Development and Validation of a High-Throughput Mass Spectrometry Based Urine Metabolomic Test for the Detection of Colonic Adenomatous Polyps
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants and Sample Collection
2.2. NMR Analysis
2.3. Mass Spectrometry Analysis
2.4. Standards
2.5. Sample Processing
2.6. LC-MS Analysis
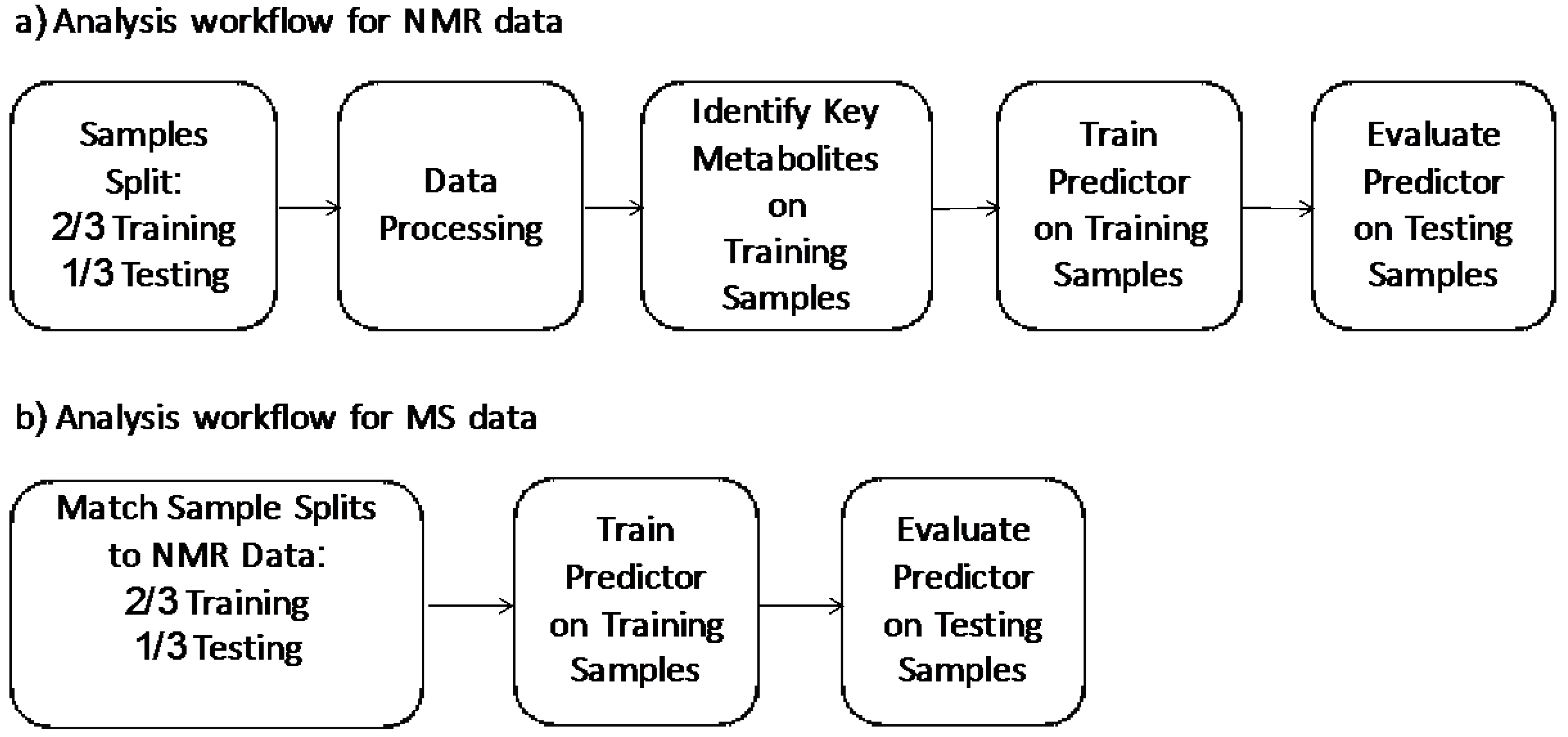
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Key Metabolite Identification
4. LC-MS Measurements
4.1. Development and Validation of the MS Based Test
4.2. Comparison of the MS-Based Metabolomics Test with NMR-Based Test
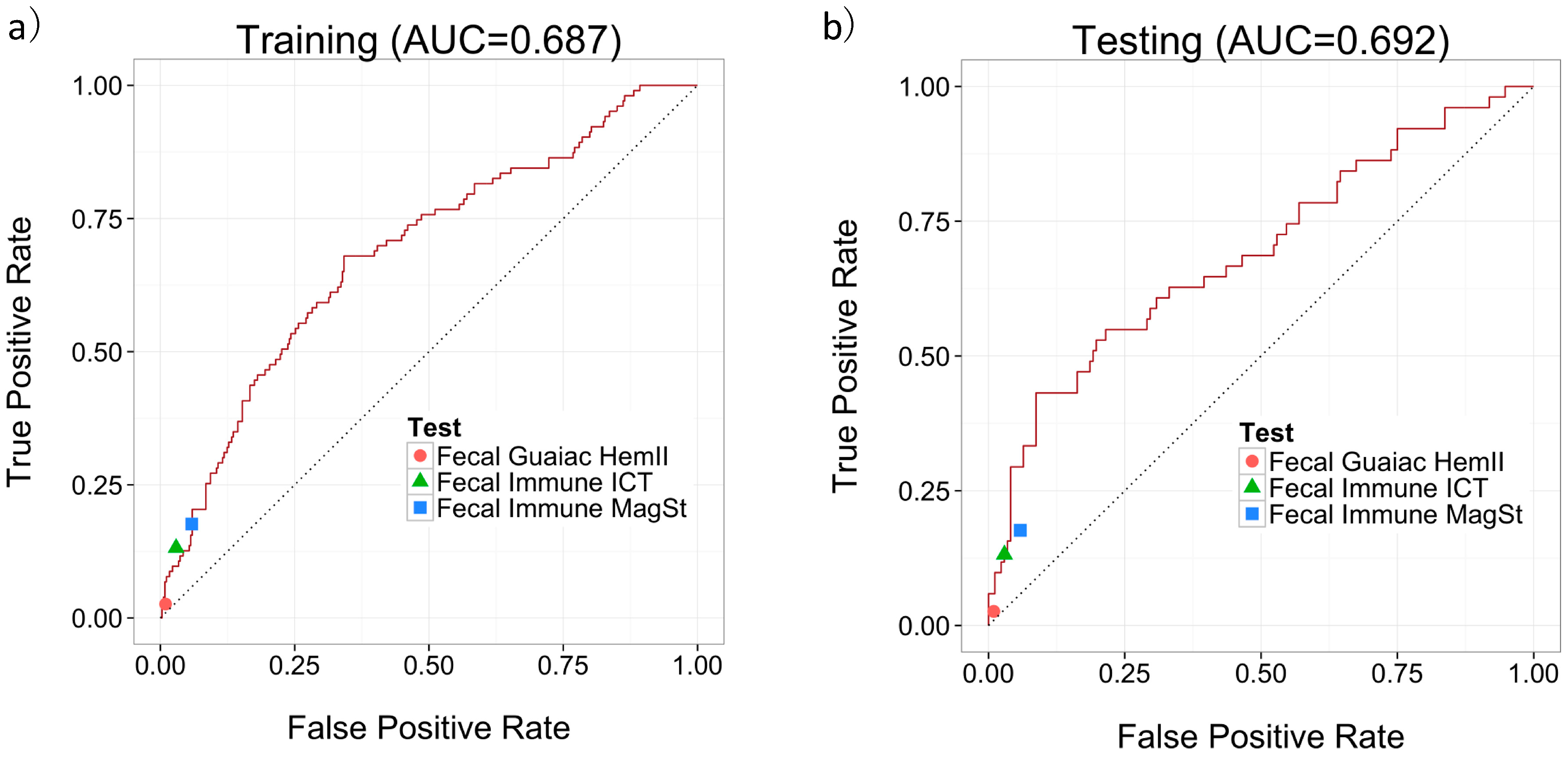
4.3. Comparison of the MS-Based Urine Metabolomics Test with Commercially Available Fecal-Based Tests
5. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Ervik, M.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Globocan 2012 v1.0, Cancer Incidence and Mortality Worldwide: Iarc Cancerbase No. 11; International Agency for Research on Cancer: Lyon, France, 2013. [Google Scholar]
- Parkin, D.M.; Bray, F.; Ferlay, J.; Pisani, P. Global cancer statistics, 2002. CA Cancer J. Clin. 2005, 55, 74–108. [Google Scholar] [CrossRef] [PubMed]
- From Polyp to Cancer. Available online: http://www.hopkinscoloncancercenter.org/CMS/CMS_Page.aspx?CurrentUDV=59&CMS_Page_ID=0B34E9BE-5DE6-4CB4-B387-4158CC924084 (accessed on 20 August 2016).
- Maroun, J.; Ng, E.; Berthelot, J.M.; Le Petit, C.; Dahrouge, S.; Flanagan, W.M.; Walker, H.; Evans, W.K. Lifetime costs of colon and rectal cancer management in canada. Chron. Dis. Can. 2003, 24, 91–101. [Google Scholar]
- Leddin, D.J.; Enns, R.; Hilsden, R.; Plourde, V.; Rabeneck, L.; Sadowski, D.C.; Signh, H. Canadian association of gastroenterology position statement on screening individuals at average risk for developing colorectal cancer: 2010. Can. J. Gastroenterol. 2010, 24, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.P.; Cannon-Albright, L.A.; Sweeney, C.; Williams, M.S.; Haug, P.J.; Mitchell, J.A.; Burt, R.W. Comparison of compliance for colorectal cancer screening and surveillance by colonoscopy based on risk. Genet. Med. 2011, 13, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Eisner, R.; Greiner, R.; Tso, V.; Wang, H.; Fedorak, R.N. A machine-learned predictor of colonic polyps based on urinary metabolomics. Biomed. Res. Int. 2013, 2013, 303982. [Google Scholar] [CrossRef] [PubMed]
- Allison, J.E.; Tekawa, I.S.; Ransom, L.J.; Adrain, A.L. A comparison of fecal occult-blood tests for colorectal-cancer screening. N. Engl. J. Med. 1996, 334, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Fedorak, R.N.; Prosser, C.I.; Stewart, M.E.; van Zanten, S.V.; Sadowski, D.C. The sensitivity and specificity of guaiac and immunochemical fecal occult blood tests for the detection of advanced colonic adenomas and cancer. Int. J. Colorectal Dis. 2012, 27, 1657–1664. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, E.P.; Lin, J.S.; Liles, E.; Beil, T.L.; Fu, R. Screening for colorectal cancer: A targeted, updated systematic review for the u.S. Preventive services task force. Ann. Intern. Med. 2008, 149, 638–658. [Google Scholar] [CrossRef] [PubMed]
- Claudino, W.M.; Quattrone, A.; Biganzoli, L.; Pestrin, M.; Bertini, I.; Di Leo, A. Metabolomics: Available results, current research projects in breast cancer, and future applications. J. Clin. Oncol. 2007, 25, 2840–2846. [Google Scholar] [CrossRef] [PubMed]
- Wishart, D.S.; Jewison, T.; Guo, A.C.; Wilson, M.; Knox, C.; Liu, Y.; Djoumbou, Y.; Mandal, R.; Aziat, F.; Dong, E.; et al. Hmdb 3.0—The human metabolome database in 2013. Nucleic Acids Res. 2013, 41, D801–D807. [Google Scholar] [CrossRef] [PubMed]
- Bouatra, S.; Aziat, F.; Mandal, R.; Guo, A.C.; Wilson, M.R.; Knox, C.; Bjorndahl, T.C.; Krishnamurthy, R.; Saleem, F.; Liu, P.; et al. The human urine metabolome. PLoS ONE 2013, 8, e73076. [Google Scholar] [CrossRef] [PubMed]
- Yoshie, T.; Nishiumi, S.; Izumi, Y.; Sakai, A.; Inoue, J.; Azuma, T.; Yoshida, M. Regulation of the metabolite profile by an apc gene mutation in colorectal cancer. Cancer Sci. 2012, 103, 1010–1021. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.J.; Rawls, J.F.; Randall, T.; Burcal, L.; Mpande, C.N.; Jenkins, N.; Jovov, B.; Abdo, Z.; Sandler, R.S.; Keku, T.O. Molecular characterization of mucosal adherent bacteria and associations with colorectal adenomas. Gut Microbes 2010, 1, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tso, V.K.; Slupsky, C.M.; Fedorak, R.N. Metabolomics and detection of colorectal cancer in humans: A systematic review. Future Oncol. 2010, 6, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Feng, B.; Li, X.; Yin, P.; Gao, P.; Zhao, X.; Lu, X.; Zheng, M.; Xu, G. Urinary metabolic profiling of colorectal carcinoma based on online affinity solid phase extraction-high performance liquid chromatography and ultra performance liquid chromatography-mass spectrometry. Mol. Biosyst. 2010, 6, 1947–1955. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tso, V.; Wong, C.; Sadowski, D.; Fedorak, R.N. Development and validation of a highly sensitive urine-based test to identify patients with colonic adenomatous polyps. Clin. Transl. Gastroenterol. 2014, 5, e54. [Google Scholar] [CrossRef] [PubMed]
- Tso, V.; Eisner, R.; Macleod, S.; Ismond, K.P.; Foshaug, R.R.; Wang, H.; Joseph, R.; Chang, D.; Taylor, N.; Fedorak, R.N. Consistency of metabolite determination from nmr spectra over time and between operators. Metabolomics 2015, 5, 151. [Google Scholar]
- Hastie, T.; Tibshirani, R.; Friedman, J.H. The Elements of Statistical Learning: Data Mining, Inference, and Prediction: With 200 Full-Color Illustrations; Springer: New York, NY, USA, 2001; pp. xvi, 533. [Google Scholar]
- Spratlin, J.L.; Serkova, N.J.; Eckhardt, S.G. Clinical applications of metabolomics in oncology: A review. Clin. Cancer Res. 2009, 15, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Cherkassky, V. The nature of statistical learning theory. IEEE Trans. Neural Netw. 1997, 8, 1564. [Google Scholar] [CrossRef] [PubMed]
- Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. B Met. 1996, 58, 267–288. [Google Scholar]
- Lynch, K.L. Clsi c62-a: A new standard for clinical mass spectrometry. Clin. Chem. 2016, 62, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Arboretti, R.; Bordignon, P.; Corain, L.; Palermo, G.; Pesarin, F.; Salmaso, L. Statistical tests in medical research: Traditional methods vs. Multivariate npc permutation tests. Urologia 2015, 82, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Bilic-Zulle, L. Comparison of methods: Passing and bablok regression. Biochem. Med. (Zagreb) 2011, 21, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Passing, H.; Bablok, W. A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, part I. J. Clin. Chem. Clin. Biochem. 1983, 21, 709–720. [Google Scholar] [PubMed]
- Giovannucci, E.; Colditz, G.A.; Stampfer, M.J.; Hunter, D.; Rosner, B.A.; Willett, W.C.; Speizer, F.E. A prospective study of cigarette smoking and risk of colorectal adenoma and colorectal cancer in US Women. J. Natl. Cancer Inst. 1994, 86, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, C.S.; Giovannucci, E.L.; Colditz, G.A.; Hunter, D.J.; Speizer, F.E.; Willett, W.C. A prospective study of family history and the risk of colorectal cancer. N. Engl. J. Med. 1994, 331, 1669–1674. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.; Xie, G.; Jia, W. Metabonomics of human colorectal cancer: New approaches for early diagnosis and biomarker discovery. J. Proteom. Res. 2014, 13, 3857–3870. [Google Scholar] [CrossRef] [PubMed]
- Rai, B.; Kharb, S.; Jain, R.; Anand, S.C. Salivary vitamins e and c in oral cancer. Redox Rep. 2007, 12, 163–164. [Google Scholar] [CrossRef] [PubMed]
- Wishart, D.S.; Tzur, D.; Knox, C.; Eisner, R.; Guo, A.C.; Young, N.; Cheng, D.; Jewell, K.; Arndt, D.; Sawhney, S.; et al. Hmdb: The human metabolome database. Nucleic Acids Res. 2007, 35, D521–D526. [Google Scholar] [CrossRef] [PubMed]
- Wishart, D.S.; Knox, C.; Guo, A.C.; Eisner, R.; Young, N.; Gautam, B.; Hau, D.D.; Psychogios, N.; Dong, E.; Bouatra, S.; et al. Hmdb: A knowledgebase for the human metabolome. Nucleic Acids Res. 2009, 37, D603–D610. [Google Scholar] [CrossRef] [PubMed]
- Frolkis, A.; Knox, C.; Lim, E.; Jewison, T.; Law, V.; Hau, D.D.; Liu, P.; Gautam, B.; Ly, S.; Guo, A.C.; et al. Smpdb: The small molecule pathway database. Nucleic Acids Res. 2010, 38, D480–D487. [Google Scholar] [CrossRef] [PubMed]
| Label | Colonoscopy Results | Age | Sex | Smoker |
|---|---|---|---|---|
| Normal | Normal (n = 446) | μ = 56.1 | F = 308 | Yes = 50 |
| n = 530 | Hyperplastic (n =84) | σ = 8.2 | M = 222 | Ex-Smoker = 12 |
| No = 449 | ||||
| Unknown = 19 | ||||
| Polyp | Adenoma (n = 154) | μ = 59.9 | F = 60 | Yes = 26 |
| n = 155 | CRC (n = 1) | σ = 7.4 | M = 95 | Ex-Smoker = 4 |
| No = 119 | ||||
| Unknown = 6 |
| P-Value | Metabolite |
|---|---|
| 0.0059 | Succinic acid |
| 0.0100 | Ascorbic acid |
| 0.0280 | Carnitine |
| 0.0595 | Creatine |
| 0.0739 | Citric acid |
| 0.0861 | Methylamine |
| 0.0945 | Pantothenic acid |
| 0.1198 | Fumaric acid |
| 0.1346 | 1-Methylnicotinamide |
| 0.1703 | Trigonelline |
| Training Set | Testing Set | |||||||
|---|---|---|---|---|---|---|---|---|
| Threshold Criteria | Sensitivity | Specificity | PPV | NPV | Sensitivity | Specificity | PPV | NPV |
| Urine tests | ||||||||
| Sens = 90% (95% CI *) | 90.3% (84.6–96.0%) | 20.9% (16.7–25.1%) | 24.9% | 88.0% | 92.2% (84.8–99.5%) | 19.2% (13.3–25.1%) | 25.3% | 89.2% |
| Sens = 80% (95% CI) | 79.6% (71.8–87.4%) | 42.1% (36.9–47.2%) | 28.6% | 87.7% | 82.4% (71.9–92.8%) | 36.0% (28.9–43.2%) | 27.6% | 87.3% |
| Sens = 70% (95% CI) | 69.9% (61.0–78.8%) | 59.0% (53.9–64.2%) | 33.2% | 87.1% | 66.7% (53.7–79.6%) | 55.2% (47.8–62.7%) | 30.6% | 84.8% |
| Spec = 70% (95% CI) | 59.2% (49.7–68.7%) | 70.1% (65.3–74.8%) | 36.5% | 85.5% | 56.9% (43.3–70.5%) | 70.9% (64.1–77.4%) | 35.4% | 84.7% |
| Spec = 80% (95% CI) | 46.6% (37.2–56.2%) | 80.0% (75.8–84.1%) | 40.3% | 83.7% | 49.0% (35.3–62.7%) | 80.8% (74.9–86.7%) | 43.1% | 84.2% |
| Spec = 90% (95% CI) | 31.1% (22.1–40.0%) | 88.1% (84.8–91.5%) | 43.2% | 81.4% | 43.1% (29.5–56.7%) | 91.3% (87.1–95.5%) | 59.5% | 84.4% |
| Fecal Tests | ||||||||
| Guaiac HemII | 2.0% | 98.8% | 33.3% | 77.5% | 3.8% | 99.4% | 66.7% | 77.1% |
| Immune ICT | 10.9% | 97.1% | 52.4% | 78.7% | 17.6% | 97.0% | 64.3% | 79.6% |
| Immune MagSt | 15.8% | 95.4% | 50.0% | 79.5% | 21.2% | 91.7% | 44.0% | 79.1% |
| Feature | PubChem CID | HMDB | Correlation |
|---|---|---|---|
| Smoker | N/A | N/A | 0.09 |
| Age | N/A | N/A | 0.13 |
| Sex | N/A | N/A | 0.17 |
| Succinic Acid | 1110 | HMDB00254 | −0.16 |
| Ascorbic Acid | 54670067 | HMDB00044 | −0.15 |
| Carnitine | 2724480 | HMDB00062 | −0.13 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deng, L.; Chang, D.; Foshaug, R.R.; Eisner, R.; Tso, V.K.; Wishart, D.S.; Fedorak, R.N. Development and Validation of a High-Throughput Mass Spectrometry Based Urine Metabolomic Test for the Detection of Colonic Adenomatous Polyps. Metabolites 2017, 7, 32. https://doi.org/10.3390/metabo7030032
Deng L, Chang D, Foshaug RR, Eisner R, Tso VK, Wishart DS, Fedorak RN. Development and Validation of a High-Throughput Mass Spectrometry Based Urine Metabolomic Test for the Detection of Colonic Adenomatous Polyps. Metabolites. 2017; 7(3):32. https://doi.org/10.3390/metabo7030032
Chicago/Turabian StyleDeng, Lu, David Chang, Rae R. Foshaug, Roman Eisner, Victor K. Tso, David S. Wishart, and Richard N. Fedorak. 2017. "Development and Validation of a High-Throughput Mass Spectrometry Based Urine Metabolomic Test for the Detection of Colonic Adenomatous Polyps" Metabolites 7, no. 3: 32. https://doi.org/10.3390/metabo7030032
APA StyleDeng, L., Chang, D., Foshaug, R. R., Eisner, R., Tso, V. K., Wishart, D. S., & Fedorak, R. N. (2017). Development and Validation of a High-Throughput Mass Spectrometry Based Urine Metabolomic Test for the Detection of Colonic Adenomatous Polyps. Metabolites, 7(3), 32. https://doi.org/10.3390/metabo7030032





