Time to Death and Associated Factors among Tuberculosis Patients in South West Ethiopia: Application of Shared Frailty Model
Abstract
1. Introduction
2. Methods
2.1. Data Source, Sampling Design, and Sample Size
2.2. Institutional Review Board Statement
2.3. Inclusion and Exclusion Criteria of the Patients
2.4. Study Variables
2.5. Statistical Analysis
2.5.1. Shared Frailty Model
2.5.2. A Shared Gamma Frailty Model
2.5.3. The Inverse Gaussian Frailty Model
2.6. Parameter Estimation
2.7. Models Comparison and Selection
3. Results
3.1. Patients’ Characteristics
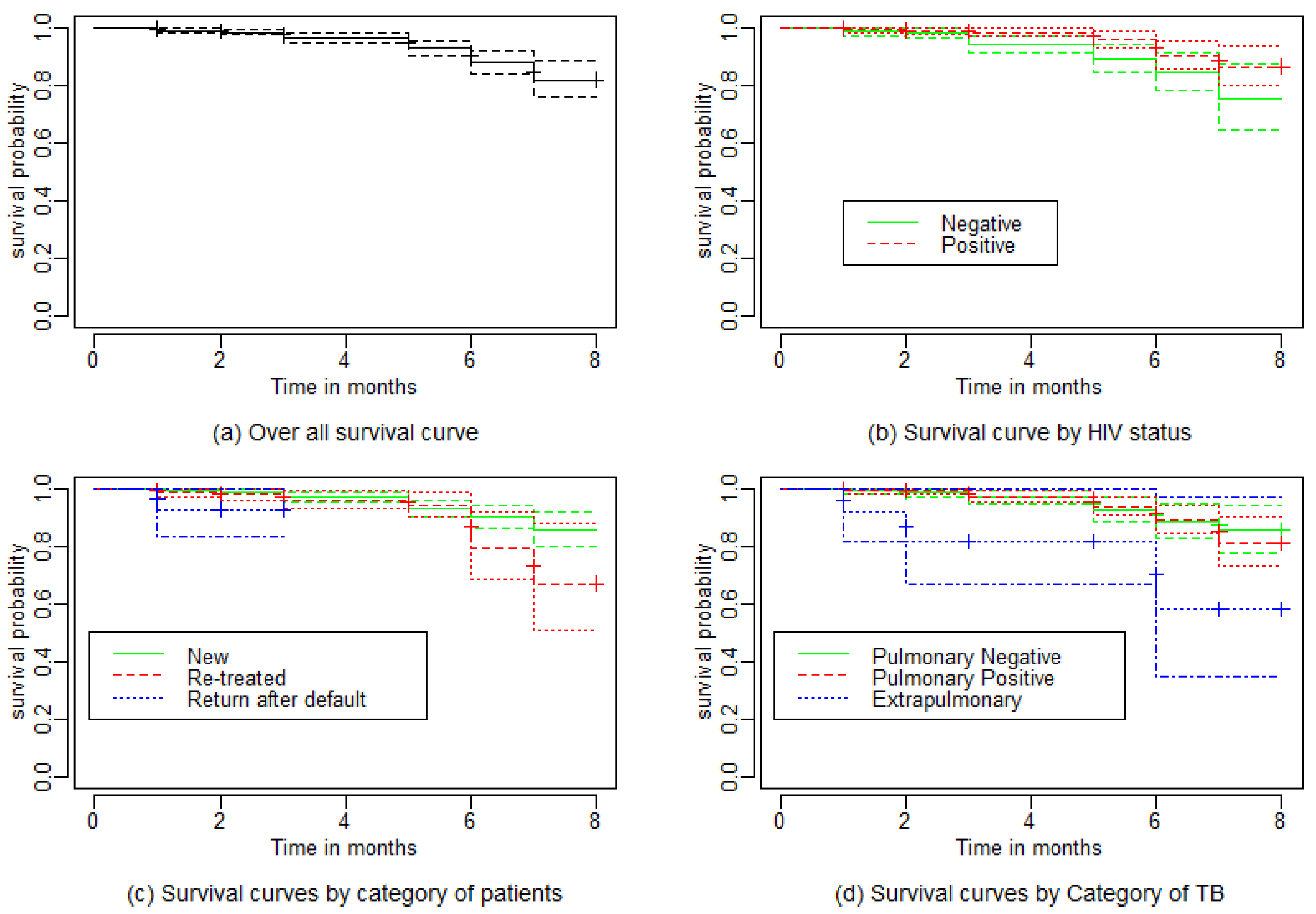
3.2. Comparison of Survival Curves
3.3. Model Selection and Inference
4. Discussion
5. Limitation and Importance of the Study
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIC | Akaki Information Criteria |
| ART | Antiretroviral therapy |
| CI | Confidence interval |
| DOTS | Directly observed treatment, short-course |
| EPTB | Extrapulmonary tuberculosis |
| HIV | Human immunodeficiency virus |
| MOH | Ministry of Health |
| TB | Tuberculosis |
| WHO | World Health Organization |
References
- Gagneux, S. Ecology and evolution of mycrobacterium tuberculosis. Nat. Rev. Microbiol. 2018, 16, 202–213. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2021: Executive Summary; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2020: Executive Summary; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Oursler, K.K.; Moore, R.D.; Bishai, W.R.; Harrington, S.M.; Pope, D.S.; Chaisson, R.E. Survival of Patients with Pulmonary Tuberculosis: Clinical and Molecular Epidemiologic Factors. Clin. Infect. Dis. 2002, 34, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Simwaka, B.N.; Nkhonjera, P.; Sanudi, L.; Gondwe, M.; Bello, G.; Chimzizi, R.; Theobald, S. The malawi national tuberculosis programme: An equity analysis. Malawi Med. J. 2007, 18, 13–18. [Google Scholar] [CrossRef][Green Version]
- Mugusi, F.M.; Mehta, S.; Villamor, E.; Urassa, W.; Saathoff, E.; Bosch, R.J.; Fawzi, W.W. Factors associated with mortality in hiv-infected and uninfected patients with pulmonary tuberculosis. BMC Public Health 2009, 9, 409. [Google Scholar] [CrossRef]
- MOH: Tuberculosis, Leprosy and TB/HIV Prevention and Control Programme Manual; Federal Ministry of Health: Addis Ababa, Ethiopia, 2008.
- MOH: Ethiopian National TB Prevalence Survey 2010–2011 Preliminary Result; Federal Ministry of Health: Addis Ababa, Ethiopia, 2011.
- Lo, H.-Y.; Suo, J.; Chang, H.-J.; Yang, S.-L.; Chou, P. Risk factors associated with death in a 12-month cohort analysis of tuberculosis patients: 12-month follow-up after registration. Asia Pac. J. Public Health 2015, 27, 758–768. [Google Scholar] [CrossRef]
- Simonovska, L.; Trajcevska, M.; Mitreski, V.; Simonovska, I. The causes of death among patients with tuberculosis. Int. J. Tuberc. Lung Dis. 2014, 18, S324. [Google Scholar]
- MOH: Guidelines for Clinical and Programmatic Managment of TB, TB/HIV and Leprosy in Ethiopia; Federal Ministry of Health: Addis Ababa, Ethiopia, 2013.
- Biadglegne, F.; Anagaw, B.; Debebe, T.; Anagaw, B.; Tesfaye, W.; Tessema, B.; Rodloff, A.C.; Sack, U. A retrospective study on the outcomes of tuberculosis treatment in felege hiwot referral hospital, northwest ethiopia. Int. J. Med. Med. Sci. 2013, 5, 85–91. [Google Scholar]
- Tessema, B.; Muche, A.; Bekele, A.; Reissig, D.; Emmrich, F.; Sack, U. Treatment outcome of tuberculosis patients at gondar university teaching hospital, northwest ethiopia. A five-year retrospective study. BMC Public Health 2009, 9, 371. [Google Scholar] [CrossRef]
- Nigus, D.; Lingerew, W.; Beyene, B.; Tamiru, A.; Lemma, M.; Melaku, M.Y. Prevalence of multi drug resistant tuberculosis among presumptive multi drug resistant tuberculosis cases in amhara national regional state, ethiopia. J. Mycobac. Dis. 2014, 4, 1068–2161. [Google Scholar] [CrossRef]
- Tolosie, K.; Sharma, M.K. Application of cox proportional hazards model in case of tuberculosis patients in selected addis ababa health centres, ethiopia. Tuberc. Res. Treat. 2014, 2014, 536976. [Google Scholar] [CrossRef]
- Vasankari, T.; Holmström, P.; Ollgren, J.; Liippo, K.; Kokki, M.; Ruutu, P. Risk factors for poor tuberculosis treatment outcome in Finland: A cohort study. BMC Public Health 2007, 7, 291. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, M.D.; Batista, J.D.; Ximenes, R.A.; Carvalho, M.S.; Diniz, G.T.; Rodrigues, L.C. Risk factors associated with death in patients who initiate treatment for tuberculosis after two different follow-up periods. Rev. Bras. Epidemiol. 2009, 12, 513–522. [Google Scholar] [CrossRef]
- Harries, A.D.; Hargreaves, N.J.; Gausi, F.; Kwanjana, J.H.; Salaniponi, F.M. High early death rate in tuberculosis patients in Malawi. Int. J. Tuberc. Lung Dis. 2001, 5, 1000–1005. [Google Scholar] [PubMed]
- Cochran, W.G. Sampling Techniques; John Wiley & Sons: Hoboken, NJ, USA, 1977. [Google Scholar]
- van der Meulen, A. Life Tables and Survival Analysis; Statstics: The Hague, The Netherlands, 2012. [Google Scholar]
- Kleinbaum, D.G.; Klein, M. Kaplan-Meier survival curves and the log-rank test. In Survival Analysis; Springer: New York, NY, USA, 2012; pp. 55–96. [Google Scholar]
- Brookmeyer, R. Median Survival Time; Wiley: Hoboken, NJ, USA, 2014. [Google Scholar]
- Gutierrez, R.G. Parametric frailty and shared frailty survival models. Stata J. 2002, 2, 22–44. [Google Scholar] [CrossRef]
- Duchateau, L.; Janssen, P. The Frailty Model; Springer: New York, NY, USA, 2008. [Google Scholar]
- Wienke, A. Frailty Models in Survival Analysis; Chapman and Hall/CRC: Boca Raton, FL, USA, 2010. [Google Scholar]
- Lemeshow, S.; May, S.; Hosmer, D.W., Jr. Applied Survival Analysis: Regression Modeling of Time-to-Event Data; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Munda, M.; Rotolo, F.; Legr, C. parfm: Parametric frailty models in R. J. Stat. Softw. 2012, 51, 1–20. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Claeskens, G.; Nguti, R.; Janssen, P. One-sided tests in shared frailty models. Test 2008, 17, 69–82. [Google Scholar] [CrossRef]
- Berhe, G.; Enquselassie, F.; Aseffa, A. Treatment outcome of smear-positive pulmonary tuberculosis patients in Tigray Region, Northern Ethiopia. BMC Public Health 2012, 12, 537. [Google Scholar] [CrossRef]
- Beza, M.G.; Wubie, M.T.; Teferi, M.D.; Getahun, Y.S.; Bogale, S.M.; Tefera, S.B. A five years tuberculosis treatment outcome at Kolla Diba Health Center, Dembia District, Northwest Ethiopia: A retrospective crosssectional analysis. J. Infect. Dis. Ther. 2013, 1, 101. [Google Scholar] [CrossRef]
- Ballayira, Y.; Yanogo, P.K.; Konaté, B.; Diallo, F.; Sawadogo, B.; Antara, S.; Méda, N. Time and risk factors for death among smear-positive pulmonary tuberculosis patients in the Health District of commune VI of Bamako, Mali, 2016. BMC Public Health 2021, 21, 942. [Google Scholar] [CrossRef]
- Xie, Y.; Han, J.; Yu, W.; Wu, J.; Li, X.; Chen, H. Survival Analysis of Risk Factors for Mortality in a Cohort of Patients with Tuberculosis. Can. Respir. J. 2020, 2020, 1654653. [Google Scholar] [CrossRef] [PubMed]
- Wu, I.L.; Chitnis, A.S.; Jaganath, D. A narrative review of tuberculosis in the United States among persons aged 65 years and older. J. Clin. Tuberc. Other Mycobact. Dis. 2022, 2022, 100321. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.I.; Ceccato, M.D.; Silveira, M.R.; Mir, S.S.; Gomes, R.M.; Haddad, J.P.; Carvalho, W.S. Predictors of mortality among individuals with tuberculosis and human immunodeficiency virus coinfection at a reference center in southeastern Brazil: A retrospective cohort study. J. Young Pharm. 2018, 10, 476. [Google Scholar] [CrossRef]
- Horne, D.J.; Hubbard, R.; Narita, M.; Exarchos, A.; Park, D.R.; Goss, C.H. Factors associated with mortality in patients with tuberculosis. BMC Infect Dis. 2010, 10, 258. [Google Scholar] [CrossRef]
- Birlie, A.; Tesfaw, G.; Dejene, T.; Woldemichael, K. Time to Death and Associated Factors among Tuberculosis Patients in Dangila Woreda, Northwest Ethiopia. PLoS ONE 2015, 10, e0144244. [Google Scholar] [CrossRef]
- Low, S.; Ang, L.W.; Cutter, J.; James, L.; Chee, C.B.; Wang, Y.T.; Chew, S.K. Mortality among tuberculosis patients on treatment in Singapore. Int. J. Tuberc. Lung Dis. 2009, 13, 328–334. [Google Scholar]
- Demissie, M.; Kebede, D. Defaulting from tuberculosis treatment at the Addis Abeba Tuberculosis Centre and factors associated with it. Ethiop Med. J. 1994, 32, 97–106. [Google Scholar]
- Girum, T.; Tariku, Y.; Dessu, S. Survival status and treatment outcome of multidrug resistant tuberculosis (MDR-TB) among patients treated in treatment initiation centers (TIC) in South Ethiopia: A retrospective cohort study. Ann. Med. Health Sci. Res. 2017, 7. Available online: https://www.amhsr.org/abstract/survival-status-and-treatment-outcome-of-multidrug-resistant-tuberculosis-mdrtb-among-patients-treated-in-treatment-init-3707.html (accessed on 17 June 2022).
- Zhao, Y.J.; Zhao, Y.H.; Zhang, X.Y.; Sun, X.J.; Liu, Y.Q.; Hou, Y.J.; Wu, J.Q.; Jia, H.; Han, Y.N.; Dong, W.; et al. First Report of Toxoplasma gondii Infection in Tuberculosis Patients in China. Vector Borne Zoonotic Dis. 2017, 17, 799–803. [Google Scholar] [CrossRef]
- Shaweno, D.; Worku, A. Tuberculosis treatment survival of HIV-positive TB patients on directly observed treatment short-course in Southern Ethiopia: A retrospective cohort study. BMC Res. Notes 2012, 5, 682. [Google Scholar] [CrossRef]
| Censored | Death | Total | ||||
|---|---|---|---|---|---|---|
| Covariates | Categories | N (%) | N (%) | N (%) | Mean | Median |
| Sex | Male | 281(93.7) | 19(6.3) | 300(49.7) | 4.286 | 3 |
| Female | 277(91.1) | 27(8.9) | 304(50.3) | 4.098 | 3 | |
| Place | Rural | 517(92.3) | 43(7.7) | 560(92.7) | 4.196 | 3 |
| Urban | 41(93.2) | 3(6.8) | 44(7.3) | 4.136 | 3 | |
| HIV status | Negative | 303(94.1) | 19(5.9) | 322(53.3) | 3.865 | 5 |
| Positive | 255(90.4) | 27(9.6) | 282(46.7) | 4.478 | 3 | |
| Smear results | Negative | 334(90.3) | 36(9.7) | 370(61.3) | 4.254 | 5 |
| Positive | 224(95.7) | 10(4.3) | 234(38.7) | 4.094 | 3 | |
| Type of TB | Pulmonary positives | 217(93.5) | 15(6.5) | 232(38.4) | 4.296 | 3 |
| Pulmonary negative | 323(92.8) | 25(7.2) | 348(57.6) | 4.116 | 5 | |
| Extrapulmonary | 18(75.0) | 6(25.0) | 24(4.0) | 3.416 | 5 | |
| Categories of TB | New | 354(92.7) | 28(7.3) | 382(63.2) | 4.662 | 5 |
| Retreated | 179(91.8) | 16(8.2) | 195(32.3) | 3.589 | 3 | |
| Return after default | 25(92.6) | 2(7.4) | 27(4.5) | 1.888 | 2 | |
| History of previous | Yes | 311(91.7) | 28(8.3) | 339(56.1) | 4.395 | 5 |
| treatment | No | 247(93.2) | 18(6.8) | 265(43.9) | 3.932 | 3 |
| Outcome | N | Percent | Mean | SD | Median | IQR | |
|---|---|---|---|---|---|---|---|
| Status of patients | |||||||
| Censored | 558 | 92.4 | 4.19 | 2.00 | 4.00 | [3.00, 6.00] | |
| Dead | 46 | 7.60 | 4.26 | 2.00 | 5.00 | [3.00, 6.00] | |
| Baseline age | 604 | 42.78 | 18.64 | 43.00 | [27.75, 58.00] | ||
| Baseline weight | 604 | 40.78 | 16.01 | 35.00 | [32.00, 53.00] | ||
| Log Rank Test | Breslow Test | ||
|---|---|---|---|
| Covariates | Categories | (p-Value) | (p-Value) |
| Sex | Male | 2.22 (0.135) | 2.21 ( 0.139) |
| Female | |||
| Place | Rural | 0.03 ( 0.857) | 0.03 (0.857) |
| Urban | |||
| HIV status | Negative | 6.20 (0.012) | 6.36 (0.011) |
| Positive | |||
| Smear results | Negative | 5.31 (0.021) | 4.90 (0.030) |
| Positive | |||
| Type of TB | Pulmonary negative | 14.14 (0.009) | 22.10 (0.000) |
| Pulmonary positives | |||
| Extra pulmonary | |||
| Category of TB | New | 7.47 (0.023) | 6.26 ( 0.045) |
| Retreated | |||
| Return after default | |||
| History of previous | Yes | 0.001 (0.979) | 0.34 (0.559) |
| treatment | No |
| Weibull | Loglogistics | lognormal | |
|---|---|---|---|
| Covariates | Estimate (se, p) | Estimate (se, p) | Estimate (se, p) |
| Sex (Male) | −0.249 (0.311, 0.423) | −0.221 (0.314, 0.481) | −0.198 (0.316, 0.531) |
| Age in years | 0.015 (0.008, 0.054) | 0.017 (0.008, 0.035) | 0.017 (0.008, 0.029) |
| Weight in Kg | −0.030 (0.011, 0.004) | −0.025 (0.011, 0.019) | −0.022 (0.011, 0.040) |
| Residence (Rural) | 0.088 (0.535, 0.869) | 0.348 (0.628, 0.579) | 0.507 (0.698, 0.468) |
| HIV status (Negative) | −0.840 (0.303, 0.006) | −0.815 (0.305, 0.007) | −0.783 (0.306, 0.010) |
| Smear results (Positive) | −0.892 (0.365, 0.015) | −0.858 (0.367, 0.019) | −0.843 (0.368, 0.022) |
| Type of TB | |||
| Pulmonary positive | 0.037 (0.322, 0.909) | 0.088 (0.329, 0.790) | 0.114 (0.333, 0.733) |
| Extrapulmonary | 1.642 (0.508, 0.001) | 1.661 (0.511, 0.001) | 1.699 (0.514, 0.001) |
| Category of patient | |||
| Re-treated | 0.653 (0.322, 0.042) | 0.653 (0.322, 0.043) | 0.618 (0.322, 0.055) |
| Return after default | 2.466 (0.795, 0.002) | 2.469 (0.805, 0.002) | 2.323 (0.794, 0.003) |
| Previous treatment history (Yes) | −0.233 (0.327, 0.477) | −0.161 (0.334, 0.630) | −0.116 (0.336, 0.729) |
| Loglikelihood | −194.797 | −195.665 | −199.025 |
| Likelihood ratio test | ( = 39.2 0.0001) | ( = 38.3, 0.0001) | ( = 36.9, 0.0001) |
| Weibull | Loglogistics | Lognormal | |
|---|---|---|---|
| Covariates | Estimate (se, p) | Estimate (se, p) | Estimate (se, p) |
| Gamma frailty model | |||
| Sex (Male) | −0.458 (0.328, 0.163) | −0.407 (0.333, 0.221) | −0.376 (0.334, 0.261) |
| Age in years | 0.022 (0.009, 0.014) | 0.023 (0.009, 0.008) | 0.023 (0.009, 0.009) |
| Weight in Kg | −0.038 (0.012, 0.001) | −0.032 (0.011, 0.004) | −0.028 (0.011, 0.012) |
| Residence (Rural) | 0.030 (0.564, 0.958) | 0.374 (0.640, 0.558) | 0.520 (0.713, 0.465) |
| HIV status (Negative) | −0.801 (0.305, 0.009) | −0.777 (0.307, 0.011) | −0.744 (0.307, 0.015) |
| Smear results (Positive) | −0.634 (0.386, 0.101) | −0.611 (0.386, 0.114) | −0.615 (0.387, 0.112) |
| Type of TB | |||
| Pulmonary positive | 0.049 (0.327, 0.880) | 0.104 (0.332, 0.755) | 0.131 (0.335, 0.696) |
| Extrapulmonary | 1.456 ( 0.525, 0.006) | 1.505 (0.525, 0.004) | 1.567 (0.525, 0.003) |
| Category of patient | |||
| Re-treated | 0.762 (0.326, 0.020) | 0.758 (0.328, 0.021) | 706 (0.327, 0.031) |
| Return after default | 2.591 (0.810, 0.001) | 2.593 (0.818, 0.002) | 2.437 (0.805, 0.002) |
| Previous treatment history (Yes) | −0.226 (0.331, 0.494) | −0.144 (0.332, 0.664) | −0.100 (0.334, 0.765) |
| Kendal’s | 0.106 | 0.098 | 0.09 |
| Loglikelihood | −192.17 | −193.386 | −197.062 |
| Likelihood Ratio Test | ( = 5.254, 0.012) | ( = 4.123, 0.000) | ( = 3.421, 0.000) |
| Inverse-Gaussian frailty model | |||
| Sex (Male) | −0.454 (0.329, 0..168) | −0.405 (0.334, 0.225) | −0.373 (0.335, 0.266) |
| Age in years | 0.021 (0.009, 0.015) | 0.023 (0.009, 0.009) | 0.023 (0.009, 0.009) |
| Weight in Kg | −0.038 (0.012, 0.001) | −0.032 (0.011, 0.005) | −0.028 (0.011, 0.012) |
| Residence (Rural) | 0.031 (0.568, 0.956) | 0.372 (0.639, 0.560) | 0.519 (0.713, 0.466) |
| HIV status (Negative) | −0.802 (0.305, 0.009) | −0.778 (0.307, 0.011) | −0.745 (0.307, 0.015) |
| Smear results (Positive) | −0.640 (0.386, 0.097) | −0.616 (0.386, 0.111) | −0.619 (0.38, 0.110) |
| Type of TB | |||
| Pulmonary positive | 0.049 (0.327, 0.880) | 0.104 (0.332, 0.755) | 0.131 (0.335, 0.697) |
| Extrapulmonary | 1.461 (0.526, 0.006) | 1.509 (0.527, 0.004) | 1.570 (0.527, 0.003) |
| Category of patient | |||
| Re-treated | 0.760 (0.327, 0.020) | 0.756 (0.328, 0.021) | 0.704 (0.327, 0.031) |
| Return after default | 2.588 (0.811, 0.001) | 2.591 (0.818, 0.002) | 2.435 (0.805, 0.002) |
| Previous treatment history (Yes) | −0.227 (0.331, 0.494) | −0.145 (0.332, 0.662) | −0.101 (0.334, 0.763) |
| Kendal’s | 0.104 | 0.092 | 0.084 |
| Loglikelihood | −192.219 | −193.421 | −197.089 |
| Likelihood Ratio Test | ( = 8.143 0.000) | ( = 6.213, 0.000) | ( = 3.456, 0.000) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jabir, Y.N.; Aniley, T.T.; Bacha, R.H.; Debusho, L.K.; Chikako, T.U.; Hagan, J.E., Jr.; Seidu, A.-A.; Ahinkorah, B.O. Time to Death and Associated Factors among Tuberculosis Patients in South West Ethiopia: Application of Shared Frailty Model. Diseases 2022, 10, 51. https://doi.org/10.3390/diseases10030051
Jabir YN, Aniley TT, Bacha RH, Debusho LK, Chikako TU, Hagan JE Jr., Seidu A-A, Ahinkorah BO. Time to Death and Associated Factors among Tuberculosis Patients in South West Ethiopia: Application of Shared Frailty Model. Diseases. 2022; 10(3):51. https://doi.org/10.3390/diseases10030051
Chicago/Turabian StyleJabir, Yasin Negash, Tafere Tilahun Aniley, Reta Habtamu Bacha, Legesse Kassa Debusho, Teshita Uke Chikako, John Elvis Hagan, Jr., Abdul-Aziz Seidu, and Bright Opoku Ahinkorah. 2022. "Time to Death and Associated Factors among Tuberculosis Patients in South West Ethiopia: Application of Shared Frailty Model" Diseases 10, no. 3: 51. https://doi.org/10.3390/diseases10030051
APA StyleJabir, Y. N., Aniley, T. T., Bacha, R. H., Debusho, L. K., Chikako, T. U., Hagan, J. E., Jr., Seidu, A.-A., & Ahinkorah, B. O. (2022). Time to Death and Associated Factors among Tuberculosis Patients in South West Ethiopia: Application of Shared Frailty Model. Diseases, 10(3), 51. https://doi.org/10.3390/diseases10030051










