Adipose Tissue Lactate Clearance but Not Blood Lactate Clearance Is Associated with Clinical Outcome in Sepsis or Septic Shock during the Post-Resuscitation Period
Abstract
:1. Introduction
2. Results
2.1. Patients’ Characteristics
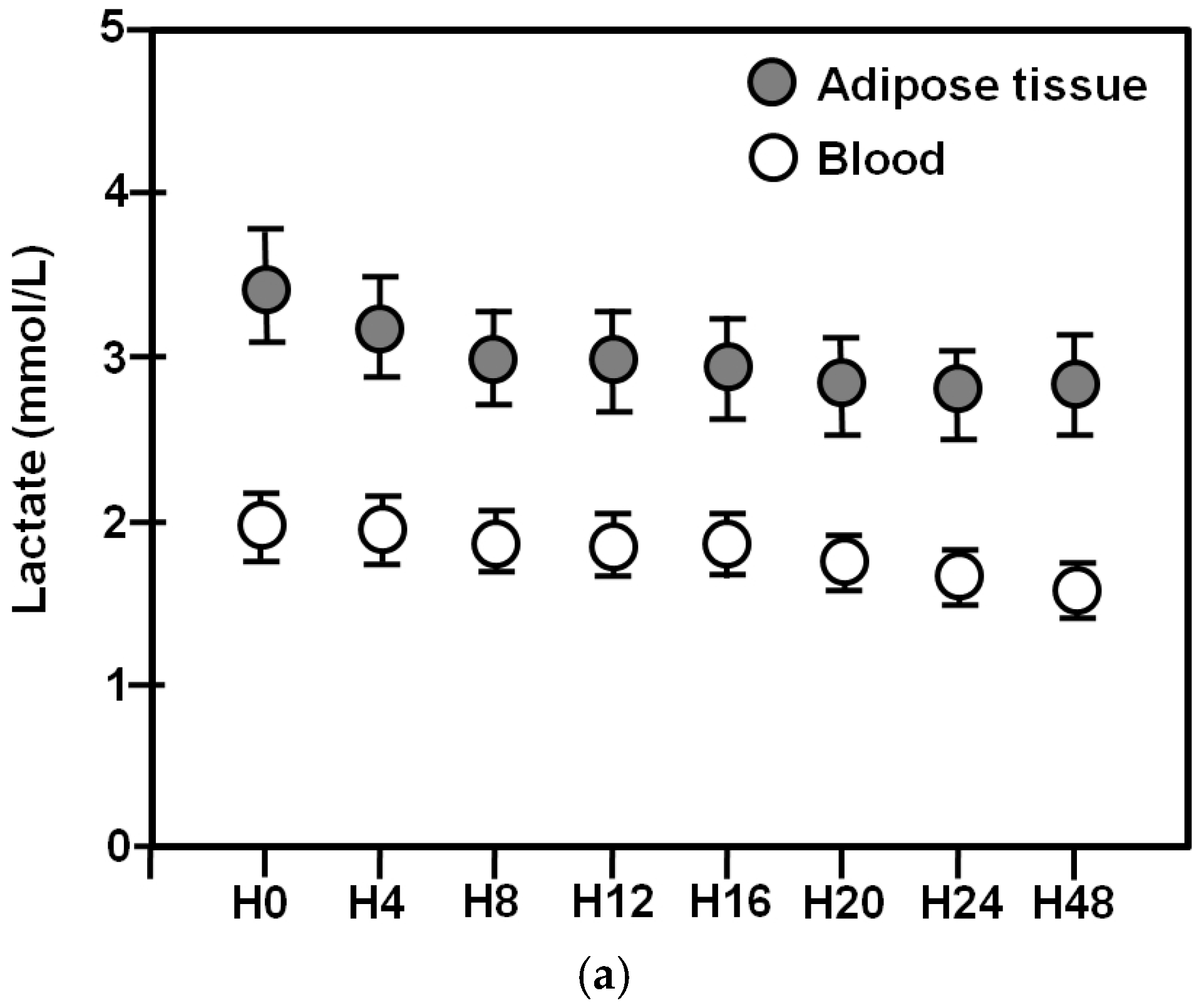
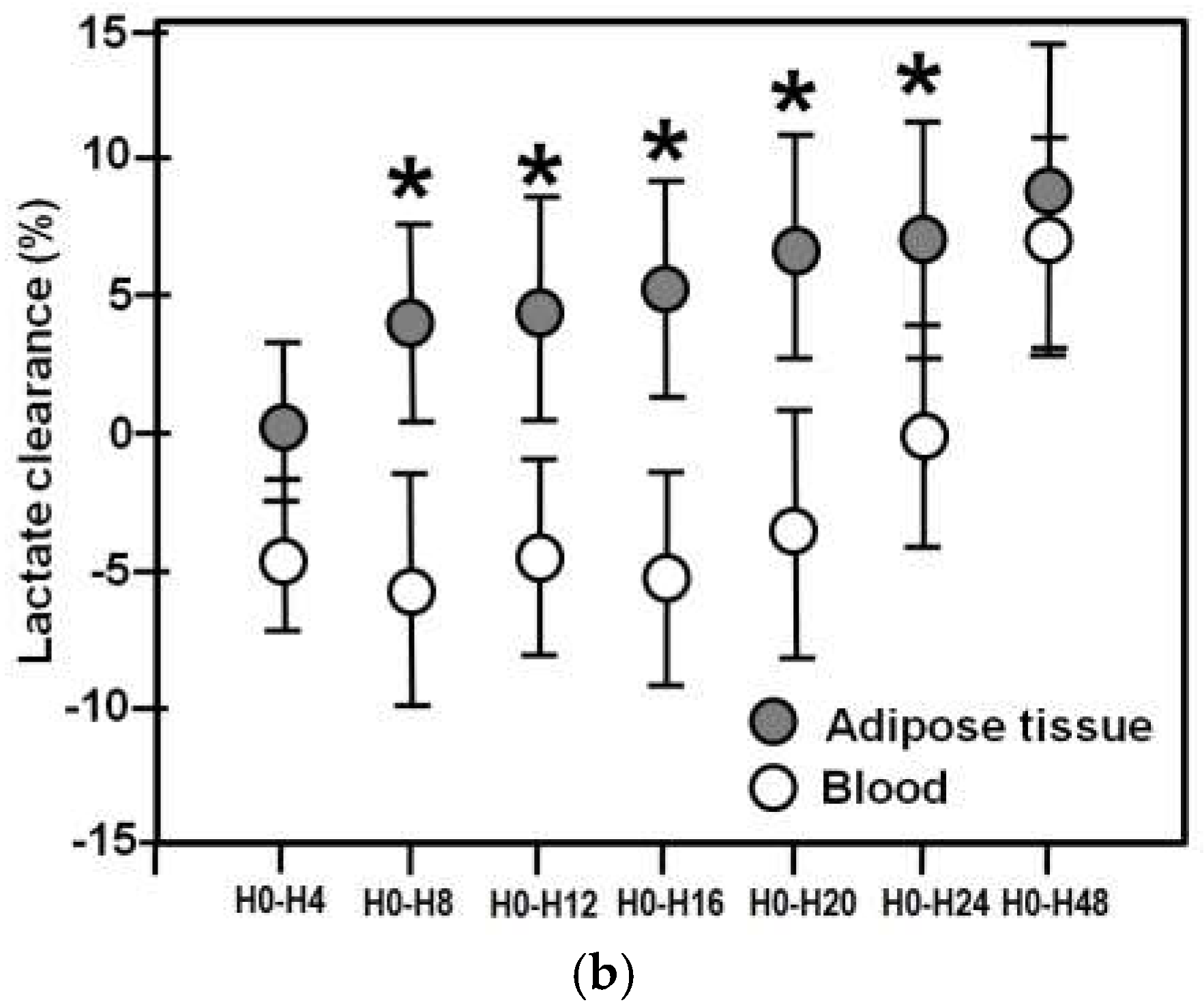
2.2. Blood/Adipose Tissue Lactate Concentrations and Clearances in the Entire Cohort
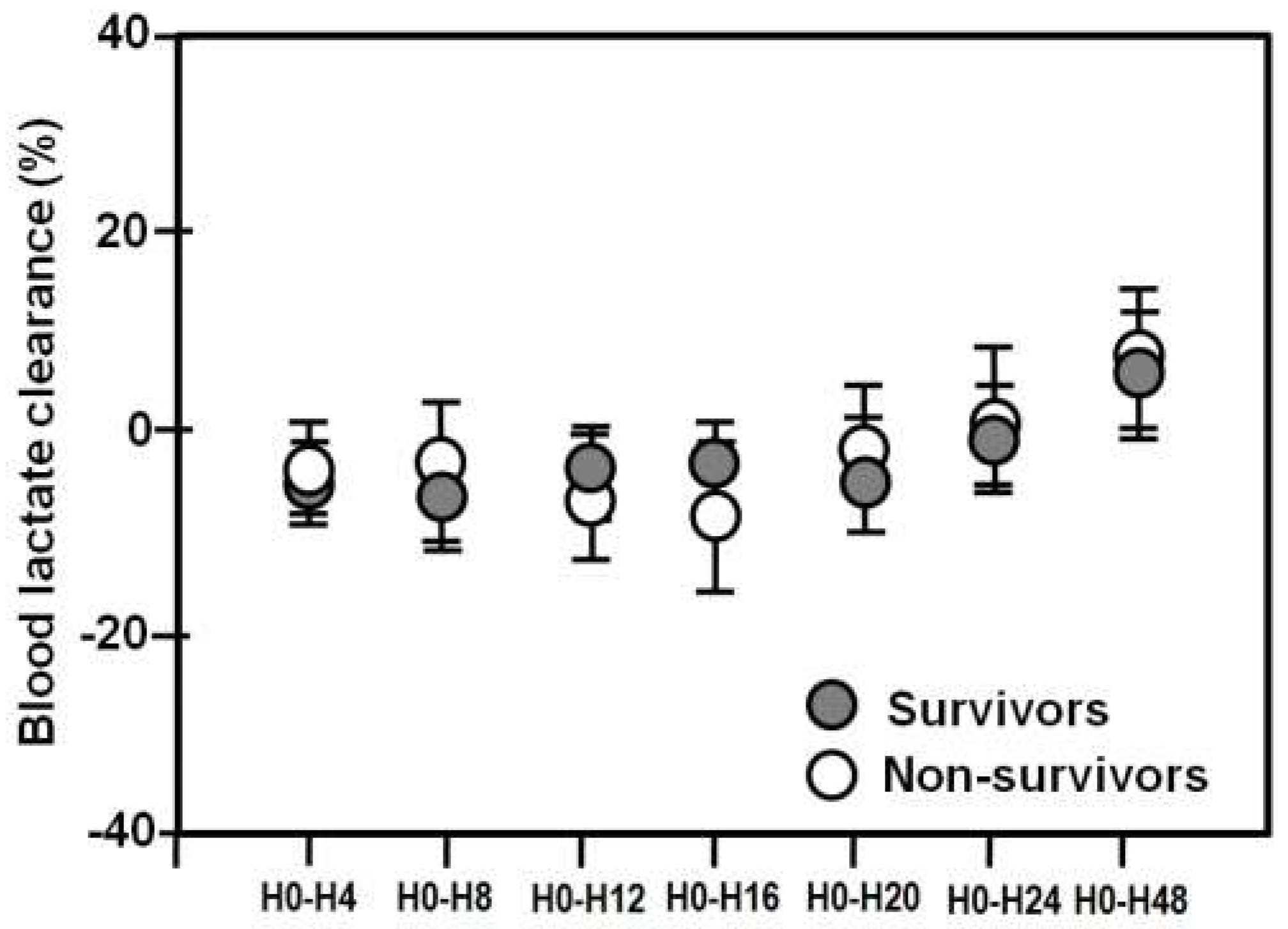
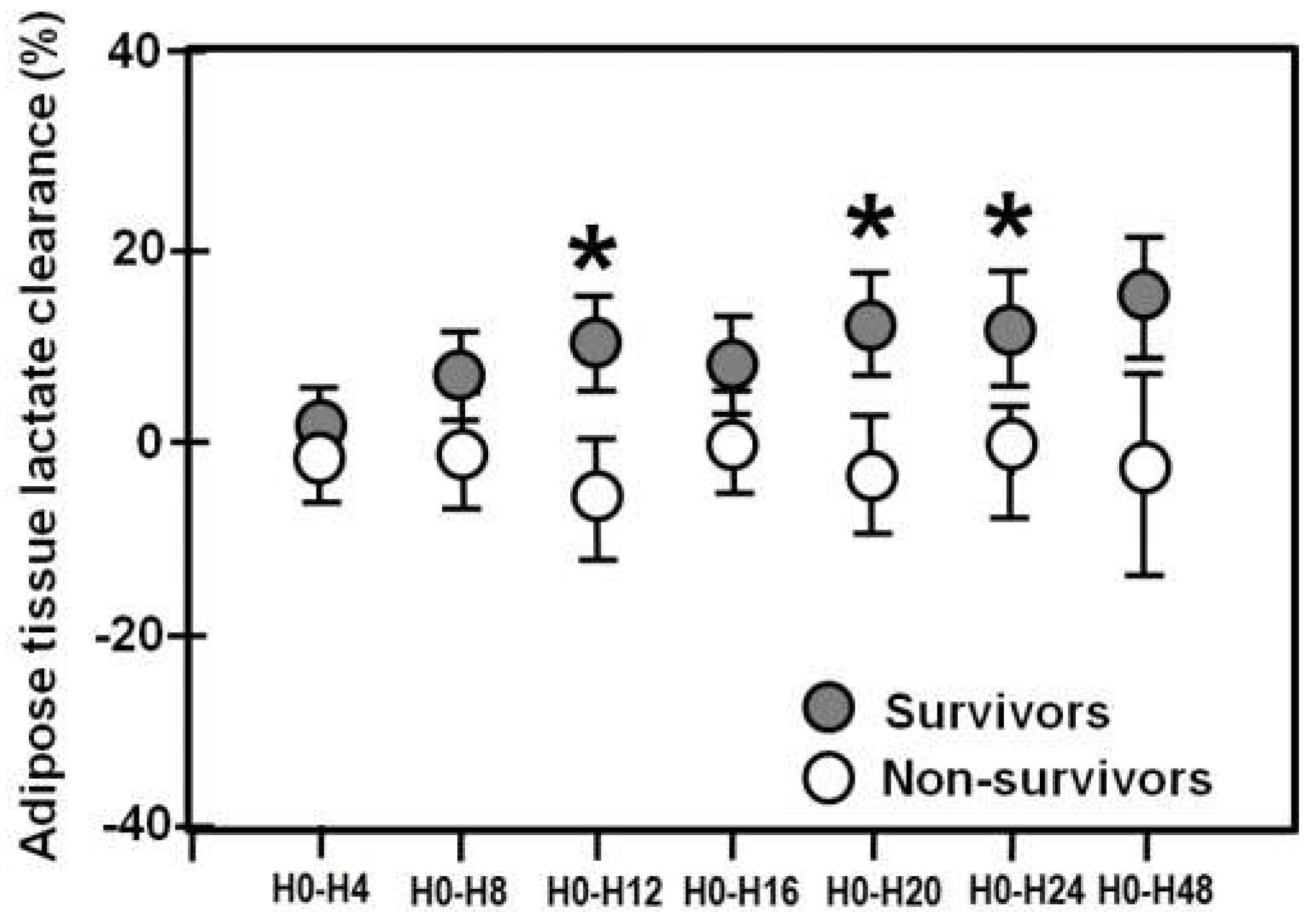
2.3. Blood/Adipose Tissue Lactate Clearances in Survivors and Non-Survivors
3. Discussion
4. Materials and Methods
4.1. Subjects
4.2. Microdialysis
4.3. Other Measurements
4.4. Blood and Tissue Lactate Clearance Definitions
4.5. Data Collection
4.6. Statistical Analysis
5. Conclusions
Authors Contributions
Funding
Conflicts of Interest
References
- Hotchkiss, R.S.; Karl, I.E. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 2003, 348, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Angus, D.C.; van der Poll, T. Severe sepsis and septic shock. N. Engl. J. Med. 2013, 369, 840–851. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Levy, M.; Rhodes, A.; Annane, D.; Gerlach, H.; Opal, S.; Sevransky, J.; Sprung, C.; Douglas, I.; Jaeschke, R.; et al. International Guidelines for Management of Severe Sepsis and Septic Shock. Crit. Care Med. 2013, 41, 580–637. [Google Scholar] [CrossRef] [PubMed]
- Abramson, D.; Scalea, T.M.; Hitchcock, R.; Trooskin, S.Z.; Henry, S.M.; Greenspan, J. Lactate clearance and survival following injury. J. Trauma 1993, 35, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Bakker, J.; Gris, P.; Coffernils, M.; Kahn, R.J.; Vincent, J.L. Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am. J. Surg. 1996, 171, 221–226. [Google Scholar] [CrossRef]
- Levraut, J.; Ichai, C.; Petit, I.; Ciebiera, J.P.; Perus, O.; Grimaud, D. Low exogenous lactate clearance as an early predictor of mortality in normolactatemic critically ill septic patients. Crit. Care Med. 2003, 31, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.B.; Rivers, E.P.; Knoblich, B.P.; Jacobsen, G.; Muzzin, A.; Ressler, J.A.; Tomlanovich, M.C. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit. Care Med. 2004, 32, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Arnold, R.C.; Shapiro, N.I.; Jones, A.E.; Schorr, C.; Pope, J.; Casner, E.; Parrillo, J.E.; Dellinger, R.P.; Trzeciak, S. Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock 2009, 32, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.A.; Griffith, D.M.; Gray, A.J.; Datta, D.; Hay, A.W. Early lactate clearance in septic patients with elevated lactate levels admitted from the emergency department to intensive care: Time to aim higher? J. Crit. Care 2013, 28, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Marty, P.; Roquilly, A.; Vallee, F.; Luzi, A.; Ferre, F.; Fourcade, O.; Asehoune, K.; Minville, V. Lactate clearance for death prediction in severe sepsis or septic shock patients during the first 24 hours in intensive care: An observational study. Ann. Intensive Care 2013, 3, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Jansen, T.C.; van Bommel, J.; Bakker, J. Blood lactate monitoring in critically ill: A systematic technology assessment. Crit. Care Med. 2009, 37, 2827–2839. [Google Scholar] [PubMed]
- De Backer, D.; Ospina-Tascon, G.; Salgado, D.; Favory, R.; Creteur, J.; Vincent, J. Monitoring the microcirculation in the critically ill patient: Current methods and future approaches. Intensive Care Med. 2010, 36, 1813–1825. [Google Scholar] [CrossRef] [PubMed]
- Ekbal, N.J.; Dyson, A.; Black, C.; Singer, M. Monitoring tissue perfusion, oxygenation, and metabolism in critically ill patients. Chest 2013, 143, 1799–1808. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, B.; Morgan, T.J.; Cohen, J. Interstitium: The next diagnostic and therapeutic platform in critical illness. Crit. Care Med. 2010, 38, S630–S636. [Google Scholar] [CrossRef] [PubMed]
- Ungerstedt, U. Microdialysis: Principles and applications for studies in animals and man. J. Intern. Med. 1991, 230, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Ungerstedt, U.; Rostami, E. Microdialysis in neurointensive care. Curr. Pharm. Des. 2004, 10, 2145–2152. [Google Scholar] [CrossRef] [PubMed]
- Bellander, B.M.; Cantais, E.; Enblad, P.; Hutchinson, P.; Nordström, C.H.; Robertson, C.; Sahuquillo, J.; Smith, M.; Stocchetti, N.; Ungerstedt, U.; et al. Consensus meeting on microdialysis in neurointensive care. Intensive Care Med. 2004, 30, 2166–2169. [Google Scholar] [CrossRef] [PubMed]
- Ilias, I.; Nikitas, N.; Theodorakopoulou, M.; Dimopoulou, I. Microdialysis-Assessed Adipose Tissue Metabolism in Critically Ill Patients. Recent Pat. Endocr. Metab. Immune Drug Discov. 2017. [Google Scholar] [CrossRef]
- Kopterides, P.; Theodorakopoulou, M.; Ilias, I.; Nikitas, N.; Frantzeskaki, F.; Vassiliadi, D.A.; Armaganidis, A.; Dimopoulou, I. Interrelationship between blood and tissue lactate in a general intensive care unit: A subcutaneous adipose tissue microdialysis study on 162 critically ill patients. J. Crit. Care 2012, 27, 742. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulou, I.; Nikitas, N.; Orfanos, S.E.; Theodorakopoulou, M.; Vassiliadi, D.; Ilias, I.; Ikonomidis, I.; Boutati, E.; Maratou, E.; Tsangaris, I.; et al. Kinetics of adipose tissue microdialysis-derived metabolites in critically ill septic patients: Associations with sepsis severity and clinical outcome. Shock 2011, 35, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Kopterides, P.; Nikitas, N.; Vassiliadi, D.; Orfanos, S.E.; Theodorakopoulou, M.; Ilias, I.; Boutati, E.; Dimitriadis, G.; Maratou, E.; Diamantakis, A.; et al. Microdialysis-assessed interstitium alterations during sepsis: Relationship to stage, infection, and pathogen. Intensive Care Med. 2011, 37, 1756–1764. [Google Scholar] [CrossRef] [PubMed]
- Kopterides, P.; Theodorakopoulou, M.; Nikitas, N.; Ilias, I.; Vassiliadi, D.A.; Orfanos, S.E.; Tsangaris, I.; Maniatis, N.A.; Tsantes, A.E.; Travlou, A.; et al. Red blood cell transfusion affects microdialysis-assessed interstitial lactate/pyruvate ratio in critically ill patients with late sepsis. Intensive Care Med. 2012, 38, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Vassiliadi, D.A.; Ilias, I.; Tzanela, M.; Nikitas, N.; Theodorakopoulou, M.; Kopterides, P.; Maniatis, N.; Diamantakis, A.; Orfanos, S.E.; Perogamvros, I.; et al. Interstitial cortisol obtained by microdialysis in mechanically ventilated septic patients: Correlations with total and free serum cortisol. J. Crit. Care 2013, 28, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Nikitas, N.; Kopterides, P.; Ilias, I.; Theodorakopoulou, M.; Vassiliadi, D.A.; Armaganidis, A.; Dimopoulou, I. Elevated adipose tissue lactate to pyruvate (L/P) ratio predicts poor outcome in critically ill patients with septic shock: A microdialysis study. Min. Anestesiol. 2013, 79, 1229–1237. [Google Scholar]
- Martinez, A.; Chiolero, R.; Bollman, M.; Revelly, J.P.; Berger, M.; Cayeux, C.; Tappy, L. Assessment of adipose tissue metabolism by means of subcutaneous microdialysis in patients with sepsis or circulatory failure. Clin. Physiol. Funct. Imaging 2003, 23, 286–292. [Google Scholar] [CrossRef] [PubMed]
- De Boer, J.; Potthoff, H.; Mulder, P.O.; Dofferhof, A.S.; van Thiel, R.J.; Plijter-Grondijk, H.; Korf, J. Lactate monitoring with subcutaneous microdialysis in patients with shock: A pilot study. Circ. Shock 1994, 43, 57–63. [Google Scholar] [PubMed]
- Levy, B.; Gibot, S.; Franck, P.; Cravoisy, A.; Bollaert, P.E. Relation between muscle Na+ K+ ATPase activity and raised lactate concentrations in septic shock: A prospective study. Lancet 2005, 365, 871–875. [Google Scholar] [CrossRef]
- Levy, B.; Perez, P.; Gibot, S.; Gerard, A. Increased muscle-to-serum lactate gradient predicts progression towards septic shock in septic patients. Intensive Care Med. 2010, 36, 1703–1709. [Google Scholar] [CrossRef] [PubMed]
- Joukhadar, C.; Derendorf, H.; Muller, M. Microdialysis. A novel tool for clinical studies of anti-infective agents. Eur. J. Clin. Pharmacol. 2001, 57, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, A.; Steinvall, I.; Sjoberg, F. Microdialysis shows metabolic effects in skin during fluid resuscitation in burn-injured patients. Crit. Care 2006, 10, R172. [Google Scholar] [CrossRef] [PubMed]
- Fall, P.J.; Szerlip, H.M. Lactic acidosis: From sour milk to septic shock. J. Intensive Care Med. 2005, 20, 255–271. [Google Scholar] [CrossRef] [PubMed]
- Michaeli, B.; Martinez, A.; Revelly, J.P.; Cayeux, M.C.; Chiolero, R.L.; Tappy, L.; Berger, M.M. Effects of endotoxin on lactate metabolism in humans. Crit. Care 2012, 16, R139. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Gil, A.; Carrizosa, F.; Herrero, A.; Martin, J.; González, J.; Jareño, A.; Rivero, J. Influence of mechanical ventilation on blood lactate in patients with acute respiratory failure. Intensive Care Med. 1998, 24, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Tantisiriwat, W.; Tebas, P.; Polish, L.B.; Casabar, E.; Powderly, W.G.; Fichtenbaum, C.J. Elevated lactate levels in hospitalized persons with HIV infection. AIDS Res. Hum. Retrovir. 2001, 17, 195–201. [Google Scholar] [CrossRef] [PubMed]
- CMA Microdialysis AB. User Manual for CMA 600 Microdialysis Analyser; CMA Microdialysis AB: Stockholm, Sweden, 2010. [Google Scholar]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; de Mendonca, A.; Cantraine, F.; Moreno, R.; Takala, J.; Suter, P.M.; Sprung, C.L.; Colardyn, F.; Blecher, S. Use of SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit. Care Med. 1998, 26, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
| Age (years) | 67 (24–92) |
|---|---|
| Gender (men/women) | 71/40 |
| APACHE II score | 19 (5–32) |
| SOFA score | 8 (2–15) |
| Mechanical ventilation | 111 |
| HR (beat/min) | 94 (52–200) |
| MAP (mmHg) | 77 (71–120) |
| Temperature (°C) | 36.5 (35.0–39.6) |
| White blood cell count (×103/μL) | 12.400 (12.100–47.910) |
| Hemoglobin (g/L) | 9.9 (5.7–16.4) |
| Creatinine (mg/dL) | 1.6 (0.3–7.9) |
| Bilirubin (mg/dL) | 0.70 (0.20–20.50) |
| PO2/FIO2 | 203 (71–440) |
| C-reactive protein (mg/L) | 130 (71–470) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilias, I.; Apollonatou, S.; Vassiliadi, D.-A.; Nikitas, N.; Theodorakopoulou, M.; Diamantakis, A.; Kotanidou, A.; Dimopoulou, I. Adipose Tissue Lactate Clearance but Not Blood Lactate Clearance Is Associated with Clinical Outcome in Sepsis or Septic Shock during the Post-Resuscitation Period. Metabolites 2018, 8, 28. https://doi.org/10.3390/metabo8020028
Ilias I, Apollonatou S, Vassiliadi D-A, Nikitas N, Theodorakopoulou M, Diamantakis A, Kotanidou A, Dimopoulou I. Adipose Tissue Lactate Clearance but Not Blood Lactate Clearance Is Associated with Clinical Outcome in Sepsis or Septic Shock during the Post-Resuscitation Period. Metabolites. 2018; 8(2):28. https://doi.org/10.3390/metabo8020028
Chicago/Turabian StyleIlias, Ioannis, Sofia Apollonatou, Dimitra-Argyro Vassiliadi, Nikitas Nikitas, Maria Theodorakopoulou, Argyris Diamantakis, Anastasia Kotanidou, and Ioanna Dimopoulou. 2018. "Adipose Tissue Lactate Clearance but Not Blood Lactate Clearance Is Associated with Clinical Outcome in Sepsis or Septic Shock during the Post-Resuscitation Period" Metabolites 8, no. 2: 28. https://doi.org/10.3390/metabo8020028
APA StyleIlias, I., Apollonatou, S., Vassiliadi, D.-A., Nikitas, N., Theodorakopoulou, M., Diamantakis, A., Kotanidou, A., & Dimopoulou, I. (2018). Adipose Tissue Lactate Clearance but Not Blood Lactate Clearance Is Associated with Clinical Outcome in Sepsis or Septic Shock during the Post-Resuscitation Period. Metabolites, 8(2), 28. https://doi.org/10.3390/metabo8020028







