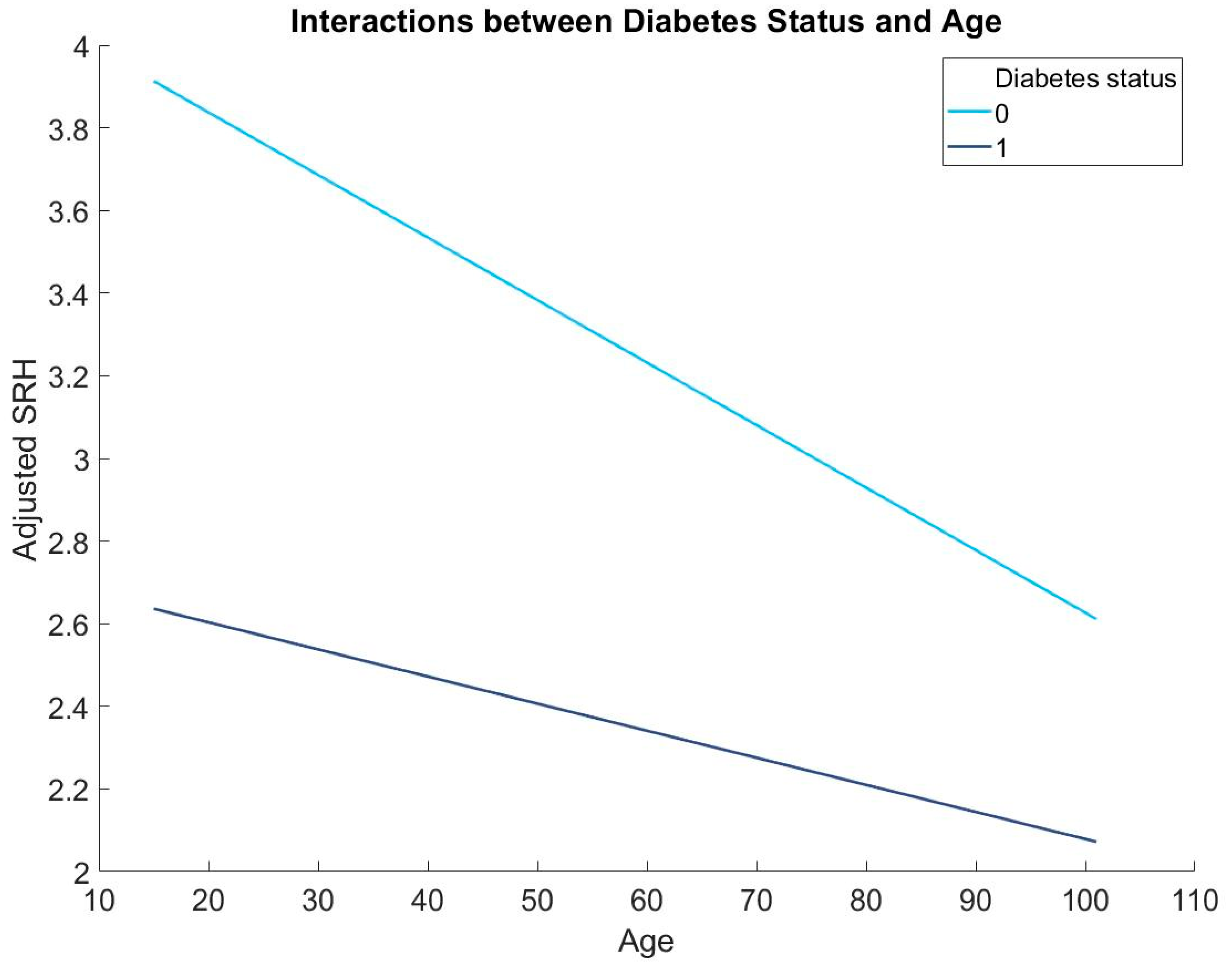
People with Diabetes Have Poorer Self-Rated Health (SRH) and Diabetes Moderates the Association between Age and SRH
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, N.; Gariépy, G.; Smith, K.J.; Malla, A.; Boyer, R.; Strychar, I.; Lesage, A.; Wang, J. Trajectories of self-rated health in people with diabetes: Associations with functioning in a prospective community sample. PLoS ONE 2013, 8, e83088. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.; Marmot, M.; Oldfield, Z.; Smith, J.P. Disease and disadvantage in the United States and in England. JAMA 2006, 295, 2037–2045. [Google Scholar] [CrossRef]
- Dowd, J.B.; Zajacova, A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int. J. Epidemiol. 2007, 36, 1214–1221. [Google Scholar] [CrossRef]
- Shavelle, R.M.; MacKenzie, R.; Paculdo, D.R. Inflammation, disability and morbidity in aging. Aging Dis. 2021, 12, 1–14. [Google Scholar]
- Waller, G. Self-rated health in general practice: A plea for subjectivity. Br. J. Gen. Pract. 2015, 65, 110–111. [Google Scholar] [CrossRef]
- Cullinan, J.; Gillespie, P. Does Overweight and Obesity Impact on Self-Rated Health? Evidence Using Instrumental Variables Ordered Probit Models. Health Econ. 2016, 25, 1341–1348. [Google Scholar] [CrossRef]
- Harris, S.; Hagenaars, S.; Davies, G.; Hill, D.; Liewald, D.; Ritchie, S.; Marioni, R.; METASTROKE Consortium; International Consortium for Blood Pressure Genome-Wide Association Studies; International Consortium for Blood Pressure Genome-Wide Association Studies; et al. Molecular genetic contributions to self-rated health. Int. J. Epidemiol. 2016, 46, 994–1009. [Google Scholar] [CrossRef] [PubMed]
- Zarini, G.; Vaccaro, J.; Terris, M.C.; Exebio, J.; Tokayer, L.; Antwi, J.; Ajabshir, S.; Cheema, A.; Huffman, F. Lifestyle behaviors and self-rated health: The living for health program. J. Environ. Public Health 2014, 2014, 315042. [Google Scholar] [CrossRef]
- Warnoff, C.; Lekander, M.; Hemmingsson, T.; Sorjonen, K.; Melin, B. Anna Andreasson Is poor self-rated health associated with low-grade inflammation in 43,110 late adolescent men of the general population? A cross-sectional study. BMJ Open 2016, 6, e009440. [Google Scholar] [CrossRef]
- Kim, E.S.; Hagan, K.A.; Grodstein, F.; DeMeo, D.L.; De Vivo, I.; Kubzansky, L.D. Optimism and cause-specific mortality: A prospective cohort study. Am. J. Epidemiol. 2017, 185, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Bao, W.; Liu, J.; Ouyang, Y.-Y.; Wang, D.; Rong, S.; Xiao, X.; Shan, Z.-L.; Zhang, Y.; Yao, P.; et al. Inflammatory markers and risk of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2013, 36, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Christian, L.; Glaser, R.; Porter, K.; Malarkey, W.; Beversdorf, D.; Kiecolt-Glaser, J. Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology 2011, 36, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Jylhä, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009, 69, 307–316. [Google Scholar] [CrossRef]
- Du, S.; Lu, B.; Zhai, F.; Popkin, B.M. A new stage of the nutrition transition in China. Public Health Nutr. 2002, 5, 169–174. [Google Scholar] [CrossRef]
- Lee, H.-W.; Song, M.; Yang, J.J.; Kang, D. Determinants of poor self-rated health in Korean adults with diabetes. J. Prev. Med. Public Health 2015, 48, 287. [Google Scholar] [CrossRef]
- Taloyan, M.; Wajngot, A.; Johansson, S.-E.; Tovi, J.; Sundquist, J. Poor self-rated health in adult patients with type 2 diabetes in the town of Södertälje: A cross-sectional study. Scand. J. Prim. Health Care 2010, 28, 216–220. [Google Scholar] [CrossRef]
- Latham, K.; Peek, C.W. Self-rated health and morbidity onset among late midlife US adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2012, 68, 107–116. [Google Scholar]
- Wennberg, P.; Rolandsson, O.; van der A, D.; Spijkerman, A.; Kaaks, R.; Boeing, H.; Feller, S.; Bergmann, M.; Langenberg, C.; Sharp, S.; et al. Self-rated health and type 2 diabetes risk in the European Prospective Investigation into Cancer and Nutrition-InterAct study: A case-cohort study. BMJ Open 2013, 3, e002436. [Google Scholar] [CrossRef]
- Lara-Cinisomo, S.; Loret de Mola, J.R.; Flores-Carter, K.; Tabb, K.M.; Roloff, K. Prenatal Depressive Symptoms, Self-Rated Health, and Diabetes Self-Efficacy: A Moderated Mediation Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13603. [Google Scholar] [CrossRef]
- Aboagye-Mensah, E.B.; Azap, R.A.; Odei, J.B.; Gray, D.M.; Nolan, T.S., 2nd; Elgazzar, R.; White, D.; Gregory, J.; Joseph, J.J. The association of ideal cardiovascular health with self-reported health, diabetes, and adiposity in African American males. Prev. Med. Rep. 2020, 19, 101151. [Google Scholar] [CrossRef] [PubMed]
- Wuorela, M.; Lavonius, S.; Salminen, M.; Vahlberg, T.; Viitanen, M.; Viikari, L. Self-rated health and objective health status as predictors of all-cause mortality among older people: A prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Zajacova, A.; Huzurbazar, S.; Todd, M. Gender and the structure of self-rated health across the adult life span. Soc. Sci. Med. 2017, 187, 58–66. [Google Scholar] [CrossRef] [PubMed]
- University of Essex; Institute for Social and Economic Research. Understanding Society: Waves 1–11, 2009–2020 and Harmonised BHPS: Waves 1–18, 1991–2009 [Data Collection], 16th ed.; UK Data Service. SN, 2022; p. 6614. [Google Scholar]
- Moradpour, F.; Piri, N.; Dehghanbanadaki, H.; Moradi, G.; Fotouk-Kiai, M.; Moradi, Y. Socio-demographic correlates of diabetes self-reporting validity: A study on the adult Kurdish population. BMC Endocr. Disord. 2022, 22, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, O.; Manderbacka, K. Assessing reliability of a measure of self-rated health. Scand. J. Soc. Med. 1996, 24, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Al-Khaledi, M.; Al-Dousari, H.; Al-Dhufairi, S.; Al-Mousawi, T.; Al-Azemi, R.; Al-Azimi, F.; Badr, H.E. Impact of diabetes self-care management on quality of life among type 2 diabetic patients in primary health care in Kuwait: A cross-sectional study. BMC Public Health 2019, 19, 68. [Google Scholar]
- Fisher, L.; Hessler, D.M.; Polonsky, W.H.; Mullan, J. When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care 2012, 35, 259–264. [Google Scholar] [CrossRef]
- Wu, S.F.V.; Courtney, M.; Edwards, H.; McDowell, J.; Shortridge-Baggett, L.M.; Chang, P.J. Self-efficacy, self-care behaviors, and glycemic control among Taiwanese with type 2 diabetes. J. Nurs. Scholarsh. 2013, 45, e30–e38. [Google Scholar]
- Badawi, G.; Gariépy, G.; Pagé, V.; Schmitz, N. Indicators of self-rated health in the Canadian population with diabetes. Diabet. Med. 2012, 29, 1021–1028. [Google Scholar] [CrossRef]
- Seaquist, E.R. The final frontier: How does diabetes affect the brain? Diabetes 2010, 59, 4. [Google Scholar] [CrossRef]
- Zhang, T.; Shaw, M.; Cherbuin, N. Association between type 2 diabetes mellitus and brain atrophy: A meta-analysis. Diabetes Metab. J. 2022, 46, 781–802. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.A.; Walker, R.J.; Smalls, B.L.; Egede, L.E. Glucose control in diabetes: The impact of racial differences on monitoring and outcomes. Endocrine 2016, 53, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Ichida, Y.; Hirai, H.; Kondo, K.; Kawachi, I.; Takeda, T.; Endo, H. Does social participation improve self-rated health in the older population? A quasi-experimental intervention study. Soc. Sci. Med. 2013, 94, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Seiwert, K.A.; Butler, L.; Maynard, D.; Kinkade, M.; Nill, D.T. Improving Adolescent Self-Rated Health Using a Multiple Health Behavior Change eHealth Intervention. Am. J. Health Educ. 2022, 53, 35–44. [Google Scholar] [CrossRef]
- Abuladze, L.; Kunder, N.; Lang, K.; Vaask, S. Associations between self-rated health and health behaviour among older adults in A cross-sectional analysis. BMJ Open 2017, 7, e013257. [Google Scholar] [CrossRef]
| Variables | Mean | S.D. |
|---|---|---|
| Age (year) | 45.94 (15–101) | 18.14 |
| Monthly income (£) | 1219.67 (0–47, 442.9) | 1327.57 |
| SRH | 3.39 (1–5) | 1.15 |
| N | % | |
| Sex | ||
| Male | 20,913 | 44.02 |
| Female | 26,594 | 55.98 |
| Highest educational qualification | ||
| Below college | 34,245 | 72.08 |
| College | 13,262 | 27.92 |
| Present legal marital status | ||
| Single | 23,433 | 49.33 |
| Married | 24,074 | 50.67 |
| Diabetes status | ||
| Yes | 2869 | 6.04 |
| No | 44,638 | 93.96 |
| Variables | b | SE | P | 95% C.I. |
|---|---|---|---|---|
| Age | −0.02 *** | 0.00 | 0.03 | [−0.02, −0.01] |
| Sex | −0.02 *** | 0.01 | 0.00 | [−0.04, 0.00] |
| Monthly income | 0.00 *** | 0.00 | 0.00 | [0.00, 0.00] |
| Highest educational qualification | 0.31 *** | 0.01 | 0.00 | [0.29, 0.33] |
| Marital status | 0.17 *** | 0.01 | 0.00 | [0.15, 0.19] |
| Diabetes status | −1.41 *** | 0.08 | 0.00 | [−1.57, −1.24] |
| Diabetes status: Age | 0.01 | 0.00 | 0.00 | [0.01, 0.01] |
| R2 | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, W.; Malvaso, A. People with Diabetes Have Poorer Self-Rated Health (SRH) and Diabetes Moderates the Association between Age and SRH. Diseases 2023, 11, 73. https://doi.org/10.3390/diseases11020073
Kang W, Malvaso A. People with Diabetes Have Poorer Self-Rated Health (SRH) and Diabetes Moderates the Association between Age and SRH. Diseases. 2023; 11(2):73. https://doi.org/10.3390/diseases11020073
Chicago/Turabian StyleKang, Weixi, and Antonio Malvaso. 2023. "People with Diabetes Have Poorer Self-Rated Health (SRH) and Diabetes Moderates the Association between Age and SRH" Diseases 11, no. 2: 73. https://doi.org/10.3390/diseases11020073
APA StyleKang, W., & Malvaso, A. (2023). People with Diabetes Have Poorer Self-Rated Health (SRH) and Diabetes Moderates the Association between Age and SRH. Diseases, 11(2), 73. https://doi.org/10.3390/diseases11020073






