Association of Maternal Sociodemographic, Anthropometric, and Lifestyle Factors with Childhood Anthropometric Measures and Anxiety Symptoms: A Nationally Representative Cross-Sectional Study of Preschool-Aged Children in Greece
Abstract
1. Introduction
2. Methods
2.1. Study Population
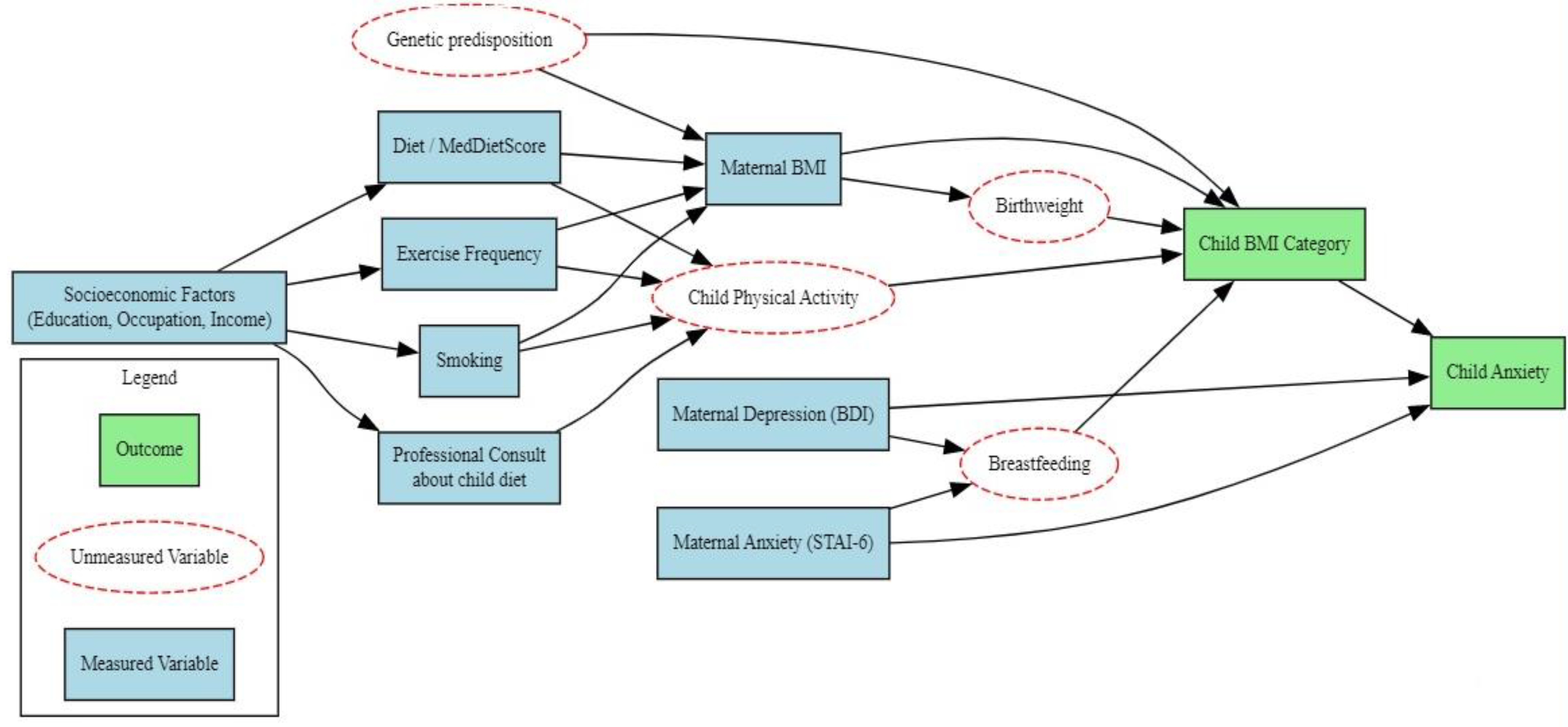
2.2. Study Design
2.3. Assessment of Adherence to the Mediterranean Diet
2.4. Assessment of Depressive Symptoms
2.5. Assessment of Anxiety Disorder
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics of the Study Population
3.2. Anthropometric Characteristics, Health Indicators, and Lifestyle Factors of the Study Population
3.2.1. Maternal Health Indicators and Anthropometric Characteristics
3.2.2. Children’s Health Indicators and Anthropometric Characteristics
3.2.3. Lifestyle Factors: Nutrition, Mental Well-Being, and Daily Routines of Mothers
3.2.4. Children’s Dietary Behaviors and Anxiety Levels
3.3. Comparative Analysis of Demographic, Anthropometric, Psychological, and Lifestyle Characteristics of Mothers in Relation to Children’s BMI Categories
3.4. Association of Maternal Socio-Demographic, Anthropometric, Psychological, and Lifestyle Characteristics with Children’s Anxiety Levels
3.4.1. Association Between Maternal Factors and Children’s Anxiety
3.4.2. Multivariable Logistic Regression Analysis of Maternal Predictors of Anxiety Absence in Preschool-Aged Children
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 July 2025).
- Wójcik, M.; Alvarez-Pitti, J.; Kozioł-Kozakowska, A.; Brzeziński, M.; Gabbianelli, R.; Herceg-Čavrak, V.; Wühl, E.; Lucas, I.; Radovanović, D.; Melk, A.; et al. Psychosocial and environmental risk factors of obesity and hypertension in children and adolescents—A literature overview. Front. Cardiovasc. Med. 2023, 10, 1268364. [Google Scholar] [CrossRef]
- Karavida, V.; Tympa, E. Nutrition in the Life of the Child; Kallipos, Open Academic Editions: Athens, Greece, 2023; ISBN 978-618-5667-25-2. [Google Scholar]
- Bel-Serrat, S.; Heinen, M.; Mehegan, J.; O’Brien, S.; Eldin, N.; Murrin, C.M.; Kelleher, C. Predictors of weight status in school-aged children: A prospective cohort study. Eur. J. Clin. Nutr. 2019, 73, 1299–1306. [Google Scholar] [CrossRef]
- World Health Organization. Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016; Available online: https://iris.who.int/bitstream/handle/10665/204176/9789241510066_eng.pdf?sequence=1 (accessed on 18 July 2025).
- Peng, W.; Wang, Y. Fighting obesity and non-communicable diseases needs different perspectives and new actions. Glob. Health J. 2022, 6, 115–117. [Google Scholar] [CrossRef]
- de Onis, M.; Blössner, M.; Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 2010, 92, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Miguel, M.; Oliveira, A.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, P.; Soriano-Cano, A.; Martínez-Vizcaíno, V. Prevalence of overweight and obesity among european preschool children: A systematic review and meta-regression by food group consumption. Nutrients 2019, 11, 1698. [Google Scholar] [CrossRef]
- European Association for the Study of Obesity (EASO). New WHO research reveals wide gradient of severe child obesity across Europe, with southern Europe having the highest levels. Obesity Facts. Peer-Reviewed Publication. 2019. Available online: https://www.eurekalert.org/news-releases/750565 (accessed on 17 July 2025).
- Lissner, L.; Wijnhoven, T.M.; Mehlig, K.; Sjöberg, A.; Kunesova, M.; Yngve, A.; Petrauskiene, A.; Duleva, V.; Rito, A.I.; Breda, J. Socioeconomic inequalities in childhood overweight: Heterogeneity across five countries in the WHO European Childhood Obesity Surveillance Initiative (COSI-2008). Int. J. Obes. 2016, 40, 796–802. [Google Scholar] [CrossRef]
- Manios, I.; Moschonis, G.; Androutsos, O.; Mavrogianni, C.; Malakou, E. Obesity and Co–Morbid Cardiometabolic Diseases: Causes–Consequences–Solutions; Dianeosis–Research & Analysis Organization: Athens, Greece, 2022. [Google Scholar]
- Greek National Action Plan Against Childhood Obesity. Childhood Obesity in Greece; Greek National Action Plan Against Childhood Obesity: Athens, Greece, 2022. Available online: https://paxisarkiakaipaidi.gov.gr/ (accessed on 18 July 2025).
- Kansra, A.; Lakkunarajah, S.; Jay, S. Childhood and adolescent obesity: A review. Front. Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- World Health Organization. Taking Action on Childhood Obesity Report; World Health Organization: Geneva, Switzerland, 2021; Available online: https://iris.who.int/bitstream/handle/10665/274792/WHO-NMH-PND-ECHO-18.1-eng.pdf (accessed on 15 July 2025).
- Förster, L.J.; Vogel, M.; Stein, R.; Hilbert, A.; Breinker, J.L.; Böttcher, M.; Kiess, W.; Poulain, T. Mental health in children and adolescents with overweight or obesity. BMC Public Health 2023, 23, 135. [Google Scholar] [CrossRef]
- Beynon, C. Association between children living with obesity and mental health problems: A data analysis of the Welsh Health Survey, UK. BMC Public Health 2023, 23, 383. [Google Scholar] [CrossRef] [PubMed]
- Uslu, N.; Evgin, D. Bullying and coping with bullying among obese/overweight and normal weight children. Arch. Psychiatr. Nurs. 2022, 36, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Rupp, K.; McCoy, S.M. Bullying perpetration and victimization among adolescents with overweight and obesity in a nationally representative sample. Child. Obes. 2019, 15, 323–330. [Google Scholar] [CrossRef]
- Jansen, P.W.; Verlinden, M.; Dommisse-van Berkel, A.; Mieloo, C.L.; Raat, H.; Hofman, A.; Jaddoe, V.W.; Verhulst, F.C.; Jansen, W.; Tiemeier, H. Teacher and peer reports of overweight and bullying among young primary school children. Pediatrics 2014, 134, 473–480. [Google Scholar] [CrossRef]
- Feretzakis, G.; Harokopou, A.; Fafoula, O.; Balaska, A.; Koulountzou, A.; Katoikou, E.; Anastasiou, A.; Zagkavieros, G.; Dalainas, I.; Gkritzelas, G. The impact of psychological health on childhood obesity: A cross-developmental stage Analysis. Appl. Sci. 2024, 14, 3208. [Google Scholar] [CrossRef]
- Jebeile, H.; Kelly, A.; O’MAlley, G.; Baur, L. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef]
- Cheng, S.; Kaminga, A.C.; Liu, Q.; Wu, F.; Wang, Z.; Wang, X.; Liu, X. Association between weight status and bullying experiences among children and adolescents in schools: An updated meta-analysis. Child Abuse Negl. 2022, 134, 105833. [Google Scholar] [CrossRef] [PubMed]
- Haqq, A.; Kebbe, M.; Tan, Q.; Manco, M.; Salas, X.R. The complexity and stigma of pediatric obesity. Child. Obes. 2021, 17, 229–240. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe; UNICEF. Child and Adolescent Health in the WHO European Region: Overweight and Obesity Fact Sheet; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2024; Available online: https://iris.who.int/handle/10665/379208 (accessed on 15 July 2025).
- Li, S.; Guo, J.; Zheng, K.; Shi, M.; Huang, T. Is sedentary behavior associated with executive function in children and adolescents? A systematic review. Front. Public Health 2022, 2, 832845. [Google Scholar] [CrossRef] [PubMed]
- Männikkö, N.; Ruotsalainen, H.; Miettunen, J.; Marttila-Tornio, K.; Kääriäinen, M. Parental socioeconomic status, adolescents’ screen time and sports participation through externalizing and internalizing characteristics. Heliyon 2020, 6, e03415. [Google Scholar] [CrossRef]
- Watson, A.; D’Souza, N.; Timperio, A.; Cliff, D.; Okely, A.; Hesketh, K. Longitudinal associations between weight status and academic achievement in primary school children. Pediatr. Obes. 2023, 18, e12975. [Google Scholar] [CrossRef] [PubMed]
- Sekouli, E.; Faki, I.; Katsaras, G.; Karachrysafi, S.; Papamitsou, T. Childhood obesity: Causes and consequences. Arch. Hell. Med. 2024, 41, 599–610. [Google Scholar]
- Costa, A.; Oliveira, A. Parental feeding practices and children’s eating behaviors: An overview of their complex relationship. Healthcare 2023, 11, 400. [Google Scholar] [CrossRef]
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The influence of parental dietary behaviors and practices on children’s eating habits. Nutrients 2021, 13, 1138. [Google Scholar] [CrossRef]
- Almaatani, D.; Cory, E.; Gardner, J.; Alexanian-Farr, M.; Hulst, J.M.; Bandsma, R.H.J.; Van Den Heuvel, M. Child and maternal factors associated with feeding practices in children with poor growth. Nutrients 2023, 15, 4850. [Google Scholar] [CrossRef]
- Berge, J.; Hjelmesaeth, J.; Hertel, J.K.; Gjevestad, E.; Småstuen, M.C.; Johnson, L.K.; Martins, C.; Andersen, E.; Helgerud, J.; Støren, Ø. Effect of aerobic exercise intensity on energy expenditure and weight loss in severe obesity-A randomized controlled trial. Obesity 2021, 29, 359–369. [Google Scholar] [CrossRef]
- Shipp, G.M.; Wosu, A.C.; Knapp, E.A.; Sauder, K.A.; Dabelea, D.; Perng, W.; Zhu, Y.; Ferrara, A.; Dunlop, A.L.; Deoni, S.; et al. Maternal pre-pregnancy BMI, breastfeeding, and child BMI. Pediatrics 2024, 153, e2023061466. [Google Scholar] [CrossRef]
- Hu, S.; Wacharasin, C.; Sangin, S. Factors associated with feeding behaviors among mothers of obese infants: A cross-sectional study. Transl. Pediatr. 2023, 12, 1004–1016. [Google Scholar] [CrossRef]
- Singh, S.; Cordeiro, A.; Epel, E.; Coccia, M.; Laraia, B.; Adler, N.; Bush, N. Association between maternal eating and young child feeding in a community sample. BMC Pregnancy Childbirth 2023, 23, 470. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.; Guthrie-Dixon, N.; Tulloch-Reid, M.; Chang, S.; Walker, S. Maternal feeding styles in infancy predict child body mass index z-scores at 72 months: Findings from a cohort of Jamaican children. Front. Public Health 2023, 11, 1161808. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.; Hart, C.N.; Phelan, S.; Ventura, A.; Wing, R.; Jelalian, E. Maternal depressive symptom trajectories and associations with child feeding. BMC Public Health 2024, 24, 1636. [Google Scholar] [CrossRef]
- O’Dea, G.A.; Youssef, G.J.; Hagg, L.J.; Francis, L.M.; Spry, E.A.; Rossen, L.; Smith, I.; Teague, S.J.; Mansour, K.; Booth, A.; et al. Associations between maternal psychological distress and mother-infant bonding: A systematic review and meta-analysis. Arch. Women’s Ment. Health 2023, 26, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Lampard, A.; Franckle, R.; Davison, K. Maternal depression and childhood obesity: A systematic review. Prev. Med. 2014, 59, 60–67. [Google Scholar] [CrossRef]
- Ahmadinezhad, G.S.; Karimi, F.Z.; Abdollahi, M.; NaviPour, E. Association between postpartum depression and breastfeeding self-efficacy in mothers: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2024, 24, 273. [Google Scholar] [CrossRef]
- Shrestha, D.; Bhandari, A.; Ogawa, K.; Tanaka, H.; Miyayama, C.; Horikawa, R.; Urayama, K.Y.; Morisaki, N. Effect of postpartum depression and role of infant feeding practices on relative weight of child at 1 and 3 years of age. BMC Pregnancy Childbirth 2024, 24, 336. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health, Brain Health and Substance Use. 2022. Available online: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/maternal-mental-health (accessed on 16 July 2025).
- Santos, I.S.; Blumenberg, C.; Munhoz, T.N.; Matijasevich, A.; Salum, C.; Santos Júnior, H.G.; Dos Santos, L.M.; Correia, L.L.; de Souza, M.R.; Lira, P.I.C.; et al. Maternal depression and child development at 3 years of age: A longitudinal study in a Brazilian child development promotion program. Pediatr. Res. 2024, 95, 1139–1146. [Google Scholar] [CrossRef]
- Murray, L.; Halligan, S.; Cooper, P. Postnatal Depression and Young Children’s Development. 2019. Available online: https://massaimh.org/wp-content/uploads/2020/02/Chapter10PostnatalDepression.pdf (accessed on 15 July 2025).
- Orovou, E.; Antoniou, E.; Zervas, I.; Sarantaki, A. Prevalence and correlates of postpartum PTSD following emergency cesarean sections: Implications for perinatal mental health care: A systematic review and meta-analysis. BMC Psychol. 2025, 13, 26. [Google Scholar] [CrossRef]
- Brookman, R.; Kalashnikova, M.; Levickis, P.; Conti, J.; Xu Rattanasone, N.; Grant, K.A.; Demuth, K.; Burnham, D. Effects of maternal depression on maternal responsiveness and infants’ expressive language abilities. PLoS ONE 2023, 18, e0277762. [Google Scholar] [CrossRef]
- Nguyen, M.H.; Do, T.X.; Nguyen, T.T.; Pham, M.D.; Pham, T.T.M.; Pham, K.M.; Kim, G.B.; Do, B.N.; Nguyen, H.T.; Nguyen, N.M.; et al. Fear of COVID-19, healthy eating behaviors, and health-related behavior changes as associated with anxiety and depression among medical students: An online survey. Front. Nutr. 2022, 9, 938769. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years—United States, 2018–2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1278–1283. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.L.; Valiauga, R.; Tallo, C.; Hong, C.B.; Manoranjithan, S.; Domingo, C.; Paudel, M.; Untaroiu, A.; Barr, S.; Goldhaber, K. Contributing factors to the rise in adolescent anxiety and associated mental health disorders: A narrative review of current literature. J. Child Adolesc. Psychiatr. Nurs. 2025, 38, e70009. [Google Scholar] [CrossRef] [PubMed]
- Barshay, J. Proof points: Overscheduling kids’ lives causes depression and anxiety, study finds. Covering Innovation & Inequality in Education. 2024. Available online: https://hechingerreport.org/proof-points-overscheduling-kids-lives-causes-depression-and-anxiety-study-finds/ (accessed on 18 July 2025).
- Inchley, J.C.; Stevens, G.W.J.M.; Samdal, O.; Currie, D.B. Enhancing understanding of adolescent health and well-being: The health behaviour in school-aged children study. J. Adolesc. Health 2020, 66, 3–5. [Google Scholar] [CrossRef]
- World Health Organization. Health Promoting Schools. 2018. Available online: https://www.who.int/health-topics/health-promoting-schools#tab=tab_1 (accessed on 18 July 2025).
- Grieshaber, A.; Silver, J.; Bufferd, S.J.; Dougherty, L.; Carlson, G.; Klein, D.N. Early childhood anxiety disorders: Continuity and predictors in adolescence. Eur. Child. Adolesc. 2024, 33, 1817–1825. [Google Scholar] [CrossRef]
- Ramsawh, H.J.; Chavira, D.A. Association of childhood anxiety disorders and quality of life in a primary care sample. J. Dev. Behav. Pediatr. 2016, 37, 269–276. [Google Scholar] [CrossRef]
- European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data (General Data Protection Regulation). Off. J. Eur. Union 2016, 119, 1–88. Available online: http://data.europa.eu/eli/reg/2016/679/oj (accessed on 13 August 2025).
- World Medical Association (WMA). World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Polit, F.D.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2021; ISBN 978-1975110642. [Google Scholar]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th ed.; Sage Publications: Los Angeles, CA, USA, 2017; ISBN 978-1-5063-8670-6. [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2011; Available online: https://iris.who.int/handle/10665/44583 (accessed on 20 July 2025).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Milias, G.A.; Pitsavos, C.; Stefanadis, C. MedDietScore: A computer program that evaluates the adherence to the Mediterranean dietary pattern and its relation to cardiovascular disease risk. Comput. Methods Programs Biomed. 2006, 83, 73–77. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Serra-Majem, L.; Carrasco, J.L.; Roman, B.; Ngo, J.; Bertomeu, I.; Obrador, B. The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: A review. Public Health Nutr. 2006, 9, 132–146. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual for the Beck Depression Inventory-II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Fountoulakis, K.; Iacovides, A.; Kleanthous, S.; Samolis, S.; Kaprinis, S.G.; Sitzoglou, K.; Kaprinis, S.G.; Bech, P. Reliability, validity and psychometric properties of the Greek translation of the Center for Epidemiological Studies-Depression (CES-D) Scale. BMC Psychiatry 2001, 1, 3. [Google Scholar] [CrossRef]
- Wang, Y.P.; Gorenstein, C. Psychometric properties of the Beck Depression Inventory-II: A comprehensive review. Rev. Bras. Psiquiatr. 2013, 35, 416–431. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Iacovides, A.; Kleanthous, S.; Samolis, S.; Gougoulias, K.; Tsiptsios, I.; Kaprinis, G.S.; Bech, P. Reliability, validity and psychometric properties of the Greek translation of the Major Depression Inventory. BMC Psychiatry 2003, 3, 2. [Google Scholar] [CrossRef]
- Marteau, T.M.; Bekker, H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Julian, L.J. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011, 63 (Suppl. S11), 467–472. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Edwards, C.D.; Lushene, R.E.; Montuori, J.; Platzek, D. The State-Trait Anxiety Inventory for Children (Preliminary Manual); Consulting Psychologists Press: Palo Alto, CA, USA, 1973. [Google Scholar]
- Psychountaki, M.; Zervas, Y.; Karteroliotis, K.; Spielberger, C. Reliability and validity of the Greek version of the STAIC. Eur. J. Psychol. Assess. 2003, 19, 124–130. [Google Scholar] [CrossRef]
- Shai, L.; Pao, M.; Tipton, M.; Bedoya, S.Z.; Kang, S.; Horowitz, L.; Wiener, L. Comparing parent and child self-report measures of the State-Trait Anxiety Inventory in children and adolescents with a chronic health condition. J. Clin. Psychol. Med. Setting 2020, 27, 173–181. [Google Scholar] [CrossRef]
- Nilsson, S.; Buchholz, M.; Thunberg, G. Assessing children’s anxiety using the modified short State-Trait Anxiety and Talking Mats: A pilot study. Nurs. Res. Pract. 2012, 2012, 932570. [Google Scholar] [CrossRef] [PubMed]
- De Los Reyes, A.; Kazdin, A.E. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychol. Bull. 2005, 131, 483–509. [Google Scholar] [CrossRef]
- Greene, J.W.; Walker, L.S. Pain and stress in children: A developmental approach. In Handbook of Pediatric Psychology, 5th ed.; Roberts, M.C., Steele, R.G., Eds.; Guilford Press: New York, NY, USA, 2021; pp. 123–138. ISBN 9781462536085. [Google Scholar]
- World Health Organization. WHO Guidelines on Ethical Issues in Public Health Surveillance; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/who-guidelines-on-ethical-issues-in-public-health-surveillance (accessed on 20 July 2025).
- Digitale, J.C.; Martin, J.N.; Glymour, M.M. Tutorial on directed acyclic graphs. J. Clin. Epidemiol. 2022, 142, 264–267. [Google Scholar] [CrossRef]
- Whitaker, R.C. Predicting preschooler obesity at birth: The role of maternal obesity in early pregnancy. Pediatrics 2004, 114, e29–e36. [Google Scholar] [CrossRef]
- Sekine, M.; Yamagami, T.; Hamanishi, S.; Handa, K.; Saito, T.; Nanri, S.; Kawaminami, K.; Tokui, N.; Yoshida, K.; Kagamimori, S. Parental obesity, lifestyle factors and obesity in preschool children: Results of the Toyama Birth Cohort study. J. Epidemiol. 2002, 12, 33–39. [Google Scholar] [CrossRef]
- Voerman, E.; Santos, S.; Patro Golab, B.; Amiano, P.; Ballester, F.; Barros, H.; Bergström, A.; Charles, M.A.; Chatzi, L.; Chevrier, C.; et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLoS Med. 2019, 16, e1002744. [Google Scholar] [CrossRef]
- Hughes, A.R.; Sherriff, A.; Lawlor, D.A.; Ness, A.R.; Reilly, J.J. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev. Med. 2011, 52, 300–304. [Google Scholar] [CrossRef]
- Mao, A.; Yang, S.-Q.; Luo, Y.-J.; Ren, Y.; Yan, X.; Qiu, Y.-R.; Yang, X. Long-term impact of maternal pre-pregnancy BMI on the risk of overweight/obesity in preschool children: Mediation by infant birth weight and BMI trajectory group from 0 to 2 years. BMC Public Health 2024, 24, 3404. [Google Scholar] [CrossRef] [PubMed]
- Hudson, P.; Emmett, P.M.; Taylor, C.M. Pre-pregnancy maternal BMI classification is associated with preschool childhood diet quality and childhood obesity in the Avon Longitudinal Study of Parents and Children. Public Health Nutr. 2021, 24, 6137–6144. [Google Scholar] [CrossRef]
- Liang, J.J.; Hu, Y.; Xing, Y.F.; Ma, Y.; Jiang, L.; Liu, H.Y.; Hu, F.; Lu, S.M.; Lin, S.F. Association between both maternal pre-pregnancy body mass index/ gestational weight gain and overweight/obesity children at preschool stage. Zhonghua Liu Xing Xue Za Zhi 2019, 40, 976–981. [Google Scholar] [CrossRef]
- Risvas, G.; Papaioannou, I.; Panagiotakos, D.B.; Farajian, P.; Bountziouka, V.; Zampelas, A. Perinatal and family factors associated with preadolescence overweight/obesity in Greece: The GRECO study. J. Epidemiol. Glob. Health 2012, 2, 145–153. [Google Scholar] [CrossRef]
- Nguyen, G.; Hayes, L.; Ngongalah, L.; Bigirumurame, T.; Gaudet, L.; Odeniyi, A.; Flynn, A.; Crowe, L.; Skidmore, B.; Simon, A.; et al. Association between maternal adiposity measures and infant health outcomes: A systematic review and meta-analysis. Obes. Rev. 2022, 23, e13491. [Google Scholar] [CrossRef] [PubMed]
- Salem, W.; Adler, A.I.; Lee, C.; Smith, G.C. Maternal waist to hip ratio is a risk factor for macrosomia. BJOG 2012, 119, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Hirschler, V.; Roque, M.I.; Calcagno, M.L.; Gonzalez, C.; Aranda, C. Maternal waist circumference and the prediction of children’s metabolic syndrome. Arch. Pediatr. Adolesc. Med. 2007, 161, 1205–1210. [Google Scholar] [CrossRef]
- Soares, M.M.; Juvanhol, L.L.; Ribeiro, A.Q.; Pereira, P.F.; Franceschini, S.; Amaral Araújo, R.M. Maternal overweight and its relation with child’s anthropometric indices. Rev. Bras. Saúde Materno Infant. 2021, 21, 379–388. [Google Scholar] [CrossRef]
- Hunt, K.J.; Ferguson, P.L.; Neelon, B.; Commodore, S.; Bloom, M.S.; Sciscione, A.C.; Grobman, W.A.; Kominiarek, M.A.; Newman, R.B.; Tita, A.T.; et al. The association between maternal pre-pregnancy BMI, gestational weight gain and child adiposity: A racial-ethnically diverse cohort of children. Pediatr. Obes. 2022, 17, e12911. [Google Scholar] [CrossRef]
- Lu, W.; Zhang, X.; Wu, J.; Mao, X.; Shen, X.; Chen, Q.; Zhang, J.; Huang, L.; Tang, Q. Association between trimester-specific gestational weight gain and childhood obesity at 5 years of age: Results from Shanghai obesity cohort. BMC Pediatr. 2019, 19, 139. [Google Scholar] [CrossRef]
- Kaar, J.L.; Crume, T.; Brinton, J.T.; Bischoff, K.J.; McDuffie, R.; Dabelea, D. Maternal obesity, gestational weight gain, and offspring adiposity: The exploring perinatal outcomes among children study. J. Pediatr. 2014, 165, 509–515. [Google Scholar] [CrossRef]
- Hohwü, L.; Zhu, J.L.; Graversen, L.; Li, J.; Sørensen, T.I.; Obel, C. Prenatal parental separation and body weight, including development of overweight and obesity later in childhood. PLoS ONE 2015, 10, e0119138. [Google Scholar] [CrossRef]
- Biehl, A.; Hovengen, R.; Grøholt, E.K.; Hjelmesæth, J.; Strand, B.H.; Meyer, H.E. Parental marital status and childhood overweight and obesity in Norway: A nationally representative cross-sectional study. BMJ Open 2014, 4, e004502. [Google Scholar] [CrossRef] [PubMed]
- Luscombe, B. Boys of Divorced Parents Twice as Likely to be Obese. TIME. 4 June 2014. Available online: https://time.com/2822082/divorce-obese-kids-boys-overweight/ (accessed on 2 August 2025).
- Chen, A.Y.; Escarce, J.J. Family structure and childhood obesity, Early Childhood Longitudinal Study—Kindergarten Cohort. Prev. Chronic Dis. 2010, 7, A50. [Google Scholar] [PubMed]
- Schmeer, K.K. Family structure and obesity in early childhood. Soc. Sci. Res. 2012, 41, 820–832. [Google Scholar] [CrossRef]
- Yannakoulia, M.; Papanikolaou, K.; Hatzopoulou, I.; Efstathiou, E.; Papoutsakis, C.; Dedoussis, G.V. Association between family divorce and children’s BMI and meal patterns: The GENDAI Study. Obesity 2008, 16, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Charach, A.; Mohammadzadeh, F.; Belanger, S.A.; Easson, A.; Lipman, E.L.; McLennan, J.D.; Parkin, P.; Szatmari, P. Identification of preschool children with mental health problems in primary care: Systematic review and meta-analysis. J. Can. Acad. Child Adolesc. Psychiatry 2020, 29, 76–105. [Google Scholar]
- Goodman, S.H.; Rouse, M.H.; Connell, A.M.; Broth, M.R.; Hall, C.M.; Heyward, D. Maternal depression and child psychopathology: A meta-analytic review. Clin. Child Fam. Psychol. Rev. 2011, 14, 1–27. [Google Scholar] [CrossRef]
- Morgan, J.E.; Channon, S.; Penny, H.; Waters, C.S. Longitudinal studies examining the impact of prenatal and subsequent episodes of maternal depression on offspring antisocial behaviour. Eur. Child Adolesc. Psychiatry 2021, 30, 5–40. [Google Scholar] [CrossRef]
- Elgar, F.J.; McGrath, P.J.; Waschbusch, D.A.; Stewart, S.H.; Curtis, L.J. Mutual influences on maternal depression and child adjustment problems. Clin. Psychol. Rev. 2004, 24, 441–459. [Google Scholar] [CrossRef]
- Aktar, E.; Majdandžić, M.; De Vente, W.; Bögels, S.M. Parental expressions of anxiety and child temperament in toddlerhood jointly predict preschoolers’ avoidance of novelty. J. Clin. Child Adolesc. Psychol. 2017, 47, S421–S434. [Google Scholar] [CrossRef]
- Madigan, S.; Oatley, H.; Racine, N.; Fearon, R.M.P.; Schumacher, L.; Akbari, E.; Cooke, J.E.; Tarabulsy, G.M. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 645–657.e8. [Google Scholar] [CrossRef]

| Independent Maternal Variables | N | Category A: BMI—Underweight Children | Category B: BMI—Children with Normal Weight | Category C: BMI—Overweight & Obese Children | p | |
|---|---|---|---|---|---|---|
| Age | 23–34 years old | 46 | 4 (8.7%) | 33 (71.7%) | 9 (19.6%) | 0.486 |
| 35–42 years old | 122 | 24 (19.7%) | 80 (65.6%) | 18 (14.8%) | ||
| 43+ years old | 32 | 5 (15.6%) | 23 (71.9%) | 4 (12.5%) | ||
| Permanent residence | Urban | 29 | 5 (17.2%) | 19 (65.5%) | 5 (17.2%) | 0.947 |
| Rural | 171 | 28 (16.4%) | 117 (68.4%) | 26 (15.2%) | ||
| Nationality | Greek | 191 | 33 (17.3%) | 128 (67%) | 30 (15.7%) | 0.320 |
| Non-Greek | 9 | 0 (0%) | 8 (88.9%) | 1 (11.1%) | ||
| Number of children | 1–2 children | 159 | 25 (15.7%) | 109 (68.6%) | 25 (15.7%) | 0.435 |
| 3–4 children | 34 | 5 (14.7%) | 24 (70.6%) | 5 (14.7%) | ||
| 5+ children | 7 | 3 (42.9%) | 3 (42.9%) | 1 (14.3%) | ||
| Weight | 44–60 kg | 72 | 9 (12.5%) | 57 (79.2%) | 6 (8.3%) | 0.013 |
| 61–75 kg | 76 | 18 (23.7%) | 47 (61.8%) | 11 (14.5%) | ||
| 75+ kg | 52 | 6 (11.5%) | 32 (61.5%) | 14 (26.9%) | ||
| Height | 1.50–1.60 m | 60 | 10 (16.7%) | 41 (68.3%) | 9 (15%) | 0.133 |
| 1.61–1.70 m | 111 | 18 (16.2%) | 71 (64%) | 22 (19.8%) | ||
| 1.71+ m | 29 | 5 (17.2%) | 24 (82.8%) | 0 (0%) | ||
| BMI | Normal weight | 115 | 21 (18.3%) | 83 (72.2%) | 11 (9.6%) | 0.009 |
| Overweight | 55 | 9 (16.4%) | 37 (67.3%) | 9 (16.4%) | ||
| Obesity | 30 | 3 (10%) | 16 (53.3%) | 11 (36.7%) | ||
| Waist circumference | 60–75 cm | 57 | 6 (10.5%) | 46 (80.7%) | 5 (8.8%) | 0.032 |
| 76–90 cm | 85 | 18 (21.2%) | 56 (65.9%) | 11 (12.9%) | ||
| 91+ cm | 58 | 9 (15.5%) | 34 (58.6%) | 15 (25.9%) | ||
| Hip circumference | 70–95 cm | 56 | 8 (14.3%) | 41 (73.2%) | 7 (12.5%) | 0.031 |
| 96–110 cm | 111 | 19 (17.1%) | 79 (71.2%) | 13 (11.7%) | ||
| 111+ cm | 33 | 6 (18.2%) | 16 (48.5%) | 11 (33.3%) | ||
| WHR | ≥0.75 | 35 | 5 (14.3%) | 28 (80%) | 2 (5.7%) | 0.061 |
| 0.76–0.85 | 111 | 22 (19.8%) | 74 (66.7%) | 15 (13.5%) | ||
| 0.86+ | 54 | 6 (11.1%) | 34 (63%) | 14 (25.9%) | ||
| Pre-pregnancy weight | 44–55 kg | 60 | 8 (13.3%) | 46 (76.7%) | 6 (10%) | 0.052 |
| 56–70 kg | 104 | 23 (22.1%) | 65 (62.5%) | 16 (15.4%) | ||
| 71+ kg | 36 | 2 (5.6%) | 25 (69.4%) | 9 (25%) | ||
| Weight before delivery | 50–65 kg | 47 | 4 (8.5%) | 38 (80.9%) | 5 (10.6%) | 0.176 |
| 66–80 kg | 96 | 20 (20.8%) | 62 (64.6%) | 14 (14.6%) | ||
| 81+ kg | 57 | 9 (15.8%) | 36 (63.2%) | 12 (21.1%) | ||
| Frequency of exercise/week | None | 75 | 13 (17.3%) | 48 (64%) | 14 (18.7%) | 0.409 |
| A little | 67 | 12 (17.9%) | 43 (64.2%) | 12 (17.9%) | ||
| Often | 58 | 8 (13.8%) | 45 (77.6%) | 5 (8.6%) | ||
| Smoking | Yes | 41 | 6 (14.6%) | 31 (75.6%) | 4 (9.8%) | 0.439 |
| No | 159 | 27 (17%) | 105 (66%) | 27 (17%) | ||
| Illness | Yes | 39 | 2 (5.1%) | 29 (74.4%) | 8 (20.5%) | 0.088 |
| No | 161 | 31 (19.3%) | 107 (66.5%) | 23 (14.3%) | ||
| Medication use | Yes | 33 | 3 (9.1%) | 22 (66.7%) | 8 (24.2%) | 0.073 |
| No | 167 | 30 (18%) | 114 (68.3%) | 23 (13.8%) | ||
| Diet (type) | Non-specific diet | 191 | 33 (17.3%) | 127 (66.5%) | 31 (16.2%) | 0.109 |
| Special diet | 9 | 0 (0%) | 9 (100%) | 0 (0%) | ||
| Marital status | Single | 5 | 0 (0%) | 5 (100%) | 0 (0%) | 0.017 |
| Married | 188 | 32 (17%) | 129 (68.6%) | 27 (14.4%) | ||
| Divorced | 7 | 1 (14.3%) | 2 (28.6%) | 4 (57.1%) | ||
| Economic status | Low | 82 | 15 (18.3%) | 53 (64.6%) | 14 (17.1%) | 0.837 |
| Medium | 105 | 15 (14.3%) | 75 (71.4%) | 15 (14.3%) | ||
| High | 13 | 3 (23.1%) | 8 (61.5%) | 2 (15.4%) | ||
| Occupation | Unemployed | 37 | 8 (21.6%) | 25 (67.6%) | 4 (10.8%) | 0.507 |
| Employed | 162 | 25 (15.4%) | 110 (67.9%) | 27 (16.7%) | ||
| Educational level | Low | 5 | 2 (40%) | 2 (40%) | 1 (20%) | 0.654 |
| Medium | 60 | 9 (15%) | 42 (70%) | 9 (15%) | ||
| High | 135 | 22 (16.3%) | 92 (68.1%) | 21 (15.6%) | ||
| MedDietScore | Low adherence | 54 | 7 (13%) | 37 (68.5%) | 10 (18.5%) | 0.607 |
| High adherence | 146 | 26 (17.8%) | 99 (67.8%) | 21 (14.4%) | ||
| Depressive symptomatology (BDI-II) | Minimal depressive symptoms | 156 | 26 (16.7%) | 107 (68.6%) | 23 (14.7%) | 0.856 |
| Depressive symptoms | 44 | 7 (15.9%) | 29 (65.9%) | 8 (18.2%) | ||
| Anxiety (STAI-6) | Normal level | 99 | 17 (17.2%) | 64 (64.2%) | 18 (18.2%) | 0.525 |
| High level | 10 | 16 (15.8%) | 72 (71.3%) | 13 (12.9%) | ||
| Child dietary counseling | Yes | 25 | 3 (12%) | 17 (68%) | 5 (20%) | 0.696 |
| No | 175 | 30 (17.1%) | 119 (68%) | 31 (15.5%) |
| Maternal Variables | N | Category/Mean Value | Anxiety (Median [IQR]) | No Anxiety (Median [IQR]) | p-Value |
|---|---|---|---|---|---|
| Age | 200 | 38.02 | 38 [6.75] | 38 [4] | 0.213 |
| Place of residence | Urban (Ν = 29) | 1:Urban / 2:Rural | 2 [0] | 2 [0] | 0.616 |
| Rural (Ν = 171) | |||||
| Nationality | Greek (Ν = 191) | 1:Greek / 2:Other | 1 [0] | 1 [0] | 0.248 |
| Other (Ν = 9) | |||||
| Number of children | 200 | 2.03 | 2 [1] | 2 [1] | 0.356 |
| Weight (kg) | 200 | 67.56 | 65 [19.75] | 64.75 [16] | 0.771 |
| Height (cm) | 200 | 164.81 | 165 [10] | 165 [8] | 0.199 |
| ΒΜΙ | 200 | 24.87 | 23.98 [6.13] | 23.77 [6.14] | 0.857 |
| Waist circumference | 200 | 84.48 | 80.5 [17] | 80 [19.75] | 0.833 |
| Hip circumference | 200 | 102.53 | 100 [12.75] | 100.5 [14.5] | 0.865 |
| WHR | 200 | 4,95 | 0.82 [0.093] | 0.80 [0.08] | 0.462 |
| Pre-pregnancy weight | 200 | 62.55 | 60 [14.75] | 58.5 [10] | 0.286 |
| Weight before delivery | 200 | 75.36 | 74 [17.25] | 72 [16.5] | 0.181 |
| GWG | 200 | 12.81 | 13 [7.25] | 10 [8.5] | 0.074 |
| Exercise frequency/per week | 200 | 1.64 | 2 [3] | 1 [2] | 0.937 |
| Smoking status | Yes (Ν = 41) | 1:Yes / 2:No | 2 [0] | 2 [0] | 0.333 |
| No (Ν = 159) | |||||
| Illness | Yes (Ν = 39) | 1:Yes / 2:No | 2 [0] | 2 [0] | 0.668 |
| No (Ν = 161) | |||||
| Medication use | Yes (Ν = 33) | 1:Yes / 2:No | 2 [0] | 2 [0] | 0.747 |
| No (Ν = 167) | |||||
| Diet type | Non-specific diet (Ν = 191) | 1:Non-specific / 2: Special diet | 1 [0] | 1 [0] | 0.261 |
| Special diet (Ν = 9) | |||||
| Marital status | Single (Ν = 5) | 1: Single / 2: Married /3: Divorced | 2 [0] | 2 [0] | 0.271 |
| Married (Ν = 188) | |||||
| Divorced (Ν = 7) | |||||
| Economic status | Low (Ν = 82) | 1:Low / 2:Medium / 3:High | 2 [1] | 2 [1] | 0.430 |
| Medium (Ν = 105) | |||||
| High (Ν = 13) | |||||
| Employment status | Unemployed (Ν = 37) | 0: Unemployed / 1: Employed | 1 [0] | 1 [0] | 0.328 |
| Employed (Ν = 162) | |||||
| Educational level | Low (Ν = 5) | 1:Low / 2:Medium/3: High | 3 [1] | 3 [1] | 0.921 |
| Medium (Ν = 60) | |||||
| High (Ν = 135) | |||||
| MedDietScore | Low compliance (Ν = 54) | 1: Low / 2: High compliance | 2 [1] | 2 [1] | 0.505 |
| High compliance (Ν = 146) | |||||
| Depressive symptomatology (BDI) | Minimal symptoms (Ν = 156) | Minimal symptoms / 2: Depressive symptoms | 1 [0] | 1 [1] | <0.001 |
| Depressive symptoms (Ν = 44) | |||||
| Anxiety (STAI-6) | Normal (Ν = 99) | 1:Normal / 2:High level | 2 [0] | 1 [1] | <0.001 |
| High level (Ν = 10) | |||||
| Child dietary counseling | Yes (Ν = 25) | 1:Yes / 2:No | 2 [0] | 2 [0] | 1 |
| No (Ν = 175) |
| Maternal Variables | B | Odds Ratio (OR) | 95%CI | p-Value | N |
|---|---|---|---|---|---|
| Constant | −4.017 | 0.000 | 200 | ||
| Pre-pregnancy weight | −0.376 | 0.687 | 0.392–1.202 | 0.189 | 200 |
| Depressive symptoms (BDI) | 0.998 | 2.712 | 1.222–6.020 | 0.014 | 200 |
| Anxiety (STAI-6) | 1.676 | 5.346 | 2.471–11.565 | 0.000 | 200 |
| Height | 0.225 | 1.253 | 0.705–2.226 | 0.442 | 200 |
| GWG | –0.041 | 0.960 | 0.908–1.014 | 0.145 | 200 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelakou, E.-P.; Spyrilioti, A.; Tsiakara, M.; Vasilakaki, M.; Giaginis, C. Association of Maternal Sociodemographic, Anthropometric, and Lifestyle Factors with Childhood Anthropometric Measures and Anxiety Symptoms: A Nationally Representative Cross-Sectional Study of Preschool-Aged Children in Greece. Diseases 2025, 13, 327. https://doi.org/10.3390/diseases13100327
Angelakou E-P, Spyrilioti A, Tsiakara M, Vasilakaki M, Giaginis C. Association of Maternal Sociodemographic, Anthropometric, and Lifestyle Factors with Childhood Anthropometric Measures and Anxiety Symptoms: A Nationally Representative Cross-Sectional Study of Preschool-Aged Children in Greece. Diseases. 2025; 13(10):327. https://doi.org/10.3390/diseases13100327
Chicago/Turabian StyleAngelakou, Exakousti-Petroula, Athina Spyrilioti, Maria Tsiakara, Maria Vasilakaki, and Constantinos Giaginis. 2025. "Association of Maternal Sociodemographic, Anthropometric, and Lifestyle Factors with Childhood Anthropometric Measures and Anxiety Symptoms: A Nationally Representative Cross-Sectional Study of Preschool-Aged Children in Greece" Diseases 13, no. 10: 327. https://doi.org/10.3390/diseases13100327
APA StyleAngelakou, E.-P., Spyrilioti, A., Tsiakara, M., Vasilakaki, M., & Giaginis, C. (2025). Association of Maternal Sociodemographic, Anthropometric, and Lifestyle Factors with Childhood Anthropometric Measures and Anxiety Symptoms: A Nationally Representative Cross-Sectional Study of Preschool-Aged Children in Greece. Diseases, 13(10), 327. https://doi.org/10.3390/diseases13100327







