Abstract
Istaroxime, an intravenous inotropic agent with a dual mechanism—increasing both cardiomyocyte contractility and relaxation—is a novel treatment for acute heart failure (AHF), the leading cause of morbidity and mortality in heart failure. We conducted a systematic review and meta-analysis that synthesized randomized controlled trials (RCTs), which were retrieved by systematically searching PubMed, Web of Science, SCOPUS, and Cochrane until 24 April 2023. We used a fixed-effect or random-effect model—according to heterogeneity—to pool dichotomous data using the risk ratio (RR) and continuous data using the mean difference (MD), with a 95% confidence interval (CI). We included three RCTs with a total of 300 patients. Istaroxime was significantly associated with an increased left ventricular ejection fraction (mL) (MD: 1.06, 95% CI: 0.29, 1.82; p = 0.007), stroke volume index (MD: 3.04, 95% CI: 2.41, 3.67; p = 0.00001), and cardiac index (L/min/m2) (MD: 0.18, 95% CI: 0.11, 025; p = 0.00001). Also, istaroxime was significantly associated with a decreased E/A ratio (MD: −0.39, 95% CI: −0.58, −0.19; p = 0.0001) and pulmonary artery systolic pressure (mmHg) (MD: 2.30, 95% CI: 3.20, 1.40; p = 0.00001). Istaroxime was significantly associated with increased systolic blood pressure (mmHg) (MD: 5.32, 95% CI: 2.28, 8.37; p = 0.0006) and decreased heart rate (bpm) (MD: −3.05, 95% CI: −5.27, −0.82; p = 0.007). Since istaroxime improved hemodynamic and echocardiographic parameters, it constitutes a promising strategy for AHF management. However, the current literature is limited to a small number of RCTs, warranting further large-scale phase III trials before clinical endorsement.
1. Introduction
Heart failure (HF) is a chronic and progressive disease estimated to have a prevalence of over 26 million worldwide, and it is on the rise, with an overwhelming global healthcare-related burden [1,2,3]. The exacerbation of acute heart failure (AHF) is the leading cause of morbidity and mortality associated with HF. The natural history of AHF has largely remained unchanged in the last decade [4,5]. Patients with low systolic blood pressure (SBP) or overt cardiogenic shock (CS) continue to be at the highest risk of poor outcomes [6,7,8]. The Society of Cardiovascular Angiography and Interventions (SCAI) has recently proposed the classification of CS into five stages (A to E) to characterize patients for better-targeted treatment [9]. Pre-cardiogenic shock (Pre-CS) refers to the period of rapid hemodynamic deterioration that precedes overt CS with hypotension, inflammatory response, and end-organ damage [10].
The current management strategies for AHF with CS are inotropic agents (e.g., dobutamine, milrinone, and enoximone) and vasoactive agents (e.g., norepinephrine). Unfortunately, despite the transient improvement in hemodynamic status with these agents, they have not shown survival benefits [11,12]. In addition, all inotropic drugs recommended for patients with AHF activate adrenergic signaling to some extent, and extended use of these drugs can be potentially harmful [12]. Istaroxime is a novel intravenous inotropic agent with a dual mechanism that inhibits Na+/K+ adenosine triphosphatase activity while activating sarcoplasmic reticulum Ca+2 adenosine triphosphatase isoform 2a (SERCA2a) [13,14,15]. This dual mechanism causes an increase in intracellular calcium and promotes calcium reuptake in the sarcoplasmic reticulum, resulting in both increased cardiomyocyte contractility (during systole) and relaxation (during diastole) [16,17,18]. This could offset the risk of arrhythmias associated with traditional inotropes. These effects support a potential therapeutic role for istaroxime in treating AHF, and recent clinical trials have studied its use in these patients [19,20,21,22,23].
To clarify the safety and efficacy of istaroxime for AHF, a systematic review and meta-analysis determined that istaroxime is effective in (A) increasing the left ventricular ejection fraction (LVEF), cardiac index, and systolic blood pressure (SBP) and (B) reducing the E/A ratio, indicating improved left ventricular function, left ventricular end-diastolic volume (LVEDV), and left ventricular end-systolic volume (LVESV) [24]. We sought to conduct a systematic review and meta-analysis utilizing more extensive criteria to extract more data [25,26] to further investigate the safety and efficacy of istaroxime in AHF.
2. Materials and Methods
2.1. Protocol Registration
We conducted this review by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [27] and the Cochrane Handbook for Systematic Reviews and Meta-Analyses [28]. We pre-registered and published the protocol for this study on PROSPERO (CRD42023424614).
2.2. Data Sources and Search Strategy
M.A. and B.A. conducted an electronic search through five databases: PubMed (MEDLINE), Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science (WoS), and EMBASE were searched until 24 April 2023. We also conducted an updated search just before starting the analysis to include any recently published articles after the original search. We modified the search terms and keywords for each database (Table S1).
2.3. Eligibility Criteria and Study Selection
We included studies that followed the following PICO criteria: population (patients with AHF); intervention (istaroxime irrespective of the dosage); comparison (placebo); outcomes (echocardiographic parameters (left ventricle (LV) end-diastolic volume, LV end-systolic volume, LV ejection fraction, stroke volume index, cardiac index, E/A ratio, E/e′ ratio, inferior vena cava (IVC) diameter, and pulmonary artery systolic pressure), hemodynamic parameters (systolic blood pressure (SBP), mean arterial pressure (MAP), and heart rate (HR)), clinical outcomes (NT-proBNP change, length of hospital stay, worsening HF, and hospital readmission), and safety outcomes (the incidence of any adverse events including non-serious adverse events (nausea, vomiting, and injection site pain) and serious adverse events (cardiac arrest, ventricular tachycardia, pneumonia, acute renal failure, and newly diagnosed coronary artery disease)); and study design (randomized clinical trials (RCTs)).
We excluded studies that met any of the following criteria: (1) non-original studies (e.g., reviews, book chapters, correspondence, letters to editors, commentaries, press articles, and guidelines), (2) any study designs other than RCTs, (3) studies with overlapping datasets or duplications, (4) studies with a sample size of fewer than ten participants, (5) studies that did not report on istaroxime or lacked a primary outcome, (6) in vitro experiments and non-human studies, and (7) studies that were not conducted in the English language.
2.4. Study Selection
We utilized the online Covidence tool [29] to conduct the review process. After removing any duplicate records, M.M.A. and M.T. independently reviewed the retrieved records. During the full-text screening, M.M.A. and M.T. checked the full texts of the records that met the original eligibility requirements. Any disagreements that arose were resolved through discussion and agreement with a senior author.
2.5. Data Extraction
Four reviewers (A.M., H.A., M.A., and M.T.) independently used a well-designed online extraction form to extract the upcoming data. The first part included the summary characteristics of the included studies (name of first author, year of publication, country, name of journal, and study design). The second part included the baseline information of the participants (sample size, age, gender, follow-up period, SBP, HR, LV end-diastolic volume, LV end-systolic volume, LV ejection fraction, stroke volume index, cardiac index (L/min/m2), E/A ratio, and E/e′ ratio). Finally, the third part included outcome data. The data extraction process was carried out by two reviewers (M.M.A. and M.T.). Any disagreements that arose were resolved through discussion and agreement with a senior author.
2.6. Risk of Bias and Certainty of Evidence
Two investigators (H.A. and M.T.) independently appraised the property of the studies using the Cochrane ROB2 tool [30]. Any disagreements that arose were resolved through discussion and agreement with a senior author. To evaluate the quality of the evidence, two reviewers (M.A. and B.A.) used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines [25,26]. Any differences were settled via consensus.
2.7. Statistical Analysis
The RevMan v5.3 software [31] was the statistical analysis application of choice for conducting the analysis. The mean difference (MD) was used for continuous results, and the risk ratio (RR) was used for dichotomous outcomes. Both were calculated with a 95% confidence interval (CI) using a fixed-effect model. If the heterogeneity was high, we used a random-effect model. The heterogeneity was evaluated using the Chi-square and I-square tests, respectively, according to the Cochrane Handbook (chapter nine) [26].
3. Results
3.1. Search Results and Study Selection
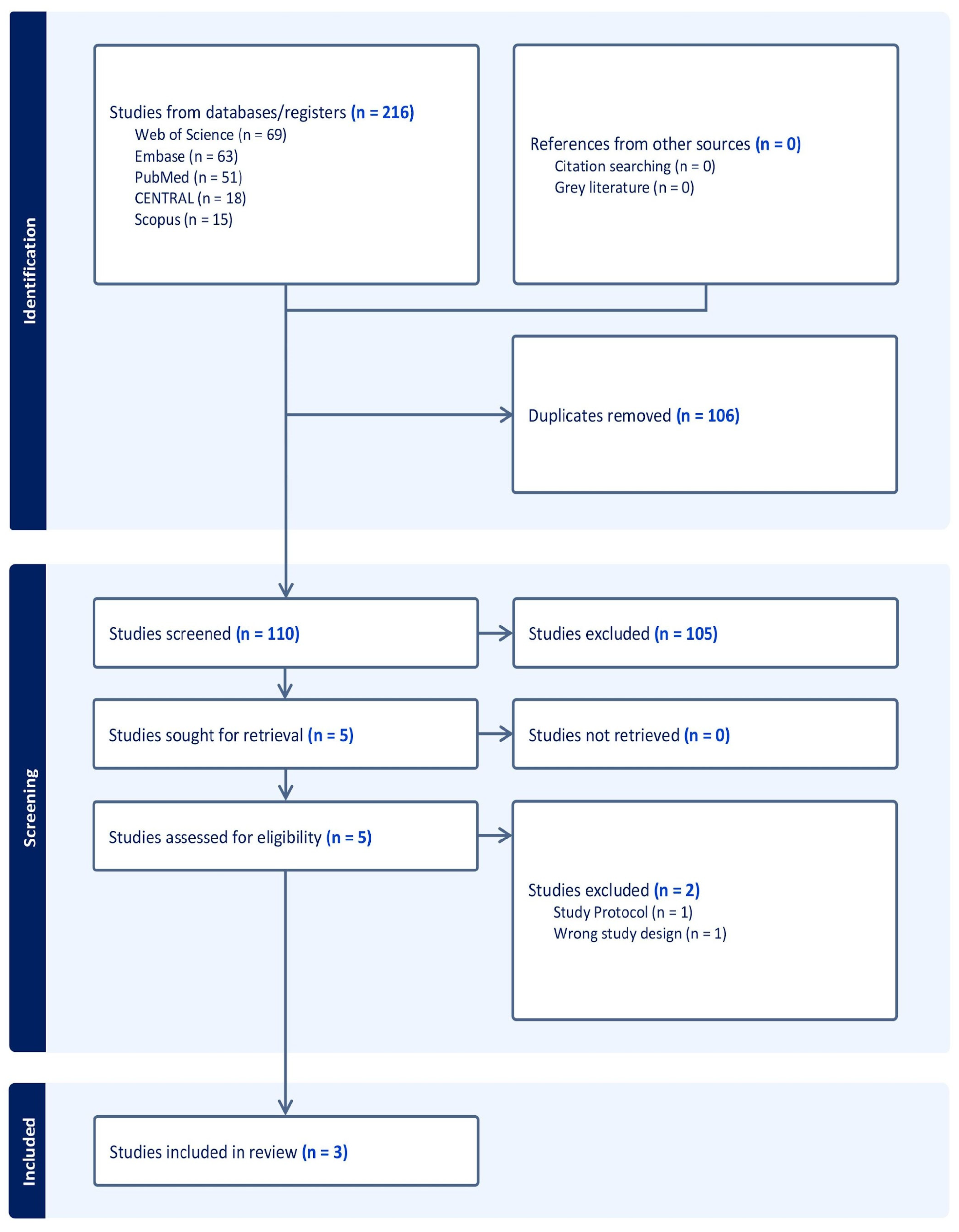
The search process yielded 216 studies that were screened and evaluated for their titles and abstracts. After duplicates (106) and irrelevant studies (105) were excluded, five full-text articles were screened. Finally, three studies were included in the qualitative and quantitative synthesis (Figure 1).
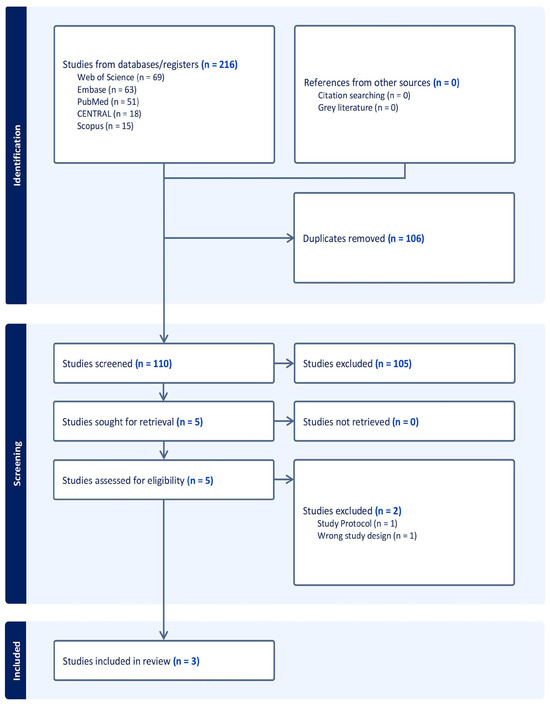
Figure 1.
PRISMA flowchart of the screening process.
3.2. Characteristics of the Included Studies
We included three RCTs [19,20,21], with a total of 300 participants. Details of the included RCTs and the baseline characteristics of the participants are reported in Table 1 and Table 2, respectively.

Table 1.
Summary characteristics of the included RCTs.

Table 2.
Baseline characteristics of the participants.
3.3. Risk of Bias and Certainty of Evidence
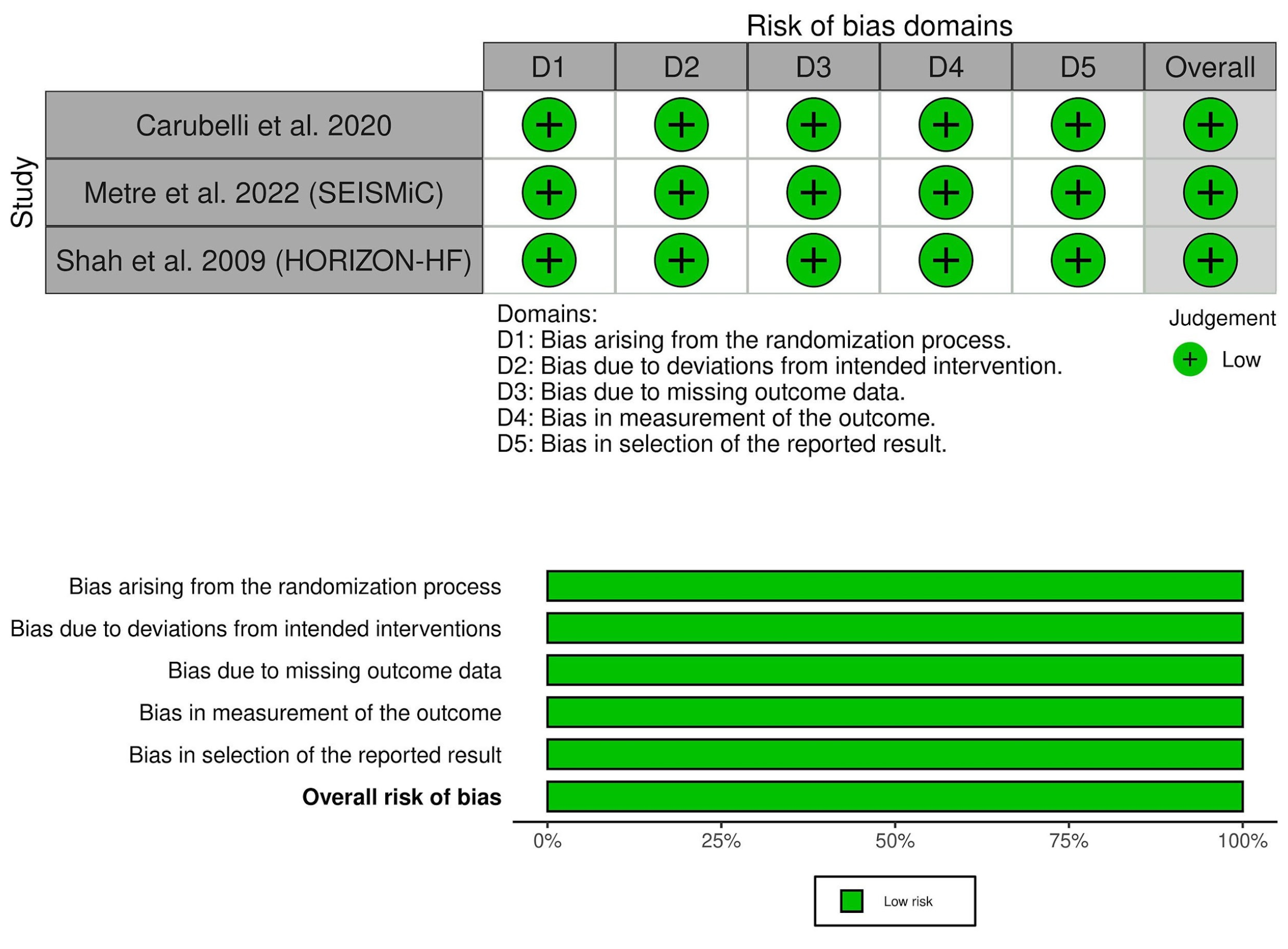
All of the included trials showed a low risk of bias across the assessed domains (Figure 2, Tables S2–S4). Also, the certainty of evidence was outlined in a GRADE evidence profile (Table 3).
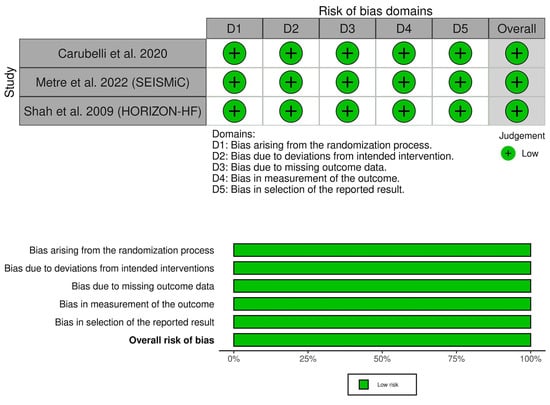
Figure 2.
Quality assessment of the risk of bias in the included studies. Carubelli et al., 2020 [20], Metra et al., 2022 [19] (SEISMiC), Shah et al., 2009 [21] (HORIZON-HF).

Table 3.
GRADE evidence profile.
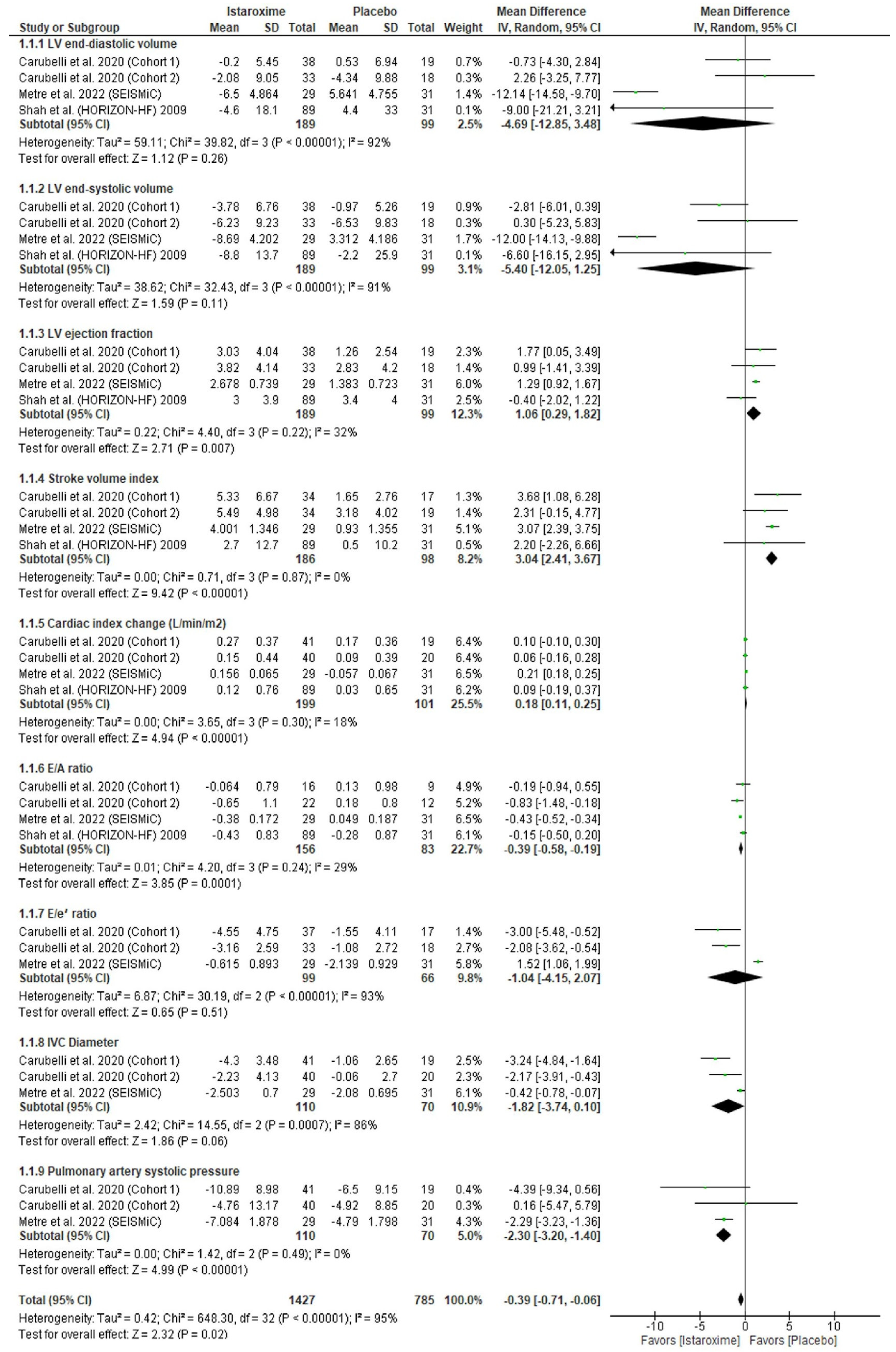
3.4. Echocardiographic Parameters
Istaroxime was significantly associated with an increased LV ejection fraction (mL) (MD: 1.06; 95% CI: 0.29, 1.82; p = 0.007), stroke volume index (MD: 3.04; 95% CI: 2.41, 3.67; p = 0.00001), and cardiac index (L/min/m2) (MD: 0.18; 95% CI: 0.11, 0.25; p = 0.00001). Also, istaroxime was significantly associated with a decreased E/A ratio (MD: −0.39; 95% CI: −0.58, −0.19; p = 0.0001) and pulmonary artery systolic pressure (MD: −2.30; 95% CI: −3.20, −1.40; p = 0.00001). However, there was no difference between istaroxime and the placebo regarding the LV end-diastolic volume (MD: −4.69; 95% CI: 12.85, 3.48; p = 0.26), LV end-systolic volume (MD: −5.40; 95% CI: −12.05, 1.25; p = 0.11), E/e′ ratio (MD: −1.04; 95% CI: −4.15, 2.07; p = 0.51), and IVC diameter (mm) (MD: −1.82; 95% CI: −3.74, 0.15; p = 0.06) (Figure 3).
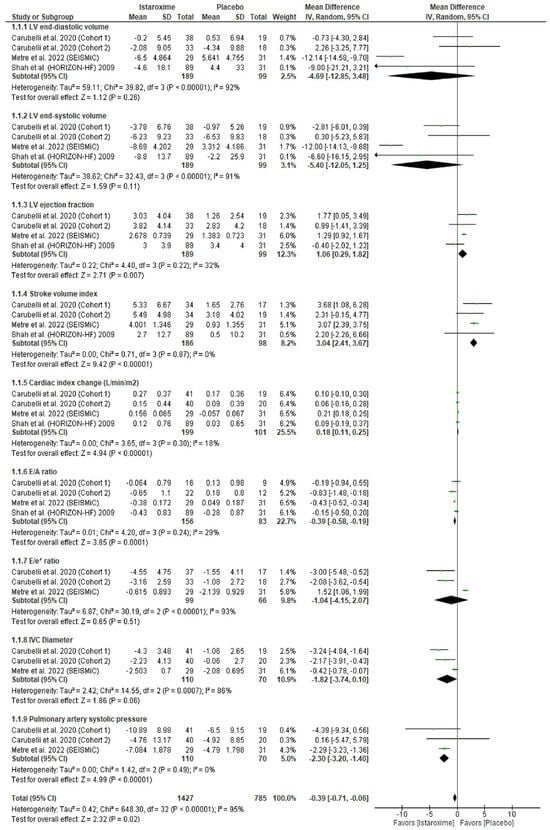
Figure 3.
Forest plot of the echocardiographic parameters. CI: confidence interval; MD: mean difference. Carubelli et al., 2020 [20], Metra et al., 2022 [19] (SEISMiC), Shah et al., 2009 [21] (HORIZON-HF).
Our results were homogenous for the LV ejection fraction (p = 0.22, I2 = 32%), stroke volume index (p = 0.87, I2 = 0%), cardiac index (p = 0.30, I2 = 18%), E/A ratio (p = 0.24, I2 = 29%), and pulmonary artery systolic pressure (p = 0.49, I2 = 0%). However, our results were heterogenous for the LV end-diastolic volume (p = 0.26, I2 = 92%), LV end-systolic volume (p = 0.00001, I2 = 91%), E/e′ ratio (p = 0.00001, I2 = 93%), and IVC diameter (p = 0.0007, I2 = 86%). We performed a sensitivity analysis, and the heterogeneity was best resolved by excluding Metra et al. (2022) [19] (p = 0.81, I2 = 29%; p = 0.84, I2 = 32%; p = 0.54, I2 = 0%; p = 0.38, I2 = 0%) (Table S5).
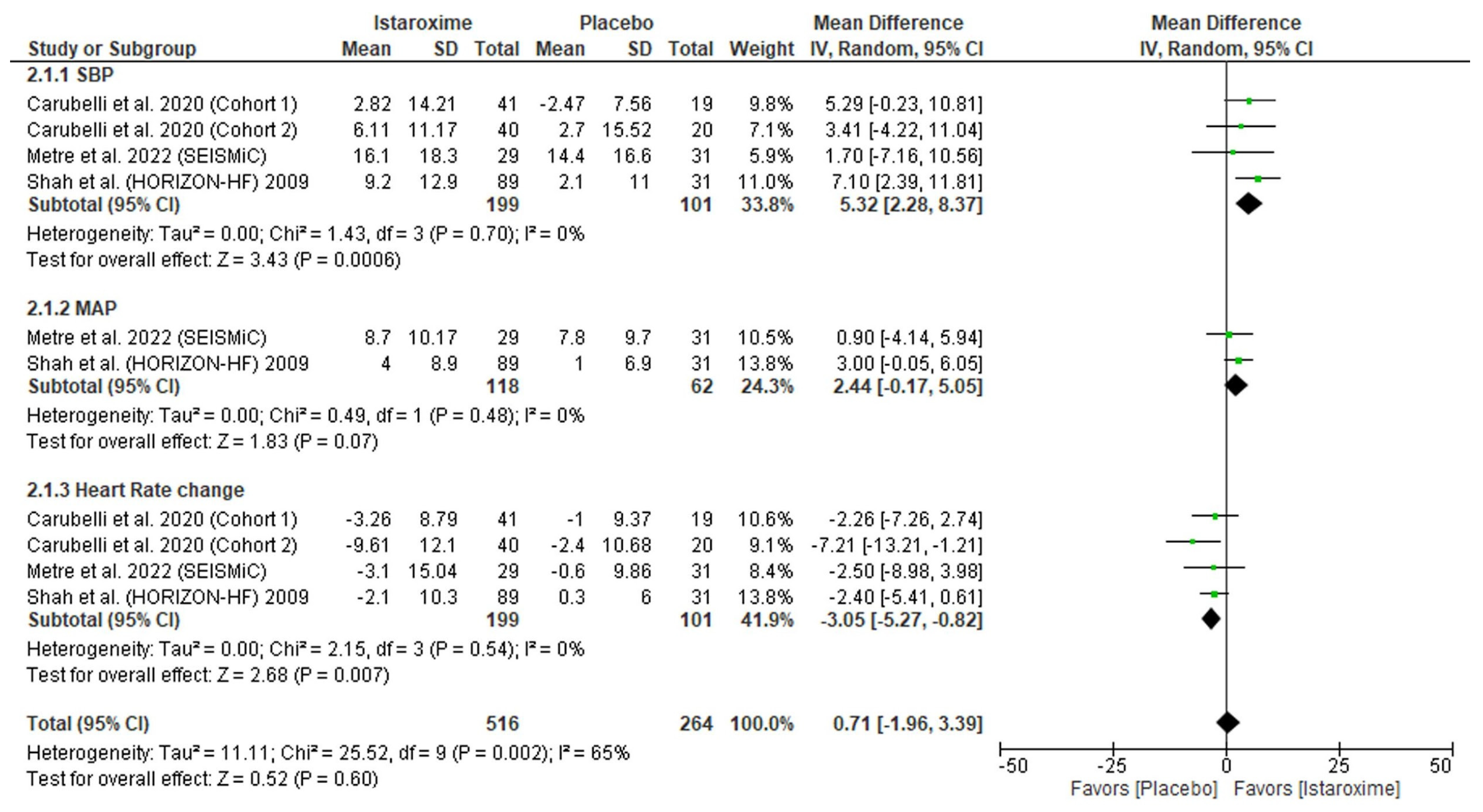
3.5. Hemodynamic Parameters
Istaroxime was significantly associated with increased SBP (mmHg) (MD: 5.32; 95% CI: 2.28, 8.37; p = 0.0006) and decreased HR (MD: −3.05; 95% CI: −5.27, −0.82; p = 0.007). However, there was no difference between istaroxime and the placebo regarding MAP (mmHg) (MD: 2.44; 95% CI: −0.17, 5.05; p = 0.06) (Figure 4). Our results were homogenous for SBP (p = 0.70, I2 = 0%), HR (p = 0.54, I2 = 0%), and MAP (p = 0.48, I2 = 0%).
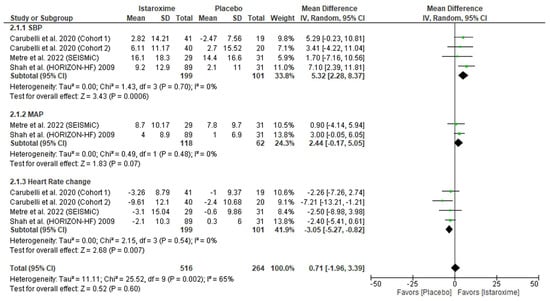
Figure 4.
Forest plot of the hemodynamic parameters. CI: confidence interval; MD: mean difference. Carubelli et al., 2020 [20], Metra et al., 2022 [19] (SEISMiC), Shah et al., 2009 [21] (HORIZON-HF).
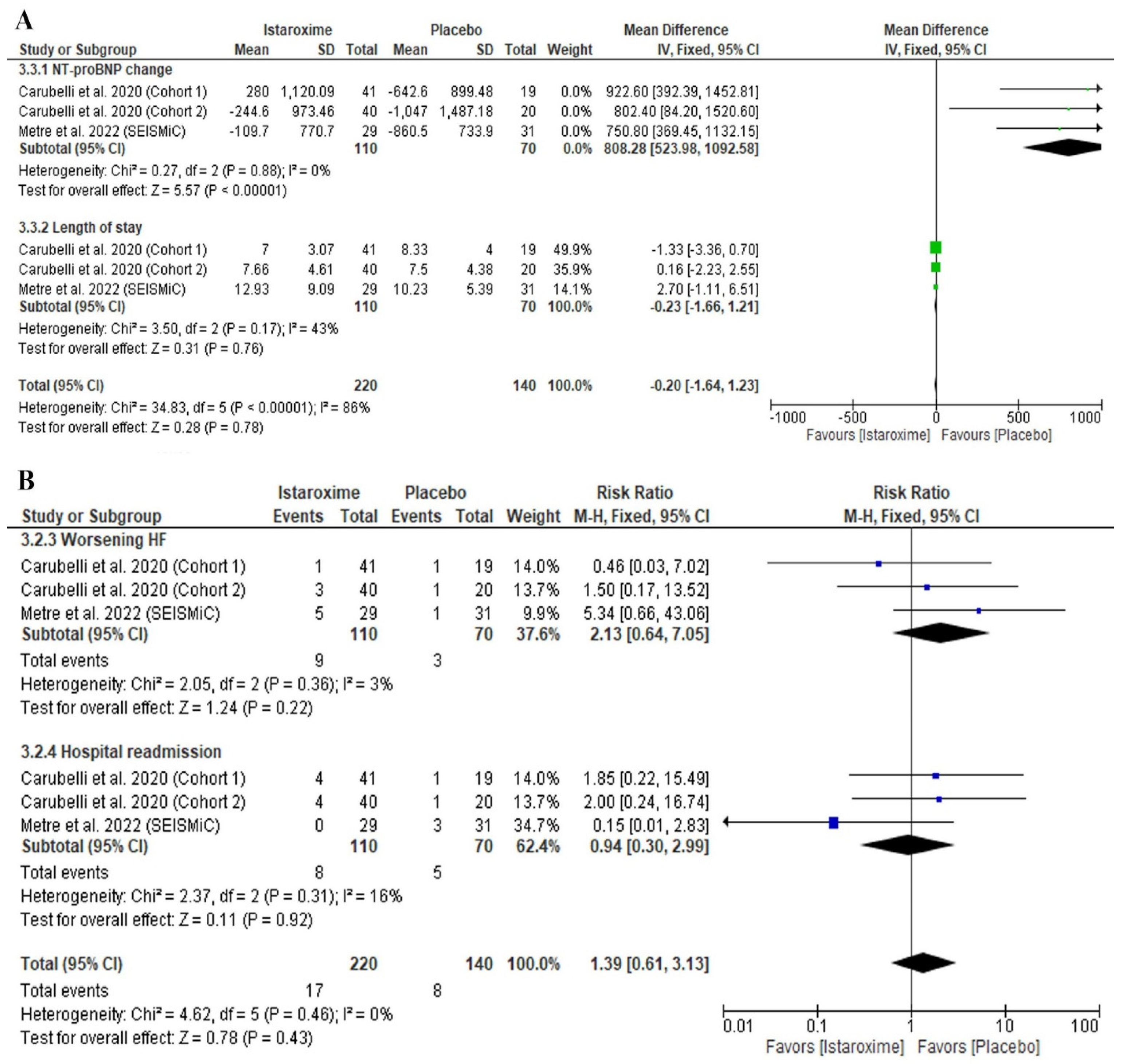
3.6. Clinical Parameters
Istaroxime was significantly associated with an increased NT-proBNP level (MD: 808.28; 95% CI: 523.98, 1092.58; p = 0.00001) (Figure 5A). However, there was no difference between istaroxime and the placebo regarding the length of stay in the hospital (days) (MD: −0.23; 95% CI: −1.66, 1.21; p = 0.76) (Figure 5A), worsening HF (RR: 1.88 (95% CI: 0.49, 7.20; p = 0.35), or hospital readmission (RR: 1.09 (95% CI: 0.25, 4.71; p = 0.91) (Figure 5B).
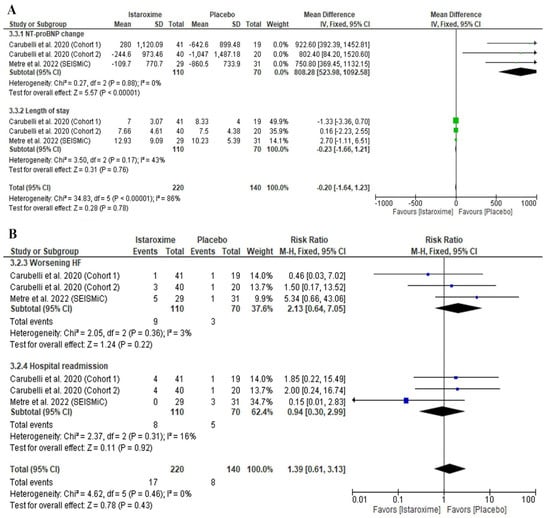
Figure 5.
Forest plot of the clinical outcomes [(A) continuous outcomes; (B) dichotomous outcomes]. MD: mean difference, RR: risk ratio, CI: confidence interval. Carubelli et al., 2020 [20], Metra et al., 2022 [19] (SEISMiC), Shah et al., 2009 [21] (HORIZON-HF).
Our results were homogenous for the NT-proBNP level (p = 0.88, I2 = 0%), length of stay in the hospital (p = 0.17, I2 = 43%), worsening HF (p = 0.36, I2 = 3%), and hospital readmission (p = 0.31, I2 = 16%).
3.7. Safety Outcomes
Istaroxime was significantly associated with an increased rate of incidence of any adverse events (RR: 1.26; 95% CI: 1.05, 1.51; p = 0.01). However, there were no differences between istaroxime and the placebo regarding any serious adverse events (RR: 1.34; 95% CI: 0.58, 3.11; p = 0.49) (Figure S1). Our results were homogenous for the incidence of any adverse events (p = 0.34, I2 = 0%) and any serious adverse events (p = 0.52, I2 = 0%).
4. Discussion
We report several noteworthy findings in this meta-analysis of RCTs evaluating the efficacy and safety of istaroxime in AHF patients. First, istaroxime was significantly associated with an increased LV ejection fraction, stroke volume, and cardiac index, as well as a decreased E/A ratio and pulmonary artery systolic pressure. However, there was no significant difference between LV end-diastolic volume and LV end-systolic volume compared to the placebo. Second, istaroxime therapy was significantly associated with increased SBP and decreased HR, but it could not achieve statistical significance regarding a higher MAP than that of the placebo group. Third, despite a significant increase in the NT-proBNP level, there was no difference in other important clinical outcomes, including the length of stay, hospital readmission rate, and worsening of HF. Finally, there was no statistically significant difference in the incidence of serious adverse events compared to the placebo. However, it increased the rate of other non-serious adverse events, such as infusion-related side effects.
The mechanism of action of istaroxime can explain the echocardiographic findings observed in our study. Understanding the pathophysiology of excitation–contraction (EC) coupling is vital when interpreting the effects of any inotropic therapy for HF. In patients with AHF, the inability of the heart to eject sufficient blood for peripheral tissue perfusion is caused by defects in EC coupling in cardiac myocytes [32]. Istaroxime works through a dual mechanism that inhibits Na+/K+ adenosine triphosphatase activity while activating sarcoplasmic reticulum Ca+2 adenosine triphosphatase isoform 2a (SERCA2a) [6,13,14]. The inhibition of Na+/K+ adenosine triphosphatase increases intracellular sodium levels, affecting Ca+2 homeostasis through Na+/Ca+2 exchange (NCX) and resulting in increased levels of intracellular Ca+2. Intracellular Ca+2 then binds to troponin C, facilitating actin–myosin interaction, which induces the contraction of the cardiac myocytes. The role of intracellular Ca+2 in homeostasis for cardiomyocyte contractility has been extensively investigated [33,34].
To clarify, during diastole, Ca+2 diffuses away from troponin C, initiating relaxation. The Ca+2 that was released from the sarcoplasmic reticulum is taken back up by the SERCA2a, whereas the amount of Ca+2 that entered the cell via L-type calcium channels is exported by the NCX [35]. However, in a failing heart, the increased cytosolic concentration of Ca+2—even during diastole due to impaired Ca+2 expulsion via the forward mechanism of NCX—can result in slower relaxation [35]. This can be problematic, especially with an elevated HR, when the diastolic period is already shortened, leading to impaired filling and, subsequently, a progressive decline in cardiac output. Theoretically, through a dual mechanism, istaroxime can offset this effect by improving contractility during systole and relaxation during diastole, leading to an improved stroke volume, LV ejection fraction, and cardiac index, as observed in our analysis. Similarly, we noticed a trend toward decreased end-diastolic and systolic volumes, which did not achieve statistical significance.
The current literature is limited in in its comparison of istaroxime with classic inotropic agents (digoxin, dobutamine) and Ca+2 sensitizers (levosimendan). Digitalis-derived cardiotropic glycosides, e.g., digoxin, are the oldest inotropic drugs, and they may be considered in symptomatic HF with a reduced ejection fraction (HFrEF) despite being at the maximum tolerated dose of guideline-directed medical therapy [4,35,36]. In a trial by the Digitalis Investigation Group (DIG), digoxin did not improve all-cause mortality but reduced hospitalization due to HF [35]. However, this trial was conducted before the advent of the current guideline-directed medical therapy for HFrEF. The current American College of Cardiology/American Heart Association (ACC/AHA) and European Society of Cardiology (ESC) guidelines recommend against the routine use of inotropes, except in certain high-risk patient populations with AHF, e.g., patients with signs of cardiogenic shock, SBP < 90 mmHg refractory to fluid challenge, or persistent symptomatic hypoperfusion [4,37]. These guidelines were based on studies evaluating the safety and efficacy of inotropes (dobutamine, dopamine, and phosphodiesterase inhibitors), and neutral effects were reported in the short term, while long-term use was associated with adverse outcomes in patients hospitalized for AHF [38,39,40].
There are no extant data for directly comparing istaroxime with pimobendan and levosimendan, which are calcium sensitizers that increase cardiac myocyte contractility. Nevertheless, drugs in this class may have variable mechanisms. Still, the endpoint is an increased affinity of troponin C to binding Ca+2, resulting in an increased force of contraction during systole for any given amount of intracellular Ca+2 in cardiac myocytes [41,42]. On the other hand, this also impairs diastolic relaxation due to the slowing of calcium reuptake. However, istaroxime can improve diastolic relaxation by stimulating calcium reuptake. Moreover, the increase in myofilament Ca+2 sensitization has been reported to be arrhythmogenic, which is another concern with the use of calcium sensitizers [43].
In this context, it is essential to notice that in the SURVIVE trial, patients on levosimendan with β-blocker pre-treatment had improved short-term survival compared to those taking dobutamine [44]. Another study reported the potential benefit of levosimendan in patients with ischemic heart disease [45]. Conversely, in septic shock patients co-treated with catecholamines, levosimendan was associated with higher rates of supraventricular tachycardia [46]. These observed findings point towards the possibility of adrenergic properties of calcium sensitizers similar to those of classic inotropes; hence, their role in AHF management is not yet fully established [4,12,36]. In our study, istaroxime was associated with decreased HR without significant differences in serious adverse events compared to the control group. This can be clinically important, as the role of beta blockers in acute HF for achieving the desired chronotropic effect is limited due to their negative inotropic effect. Landiolol is an ultra-short-acting cardioselective B1-blocker that has been used for tachyarrhythmias in patients with LV dysfunction [47,48,49,50]. However, there are very limited data to establish its safety in acute HF patients. Hence, future studies should consider a direct comparison of istaroxime with calcium sensitizers and digitalis to evaluate the efficacy and safety of these drugs in comparison with each other.
Finally, our study highlighted a significant increase in NT-proBNP with istaroxime. Although NT-ProBNP is widely used as a diagnostic marker for HF, its prognostic value is still uncertain. It is not well known whether elevated NT-proBNP can be associated with overall poor outcomes, as its levels can be affected by multiple factors, including advanced age, renal insufficiency, and arrhythmias [51,52]. Furthermore, we did not observe any significant differences in other clinically important outcomes, such as the length of hospital stays, worsening HF, hospital readmission rates, or safety outcomes such as serious side effects. On theoretical grounds, treatments that restore the defects of cytosolic Ca+2 handling in HF without activating adrenergic signaling can be promising, since they avoid diastolic dysfunction and the long-term adverse consequences of adrenergic activation. However, it is vital to highlight that any therapy (including istaroxime) targeting EC coupling and mitochondrial energetics in cardiomyocytes can potentially induce maladaptive cardiac remodeling and apoptosis through a transition in mitochondrial permeability [53].
Strengths and Limitations
To the best of our knowledge, this is the most extensive meta-analysis to investigate the efficacy and safety of istaroxime for AHF management, constituting gold-standard evidence, with an extensive assessment of the certainty of the evidence by using the GRADE approach [25,26]. However, the following limitations of our study should be considered before interpreting our results. The studies included in our meta-analysis had a relatively younger patient population with a mean age ranging between 50 and 65 years. Patients with extreme heart rates were excluded from the trials. For example, Shah et al. included only patients with HRs from 60 to 110 beats per minute (bpm) [21], and Carubelli et al. excluded patients with resting HRs of <50 bpm or >120 bpm [20].
The HORIZON-HF trial [21] lacked a core laboratory for the review and quantification of echocardiographic images, which could have potentially resulted in discrepancies in the echocardiographic readings of the study. Also, maneuvers such as preload reduction were not performed for the pressure–volume analyses, which could have impaired their overall accuracy. Furthermore, the pulse-wave tissue Doppler imaging used in this trial had limitations, such as the angle dependence of the Doppler beam, which can be important, especially in patients with dilated cardiomyopathy. Similarly, Carubelli et al. [20] had enrollment discrepancies between the study population and the selection of the two cohorts, with one cohort enrolling only Asian patients. Also, the patients enrolled in this trial were younger and had better renal function than in other studies [20]. Moreover, SEISMiC [19] only enrolled patients without signs or symptoms of hypoperfusion, which could have led to a selection bias by enrolling a relatively less sick cohort to determine the overall efficacy and safety of istaroxime. Finally, we included only three RCTs with a relatively small number of patients, thus impairing the generalizability of our findings.
5. Conclusions
Istaroxime improved hemodynamic and echocardiographic parameters, forming a promising strategy for AHF management. However, there were no significant differences in clinical outcomes, and there was an increase in adverse events with istaroxime. Furthermore, the current evidence is limited to a small number of RCTs; therefore, future large-scale phase III trials are needed to fully understand the short- and long-term effects of istaroxime on EC coupling and mitochondrial energetics, to further investigate hard cardiovascular outcomes, and to compare istaroxime with other inotropes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diseases11040183/s1, Table S1. Search strategy; Table S2. Risk of bias assessment for Carubelli et al., 2020 [20]; Table S3. Risk of bias assessment for Metre et al., 2022 [19]; Table S4. Risk of bias assessment for Shah et al., 2009 [21]; Table S5. Sensitivity analysis; Figure S1. Forest plot of the safety outcomes.
Author Contributions
Conceptualization, M.A.; methodology, M.A. and B.A.; software, M.A. and B.A.; validation, M.A., B.A. and J.R.B.; formal analysis, A.M.; investigation, M.M.A., M.T. and H.A.S.; data curation, M.A. and B.A.; writing—original draft preparation, M.A., S.A. and H.A.S.; writing—review and editing, M.A., S.A., H.A.S. and J.R.B.; supervision, B.A. and J.R.B.; project administration, M.A. and B.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are included in the manuscript.
Acknowledgments
The authors thank Welch Medicine Library of the Johns Hopkins University School of Medicine, Baltimore, Maryland, USA, for providing access to publications.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ACA/AHA | American College of Cardiology/American Heart Association |
| AF | Atrial fibrillation |
| AHF | Acute heart failure |
| BMI | Body mass index |
| bpm | Beats per minute |
| CABG | Coronary artery bypass graft |
| CI | Confidence interval |
| CKD | Chronic kidney disease |
| CS | Cardiogenic shock |
| DIG | Digitalis Investigation Group |
| DBP | Diastolic blood pressure |
| df | Degrees of freedom |
| DM | Diabetes mellitus |
| EC | Excitation–contraction |
| ESC | European Society of Cardiology |
| HFrEF | Heart failure with reduced ejection fraction |
| HR | Heart rate |
| HTN | Hypertension |
| I | Istaroxime |
| IVC | Inferior vena cava |
| ID | Identification |
| L | Liter |
| LV | Left ventricle |
| LVEDV | Left ventricular end-diastolic volume |
| LVEF | Left ventricular ejection fraction |
| LVESV | Left ventricular end-systolic volume |
| M | Mean |
| MAP | Mean arterial pressure |
| MD | Mean difference |
| N | Number |
| NCX | Na+/Ca+2 exchange |
| p | Probability |
| PICO | Population Intervention Comparison Outcomes |
| Pl | Placebo |
| PCI | Percutaneous coronary intervention |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized controlled trial |
| SBP | Systolic blood pressure |
| SCAI | Society of Cardiovascular Angiography and Interventions |
| SD | Standard deviation |
| SERCA2a | Sarcoplasmic reticulum Ca+2 adenosine triphosphatase isoform 2a |
| US | United States |
| . (period) | Missing data. |
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics--2022 Update: A report from the American Heart Association. Circulation 2022, 145, E153–E639. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Yusuf, S.; Reddy, S.; Ôunpuu, S.; Anand, S. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001, 104, 2746–2753. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J. Am. Coll. Cardiol. 2022, 79, 1757–1780. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Abraham, W.T.; Albert, N.M.; Greenberg, B.H.; O’Connor, C.M.; She, L.; Stough, W.G.; Yancy, C.W.; Young, J.B.; Fonarow, G.C. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA 2006, 296, 2217–2226. [Google Scholar] [CrossRef] [PubMed]
- van Diepan, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K.; et al. Contemporary management of cardiogenic shock: A scientific statement from the American Heart Association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef] [PubMed]
- Chioncel, O.; Parissis, J.; Mebazaa, A.; Thiele, H.; Desch, S.; Bauersachs, J.; Harjola, V.P.; Antohi, E.L.; Arrigo, M.; Ben Gal, T.; et al. Epidemiology, pathophysiology and contemporary management of cardiogenic shock—A position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22, 1315–1341. [Google Scholar] [CrossRef]
- Baran, D.A.; Grines, C.L.; Bailey, S.; Burkhoff, D.; Hall, S.A.; Henry, T.D.; Hollenberg, S.M.; Kapur, N.K.; O’Neill, W.; Ornato, J.P.; et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock: This document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter. Cardiovasc. Interv. 2019, 94, 29–37. [Google Scholar] [CrossRef]
- Singh, T.; Samson, R.; Ayinapudi, K.; Motwani, A.; Le Jemtel, T.H. Precardiogenic shock: A new clinical entity. Cardiol. Rev. 2019, 27, 198–201. [Google Scholar] [CrossRef]
- Mebazaa, A.; Nieminen, M.S.; Packer, M.; Cohen-Solal, A.; Kleber, F.X.; Pocock, S.J.; Thakkar, R.; Padley, R.J.; Põder, P.; Kivikko, M.; et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: The SURVIVE Randomized Trial. JAMA 2007, 297, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Maack, C.; Eschenhagen, T.; Hamdani, N.; Heinze, F.R.; Lyon, A.R.; Manstein, D.J.; Metzger, J.; Papp, Z.; Tocchetti, C.G.; Yilmaz, M.B.; et al. Treatments targeting inotropy. Eur. Heart J. 2019, 40, 3626–3644. [Google Scholar] [CrossRef] [PubMed]
- Micheletti, R.; Palazzo, F.; Barassi, P.; Giacalone, G.; Ferrandi, M.; Schiavone, A.; Moro, B.; Parodi, O.; Ferrari, P.; Bianchi, G. Istaroxime, a stimulator of sarcoplasmic reticulum calcium adenosine triphosphatase isoform 2a activity, as a novel yherapeutic approach to heart failure. Am. J. Cardiol. 2007, 99, S24–S32. [Google Scholar] [CrossRef] [PubMed]
- Mattera, G.G.; Lo Giudice, P.; Loi, F.M.P.; Vanoli, E.; Gagnol, J.P.; Borsini, F.; Carminati, P. Istaroxime: A new luso-inotropic agent for heart failure. Am. J. Cardiol. 2007, 99, S33–S40. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Sabbah, H.N. Istaroxime: An investigational luso-inotropic agent for acute heart failure syndromes. Am. J. Cardiol. 2007, 99, 1A–3A. [Google Scholar] [CrossRef] [PubMed]
- Teerlink, J.R.; Metra, M.; Zacà, V.; Sabbath, H.N.; Cotter, G.; Gheorghiade, M.; Cas, L.D. Agents with inotropic properties for the management of acute heart failure syndromes. Traditional agents and beyond. Heart Fail. Rev. 2009, 14, 243–253. [Google Scholar] [CrossRef]
- Chioncel, O.; Collins, S.P.; Butler, J. Istaroxime in acute heart failure: The holy grail is at HORIZON? Eur. J. Heart Fail. 2020, 22, 1694–1697. [Google Scholar] [CrossRef]
- Forzano, I.; Mone, P.; Mottola, G.; Kansakar, U.; Salemme, L.; De Luca, A.; Tesorio, T.; Varzideh, F.; Santulli, G. Efficacy of the new inotropic agent istaroxime in acute heart failure. J. Clin. Med. 2022, 11, 7503. [Google Scholar] [CrossRef]
- Metra, M.; Chioncel, O.; Cotter, G.; Davison, B.; Filippatos, G.; Mebazaa, A.; Novosadova, M.; Ponikowski, P.; Simmons, P.; Soffer, J.; et al. Safety and efficacy of istaroxime in patients with acute heart failure-related pre-cardiogenic shock—A multicentre, randomized, double-blind, placebo-controlled, parallel group study (SEISMiC). Eur. J. Heart Fail. 2022, 24, 1967–1977. [Google Scholar] [CrossRef]
- Carubelli, V.; Zhang, Y.; Metra, M.; Lombardi, C.; Felker, G.M.; Filippatos, G.; O’Connor, C.M.; Teerlink, J.R.; Simmons, P.; Segal, R.; et al. Treatment with 24 hour istaroxime infusion in patients hospitalised for acute heart failure: A randomised, placebo-controlled trial. Eur. J. Heart Fail. 2020, 22, 1684–1693. [Google Scholar] [CrossRef]
- Shah, S.J.; Blair, J.E.A.; Filippatos, G.S.; MacArie, C.; Ruzyllo, W.; Korewicki, J.; Bubenek-Turconi, S.I.; Ceracchi, M.; Bianchetti, M.; Carminati, P.; et al. Effects of istaroxime on diastolic stiffness in acute heart failure syndromes: Results from the Hemodynamic, Echocardiographic, and Neurohormonal Effects of Istaroxime, a Novel Intravenous Inotropic and Lusitropic Agent: A Randomized Controlled Trial in Patients with Heart Failure (HORIZON-HF) trial. Am. Heart J. 2009, 157, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiade, M.; Blair, J.E.A.; Filippatos, G.S.; Macarie, C.; Ruzyllo, W.; Korewicki, J.; Bubenek-Turconi, S.I.; Ceracchi, M.; Bianchetti, M.; Carminati, P.; et al. Hemodynamic, echocardiographic, and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: A randomized controlled trial in patients hospitalized with heart failure. J. Am. Coll. Cardiol. 2008, 51, 2276–2285. [Google Scholar] [CrossRef] [PubMed]
- Dec, G.W. Istaroxime in heart failure new hope or more hype. J. Am. Coll. Cardiol. 2008, 51, 2286–2288. [Google Scholar] [CrossRef] [PubMed]
- Khalid Khan, S.; Rawat, A.; Khan, Z.; Reyaz, I.; Kumar, V.; Batool, S.; Yadav, R.; Hirani, S. Safety and efficacy of istaroxime in patients with acute heart failure: A meta-analysis of randomized controlled trials. Cureus 2023, 15, e41084. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Kunz, R.; Vist, G.E.; Falck-Ytter, Y.; Schünemann, H.J. What is “quality of evidence” and why is it important to clinicians? BMJ 2008, 336, 995. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley: Chichester, UK, 2019; pp. 1–694. [Google Scholar] [CrossRef]
- Covidence. Available online: http://www.covidence.org/ (accessed on 11 November 2023).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Cochrane Training. RevMan. Available online: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman (accessed on 11 November 2023).
- Bers, D.M. Altered cardiac myocyte Ca regulation in heart failure. Physiology 2006, 21, 380–387. [Google Scholar] [CrossRef]
- Boroń, L.; Szczyglowski, K.; Konieczny, A.; Legocki, A.B. Glutamine synthetase in Lupinus luteus. Identification and preliminary characterization of nodule-specific CDNA clone. Acta Biochim. Pol. 1989, 36, 295–301. [Google Scholar]
- Grandi, E.; Pasqualini, F.S.; Bers, D.M. A novel computational model of the human ventricular action potential and Ca transient. J. Mol. Cell. Cardiol. 2010, 48, 112–121. [Google Scholar] [CrossRef] [PubMed]
- The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N. Engl. J. Med. 1997, 336, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, e263–e421. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.J.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Tacon, C.L.; McCaffrey, J.; Delaney, A. Dobutamine for patients with severe heart failure: A systematic review and meta-analysis of randomised controlled trials. Intensive Care Med. 2012, 38, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; Carver, J.R.; Rodeheffer, R.J.; Ivanhoe, R.J.; DiBianco, R.; Zeldis, S.M.; Hendrix, G.H.; Bommer, W.J.; Elkayam, U.; Kukin, M.L.; et al. Effect of oral milrinone on mortality in severe chronic heart failure. N. Engl. J. Med. 1991, 325, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Parissis, J.; Porcher, R.; Gayat, E.; Nikolaou, M.; Boas, F.V.; Delgado, J.F.; Follath, F. Short-term survival by treatment among patients hospitalized with acute heart failure: The global ALARM-HF registry using propensity scoring methods. Intensive Care Med. 2011, 37, 290–301. [Google Scholar] [CrossRef] [PubMed]
- Radke, M.B.; Taft, M.H.; Stapel, B.; Hilfiker-Kleiner, D.; Preller, M.; Manstein, D.J. Small molecule-mediated refolding and activation of myosin motor function. eLife 2014, 3, e01603. [Google Scholar] [CrossRef]
- Schlecht, W.; Li, K.L.; Hu, D.; Dong, W. Fluorescence based characterization of calcium sensitizer action on the troponin complex. Chem. Biol. Drug Des. 2016, 87, 171–181. [Google Scholar] [CrossRef]
- Schober, T.; Huke, S.; Venkataraman, R.; Gryshchenko, O.; Kryshtal, D.; Hwang, H.S.; Baudenbacher, F.J.; Knollmann, B.C. Myofilament Ca sensitization increases cytosolic Ca binding affinity, alters intracellular Ca homeostasis, and causes pause-dependent Ca-triggered arrhythmia. Circ. Res. 2012, 111, 170–179. [Google Scholar] [CrossRef]
- Mebazaa, A.; Nieminen, M.S.; Filappatos, G.S.; Cleland, J.G.; Salon, J.E.; Thakkar, R.; Padley, R.J.; Huang, B.; Cohen-Solal, A. Levosimendan vs. dobutamine: Outcomes for acute heart failure patients on beta-blockers in SURVIVE. Eur. J. Heart Fail. 2009, 11, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Tumminello, G.; Cereda, A.; Barbieri, L.; Biondi-Zoccai, G.; Lucreziotti, S.; Mafrici, A.; Carugo, S. Meta-analysis of placebo-controlled trials of levosimendan in acute myocardial infarction. J. Cardiovasc. Dev. Dis. 2021, 8, 129. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.C.; Perkins, G.D.; Singer, M.; McAuley, D.F.; Orme, R.M.L.; Santhakumaran, S.; Mason, A.J.; Cross, M.; Al-Beidh, F.; Best-Lane, J.; et al. Levosimendan for the prevention of acute organ dysfunction in sepsis. N. Engl. J. Med. 2016, 375, 1638–1648. [Google Scholar] [CrossRef] [PubMed]
- Syed, Y.Y. Landiolol: A review in tachyarrhythmias. Drugs 2018, 78, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Cereda, A.; Laricchia, A.; Marini, C.; Franchina, G.; Conconi, B.; Lucreziotti, S. Literature case series review on landiolol in acute decompensated heart failure secondary to tachyarrhythmias. Eur. Heart J. Suppl. 2022, 24 (Suppl. K), suac121.143. [Google Scholar] [CrossRef]
- Cereda, A.; Laricchia, A.; Franchina, G.A.; Tumminello, G.; Sangiorgi, G.M.; Lucreziotti, S. Case series review on landiolol in acute decompensated heart failure secondary to tachyarrhythmias: New drug applications for an unmet medical need in critically ill patients. Medp. Cardiol. Vasc. Med. 2022, 2, mpcvm-202205002. [Google Scholar]
- Rao, S.J.; Kanwal, A.; Kanwal, A.; Danilov, A.; Frishman, W.H. Landiolol: An Ultra-Short-Acting β-Blocker. Cardiol. Rev. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Liang, L.; Huang, L.; Zhao, X.; Zhao, L.; Tian, P.; Huang, B.; Feng, J.; Zhang, J.; Zhang, Y. Prognostic value of RDW alone and in combination with NT-ProBNP in patients with heart failure. Clin. Cardiol. 2022, 45, 802–813. [Google Scholar] [CrossRef]
- Ibrahim, N.E.; Januzzi, J.L., Jr. Established and emerging roles of biomarkers in heart failure. Circ. Res. 2018, 123, 614–629. [Google Scholar] [CrossRef]
- Bertero, E.; Maack, C. Calcium signaling and reactive oxygen species in mitochondria. Circ. Res. 2018, 122, 1460–1478. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).