Sex-Specific Relationship between the Cardiorespiratory Fitness and Plasma Metabolite Patterns in Healthy Humans—Results of the KarMeN Study
Abstract
:1. Introduction
2. Results
2.1. Metabolomics Data
2.2. Basic Characteristics of Study Participants
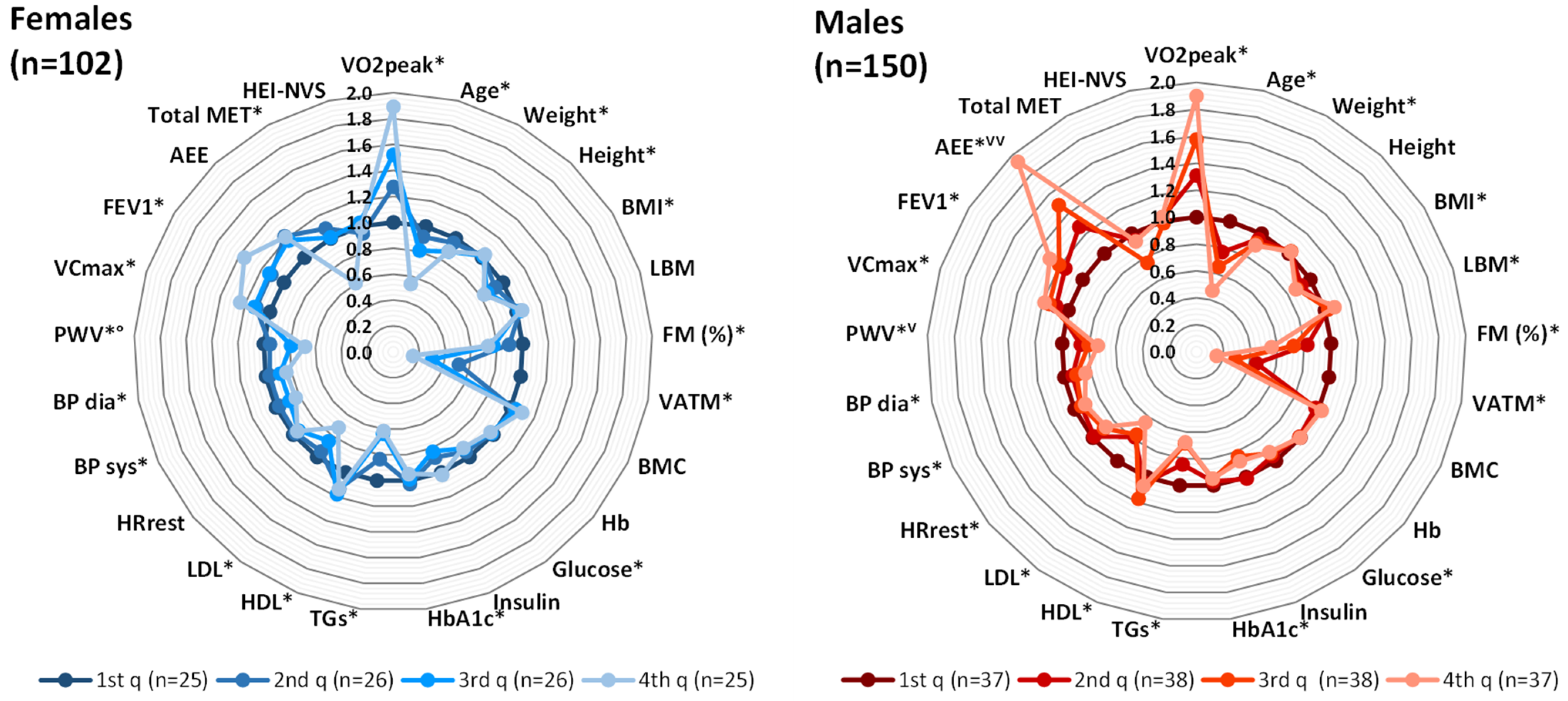
2.3. Sex-Specific Relationship between CRF and Phenotypical/Clinical Variables
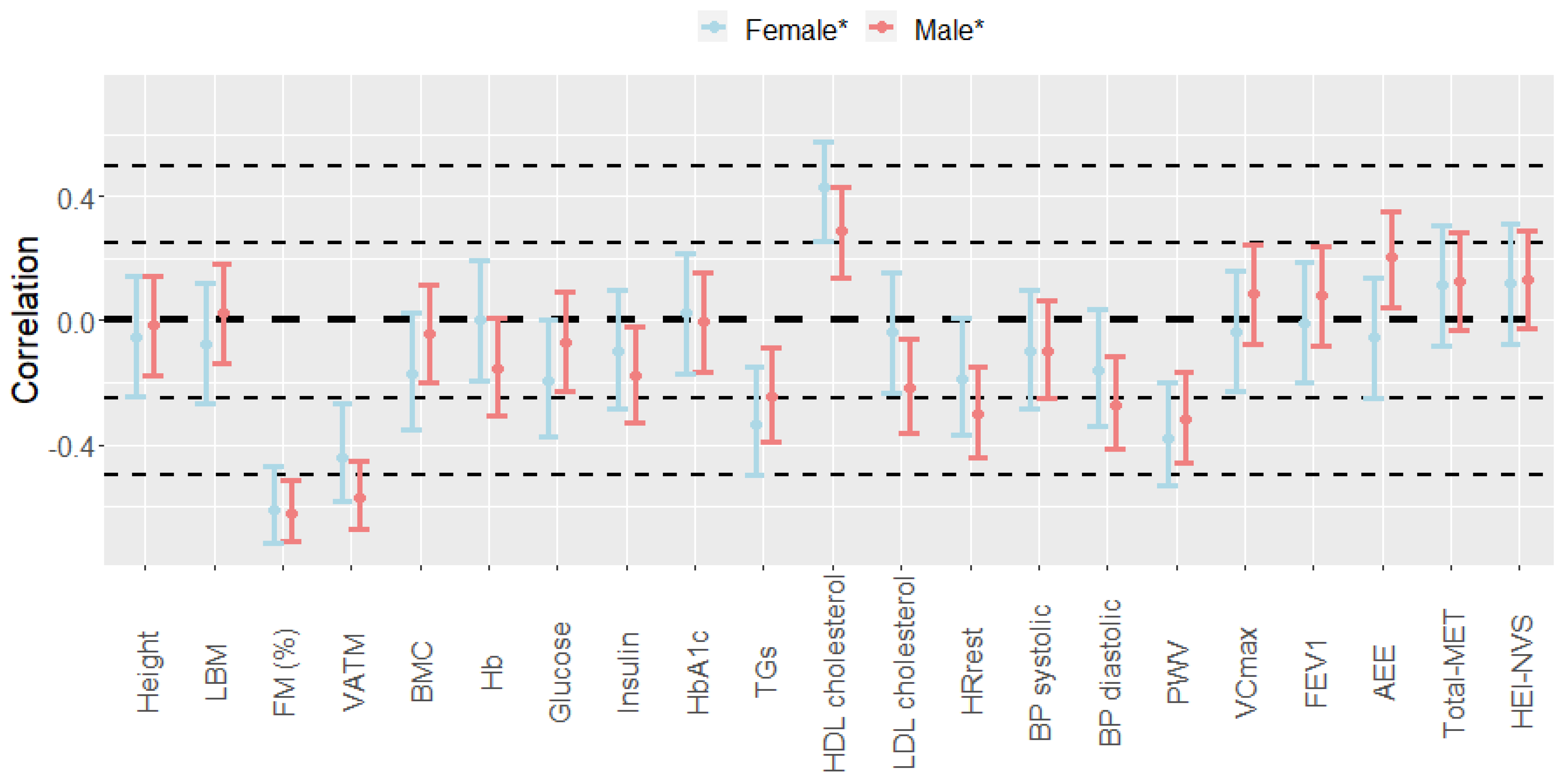
2.4. Sex-Specific Relationship between CRF and Plasma Metabolites
2.4.1. Bivariate Association Analyses
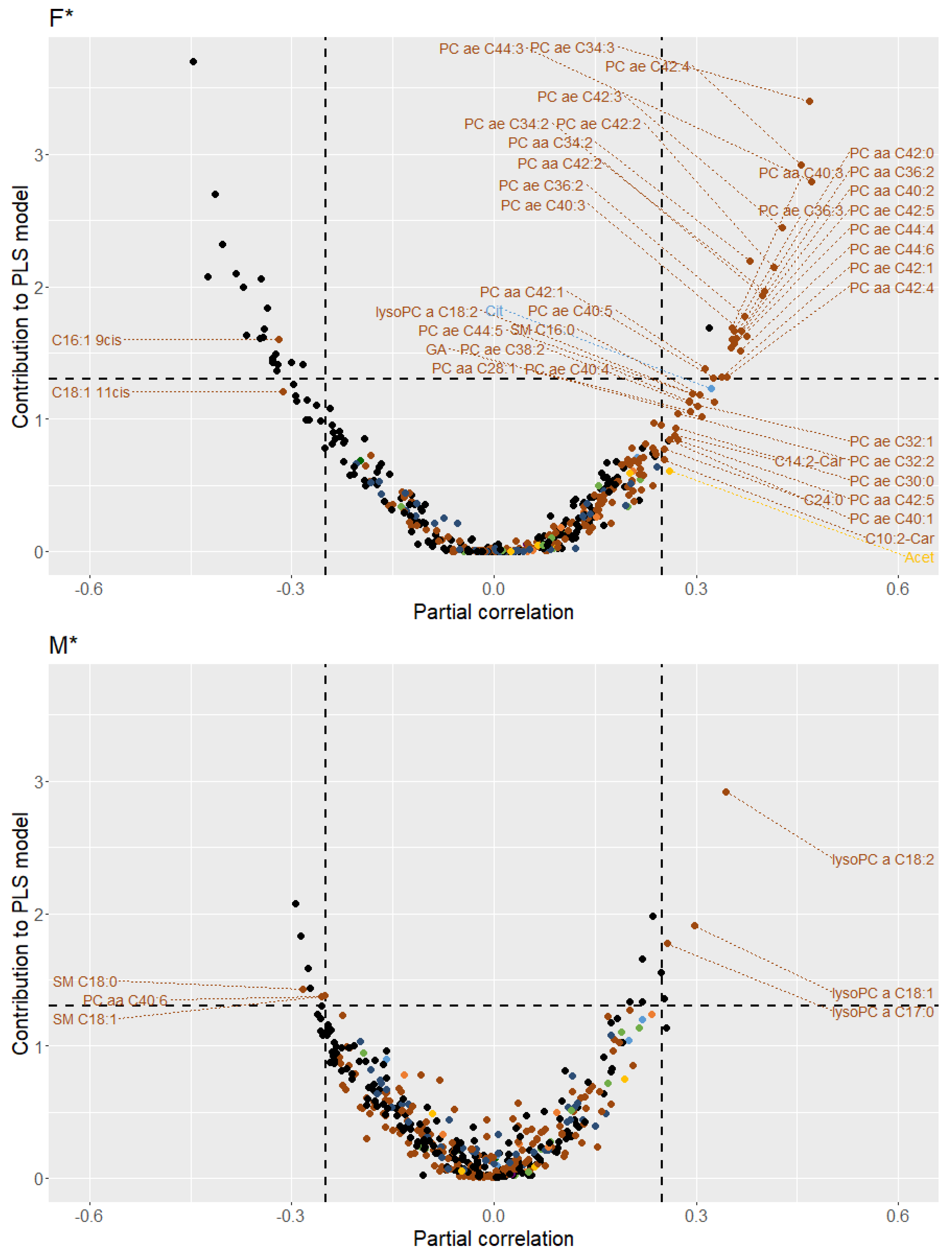
2.4.2. Multivariate Association Analyses
2.4.3. Multiple Regression Analyses
3. Discussion
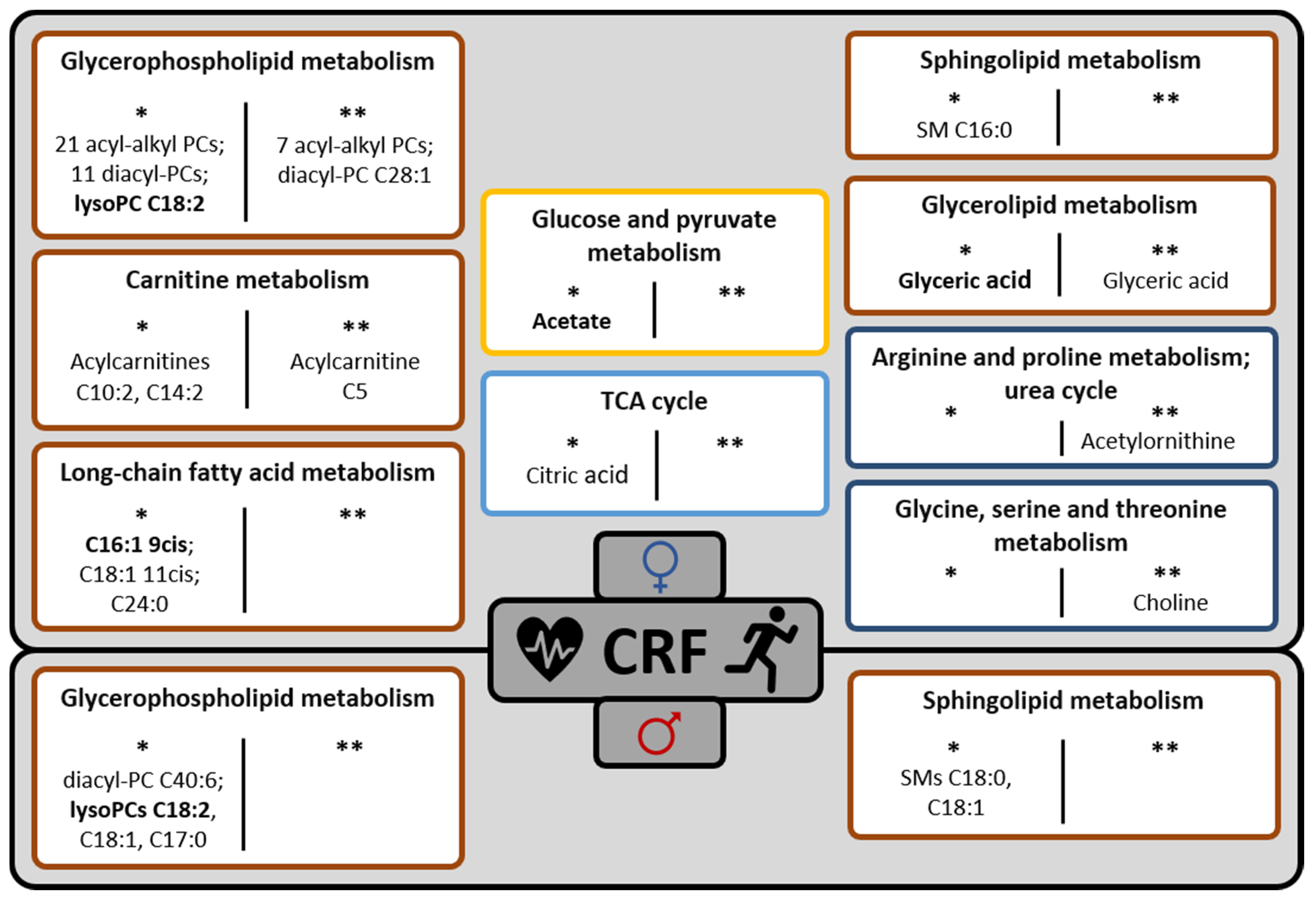
3.1. Sex-Specific Plasma Metabolite Patterns Related to CRF
3.1.1. Age- and Menopausal Status-Adjusted Findings
3.1.2. Age-, Menopausal Status- and Phenotypical/Clinical Variables-Adjusted Findings
3.2. Sex-Specific CRF Explanation Models
3.3. Strengths and Limitations
4. Materials and Methods
4.1. Subjects and Study Design
4.2. Anthropometry and Body Composition Assessment
4.3. PF and PA Assessment
4.4. Dietary Assessment
4.5. Clinical Examinations
4.6. Metabolomics Analyses
4.7. Data Handling and Statistical Analysis
- (i)
- Bivariate association analyses
- (ii)
- Multivariate association analyses
- (iii)
- Multiple linear regression analyses
- Approach 1: Only phenotypical/clinical variables (n = 21) were stepwise selected.
- Approach 2: All Phenotypical/clinical variables (n = 21) were included and only plasma metabolite variables (n = 427) were stepwise selected.
- Approach 3: Phenotypical/clinical variables (n = 21) as well as plasma metabolite variables (n = 427) were stepwise selected.
4.8. Metabolite Classification
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | amino acid |
| AEE | activity energy expenditure |
| BP | blood pressure |
| BMC | bone mineral content |
| BMI | body mass index |
| CIs | confidence intervals |
| CRF | cardiorespiratory fitness |
| FEV1 | forced expiratory pressure in one second |
| FM | fat mass |
| GC | gas chromatography |
| GC × GC | two-dimensional gas chromatography |
| Hb | hemoglobin |
| HDL | high-density lipoprotein |
| HEI-NVS | Healthy Eating Index (modified version) |
| HRrest | resting heart rate |
| KarMeN | Karlsruhe Metabolomics and Nutrition |
| LBM | lean body mass |
| LC | liquid chromatography |
| LCFA | long-chain fatty acid |
| LDL | low-density lipoprotein |
| LysoPC | lyso-phosphatidylcholine |
| MET | metabolic equivalent of task |
| MS | mass spectrometry |
| NMR | nuclear magnetic resonance |
| PA | physical activity |
| PC | phosphatidylcholine |
| PC aa | diacyl-phosphatidylcholine |
| PC ae | acyl-alkyl-phosphatidylcholine |
| PE | physical exercise |
| PF | physical fitness |
| PLS | partial least squares |
| PWV | pulse wave velocity |
| q | quarter |
| QC | quality control |
| r | Pearson correlation coefficient |
| R2 | coefficient of determination |
| R2 (adjusted) | adjusted coefficient of determination |
| RMSE | root mean square error |
| SM | sphingomyelin |
| TCA | tricarboxylic acid |
| TGs | triglycerides |
| U | unknown |
| VATM | visceral adipose tissue mass |
| VCmax | maximal vital capacity |
| VdW | Van der Waerden |
| VO2max | maximal oxygen uptake |
| VO2peak | peak oxygen uptake |
References
- Bouchard, C.; Blair, S.N.; Haskell, W.L. Physical Activity and Health; Human Kinetics: Champaign, IL, USA, 2007. [Google Scholar]
- Hill, A.V.; Long, C.; Lupton, H. Muscular exercise, lactic acid and the supply and utilisation of oxygen—Parts VII–VIII. Proc. R. Soc. Lond. Ser. B Contain. Pap. Biol. Character 1924, 97, 155–176. [Google Scholar] [CrossRef]
- Al-Mallah, M.H.; Juraschek, S.; Whelton, S.; Dardari, Z.; Ehrman, J.K.; Michos, E.; Blumenthal, R.S.; Nasir, K.; Qureshi, W.T.; Brawner, C.A.; et al. Sex Differences in Cardiorespiratory Fitness and All-Cause Mortality. Mayo Clin. Proc. 2016, 91, 755–762. [Google Scholar] [CrossRef] [Green Version]
- Laukkanen, J.; Laaksonen, D.; Lakka, T.; Savonen, K.; Rauramaa, R.; Mäkikallio, T.; Kurl, S. Determinants of Cardiorespiratory Fitness in Men Aged 42 to 60 Years With and Without Cardiovascular Disease. Am. J. Cardiol. 2009, 103, 1598–1604. [Google Scholar] [CrossRef] [PubMed]
- Zeiher, J.; Ombrellaro, K.J.; Perumal, N.; Keil, T.; Mensink, G.B.; Finger, J.D. Correlates and Determinants of Cardiorespiratory Fitness in Adults: A Systematic Review. Sports Med. Open 2019, 5, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, S.Y.S.; Chan, F.W.K.; Lee, C.K.; Li, M.; Yeung, F.; Lum, C.C.M.; Woo, J.; Choy, D.T. Maximum oxygen uptake and body composition of healthy Hong Kong Chinese adult men and women aged 20–64 years. J. Sports Sci. 2008, 26, 295–302. [Google Scholar] [CrossRef]
- Bouchard, C.; Boulay, M.R.; Simoneau, J.-A.; Lortie, G.; Pérusse, L. Heredity and Trainability of Aerobic and Anaerobic Performances an Update. Sports Med. 1988, 5, 69–73. [Google Scholar] [CrossRef] [PubMed]
- McKinney, J.; Lithwick, D.J.; Morrison, B.N.; Nazzari, H.; Isserow, S.H.; Heilbron, B.; Krahn, A.D. The health benefits of physical activity and cardiorespiratory fitness. Br. Columbia Med. J. 2016, 58, 131–137. [Google Scholar]
- Harber, M.P.; Kaminsky, L.A.; Arena, R.; Blair, S.N.; Franklin, B.A.; Myers, J.; Ross, R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017, 60, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Egan, B.; Zierath, J. Exercise Metabolism and the Molecular Regulation of Skeletal Muscle Adaptation. Cell Metab. 2013, 17, 162–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zierath, J.R.; Wallberg-Henriksson, H. Looking Ahead Perspective: Where Will the Future of Exercise Biology Take Us? Cell Metab. 2015, 22, 25–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heaney, L.M.; Deighton, K.; Suzuki, T. Non-targeted metabolomics in sport and exercise science. J. Sports Sci. 2017, 37, 959–967. [Google Scholar] [CrossRef]
- Bujak, R.; Struck-Lewicka, W.; Markuszewski, M.J.; Kaliszan, R. Metabolomics for laboratory diagnostics. J. Pharm. Biomed. Anal. 2015, 113, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Kujala, U.M.; Makinen, V.P.; Heinonen, I.; Soininen, P.; Kangas, A.J.; Leskinen, T.H.; Rahkila, P.; Wurtz, P.; Kovanen, V.; Cheng, S.; et al. Long-term leisure-time physical activity and serum metabolome. Circulation 2013, 127, 340–348. [Google Scholar] [CrossRef] [Green Version]
- Morris, C.; Grada, C.O.; Ryan, M.; Roche, H.M.; De Vito, G.; Gibney, M.J.; Gibney, E.R.; Brennan, L. The relationship between aerobic fitness level and metabolic profiles in healthy adults. Mol. Nutr. Food Res. 2013, 57, 1246–1254. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Moore, S.C.; Keadle, S.K.; Xiang, Y.-B.; Zheng, W.; Peters, T.M.; Leitzmann, M.F.; Ji, B.-T.; Sampson, J.N.; Shu, X.-O. Objectively measured physical activity and plasma metabolomics in the Shanghai Physical Activity Study. Int. J. Epidemiol. 2016, 45, 1433–1444. [Google Scholar] [CrossRef] [PubMed]
- Kujala, U.M.; Vaara, J.P.; Kainulainen, H.; Vasankari, T.; Vaara, E.; Kyröläinen, H. Associations of aerobic fitness and maximal muscular strength with metabolites in young men. JAMA Netw. Open 2019, 2, e198265. [Google Scholar] [CrossRef]
- Bye, A.; Vettukattil, R.; Aspenes, S.T.; Giskeodegard, G.F.; Gribbestad, I.S.; Wisloff, U.; Bathen, T.F. Serum levels of choline-containing compounds are associated with aerobic fitness level: The HUNT-study. PLoS ONE 2012, 7, e42330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Floegel, A.; Wientzek, A.; Bachlechner, U.; Jacobs, S.; Drogan, D.; Prehn, C.; Adamski, J.; Krumsiek, J.; Schulze, M.B.; Pischon, T.; et al. Linking diet, physical activity, cardiorespiratory fitness and obesity to serum metabolite networks: Findings from a population-based study. Int. J. Obes. 2014, 38, 1388–1396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wientzek, A.; Floegel, A.; Knuppel, S.; Vigl, M.; Drogan, D.; Adamski, J.; Pischon, T.; Boeing, H. Serum metabolites related to cardiorespiratory fitness, physical activity energy expenditure, sedentary time and vigorous activity. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.; O’Grada, C.M.; Ryan, M.F.; Gibney, M.J.; Roche, H.M.; Gibney, E.R.; Brennan, L. Modulation of the lipidomic profile due to a lipid challenge and fitness level: A postprandial study. Lipids Health Dis. 2015, 14, 65. [Google Scholar] [CrossRef] [Green Version]
- Lustgarten, M.S.; Price, L.L.; Logvinenko, T.; Hatzis, C.; Padukone, N.; Reo, N.V.; Phillips, E.M.; Kirn, D.; Mills, J.; Fielding, R.A. Identification of serum analytes and metabolites associated with aerobic capacity. Eur. J. Appl. Physiol. 2013, 113, 1311–1320. [Google Scholar] [CrossRef]
- Koh, A.S.; Gao, F.; Tan, R.S.; Zhong, L.; Leng, S.; Zhao, X.; Fridianto, K.T.; Ching, J.; Lee, S.Y.; Keng, B.M.H.; et al. Metabolomic correlates of aerobic capacity among elderly adults. Clin. Cardiol. 2018, 41, 1300–1307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chorell, E.; Svensson, M.B.; Moritz, T.; Antti, H. Physical fitness level is reflected by alterations in the human plasma metabolome. Mol. BioSyst. 2012, 8, 1187–1196. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.S.; Kelly, M.P.; Kelly, P. Metabolomics, physical activity, exercise and health: A review of the current evidence. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2020, 1866, 165936. [Google Scholar] [CrossRef]
- Bub, A.; Kriebel, A.; Dörr, C.; Bandt, S.; Rist, M.; Roth, A.; Hummel, E.; Kulling, S.; Hoffmann, I.; Watzl, B. The Karlsruhe Metabolomics and Nutrition (KarMeN) Study: Protocol and Methods of a Cross-Sectional Study to Characterize the Metabolome of Healthy Men and Women. JMIR Res. Protoc. 2016, 5, e146. [Google Scholar] [CrossRef]
- Mercuro, G.; Saiu, F.; Deidda, M.; Mercuro, S.; Vitale, C.; Rosano, G.M. Impairment of physical exercise capacity in healthy postmenopausal women. Am. Heart J. 2006, 151, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Rist, M.J.; Roth, A.; Frommherz, L.; Weinert, C.H.; Krüger, R.; Merz, B.; Bunzel, D.; Mack, C.; Egert, B.; Bub, A.; et al. Metabolite patterns predicting sex and age in participants of the Karlsruhe Metabolomics and Nutrition (KarMeN) study. PLoS ONE 2017, 12, e0183228. [Google Scholar] [CrossRef]
- Tobita, Y.; Kusaka, Y.; Ohtaki, H.; Hashizume, K. Factors affecting the estimated maximal oxygen uptake: A follow-up study of participants in the total health promotion plan. Environ. Health Prev. Med. 2003, 8, 173–177. [Google Scholar] [CrossRef]
- Wong, S.L.; Katzmarzyk, P.; Nichaman, M.Z.; Church, T.S.; Blair, S.N.; Ross, R. Cardiorespiratory fitness is associated with lower abdominal fat independent of body mass index. Med. Sci. Sports Exerc. 2004, 36, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Fernberg, U.; Fernström, M.; Hurtig-Wennlöf, A. Arterial stiffness is associated to cardiorespiratory fitness and body mass index in young Swedish adults: The Lifestyle, Biomarkers, and Atherosclerosis study. Eur. J. Prev. Cardiol. 2017, 24, 1809–1818. [Google Scholar] [CrossRef] [PubMed]
- Carnethon, M.R.; Gulati, M.; Greenland, P. Prevalence and Cardiovascular Disease Correlates of Low Cardiorespiratory Fitness in Adolescents and Adults. JAMA 2005, 294, 2981–2988. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kuk, J.L.; Katzmarzyk, P.T.; Blair, S.N.; Church, T.S.; Ross, R. Cardiorespiratory Fitness Attenuates Metabolic Risk Independent of Abdominal Subcutaneous and Visceral Fat in Men. Diabetes Care 2005, 28, 895–901. [Google Scholar] [CrossRef] [Green Version]
- Lakoski, S.G.; Barlow, C.E.; Farrell, S.W.; Berry, J.D.; Morrow, J.R., Jr.; Haskell, W.L. Impact of body mass index, physical activity, and other clinical factors on cardiorespiratory fitness (from the Cooper Center longitudinal study). Am. J. Cardiol. 2011, 108, 34–39. [Google Scholar] [CrossRef]
- Cole, L.; Vance, J.; Vance, D. Phosphatidylcholine biosynthesis and lipoprotein metabolism. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids 2011, 1821, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Wallner, S.; Schmitz, G. Plasmalogens the neglected regulatory and scavenging lipid species. Chem. Phys. Lipids 2011, 164, 573–589. [Google Scholar] [CrossRef] [PubMed]
- Pietiläinen, K.H.; Sysi-Aho, M.; Rissanen, A.; Seppänen-Laakso, T.; Yki-Järvinen, H.; Kaprio, J.; Orešič, M. Acquired Obesity Is Associated with Changes in the Serum Lipidomic Profile Independent of Genetic Effects—A Monozygotic Twin Study. PLoS ONE 2007, 2, e218. [Google Scholar] [CrossRef] [PubMed]
- Floegel, A.; Stefan, N.; Yu, Z.; Mühlenbruch, K.; Drogan, D.; Joost, H.G.; Fritsche, A.; Häring, H.U.; Hrabě de Angelis, M.; Peters, A.; et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes 2013, 62, 639–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmitz, G.; Ruebsaamen, K. Metabolism and atherogenic disease association of lysophosphatidylcholine. Atherosclerosis 2010, 208, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Hung, N.D.; Sok, D.E.; Kim, M.R. Prevention of 1-palmitoyl lysophosphatidylcholine-induced inflammation by polyunsaturated acyl lysophosphatidylcholine. Inflamm. Res. 2012, 61, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Barber, M.N.; Risis, S.; Yang, C.; Meikle, P.J.; Staples, M.; Febbraio, M.A.; Bruce, C.R. Plasma Lysophosphatidylcholine Levels Are Reduced in Obesity and Type 2 Diabetes. PLoS ONE 2012, 7, e41456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.K.; Lee, D.H.; Kim, J.K.; Park, M.J.; Yan, J.J.; Song, D.K.; Vaziri, N.D.; Noh, J.W. Lysophosphatidylcholine, oxidized low-density lipoprotein and cardiovascular disease in Korean hemodialysis patients: Analysis at 5 years of follow-up. J. Korean Med. Sci. 2013, 28, 268–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyene, H.B.; Olshansky, G.T.; Smith, A.A.; Giles, C.; Huynh, K.; Cinel, M.; Mellett, N.A.; Cadby, G.; Hung, J.; Hui, J.; et al. High-coverage plasma lipidomics reveals novel sex-specific lipidomic fingerprints of age and BMI: Evidence from two large population cohort studies. PLoS Biol. 2020, 18, e3000870. [Google Scholar] [CrossRef]
- Iqbal, J.; Walsh, M.T.; Hammad, S.M.; Hussain, M.M. Sphingolipids and Lipoproteins in Health and Metabolic Disorders. Trends Endocrinol. Metab. TEM 2017, 28, 506–518. [Google Scholar] [CrossRef]
- Jiang, X.-c.; Paultre, F.; Pearson, T.A.; Reed, R.G.; Francis, C.K.; Lin, M.; Berglund, L.; Tall, A.R. Plasma Sphingomyelin Level as a Risk Factor for Coronary Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 2614–2618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanamatsu, H.; Ohnishi, S.; Sakai, S.; Yuyama, K.; Mitsutake, S.; Takeda, H.; Hashino, S.; Igarashi, Y. Altered levels of serum sphingomyelin and ceramide containing distinct acyl chains in young obese adults. Nutr. Diabetes 2014, 4, e141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saleem, M.; Herrmann, N.; Dinoff, A.; Marzolini, S.; Mielke, M.M.; Andreazza, A.; Oh, P.I.; Vattem Venkata, S.L.; Haughey, N.J.; Lanctôt, K.L. Association Between Sphingolipids and Cardiopulmonary Fitness in Coronary Artery Disease Patients Undertaking Cardiac Rehabilitation. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2020, 75, 671–679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tricò, D.; Mengozzi, A.; Nesti, L.; Hatunic, M.; Gabriel Sanchez, R.; Konrad, T.; Lalić, K.; Lalić, N.M.; Mari, A.; Natali, A.; et al. Circulating palmitoleic acid is an independent determinant of insulin sensitivity, beta cell function and glucose tolerance in non-diabetic individuals: A longitudinal analysis. Diabetologia 2020, 63, 206–218. [Google Scholar] [CrossRef] [Green Version]
- McCann, M.R.; George De la Rosa, M.V.; Rosania, G.R.; Stringer, K.A. L-Carnitine and Acylcarnitines: Mitochondrial Biomarkers for Precision Medicine. Metabolites 2021, 11, 51. [Google Scholar] [CrossRef]
- Koves, T.R.; Ussher, J.R.; Noland, R.C.; Slentz, D.; Mosedale, M.; Ilkayeva, O.; Bain, J.; Stevens, R.; Dyck, J.R.; Newgard, C.B.; et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 2008, 7, 45–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soeters, M.R.; Sauerwein, H.P.; Duran, M.; Wanders, R.J.; Ackermans, M.T.; Fliers, E.; Houten, S.; Serlie, M.J. Muscle acylcarnitines during short-term fasting in lean healthy men. Clin. Sci. 2009, 116, 585–592. [Google Scholar] [CrossRef] [Green Version]
- Huffman, K.M.; Koves, T.R.; Hubal, M.J.; Abouassi, H.; Beri, N.; Bateman, L.A.; Stevens, R.D.; Ilkayeva, O.R.; Hoffman, E.P.; Muoio, D.M.; et al. Metabolite signatures of exercise training in human skeletal muscle relate to mitochondrial remodelling and cardiometabolic fitness. Diabetologia 2014, 57, 2282–2295. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Cooper, D.E.; Cluntun, A.A.; Warmoes, M.O.; Zhao, S.; Reid, M.A.; Liu, J.; Lund, P.J.; Lopes, M.; Garcia, B.A. Acetate production from glucose and coupling to mitochondrial metabolism in mammals. Cell 2018, 175, 502–513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frampton, J.; Murphy, K.G.; Frost, G.; Chambers, E.S. Short-chain fatty acids as potential regulators of skeletal muscle metabolism and function. Nat. Metab. 2020, 2, 840–848. [Google Scholar] [CrossRef]
- Antunes, B.M.; Rosa-Neto, J.C.; Batatinha, H.A.P.; Franchini, E.; Teixeira, A.M.; Lira, F.S. Physical fitness status modulates the inflammatory proteins in peripheral blood and circulating monocytes: Role of PPAR-gamma. Sci. Rep. 2020, 10, 14094. [Google Scholar] [CrossRef]
- Bressa, C.; Bailén-Andrino, M.; Pérez-Santiago, J.; González-Soltero, R.; Pérez, M.; Montalvo-Lominchar, M.G.; Maté-Muñoz, J.L.; Domínguez, R.; Moreno, D.; Larrosa, M. Differences in gut microbiota profile between women with active lifestyle and sedentary women. PLoS ONE 2017, 12, e0171352. [Google Scholar] [CrossRef] [Green Version]
- Okamoto, T.; Morino, K.; Ugi, S.; Nakagawa, F.; Lemecha, M.; Ida, S.; Ohashi, N.; Sato, D.; Fujita, Y.; Maegawa, H. Microbiome potentiates endurance exercise through intestinal acetate production. Am. J. Physiol. Metab. 2019, 316, E956–E966. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.; Grapov, D.; Fiehn, O.; Chandler, C.J.; Burnett, D.J.; Souza, E.C.; Casazza, G.A.; Gustafson, M.B.; Keim, N.L.; Newman, J.W.; et al. Improved Metabolic Health Alters Host Metabolism in Parallel with Changes in Systemic Xeno-Metabolites of Gut Origin. PLoS ONE 2014, 9, e84260. [Google Scholar] [CrossRef] [Green Version]
- Castro, A.; Duft, R.G.; Silva, L.M.; Ferreira, M.L.V.; Andrade, A.L.L.; Bernardes, C.F.; Cavaglieri, C.R.; Chacon-Mikahil, M.P.T. Understanding the Relationship between Intrinsic Cardiorespiratory Fitness and Serum and Skeletal Muscle Metabolomics Profile. J. Proteome Res. 2021, 20, 2397–2409. [Google Scholar] [CrossRef]
- Parto, P.; Lavie, C.J.; Swift, D.; Sui, X. The role of cardiorespiratory fitness on plasma lipid levels. Expert Rev. Cardiovasc. Ther. 2015, 13, 1177–1183. [Google Scholar] [CrossRef]
- Zeisel, S.H.; da Costa, K.-A. Choline: An essential nutrient for public health. Nutr. Rev. 2009, 67, 615–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Høeg, T.B.; Chmiel, K.; Warrick, A.E.; Taylor, S.L.; Weiss, R.H. Ultramarathon Plasma Metabolomics: Phosphatidylcholine Levels Associated with Running Performance. Sports 2020, 8, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, T.; Zhang, B.; Duan, W.; Zhang, J.; Wang, M. Nutrients and bioactive components from vinegar: A fermented and functional food. J. Funct. Foods 2020, 64, 103681. [Google Scholar] [CrossRef]
- Regueiro, J.; Vallverdu-Queralt, A.; Simal-Gandara, J.; Estruch, R.; Lamuela-Raventos, R.M. Urinary tartaric acid as a potential biomarker for the dietary assessment of moderate wine consumption: A randomised controlled trial. Br. J. Nutr. 2014, 111, 1680–1685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kistner, S.; Rist, M.J.; Döring, M.; Dörr, C.; Neumann, R.; Härtel, S.; Bub, A. An NMR-Based Approach to Identify Urinary Metabolites Associated with Acute Physical Exercise and Cardiorespiratory Fitness in Healthy Humans-Results of the KarMeN Study. Metabolites 2020, 10, 212. [Google Scholar] [CrossRef] [PubMed]
- Wallace, M.; Hashim, Y.-Y.; Wingfield, M.; Culliton, M.; McAuliffe, F.; Gibney, M.; Brennan, L. Effects of menstrual cycle phase on metabolomic profiles in premenopausal women. Hum. Reprod. 2010, 25, 949–956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biniaminov, N.; Bandt, S.; Roth, A.; Haertel, S.; Neumann, R.; Bub, A. Irisin, physical activity and fitness status in healthy humans: No association under resting conditions in a cross-sectional study. PLoS ONE 2018, 13, e0189254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merz, B.; Frommherz, L.; Rist, M.J.; Kulling, S.E.; Bub, A.; Watzl, B. Dietary Pattern and Plasma BCAA-Variations in Healthy Men and Women-Results from the KarMeN Study. Nutrients 2018, 10, 623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittig, F.; Heuer, T.; Claupein, E.; Pfau, C.; Cordts, A.; Schulze, B.; Padilla Bravo, C.A. Auswertung der Daten der Nationalen Verzehrsstudie II (NVS II): Eine integrierte verhaltens- und lebensstilbasierte Analyse des Bio-Konsums: BÖL Abschlussbericht FKZ: 08 OE 056, 08 OE 069. 2010. Available online: http://orgprints.org/18055/ (accessed on 16 July 2021).
- Weinert, C.H.; Egert, B.; Kulling, S.E. On the applicability of comprehensive two-dimensional gas chromatography combined with a fast-scanning quadrupole mass spectrometer for untargeted large-scale metabolomics. J. Chromatogr. 2015, 1405, 156–167. [Google Scholar] [CrossRef]
- Egert, B.; Weinert, C.H.; Kulling, S.E. A peaklet-based generic strategy for the untargeted analysis of comprehensive two-dimensional gas chromatography mass spectrometry data sets. J. Chromatogr. 2015, 1405, 168–177. [Google Scholar] [CrossRef]
- Ecker, J.; Scherer, M.; Schmitz, G.; Liebisch, G. A rapid GC–MS method for quantification of positional and geometric isomers of fatty acid methyl esters. J. Chromatogr. B 2012, 897, 98–104. [Google Scholar] [CrossRef]
- Römisch-Margl, W.; Prehn, C.; Bogumil, R.; Röhring, C.; Suhre, K.; Adamski, J. Procedure for tissue sample preparation and metabolite extraction for high-throughput targeted metabolomics. Metabolomics 2012, 8, 133–142. [Google Scholar] [CrossRef]
- Weinert, C.H.; Empl, M.T.; Krüger, R.; Frommherz, L.; Egert, B.; Steinberg, P.; Kulling, S.E. The influence of a chronic L-carnitine administration on the plasma metabolome of male Fischer 344 rats*. Mol. Nutr. Food Res. 2017, 61, 1600651. [Google Scholar] [CrossRef] [PubMed]
- Frommherz, L.; Bub, A.; Hummel, E.; Rist, M.J.; Roth, A.; Watzl, B.; Kulling, S.E. Age-Related Changes of Plasma Bile Acid Concentrations in Healthy Adults—Results from the Cross-Sectional KarMeN Study. PLoS ONE 2016, 11, e0153959. [Google Scholar] [CrossRef] [Green Version]
- R Code Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org (accessed on 16 July 2021).
- Kuhn, M. Caret: Classification and Regression Training. R Package Version 6.0-86. 2020. Available online: https://CRAN.R-project.org/package=caret (accessed on 16 July 2021).
- Schauberger, P.; Walker, A. Openxlsx: Read, Write and Edit Xlsx Files. R Package Version 4.1.5. 2020. Available online: https://CRAN.R-project.org/package=openxlsx (accessed on 16 July 2021).
- Stekhoven, D.J. missForest: Nonparametric Missing Value Imputation Using Random Forest. R Package Version 1.4. 2013. Available online: https://cran.r-project.org/web/packages/missForest/missForest.pdf (accessed on 16 July 2021).
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Slowikowski, K. Ggrepel: Automatically Position Non-Overlapping Text Labels with ‘ggplot2’. R Package Version 0.9.0. 2020. Available online: https://github.com/slowkow/ggrepel (accessed on 16 July 2021).
- Kassambara, A. Ggpubr: ‘ggplot2’ Based Publication Ready Plots. R Package Version 0.3.0. 2020. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 16 July 2021).
- Xie, Y. Knitr: A General-Purpose Package for Dynamic Report Generation in R. R Package Version 1.31. 2021. Available online: https://yihui.org/knitr/ (accessed on 16 July 2021).
- Sumner, L.W.; Amberg, A.; Barrett, D.; Beale, M.H.; Beger, R.; Daykin, C.A.; Fan, T.W.; Fiehn, O.; Goodacre, R.; Griffin, J.L.; et al. Proposed minimum reporting standards for chemical analysis Chemical Analysis Working Group (CAWG) Metabolomics Standards Initiative (MSI). Metabolomics 2007, 3, 211–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wishart, D.S.; Feunang, Y.D.; Marcu, A.; Guo, A.C.; Liang, K.; Vazquez-Fresno, R.; Sajed, T.; Johnson, D.; Li, C.; Karu, N.; et al. HMDB 4.0: The human metabolome database for 2018. Nucleic Acids Res. 2018, 46, D608–D617. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.F.; Kanehisa, M. Using the KEGG Database Resource. Curr. Protoc. Bioinform. 2005, 11, 1.12.1–1.12.54. [Google Scholar] [CrossRef] [PubMed]
- Ulaszewska, M.; Weinert, C.; Trimigno, A.; Portmann, R.; Andres-Lacueva, C.; Badertscher, R.; Brennan, L.; Brunius, C.; Bub, A.; Capozzi, F.; et al. Nutrimetabolomics: An Integrative Action for Metabolomic Analyses in Human Nutritional Studies. Mol. Nutr. Food Res. 2019, 63, e1800384. [Google Scholar] [CrossRef] [PubMed]
| Pathway | Total Number of Plasma Metabolites | Number of Plasma Metabolites Correlating with the VO2peak | |||
|---|---|---|---|---|---|
| Females (n = 102) | Males (n = 150) | ||||
| * | ** | * | ** | ||
| All | 427 | 125 | 59 | 112 | 24 |
| Lipid metabolism | 164 | 63 | 27 | 36 | 8 |
| Amino acid metabolism | 41 | 4 | 6 | 8 | 2 |
| Xenobiotics and related metabolism | 12 | 2 | 2 | 4 | 1 |
| Mammalian-microbial cometabolism | 7 | 2 | 0 | 1 | 0 |
| Carbohydrate metabolism | 5 | 2 | 1 | 1 | 0 |
| Energy metabolism | 5 | 3 | 1 | 2 | 0 |
| Cofactors and vitamins metabolism | 1 | 1 | 0 | 0 | 0 |
| Nucleotide metabolism | 1 | 0 | 0 | 0 | 0 |
| Unknown | 191 | 48 | 22 | 60 | 13 |
| Positive Correlations | Negative Correlations | |||
|---|---|---|---|---|
| Variables | r (95% CIs) | Variables | r (95% CIs) | |
| Females | ||||
| 1 | PC ae C40:3 | 0.37 (0.19; 0.53) | U3.961 | −0.39 (−0.55; −0.22) |
| 2 | PC ae C42:4 | 0.31 (0.13; 0.48) | U3.956 | −0.32 (−0.49; −0.14) |
| 3 | C5-Carnitine | 0.31 (0.12; 0.47) | U3.950 | −0.31 (−0.48; −0.12) |
| 4 | PC ae C38:3 | 0.28 (0.09; 0.45) | U4.252 | −0.31 (−0.47; −0.12) |
| 5 | Choline | 0.27 (0.08; 0.44) | U3.971 | −0.31 (−0.47; −0.12) |
| 6 | Glyceric Acid | 0.27 (0.08; 0.44) | U0978 | −0.30 (−0.46; −0.11) |
| 7 | U0856 | 0.27 (0.08; 0.44) | U0975 | −0.28 (−0.45; −0.09) |
| 8 | PC ae C36:2 | 0.26 (0.07; 0.44) | U2.656 | −0.28 (−0.45; −0.09) |
| 9 | Acetylornithine | 0.26 (0.07; 0.43) | U1.156 | −0.28 (−0.45; −0.09) |
| 10 | PC ae C44:3 | 0.26 (0.07; 0.43) | U3.060 | −0.26 (−0.43; −0.07) |
| Males | ||||
| 1 | U0130 | 0.19 (0.03; 0.34) | U2.250 | −0.25 (−0.39; −0.09) |
| 2 | Alanine | 0.18 (0.02; 0.33) | U2.822 | −0.21 (−0.36; −0.05) |
| 3 | C6 (C4:1-DC)-Carnitine | 0.18 (0.02; 0.33) | U (Sugar-like 4) | −0.21 (−0.36; −0.05) |
| 4 | U2.910 | 0.18 (0.02; 0.33) | U1331 | −0.21 (−0.36; −0.05) |
| 5 | PC aa C36:3 | 0.18 (0.02; 0.33) | Tartaric acid | −0.21 (−0.36; −0.05) |
| 6 | U3.385 | 0.17 (0.01; 0.32) | U1.156 | −0.20 (−0.35; −0.04) |
| 7 | Glutamate | 0.17 (0.01; 0.32) | U0.936 | −0.19 (−0.34; −0.03) |
| 8 | - | - | U1.159 | −0.19 (−0.34; −0.03) |
| 9 | - | - | U1.166 | −0.19 (−0.34; −0.03) |
| 10 | - | - | PC ae C38:6 | −0.18 (−0.33; −0.02) |
| Model | Females (n = 102) | Males (n = 150) |
|---|---|---|
| Approach 1 Selection | R² (adjusted) = 0.40 FM (%), HDL cholesterol, LBM, PWV, Hb, BP systolic, BP diastolic | R² (adjusted) = 0.43 FM (%), HDL cholesterol, BMC, AEE, TGs, LDL cholesterol |
| Approach 2 Selection | R² (adjusted) = 0.72 All phenotypical/clinical variables + PC ae C40:3, U3.961, S-Methylcysteine, Tartaric acid, U1.148, Serine, C24:0, Kynurenine, U0992 | R² (adjusted) = 0.62 All phenotypical/clinical variables + PC aa C36:3, U0130, Tartaric acid, C6 (C4:1-DC)-Carnitine, C14:1-OH-Carnitine, U2.250, Malic acid, Glutamate, C24:0, U1.226 |
| Approach 3 Selection | R² (adjusted) = 0.68 FM (%), PC ae C40:3, myo-Inositol, U0975, U3.961, U7.294, Glycine, U2.313, Lysine, C18:1-Carnitine | R² (adjusted) = 0.59 FM (%), Malic Acid, Taurocholate, PC aa C36:3, U0130, PC aa C36:6, Glutamate, U(Similar to Uracil), U1.226 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kistner, S.; Döring, M.; Krüger, R.; Rist, M.J.; Weinert, C.H.; Bunzel, D.; Merz, B.; Radloff, K.; Neumann, R.; Härtel, S.; et al. Sex-Specific Relationship between the Cardiorespiratory Fitness and Plasma Metabolite Patterns in Healthy Humans—Results of the KarMeN Study. Metabolites 2021, 11, 463. https://doi.org/10.3390/metabo11070463
Kistner S, Döring M, Krüger R, Rist MJ, Weinert CH, Bunzel D, Merz B, Radloff K, Neumann R, Härtel S, et al. Sex-Specific Relationship between the Cardiorespiratory Fitness and Plasma Metabolite Patterns in Healthy Humans—Results of the KarMeN Study. Metabolites. 2021; 11(7):463. https://doi.org/10.3390/metabo11070463
Chicago/Turabian StyleKistner, Sina, Maik Döring, Ralf Krüger, Manuela J. Rist, Christoph H. Weinert, Diana Bunzel, Benedikt Merz, Katrin Radloff, Rainer Neumann, Sascha Härtel, and et al. 2021. "Sex-Specific Relationship between the Cardiorespiratory Fitness and Plasma Metabolite Patterns in Healthy Humans—Results of the KarMeN Study" Metabolites 11, no. 7: 463. https://doi.org/10.3390/metabo11070463
APA StyleKistner, S., Döring, M., Krüger, R., Rist, M. J., Weinert, C. H., Bunzel, D., Merz, B., Radloff, K., Neumann, R., Härtel, S., & Bub, A. (2021). Sex-Specific Relationship between the Cardiorespiratory Fitness and Plasma Metabolite Patterns in Healthy Humans—Results of the KarMeN Study. Metabolites, 11(7), 463. https://doi.org/10.3390/metabo11070463






