A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues
Abstract
:1. Introduction
1.1. Major Contributions
- A thorough examination of IoT devices utilized in the healthcare industry.
- A detailed analysis of IoT-based devices and the cloud in a fog computing environment.
- Highlights of recent IoT-based research in the field of healthcare.
- A comparison of several healthcare technologies with varied ailments and sensors employed by researchers.
- Comparing past studies of various parameters of healthcare techniques.
- A visualized systematic review technique using a flow diagram.
- The methodological quality of the systematic review technique is evaluated through standard checklists.
- Highlights of various challenges and open research issues in IoT-based healthcare.
1.2. Research Motivation
1.3. Paper Organization
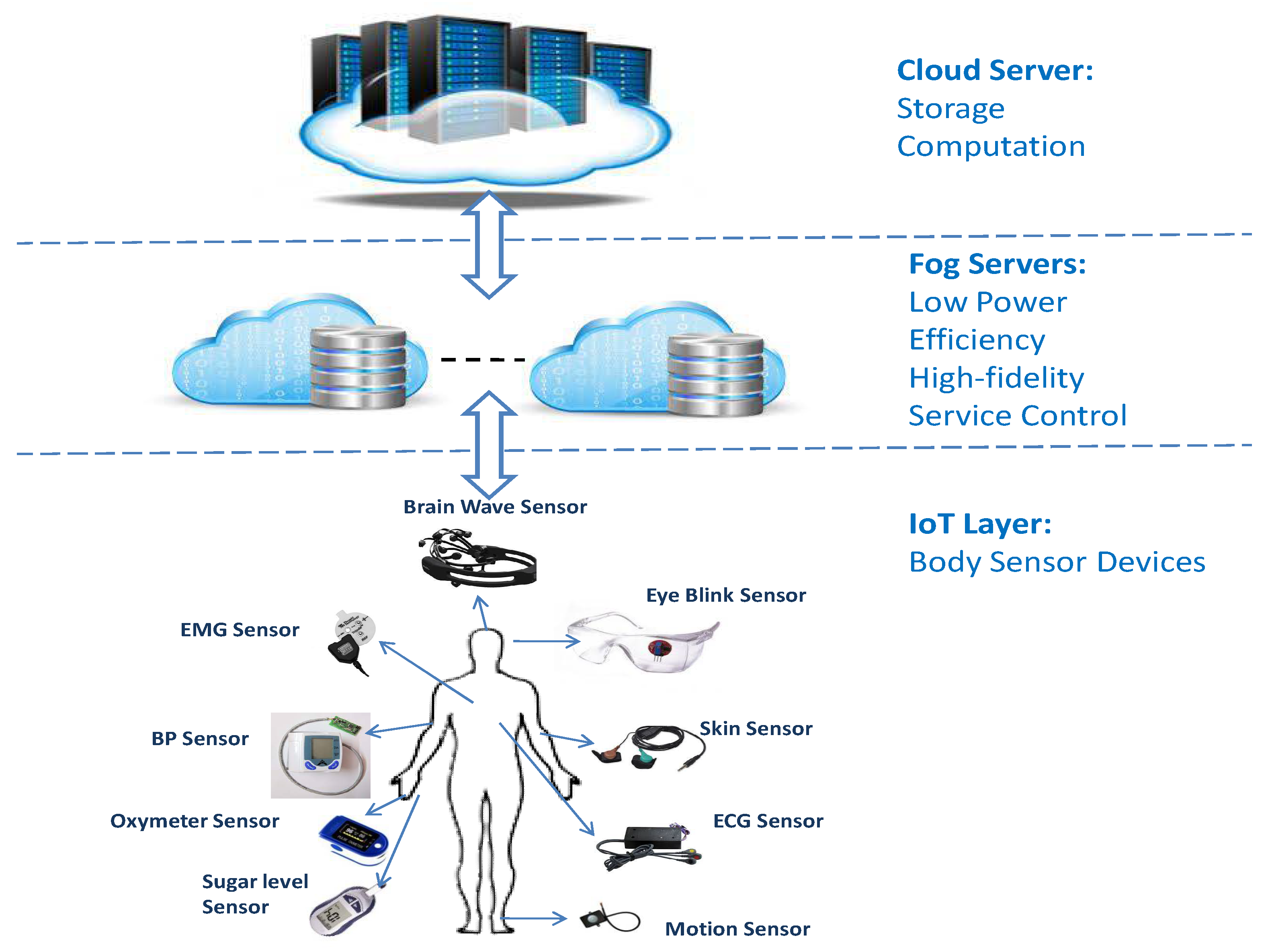
2. Background
Sensors Used
- Respiratory devices
- Sleep diagnostic devices
- Sleep apnea therapy devices
- Spiro meters
- Anesthetic meter
- Dialysis machines
- Infusion pumps
- Oxygen concentrator
- Vacuum suction pumps
- Videoscopes
- Blood sugar measuring device
- Pulse oximeters
- Computer tomographs
- Gamma probes
3. Literature Survey and Related Work
3.1. Comparison of Various Healthcare Techniques
3.2. Comparative Analysis of Various Parameters of Healthcare Techniques
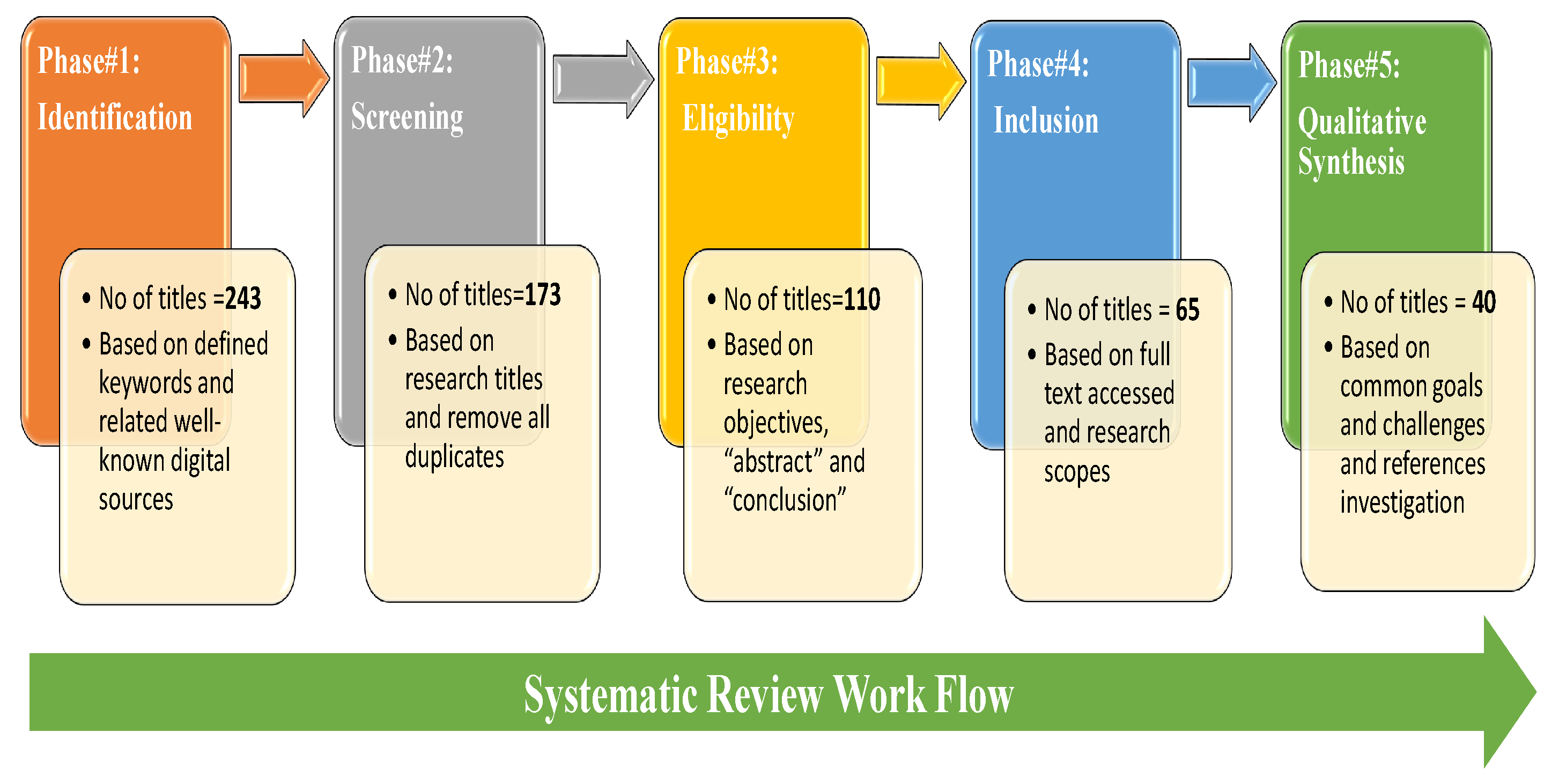
4. Review Technique
4.1. Quality Assessment of Flow-Diagram
4.2. Search Criteria
5. Challenges and Open Research Issues in Healthcare
5.1. Loss of Data
5.2. Time Limits and Prospective
5.3. Storing and Analyzing the Enormous Quantum of Unstructured Data
5.4. High Energy Consumption Issue
5.5. Discrete Transmission of Data
5.6. Security of the Data
5.7. Lack of Communication between Fog and Cloud Layer
5.8. Interoperability, Dependability, and Cost
5.9. Synchronization and Standardization
6. Discussions
7. Conclusions and Future Directions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676. [Google Scholar] [CrossRef]
- Swayamsiddha, S.; Mohanty, C. Application of cognitive Internet of Medical Things for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 911–915. [Google Scholar] [CrossRef]
- Ben Dhaou, I.; Ebrahimi, M.; Ben Ammar, M.; Bouattour, G.; Kanoun, O. Edge Devices for Internet of Medical Things: Technologies, Techniques, and Implementation. Electronics 2021, 10, 2104. [Google Scholar] [CrossRef]
- Muhammad, G.; Alhamid, M.F.; Long, X. Computing and processing on the edge: Smart pathology detection for connected healthcare. IEEE Netw. 2019, 33, 44–49. [Google Scholar] [CrossRef]
- Yang, G.; Xie, L.; Mäntysalo, M.; Zhou, X.; Pang, Z.; Xu, L.D.; Kao-Walter, S.; Chen, Q.; Zheng, L. A Health-IoT Platform Based on the Integration of Intelligent Packaging, Unobtrusive Bio-Sensor, and Intelligent Medicine Box. IEEE Trans. Ind. Inform. 2014, 10, 2180–2191. [Google Scholar] [CrossRef]
- Yan, Y.; Li, Q.; Li, H.; Zhang, X.; Wang, L. A home-based health information acquisition system. Health Inf. Sci. Syst. 2013, 1, 12. [Google Scholar] [CrossRef]
- Azimi, I.; Anzanpour, A.; Rahmani, A.M.; Liljeberg, P.; Salakoski, T. Medical warning system based on Internet of Things using fog computing. In Proceedings of the 2016 International Workshop on Big Data and Information Security (IWBIS), Jakarta, Indonesia, 18–19 October 2016; pp. 19–24. [Google Scholar]
- Kashyap, V.; Kumar, A. A Systematic Survey on Fog and IoT Enabled Healthcare. Available online: https://spast.org/techrep/article/view/3254 (accessed on 10 July 2022).
- Bibani, O.; Mouradian, C.; Yangui, S.; Glitho, R.H.; Gaaloul, W.; Hadj-Alouane, N.B.; Morrow, M.; Polakos, P. A demo of iot healthcare application provisioning in hybrid cloud/fog environment. In Proceedings of the 2016 IEEE International Conference on Cloud Computing Technology and Science (CloudCom), Luxembourg, 12–15 December 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 472–475. [Google Scholar]
- Goel, R.; Jain, A.; Verma, K.; Bhushan, M.; Kumar, A.; Negi, A. Mushrooming Trends and Technologies to Aid Visually Impaired People. In Proceedings of the 2020 International Conference on Emerging Trends in Information Technology and Engineering (ic-ETITE), Vellore, India, 24–25 February 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–5. [Google Scholar]
- Bukhari, M.M.; Ghazal, T.M.; Abbas, S.; Khan, M.; Farooq, U.; Wahbah, H.; Ahmad, M.; Adnan, K.M. An Intelligent Proposed Model for Task Offloading in Fog-Cloud Collaboration Using Logistics Regression. Comput. Intell. Neurosci. 2022, 2022, 3606068. [Google Scholar] [CrossRef]
- Cerina, L.; Notargiacomo, S.; Paccanit, M.G.; Santambrogio, M.D. A fog-computing architecture for preventive healthcare and assisted living in smart ambients. In Proceedings of the 2017 IEEE 3rd International Forum on Research and Technologies for Society and Industry (RTSI), Modena, Italy, 11–13 September 2017; pp. 1–6. [Google Scholar]
- Ben Ammar, M.; Ben Dhaou, I.; El Houssaini, D.; Sahnoun, S.; Fakhfakh, A.; Kanoun, O. Requirements for Energy-Harvesting-Driven Edge Devices Using Task-Offloading Approaches. Electronics 2022, 11, 383. [Google Scholar] [CrossRef]
- Peng, H.; Tian, Y.; Kurths, J.; Li, L.; Yang, Y.; Wang, D. Secure and energy-efficient data transmission system based on chaotic compressive sensing in body-to-body networks. IEEE Trans. Biomed. Circuits Syst. 2017, 11, 558–573. [Google Scholar] [CrossRef]
- Wang, Z.; Luo, N.; Zhou, P. GuardHealth: Blockchain empowered secure data management and Graph Convolutional Network enabled anomaly detection in smart healthcare. J. Parallel Distrib. Comput. 2020, 142, 1–12. [Google Scholar] [CrossRef]
- Manogaran, G.; Varatharajan, R.; Lopez, D.; Kumar, P.M.; Sundarasekar, R.; Thota, C. A new architecture of Internet of Things and big data ecosystem for secured smart healthcare monitoring and alerting system. Future Gener. Comput. Syst. 2018, 82, 375–387. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Gia, T.N.; Negash, B.; Anzanpour, A.; Azimi, I.; Jiang, M.; Liljeberg, P. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Future Gener. Comput. Syst. 2018, 78, 641–658. [Google Scholar] [CrossRef]
- Dang, L.M.; Piran, M.; Han, D.; Min, K.; Moon, H. A survey on internet of things and cloud computing for healthcare. Electronics 2019, 8, 768. [Google Scholar] [CrossRef]
- Rajan, J.P.; Rajan, S.E.; Martis, R.J.; Panigrahi, B.K. Fog computing employed computer aided cancer classification system using deep neural network in internet of things based healthcare system. J. Med Syst. 2020, 44, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Ding, G.; Wang, H.; Roman, H.E.; Lu, S. The fog computing service for healthcare. In Proceedings of the 2015 2nd International Symposium on Future Information and Communication Technologies for Ubiquitous HealthCare (Ubi-HealthTech), Beijing, China, 28–30 May 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 1–5. [Google Scholar]
- Kumar, A.; Kumar, R.; Sharma, A. Equal: Energy and qos aware resource allocation approach for clouds. Comput. Inform. 2018, 37, 781–814. [Google Scholar] [CrossRef]
- Sultan, N. Making use of cloud computing for healthcare provision: Opportunities and challenges. Int. J. Inf. Manag. 2014, 34, 177–184. [Google Scholar] [CrossRef]
- Kumari, A.; Tanwar, S.; Tyagi, S.; Kumar, N. Fog computing for Healthcare 4.0 environment: Opportunities and challenges. Comput. Electr. Eng. 2018, 72, 1–13. [Google Scholar] [CrossRef]
- Dautov, R.; Distefano, S.; Buyya, R. Hierarchical data fusion for Smart Healthcare. J. Big Data 2019, 6, 1–23. [Google Scholar] [CrossRef]
- Aceto, G.; Persico, V.; Pescapé, A. Industry 4.0 and health: Internet of things, big data, and cloud computing for healthcare 4.0. J. Ind. Inf. Integr. 2020, 18, 100129. [Google Scholar] [CrossRef]
- Stantchev, V.; Barnawi, A.; Ghulam, S.; Schubert, J.; Tamm, G. Smart items, fog and cloud computing as enablers of servitization in healthcare. Sens. Transducers 2015, 185, 121. [Google Scholar]
- Kaur, N.; Kumar, A.; Kumar, R. A systematic review on task scheduling in Fog computing: Taxonomy, tools, challenges, and future directions. Concurr. Comput. Pract. Exp. 2021, 33, e6432. [Google Scholar] [CrossRef]
- Verma, K.; Kumar, A.; Islam, M.S.U.; Kanwar, T.; Bhushan, M. Rank based mobility-aware scheduling in Fog computing. Inform. Med. Unlocked 2021, 24, 100619. [Google Scholar] [CrossRef]
- Pareek, K.; Tiwari, P.K.; Bhatnagar, V. Fog Computing in Healthcare: A Review. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2021; Volume 1099, p. 012025. [Google Scholar]
- Islam, M.S.U.; Kumar, A.; Hu, Y.C. Context-aware scheduling in Fog computing: A survey, taxonomy, challenges and future directions. J. Netw. Comput. Appl. 2021, 180, 103008. [Google Scholar] [CrossRef]
- Rani, R.; Kumar, N.; Khurana, M.; Kumar, A.; Barnawi, A. Storage as a service in fog computing: A systematic review. J. Syst. Archit. 2021, 116, 102033. [Google Scholar] [CrossRef]
- Bellavista, P.; Berrocal, J.; Corradi, A.; Das, S.K.; Foschini, L.; Zanni, A. A survey on fog computing for the Internet of Things. Pervasive Mob. Comput. 2019, 52, 71–99. [Google Scholar] [CrossRef]
- Awaisi, K.S.; Hussain, S.; Ahmed, M.; Khan, A.A.; Ahmed, G. Leveraging IoT and fog computing in healthcare systems. IEEE Internet Things Mag. 2020, 3, 52–56. [Google Scholar] [CrossRef]
- Alshehri, F.; Muhammad, G. A comprehensive survey of the Internet of Things (IoT) and AI-based smart healthcare. IEEE Access 2021, 9, 3660–3678. [Google Scholar] [CrossRef]
- Lakkis, S.I.; Elshakankiri, M. IoT based emergency and operational services in medical care systems. In Proceedings of the 2017 Internet of Things Business Models, Users, and Networks, Copenhagen, Denmark, 23–24 November 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1–5. [Google Scholar]
- AbdulRaheem, M.; Oladipo, I.D.; González-Briones, A.; Awotunde, J.B.; Tomori, A.R.; Jimoh, R.G. An efficient lightweight speck technique for edge-IoT-based smart healthcare systems. In 5G IoT and Edge Computing for Smart Healthcare; Elsevier: Amsterdam, The Netherlands, 2022; pp. 139–162. [Google Scholar]
- Sood, S.K.; Mahajan, I. Wearable IoT sensor based healthcare system for identifying and controlling chikungunya virus. Comput. Ind. 2017, 91, 33–44. [Google Scholar] [CrossRef]
- Zaman, U.; Mehmood, F.; Iqbal, N.; Kim, J.; Ibrahim, M. Towards Secure and Intelligent Internet of Health Things: A Survey of Enabling Technologies and Applications. Electronics 2022, 11, 1893. [Google Scholar] [CrossRef]
- de Moura Costa, H.J.; da Costa, C.A.; da Rosa Righi, R.; Antunes, R.S. Fog computing in health: A systematic literature review. Health Technol. 2020, 10, 1025–1044. [Google Scholar] [CrossRef]
- Tokognon, C.A.; Gao, B.; Tian, G.Y.; Yan, Y. Structural health monitoring framework based on Internet of Things: A survey. IEEE Internet Things J. 2017, 4, 619–635. [Google Scholar] [CrossRef]
- Dash, S.P. The Impact of IoT in Healthcare: Global Technological Change & The Roadmap to a Networked Architecture in India. J. Indian Inst. Sci. 2020, 100, 773–785. [Google Scholar] [PubMed]
- De Fazio, R.; De Vittorio, M.; Visconti, P. Innovative IoT solutions and wearable sensing systems for monitoring human biophysical parameters: A review. Electronics 2021, 10, 1660. [Google Scholar] [CrossRef]
- Malik, S.; Gupta, K.; Gupta, D.; Singh, A.; Ibrahim, M.; Ortega-Mansilla, A.; Goyal, N.; Hamam, H. Intelligent Load-Balancing Framework for Fog-Enabled Communication in Healthcare. Electronics 2022, 11, 566. [Google Scholar] [CrossRef]
- Index, C.V.N. Global Mobile Data Traffic Forecast Update, 2016–2021 White Paper; Cisco: San Jose, CA, USA, 2017; Volume 7, p. 180. [Google Scholar]
- Barnett, T.; Jain, S.; Andra, U.; Khurana, T. Cisco Visual Networking Index (Vni) Complete Forecast Update, 2017–2022; Cisco: San Jose, CA, USA, 2018; pp. 1–30. [Google Scholar]
- Pradhan, B.; Bhattacharyya, S.; Pal, K. IoT-based applications in healthcare devices. J. Healthc. Eng. 2021, 2021, 6632599. [Google Scholar] [CrossRef] [PubMed]
- Dubey, H.; Yang, J.; Constant, N.; Amiri, A.M.; Yang, Q.; Makodiya, K. Fog Data: Enhancing Telehealth Big Data Through Fog Computing. In ASE Big Data and Social Informatics 2015; Association for Computing Machinery: New York, NY, USA, 2015. [Google Scholar] [CrossRef]
- Kaur, A.; Jasuja, A. Health monitoring based on IoT using Raspberry PI. In Proceedings of the 2017 International Conference on Computing, Communication and Automation (ICCCA), Greater Noida, India, 5–6 May 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1335–1340. [Google Scholar]
- Kraemer, F.A.; Braten, A.E.; Tamkittikhun, N.; Palma, D. Fog Computing in Healthcare—A Review and Discussion. IEEE Access 2017, 5, 9206–9222. [Google Scholar] [CrossRef]
- Negash, B.; Gia, T.N.; Anzanpour, A.; Azimi, I.; Jiang, M.; Westerlund, T.; Rahmani, A.M.; Liljeberg, P.; Tenhunen, H. Leveraging fog computing for healthcare iot. In Fog Computing in the Internet of Things; Springer: Berlin/Heidelberg, Germany, 2018; pp. 145–169. [Google Scholar]
- Verma, P.; Sood, S.K. Fog Assisted-IoT Enabled Patient Health Monitoring in Smart Homes. IEEE Internet Things J. 2018, 5, 1789–1796. [Google Scholar] [CrossRef]
- Mahmud, R.; Koch, F.L.; Buyya, R. Cloud-fog interoperability in IoT-enabled healthcare solutions. In Proceedings of the 19th International Conference on Distributed Computing and Networking, Varanasi, India, 4–7 January2018; pp. 1–10. [Google Scholar]
- Nandyala, C.S.; Kim, H.K. From cloud to fog and IoT-based real-time U-healthcare monitoring for smart homes and hospitals. Int. J. Smart Home 2016, 10, 187–196. [Google Scholar] [CrossRef]
- Firouzi, F.; Rahmani, A.M.; Mankodiya, K.; Badaroglu, M.; Merrett, G.; Wong, P.; Farahani, B. Internet-of-Things and big data for smarter healthcare: From device to architecture, applications and analytics. Future Gener. Comput. Syst. 2018, 78, 583–586. [Google Scholar] [CrossRef]
- Jagadeeswari, V.; Subramaniyaswamy, V.; Logesh, R.; Vijayakumar, V. A study on medical Internet of Things and Big Data in personalized healthcare system. Health Inf. Sci. Syst. 2018, 6, 14. [Google Scholar] [CrossRef]
- Akrivopoulos, O.; Chatzigiannakis, I.; Tselios, C.; Antoniou, A. On the Deployment of Healthcare Applications over Fog Computing Infrastructure. In Proceedings of the 2017 IEEE 41st Annual Computer Software and Applications Conference (COMPSAC), Madrid, Spain, 13–17 July 2017; Volume 2, pp. 288–293. [Google Scholar]
- Sood, S.K.; Mahajan, I. A Fog-Based Healthcare Framework for Chikungunya. IEEE Internet Things J. 2018, 5, 794–801. [Google Scholar] [CrossRef]
- Gia, T.N.; Jiang, M.; Sarker, V.K.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Low-cost fog-assisted health-care IoT system with energy-efficient sensor nodes. In Proceedings of the 2017 13th International Wireless Communications and Mobile Computing Conference (IWCMC), Valencia, Spain, 26–30 June 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 1765–1770. [Google Scholar]
- Elmisery, A.M.; Rho, S.; Aborizka, M. A new computing environment for collective privacy protection from constrained healthcare devices to IoT cloud services. Clust. Comput. 2019, 22, 1611–1638. [Google Scholar] [CrossRef]
- Abdel-Basset, M.; Manogaran, G.; Gamal, A.; Chang, V. A Novel Intelligent Medical Decision Support Model Based on Soft Computing and IoT. IEEE Internet Things J. 2019, 7, 4160–4170. [Google Scholar] [CrossRef]
- Mahmoud, M.M.; Rodrigues, J.J.; Saleem, K.; Al-Muhtadi, J.; Kumar, N.; Korotaev, V. Towards energy-aware fog-enabled cloud of things for healthcare. Comput. Electr. Eng. 2018, 67, 58–69. [Google Scholar] [CrossRef]
- Saxena, D.; Raychoudhury, V. Design and Verification of an NDN-Based Safety-Critical Application: A Case Study With Smart Healthcare. IEEE Trans. Syst. Man, Cybern. Syst. 2019, 49, 991–1005. [Google Scholar] [CrossRef]
- Chakraborty, S.; Bhowmick, S.; Talaga, P.; Agrawal, D.P. Fog Networks in Healthcare Application. In Proceedings of the 2016 IEEE 13th International Conference on Mobile Ad Hoc and Sensor Systems (MASS), Brasilia, Brazil, 10–13 October 2016; pp. 386–387. [Google Scholar]
- Andriopoulou, F.; Dagiuklas, T.; Orphanoudakis, T. Integrating IoT and fog computing for healthcare service delivery. In Components and Services for IoT Platforms; Springer: Berlin/Heidelberg, Germany, 2017; pp. 213–232. [Google Scholar]
- Tuli, S.; Basumatary, N.; Gill, S.S.; Kahani, M.; Arya, R.C.; Wander, G.S.; Buyya, R. HealthFog: An ensemble deep learning based Smart Healthcare System for Automatic Diagnosis of Heart Diseases in integrated IoT and fog computing environments. Future Gener. Comput. Syst. 2020, 104, 187–200. [Google Scholar] [CrossRef]
- Jia, X.; He, D.; Kumar, N.; Choo, K.K.R. Authenticated key agreement scheme for fog-driven IoT healthcare system. Wirel. Networks 2019, 25, 4737–4750. [Google Scholar] [CrossRef]
- Jaiswal, K.; Sobhanayak, S.; Mohanta, B.K.; Jena, D. IoT-cloud based framework for patient’s data collection in smart healthcare system using raspberry-pi. In Proceedings of the 2017 International Conference on Electrical and Computing Technologies and Applications (ICECTA), Ras Al Khaimah, United Arab Emirates, 21–23 November 2017; pp. 1–4. [Google Scholar]
- Aazam, M.; Zeadally, S.; Flushing, E.F. Task offloading in edge computing for machine learning-based smart healthcare. Comput. Netw. 2021, 191, 108019. [Google Scholar] [CrossRef]
- Gia, T.N.; Jiang, M.; Rahmani, A.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fog Computing in Healthcare Internet of Things: A Case Study on ECG Feature Extraction. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 356–363. [Google Scholar]
- Vijayakumar, V.; Malathi, D.; Subramaniyaswamy, V.; Saravanan, P.; Logesh, R. Fog computing-based intelligent healthcare system for the detection and prevention of mosquito-borne diseases. Comput. Hum. Behav. 2019, 100, 275–285. [Google Scholar] [CrossRef]
- Kishor, A.; Chakraborty, C.; Jeberson, W. A novel fog computing approach for minimization of latency in healthcare using machine learning. Int. J. Interact Multimed Artif. Intell. 2021, 6, 10–20. [Google Scholar] [CrossRef]
- Hassan, S.R.; Ahmad, I.; Ahmad, S.; Alfaify, A.; Shafiq, M. Remote pain monitoring using fog computing for e-Healthcare: An efficient architecture. Sensors 2020, 20, 6574. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.K.; Sood, V.; Mahajan, I. An intelligent healthcare system for predicting and preventing dengue virus infection. Computing 2021, 1–39. [Google Scholar] [CrossRef]
- Shynu, P.; Menon, V.G.; Kumar, R.L.; Kadry, S.; Nam, Y. Blockchain-based secure healthcare application for diabetic-cardio disease prediction in fog computing. IEEE Access 2021, 9, 45706–45720. [Google Scholar] [CrossRef]
- Kumar, P.R.; Arunprasath, T.; Rajasekaran, M.P.; Vishnuvarthanan, G. Computer-aided automated discrimination of Alzheimer’s disease and its clinical progression in magnetic resonance images using hybrid clustering and game theory-based classification strategies. Comput. Electr. Eng. 2018, 72, 283–295. [Google Scholar] [CrossRef]
- Ahmad, H.F.; Mukhtar, H.; Alaqail, H.; Seliaman, M.; Alhumam, A. Investigating Health-Related Features and Their Impact on the Prediction of Diabetes Using Machine Learning. Appl. Sci. 2021, 11, 1173. [Google Scholar] [CrossRef]
- Syed, A.H.; Khan, T. Machine Learning-Based Application for Predicting Risk of Type 2 Diabetes Mellitus (T2DM) in Saudi Arabia: A Retrospective Cross-Sectional Study. IEEE Access 2020, 8, 199539–199561. [Google Scholar] [CrossRef]
- Roy, A.; Roy, C.; Misra, S.; Rahulamathavan, Y.; Rajarajan, M. Care: Criticality-aware data transmission in cps-based healthcare systems. In Proceedings of the 2018 IEEE International Conference on Communications Workshops (ICC Workshops), Kansas City, MO, USA, 20–24 May 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–6. [Google Scholar]
- Misra, S.; Roy, A.; Roy, C.; Mukherjee, A. DROPS: Dynamic radio protocol selection for energy-constrained wearable IoT healthcare. IEEE J. Sel. Areas Commun. 2020, 39, 338–345. [Google Scholar] [CrossRef]
- Aladwani, T. Scheduling IoT healthcare tasks in fog computing based on their importance. Procedia Comput. Sci. 2019, 163, 560–569. [Google Scholar] [CrossRef]
- Guo, C.; Tian, P.; Choo, K.K.R. Enabling privacy-assured fog-based data aggregation in E-healthcare systems. IEEE Trans. Ind. Informatics 2020, 17, 1948–1957. [Google Scholar] [CrossRef]
- Azeem, M.; Ullah, A.; Ashraf, H.; Jhanjhi, N.; Humayun, M.; Aljahdali, S.; Tabbakh, T.A. FoG-Oriented Secure and Lightweight Data Aggregation in IoMT. IEEE Access 2021, 9, 111072–111082. [Google Scholar] [CrossRef]
- Ramesh, J.; Aburukba, R.; Sagahyroon, A. A remote healthcare monitoring framework for diabetes prediction using machine learning. Healthc. Technol. Lett. 2021, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Chatrati, S.P.; Hossain, G.; Goyal, A.; Bhan, A.; Bhattacharya, S.; Gaurav, D.; Tiwari, S.M. Smart home health monitoring system for predicting type 2 diabetes and hypertension. J. King Saud-Univ.-Comput. Inf. Sci. 2020, 34, 862–870. [Google Scholar] [CrossRef]
- Hasan, M.K.; Alam, M.A.; Das, D.; Hossain, E.; Hasan, M. Diabetes prediction using ensembling of different machine learning classifiers. IEEE Access 2020, 8, 76516–76531. [Google Scholar] [CrossRef]
- Kaur, P.; Sharma, N.; Singh, A.; Gill, B. CI-DPF: A cloud IoT based framework for diabetes prediction. In Proceedings of the 2018 IEEE 9th Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON), Vancouver, BC, Canada, 1–3 November 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 654–660. [Google Scholar]
- Reddy, G.T.; Bhattacharya, S.; Ramakrishnan, S.S.; Chowdhary, C.L.; Hakak, S.; Kaluri, R.; Reddy, M.P.K. An ensemble based machine learning model for diabetic retinopathy classification. In Proceedings of the 2020 International Conference on Emerging Trends in Information Technology and Engineering (ic-ETITE), Vellore, India, 24–25 February 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–6. [Google Scholar]
- Barbara Kitchenham, O. Pearl Brereton, David Budgen, Mark Turner, John Bailey and Stephen Linkman. Systematic literature reviews in software engineering—A systematic literature review. Inf. Softw. Technol. 2009, 51, 7–15. [Google Scholar] [CrossRef]
- Vu-Ngoc, H.; Elawady, S.S.; Mehyar, G.M.; Abdelhamid, A.H.; Mattar, O.M.; Halhouli, O.; Vuong, N.L.; Ali, C.D.M.; Hassan, U.H.; Kien, N.D.; et al. Quality of flow diagram in systematic review and/or meta-analysis. PLoS ONE 2018, 13, e0195955. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Verma, G.; Prakash, S. Internet of Things for healthcare: Research challenges and future prospects. In Advances in Communication and Computational Technology; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1055–1067. [Google Scholar]
- Losada, M.; Cortés, A.; Irizar, A.; Cejudo, J.; Pérez, A. A flexible fog computing design for low-power consumption and low latency applications. Electronics 2020, 10, 57. [Google Scholar] [CrossRef]
- Boru, D.; Kliazovich, D.; Granelli, F.; Bouvry, P.; Zomaya, A.Y. Energy-efficient data replication in cloud computing datacenters. Clust. Comput. 2015, 18, 385–402. [Google Scholar] [CrossRef]
- Mostafa, B.; Benslimane, A.; Saleh, M.; Kassem, S.; Molnar, M. An energy-efficient multiobjective scheduling model for monitoring in internet of things. IEEE Internet Things J. 2018, 5, 1727–1738. [Google Scholar] [CrossRef]
- Atlam, H.F.; Walters, R.J.; Wills, G.B. Fog computing and the internet of things: A review. Big Data Cogn. Comput. 2018, 2, 10. [Google Scholar] [CrossRef] [Green Version]




| S# | Author(s) | Diseases | Tools and Technique | Sensors Used | Description |
|---|---|---|---|---|---|
| 1 | Gia et al. [69] | Cardiac disease | WBAN, Arduino with Wi-Fi shield, TI CC2538, Zigduino, Z1 | HC-05 Bluetooth module as wireless sensor network nodes | A health monitoring system by exploiting the concept of fog computing at smart gateways providing advanced techniques and services such as embedded data mining, distributed storage, and notification service at the edge of network. |
| 2 | Dubey et al. [47] | Speech disorder and Heart Disease | Pan-Tompkins algorithm, The DTW algorithm was implemented in C program and UCR Suit | Smartwatch, ECG sensor | have implemented a system that is wearable telehealth based on the Intel@ Edison embedded processor which work for the speech disorder |
| 3 | Rahmani et al. [17] | Cardiac Disease | LZW algorithm,6LoWPAN | Arduino Due, Bluetooth, Wi-Fi, ZigBee or 6LoWPAN. | A monitoring system for health that uses secondary networks based on IoT and includes many sensors such as Wi-Fi and Bluetooth |
| 4 | Manogaran et al. [16] | BP, Sugar, Heart rate and body temperature. | S3, cmd method, Apache Pig-Pig algorithm, Amazon S3 bucket, EMR, Apache Hbase | Wearable sensor devices | Used some sensors to monitor individual health conditions in a constant manner, such as ECG, EMG, pulse oximeter, mica2 motes, and SpO2 sensor. |
| 5 | Verma et al. [51] | Cardiac disease, diabetes, other problems | Bayesian belief network, THI, Weka tool | Smart wearable sensors, gastro sensors, heart sensors | They expertly monitor by using IoT devices, smart sensors, and other internet-connected devices to capture various patient records |
| 6 | Mahmud et al. [52] | Health issues | VM, MCI, iFogSim | Intelliegent health sensors | Their method, such as intelligent health sensors, service composition, cloud-edge service management, sensor-edge service management, distributed health care applications, and security and privacy solutions. |
| 7 | Negash et al. [50] | Cardiac disease | LZW algorithm, Python-tornado | 6LoWPAN, Bluetooth | They gather the data from sensor nodes with bio-signals such as ECG and EMG. The sensor node is made up of medical sensors, a microcontroller, and a wireless communication IC. |
| 8 | Akrivopoulos et al. [56] | Heart rate | Integrated 4Gbit (8x512Mb) NAND Furthermore, ADC converter, Spark-IoT | Smart devices, wearable devices | They enlarge the cloud computing model through moving processed data near to the production site; speed up the system’s awareness to actions next to its complete awareness; and by removing the data round-trip to the cloud. |
| 9 | Sood et al. [37] | Chikungunya | Fuzzy C-Means SNA graph, Matlab | Body sensor, water sensors, GPS sensors, climate detector sensor | Using fog architecture, the information is sent to the fog layer for continuous preparation and diagnosis of contaminated clients from CHV |
| 10 | Sood et al. [57] | Chikungunya | J48 decision tree, TNA, Weka 3.6, Gephi 0.9.1 tool | GPS Sensor, RFID, Bio Sensors and Body Sensors, climate sensor, mosquito sensor, water quality detector sensor, temperature sensor | Their calculation rethinks the class of client and produces an alarm; the subsequent calculation is to create and refresh the Time and Action (TNA) graph |
| 11 | Gia et al. [58] | Respiration and heart rate | AES-256, Orange Pi | BME280 sensors | The little wearable gadget will be ready to assemble and communicate a huge high-gain signal remotely |
| 12 | Basset et al. [60] | Type 2-diabetes | Decision tree, WBAN and mobile application, Neutrosophic with VIKOR method, TOPSIS method | Glucose detection sensor, the skin-like sensor | A model dependent on fog and IoT for recognizing and observing Type-2 diabetes persist progressively |
| 13 | Cerina et al. [12] | Respiratory problems | FPGA, Xilinx Pynq-Z ARM Cortex A9 CPU and a Zynq XC7Z020 FPGA. | Cozir CO2 sensor | A fog engineering made by various gadgets specifically intended for the organization of preventing social insurance applications, utilizing extensive quality control |
| 14 | Mahmoud et al. [61] | Chronic disease | DVFS, two-tier CoT, iFogSim | Wearable sensors devices | They represent a new trend in imaginative e-health arrangements, with improved dormancy, vitality utilization, portability, and quality of service. |
| 15 | Saxena et al. [62] | Chronic diseases, other vitals | Expectation-Maximization (EM) algorithm, NDNoT, HMM, S, Raspberry Pi, Arduinos | Health sensors, | Investigated the fundamental Named Data Networking (NDN) design to build up the NDN-IoT stage for the smart healthcare system. |
| 16 | Elmisery et al. [59] | Blood pressure, heart rate, electrocardiogram, blood glucose, and respiratory rate | Local concealment algorithms, Paillier encryption scheme, EVS, C++, octave libraries, Number Theory Library (NTL) | Implantable medical sensors | Proposed the topological development of IoHT gadgets when assembling the client’s information for cloud administration. |
| 17 | Azimi et al. [7] | Cardiac Disease | Machine learning algorithm, Raspberry pi, Biopsy toolbox in Python | Real sensor network | An innovative IoT-based approach for a smart healthcare system that gives a medical warning for the patient monitoring system. |
| 18 | Kaur et al. [48] | Pulse rate, heart rate and temperature | Node-Red, MQTT protocol, Raspberry pi, Arduino | Wearable sensors devices | Proposed a system for monitoring the different parameters of the patient such as pulse rate and temperature with the help of a sensor connected to the Raspberry Pi and IoT. |
| 19 | Tuli et al. [65] | Heart disease | Deep learning in Edge computing, Python, scikit library | Medical sensors, activity sensors and environment sensors | Proposed a new system called Health-Fog for gathering deep learning in edge processing gadgets and introducing it for the genuine use of programmed coronary illness examination. |
| 20 | Rajan et al. [19] | Oral cancer | Deep convolutional neural network, myRIO-1900 | Intelligent medical sensors | Proposed a novel method which utilizes a modified vesselness measurement and a Deep Convolutional Neural Network (DCNN) to identify the oral cancer region structure in IoT based smart healthcare system. |
| 21 | Kumar et al. [70] | Mosquito-borne diseases | Fuzzy KNN classifier, MATLAB | Wearable and IoT sensors, Mosquito sensors | Utilized similarity coefficient to differentiate the various mosquito-borne diseases based on patient’s symptoms, and the fuzzy k-nearest neighbor approach is employed to categorize the user into infected or uninfected class |
| 22 | Muhammad et al. [4] | Chronic and psychological diseases | Deep Learning, Edge computing | TUH EEG Abnormal Corpus v2.0.0, EEG | Proposed a new smart pathology detection system using these technologies. Sensors will capture EEG signals of a person and send the signals to a nearby edge computing server. |
| 23 | Kishor et al. [71] | Healthcare heart disease | Random forest machine learning algorithm, Python 3.7 | Wearable and IoT sensors | They improve the latency minimization in e-healthcare through fog computing. |
| 24 | Hassan et al. [72] | Pain Conditions | FCFS, iFogSim | Bio-sensors | Proposed for deploying a remote pain monitoring system by adopting the fog paradigm to reduce latency and network consumption. |
| 25 | Sood et al. [73] | Dengue Virus | Naive bayesian network, Java-based simulator Cup Carbon U-one 3.8.2, Weka 3.6 | IoT, Environmental sensor and mosquito sensor | Proposed an intelligent healthcare system which identifies, monitors, and alerts Dengue Virus (DeV) infected individuals in real-time and control the DeV infection outbreak using Fog computing |
| 26 | Shynu et al. [74] | Diabetic-Cardio disease | Blockchain, Java (version 1.8) | Medical sensors | Proposed an efficient Blockchain-based secure healthcare services for disease prediction such as Diabetes and cardio diseases |
| 27 | Kumar et al. [75] | Alzheimer’s disease | K -means clustering and graph-cut methods, MATLAB | MRI | An effective segmentation and classification techniques are proposed for Alzheimer’s disease, mild cognitive impairment and normal control subjects |
| 28 | Ahmad et al. [76] | Diabetes | Machine learning algorithm, scikit-learn library | Glucose detection sensor | Investigated the prediction of diabetic patients and compare the role of HbA1c and FPG as input features. |
| 29 | Syed et al. [77] | Type 2-diabetes | Machine learning algorithm, SPSS | Glucose detection sensor | Implemented a questionnaire-based cross-sectional study using conventional diabetes risk factors for studying the prevalence and the association between the outcomes and exposure |
| 30 | Roy et al. [78] | Health criticality of any patient | Cooperative game-theoretic Nash bargaining approach, MATLAB | Body sensors | Proposed a scheme, Criticality Aware data transmission (CARE), in CPS-based healthcare systems, for increasing the processing rate of the sensed physiological parameters’ values of a patient |
| 31 | Misra et al. [79] | Critical patients | Dynamic radio protocol selection and linear regression, MATLAB R2015a | Body sensors | Proposed “DROPS”, a scheme which Dynamically selects Radio Protocols in an energy-constrained wearable IoT healthcare system |
| 32 | Aladwani [80] | Patient Monitoring | Max-Min scheduling algorithm, Cloud simulator | Body sensors | Improved the static task scheduling algorithm by using task classification and VM categorization |
| 33 | Guo et al. [81] | COVID-19 | Public key homomorphic encryption technologies such as ElGamal, Microsoft Azure | Medical sensors | Presented two attack games to demonstrate that our approach is secure (i.e., chosen-plaintext attack resilience under the computational Diffie–Hellman assumption), and evaluate the complexity of its computations |
| 34 | Azeem et al. [82] | Patient Monitoring | Secure Message Aggregation and Decryption algorithm, NS 2.35 | Medical sensors | An Efficient and Secure Data Transmission and Aggregation (ESDTA) scheme to enhance aggregation efficiency and data security |
| Author(s) | Techniques | A | B | C | D | E | F | G | H | I |
|---|---|---|---|---|---|---|---|---|---|---|
| Sood et al. (2021) [73] | Naive Bayesian Network (NBN) | √ | √ | √ | × | √ | √ | × | × | √ |
| Ahmad et al. (2021) [76] | Random Forest, Recursive Feature Elimination | √ | × | × | × | √ | × | × | × | × |
| Jayroop et al. (2021) [83] | SVM, Logistic Regression, Neural Network and Deep-NN | √ | √ | √ | × | × | × | × | × | × |
| Shynu et al. (2021) [74] | Block chain | √ | √ | × | × | × | × | × | × | × |
| Ahmad et al. (2021) [76] | Machine Learning Classifiers | √ | √ | × | √ | √ | × | × | × | × |
| Chatrati et at. (2020) [84] | SVM, Logistic Regression, KNN, Decision Tree | √ | √ | √ | √ | × | × | × | × | × |
| Kishor et al. (2020) [71] | Random forest machine learning algorithm | √ | √ | √ | × | × | × | × | × | × |
| Rajan et al. (2020) [19] | Deep convolution neural network | √ | √ | √ | × | × | × | × | × | × |
| Hasan et al. (2020) [85] | Random Forest, KNN, Decision tree, Naïve Bias | √ | √ | √ | √ | √ | √ | √ | × | × |
| Kaur et al. (2018) [86] | Cloud IoT based framework | √ | √ | √ | × | √ | √ | × | × | × |
| Verma et al. (2018) [51] | Bayesian belief network | × | × | √ | × | √ | √ | × | × | √ |
| Kumar et al. (2019) [70] | Fuzzy K-means | √ | √ | √ | × | √ | × | × | × | × |
| Reddy et al. (2020) [87] | Randon Forest, AdaBoost, Logistic Regression, KNN, Grid Search | √ | √ | √ | × | × | × | × | × | × |
| Manogaran et al. (2017) [16] | S3, cmd method, Apache pig-Pig algorithm | √ | √ | √ | × | × | √ | × | × | √ |
| Sood et al. (2017) [37] | Fuzzy C-Means, SNA graph | √ | √ | √ | × | √ | √ | × | × | √ |
| Sood et al. (2017) [57] | J48 decision tree, TNA | × | √ | √ | × | √ | √ | × | × | √ |
| Cerina et al. (2017) [12] | FPGA | √ | √ | √ | × | √ | √ | × | × | × |
| Criteria No. | Criteria Description | Proportion of the Titles |
|---|---|---|
| 1. | Identify the total number of titles | 90.20% |
| 2. | Define various sources including databases/search-engine | 55.30% |
| 3. | Identification of each databases | 35.50% |
| 4. | Identification of other sources such as search-engine, web-reports | 20.10% |
| 5. | Offline manual search | 03.55% |
| 6. | Number of duplicate titles removed | 30.50% |
| 7. | Tools and techniques used in filtering the duplicate titles | 03.30% |
| 8. | Assessed the publication year, language and status | 94.50% |
| 9. | Accessed the abstract and conclusions of the titles | 91.30 % |
| 10. | Number of titles eliminated | 85.60% |
| 11. | Accessed te full-text title for inclusion | 74.90% |
| 12. | Number of titles removed after full-text accessed | 52.80% |
| 13. | Conduct synthesis process | 59.80% |
| 14. | Conduct qualitative synthesis based on common challenges | 37.40% |
| 15. | Conduct quantitative synthesis based on common challenges | – |
| 16. | References investigation | 68.10% |
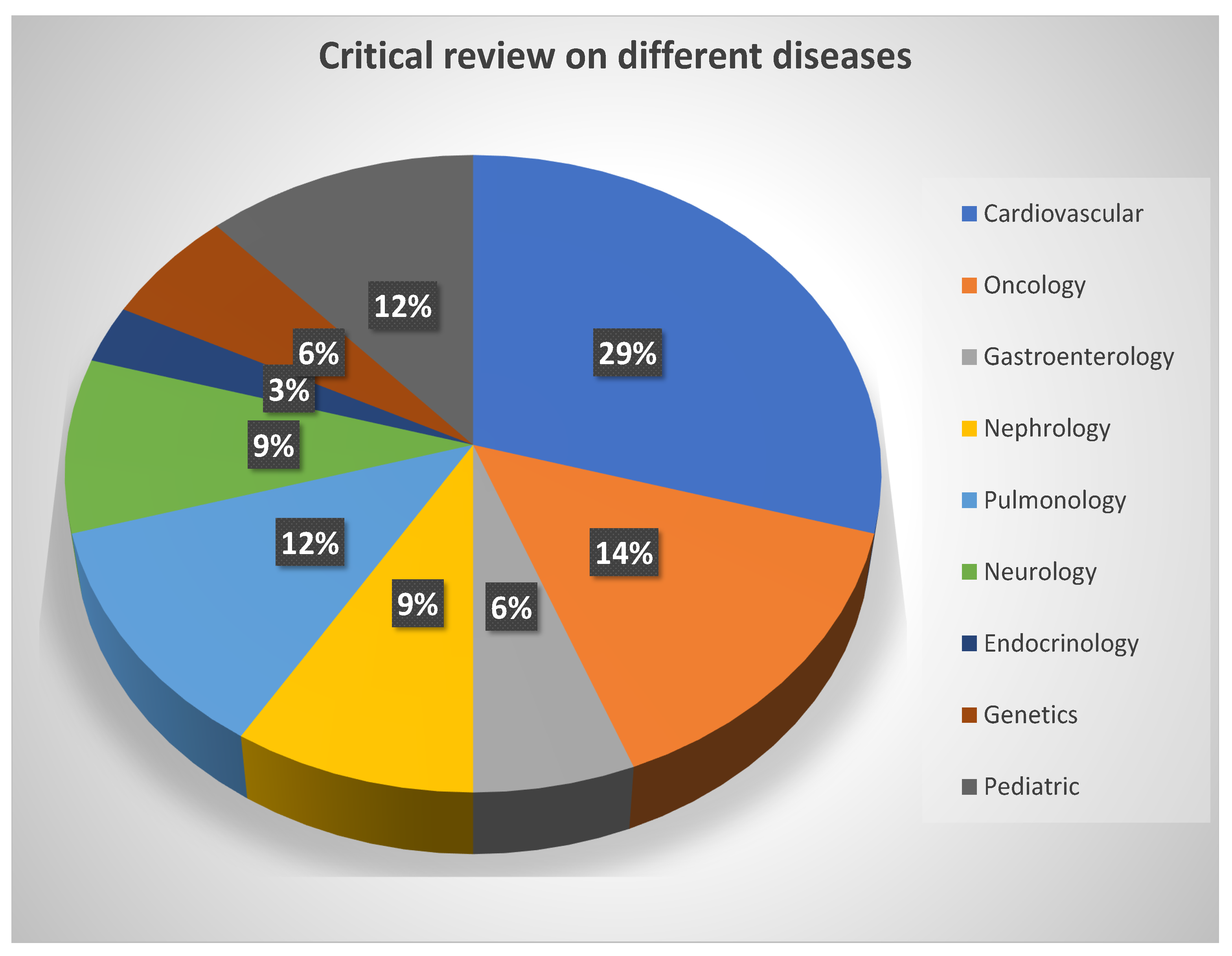
| S.No | Diseases | Review% | References |
|---|---|---|---|
| 1 | Cardiovascular | 29% | [1,3,5,7,10,12,50,58,59,65,71,74] |
| 2 | Oncology | 14% | [9,10,19,51,78,79] |
| 3 | Gastroenterology | 6% | [16,59] |
| 4 | Nephrology | 9% | [9,10,12] |
| 5 | Pulmonology | 12% | [60,74,76,77] |
| 6 | Neurology | 9% | [51,52] |
| 7 | Endocrinology | 3% | [16,72] |
| 8 | Genetics | 6% | [37,57,61,62] |
| 9 | Pediatric | 12% | [4,61,62] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kashyap, V.; Kumar, A.; Kumar, A.; Hu, Y.-C. A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues. Electronics 2022, 11, 2668. https://doi.org/10.3390/electronics11172668
Kashyap V, Kumar A, Kumar A, Hu Y-C. A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues. Electronics. 2022; 11(17):2668. https://doi.org/10.3390/electronics11172668
Chicago/Turabian StyleKashyap, Vijaita, Ashok Kumar, Ajay Kumar, and Yu-Chen Hu. 2022. "A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues" Electronics 11, no. 17: 2668. https://doi.org/10.3390/electronics11172668
APA StyleKashyap, V., Kumar, A., Kumar, A., & Hu, Y.-C. (2022). A Systematic Survey on Fog and IoT Driven Healthcare: Open Challenges and Research Issues. Electronics, 11(17), 2668. https://doi.org/10.3390/electronics11172668







