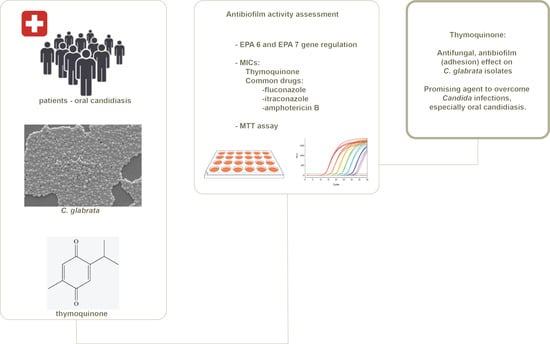
Thymoquinone Antifungal Activity against Candida glabrata Oral Isolates from Patients in Intensive Care Units—An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Thymoquinone and Antifungal Drugs
2.3. Patients’ Characteristics
2.4. Clinical Specimens Processing and Identification of Isolates
2.5. Antifungal Susceptibility Testing (AFST)
2.6. Real-Time PCR Assay
2.7. Antibiofilm Activity of TQ
3. Results
3.1. Clinical Data of the Patients
3.2. Antifungal Susceptibility Testing (AFST) against TQ and Antifungal Drugs and the Effects of TQ on the Biofilm Formation of C. glabrata
3.3. Effects of TQ on the Expression of EPA6 and EPA7 Genes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dongari-Bagtzoglou, A.; Dwivedi, P.; Ioannidou, E.; Shaqman, M.; Hull, D.; Burleson, J. Oral Candida infection and colonization in solid organ transplant recipients. Oral Microbiol. Immunol. 2009, 24, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Rossoni, R.D.; Barbosa, J.O.; Vilela, S.F.G.; dos Santos, J.D.; de Barros, P.P.; de Azevedo Prata, M.C.; Anbinder, A.L.; Fuchs, B.B.; Jorge, A.O.C.; Mylonakis, E.; et al. Competitive interactions between C. albicans, C. glabrata and C. krusei during biofilm formation and development of experimental candidiasis. PLoS ONE 2015, 10, e0131700. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.; Benjamin Jr, D.K.; Calandra, T.F.; Edwards, J.E., Jr.; Filler, S.G.; Fisher, J.F.; Kullberg, B.-J.; Ostrosky-Zeichner, L.; et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2009, 48, 503. [Google Scholar] [CrossRef] [PubMed]
- Soysa, N.; Ellepola, A. The impact of cigarette/tobacco smoking on oral candidosis: An overview. Oral Dis. 2005, 11, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Jan, A.; Bashir, G.; Fomda, B.A.; Fatima, A.; Lone, M.S.; Roohi, S. Molecular identification of Candida dubliniensis among Candida albicans isolated from oral cavity of cancer patients using PCR-RFLP, in a tertiary care Hospital in Kashmir, India. Br. Microbiol. Res. J. 2016, 14, 1–7. [Google Scholar] [CrossRef]
- Lamoth, F.; Lockhart, S.R.; Berkow, E.L.; Calandra, T. Changes in the epidemiological landscape of invasive candidiasis. J. Antimicrob. Chemother. 2018, 73, i4–i13. [Google Scholar] [CrossRef]
- Whaley, S.G.; Berkow, E.L.; Rybak, J.M.; Nishimoto, A.T.; Barker, K.S.; Rogers, P.D. Azole antifungal resistance in Candida albicans and emerging non-albicans Candida species. Front. Microbiol. 2017, 7, 2173. [Google Scholar] [CrossRef]
- Almirante, B.; Rodríguez, D.; Park, B.J.; Cuenca-Estrella, M.; Planes, A.M.; Almela, M.; Mensa, J.; Sanchez, F.; Ayats, J.; Gimenez, M.; et al. Epidemiology and predictors of mortality in cases of Candida bloodstream infection: Results from population-based surveillance, Barcelona, Spain, from 2002 to 2003. J. Clin. Microbiol. 2005, 43, 1829–1835. [Google Scholar] [CrossRef]
- Fidel Jr, P.L.; Vazquez, J.A.; Sobel, J.D. Candida glabrata: Review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin. Microbiol. Rev. 1999, 12, 80–96. [Google Scholar] [CrossRef]
- Kao, A.S.; Brandt, M.E.; Pruitt, W.R.; Conn, L.A.; Perkins, B.A.; Stephens, D.S.; Baughman, W.S.; Reingold, A.L.; Rothrock, G.A.; Pfaller, M.A.; et al. The epidemiology of candidemia in two United States cities: Results of a population-based active surveillance. Clin. Infect. Dis. 1999, 29, 1164–1170. [Google Scholar] [CrossRef]
- Kusne, S.; Tobin, D.; Pasculle, A.W.; Van Thiel, D.H.; Ho, M.; Starzl, T.E. Candida carriage in the alimentary tract of liver transplant candidates. Transplantation 1994, 57, 398. [Google Scholar] [CrossRef] [PubMed]
- Lass-Flörl, C. The changing face of epidemiology of invasive fungal disease in Europe. Mycoses 2009, 52, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.F.; Silva, S.; Henriques, M. Candida glabrata: A review of its features and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 673–688. [Google Scholar] [CrossRef]
- Sánchez-Vargas, L.O.; Estrada-Barraza, D.; Pozos-Guillen, A.J.; Rivas-Caceres, R. Biofilm formation by oral clinical isolates of Candida species. Arch. Oral Biol. 2013, 58, 1318–1326. [Google Scholar] [CrossRef] [PubMed]
- Martins, C.H.G.; Pires, R.H.; Cunha, A.O.; Pereira, C.A.M.; de Lacorte Singulani, J.; Abrão, F.; de Moraes, T.; Mendes-Giannini, M.J.S. Candida/Candida biofilms. First description of dual-species Candida albicans/C. rugosa biofilm. Fungal Biol. 2016, 120, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Coordination, G.; Alastruey-Izquierdo, A.; World Health Organization. WHO Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Vila, T.; Sultan, A.S.; Montelongo-Jauregui, D.; Jabra-Rizk, M.A. Oral candidiasis: A disease of opportunity. J. Fungi 2020, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- d’Enfert, C.; Janbon, G. Biofilm formation in Candida glabrata: What have we learnt from functional genomics approaches? FEMS Yeast Res. 2016, 16. [Google Scholar] [CrossRef]
- Valotteau, C.; Prystopiuk, V.; Cormack, B.P.; Dufrêne, Y.F. Atomic force microscopy demonstrates that Candida glabrata uses three Epa proteins to mediate adhesion to abiotic surfaces. Msphere 2019, 4, e00277-19. [Google Scholar] [CrossRef] [PubMed]
- Tam, P.; Gee, K.; Piechocinski, M.; Macreadie, I. Candida glabrata, friend and foe. J. Fungi 2015, 1, 277–292. [Google Scholar] [CrossRef]
- Modrzewska, B.; Kurnatowski, P. Adherence of Candida sp. to host tissues and cells as one of its pathogenicity features. Ann. Parasitol. 2015, 61, 3–9. [Google Scholar]
- de Groot, P.W.; Bader, O.; de Boer, A.D.; Weig, M.; Chauhan, N. Adhesins in human fungal pathogens: Glue with plenty of stick. Eukaryot. Cell 2013, 12, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.F.; Rodrigues, M.E.; Silva, S.; Henriques, M. Candida glabrata biofilms: How far have we come? J. Fungi 2017, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Kucharíková, S.; Tournu, H.; Lagrou, K.; Van Dijck, P.; Bujdakova, H. Detailed comparison of Candida albicans and Candida glabrata biofilms under different conditions and their susceptibility to caspofungin and anidulafungin. J. Med. Microbiol. 2011, 60, 1261–1269. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, A.; Roudbary, M.; Mohammadi, R.; Černáková, L.; Rodrigues, C.F. Overview on the Infections Related to Rare Candida Species. Pathogens 2022, 11, 963. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Voss, A.; Meis, J. Multidrug-resistant Candida auris: ‘New kid on the block’ in hospital-associated infections? J. Hosp. Infect. 2016, 94, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Farmakiotis, D.; Kontoyiannis, D.P. Epidemiology of antifungal resistance in human pathogenic yeasts: Current viewpoint and practical recommendations for management. Int. J. Antimicrob. Agents 2017, 50, 318–324. [Google Scholar] [CrossRef]
- Salem, M.L. Immunomodulatory and therapeutic properties of the Nigella sativa L. seed. Int. Immunopharmacol. 2005, 5, 1749–1770. [Google Scholar] [CrossRef]
- Nasser, V.H.; Hassan, R. Antibacterial and antifungal effects of Nigella sativa extracts against S. aureus, P. aeroginosa and C. albicans. Pak. J. Med. Sci. 2015, 21, 47–52. [Google Scholar]
- İşcan, G.; İşcan, A.; Demirci, F. Anticandidal effects of thymoquinone: Mode of action determined by transmission electron microscopy (TEM). Nat. Prod. Commun. 2016, 11, 1934578X1601100726. [Google Scholar] [CrossRef]
- Mahmoudvand, H.; Sepahvand, A.; Jahanbakhsh, S.; Ezatpour, B.; Mousavi, S.A. Evaluation of antifungal activities of the essential oil and various extracts of Nigella sativa and its main component, thymoquinone against pathogenic dermatophyte strains. J. De Mycol. Med. 2014, 24, e155–e161. [Google Scholar] [CrossRef]
- Aftab, A.; Yousaf, Y.; Javaid, A.; Riaz, N.; Younas, A.; Rashid, M.; Bushra, H.; Chahel, A.A. Antifungal activity of vegetative methanolic extracts of Nigella sativa against Fusarium oxysporum and Macrophomina phaseolina and its phytochemical profiling by GC-MS analysis. Int. J. Agric. Biol. 2019, 21, 569–576. [Google Scholar]
- Akhtar, N.; Alakloby, O.M.; Aljabre, S.H.M.; Alqurashi, A.R.M.; Randhawa, M.A. Comparison of antifungal activity of thymoquinone and amphotericin B against Fusarium solani in vitro. Sci. J. King Faisal Univ. (Basic Appl. Sci.) 2007, 8, 1428H. [Google Scholar]
- Özdal Zincir, Ö.; Özdal, U.; Ünlü, Ö.; Demirci, M.; Katiboğlu, A.B.; Egil, E.; Altan Şallı, G. Synergistic effect of thymoquinone and nystatin in the treatment of oral candidiasis; an in vitro study. Odontology 2022, 110, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Rahsepar, S.; Delavari Kiadeh, H.; Roudbari, M. Design and Synthesis of Novel Thymoquinone-Zein Nanoparticles; Evaluation of the Inhibitory Effect on Candida albicans and Biofilm Formation In Vitro. Infect. Epidemiol. Microbiol. 2022, 8, 169–176. [Google Scholar] [CrossRef]
- Akpan, A.; Morgan, R. Oral candidiasis. Postgrad. Med. J. 2002, 78, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Lalla, R.V.; Sonis, S.T.; Peterson, D.E. Management of oral mucositis in patients who have cancer. Dent. Clin. North Am. 2008, 52, 61–77. [Google Scholar] [CrossRef]
- SÁnchez, M.E.G.; Ramirez-Amador, V.; Saavedra, G.A.; Camacho, M.E.I.; Vargas, L.O.S. Oral Candida colonization and infection in hiv-infected patients in a referral center in Mexico City. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, e32. [Google Scholar] [CrossRef]
- Arastehfar, A.; Fang, W.; Pan, W.; Lackner, M.; Liao, W.; Badiee, P.; Zomorodian, K.; Badali, H.; Hagen, F.; Lass-Flörl, C.; et al. YEAST PANEL multiplex PCR for identification of clinically important yeast species: Stepwise diagnostic strategy, useful for developing countries. Diagn. Microbiol. Infect. Dis. 2019, 93, 112–119. [Google Scholar] [CrossRef]
- Santos, E.R.d.; Forno, C.F.D.; Hernandez, M.G.; Kubiça, T.F.; Venturini, T.P.; Chassot, F.; Santurio, J.M.; Alves, S.H. Susceptibility of Candida spp. isolated from blood cultures as evaluated using the M27-A3 and new M27-S4 approved breakpoints. Rev. Do Inst. De Med. Trop. De São Paulo 2014, 56, 477–482. [Google Scholar] [CrossRef]
- Pfaller, M.; Diekema, D. Progress in antifungal susceptibility testing of Candida spp. by use of Clinical and Laboratory Standards Institute broth microdilution methods, 2010 to 2012. J. Clin. Microbiol. 2012, 50, 2846–2856. [Google Scholar] [CrossRef]
- Roudbary, M.; Alimohammadi, A.; Tavallaei, M.R.; Zarimeidani, R.; Nikoomanesh, F. Antifungal activity of Thymus kotschyanus extract: An in vitro study on the expression of CDR1 and CDR2 genes in clinical isolates of Candida albicans. J. Herb. Med. 2023, 38, 100644. [Google Scholar] [CrossRef]
- Almshawit, H.; Macreadie, I. Fungicidal effect of thymoquinone involves generation of oxidative stress in Candida glabrata. Microbiol. Res. 2017, 195, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, H. Factors influencing the virulence of Candida spp. West Indian Med. J. 2009, 58, 160. [Google Scholar] [PubMed]
- Benazzouz-Smail, L.; Achat, S.; Brahmi, F.; Bachir-Bey, M.; Arab, R.; Lorenzo, J.M.; Benbouriche, A.; Boudiab, K.; Hauchard, D.; Boulekbache, L.; et al. Biological Properties, Phenolic Profile, and Botanical Aspect of Nigella sativa L. and Nigella damascena L. Seeds: A Comparative Study. Molecules 2023, 28, 571. [Google Scholar] [CrossRef] [PubMed]
- Khedri, S.; Santos, A.; Roudbary, M.; Hadighi, R.; Falahati, M.; Farahyar, S.; Khoshmirsafa, M.; Kalantari, S. Iranian HIV/AIDS patients with oropharyngeal candidiasis: Identification, prevalence and antifungal susceptibility of Candida species. Lett. Appl. Microbiol. 2018, 67, 392–399. [Google Scholar] [CrossRef]
- Miranda-Cadena, K.; Marcos-Arias, C.; Mateo, E.; Aguirre, J.M.; Quindós, G.; Eraso, E. Prevalence and antifungal susceptibility profiles of Candida glabrata, Candida parapsilosis and their close-related species in oral candidiasis. Arch. Oral Biol. 2018, 95, 100–107. [Google Scholar] [CrossRef]
- Khalil, M.A.; El-Ansary, M.R.; Bassyouni, R.H.; Mahmoud, E.E.; Ali, I.A.; Ahmed, T.I.; Hassan, E.A.; Samir, T.M. Oropharyngeal candidiasis among Egyptian COVID-19 patients: Clinical characteristics, species identification, and antifungal susceptibility, with disease severity and fungal coinfection prediction models. Diagnostics 2022, 12, 1719. [Google Scholar] [CrossRef]
- de la Rosa-García, E.; Olalde-Hernández, M.; Irigoyen-Camacho, M.; Mondragón-Padilla, A.; Mendoza-Juache, A.; Sánchez-Vargas, L. Antifungal susceptibility of oral isolates of Candida species from chronic kidney disease patients on chronic dialysis. J. De Mycol. Médicale 2020, 30, 101009. [Google Scholar] [CrossRef]
- McCall, A.; Edgerton, M. Real-time approach to flow cell imaging of Candida albicans biofilm development. J. Fungi 2017, 3, 13. [Google Scholar] [CrossRef]
- Al-Thobity, A.M.; Al-Khalifa, K.S.; Gad, M.M.; Al-Hariri, M.; Ali, A.A.; Alnassar, T. In vitro evaluation of the inhibitory activity of thymoquinone in combatting Candida albicans in denture stomatitis prevention. Int. J. Environ. Res. Public Health 2017, 14, 743. [Google Scholar] [CrossRef]
- Randhawa, M.A.; Gondal, M.A.; Al-Zahrani, A.-H.J.; Rashid, S.G.; Ali, A. Synthesis, morphology and antifungal activity of nano-particulated amphotericin-B, ketoconazole and thymoquinone against Candida albicans yeasts and Candida biofilm. J. Environ. Sci. Health Part A 2015, 50, 119–124. [Google Scholar] [CrossRef]
- Khan, M.A.; Aljarbou, A.N.; Khan, A.; Younus, H. Liposomal thymoquinone effectively combats fluconazole-resistant Candida albicans in a murine model. Int. J. Biol. Macromol. 2015, 76, 203–208. [Google Scholar] [CrossRef] [PubMed]
- El-Kirat-Chatel, S.; Beaussart, A.; Derclaye, S.; Alsteens, D.; Kucharikova, S.; Van Dijck, P.; Dufrêne, Y.F. Force nanoscopy of hydrophobic interactions in the fungal pathogen Candida glabrata. Acs Nano 2015, 9, 1648–1655. [Google Scholar] [CrossRef] [PubMed]
- Tsang, P.W.-K.; Bandara, H.; Fong, W.-P. Purpurin suppresses Candida albicans biofilm formation and hyphal development. PLoS ONE 2012, 7, e50866. [Google Scholar] [CrossRef] [PubMed]
- Deorukhkar, S.C.; Saini, S.; Mathew, S. Non-albicans Candida infection: An emerging threat. Interdiscip. Perspect. Infect. Dis. 2014, 2014, 615958. [Google Scholar] [CrossRef]
- Mushi, M.F.; Mtemisika, C.I.; Bader, O.; Bii, C.; Mirambo, M.M.; Groß, U.; Mshana, S.E. High oral carriage of non-albicans Candida spp. among HIV-infected individuals. Int. J. Infect. Dis. 2016, 49, 185–188. [Google Scholar] [CrossRef] [PubMed]
| Gene | Primer | Sequence |
|---|---|---|
| ACT1 | Forward | 5′-AGAGCCGTCTTCCCTTCCAT-3′ |
| ACT1 | Reverse | 5′-TTGACCCATACCGACCATGA-3 |
| EPA6 | Forward | 5′-AAAGCCTCAATGGTATGACAGAAGAC-3′ |
| EPA6 | Reverse | 5′-CAGATGAATTTTGGAATGGGAAA-3′ |
| EPA7 | Forward | 5′-GGCTGGCTTTCGTGCAATA-3′ |
| EPA7 | Reverse | 5′-CGACGGACCCTTGTAAGATTGT-3′ |
| Feature | Total n (%) | p Value |
|---|---|---|
| Age (age range 15–95 years mean ± SD 59 ± 11.4) | <30 5 (5.5%) | 0.06 |
| >30 85 (94.4) | 0.002 | |
| Gender (total n) | n = 40 | 0.101 |
| Male | 19 (47.5) | |
| Female | 21 (52.5) | |
| Cancer Positive | 13 (32.5) | |
| 1 COPD Positive | 6 (15) | |
| Pneumonia Positive | 6 (15) | 0.021 |
| Previous use antifungal drugs | 12 (30) | 0.06 |
| Antibacterial therapy | 40 (100) | 0.008 |
| Immunosuppressive drugs | 19 (47.5) | 0.006 |
| Duration of admission | 3–10 days (>6 days) | 0.007 |
| TQ MIC Range 25–100 | FLZ GM;10.11 | ITZ GM;0.51 | AMB GM;0.57 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC50 | MIC90 | MIC50 | MIC90 | MIC range | R ≥64 | S | SDD ≤32 | MIC50 | MIC90 | MIC range | R ≥2 | SDD 0.5 ≤ MIC ≤ 0.25 | S ≤0.125 | MIC50 | MIC90 | MIC range | R ≥ 2 | S ≤1 |
| 50 | 100 | 16 | 64 | 4–64 | (n = 29, 72.5%) | 0 | (n = 11, 27.5%) | 0.5 | 1 | 0.125–0.2 | (n = 5, 12.5%) | (n = 20, 50%) | (n = 15, 37.5%) | 0.5 | 1 | 0.25–2 | (n = 2,−5% | (n = 38, −95% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nouri, N.; Mohammadi, S.R.; Beardsley, J.; Aslani, P.; Ghaffarifar, F.; Roudbary, M.; Rodrigues, C.F. Thymoquinone Antifungal Activity against Candida glabrata Oral Isolates from Patients in Intensive Care Units—An In Vitro Study. Metabolites 2023, 13, 580. https://doi.org/10.3390/metabo13040580
Nouri N, Mohammadi SR, Beardsley J, Aslani P, Ghaffarifar F, Roudbary M, Rodrigues CF. Thymoquinone Antifungal Activity against Candida glabrata Oral Isolates from Patients in Intensive Care Units—An In Vitro Study. Metabolites. 2023; 13(4):580. https://doi.org/10.3390/metabo13040580
Chicago/Turabian StyleNouri, Noura, Shahla Roudbar Mohammadi, Justin Beardsley, Peyman Aslani, Fatemeh Ghaffarifar, Maryam Roudbary, and Célia Fortuna Rodrigues. 2023. "Thymoquinone Antifungal Activity against Candida glabrata Oral Isolates from Patients in Intensive Care Units—An In Vitro Study" Metabolites 13, no. 4: 580. https://doi.org/10.3390/metabo13040580
APA StyleNouri, N., Mohammadi, S. R., Beardsley, J., Aslani, P., Ghaffarifar, F., Roudbary, M., & Rodrigues, C. F. (2023). Thymoquinone Antifungal Activity against Candida glabrata Oral Isolates from Patients in Intensive Care Units—An In Vitro Study. Metabolites, 13(4), 580. https://doi.org/10.3390/metabo13040580