J.; Hardelin, J.P. Molecular genetics of hearing loss. Ann. Rev. Genet. 2001, 35, 589–646. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.J.; Bale, J.F.; White, K.R. Sensorineural hearing loss in children. Lancet 2005, 365, 879–890. [Google Scholar] [CrossRef]
- Gates, G.A.; Mills, J.H. Presbycusis. Lancet 2005, 366, 1111–1120. [Google Scholar] [CrossRef]
- O’Donoghue, G. Cochlear implants: Science, serendipity, and success. N. Engl. J. Med. 2013, 369, 1190–1193. [Google Scholar]
- Niparko, J.K.; Obey, E.A.; Thal, D.J.; Eisenberg, L.S.; Wang, N.Y.; Quittner, A.L.; Fink, N.E.; CDaCI Investigative Team. Spoken language development in children following cochlear implantation. JAMA 2011, 303, 1498–1506. [Google Scholar] [CrossRef]
- Blamey, P.; Artieres, F.; Başkent, D.; Bergeron, F.; Beynon, A.; Burke, E.; Dillier, N.; Dowell, R.; Fraysse, B.; Gallégo, S.; et al. Factors affecting auditory performance of postlinguistically deaf adults using cochlear implants: An update with 2251 patients. Audiol. Neurotol. 2012, 18, 36–47. [Google Scholar] [CrossRef]
- Wong, A.C.Y.; Ryan, A.F. Mechanisms of sensorineural cell damage, death and survival in the cochlea. Front. Aging Neurosci. 2015, 7, 1–15. [Google Scholar] [CrossRef]
- Tirko, N.N.; Ryugo, D.K. Synaptic plasticity in the medial superior olive of hearing, deaf, and cochlear-implanted cats. J. Comp. Neuro. 2014, 520, 2202–2217. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.; Sharma, A. Visual cross-modal re-organization in children with cochlear implants. PLoS ONE 2016, 11, e0147793. [Google Scholar] [CrossRef] [PubMed]
- Madji Hounoum, B.; Mavel, S.; Coque, E.; Patin, F.; Vourc’h, P.; Marouillat, S.; Nadal-Desbarats, L.; Emond, P.; Corcia, P.; Andres, C.R.; et al. Wildtype motoneurons, ALS-linked SOD1 mutation and glutamate profoundly modify astrocyte metabolism and lactate shuttling. Glia 2017, 65, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Lysaght, A.C.; Kao, S.Y.; Paulo, J.A.; Merchant, S.N.; Steen, H.; Stankovic, K.M. The proteome of human perilymph. J. Proteome Res. 2011, 10, 3845–3851. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, H.A.; Pich, A.; Schröder, A.; Scheper, V.; Lilli, G.; Reuter, G.; Lenarz, T. Proteome analysis of human perilymph using an intraoperative sampling method. J. Proteome Res. 2017, 16, 1911–1923. [Google Scholar] [CrossRef]
- Mavel, S.; Lefèvre, A.; Bakhos, D.; Dufour-Rainfray, D.; Blasco, H.; Emond, P. Validation of metabolomics analysis of human perilymph fluid using liquid chromatography-mass spectroscopy. Hear. Res. 2018, 22. [Google Scholar] [CrossRef]
- Fujita, T.; Yamashita, D.; Irino, Y.; Kitamoto, J.; Fukuda, Y.; Inokuchi, G.; Hasegawa, S.; Otsuki, N.; Yoshida, M.; Nibu, K.I. Metabolomic profiling in inner ear fluid by gas chromatography/mass spectrometry in guinea pig cochlea. Neurosci. Lett. 2015, 606, 188–193. [Google Scholar] [CrossRef]
- Fransson, A.E.; Kisiel, M.; Pirttilä, K.; Pettersson, C.; Videhult Pierre, P.; Laurell, G.F. Hydrogen inhalation protects against ototoxicity induced by intravenous cisplatin in the guinea pig. Front. Cell. Neurosci. 2017, 11, 280. [Google Scholar] [CrossRef]
- Alawieh, A.; Mondello, S.; Kobeissy, F.; Shibbani, K.; Bassim, M. Proteomics studies in inner ear disorders: Pathophysiology and biomarkers. Expert Rev. Proteomics 2015, 12, 185–196. [Google Scholar] [CrossRef]
- Thalmann, I.; Kohut, R.; Ryu, J.; Thalmann, R. High resolution 2D electrophoresis: Technique and potential applicability to the study of inner ear disease. Am. J. Otol. 1995, 16, 153–157. [Google Scholar]
- Schmitt, H.; Roemer, A.; Zeilinger, C.; Salcher, R.; Durisin, M.; Staecker, H.; Lenarz, T.; Warnecke, A. Heat shock proteins in human perilymph. Otol. Neurotol. 2018, 39, 37–44. [Google Scholar] [CrossRef] [PubMed]
| Group 1 (≤12 y) | Group 2 (>12 y) | p; U | |
|---|---|---|---|
| N | 10 | 9 | |
| Mean age at CI (y) | 38 ± 30 | 65 ± 19 | p = 0.062; U = 22.0 |
| Mean age onset of deafness (y) | 33 ± 30 | 28 ± 26 | p = 0.733; U = 40.5 |
| Mean duration of deafness (y) | 5 ± 4 | 36 ± 15 | p < 0.001; U = 0.0 * |
| Mean duration of HA use (y) | 3 ± 2 | 20 ± 13 | p < 0.001; U = 0.0 * |
| Pre-surgical PTA (dB) | 98 ± 16 | 91 ± 14 | p = 0.561; U = 37.5 |
| SAT (dB) | >100 dB | >100 dB |
| Subjects | Sex | Age at CI (y) | Age at Onset of Deafness (y) | Duration of Deafness (y) | Duration of HA (y) | Pre-Surgical PTA (dB) | Etiology | Site of CI | Type of CI | Comorbidities |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 39 | 2 | 37 | 37 | 81.25 | Congenital | Left | Cochlear CI 512 | # |
| 2 | M | 86 | 26 | 60 | 22 | 81.25 | Traumatic | Left | Cochlear CI 512 | # |
| 3 | M | 63 | 53 | 10 | 1 | 85 | Meniere’s | Right | Cochlear CI 512 | # |
| 4 | F | 9 | 2 | 7 | 7 | 78.5 | Congenital | Right | MedEl Synchrony Pin | # |
| 5 | F | 79 | 67 | 12 | 4 | 116.25 | Temporal bone fracture | Left | Cochlear CI 512 | High blood pressure |
| 6 | M | 63 | 62 | 0.5 | 5 | 116.25 | Sudden HL | Left | Cochlear CI 512 | # |
| 7 | F | 42 | 2 | 40 | 40 | 83.75 | Congenital | Right | Cochlear CI 512 | # |
| 8 | F | 59 | 58 | 1 | 1 | 110 | Sudden HL | Right | Cochlear CI 512 | # |
| 9 | F | 74 | 54 | 20 | 10 | 77.5 | Presbycusis | Right | Cochlear CI 512 | # |
| 10 | M | 80 | 60 | 20 | 18 | 87.5 | Presbycusis | Left | Cochlear CI 512 | dyslipidemia |
| 11 | F | 6 | 0 | 6 | 5 | 113.75 | Congenital | Right | MedEl Synchrony Pin | # |
| 12 | M | 4 | 0 | 4 | 3 | 80 | Congenital | Left | Cochlear CI 422 | # |
| 13 | F | 4 | 0 | 4 | 4 | 81.25 | Congenital | Right | MedEl Concerto Pin | # |
| 14 | M | 64 | 62 | 2 | 2 | 87.5 | Presbycusis | Right | Neurelec | # |
| 15 | M | 76 | 58 | 18 | 18 | 92.5 | Presbycusis | Right | Advanced Bionics | # |
| 16 | M | 54 | 0 | 54 | 45 | 112.5 | Congenital | Right | Cochlear CI 512 | # |
| 17 | M | 85 | 45 | 40 | 40 | 115 | Presbycusis | Right | Cochlear CI 512 | # |
| 18 | M | 45 | 7 | 38 | 38 | 91.25 | Congenital | Right | Cochlear CI 512 | # |
| 19 | M | 31 | 29 | 2 | 0 | 107.25 | Temporal bone fracture | Left | Cochlear CI 512 | HIV |
| Mean (SD) | 50.7 (28.4) | 30.9 (27.6) | 19.8 (19.2) | 15.5 (16.1) | 89.5 (24.2) | |||||
| Median | 59.0 | 29.0 | 12.0 | 7.0 | 87.5 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trinh, T.-T.; Blasco, H.; Emond, P.; Andres, C.; Lefevre, A.; Lescanne, E.; Bakhos, D. Relationship between Metabolomics Profile of Perilymph in Cochlear-Implanted Patients and Duration of Hearing Loss. Metabolites 2019, 9, 262. https://doi.org/10.3390/metabo9110262
Trinh T-T, Blasco H, Emond P, Andres C, Lefevre A, Lescanne E, Bakhos D. Relationship between Metabolomics Profile of Perilymph in Cochlear-Implanted Patients and Duration of Hearing Loss. Metabolites. 2019; 9(11):262. https://doi.org/10.3390/metabo9110262
Chicago/Turabian StyleTrinh, Thuy-Trân, Hélène Blasco, Patrick Emond, Christian Andres, Antoine Lefevre, Emmanuel Lescanne, and David Bakhos. 2019. "Relationship between Metabolomics Profile of Perilymph in Cochlear-Implanted Patients and Duration of Hearing Loss" Metabolites 9, no. 11: 262. https://doi.org/10.3390/metabo9110262
APA StyleTrinh, T.-T., Blasco, H., Emond, P., Andres, C., Lefevre, A., Lescanne, E., & Bakhos, D. (2019). Relationship between Metabolomics Profile of Perilymph in Cochlear-Implanted Patients and Duration of Hearing Loss. Metabolites, 9(11), 262. https://doi.org/10.3390/metabo9110262






