Predictors of New and Persistent New Left Bundle Branch Block One Year after the Implantation of a Sutureless and Rapid-Deployment Aortic Valve Prosthesis
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Surgical Techniques
2.3. Technique for Implanting the SURD EDWARDS INTUITY Valve
2.4. Anaesthetic and Intensive Care Treatment
2.5. Data Acquisition and Statistical Analysis
3. Results
3.1. Baseline Clinical Characteristics, Echocardiography and Electrocardiography before Aortic Valve Replacement Surgery
3.2. Procedural Indices
3.3. Procedural Complications
3.4. One Year Follow-Up
3.5. Predictors of New LBBB after AVR and Persistent New LBBB 1 Year after AVR—Univariate Analysis
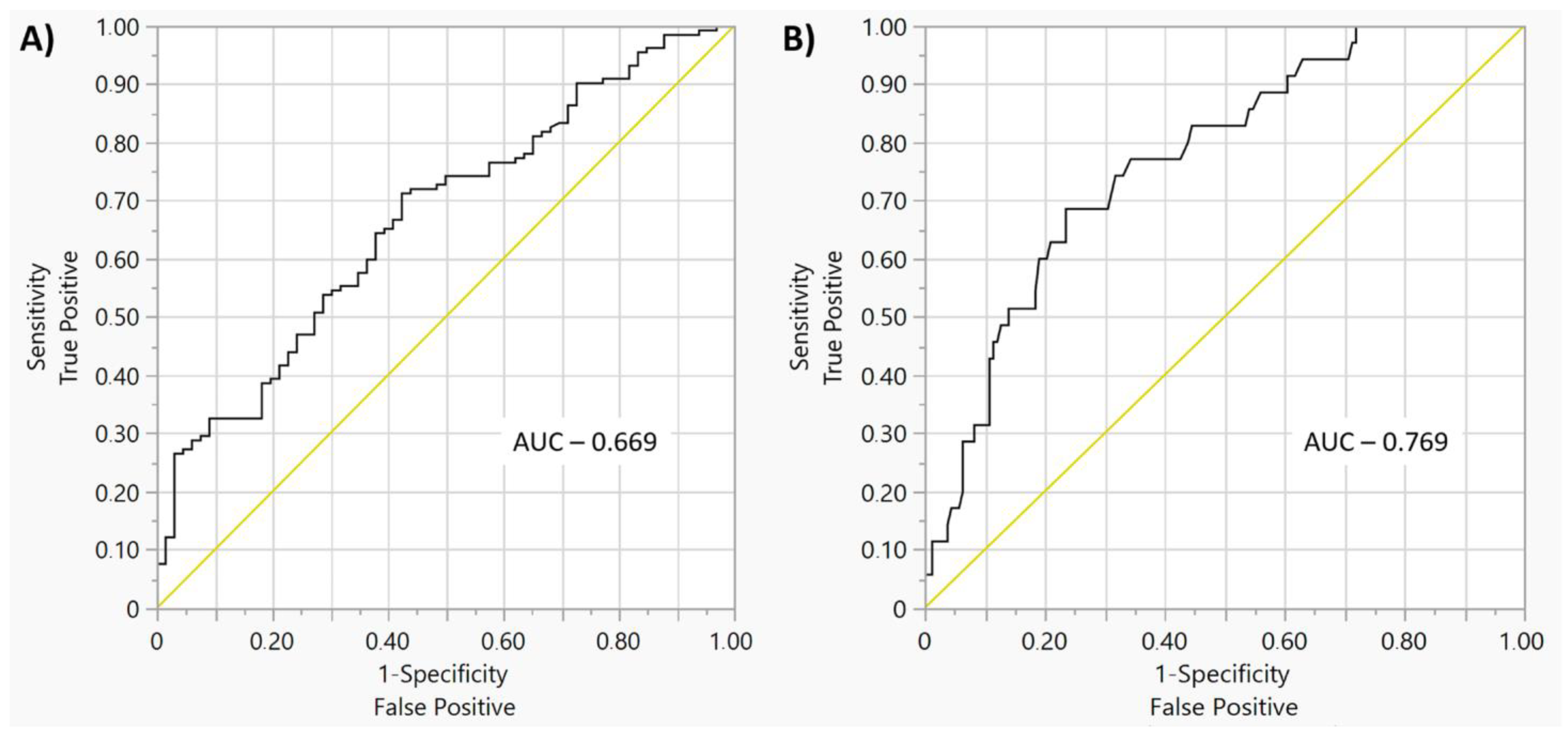
3.6. Predictors of New LBBB after AVR and Persistent New LBBB 1 Year after AVR—Multivariate Regression Analysis
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hwang, Y.M.; Kim, J.; Lee, J.H.; Kim, M.; Hwang, J.; Kim, J.B.; Kim, Y.H. Conduction disturbance after isolated surgical aortic valve replacement in degenerative aortic stenosis. J. Thorac. Cardiovasc. Surg. 2017, 154, 1556–1565. [Google Scholar]
- Sa, M.P.; Jabagi, H.; Dokollari, A.; Awad, A.K.; Van den Eynde, J.; Malin, J.H.; Ramlawi, B. Early and late outcomes of surgical aortic valve replacement with sutureless and rap-id-deployment valves versus transcatheter aortic valve implantation: Meta-analysis with reconstructed time-to-event data of matched studies. Catheter. Cardiovasc. Interv. 2022, 99, 1886–1896. [Google Scholar]
- Todaro, D.; Picci, A.; Barbanti, M. Current TAVR devices—Technical characteristics and evidence to date for FDA- and CE Mark-approved valves. Cardiac. Interv. Today 2017, 11, 6. [Google Scholar]
- Schroeter, T.; Linke, A.; Haensig, M.; Merk, D.R.; Borger, M.A.; Mohr, F.W.; Schuler, G. Predictors of permanent pacemaker implantation after Medtronic CoreValve bioprosthesis implantation. Europace 2012, 14, 1759–1763. [Google Scholar]
- Zhang, X.L.; Wei, Z.H.; Wang, H.W.; Xu, W.; Wang, Y.; Xu, B. Early and midterm outcomes of transcatheter aortic-valve replacement with bal-loon-expandable versus self-expanding valves: A meta-analysis. J. Cardiol. 2022, 80, 204–210. [Google Scholar]
- Lorusso, R.; Ravaux, J.M.; Pollari, F.; Folliguet, T.A.; Kappert, U.; Meuris, B.; Shrestha, M.L.; Roselli, E.E.; Bonaros, N.; Fabre, O.; et al. Pacemaker implantation after sutureless or stented valve: Results from a controlled randomized trial. Eur. J. Cardio-Thorac. Surg. 2022, 62, ezac164. [Google Scholar] [CrossRef]
- El-Khally, Z.; Thibault, B.; Staniloae, C.; Theroux, P.; Dubuc, M.; Roy, D.; Talajic, M. Prognostic significance of newly acquired bundle branch block after aortic valve re-placement. Am. J. Cardiol. 2004, 94, 1008–1011. [Google Scholar]
- Poels, T.T.; Houthuizen, P.; Van Garsse, L.A.; Hamad, M.A.S.; Maessen, J.G.; Prinzen, F.W.; Van Straten, A.H. Frequency and prognosis of new bundle branch block induced by surgical aortic valve replacement. Eur. J. Cardio-Thorac. Surg. 2014, 47, e47–e53. [Google Scholar] [CrossRef]
- Aversa, E.; Muratore, C.A.; Nemesio, M.L.; Tentori, M.C.; Payaslian, M. New conduction disturbances and pacemaker indications after CoreValve(R) transcatheter aortic valve replacement. Incidence and follow up in a single center experience. Arch. Cardiol. Mex. 2015, 85, 278–283. [Google Scholar]
- Khounlaboud, M.; Flécher, E.; Fournet, M.; Le Breton, H.; Donal, E.; Leclercq, C.; Mabo, P.; Leguerrier, A.; Daubert, C. Predictors and prognostic impact of new left bundle branch block after surgical aortic valve replacement. Arch. Cardiovasc. Dis. 2017, 110, 667–675. [Google Scholar] [CrossRef]
- Schlömicher, M.; Useini, D.; Haldenwang, P.L.; Naraghi, H.; Moustafine, V.; Bechtel, M.; Strauch, J.T. Outcomes in Patients with Left Bundle Branch Block after Rapid Deployment Aortic Valve Replacement. Thorac. Cardiovasc. Surg. 2022. [Google Scholar] [CrossRef]
- Sohn, S.H.; Kang, Y.; Kim, J.S.; Choi, J.W.; Jang, M.J.; Hwang, H.Y. Direct comparison of rapid deployment versus sutureless aortic valve replacement: A me-ta-analysis. J. Thorac. Dis. 2021, 13, 2203–2215. [Google Scholar]
- Matthews, I.G.; Fazal, I.A.; Bates, M.G.; Turley, A.J. In patients undergoing aortic valve replacement, what factors predict the require-ment for permanent pacemaker implantation? Interact. Cardiovasc. Thorac. Surg. 2011, 12, 475–479. [Google Scholar]
- Mogilansky, C.; Balan, R.; Deutsch, C.; Czesla, M.; Massoudy, P. New postoperative conduction abnormalities after the implantation of a rap-id-deployment aortic valve prosthesis. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 581–586. [Google Scholar]
- D’Onofrio, A.; Tessari, C.; Bagozzi, L.; Migliore, F.; Filippini, C.; Cibin, G.; Gerosa, G. Conduction disorders after aortic valve replacement with rapid-deployment biopros-theses: Early occurrence and one-year evolution. Ann. Cardiothorac. Surg. 2020, 9, 396–407. [Google Scholar]
- Lam, K.Y.; Akca, F.; Verberkmoes, N.J.; Van Dijk, C.; Claessens, A.; Hamad, M.A.S.; Van Straten, A.H.M. Conduction disorders and impact on survival after sutureless aortic valve replacement compared to conventional stented bioprostheses. Eur. J. Cardio-Thorac. Surg. 2018, 55, 1168–1173. [Google Scholar] [CrossRef]
- Regeer, M.; Merkestein, L.; de Weger, A.; Kamperidis, V.; van der Kley, F.; van Rosendael, P.; Marsan, N.; Klautz, R.; Schalij, M.; Bax, J.; et al. Left bundle branch block after sutureless, transcatheter, and stented biological aortic valve replacement for aortic stenosis. Eurointervention 2017, 12, 1660–1666. [Google Scholar] [CrossRef]
- Piazza, N.; Onuma, Y.; Jesserun, E.; Kint, P.P.; Maugenest, A.-M.; Anderson, R.H.; de Jaegere, P.P.T.; Serruys, P.W. Early and Persistent Intraventricular Conduction Abnormalities and Requirements for Pacemaking After Percutaneous Replacement of the Aortic Valve. JACC Cardiovasc. Interv. 2008, 1, 310–316. [Google Scholar] [CrossRef]
- Calvi, V.; Puzzangara, E.; Pruiti, G.P.; Conti, S.; Di Grazia, A.; Ussia, G.P.; Capodanno, D.; Tamburino, C. Early Conduction Disorders Following Percutaneous Aortic Valve Replacement. Pacing Clin. Electrophysiol. 2009, 32, S126–S130. [Google Scholar] [CrossRef]
- Roten, L.; Wenaweser, P.; Delacrétaz, E.; Hellige, G.; Stortecky, S.; Tanner, H.; Windecker, S. Incidence and predictors of atrioventricular conduction impairment after transcathe-ter aortic valve implantation. Am. J. Cardiol. 2010, 106, 1473–1480. [Google Scholar]
- Fraccaro, C.; Buja, G.; Tarantini, G.; Gasparetto, V.; Leoni, L.; Razzolini, R.; Corrado, D.; Bonato, R.; Basso, C.; Thiene, G.; et al. Incidence, Predictors, and Outcome of Conduction Disorders After Transcatheter Self-Expandable Aortic Valve Implantation. Am. J. Cardiol. 2011, 107, 747–754. [Google Scholar] [CrossRef]
- Khawaja, M.Z.; Rajani, R.; Cook, A.; Khavandi, A.; Moynagh, A.; Chowdhary, S.; Hildick-Smith, D. Permanent pacemaker insertion after CoreValve transcatheter aortic valve implantation: Incidence and contributing facttors (the UK CoreValve Collaborative). Circulation 2011, 123, 951–960. [Google Scholar]
- Baan, J., Jr.; Yong, Z.Y.; Koch, K.T.; Henriques, J.P.; Bouma, B.J.; Vis, M.M.; Cocchieri, R.; Piek, J.J.; de Mol, B.A. Factors associated with cardiac conduction disorders and permanent pacemaker implanta-tion after percutaneous aortic valve implantation with the CoreValve prosthesis. Am. Heart J. 2010, 159, 497–503. [Google Scholar]
- Aktug, Ö.; Dohmen, G.; Brehmer, K.; Koos, R.; Altiok, E.; Deserno, V.; Herpertz, R.; Autschbach, R.; Marx, N.; Hoffmann, R. Incidence and predictors of left bundle branch block after transcatheter aortic valve implantation. Int. J. Cardiol. 2012, 160, 26–30. [Google Scholar] [CrossRef]
- Nuis, R.-J.; Van Mieghem, N.M.; Schultz, C.J.; Tzikas, A.; Van der Boon, R.M.; Maugenest, A.-M.; Cheng, J.; Piazza, N.; van Domburg, R.T.; Serruys, P.W.; et al. Timing and potential mechanisms of new conduction abnormalities during the implantation of the Medtronic CoreValve System in patients with aortic stenosis. Eur. Heart J. 2011, 32, 2067–2074. [Google Scholar] [CrossRef]
- Urena, M.; Mok, M.; Serra, V.; Dumont, E.; Nombela-Franco, L.; DeLarochellière, R.; Doyle, D.; Igual, A.; Larose, E.; Amat-Santos, I.; et al. Predictive Factors and Long-Term Clinical Consequences of Persistent Left Bundle Branch Block Following Transcatheter Aortic Valve Implantation With a Balloon-Expandable Valve. J. Am. Coll. Cardiol. 2012, 60, 1743–1752. [Google Scholar] [CrossRef]
- Gutiérrez, M.; Rodés-Cabau, J.; Bagur, R.; Doyle, D.; DeLarochellière, R.; Bergeron, S.; Lemieux, J.; Villeneuve, J.; Côté, M.; Bertrand, O.F.; et al. Electrocardiographic changes and clinical outcomes after transapical aortic valve implantation. Am. Heart J. 2009, 158, 302–308. [Google Scholar] [CrossRef]
- Godin, M.; Eltchaninoff, H.; Furuta, A.; Tron, C.; Anselme, F.; Bejar, K.; Sanchez-Giron, C.; Bauer, F.; Litzler, P.-Y.; Bessou, J.-P.; et al. Frequency of Conduction Disturbances After Transcatheter Implantation of an Edwards Sapien Aortic Valve Prosthesis. Am. J. Cardiol. 2010, 106, 707–712. [Google Scholar] [CrossRef]
- Shiyovich, A.; Kornowski, R.; Plakht, Y.; Aviv, Y.; Assa, H.V.; Assali, A.; Hamdan, A. Increased Rate of New-onset Left Bundle Branch Block in Patients with Bicuspid Aor-tic Stenosis Undergoing Transcatheter Aortic Valve Implantation (from a National Registry). Am. J. Cardiol. 2021, 156, 101–107. [Google Scholar]
| Total | New LBBB after AVR | Persistent New LBBB 1 Year after AVR | |||||
|---|---|---|---|---|---|---|---|
| No (n = 133) | Yes (n = 67) | p-Value | No (n = 157) | Yes (n = 35) | p-Value | ||
| Group 1 vs. 2 | 100 (50%) | 66 (49.6) | 34 (50.7) | 0.88 | 81 (51.6) | 16 (45.7) | 0.52 |
| Age, years | 71.3 ± 7.5 72.5 (67; 77) | 71.8 ± 7.7 74 (68; 77) | 70.1 ± 7.2 72 (64; 76) | 0.08 | 71.1 ± 7.8 72 (67; 77) | 70.8 ± 6.5 72 (65; 76) | 0.52 |
| Gender, male | 118 (59) | 80 (60.1) | 38 (56.7) | 0.64 | 95 (60.5) | 20 (57.1) | 0.71 |
| Body mass index, kg/m2 | 28.3 ± 4.4 28 (25; 31) | 28.6 ± 4.03 28 (25; 31) | 27.6 ± 5.2 27 (24; 31) | 0.15 | 28.6 ± 4.3 28 (25; 31.5) | 26.9 ± 4.9 26 (23; 31) | 0.06 |
| Euroscore II, % | 3.8 ± 4.3 2.3 (1.3; 4.2) | 4.4 ± 5 2.5 (1.7; 4.8) | 2.5 ± 2 1.9 (1; 3.6) | <0.001 | 3.9 ± 4.4 2.4 (1.4; 4.3) | 2.4 ± 2 1.4 (1; 3.4) | 0.009 |
| New York Heart Association (NYHA) class grade | |||||||
| I | 1 (0.5) | 1 (0.7) | 0 (0) | 0.38 | 1 (0.6) | 0 (0) | 0.13 |
| II | 19 (9.5) | 12 (9) | 7 (10.4) | 13 (8.3) | 6 (17.1) | ||
| II/III | 1 (0.5) | 0 (0) | 1 (1.5) | 0 (0) | 1 (2.9) | ||
| III | 160 (80) | 105 (78.9) | 55 (82.1) | 128 (81.5) | 26 (74.3) | ||
| IV | 19 (9.5) | 15 (11.3) | 4 (6) | 15 (9.5) | 2 (5.7) | ||
| LVEF, % | 54.6 ± 9.7 60 (50; 60) | 53.7 ± 10.3 60 (50; 60) | 56.3 ± 8.2 60 (60; 60) | 0.04 | 54.5 ± 9.9 60 (50; 60) | 56.2 ± 7.6 60 (60; 60) | 0.31 |
| Endocarditis (indication for AVR) | 9 (4.5) | 9 (6.8) | 0 (0) | 0.03 | 7 (4.5) | 0 (0) | 0.35 |
| Arterial hypertension | 186 (93) | 126 (94.7) | 60 (89.5) | 0.23 | 147 (93.6) | 31 (88.6) | 0.29 |
| Diabetes mellitus | 66 (33) | 47 (35.3) | 19 (28.4) | 0.32 | 52 (33.1) | 13 (37.1) | 0.64 |
| Prior stroke | 29 (14.5) | 20 (15) | 9 (13.4) | 0.76 | 22 (14) | 5 (14.3) | 1.0 |
| Dialysotherapy | 5 (2.5) | 4 (3) | 1 (1.5) | 0.66 | 4 (2.5) | 1 (2.9) | 1.0 |
| Atrioventricular conduction and heart rhythm disturbances before AVR | |||||||
| Sinus rhythm | 166 (83) | 106 (79.7) | 60 (89.5) | 0.08 | 130 (82.8) | 32 (91.4) | 0.2 |
| Atrial fibrillation | 28 (14) | 21 (15.8) | 7 (10.4) | 0.3 | 22 (14) | 3 (8.6) | 0.58 |
| Pacemaker | 5 (2.5) | 5 (3.8) | 0 (0) | 0.17 | 4 (2.5) | 0 (0) | 1.0 |
| AICD | 4 (2) | 3 (2.3) | 1 (1.5) | 1.0 | 4 (2.5) | 0 (0) | 1.0 |
| RBBB | 16 (8) | 16 (12) | 0 (0) | 0.003 | 15 (9.5) | 0 (0) | 0.07 |
| LBBB | 11 (5.5) | 11 (8.3) | 0 (0) | 0.017 | 9 (5.7) | 1 (2.9) | 0.69 |
| LAHB | 5 (2.5) | 5 (3.8) | 0 (0) | 0.17 | 5 (3.2) | 0 (0) | 0.58 |
| Total | New LBBB after AVR | Persistent New LBBB 1 Year after AVR | |||||
|---|---|---|---|---|---|---|---|
| No (n = 133) | Yes (n = 67) | p-Value | No (n = 157) | Yes (n = 35) | p-Value | ||
| EDWARDS INTUITY Elite Rapid-Deployment Aortic Valve Prosthesis Size | |||||||
| 19 | 8 (4) | 6 (4.5) | 2 (3) | 0.62 | 6 (3.8) | 1 (2.9) | 0.48 |
| 21 | 35 (17.5) | 25 (18.8) | 10 (14.9) | 28 (17.8) | 5 (14.3) | ||
| 23 | 63 (31.5) | 42 (31.6) | 21 (31.3) | 53 (33.8) | 9 (25.7) | ||
| 25 | 75 (37.5) | 45 (33.8) | 30 (44.8) | 53 (33.8) | 18 (51.4) | ||
| 27 | 19 (9.5) | 15 (11.3) | 4 (6) | 17 (10.8) | 2 (5.7) | ||
| INTUITY second valve size, if required | |||||||
| 23 | 1 (100) | 1 (100) | - | - | 1 (100) | - | - |
| Magna size, if required | |||||||
| 21 25 | 2 (66.7) 1 (33.3) | 2 (100) 0 (0) | 0 (0) 1 (100) | 0.33 | 2 (66.7) 1 (33.3) | - - | - - |
| Tricuspid valve replacement | 2 (1) | 1 (0.7) | 1 (1.5) | 1.0 | 2 (1.3) | 0 (0) | 1.0 |
| Mitral valve replacement | 5 (2.5) | 5 (3.8) | 0 (0) | 0.17 | 3 (1.9) | 0 (0) | 1.0 |
| Coronary artery bypass grafting | 65 (32.5) | 23 (34.3) | 42 (31.6) | 0.69 | 51 (32.5) | 11 (31.4) | 0.9 |
| Ascending aorta replacement | 11 (5.5) | 9 (6.8) | 2 (3) | 0.34 | 9 (5.7) | 1 (2.9) | 0.69 |
| Pulmonary vein ablation | 14 (7) | 11 (8.3) | 3 (4.5) | 0.39 | 13 (8.3) | 1 (2.9) | 0.47 |
| Left atrial appendage clip | 11 (5.5) | 10 (7.5) | 1 (1.5) | 0.1 | 10 (6.4) | 1 (2.9) | 0.69 |
| REDO cardiac surgery | 23 (11.5) | 21 (15.8) | 2 (3) | 0.007 | 21 (13.4) | 1 (2.9) | 0.08 |
| Myectomy | 1 (0.5) | 1 (0.7) | 0 (0) | 1.0 | 1 (0.6) | 0 (0) | 1.0 |
| Surgeon * | |||||||
| 1 2 3 4 5 | 104 (52) 58 (29) 4 (2) 27 (13.5) 7 (3.5) | 64 (48.1) 40 (30.1) 4 (3) 22 (16.5) 3 (2.3) | 40 (59.7) 18 (26.9) 0 (0) 5 (7.5) 4 (6) | 0.09 | 83 (52.9) 45 (28.7) 0 (0) 3 (8.6) 4 (11.4) | 18 (51.4) 10 (28.6) 4 (2) 27 (13.5) 7 (3.5) | 0.07 |
| Partial sternotomy | 64 (32) | 35 (26.3) | 29 (43.3) | 0.015 | 51 (32.5) | 13 (37.1) | 0.59 |
| Clamp time, minutes | 74.8 ± 31.3 66.5 (53; 84.7) | 75.6 ± 30.9 69 (53.5; 86) | 73 ± 32.3 60 (53; 83) | 0.27 | 74.2 ± 30.5 68 (53; 84.5) | 69.1 ± 29 60 (52; 70) | 0.14 |
| Cardiopulmonary bypass time, minutes | 111.3 ± 46.2 97 (82; 126) | 113.6 ± 46.3 102 (84; 129) | 106.5 ± 45.8 90 (79; 115) | 0.17 | 110.6 ± 43.1 99 (83; 126) | 98.9 ± 38.3 87 (77; 105) | 0.05 |
| Duration of surgery, minutes | 206.8 ± 67.6 186 (160; 238) | 210.6 ± 67.9 188 (164; 240) | 199.4 ± 66.7 180 (156; 220) | 0.16 | 208 ± 65.5 190 (164; 239) | 182.3 ± 51.7 175 (146; 195) | 0.01 |
| Total | New LBBB after AVR | Persistent New LBBB 1 Year after AVR | |||||
|---|---|---|---|---|---|---|---|
| No (n = 133) | Yes (n = 67) | p-Value | No (n = 157) | Yes (n = 35) | p-Value | ||
| Duration of hospital stay, days | 17.5 ± 12.2 14 (11.7; 18) | 18.8 ± 12.7 15 (12; 21) | 15 ± 10.7 13 (10; 15) | 0.002 | 18.5 ± 13.3 14 (12; 19) | 13.4 ± 3 14 (11; 15) | 0.03 |
| In-hospital mortality | 6 (3) | 5 (3.8) | 1 (1.5) | 0.66 | 0 (0) | 0 (0) | - |
| Atrioventricular block III | 19 (9.5) | 16 (12.1) | 3 (4.5) | 0.08 | 15 (9.6) | 4 (11.4) | 0.75 |
| Mean gradient after operation, mmHg | 8.5 ± 3.4 8 (6; 11) | 8.5 ± 3.5 8.4 (5.9; 11) | 8.4 ± 3.3 8 (6; 11) | 0.91 | 8.4 ± 3.3 8 (6; 11) | 8.4 ± 3.6 8 (5.7; 11) | 0.99 |
| Aortic valve insufficiency | |||||||
| 0 1 2 | 171 (87.7) 22 (11.3) 2 (1.03%) | 111 (86.7) 16 (12.5) 2 (1.3) | 171 (87.7) 22 (11.3) 2 (1) | 0.7 | 138 (88.5) 16 (10.3) 2 (1.3) | 29 (82.9) 6 (17.1) 0 (0) | 0.53 |
| Paravalvular leak | |||||||
| 0 1 2 | 178 (91.3) 15 (7.7) 2 (1) | 115 (89.8) 12 (9.4) 1 (0.8) | 63 (94) 3 (4.5) 1 (1.5) | 0.48 | 141 (90.4) 13 (8.3) 2 (1.3) | 33 (94.3) 2 (5.7) 0 (0) | 0.4 |
| Stroke | 7 (3.5) | 6 (4.5) | 1 (1.5) | 0.42 | 6 (3.8) | 0 (0) | 0.59 |
| Dialysis | 11 (5.5) | 9 (6.8) | 2 (3) | 0.34 | 6 (3.8) | 0 (0) | 0.59 |
| ECMO use | 3 (1.5) | 3 (2.3) | 0 (0) | 0.55 | 2 (1.3) | 0 (0) | 1.0 |
| Pacemaker after AVR | 24 (12) | 21 (15.8) | 3 (4.5) | 0.02 | 20 (12.7) | 3 (8.6) | 0.77 |
| AICD | 5 (2.5) | 4 (3) | 1 (1.5) | 0.66 | 5 (3.2) | 0 (0) | 0.58 |
| CRTD | 1 (0.5) | 1 (0.7) | 0 (0) | 1.0 | 0 (0) | 1 (2.9) | 0.18 |
| Wound-healing disturbance | 7 (3.5) | 7 (5.3) | 0 (0) | 0.1 | 7 (4.5) | 0 (0) | 0.35 |
| Total | New LBBB after AVR | Persistent New LBBB 1 Year after AVR | |||||
|---|---|---|---|---|---|---|---|
| No (n = 133) | Yes (n = 67) | p-Value | No (n = 157) | Yes (n = 35) | p-Value | ||
| Mortality | 8 (4) | 7 (5.3) | 1 (1.5) | 0.27 | - | - | - |
| Sinus rhythm | 59 (30.7) | 7 (5.6) | 52 (78.8) | <0.001 | 29 (18.5) | 30 (85.7) | <0.001 |
| Atrial fibrillation | 11 (5.7) | 5 (4) | 6 (9.1) | 0.19 | 6 (3.8) | 5 (14.3) | 0.03 |
| RBBB | 8 (4.2) | 7 (5.6) | 1 (1.5) | 0.26 | 8 (5.1) | 0 (0) | 0.35 |
| LBBB | 35 (18.2) | 2 (1.6) | 33 (50) | <0.001 | 0 (0) | 35 (100) | <0.001 |
| LAHB | 6 (3.1) | 3 (2.4) | 3 (4.5) | 0.41 | 6 (3.8) | 0 (0) | 0.59 |
| Pacemaker | 15 (7.8) | 11 (8.7) | 4 (6.1) | 0.51 | 11 (7) | 4 (11.4) | 0.48 |
| New pacemaker implantation during follow-up | 1 (0.5) | 0 (0) | 1 (1.5) | 0.34 | 0 (0) | 1 (2.9) | 0.18 |
| AICD | 1 (0.5) | 0 (0) | 1 (1.5) | 0.34 | 1 (0.6) | 0 (0) | 1.0 |
| CRTD | 3 (1.6) | 3 (2.4) | 0 (0) | 0.55 | 2 (1.3) | 1 (2.9) | 0.45 |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| New LBBB after aortic valve replacement | |||
| Euroscore II, % | 0.834 | 0.720–0.936 | <0.001 |
| REDO operation, yes vs. no | 0.164 | 0.026–0.584 | 0.003 |
| Partial sternotomy, yes vs. no | 2.137 | 1.151–3.978 | 0.016 |
| PM after AVR, yes vs. no | 0.250 | 0.057–0.761 | 0.012 |
| Length of hospital stay, days | 0.963 | 0.922–0.995 | 0.021 |
| Persistent new LBBB one year after aortic valve replacement | |||
| Body mass index, kg/m2 | 0.916 | 0.837–0.997 | 0.042 |
| Euroscore II, % | 0.831 | 0.669–0.972 | 0.015 |
| REDO operation, yes vs. no | 0.190 | 0.010–0.962 | 0.043 |
| Length of operation, days | 0.992 | 0.983–0.999 | 0.018 |
| Length of hospital stay, days | 0.905 | 0.820–0.973 | 0.002 |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| New LBBB after aortic valve replacement (no vs. yes) | |||
| Euroscore II, % | 1.202 | 1.063–1.404 | 0.001 |
| Body mass index, kg/m2 | 1.067 | 0.995–1.148 | 0.068 |
| PM implantation after AVR, yes vs. no | 3.126 | 0.981–13.902 | 0.054 |
| Persistent new LBBB one year after aortic valve replacement (yes vs. no) | |||
| Atrial fibrillation, yes vs. no | 17.622 | 3.029–152.422 | 0.001 |
| The length of hospital stay, days | 0.896 | 0.806–0.969 | 0.001 |
| Body mass index, kg/m2 | 0.873 | 0.788–0.959 | 0.004 |
| RBBB after AVR, yes vs. no | 0.054 | 0.002–0.476 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Januszek, R.; Balan, R. Predictors of New and Persistent New Left Bundle Branch Block One Year after the Implantation of a Sutureless and Rapid-Deployment Aortic Valve Prosthesis. Diseases 2023, 11, 100. https://doi.org/10.3390/diseases11030100
Januszek R, Balan R. Predictors of New and Persistent New Left Bundle Branch Block One Year after the Implantation of a Sutureless and Rapid-Deployment Aortic Valve Prosthesis. Diseases. 2023; 11(3):100. https://doi.org/10.3390/diseases11030100
Chicago/Turabian StyleJanuszek, Rafał, and Robert Balan. 2023. "Predictors of New and Persistent New Left Bundle Branch Block One Year after the Implantation of a Sutureless and Rapid-Deployment Aortic Valve Prosthesis" Diseases 11, no. 3: 100. https://doi.org/10.3390/diseases11030100
APA StyleJanuszek, R., & Balan, R. (2023). Predictors of New and Persistent New Left Bundle Branch Block One Year after the Implantation of a Sutureless and Rapid-Deployment Aortic Valve Prosthesis. Diseases, 11(3), 100. https://doi.org/10.3390/diseases11030100







