Design and Evaluation of a Hip-Only Actuated Lower Limb Exoskeleton for Lightweight Gait Assistance
Abstract
1. Introduction
2. Materials and Methods
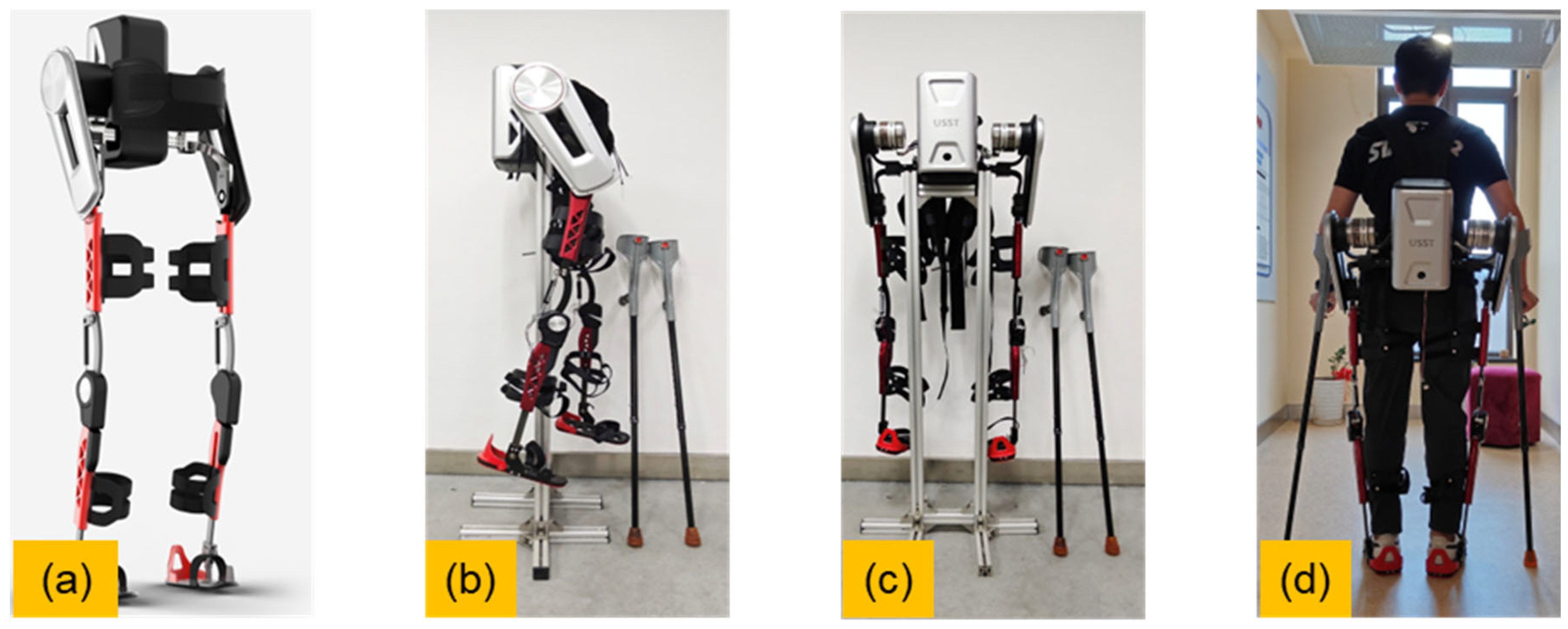
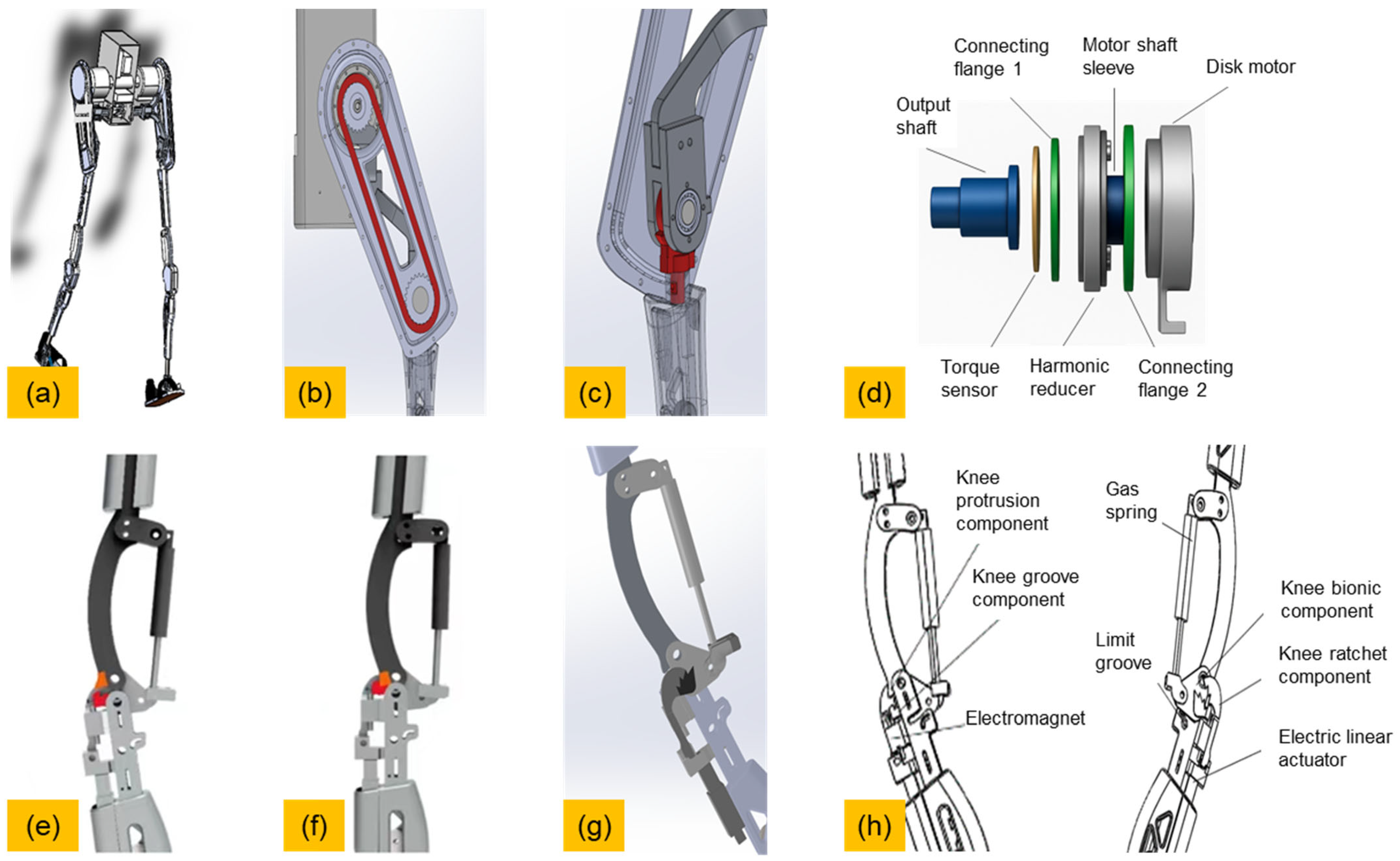
2.1. System Overview
- A rigid structural frame made of aluminum alloy;
- A brushless DC motor that actuates the bilateral hip joints via a belt-driven transmission;
- A passive knee joint with an electromagnetically controlled mechanical latch;
- A gas spring and ratchet mechanism for sit-to-stand assistance (inactive during walking).
2.2. Mechanical Structure
2.3. Sensing and Gait Phase Recognition
- Inertial Measurement Units (IMUs)
- Torque Sensors
- Joint Angle Encoders
- Foot Pressure Sensors
- During heel strike (HS), p4 (heel) dominates.
- During foot flat (FF), all pi values are near equilibrium.
- During swing, all pi values are zero.
- During heel off (HO), p1 and p2 (forefoot) increases significantly.
2.4. Control Architecture
3. Results
3.1. Human Subject Evaluation
3.2. Exoskeleton Output Torque
3.3. Gait Compliance
3.4. Evaluation of Assistive Effect
4. Discussion
5. Conclusions
- Active hip actuation is achieved via a brushless DC motor that delivers assistive torque for hip flexion and extension;
- The knee joint adopts a structurally passive design, integrated with an electromagnetically actuated locking mechanism. This allows active unlocking at the beginning of the swing phase for compliant motion, and automatic locking during stance to ensure joint stability;
- The control system fuses plantar pressure data and inertial measurements to enable real-time gait phase recognition and synchronized fuzzy PID torque control;
- An auxiliary gas spring–ratchet module is included to facilitate sit-to-stand transitions, without interfering with normal walking dynamics.
- Significant reduction in lower-limb muscle loading, as evidenced by decreased surface electromyography (sEMG) activation levels;
- Smooth and symmetric hip joint trajectories under assistive control;
- Rapid control responsiveness with sensor-to-actuator delays consistently under 40 ms, enabling accurate synchronization with gait events;
- Reliable passive locking behavior of the knee joint during dynamic overground walking.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PID | Proportional Integral Derivative |
| FSM | Finite State Machine |
| DC | Direct current |
| IMU | Inertial Measurement Unit |
| FSR | Force Sensing Resistor |
| CGA | Clinical Gait Analysis |
| STM32 | STMicroelectronics 32-bit Series Microcontroller Chip |
| sEMG | Surface Electromyography |
| RMS | Root Mean Square |
| MTH | Metatarsal Head |
References
- Yu, X.; Cai, Y.; Yang, R.; Ma, F.; Kim, W. Revisiting Sensor-Based Intelligent Fall Risk Assessment for Older People: A Systematic Review. Eng. Appl. Artif. Intell. 2025, 144, 110176. [Google Scholar] [CrossRef]
- Moon, S.W. Gait and Cognitive Function in the Elderly with AD Dementia, MCI and Healthy. Alzheimer’s Dement. 2024, 20, e083970. [Google Scholar] [CrossRef]
- Lai, X.; Bo, L.; Zhu, H.; Chen, B.; Wu, Z.; Du, H.; Huo, X. Effects of Lower Limb Resistance Exercise on Muscle Strength, Physical Fitness, and Metabolism in Pre-Frail Elderly Patients: A Randomized Controlled Trial. BMC Geriatr. 2021, 21, 447. [Google Scholar] [CrossRef] [PubMed]
- Parraca, J.A.; Adsuar, J.C.; Domínguez-Muñoz, F.J.; Barrios-Fernandez, S.; Tomas-Carus, P. Test-Retest Reliability of Isokinetic Strength Measurements in Lower Limbs in Elderly. Biology 2022, 11, 802. [Google Scholar] [CrossRef] [PubMed]
- Sitthiracha, P.; Eungpinichpong, W.; Chatchawan, U. Effect of Progressive Step Marching Exercise on Balance Ability in the Elderly: A Cluster Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 3146. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T.; Imai, A.; Fujimoto, M.; Kurihara, T.; Kagawa, K.; Nagata, T.; Sanada, K. Adverse Effects of the Coexistence of Locomotive Syndrome and Sarcopenia on the Walking Ability and Performance of Activities of Daily Living in Japanese Elderly Females: A Cross-Sectional Study. J. Phys. Ther. Sci. 2020, 32, 227–232. [Google Scholar] [CrossRef]
- Romanato, M.; Spolaor, F.; Beretta, C.; Fichera, F.; Bertoldo, A.; Volpe, D.; Sawacha, Z. Quantitative Assessment of Training Effects Using EksoGT® Exoskeleton in Parkinson’s Disease Patients: A Randomized Single Blind Clinical Trial. Contemp. Clin. Trials Commun. 2022, 28, 100926. [Google Scholar] [CrossRef]
- Wiśniowska-Szurlej, A.; Wołoszyn, N.; Brożonowicz, J.; Ciąpała, G.; Pietryka, K.; Grzegorczyk, J.; Leszczak, J.; Ćwirlej-Sozańska, A.; Sozański, B.; Korczowski, B. Enhanced Rehabilitation Outcomes of Robotic-Assisted Gait Training with EksoNR Lower Extremity Exoskeleton in 19 Stroke Patients. Med. Sci. Monit. 2023, 29, e940511-1–e940511-10. [Google Scholar] [CrossRef]
- Tefertiller, C.; Hays, K.; Jones, J.; Jayaraman, A.; Hartigan, C.; Bushnik, T.; Forrest, G.F. Initial Outcomes from a Multicenter Study Utilizing the Indego Powered Exoskeleton in Spinal Cord Injury. Top. Spinal Cord. Inj. Rehabil. 2018, 24, 78–85. [Google Scholar] [CrossRef]
- Awad, L.N.; Esquenazi, A.; Francisco, G.E.; Nolan, K.J.; Jayaraman, A. The ReWalk ReStoreTM Soft Robotic Exosuit: A Multi-Site Clinical Trial of the Safety, Reliability, and Feasibility of Exosuit-Augmented Post-Stroke Gait Rehabilitation. J. Neuroeng. Rehabil. 2020, 17, 80. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X.; Zheng, J.; Chen, G.; Jiao, G.; Peng, S. Integration of Spinal Musculoskeletal System Parameters for Predicting OVCF in the Elderly: A Comprehensive Predictive Model. Glob. Spine J. 2024, 15, 1966–1975. [Google Scholar] [CrossRef] [PubMed]
- Nasr, A.; Zhu, K.; McPhee, J. Using Musculoskeletal Models to Generate Physically-Consistent Data for 3D Human Pose, Kinematic, Dynamic, and Muscle Estimation. Multibody Syst. Dyn. 2024, 64, 737–770. [Google Scholar] [CrossRef]
- Chiu, K.I.A.; Taylor, C.; Saha, P.; Geddes, J.; Bishop, T.; Bernard, J.; Lui, D. Actively Controlled Exoskeletons Show Improved Function and Neuroplasticity Compared to Passive Control: A Systematic Review. Glob. Spine J. 2025, 21925682251343529. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, W.; Wan, C.; Wu, X.; Huang, J.; Wang, X.; Huang, G.; Ding, W.; Chen, Y.; Yang, J.; et al. Exoskeleton Rehabilitation Robot Training for Balance and Lower Limb Function in Sub-Acute Stroke Patients: A Pilot, Randomized Controlled Trial. J. Neuroeng. Rehabil. 2024, 21, 98. [Google Scholar] [CrossRef]
- Ma, Y.; Liu, D.; Yan, Z.; Yu, L.; Gui, L.; Yang, C.; Yang, W. Optimizing Exoskeleton Assistance: Muscle Synergy-Based Actuation for Personalized Hip Exoskeleton Control. Actuators 2024, 13, 54. [Google Scholar] [CrossRef]
- Kim, Y.-S. Effects of a Walking Program Using the “WalkON” Mobile App among College Students. Digit. Health 2024, 10, 20552076241269463. [Google Scholar] [CrossRef]
- Grimmer, M.; Zhao, G. Hip Exoskeleton for Cycling Assistance. Bioengineering 2024, 11, 683. [Google Scholar] [CrossRef]
- Shushtari, M.; Arami, A. Human–Exoskeleton Interaction Force Estimation in Indego Exoskeleton. Robotics 2023, 12, 66. [Google Scholar] [CrossRef]
- Fang, Q.; Xu, T.; Zheng, T.; Cai, H.; Zhao, J.; Zhu, Y. A Rehabilitation Training Interactive Method for Lower Limb Exoskeleton Robot. Math. Probl. Eng. 2022, 2022, 2429832. [Google Scholar] [CrossRef]
- Changcheng, C.; Li, Y.-R.; Chen, C.-T. Assistive Mobility Control of a Robotic Hip-Knee Exoskeleton for Gait Training. Sensors 2022, 22, 5045. [Google Scholar] [CrossRef]
- Haufe, F.L.; Kober, A.M.; Wolf, P.; Riener, R.; Xiloyannis, M. Learning to Walk with a Wearable Robot in 880 Simple Steps: A Pilot Study on Motor Adaptation. J. Neuroeng. Rehabil. 2021, 18, 157. [Google Scholar] [CrossRef]
- Kunyou, H.; Lumin, C. Research of Fuzzy PID Control for Lower Limb Wearable Exoskeleton Robot. In Proceedings of the 2021 4th International Conference on Intelligent Autonomous Systems (ICoIAS), Wuhan, China, 14–16 May 2021; IEEE: Piscataway, NJ, USA; pp. 385–389. [Google Scholar]
- Li, C.; He, Y.; Chen, T.; Chen, X.; Tian, S. Real-Time Gait Event Detection for a Lower Extremity Exoskeleton Robot by Infrared Distance Sensors. IEEE Sens. J. 2021, 21, 27116–27123. [Google Scholar] [CrossRef]
- Zhang, Y.-P.; Cao, G.-Z.; Li, L.-L.; Diao, D.-F. Interactive Control of Lower Limb Exoskeleton Robots: A Review. IEEE Sens. J. 2024, 24, 5759–5784. [Google Scholar] [CrossRef]
- Pérez-Ibarra, J.C.; Siqueira, A.A.G.; Krebs, H.I. Identification of Gait Events in Healthy Subjects and With Parkinson’s Disease Using Inertial Sensors: An Adaptive Unsupervised Learning Approach. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 2933–2943. [Google Scholar] [CrossRef]
- Moeller, T.; Beyerlein, M.; Herzog, M.; Barisch-Fritz, B.; Marquardt, C.; Dežman, M.; Mombaur, K.; Asfour, T.; Woll, A.; Stein, T.; et al. Human Motor Performance Assessment with Lower Limb Exoskeletons as a Potential Strategy to Support Healthy Aging—A Perspective Article. Prog. Biomed. Eng. 2025, 7, 013001. [Google Scholar] [CrossRef]
- Awad, L.N.; Bae, J.; O’Donnell, K.; De Rossi, S.M.M.; Hendron, K.; Sloot, L.H.; Kudzia, P.; Allen, S.; Holt, K.G.; Ellis, T.D.; et al. A Soft Robotic Exosuit Improves Walking in Patients after Stroke. Sci. Transl. Med. 2017, 9, eaai9084. [Google Scholar] [CrossRef]
- Delfi, G.; Al Bochi, A.; Dutta, T. A Scoping Review on Minimum Foot Clearance Measurement: Sensing Modalities. Int. J. Environ. Res. Public Health 2021, 18, 10848. [Google Scholar] [CrossRef]
- Shahini, N.; Bahrami, Z.; Sheykhivand, S.; Marandi, S.; Danishvar, M.; Danishvar, S.; Roosta, Y. Automatically Identified EEG Signals of Movement Intention Based on CNN Network (End-To-End). Electronics 2022, 11, 3297. [Google Scholar] [CrossRef]
- Chaisaen, R.; Autthasan, P.; Mingchinda, N.; Leelaarporn, P.; Kunaseth, N.; Tammajarung, S.; Manoonpong, P.; Mukhopadhyay, S.C.; Wilaiprasitporn, T. Decoding EEG Rhythms During Action Observation, Motor Imagery, and Execution for Standing and Sitting. IEEE Sens. J. 2020, 20, 13776–13786. [Google Scholar] [CrossRef]
- Gurve, D.; Delisle-Rodriguez, D.; Romero-Laiseca, M.; Cardoso, V.; Loterio, F.; Bastos, T.; Krishnan, S. Subject-Specific EEG Channel Selection Using Non-Negative Matrix Factorization for Lower-Limb Motor Imagery Recognition. J. Neural Eng. 2020, 17, 026029. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zhang, X.; Liu, K.; Shi, T.; Wang, J. A Multi-Joint Continuous Motion Estimation Method of Lower Limb Using Least Squares Support Vector Machine and Zeroing Neural Network Based on sEMG Signals. Neural Process Lett. 2023, 55, 2867–2884. [Google Scholar] [CrossRef]
- Sun, T.; Hu, Q.; Gulati, P.; Atashzar, S.F. Temporal Dilation of Deep LSTM for Agile Decoding of sEMG: Application in Prediction of Upper-Limb Motor Intention in NeuroRobotics. IEEE Robot. Autom. Lett. 2021, 6, 6212–6219. [Google Scholar] [CrossRef]
- Cao, W.; Ma, Y.; Chen, C.; Zhang, J.; Wu, X. Hardware Circuits Design and Performance Evaluation of a Soft Lower Limb Exoskeleton. IEEE Trans. Biomed. Circuits Syst. 2022, 16, 384–394. [Google Scholar] [CrossRef]
- Bajpai, A.; Carrasquillo, C.; Carlson, J.; Park, J.; Iyengar, D.; Herrin, K.; Young, A.J.; Mazumdar, A. Design and Validation of a Versatile High Torque Quasidirect Drive Hip Exoskeleton. IEEE/ASME Trans. Mechatron. 2024, 29, 789–797. [Google Scholar] [CrossRef]
- Wu, B.; Lv, J.; Chen, X.; Fang, S.; Pan, W.; Qiang, L.; Song, D. Design and Performance Evaluation Method of Wearable Hip Joint Power-Assisted Exoskeleton. Biomed. Signal Process. Control 2025, 101, 107229. [Google Scholar] [CrossRef]
- Cao, W.; Zhang, Z.; Chen, C.; He, Y.; Wang, D.; Wu, X. Biomechanical and Physiological Evaluation of a Multi-Joint Exoskeleton with Active-Passive Assistance for Walking. Biosensors 2021, 11, 393. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.; Shen, M.; Liu, H.; Zhao, Y.; Qian, Q.; Wang, W.; Yu, H.; Zhang, M. A Cable-Driven Exoskeleton with Personalized Assistance Improves the Gait Metrics of People in Subacute Stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 2560–2569. [Google Scholar] [CrossRef]
- Jeong, Y.J.; Kazerooni, H. Design of Low Profile Actuators for Medical Exoskeletons. In Proceedings of the ASME 2015 International Mechanical Engineering Congress and Exposition, Houston, TX, USA, 13–19 November 2015; American Society of Mechanical Engineers: New York, NY, USA, 2015; p. V003T03A094. [Google Scholar]
- Tiwari, R.S.; Das, T.K.; Tripathy, A.K.; Li, K.-C. Gait Identification Based on Deepwalk Features Using CNN and LSTM: An Advanced Biometric Approach. Telecommun. Syst. 2025, 88, 83. [Google Scholar] [CrossRef]
- Vidyarani, K.R.; Talasila, V.; Umar, R.; Prem, V.; Jagannath, R.P.K.; Prashanth, G.R. Inertial Sensor-Based Heel Strike and Energy Expenditure Prediction Using a Hybrid Machine Learning Approach. Digit. Health 2025, 11, 20552076251333375. [Google Scholar] [CrossRef]
- Luo, M.; Yin, M.; Li, J.; Li, Y.; Kobsiriphat, W.; Yu, H.; Xu, T.; Wu, X.; Cao, W. Lateral Walking Gait Recognition and Hip Angle Prediction Using a Dual-Task Learning Framework. Cyborg Bionic Syst. 2025, 6, 0250. [Google Scholar] [CrossRef]
- Laganà, F.; Pellicanò, D.; Arruzzo, M.; Pratticò, D.; Pullano, S.A.; Fiorillo, A.S. FEM-Based Modelling and AI-Enhanced Monitoring System for Upper Limb Rehabilitation. Electronics 2025, 14, 2268. [Google Scholar] [CrossRef]
- Lin, Y.; Zhang, Y.; Zhong, W.; Xiong, W.; Xi, Z.; Chen, Y.-F.; Zhang, M. Leveraging Extended Windows in End-to-End Deep Learning for Improved Continuous Myoelectric Locomotion Prediction. IEEE Trans. Neural Syst. Rehabil. Eng. 2025, 33, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, X.; Ma, W.; Gao, S. Piezoresistive Plantar Pressure Sensors and CNN-Based Body Weight and Load Estimation. Med. Biol. Eng. Comput. 2025; ahead of print. [Google Scholar] [CrossRef]







| Height (mm) | Hip Width (mm) | Thigh Length (mm) | Calf Length (mm) | Percentile (%) |
|---|---|---|---|---|
| 1545 | 273 | 414 | 324 | 1 |
| 1588 | 282 | 427 | 338 | 5 |
| 1608 | 288 | 436 | 345 | 10 |
| 1683 | 306 | 466 | 370 | 50 |
| 1755 | 327 | 495 | 397 | 90 |
| 1776 | 334 | 505 | 403 | 95 |
| 1815 | 346 | 521 | 420 | 99 |
| Height (mm) | Hip Width (mm) | Thigh Length (mm) | Calf Length (mm) | Percentile (%) |
|---|---|---|---|---|
| 1449 | 275 | 387 | 300 | 1 |
| 1481 | 290 | 402 | 313 | 5 |
| 1503 | 296 | 410 | 319 | 10 |
| 1470 | 317 | 438 | 344 | 50 |
| 1640 | 340 | 467 | 370 | 90 |
| 1659 | 346 | 476 | 376 | 95 |
| 1697 | 360 | 494 | 390 | 99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Li, H.; Su, Y.; Xie, D.; Tong, R.K.Y.; Yu, H. Design and Evaluation of a Hip-Only Actuated Lower Limb Exoskeleton for Lightweight Gait Assistance. Electronics 2025, 14, 3853. https://doi.org/10.3390/electronics14193853
Li M, Li H, Su Y, Xie D, Tong RKY, Yu H. Design and Evaluation of a Hip-Only Actuated Lower Limb Exoskeleton for Lightweight Gait Assistance. Electronics. 2025; 14(19):3853. https://doi.org/10.3390/electronics14193853
Chicago/Turabian StyleLi, Ming, Hui Li, Yujie Su, Disheng Xie, Raymond Kai Yu Tong, and Hongliu Yu. 2025. "Design and Evaluation of a Hip-Only Actuated Lower Limb Exoskeleton for Lightweight Gait Assistance" Electronics 14, no. 19: 3853. https://doi.org/10.3390/electronics14193853
APA StyleLi, M., Li, H., Su, Y., Xie, D., Tong, R. K. Y., & Yu, H. (2025). Design and Evaluation of a Hip-Only Actuated Lower Limb Exoskeleton for Lightweight Gait Assistance. Electronics, 14(19), 3853. https://doi.org/10.3390/electronics14193853








