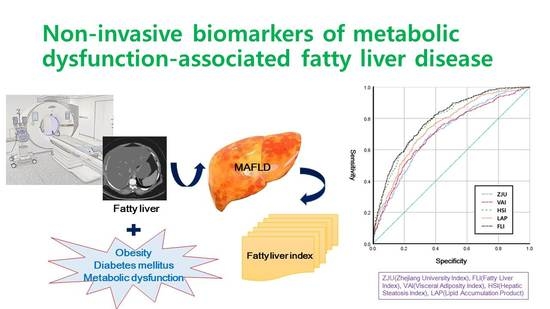
Comparison of the Diagnostic Performance of Steatosis Indices for Discrimination of CT-Diagnosed Metabolic Dysfunction-Associated Fatty Liver Disease
Abstract
:1. Introduction
2. Results
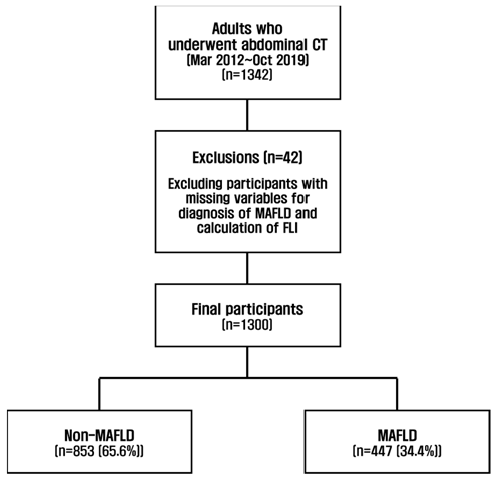
2.1. Participants
2.2. AUROC Analysis for MAFLD
2.3. Diagnostic Accuracy for MAFLD by Sex
2.4. Diagnostic Accuracy for MAFLD by Age
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Diagnosis of MAFLD
4.3. Diagnosis of Fatty Liver
4.4. Anthropometric and Biochemical Measurements
4.5. Calculations of Steatosis Indices: Formulae
4.6. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.; Park, H.S.; Kim, Y.J.; Yu, M.H.; Park, S.; Jung, S.I. Association of hepatic steatosis index with nonalcoholic fatty liver disease diagnosed by non-enhanced CT in a screening population. Diagnostics 2021, 11, 2168. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Scorletti, E.; Mosca, A.; Alisi, A.; Byrne, C.D.; Targher, G. Complications, morbidity and mortality of nonalcoholic fatty liver disease. Metabolism 2020, 111, 154170. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Henry, L. Epidemiology of non-alcoholic fatty liver disease and hepatocellular carcinoma. JHEP Rep. 2021, 3, 100305. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [Green Version]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.; Dufour, J.F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef]
- Wang, J.; Xu, C.; Xun, Y.; Lu, Z.; Shi, J.; Yu, C.; Li, Y. ZJU index: A novel model for predicting nonalcoholic fatty liver disease in a Chinese population. Sci. Rep. 2015, 5, 16494. [Google Scholar] [CrossRef] [Green Version]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A.; AlkaMeSy Study Group. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Kim, D.; Kim, H.J.; Lee, C.H.; Yang, J.I.; Kim, W.; Kim, Y.J.; Yoon, J.H.; Cho, S.H.; Sung, M.W.; et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver. Dis. 2010, 42, 503–508. [Google Scholar] [CrossRef]
- Kahn, H.S. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 2005, 5, 26. [Google Scholar] [CrossRef] [Green Version]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The fatty liver index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castellana, M.; Donhia, R.; Guerra, V.; Procino, F.; Lampignano, L.; Castellana, F.; Zupo, R.; Sardone, R.; De Pergola, G.; Romanelli, F.; et al. Performance of fatty liver index in identifying non-alcoholic fatty liver disease in population studies. A meta-analysis. J. Clin. Med. 2021, 10, 1877. [Google Scholar] [CrossRef] [PubMed]
- Sumida, Y.; Nakajima, A.; Itoh, Y. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J. Gastroenterol. 2014, 20, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.; Castera, L. Non-invasive diagnosis of hepatic steatosis. Hepatol. Int. 2017, 11, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Dhyani, M.; Grajo, J.R.; Sirlin, C.; Samir, A.E. Current status of imaging in nonalcoholic fatty liver disease. World J. Hepatol. 2018, 10, 530–542. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, S.; Huang, J.; Zhu, Y.; Lin, S. Validation of five hepatic steatosis algorithms in metabolic-associated fatty liver disease: A population based study. J. Gastroenterol. Hepatol. 2022, 37, 938–945. [Google Scholar] [CrossRef]
- Xu, Z.; Li, H.; Tian, S.; Wu, J.; Li, X.; Liu, Z.L.; Li, S.; Chen, Y.L.; Xiao, J.; Wei, J.Y.; et al. Blood biomarkers for the diagnosis of hepatic steatosis in metabolic dysfunction-associated fatty liver disease. J. Hepatol. 2020, 73, 1264–1265. [Google Scholar] [CrossRef]
- Lonardo, A.; Ballestri, S.; Bedogni, G.; Bellentani, S.; Tiribelli, C. The fatty liver index (FLI) 15 years later: A reappraisal. MTOD 2021, 1, 10. [Google Scholar] [CrossRef]
- Park, S.W.; Han, A.L. Validation of fatty liver index as a marker for non-alcoholic fatty liver disease. Korean J. Health. Promot. 2021, 21, 56–62. [Google Scholar] [CrossRef]
- Yamamura, S.; Eslam, M.; Kawaguchi, T.; Tsutsumi, T.; Nakano, D.; Yoshinaga, S.; Takahashi, H.; Anzai, K.; George, J.; Torimura, T. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020, 40, 3018–3030. [Google Scholar] [CrossRef]
- Shao, C.; Ye, J.; Li, X.; Lin, Y.; Feng, S.; Liao, B.; Zhong, B. Discrepancies between nonalcoholic and metabolic-associated fatty liver disease by multiple steatosis assessment. J. Clin. Transl. Hepatol. 2022. [Google Scholar] [CrossRef]
- Goulart, A.C.; Oliveira, I.R.; Alencar, A.P.; Santos, M.S.; Santos, I.S.; Martines, B.M.; Meireles, D.P.; Martines, J.A.; Misciagna, G.; Benseñor, I.M.; et al. Diagnostic accuracy of a noninvasive hepatic ultrasound score for non-alcoholic fatty liver disease (NAFLD) in the Brazilian longitudinal study of adult health (ELSA-Brasil). Sao Paulo Med. J. 2015, 133, 115–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, C.P.; Ali, H.; Rachakonda, V.P.; Oczypok, E.A.; DeLany, J.P.; Kershaw, E.E. The ZJU index is a powerful surrogate marker for NAFLD in severely obese North American women. PLoS ONE 2019, 14, e0224942. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; You, W.; Ren, W. The ZJU index is a powerful index for identifying NAFLD in the general Chinese population. Acta Diabetol. 2017, 54, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; He, M.; Zhang, Y.; Li, T.; Liu, Y.; Xu, Z.; Chen, W. Validation of simple indexes for nonalcoholic fatty liver Disease in Western China: A retrospective cross-sectional study. Endocr. J. 2018, 65, 373–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Wang, M.; Wang, M.; Zhang, R.; Wang, H.; Zhang, W.; Wang, J. External validation and comparison of simple tools to screen for nonalcoholic fatty liver disease in Chinese Community population. Researchsquare 2020, 34, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Murayama, K.; Okada, M.; Tanaka, K.; Inadomi, C.; Yoshioka, W.; Kubotsu, Y.; Yada, T.; Isoda, H.; Kuwashiro, T.; Oeda, S.; et al. Prediction of nonalcoholic fatty liver disease using noninvasive and non-imaging procedures in Japanese Health checkup examinees. Diagnostics 2021, 11, 132. [Google Scholar] [CrossRef] [PubMed]
- Foschi, F.G.; Conti, F.; Domenicali, M.; Giacomoni, P.; Borghi, A.; Bevilacqua, V.; Napoli, L.; Berardinelli, D.; Altini, M.; Cucchetti, A.; et al. External validation of surrogate indices of fatty liver in the general population: The Bagnacavallo Study. J. Clin. Med. 2021, 10, 520. [Google Scholar] [CrossRef]
- Cho, E.J.; Jung, G.C.; Kwak, M.S.; Yang, J.I.; Yim, J.Y.; Yu, S.J.; Chung, G.E. Fatty liver index for predicting nonalcoholic fatty liver disease in an asymptomatic Korean population. Diagnostics 2021, 11, 2233. [Google Scholar] [CrossRef]
- Delli Bovi, A.P.; Marciano, F.; Mandato, C.; Siano, M.A.; Savoia, M.; Vajro, P. Oxidative stress in non-alcoholic fatty liver disease. An updated mini review. Front. Med. 2021, 8, 595371. [Google Scholar] [CrossRef]
- Fujii, H.; Nakamura, N.; Fukumoto, S.; Kimura, T.; Nakano, A.; Nadatani, Y.; Kawada, N. Lifestyle changes during the coronavirus Disease 2019 pandemic impact metabolic dysfunction–associated fatty liver disease. Liver Int. 2022, 42, 995–1004. [Google Scholar] [CrossRef] [PubMed]

| Biochemical Markers | Other Variables | |
|---|---|---|
| Zhejiang University index (ZJU) | FPG, TG, ALT/AST ratio | BMI |
| Visceral adiposity index (VAI) | TG, HDL-C | BMI, WC |
| Hepatic steatosis index (HSI) | ALT/AST ratio | BMI |
| Lipid accumulation product (LAP) | TG | WC |
| Fatty liver index (FLI) | TG, GGT | BMI, WC |
| Total Participants (n = 1300) | MAFLD | p-Value | ||
|---|---|---|---|---|
| No (n = 853) | Yes (n = 447) | |||
| Sex | Male | 437 (51.2) | 337 (75.4) | <0.0001 |
| Female | 416 (48.8) | 110 (24.6) | ||
| Age (years) | 52 ± 11 | 52.1 ± 9.7 | 0.0429 | |
| BMI (kg/m2) | 23.5 ± 2.8 | 26.6 ± 3.2 | <0.0001 | |
| SBP (mmHg) | 122 ± 13 | 127 ± 12 | <0.0001 | |
| DBP (mmHg) | 75.5 ± 9.6 | 79.9 ± 9.8 | <0.0001 | |
| FPG (mg/dL) | 98 ± 48 | 106 ± 30 | 0.004 | |
| AST (IU/L) | 30 ± 19 | 38 ± 40 | <0.0001 | |
| ALT (IU/L) | 25 ± 21 | 41 ± 46 | <0.0001 | |
| GGT (IU/L) | 37 ± 66 | 67 ± 176 | 0.001 | |
| TC (mg/dL) | 202 ± 76 | 204 ± 44 | 0.668 | |
| TG (mg/dL) | 99 ± 65 | 155 ± 143 | <0.0001 | |
| HDL-C (mg/dL) | 57 ± 13 | 51 ± 13 | <0.0001 | |
| LDL-C (mg/dL) | 121 ± 60 | 123 ± 37 | 0.517 | |
| Creatinine (mg/dL) | 0.79 ± 0.20 | 0.85 ± 0.17 | <0.0001 | |
| Uric Acid (mg/dL) | 5.0 ± 1.4 | 5.8 ± 1.4 | <0.0001 | |
| ZJU | 224 ± 86 | 291 ± 150 | <0.0001 | |
| VAI | 138 ± 122 | 251 ± 302 | <0.0001 | |
| HSI | 31.4 ± 4.0 | 36.0 ± 4.8 | <0.0001 | |
| LAP | 2049 ± 1883 | 4352 ± 6312 | <0.0001 | |
| FLI | 23 ± 21 | 49 ± 26 | <0.0001 | |
| AUROC (95% CI) | p-Value | Sensitivity (%) | Specificity (%) | Cut-Off Value | |
|---|---|---|---|---|---|
| ZJU | 0.704 (0.675–0.734) | <0.0001 | 66.4 | 66.5 | 231.1261 |
| VAI | 0.705 (0.675–0.735) | <0.0001 | 66.0 | 65.8 | 142.9275 |
| HSI | 0.784 (0.758–0.809) | <0.0001 | 71.5 | 70.9 | 33.2182 |
| LAP | 0.747 (0.720–0.775) | <0.0001 | 68.9 | 68.2 | 2278.3 |
| FLI | 0.791 (0.766–0.816) | - | 70.9 | 70.9 | 29.9358 |
| AUROC (95% CI) for Men | p-Value | AUROC (95% CI) for Women | p-Value | |
|---|---|---|---|---|
| ZJU | 0.689 (0.652–0.726) | <0.0001 | 0.656 (0.597–0.715) | <0.0001 |
| VAI | 0.712 (0.675–0.748) | <0.0001 | 0.671 (0.611–0.731) | <0.0001 |
| HSI | 0.773 (0.740–0.806) | <0.0001 | 0.793 (0.749–0.838) | <0.0001 |
| LAP | 0.745 (0.711–0.780) | <0.0001 | 0.716 (0.664–0.769) | <0.0001 |
| FLI | 0.765 (0.732–0.798) | - | 0.762 (0.715–0.810) | - |
| AUROC for ≤40 Years (95% CI) | AUROC for 41–50 Years (95% CI) | AUROC for 51–60 Years (95% CI) | AUROC for >60 Years (95% CI) | |
|---|---|---|---|---|
| ZJU | 0.759 (0.684–0.834) | 0.763 (0.712–0.814) | 0.665 (0.617–0.713) | 0.651 (0.578–0.724) |
| VAI | 0.765 (0.683–0.847) | 0.784 (0.734–0.834) | 0.658 (0.609–0.707) | 0.628 (0.553–0.704) |
| HSI | 0.862 (0.811–0.913) | 0.814 (0.769–0.859) | 0.745 (0.702–0.789) | 0.748 (0.681–0.816) |
| LAP | 0.783 (0.711–0.856) | 0.822 (0.778–0.865) | 0.711 (0.666–0.756) | 0.667 (0.595–0.739) |
| FLI | 0.838 (0.778–0.899) | 0.849 (0.808–0.889) | 0.759 (0.717–0.801) | 0.713 (0.646–0.781) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, A.L.; Lee, H.K. Comparison of the Diagnostic Performance of Steatosis Indices for Discrimination of CT-Diagnosed Metabolic Dysfunction-Associated Fatty Liver Disease. Metabolites 2022, 12, 664. https://doi.org/10.3390/metabo12070664
Han AL, Lee HK. Comparison of the Diagnostic Performance of Steatosis Indices for Discrimination of CT-Diagnosed Metabolic Dysfunction-Associated Fatty Liver Disease. Metabolites. 2022; 12(7):664. https://doi.org/10.3390/metabo12070664
Chicago/Turabian StyleHan, A. Lum, and Hee Kyung Lee. 2022. "Comparison of the Diagnostic Performance of Steatosis Indices for Discrimination of CT-Diagnosed Metabolic Dysfunction-Associated Fatty Liver Disease" Metabolites 12, no. 7: 664. https://doi.org/10.3390/metabo12070664
APA StyleHan, A. L., & Lee, H. K. (2022). Comparison of the Diagnostic Performance of Steatosis Indices for Discrimination of CT-Diagnosed Metabolic Dysfunction-Associated Fatty Liver Disease. Metabolites, 12(7), 664. https://doi.org/10.3390/metabo12070664