Effects of Low- and High-Frequency Cardiac Rehabilitation on Risk Factors, Physical Fitness and Quality of Life in Middle-Aged Women with Coronary Heart Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Procedure and Participants
2.2. Blood Collection
2.3. Body Composition and Anthropometry
2.4. Fitness Test
2.5. SF-36
2.6. Cardiac Rehabilitation Program and Exercise Prescription
2.7. Statistical Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Blood Pressure, Body Composition, Body Mass Index, and Body Composition
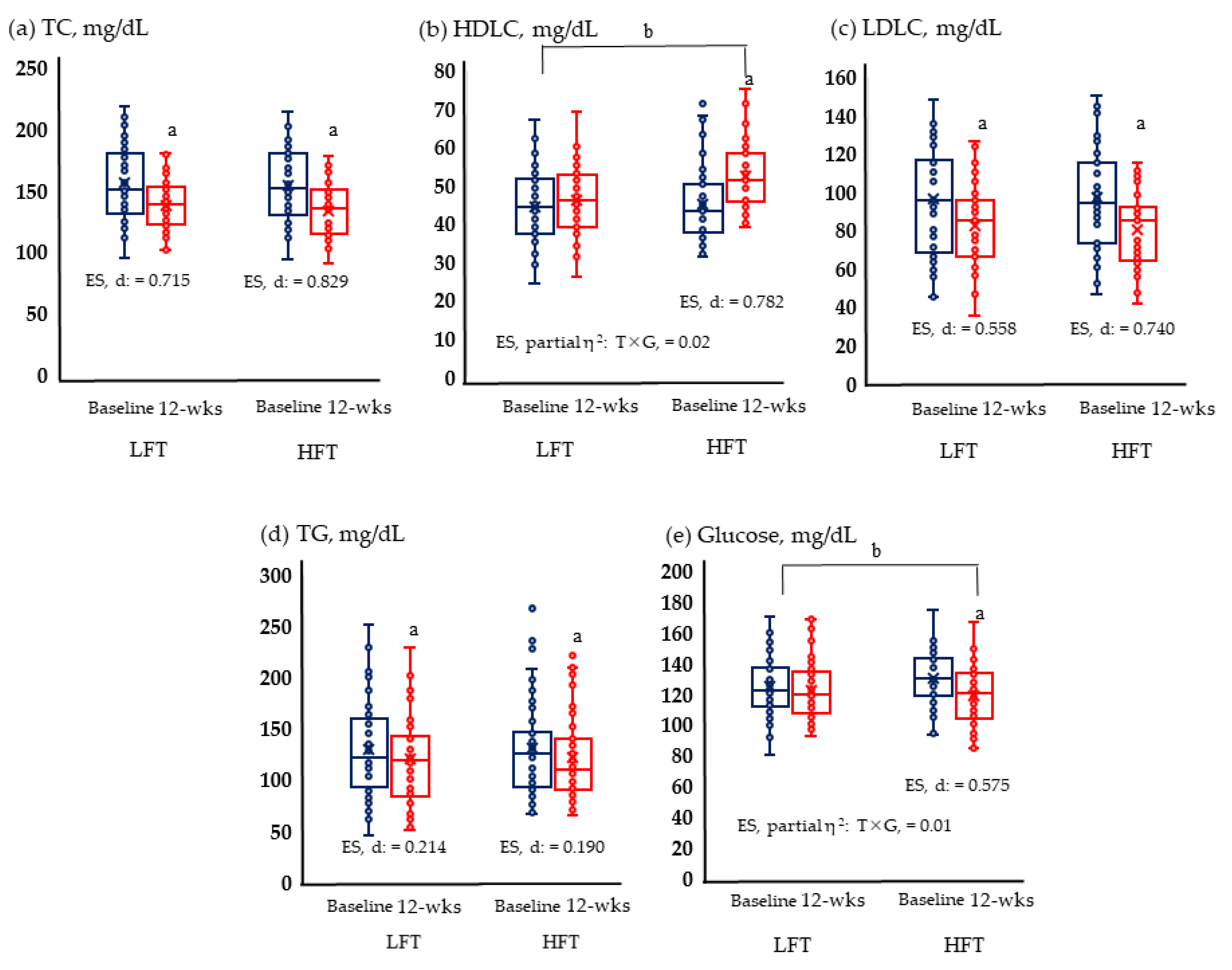
3.3. Lipid Risk Factors for Cardiovascular Disease
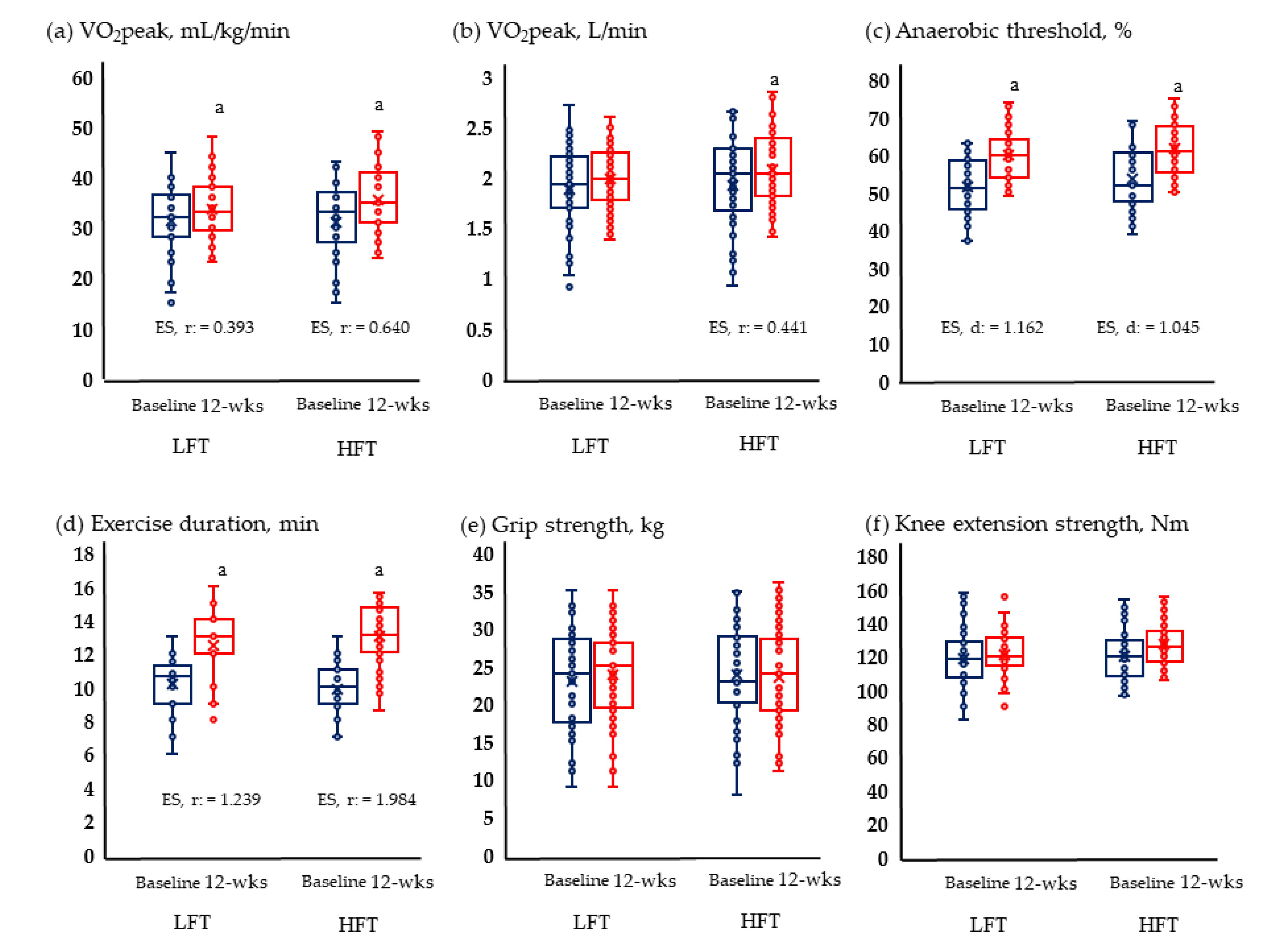
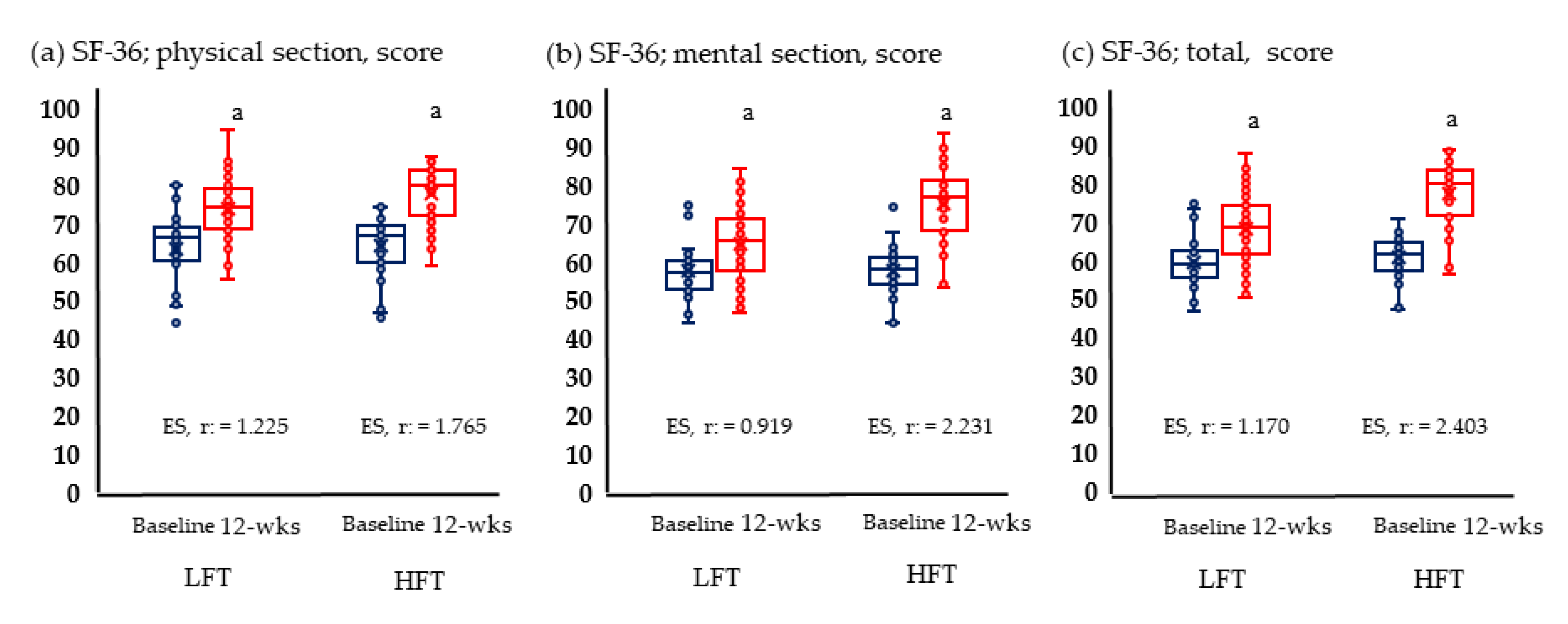
3.4. Physical Fitness and Quality of Life
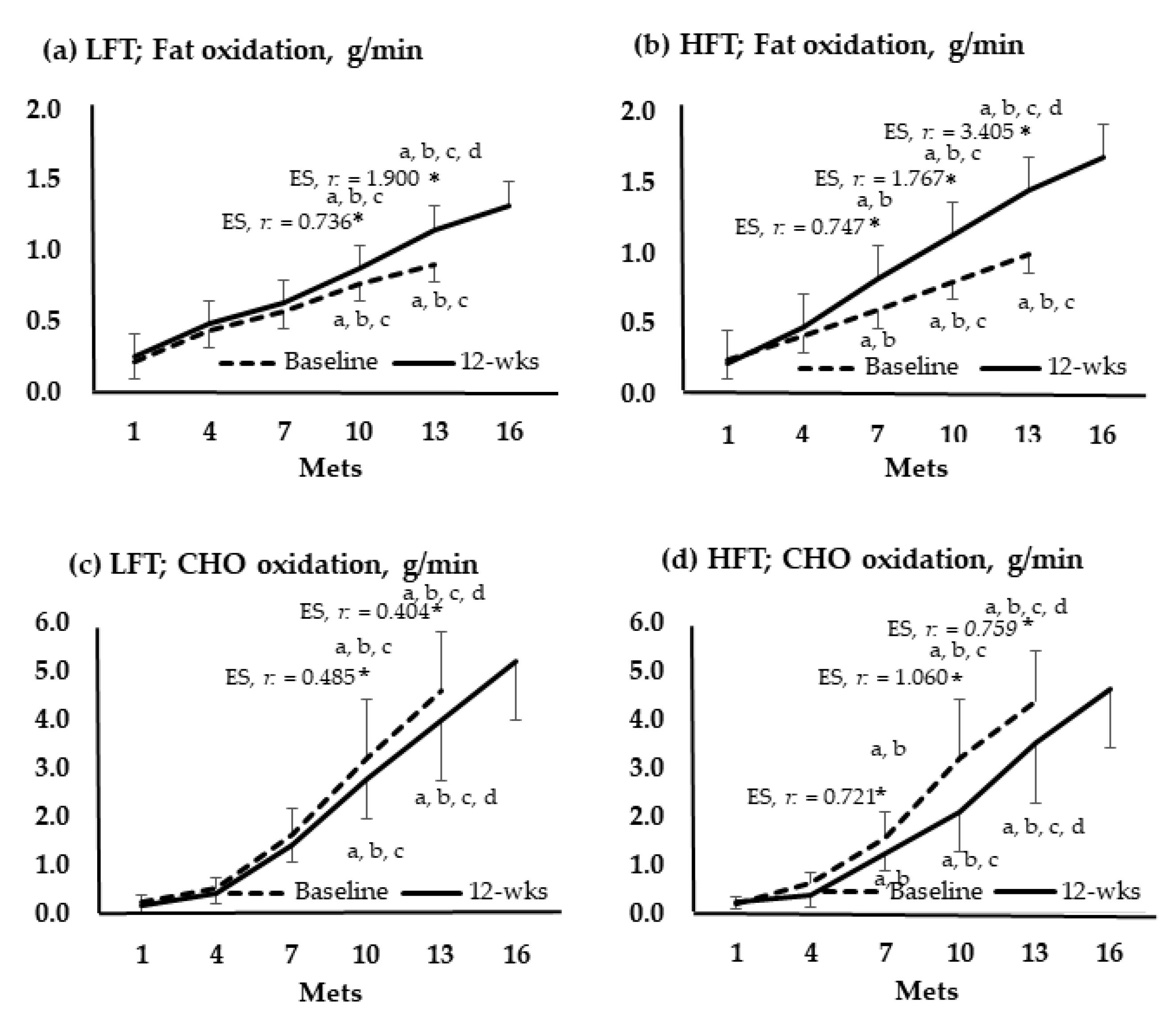
3.5. Metabolic Flexibility
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malakar, A.K.; Choudhury, D.; Halder, B.; Paul, P.; Uddin, A.; Chakraborty, S. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 2019, 234, 16812–16823. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular risks associated with gender and aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.; Colantonio, L.D.; Dai, Y.; Zhao, H.; Bittner, V.; Farkouh, M.E.; Dluzniewski, P.; Poudel, B.; Muntner, P.; Woodward, M. Trends in recurrent coronary heart disease after myocardial infarction among US women and men between 2008 and 2017. Circulation 2021, 143, 650–660. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; McCann, N.; Bluhm, M.; Zuhl, M. Exercise Prescription and Progression Practices among US Cardiac Rehabilitation Clinics. Clin. Pract. 2022, 12, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Moghei, M.; Oh, P.; Chessex, C.; Grace, S.L. Cardiac rehabilitation quality improvement: A narrative review. J. Cardiopulm. Rehabil. Prev. 2019, 39, 226–234. [Google Scholar] [CrossRef]
- Peersen, K.; Munkhaugen, J.; Gullestad, L.; Liodden, T.; Moum, T.; Dammen, T.; Perk, J.; Otterstad, J.E. The role of cardiac rehabilitation in secondary prevention after coronary events. Eur. J. Prev. Cardiol. 2017, 24, 1360–1368. [Google Scholar] [CrossRef]
- Santiago de Araújo Pio, C.; Chaves, G.; Davies, P.; Taylor, R.; Grace, S. Interventions to promote patient utilization of cardiac rehabilitation: Cochrane systematic review and meta-analysis. J. Clin. Med. 2019, 8, 189–207. [Google Scholar]
- Ji, H.; Fang, L.; Yuan, L.; Zhang, Q. Effects of exercise-based cardiac rehabilitation in patients with acute coronary syndrome: A meta-analysis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 5015–5027. [Google Scholar] [CrossRef]
- Dibben, G.O.; Dalal, H.M.; Taylor, R.S.; Doherty, P.; Tang, L.H.; Hillsdon, M. Cardiac rehabilitation and physical activity: Systematic review and meta-analysis. Heart 2018, 104, 1394–1402. [Google Scholar] [CrossRef]
- Baig, M.; Imran, H.M.; Gaw, A.; Stabile, L.; Wu, W.-C. Cardiac rehabilitation in women; comparison of enrollment, adherence and outcomes between heart failure and coronary artery disease. Heart Lung 2021, 50, 223–229. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Witt, B.J.; Allison, T.G.; Hayes, S.N.; Weston, S.A.; Koepsell, E.; Roger, V.L. Barriers to participation in cardiac rehabilitation. Am. Heart J. 2009, 158, 852–859. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Cho, K.K.; Kim, Y.H. Low 6-Minute Walk Distance and Muscle Mass Predict Drop out in Cardiac Rehabilitation. Healthcare 2020, 8, 430. [Google Scholar] [CrossRef] [PubMed]
- Chindhy, S.; Taub, P.R.; Lavie, C.J.; Shen, J. Current challenges in cardiac rehabilitation: Strategies to overcome social factors and attendance barriers. Expert Rev. Cardiovasc. Ther. 2020, 18, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Reichert, F.F.; Barros, A.J.; Domingues, M.R.; Hallal, P.C. The role of perceived personal barriers to engagement in leisure-time physical activity. Am. J. Public Health 2007, 97, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Abell, B.; Glasziou, P.; Briffa, T.; Hoffmann, T. Exercise training characteristics in cardiac rehabilitation programmes: A cross-sectional survey of Australian practice. Open Heart 2016, 3, e000374–e000382. [Google Scholar] [CrossRef] [PubMed]
- Supervía, M.; Medina-Inojosa, J.R.; Yeung, C.; Lopez-Jimenez, F.; Squires, R.W.; Pérez-Terzic, C.M.; Brewer, L.C.; Leth, S.E.; Thomas, R.J. Cardiac rehabilitation for women: A systematic review of barriers and solutions. Mayo Clin. Proc. 2017, 92, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Resurreccion, D.M.; Motrico, E.; Rigabert, A.; Rubio-Valera, M.; Conejo-Ceron, S.; Pastor, L.; Moreno-Peral, P. Barriers for nonparticipation and dropout of women in cardiac rehabilitation programs: A systematic review. J. Women’s Health 2017, 26, 849–859. [Google Scholar] [CrossRef]
- Rohrbach, G.; Schopfer, D.W.; Krishnamurthi, N.; Pabst, M.; Bettencourt, M.; Loomis, J.; Whooley, M.A. The design and implementation of a home-based cardiac rehabilitation program. Fed. Pract. 2017, 34, 34–39. [Google Scholar]
- Bostrom, J.; Sweeney, G.; Whiteson, J.; Dodson, J.A. Mobile health and cardiac rehabilitation in older adults. Clin. Cardiol. 2020, 43, 118–126. [Google Scholar] [CrossRef]
- Lear, S.A. The delivery of cardiac rehabilitation using communications technologies: The “virtual” cardiac rehabilitation program. Can. J. Cardiol. 2018, 34, S278–S283. [Google Scholar] [CrossRef]
- Berkhuysen, M.A.; Nieuwland, W.; Buunk, B.P.; Sanderman, R.; Viersma, J.; Rispens, P. Effect of high-versus low-frequency exercise training in multidisciplinary cardiac rehabilitation on health-related quality of life. J. Cardiopulm. Rehabil. Prev. 1999, 19, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Nieuwland, W.; Berkhuysen, M.A.; van Veldhuisen, D.J.; Brügemann, J.; Landsman, M.L.; van Sonderen, E.; Lie, K.; Crijns, H.J.; Rispens, P. Differential effects of high-frequency versus low-frequency exercise training in rehabilitation of patients with coronary artery disease. J. Am. Coll. Cardiol. 2000, 36, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Su, N.; Kim, Y.; Won, Y. Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study. Healthcare 2021, 9, 1093. [Google Scholar] [CrossRef]
- Sanchis-Gomar, F.; Perez-Quilis, C.; Leischik, R.; Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann. Transl. Med. 2016, 4, 256–267. [Google Scholar] [CrossRef] [PubMed]
- Liguori, G.; Medicine, A.C.O.S. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Yang, W.-H.; Park, J.-H.; Park, S.-Y.; Park, Y. Energetic Contributions Including Gender Differences and Metabolic Flexibility in the General Population and Athletes. Metabolites 2022, 12, 965. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Dvir, Z. Isokinetics: Muscle Testing, Interpretation, and Clinical Applications; Elsevier Health Sciences: Churchill Livingstone: London, UK, 2004. [Google Scholar]
- Bohannon, R.W.; Magasi, S.R.; Bubela, D.J.; Wang, Y.C.; Gershon, R.C. Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve 2012, 46, 555–558. [Google Scholar] [CrossRef]
- Kim, S.H.; Jo, M.-W.; Lee, S.-I. Psychometric properties of the Korean short form-36 health survey version 2 for assessing the general population. Asian Nurs. Res. 2013, 7, 61–66. [Google Scholar] [CrossRef]
- Cardiovascular, A.A.O.; Rehabilitation, P. Guidelines for Cardia Rehabilitation and Secondary Prevention Programs; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Kirkman, D.L.; Lee, D.-C.; Carbone, S. Resistance exercise for cardiac rehabilitation. Prog. Cardiovasc. Dis. 2022, 70, 66–72. [Google Scholar] [CrossRef]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2. [Google Scholar] [CrossRef]
- Stavrinou, P.S.; Bogdanis, G.C.; Giannaki, C.D.; Terzis, G.; Hadjicharalambous, M. High-intensity interval training frequency: Cardiometabolic effects and quality of life. Int. J. Sport. Med. 2018, 39, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Westcott, W.L.; Winett, R.A.; Annesi, J.J.; Wojcik, J.R.; Anderson, E.S.; Madden, P.J. Prescribing physical activity: Applying the ACSM protocols for exercise type, intensity, and duration across 3 training frequencies. Physician Sportsmed. 2009, 37, 51–58. [Google Scholar] [CrossRef]
- Rosa, C.; Vilaça-Alves, J.; Neves, E.B.; Saavedra, F.J.F.; Reckziegel, M.B.; Pohl, H.H.; Zanini, D. The effect of weekly low frequency exercise on body composition and blood pressure of elderly women. Arch. Med. Deporte 2017, 34, 9–14. [Google Scholar]
- Ferrari, R.; Fuchs, S.C.; Kruel, L.F.M.; Cadore, E.L.; Alberton, C.L.; Pinto, R.S.; Radaelli, R.; Schoenell, M.; Izquierdo, M.; Tanaka, H. Effects of different concurrent resistance and aerobic training frequencies on muscle power and muscle quality in trained elderly men: A randomized clinical trial. Aging Dis. 2016, 7, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Moriguchi, J.; Itoh, H.; Harada, S.; Takeda, K.; Hatta, T.; Nakata, T.; Sasaki, S. Low frequency regular exercise improves flow-mediated dilatation of subjects with mild hypertension. Hypertens. Res. 2005, 28, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Squires, R.W.; Kaminsky, L.A.; Porcari, J.P.; Ruff, J.E.; Savage, P.D.; Williams, M.A. Progression of exercise training in early outpatient cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 2018, 38, 139–146. [Google Scholar] [CrossRef]
- Safiyari-Hafizi, H.; Taunton, J.; Ignaszewski, A.; Warburton, D.E. The health benefits of a 12-week home-based interval training cardiac rehabilitation program in patients with heart failure. Can. J. Cardiol. 2016, 32, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Lehti, M.; Valkeinen, H.; Sipilä, S.; Perhonen, M.; Rottensteiner, M.; Pullinen, T.; Pietiläinen, R.; Nyman, K.; Vehkaoja, A.; Kainulainen, H. Effects of aerobic and strength training on aerobic capacity, muscle strength, and gene expression of lymphomonocytes in patients with stable CAD. Am. J. Transl. Res. 2020, 12, 4582–4593. [Google Scholar]
- Silva, M.R.; Alberton, C.L.; Portella, E.G.; Nunes, G.N.; Martin, D.G.; Pinto, S.S. Water-based aerobic and combined training in elderly women: Effects on functional capacity and quality of life. Exp. Gerontol. 2018, 106, 54–60. [Google Scholar] [CrossRef]
- Taylor, R.S.; Walker, S.; Smart, N.A.; Piepoli, M.F.; Warren, F.C.; Ciani, O.; Whellan, D.; O’Connor, C.; Keteyian, S.J.; Coats, A. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: Individual participant meta-analysis. J. Am. Coll. Cardiol. 2019, 73, 1430–1443. [Google Scholar] [CrossRef]
- Kim, S.G.; Choi, S.B.; Kim, Y.H. Effect of short-term cardiac rehabilitation on quality of life according to socioeconomic status. J. Men’s Health 2019, 15, 37–46. [Google Scholar]
- Tikkanen-Dolenc, H.; Wadén, J.; Forsblom, C.; Harjutsalo, V.; Thorn, L.M.; Saraheimo, M.; Elonen, N.; Rosengård-Bärlund, M.; Gordin, D.; Tikkanen, H.O. Frequent and intensive physical activity reduces risk of cardiovascular events in type 1 diabetes. Diabetologia 2017, 60, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Ignaszewski, M.; Lau, B.; Wong, S.; Isserow, S. The science of exercise prescription: Martti Karvonen and his contributions. Br. Columbia Med. J. 2017, 59, 38–41. [Google Scholar]
- Yang, W.-H.; Park, H.; Grau, M.; Heine, O. Decreased blood glucose and lactate: Is a useful indicator of recovery ability in athletes? Int. J. Environ. Res. Public Health 2020, 17, 5470. [Google Scholar] [CrossRef]
- Yang, W.-H.; Park, J.-H.; Shin, Y.-C.; Kim, J. Physiological profiling and energy system contributions during simulated epée matches in elite fencers. Int. J. Sport. Physiol. Perform. 2022, 17, 943–950. [Google Scholar] [CrossRef]
- Brooks, G.A. Role of the heart in lactate shuttling. Front. Nutr. 2021, 8, 132. [Google Scholar] [CrossRef]
- Lewsey, S.C.; Weiss, K.; Schär, M.; Zhang, Y.; Bottomley, P.A.; Samuel, T.J.; Xue, Q.-L.; Steinberg, A.; Walston, J.D.; Gerstenblith, G. Exercise intolerance and rapid skeletal muscle energetic decline in human age-associated frailty. JCI Insight 2020, 5, 20. [Google Scholar] [CrossRef]
- Xu, L.; Li, F.; Zhou, C.; Li, J.; Hong, C.; Tong, Q. The effect of mobile applications for improving adherence in cardiac rehabilitation: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2019, 19, 166. [Google Scholar] [CrossRef]
- Meinhart, F.; Stütz, T.; Sareban, M.; Kulnik, S.T.; Niebauer, J. Mobile technologies to promote physical activity during cardiac rehabilitation: A scoping review. Sensors 2020, 21, 65. [Google Scholar] [CrossRef] [PubMed]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Merz, C.N.B.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.; Maas, A.H. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Selleri, V.; Zanini, G.; Nasi, M.; Pinti, M.; Stefanelli, C.; Fedele, F.; Gallina, S. Physical activity and diet in older women: A narrative review. J. Clin. Med. 2022, 12, 81. [Google Scholar] [CrossRef] [PubMed]
- Grace, S.L.; Gravely-Witte, S.; Kayaniyil, S.; Brual, J.; Suskin, N.; Stewart, D.E. A multisite examination of sex differences in cardiac rehabilitation barriers by participation status. J. Women’s Health 2009, 18, 209–216. [Google Scholar] [CrossRef]
- Talaulikar, V. Menopause transition: Physiology and symptoms. Best Pract. Res. Clin. Obstet. Gynaecol. 2022, 81, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef] [PubMed]
- Micklesfield, L.K.; Munthali, R.J.; Prioreschi, A.; Said-Mohamed, R.; Van Heerden, A.; Tollman, S.; Kahn, K.; Dunger, D.; Norris, S.A. Understanding the relationship between socio-economic status, physical activity and sedentary behaviour, and adiposity in young adult South African women using structural equation modelling. Int. J. Environ. Res. Public Health 2017, 14, 1271. [Google Scholar] [CrossRef] [PubMed]
| Variables | LFT (n = 45) | HFT (n = 45) | t or χ-Value | Cohen’s d or Cramer’s v | p-Value |
|---|---|---|---|---|---|
| Age, years | 51.7 ± 6.3 | 50.6 ± 5.7 | 0.115 | 0.199 | 0.788 |
| Height, cm | 162.7 ± 3.4 | 163.2 ± 4.6 | 1.096 | 0.123 | 0.275 |
| Weight, kg | 60.3 ± 7.7 | 61.6 ± 6.9 | 0.356 | 0.177 | 0.723 |
| BMI, kg/ m2 | 22.8 ± 2.9 | 23.1 ± 2.3 | −0.363 | 0.114 | 0.718 |
| Vessels, n (%) | |||||
| One | 28 (62.2) | 31 (68.9) | 0.730 | 0.084 | 0.730 |
| Two | 15 (33.3) | 13 (28.9) | |||
| Three | 2 (4.5) | 1 (2.2) | |||
| Recurrence, n (%) | |||||
| Yes | 3 (6.7) | 2 (4.4) | 0.645 | 0.049 | 0.639 |
| No | 42 (93.3) | 43 (95.6) | |||
| Education, n (%) | |||||
| Middle | 5 (11.1) | 3 (6.7) | 0.720 | 0.089 | 0.698 |
| High | 18 (40.0) | 17 (37.8) | |||
| College | 22 (48.9) | 25 (55.5) | |||
| Income, per year, USD, n (%) | |||||
| <5000 | 24 (53.3) | 13 (28.9) | 11.299 | 0.354 | 0.004 |
| 5000–10,000 | 18 (40.0) | 17 (37.8) | |||
| >10,000 | 3 (6.7) | 15 (33.3) | |||
| Diagnosis | |||||
| Unstable angina | 39 (86.7) | 35 (77.8) | 1.216 | 0.116 | 0.409 |
| Myocardial infarction | 6 (13.3) | 10 (22.2) | |||
| Training frequency, days/week | 4.6 ± 0.3 | 4.3 ± 0.6 | 0.258 | 0.632 | <0.001 |
| Training intensity, RPE scale | 12.5 ± 1.1 | 13.1 ± 0.8 | 1.105 | 0.623 | 0.105 |
| Medication information | |||||
| β-blocker or calcium-channel blocker | 38 (84.4) | 35 (77.8) | 1.111 | 0.111 | 0.430 |
| Antilipemic medication | 33 (73.3) | 36 (80.0) | 0.241 | 0.052 | 0.807 |
| Hypoglycemic medication | 7 (15.6) | 10 (22.2) | 0.653 | 0.085 | 0.591 |
| Variables | Group | Baseline | 12-wks | Df, % | p-Value | Cohen’s d | T × G Partial η2 | T × G p-Value |
|---|---|---|---|---|---|---|---|---|
| SBP, mmHg | LFT | 128.0 ± 17.2 | 122.2 ± 16.6 | −4.5 | 0.041 | 0.343 | 0.029 | 0.014 |
| HFT | 129.2 ± 15.3 | 118.8 ± 14.8 | −8.0 | 0.017 | 0.690 | |||
| DBP, mmHg | LFT | 76.0 ± 11.1 | 74.8 ± 10.3 | −1.6 | 0.612 | 0.112 | - | 0.518 |
| HFT | 75.2 ± 9.4 | 74.5 ± 12.2 | −0.9 | 0.404 | 0.040 | |||
| Weight, kg | LFT | 60.3 ± 7.7 | 59.9 ± 6.4 | −0.7 | 0.550 | 0.056 | 0.031 | 0.005 |
| HFT | 61.6 ± 6.9 | 58.3 ± 5.8 | −5.4 | 0.011 | 0.517 | |||
| BMI, kg/m2 | LFT | 22.8 ± 2.9 | 22.6 ± 2.1 | −0.5 | 0.178 | 0.078 | 0.025 | 0.009 |
| HFT | 23.1 ± 2.3 | 21.9 ± 2.0 | −5.2 | 0.015 | 0.556 | |||
| Waist circumference, cm | LFT | 94.7 ± 6.3 | 92.4 ± 5.8 | −2.4 | 0.302 | 0.091 | 0.037 | 0.035 |
| HFT | 95.3 ± 6.8 | 91.5 ± 6.6 | −4.0 | 0.041 | 0.588 | |||
| Body fat, % | LFT | 27.1 ± 5.4 | 24.2 ± 4.2 | −10.7 | 0.133 | 0.599 | 0.015 | 0.020 |
| HFT | 27.9 ± 5.1 | 23.7 ± 4.6 | −15.1 | 0.011 | 0.864 | |||
| Skeletal muscle mass, % | LFT | 26.1 ± 2.4 | 26.7 ± 2.6 | 2.3 | 0.314 | 0.239 | - | 0.608 |
| HFT | 26.5 ± 2.3 | 27.0 ± 3.1 | 1.9 | 0.263 | 0.183 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, P.; Zhang, W.; Kim, Y.; Meng, H. Effects of Low- and High-Frequency Cardiac Rehabilitation on Risk Factors, Physical Fitness and Quality of Life in Middle-Aged Women with Coronary Heart Disease. Metabolites 2023, 13, 550. https://doi.org/10.3390/metabo13040550
Zhou P, Zhang W, Kim Y, Meng H. Effects of Low- and High-Frequency Cardiac Rehabilitation on Risk Factors, Physical Fitness and Quality of Life in Middle-Aged Women with Coronary Heart Disease. Metabolites. 2023; 13(4):550. https://doi.org/10.3390/metabo13040550
Chicago/Turabian StyleZhou, Peng, Wangyang Zhang, Yonghwan Kim, and Huan Meng. 2023. "Effects of Low- and High-Frequency Cardiac Rehabilitation on Risk Factors, Physical Fitness and Quality of Life in Middle-Aged Women with Coronary Heart Disease" Metabolites 13, no. 4: 550. https://doi.org/10.3390/metabo13040550
APA StyleZhou, P., Zhang, W., Kim, Y., & Meng, H. (2023). Effects of Low- and High-Frequency Cardiac Rehabilitation on Risk Factors, Physical Fitness and Quality of Life in Middle-Aged Women with Coronary Heart Disease. Metabolites, 13(4), 550. https://doi.org/10.3390/metabo13040550







