Demographic Profiles, Etiological Spectrum, and Anatomical Locations of the Post-Hepatic Obstructive Jaundice in Adult Population in Hadhramout Region in Yemen
Abstract
1. Introduction:
2. Materials and Methods
2.1. Study Design
2.2. Sample Size
2.3. Inclusion Criteria
2.4. Exclusion Criteria
- Patients with jaundice caused by pre-hepatic factors.
- Patients with obstructive jaundice caused by hepatic factors.
- Patients in whom the causes of obstructive jaundice were not definitively determined by ERCP (n = 88).
2.5. Data Acquisition
2.5.1. Ultrasound Imaging Procedure
2.5.2. ERCP Technique
2.6. Statistical Analysis
3. Results
3.1. Demographic Data
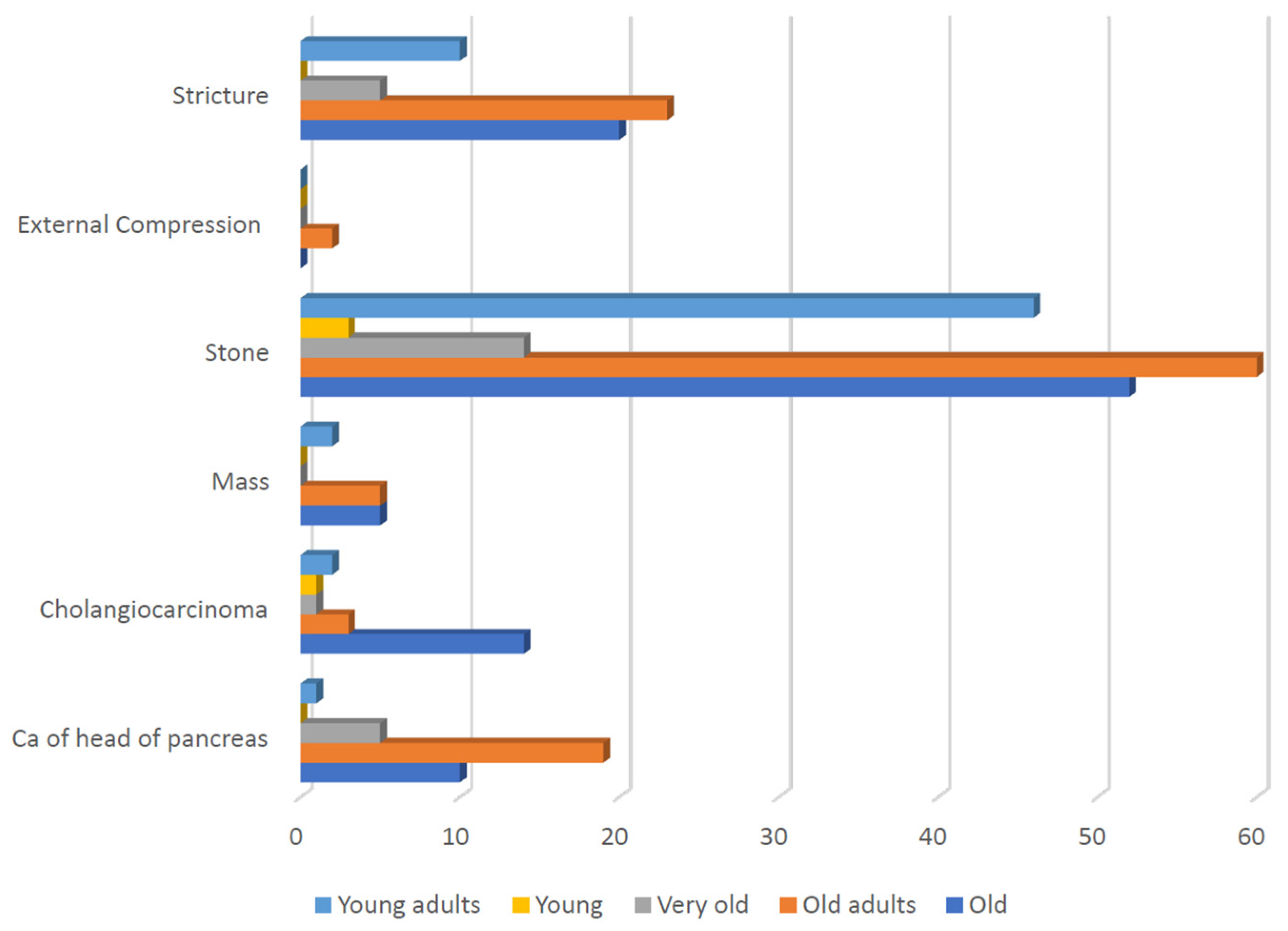
3.2. Etiological Data
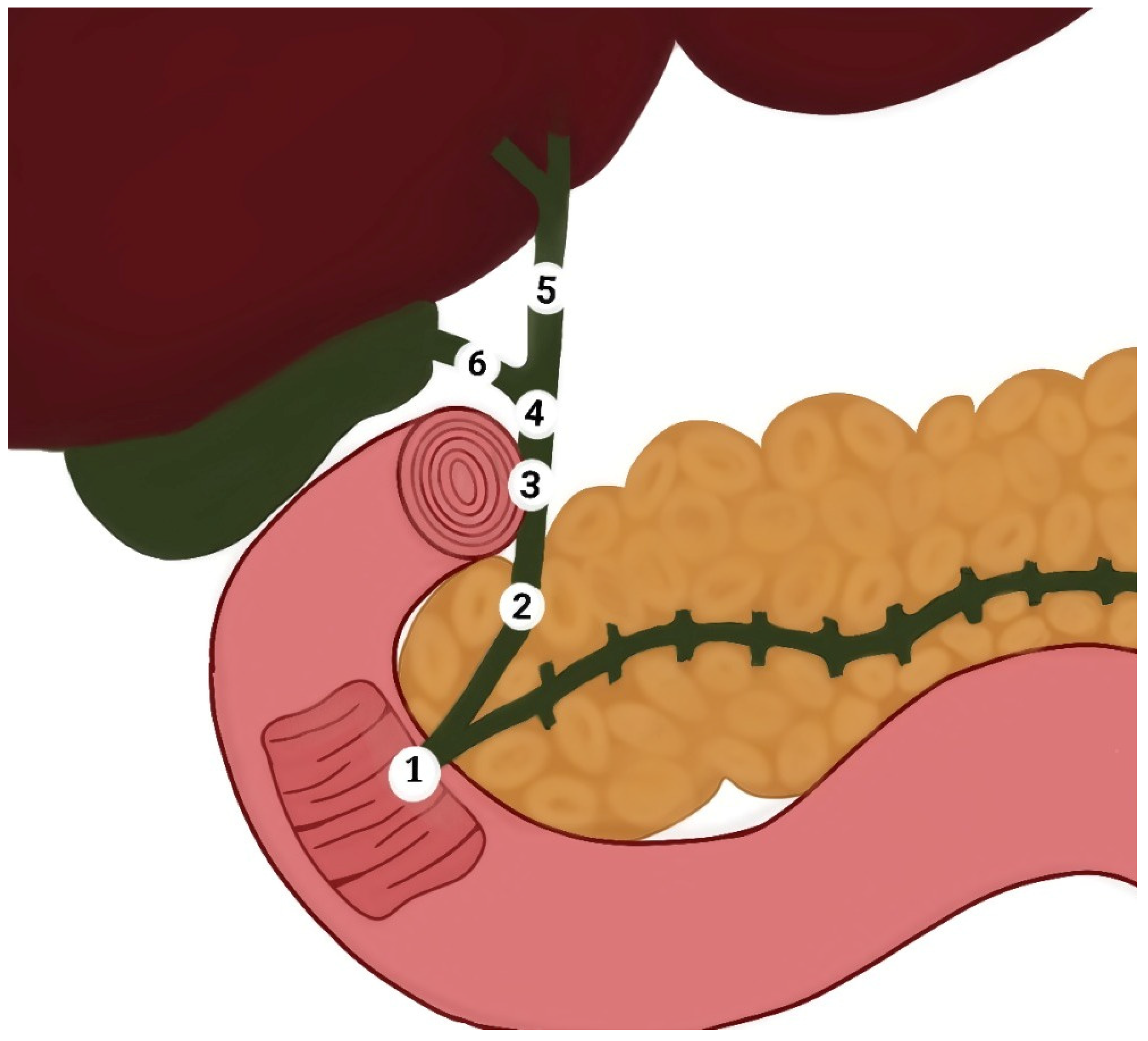
3.3. Anatomical Locations Data
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joseph, A.; Samant, H. Jaundice. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Chee, Y.Y.; Chung, P.H.; Wong, R.M.; Wong, K.K. Jaundice in infants and children: Causes, diagnosis, and management. Hong Kong Med. J. 2018, 24, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Pavlovic Markovic, A.; Stojkovic Lalosevic, M.; Mijac, D.D.; Milovanovic, T.; Dragasevic, S.; Sokic Milutinovic, A.; Krstic, M.N. Jaundice as a Diagnostic and Therapeutic Problem: A General Practitioner’s Approach. Dig. Dis. 2022, 40, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; John, S. Cholestatic Jaundice. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Bhutia, K.D.; Lachungpa, T.; Lamtha, S.C. Etiology of obstructive jaundice and its correlation with the ethnic population of Sikkim. J. Family Med. Prim. Care 2021, 10, 4189–4192. [Google Scholar] [CrossRef] [PubMed]
- Freitas, M.L.; Bell, R.L.; Duffy, A.J. Choledocholithiasis: Evolving standards for diagnosis and management. World J. Gastroenterol. 2006, 12, 3162–3167. [Google Scholar] [CrossRef]
- Alsaedi, H.I.; Krsoom, A.M.; Alshoabi, S.A.; Alsharif, W.M. Investigation Study of Ultrasound Practitioners’ Awareness about Artefacts of Hepatobiliary Imaging in Almadinah Almunawwarah. Pak. J. Med. Sci. 2022, 38, 1526–1533. [Google Scholar] [CrossRef]
- van Sonnenberg, E.; Panchanathan, R. Percutaneous Transcholecystic Management of Choledocholithiasis: A Next Horizon for Interventional Radiologists? Radiology 2019, 290, 244–245. [Google Scholar] [CrossRef]
- Zhang, W.G.; Chai, N.L.; Zhang, B.; Li, X.; Wang, J.F.; Dong, H.; Feng, Y.J.; Linghu, E.Q. Cholangioscopy-assisted extraction through novel papillary support for small-calibre and sediment-like common bile duct stones. World J. Gastroenterol. 2023, 29, 2495–2501. [Google Scholar] [CrossRef]
- Liu, J.J.; Sun, Y.M.; Xu, Y.; Mei, H.W.; Guo, W.; Li, Z.L. Pathophysiological consequences and treatment strategy of obstructive jaundice. World J. Gastrointest. Surg. 2023, 15, 1262–1276. [Google Scholar] [CrossRef]
- Jacob, J.S.; Lee, M.E.; Chew, E.Y.; Thrift, A.P.; Sealock, R.J. Evaluating the Revised American Society for Gastrointestinal Endoscopy Guidelines for Common Bile Duct Stone Diagnosis. Clin. Endosc. 2021, 54, 269–274. [Google Scholar] [CrossRef]
- Azimaraghi, O.; Bilal, M.; Amornyotin, S.; Arain, M.; Behrends, M.; Berzin, T.M.; Buxbaum, J.L.; Choice, C.; Fassbender, P.; Sawhney, M.S.; et al. Consensus guidelines for the perioperative management of patients undergoing endoscopic retrograde cholangiopancreatography. Br. J. Anaesth. 2023, 130, 763–772. [Google Scholar] [CrossRef]
- Chalya, P.L.; Kanumba, E.S.; McHembe, M. Etiological spectrum and treatment outcome of Obstructive jaundice at a University teaching Hospital in northwestern Tanzania: A diagnostic and therapeutic challenges. BMC Res. Notes 2011, 4, 147. [Google Scholar] [CrossRef] [PubMed]
- Gameraddin, M.; Omer, S.; Salih, S.; Elsayed, S.; Alshaikh, A. Sonographic Evaluation of Obstructive Jaundice. Open J. Med. Imaging 2015, 5, 24–29. [Google Scholar] [CrossRef]
- Shukla, S.; Kharat, P.R.; Patbamniya, N.; Kumar, K. Clinicopathological study on patients presenting with obstructive jaundice. Int. Surg. J. 2018, 5, 705–710. [Google Scholar] [CrossRef]
- Coucke, E.M.; Akbar, H.; Kahloon, A.; Lopez, P.P. Biliary Obstruction. In StatPearls [Internet]; StatPearls Publishing: Treasure Island FL, USA, 2022. [Google Scholar] [PubMed]
- Khan, Z.A. Clinical profile of patients with obstructive jaundice: A surgeon’s perspectives. Int. Surg. J. 2019, 6, 1876–1880. [Google Scholar] [CrossRef]
- Hasan, M.S. Factors Affecting Morbidity and Mortality after ERCP for Obstructive Jaundice. Mymensingh Med. J. 2021, 30, 523–530. [Google Scholar]
- Hu, K.C.; Chu, C.H.; Wang, H.Y.; Chang, W.H.; Lin, S.C.; Liu, C.C.; Liao, W.C.; Liu, C.J.; Wu, M.S.; Shih, S.C. How Does Aging Affect Presentation and Management of Biliary Stones? J. Am. Geriatr. Soc. 2016, 64, 2330–2335. [Google Scholar] [CrossRef]
- Aljahdli, E.S. Management of distal malignant biliary obstruction. Saudi J. Gastroenterol. 2018, 24, 71–72. [Google Scholar] [CrossRef]
- Singh, A.; Gelrud, A.; Agarwal, B. Biliary strictures: Diagnostic considerations and approach. Gastroenterol. Rep. 2015, 3, 22–31. [Google Scholar] [CrossRef]
- Shen, Z.; Tian, L.; Wang, X. Treatment of pancreatic head cancer with obstructive jaundice by endoscopy ultrasonography-guided gastrojejunostomy: A case report and literature review. Medicine 2018, 97, e11476. [Google Scholar] [CrossRef]
- Bornman, P.C.; Beckingham, I.J. ABC of diseases of liver, pancreas, and biliary system. Pancreatic tumours. BMJ 2001, 322, 721–723. [Google Scholar] [CrossRef]
- Ledenko, M.; Antwi, S.O.; Arima, S.; Driscoll, J.; Furuse, J.; Klümpen, H.J.; Larsen, F.O.; Lau, D.K.; Maderer, A.; Markussen, A.; et al. Sex-related disparities in outcomes of cholangiocarcinoma patients in treatment trials. Front. Oncol. 2022, 12, 963753. [Google Scholar] [CrossRef] [PubMed]
- Guedj, N. Pathology of Cholangiocarcinomas. Curr. Oncol. 2022, 30, 370–380. [Google Scholar] [CrossRef]
- Tazuma, S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best. Pract. Res. Clin. Gastroenterol. 2006, 20, 1075–1083. [Google Scholar] [CrossRef] [PubMed]
- Jesani, S.; Romero, A.L.; Bozkurt, S.B.; Abu Samak, A.A.; Romero, J.; Sookdeo, J.; Naik, A. Mirizzi Syndrome: An Unusual Complication of Cholelithiasis. J. Community Hosp. Intern. Med. Perspect. 2022, 12, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Shi, X.; Shan, H.; Xiao, D.; Wang, X.; Wang, F. Treatment of obstructive jaundice induced by non-hodgkin lymphoma with EUS-guided transgastric anterograde common bile duct stenting: Technical case report and literature review. Front. Surg. 2023, 9, 1031718. [Google Scholar] [CrossRef]
- Julianov, A.; Georgiev, Y. Hepatic artery aneurysm causing obstructive jaundice. Quant. Imaging Med. Surg. 2014, 4, 294–295. [Google Scholar] [CrossRef]
- Yin, T.; Wan, Z.; Chen, H.; Mao, X.; Yi, Y.; Li, D. Obstructive jaundice caused by pancreaticoduodenal artery aneurysms associated with celiac axis stenosis: Case report and review of the literature. Ann. Vasc. Surg. 2015, 29, 1016.e1–1016.e6. [Google Scholar] [CrossRef]
- Gebreselassie, A.; Bukhari, M.; Khashab, M. Recurrent Biliary Obstruction Secondary to Portal Vein Thrombosis with Cavernous Transformation and the Role of Cholangioscopy in Diagnosis: Case Report: 1301. Am. J. Gastroenterol. 2017, 112, S707. [Google Scholar] [CrossRef]
- Hoang, H.; Norris, T. A Twisted Case of Jaundice. Cureus 2020, 12, e6683. [Google Scholar] [CrossRef]
- Alexandre, K.; Hassan, O.; Hebden, J.; Barnwell, J.M. Cocaine Induced Biliary Tree Obstruction in a Middle-Aged Male. Cureus 2021, 13, e20458. [Google Scholar] [CrossRef]

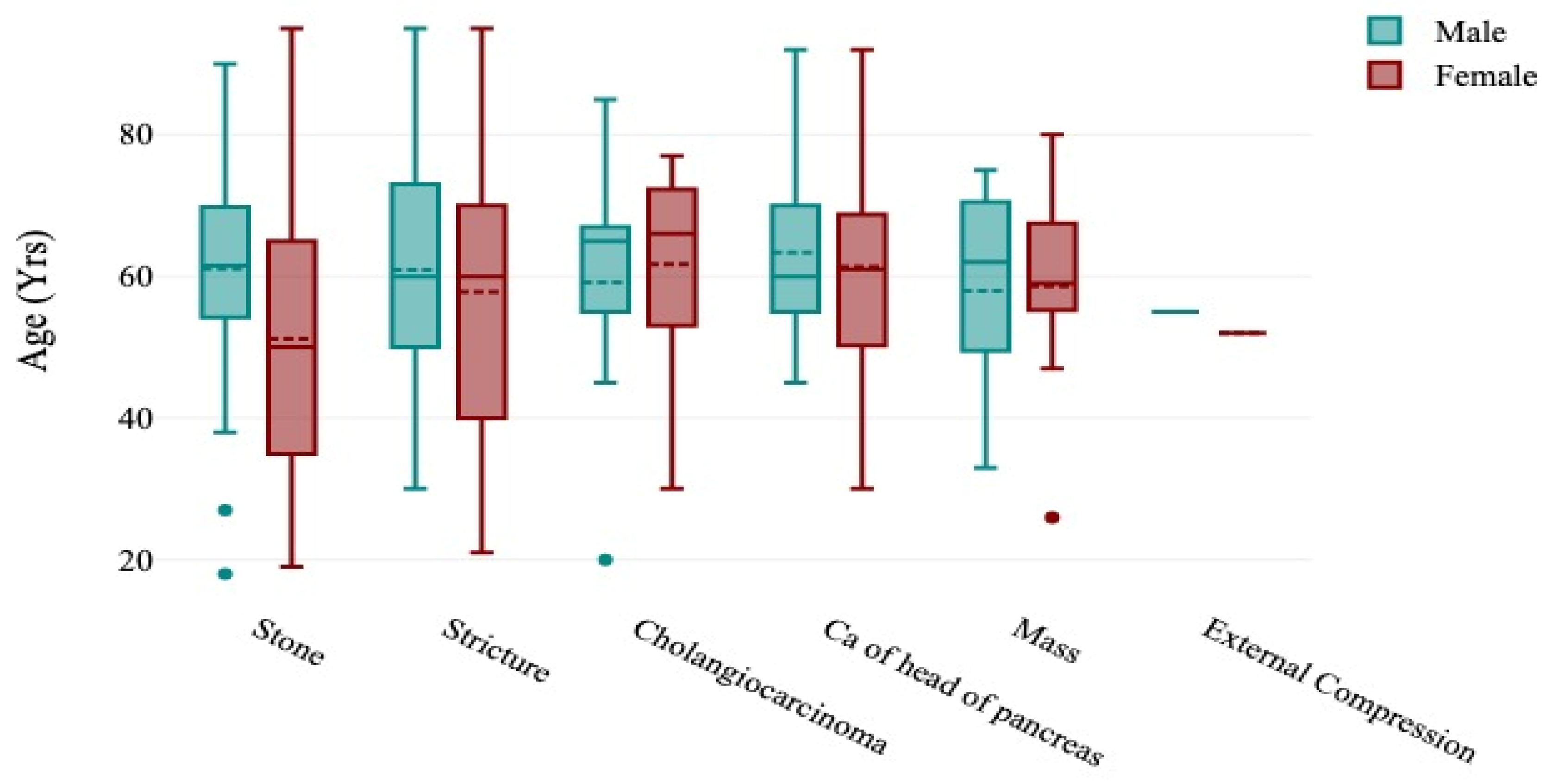

| Variable | Categories | Number | Percentage |
|---|---|---|---|
| Patient’s gender | Male | 120 | 39.60% |
| Female | 183 | 60.40% | |
| Patient’s age groups | Young (<20 years) | 4 | 1.32% |
| Young adults (21–40 years) | 61 | 20.13% | |
| Middle-aged adults (41–60 years) | 112 | 36.96% | |
| Old (61–80 years) | 101 | 33.33% | |
| Very old (>80 years) | 25 | 8.25% |
| Causes of Obstructive Jaundice | Number | Percentage |
|---|---|---|
| Common bile duct stone | 175 | 57.8% |
| Common bile duct stricture | 58 | 19.1% |
| Cholangiocarcinoma | 21 | 6.9% |
| Carcinoma of the pancreas | 35 | 11.6% |
| Mass at the ampulla of Vater | 12 | 4.0% |
| External compression | 2 | 0.7% |
| Total | 303 | 100% |
| Causes of Obstructive Jaundice | Male | Female | Total | p-Value |
|---|---|---|---|---|
| Common bile duct stone | 62 | 113 | 175 (57.8%) | 0.336 |
| Common bile duct stricture | 29 | 29 | 58 (19.1%) | |
| Cholangiocarcinoma | 7 | 14 | 21 (6.9%) | |
| Carcinoma of the pancreas | 17 | 18 | 35 (11.6%) | |
| Mass at the ampulla of Vater | 4 | 8 | 12 (4.0%) | |
| Compression | 1 | 1 | 2 (0.7%) | |
| Total | 120 | 183 | 303 (100%) |
| Causes of Obstructive Jaundice | Young | Young Adults | Middle-Aged Adults | Old | Very Old | Total | p-Value |
|---|---|---|---|---|---|---|---|
| Common bile duct stone | 3 | 46 | 60 | 52 | 14 | 175 (57.8%) | 0.025 |
| Common bile duct stricture | 0 | 10 | 23 | 20 | 5 | 58 (19.1%) | |
| Cholangiocarcinoma | 1 | 2 | 3 | 14 | 1 | 21 (6.9%) | |
| Carcinoma of the pancreas | 0 | 1 | 19 | 10 | 5 | 35 (11.6%) | |
| Mass at the ampulla of Vater | 0 | 2 | 5 | 5 | 0 | 12 (4.0%) | |
| External compression | 0 | 0 | 2 | 0 | 0 | 2 (0.7%) | |
| Total | 4 | 61 | 112 | 101 | 25 | 303 (100%) |
| Locations of Cause of Obstructive Jaundice | Number | Percentage |
|---|---|---|
| Common bile duct (CBD) | 254 | 83.8% |
| Head of pancreas | 30 | 9.9% |
| Ampulla of Vater | 13 | 4.3% |
| Liver mass causing compression | 6 | 2.0% |
| Total | 303 | 100% |
| Locations of Cause of Obstructive Jaundice | Number | Percentage |
|---|---|---|
| CBD stone (No determined part) | 101 | 33.3% |
| CBD stone in the distal part | 126 | 41.6% |
| CBD stone in the middle part | 4 | 1.3% |
| CBD stone in the proximal part | 23 | 7.6% |
| Head of pancreas | 30 | 9.9% |
| Ampulla of Vater | 13 | 4.3% |
| Liver mass causing compression | 6 | 2.0% |
| Total | 303 | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshoabi, S.A.; Binnuhaid, A.A.; Muslem, H.F.; Hamid, A.M.; Alhazmi, F.H.; Alrehily, F.A.; Qurashi, A.A.; Abdulaal, O.M.; Alshamrani, A.F.; Omer, A.M. Demographic Profiles, Etiological Spectrum, and Anatomical Locations of the Post-Hepatic Obstructive Jaundice in Adult Population in Hadhramout Region in Yemen. Diseases 2024, 12, 333. https://doi.org/10.3390/diseases12120333
Alshoabi SA, Binnuhaid AA, Muslem HF, Hamid AM, Alhazmi FH, Alrehily FA, Qurashi AA, Abdulaal OM, Alshamrani AF, Omer AM. Demographic Profiles, Etiological Spectrum, and Anatomical Locations of the Post-Hepatic Obstructive Jaundice in Adult Population in Hadhramout Region in Yemen. Diseases. 2024; 12(12):333. https://doi.org/10.3390/diseases12120333
Chicago/Turabian StyleAlshoabi, Sultan Abdulwadoud, Abdulkhaleq Ayedh Binnuhaid, Halah Fuad Muslem, Abdullgabbar M. Hamid, Fahad H. Alhazmi, Faisal A. Alrehily, Abdulaziz A. Qurashi, Osamah M. Abdulaal, Abdullah F. Alshamrani, and Awatif M. Omer. 2024. "Demographic Profiles, Etiological Spectrum, and Anatomical Locations of the Post-Hepatic Obstructive Jaundice in Adult Population in Hadhramout Region in Yemen" Diseases 12, no. 12: 333. https://doi.org/10.3390/diseases12120333
APA StyleAlshoabi, S. A., Binnuhaid, A. A., Muslem, H. F., Hamid, A. M., Alhazmi, F. H., Alrehily, F. A., Qurashi, A. A., Abdulaal, O. M., Alshamrani, A. F., & Omer, A. M. (2024). Demographic Profiles, Etiological Spectrum, and Anatomical Locations of the Post-Hepatic Obstructive Jaundice in Adult Population in Hadhramout Region in Yemen. Diseases, 12(12), 333. https://doi.org/10.3390/diseases12120333







