Delivery of B. subtilis into Animal Intestine Using Chitosan-Derived Bioresorbable Gel Carrier: Preliminary Results
Abstract
:1. Introduction
2. Results
2.1. Release of Dye from the Gel in Acidic and Alkaline Media
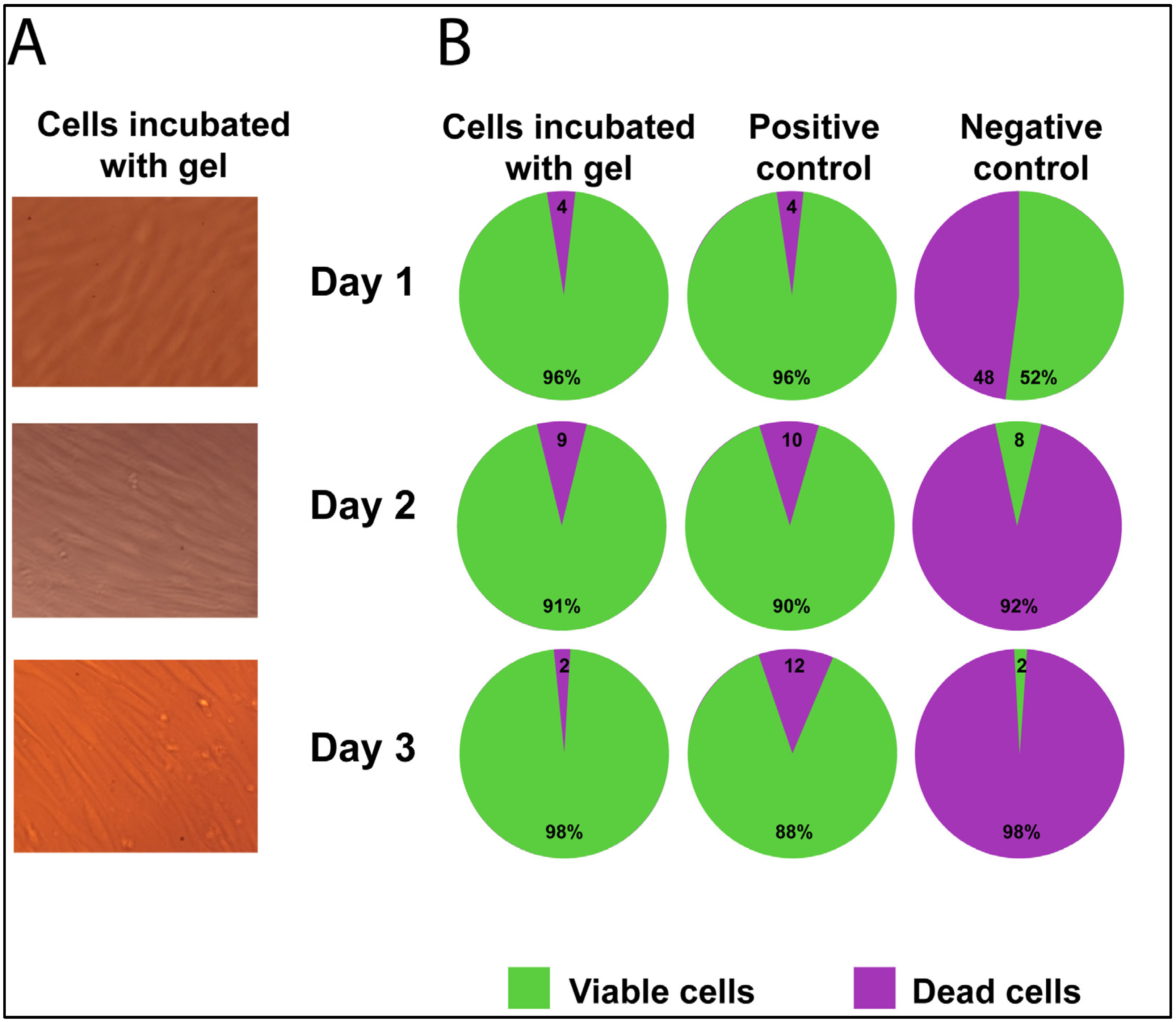
2.2. Cell Viability/Cytotoxicity of Fibroblast Culture with Gel
2.3. Test Strain of B. subtillus 20 Transit in the Gastrointestinal Tract of the Mice
3. Discussion
4. Materials and Methods
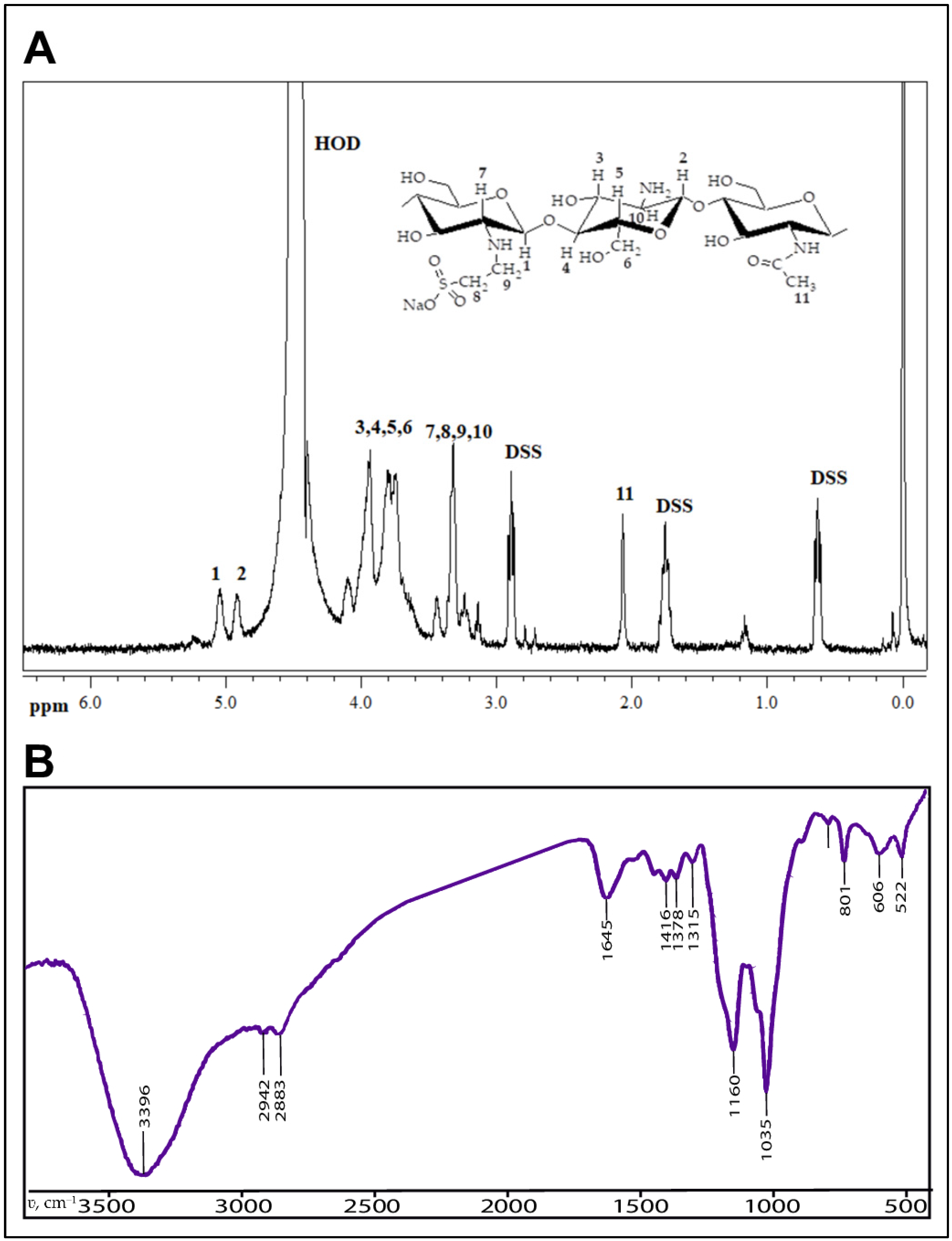
4.1. Bioresorbable Gel Carrier
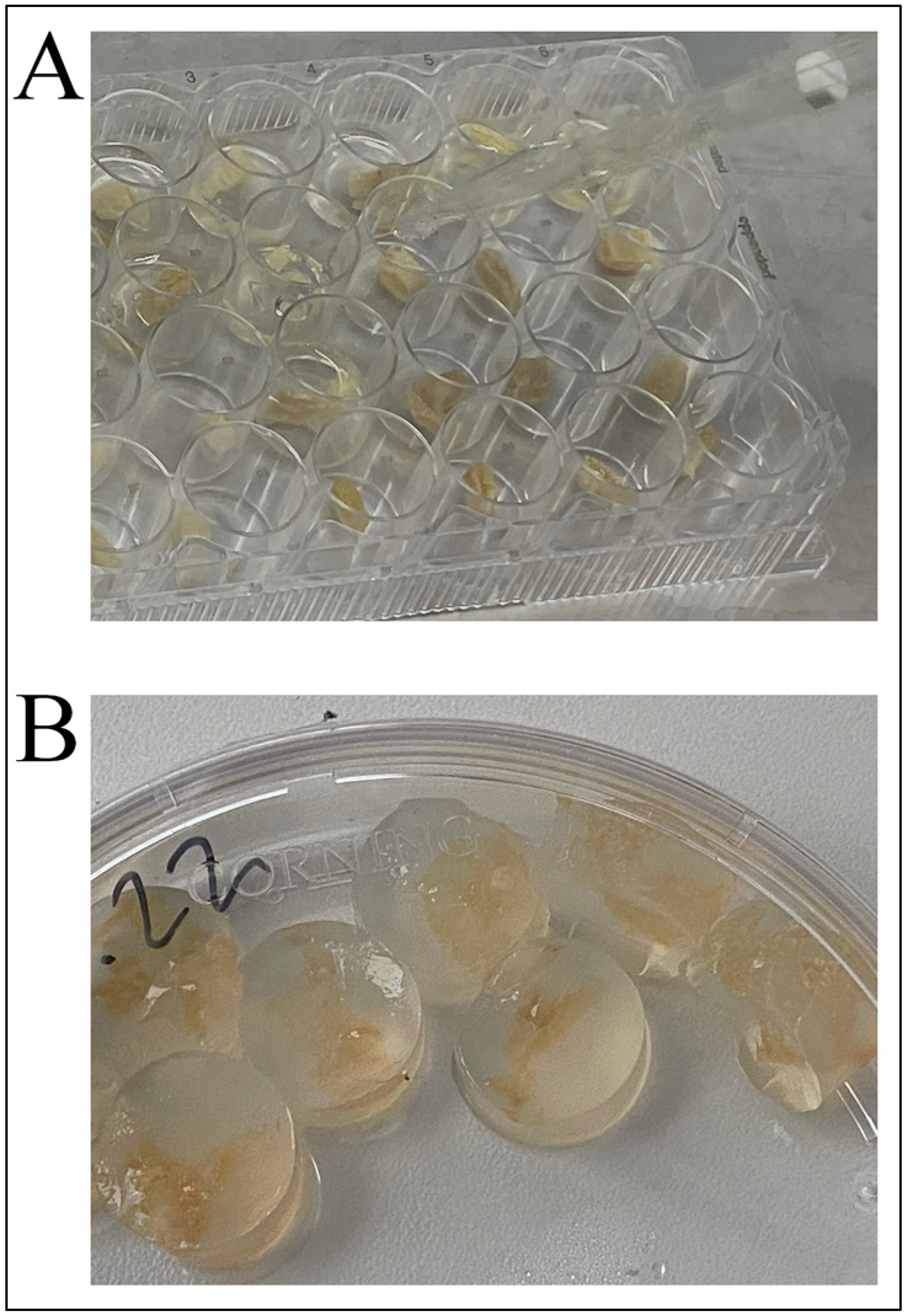
4.2. Gel Loading Procedure
4.3. Animals
4.4. Bacterial Strain and Growth Conditions
4.5. Method of Characterization of Bacillus subtilis 20 Colony Forming Units
4.6. Gel Release Model in Different pH Mediums
4.7. Cytotoxicity Evaluation
4.8. Statistics
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dixit, K.; Chaudhari, D.; Dhotre, D.; Shouche, Y.; Saroj, S. Restoration of Dysbiotic Human Gut Microbiome for Homeostasis. Life Sci. 2021, 278, 119622. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.L.; Sokol, H. The Gut Mycobiota: Insights into Analysis, Environmental Interactions and Role in Gastrointestinal Diseases. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 331–345. [Google Scholar] [CrossRef]
- Guan, Q. A Comprehensive Review and Update on the Pathogenesis of Inflammatory Bowel Disease. J. Immunol. Res. 2019, 2019, 7247238. [Google Scholar] [CrossRef]
- Ding, W.K.; Shah, N.P. Effect of Various Encapsulating Materials on the Stability of Probiotic Bacteria. J. Food Sci. 2009, 74, M100–M107. [Google Scholar] [CrossRef] [PubMed]
- Weingarden, A.R.; Vaughn, B.P. Intestinal Microbiota, Fecal Microbiota Transplantation, and Inflammatory Bowel Disease. Gut Microbes 2017, 8, 238–252. [Google Scholar] [CrossRef]
- Maher, M. Tolerance and Effect of a Probiotic Supplement Delivered in Capsule Form. FNS 2019, 10, 626–634. [Google Scholar] [CrossRef]
- Cuentas, A.M.; Deaton, J.; Khan, S.; Davidson, J.; Ardita, C. The Effect of Bacillus Subtilis DE111 on the Daily Bowel Movement Profile for People with Occasional Gastrointestinal Irregularity. J. Prob. Health 2017, 5, 4. [Google Scholar] [CrossRef]
- Paytuví-Gallart, A.; Sanseverino, W.; Winger, A.M. Daily Intake of Probiotic Strain Bacillus Subtilis DE111 Supports a Healthy Microbiome in Children Attending Day-Care. Benef. Microbes 2020, 11, 611–620. [Google Scholar] [CrossRef]
- Tohidifar, P.; Plutz, M.J.; Ordal, G.W.; Rao, C.V. The Mechanism of Bidirectional PH Taxis in Bacillus Subtilis. J. Bacteriol. 2020, 202, e00491-19. [Google Scholar] [CrossRef]
- Gauvry, E.; Mathot, A.-G.; Couvert, O.; Leguérinel, I.; Coroller, L. Effects of Temperature, PH and Water Activity on the Growth and the Sporulation Abilities of Bacillus Subtilis BSB1. Int. J. Food Microbiol. 2021, 337, 108915. [Google Scholar] [CrossRef]
- Jiménez-Delgadillo, R.; Valdés-Rodríguez, S.E.; Olalde-Portugal, V.; Abraham-Juárez, R.; García-Hernández, J.L. Efecto Del PH y Temperatura Sobre El Crecimiento y Actividad Antagónica de Bacillus Subtilis Sobre Rhizoctonia Solani. RMF 2018, 36, 256–275. [Google Scholar] [CrossRef]
- Mortazavian, A.; Razavi, S.; Ehsani, M. Principles and Methods of Microencapsulation of Probiotic Microorganisms. Iran J. Microbiol. 2007, 5, 1–18. Available online: http://www.ijbiotech.com/article_7032.html. (accessed on 10 December 2022).
- Yao, M.; Wu, J.; Li, B. Microencapsulation of Lactobacillus Salivarious Li01 for Enhanced Storage Viability and Targeted Delivery to Gut Microbiota. Food Hydrocoll. 2017, 72, 228–236. [Google Scholar] [CrossRef]
- Silva, K.; Cezarino, E.; Michelon, M. Symbiotic Microencapsulation to Enhance Lactobacillus Acidophilus Survival. LWT-Food Sci. Technol. 2018, 89, 503–509. [Google Scholar] [CrossRef]
- Liu, J.; Li, X.; Zhang, X.; Wang, R.; Han, S.; Qin, P.; Xing, X.-H.; Zhang, C. Gut Lumen-Targeted Oral Delivery System for Bioactive Agents to Regulate Gut Microbiome. J. Future Foods 2022, 2, 307–325. [Google Scholar] [CrossRef]
- Arlov, Ø.; Rütsche, D.; Asadi Korayem, M.; Öztürk, E.; Zenobi-Wong, M. Engineered Sulfated Polysaccharides for Biomedical Applications. Adv. Funct. Mater. 2021, 31, 2010732. [Google Scholar] [CrossRef]
- Petrova, Y.S.; Bukharova, A.V.; Neudachina, L.K.; Adamova, L.V.; Koryakova, O.V.; Pestov, A.V. Chemical Properties of N-2-Sulfoethylchitosan with a Medium Degree of Substitution. Polym. Sci. Ser. B 2014, 56, 487–493. [Google Scholar] [CrossRef]
- Kapitanova, E.I.; Ibragimova, A.A.; Petrova, Y.S.; Pestov, A.V.; Neudachina, L.K. Influence of the Degree of Chitosan Sulfoethylation on the Sorption of Palladium(II) Chloride Complexes from Multicomponent Solutions. Russ. J. Appl. Chem. 2018, 91, 297–303. [Google Scholar] [CrossRef]
- Petrova, Y.S.; Neudachina, L.K.; Oseeva, M.Y.; Pestov, A.V. Effect of Complex-Former Ion Concentration on the Selectivity of Metal Ion Sorption on Cross-Linked N-2-Sulfoethylchitosan. Russ. J. Inorg. Chem. 2018, 63, 400–405. [Google Scholar] [CrossRef]
- Petrova, Y.S.; Pestov, A.V.; Alifkhanova, L.M.K.; Neudachina, L.K. Effect of the Degree of Cross-Linking of N-2-Sulfoethylchitosan on the Sorption Selectivity of Copper(II) and Silver(I). Russ. J. Appl. Chem. 2015, 88, 1434–1439. [Google Scholar] [CrossRef]
- Petrova, Y.S.; Kapitanova, E.I.; Neudachina, L.K.; Pestov, A.V. Sorption Isotherms of Metal Ions onto an N-(2-Sulfoethyl)Chitosan-Based Material from Single- and Multi-Component Solutions. Sep. Sci. Technol. 2017, 52, 2385–2394. [Google Scholar] [CrossRef]
- Evdokimova, O.V.; Pestov, A.V.; Pechishcheva, N.V.; Shunyaev, K.Y. Preparation of Sorbents Based on Chitosan and Its Sulfoethyl Derivative for Sorption of Perrhenate Ions. Russ. J. Appl. Chem. 2016, 89, 1377–1382. [Google Scholar] [CrossRef]
- Petrova, Y.S.; Pestov, A.V.; Usoltseva, M.K.; Kapitanova, E.I.; Neudachina, L.K. Methods for Correction of Selectivity of N -(2-Sulfoethyl)Chitosan-Based Materials towards Platinum(IV) and Palladium(II) Ions. Sep. Sci. Technol. 2019, 54, 42–50. [Google Scholar] [CrossRef]
- Khosravi Zanjani, M.A.; Ghiassi Tarzi, B.; Sharifan, A.; Mohammadi, N. Microencapsulation of Probiotics by Calcium Alginate-Gelatinized Starch with Chitosan Coating and Evaluation of Survival in Simulated Human Gastro-Intestinal Condition. Iran J. Pharm. Res. 2014, 13, 843–852. [Google Scholar] [PubMed]
- Zhu, H.; Hart, C.A.; Sales, D.; Roberts, N.B. Bacterial Killing in Gastric Juice–Effect of PH and Pepsin on Escherichia Coli and Helicobacter Pylori. J. Med. Microbiol. 2006, 55, 1265–1270. [Google Scholar] [CrossRef]
- Higgins, D.; Dworkin, J. Recent Progress in Bacillus Subtilis Sporulation. FEMS Microbiol. Rev. 2012, 36, 131–148. [Google Scholar] [CrossRef]
- Wang, X.; Cao, Z.; Zhang, M.; Meng, L.; Ming, Z.; Liu, J. Bioinspired Oral Delivery of Gut Microbiota by Self-Coating with Biofilms. Sci. Adv. 2020, 6, eabb1952. [Google Scholar] [CrossRef] [PubMed]
- Tallawi, M.; Opitz, M.; Lieleg, O. Modulation of the Mechanical Properties of Bacterial Biofilms in Response to Environmental Challenges. Biomater. Sci. 2017, 5, 887–900. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Wang, X.; Pang, Y.; Cheng, S.; Liu, J. Biointerfacial Self-Assembly Generates Lipid Membrane Coated Bacteria for Enhanced Oral Delivery and Treatment. Nat. Commun. 2019, 10, 5783. [Google Scholar] [CrossRef] [PubMed]
- Khosravi Zanjani, M.A.; Ehsani, M.R.; Ghiassi Tarzi, B.; Sharifan, A. Promoting Probiotics Survival by Microencapsualtion with Hylon Starch and Genipin Cross-Linked Coatings in Simulated Gastro-Intestinal Condition and Heat Treatment. Iran J. Pharm. Res. 2018, 17, 753–766. [Google Scholar] [PubMed]
- Krasaekoopt, W.; Bhandari, B.; Deeth, H. The Influence of Coating Materials on Some Properties of Alginate Beads and Survivability of Microencapsulated Probiotic Bacteria. Int. Dairy J. 2004, 14, 737–743. [Google Scholar] [CrossRef]
- Bolshakov, I.N.; Gornostaev, L.M.; Fominykh, O.I.; Svetlakov, A.V. Synthesis, Chemical and Biomedical Aspects of the Use of Sulfated Chitosan. Polymers 2022, 14, 3431. [Google Scholar] [CrossRef]
- Ding, K.; Wang, Y.; Wang, H.; Yuan, L.; Tan, M.; Shi, X.; Lyu, Z.; Liu, Y.; Chen, H. 6- O -Sulfated Chitosan Promoting the Neural Differentiation of Mouse Embryonic Stem Cells. ACS Appl. Mater. Interfaces 2014, 6, 20043–20050. [Google Scholar] [CrossRef] [PubMed]
- Pestov, A.V.; Petrova, Y.S.; Bukharova, A.V.; Neudachina, L.K.; Koryakova, O.V.; Matochkina, E.G.; Kodess, M.I.; Yatluk, Y.G. Synthesis in a Gel and Sorption Properties of N-2-Sulfoethyl Chitosan. Russ. J. Appl. Chem. 2013, 86, 269–272. [Google Scholar] [CrossRef]
- Samokhin, A.G.; Tkachenko, V.O.; Kuznetsov, V.A.; Zemlyakova, E.O.; Nesterov, D.V.; Larionov, P.M.; Pestov, A.V. Selection of an Optimal Method for Sterilization of the Medical Grade Biodegradable Polymers. In Proceedings of the “2nd International Conference Modern Synthetic Methodologies for Creating Drugs and Functional Materials (MOSM2018)” (15–17 November 2018), published in AIP Conference Proceedings, Kuantan, Malaysia, 11 January 2019; p. 030017. [Google Scholar] [CrossRef]
- FELASA Working Group on Revision of Guidelines for Health Monitoring of Rodents and Rabbits; Mähler, M.; Berard, M.; Feinstein, R.; Gallagher, A.; Illgen-Wilcke, B.; Pritchett-Corning, K.; Raspa, M. FELASA Recommendations for the Health Monitoring of Mouse, Rat, Hamster, Guinea Pig and Rabbit Colonies in Breeding and Experimental Units. Lab. Anim. 2014, 48, 178–192. [Google Scholar] [CrossRef]
- Hubrecht, R.C.; Carter, E. The 3Rs and Humane Experimental Technique: Implementing Change. Animals 2019, 9, 754. [Google Scholar] [CrossRef] [PubMed]
- Pokrovskii, V.M.; Korot’ko, G.F. Human Physiology: Text-book, 3rd ed.; Revised and Complete; JSC Publishing House “Medicina”: Moscow, Russia, 2011; p. 656. ISBN 5-225-04729-7. [Google Scholar]
- McIlvaine, T.C. A Buffer Solution For Colorimetric Comparison. J. Biol. Chem. 1921, 49, 183–186. [Google Scholar] [CrossRef]
- Starostenko, A.A.; Zaikin, P.A.; Troitskij, A.V.; Bystrova, T.N. Method of Producing Oxidised Dextran, Suitable For Its Visualization In Blood Serum. Abstract of Invention RU2690380. Bulletin No. 16. 3 June 2019. Available online: https://yandex.ru/patents/doc/RU2690380C1_20190603 (accessed on 10 December 2022).

| Days of the Experiment | Number of Mice | Titer Value, CFU/g |
|---|---|---|
| Bacteria-loaded gel carrier (baseline titer) | 1 | 8.75 × 108 |
| 2 | 8.75 × 108 | |
| Day 0 (before test strain feeding) | 1 | 0.0 |
| 2 | 0.0 | |
| Day 5 after feeding every day with gel carrier additive (end of test strain feeding) | 1 | 4.65 × 108 |
| 2 | 3.75 × 108 | |
| Day 6 (feeding with standard ration only) | 1 | 0.43 × 108 |
| 2 | 0.89 × 108 | |
| Day 7 (feeding with standard ration only) | 1 | 0.10 × 108 |
| 2 | 0.09 × 108 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samokhin, A.; Korel, A.; Blinova, E.; Pestov, A.; Kalmykova, G.; Akulova, N.; Betz, V.; Tkachenko, V.; Litvinova, E. Delivery of B. subtilis into Animal Intestine Using Chitosan-Derived Bioresorbable Gel Carrier: Preliminary Results. Gels 2023, 9, 120. https://doi.org/10.3390/gels9020120
Samokhin A, Korel A, Blinova E, Pestov A, Kalmykova G, Akulova N, Betz V, Tkachenko V, Litvinova E. Delivery of B. subtilis into Animal Intestine Using Chitosan-Derived Bioresorbable Gel Carrier: Preliminary Results. Gels. 2023; 9(2):120. https://doi.org/10.3390/gels9020120
Chicago/Turabian StyleSamokhin, Alexander, Anastasia Korel, Elena Blinova, Alexander Pestov, Galina Kalmykova, Nadezhda Akulova, Viktoria Betz, Vadim Tkachenko, and Ekaterina Litvinova. 2023. "Delivery of B. subtilis into Animal Intestine Using Chitosan-Derived Bioresorbable Gel Carrier: Preliminary Results" Gels 9, no. 2: 120. https://doi.org/10.3390/gels9020120






