Remote Patient Monitoring Applications in Healthcare: Lessons from COVID-19 and Beyond
Abstract
1. Introduction
2. Methodology
3. Results
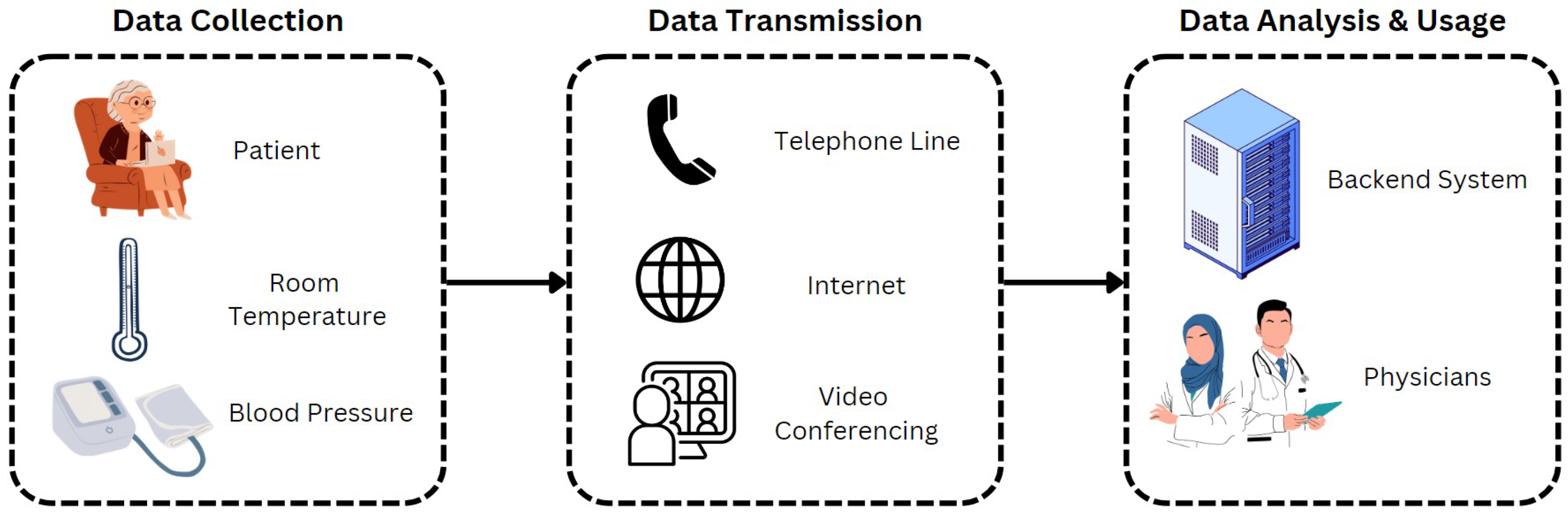
3.1. Remote Monitoring of Patients (RPM)
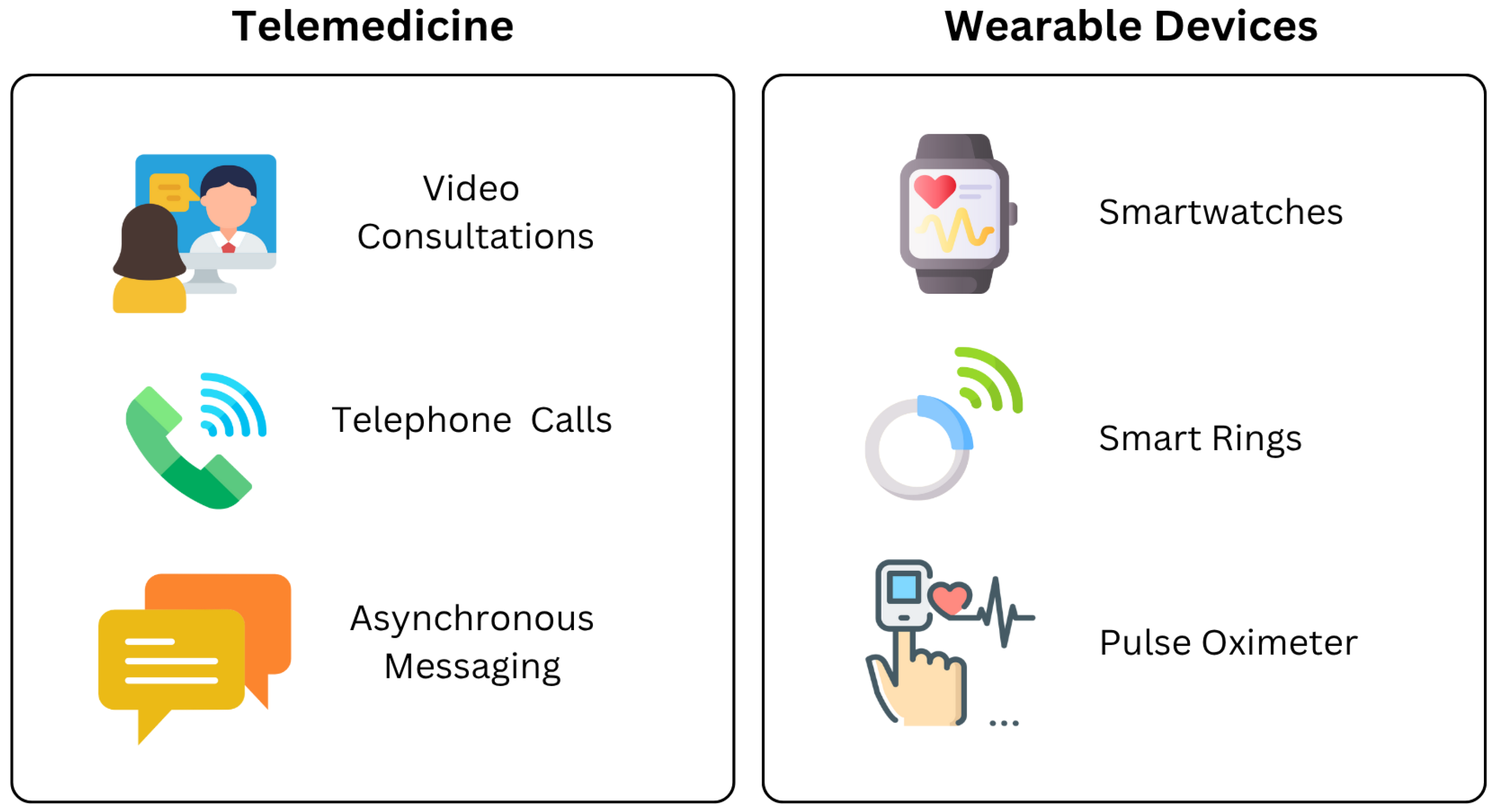
3.2. Telemedicine
3.3. Wearable Devices (WD)
4. Discussion
4.1. Telemedicine Adoption Patterns and Implications
4.2. Wearable Device Adoption and Clinical Applications
4.3. Technical Adaptations for COVID-19 Monitoring
4.4. RPM in the ERA of Long COVID and Future Preparedness
4.5. Ethical, Privacy, and Regulatory Challenges
4.6. Future Implications and Healthcare System Integration
- Infrastructure and Interoperability: Investment in modern digital infrastructure with the ability to seamlessly integrate data from RPM sources.
- Training and Workforce Development: Comprehensive training programs for healthcare providers are needed for data interpretation skills and effective virtual communication skills.
- Reimbursement: Clear guidelines on data privacy and reimbursement programs to encourage RPM use beyond post COVID-19.
- Addressing the Digital Divide: Reducing the digital divide is essential in fostering equal access across all groups of patients.
- Standardized Protocols: Developing and implementing standardized protocols for incorporating RPM data into chronic disease management and preventive care.
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duncan, D. COVID-19 data sharing and collaboration. Commun. Inf. Syst. 2021, 21, 325–340. [Google Scholar] [CrossRef]
- Williams, J.S.; Walker, R.J.; Egede, L.E. Achieving equity in an evolving healthcare system: Opportunities and challenges. Am. J. Med. Sci. 2016, 351, 33–43. [Google Scholar] [CrossRef]
- Cicatiello, J.S. A perspective of health care in the past—Insights and challenges for a health care system in the new millennium. Nurs. Adm. Q. 2000, 25, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; DiMilia, P.R.; Seo, L.M.; Fortuna, K.L.; Kennedy, M.A.; Blunt, H.B.; Bagley, P.J.; Brooks, J.; Brooks, E.; Kim, S.Y.; et al. Effectiveness of ambulatory telemedicine care in older adults: A systematic review. J. Am. Geriatr. Soc. 2019, 67, 1737–1749. [Google Scholar] [CrossRef] [PubMed]
- Lo, J.; Rae, M.; Amin, K.; Cox, C. Outpatient Telehealth Use Soared Early in the COVID-19 Pandemic but Has Since Receded. 2022. Available online: https://www.kff.org/coronavirus-COVID-19/issue-brief/outpatient-telehealth-use-soared-early-in-the-COVID-19-pandemic-but-has-since-receded/ (accessed on 1 November 2024).
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Clowse, M.E.; Overton, R.; Adagarla, B.; Economou-Zavlanos, N.; Cavalier, J.; Henao, R.; Piccini, J.P.; Thomas, L.; Pencina, M.J.; et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am. Heart J. 2021, 231, 1–5. [Google Scholar] [CrossRef]
- Helou, S.; El Helou, E.; Abou-Khalil, V.; Wakim, J.; El Helou, J.; Daher, A.; El Hachem, C. The effect of the COVID-19 pandemic on physicians’ use and perception of telehealth: The case of Lebanon. Int. J. Environ. Res. Public Health 2020, 17, 4866. [Google Scholar] [CrossRef]
- Jiménez-Rodríguez, D.; Santillán García, A.; Montoro Robles, J.; Rodríguez Salvador, M.d.M.; Muñoz Ronda, F.J.; Arrogante, O. Increase in video consultations during the COVID-19 pandemic: Healthcare professionals’ perceptions about their implementation and adequate management. Int. J. Environ. Res. Public Health 2020, 17, 5112. [Google Scholar] [CrossRef]
- Gomez, T.; Anaya, Y.B.; Shih, K.J.; Tarn, D.M. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J. Am. Board Fam. Med. 2021, 34, S61–S70. [Google Scholar] [CrossRef]
- El Naamani, K.; Abbas, R.; Mukhtar, S.; El Fadel, O.; Sathe, A.; Kazan, A.S.; El Hajjar, R.; Sioutas, G.S.; Tjoumakaris, S.I.; Bhaskar, S.M.M.; et al. Telemedicine during and post-COVID-19: The insights of neurosurgery patients and physicians. J. Clin. Neurosci. 2022, 99, 204–211. [Google Scholar] [CrossRef]
- Kyle, M.A.; Blendon, R.J.; Findling, M.G.; Benson, J.M. Telehealth use and satisfaction among US households: Results of a national survey. J. Patient Exp. 2021, 8, 23743735211052737. [Google Scholar] [CrossRef] [PubMed]
- Gordon, W.J.; Henderson, D.; DeSharone, A.; Fisher, H.N.; Judge, J.; Levine, D.M.; MacLean, L.; Sousa, D.; Su, M.Y.; Boxer, R. Remote patient monitoring program for hospital discharged COVID-19 patients. Appl. Clin. Inform. 2020, 11, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, R.; Katthula, V.; Moustakas, E. Patterns of use and key predictors for the use of wearable health care devices by US adults: Insights from a national survey. J. Med. Internet Res. 2020, 22, e22443. [Google Scholar] [CrossRef] [PubMed]
- Sanches, C.A.; Silva, G.A.; Librantz, A.F.H.; Sampaio, L.M.M.; Belan, P.A. Wearable Devices to Diagnose and Monitor the Progression of COVID-19 Through Heart Rate Variability Measurement: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2023, 25, e47112. [Google Scholar] [CrossRef]
- Esmaeilpour, Z.; Natarajan, A.; Su, H.W.; Faranesh, A.; Friel, C.; Zanos, T.P.; D’Angelo, S.; Heneghan, C. Detection of Common Respiratory Infections, Including COVID-19, Using Consumer Wearable Devices in Health Care Workers: Prospective Model Validation Study. JMIR Form. Res. 2024, 8, e53716. [Google Scholar] [CrossRef]
- Khondakar, K.R.; Kaushik, A. Role of wearable sensing technology to manage long COVID. Biosensors 2022, 13, 62. [Google Scholar] [CrossRef]
- Singh, J.; Albertson, A.; Sillerud, B. Telemedicine during COVID-19 crisis and in post-pandemic/post-vaccine world—Historical overview, current utilization, and innovative practices to increase utilization. Healthcare 2022, 10, 1041. [Google Scholar] [CrossRef]
- Hincapié, M.A.; Gallego, J.C.; Gempeler, A.; Piñeros, J.A.; Nasner, D.; Escobar, M.F. Implementation and usefulness of telemedicine during the COVID-19 pandemic: A scoping review. J. Prim. Care Community Health 2020, 11, 2150132720980612. [Google Scholar] [CrossRef]
- Perisetti, A.; Goyal, H. Successful distancing: Telemedicine in gastroenterology and hepatology during the COVID-19 pandemic. Dig. Dis. Sci. 2021, 66, 945–953. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Khan, J.Y.; Yuce, M.R.; Karami, F. Performance evaluation of a wireless body area sensor network for remote patient monitoring. In Proceedings of the 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 1266–1269. [Google Scholar]
- El-Rashidy, N.; El-Sappagh, S.; Islam, S.R.; El-Bakry, H.M.; Abdelrazek, S. Mobile health in remote patient monitoring for chronic diseases: Principles, trends, and challenges. Diagnostics 2021, 11, 607. [Google Scholar] [CrossRef] [PubMed]
- Farias, F.A.C.D.; Dagostini, C.M.; Bicca, Y.D.A.; Falavigna, V.F.; Falavigna, A. Remote patient monitoring: A systematic review. Telemed. e-Health 2020, 26, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Leichter, S.B.; Bowman, K.; Adkins, R.A.; Jelsovsky, Z. Impact of remote management of diabetes via computer: The 360 study—A proof-of-concept randomized trial. Diabetes Technol. Ther. 2013, 15, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Men, J. Lack of Reimbursement Barrier to Telehealth Adoption. Am. J. Manag. Care 2015. Available online: https://www.ajmc.com/view/lack-of-reimbursement-barrier-to-telehealth-adoption (accessed on 1 November 2024).
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. Telemedicine 2020 and the next decade. Lancet 2020, 395, 859. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J.; Shaw, S.; Morrison, C. Video consultations for COVID-19. BMJ 2020, 368, m998. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef]
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef]
- Di Rienzo, M.; Rizzo, F.; Parati, G.; Brambilla, G.; Ferratini, M.; Castiglioni, P. MagIC system: A new textile-based wearable device for biological signal monitoring. Applicability in daily life and clinical setting. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 17–18 January 2006; pp. 7167–7169. [Google Scholar]
- Dias, D.; Paulo Silva Cunha, J. Wearable health devices—Vital sign monitoring, systems and technologies. Sensors 2018, 18, 2414. [Google Scholar] [CrossRef] [PubMed]
- Jeong, I.; Bychkov, D.; Searson, P.C. Wearable devices for precision medicine and health state monitoring. IEEE Trans. Biomed. Eng. 2018, 66, 1242–1258. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Wen, D.; Liang, L.; Jia, Y.; Gao, L.; Lei, J. Evaluating the validity of current mainstream wearable devices in fitness tracking under various physical activities: Comparative study. JMIR mHealth uHealth 2018, 6, e9754. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, K.; Selvam, G.; Narayanamurthy, G. Determinants of the adoption of wearable devices for health and fitness: A meta-analytical study. Commun. Assoc. Inf. Syst. 2022, 50, 23. [Google Scholar] [CrossRef]
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A survey of wearable devices and challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620. [Google Scholar] [CrossRef]
- Kim, T.B.; Ho, C.T.B. Validating the moderating role of age in multi-perspective acceptance model of wearable healthcare technology. Telemat. Inform. 2021, 61, 101603. [Google Scholar] [CrossRef]
- Kukreti, S.; Lu, M.T.; Yeh, C.Y.; Ko, N.Y. Physiological Sensors Equipped in Wearable Devices for Management of Long COVID Persisting Symptoms: Scoping Review. J. Med. Internet Res. 2025, 27, e69506. [Google Scholar] [CrossRef]
- Cao, M.; Ramezani, R.; Katakwar, V.K.; Zhang, W.; Boda, D.; Wani, M.; Naeim, A. Developing remote patient monitoring infrastructure using commercially available cloud platforms. Front. Digit. Health 2024, 6, 1399461. [Google Scholar] [CrossRef]
- Channa, A.; Popescu, N.; Skibinska, J.; Burget, R. The rise of wearable devices during the COVID-19 pandemic: A systematic review. Sensors 2021, 21, 5787. [Google Scholar] [CrossRef]
| RPM | Specific Types | Studies |
|---|---|---|
| Telemedicine | Video conferences, Telephone calls | [5,6,7,8,9,10,11,12] |
| Wearable Devices | Invasive sensors, Non-invasive sensors | [13,14,15,16,17] |
| Study | Study Focus | Study Design | Population Size | Key Findings |
|---|---|---|---|---|
| [5] | Telemedicine | Time-series analysis | 41 million outpatient visits from 94 Epic Cosmos contributors | Telehealth usage surged from <1% to 13% during the pandemic, later stabilizing at 8%. Young patients were the primary users of telemedicine. |
| [6] | Telemedicine | Retrospective analysis at NYU Langone Health | 115,789 patients, 2656 providers | A 683% increase in urgent care telemedicine visits. Daily urgent care visits grew from 102.4 to 801.6. Telemedicine use was highest among patients aged from 20 to 44. Daily non-urgent video visits increased from <50 to 7000+. |
| [7] | Telemedicine | Retrospective cohort study at Duke University Health | 22,156 outpatient cardiology encounters in 2020 | About 9.3% of scheduled visits in 2020 were telemedicine visits. In 2020, telehealth users were generally younger and had fewer comorbidities than in-person attendees. |
| [8] | Telemedicine | Mixed-methods physician study in Lebanon | 140 physicians in Lebanon | Showed a significant positive shift in physicians’ perceptions and engagement with telemedicine. Clinical interactions via internet/phone increased during the pandemic. |
| [9] | Telemedicine | Qualitative interview study in Spain | 53 healthcare professionals in Spain | A total of 96.2% professionals considered video consultations satisfactory, especially for chronic patients; 90.6% considered it necessary to train and educate professionals in this modality. |
| [10] | Telemedicine | Qualitative interview study in Southern California | 15 primary care physicians | Physicians could observe patients’ home environments, assessing safety and support systems. Absence of in-person exams reduced diagnostic confidence. Managing telemedicine with regular duties raised concerns about provider burnout. |
| [11] | Telemedicine | Retrospective patient and physician survey | 93 patients, 33 physicians | High patient satisfaction (77%); physicians were comfortable diagnosing via telemedicine. 46.7% of patients encountered technological issues. Physicians’ primary limitations was the inability to perform physical examination. |
| [12] | Telemedicine | Cross-sectional U.S. household survey | 3454 US households | About 86% of users reported positive experiences; use was higher in urban, higher-income households. |
| [13] | Wearable Devices | Prospective cohort study of post-discharge RPM | 225 enrolled patients | An RPM program using patient-entered data was associated with minimized readmission rates. |
| [14] | Wearable Devices | Systematic review of wearables for COVID-19 | 9 studies, 10,558 participants | Consumer wearables measuring HRV demonstrated potential in detecting and predicting COVID-19. |
| [15] | Wearable Devices | Prospective validation of wearable alerting algorithm | 470 healthcare workers | Achieved 90% detection rate for PCR-confirmed COVID-19. |
| [16] | Wearable Devices | Narrative review of wearables for long COVID | N/A | Suggested that wearables can help better control and manage long COVID in a personalized way. |
| [17] | Wearable Devices | Scoping review of wearables for long COVID | 11 studies reviewed | Wearables are feasible for monitoring long COVID symptoms. Identified 10 different devices. Concluded more robust, controlled trials are needed to establish clinical guidelines. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.; Duncan, D. Remote Patient Monitoring Applications in Healthcare: Lessons from COVID-19 and Beyond. Electronics 2025, 14, 3084. https://doi.org/10.3390/electronics14153084
Khan A, Duncan D. Remote Patient Monitoring Applications in Healthcare: Lessons from COVID-19 and Beyond. Electronics. 2025; 14(15):3084. https://doi.org/10.3390/electronics14153084
Chicago/Turabian StyleKhan, Azrin, and Dominique Duncan. 2025. "Remote Patient Monitoring Applications in Healthcare: Lessons from COVID-19 and Beyond" Electronics 14, no. 15: 3084. https://doi.org/10.3390/electronics14153084
APA StyleKhan, A., & Duncan, D. (2025). Remote Patient Monitoring Applications in Healthcare: Lessons from COVID-19 and Beyond. Electronics, 14(15), 3084. https://doi.org/10.3390/electronics14153084











