Human Digital Healthcare Engineering for Enhancing the Health and Well-Being of Seafarers and Offshore Workers: A Comprehensive Review
Abstract
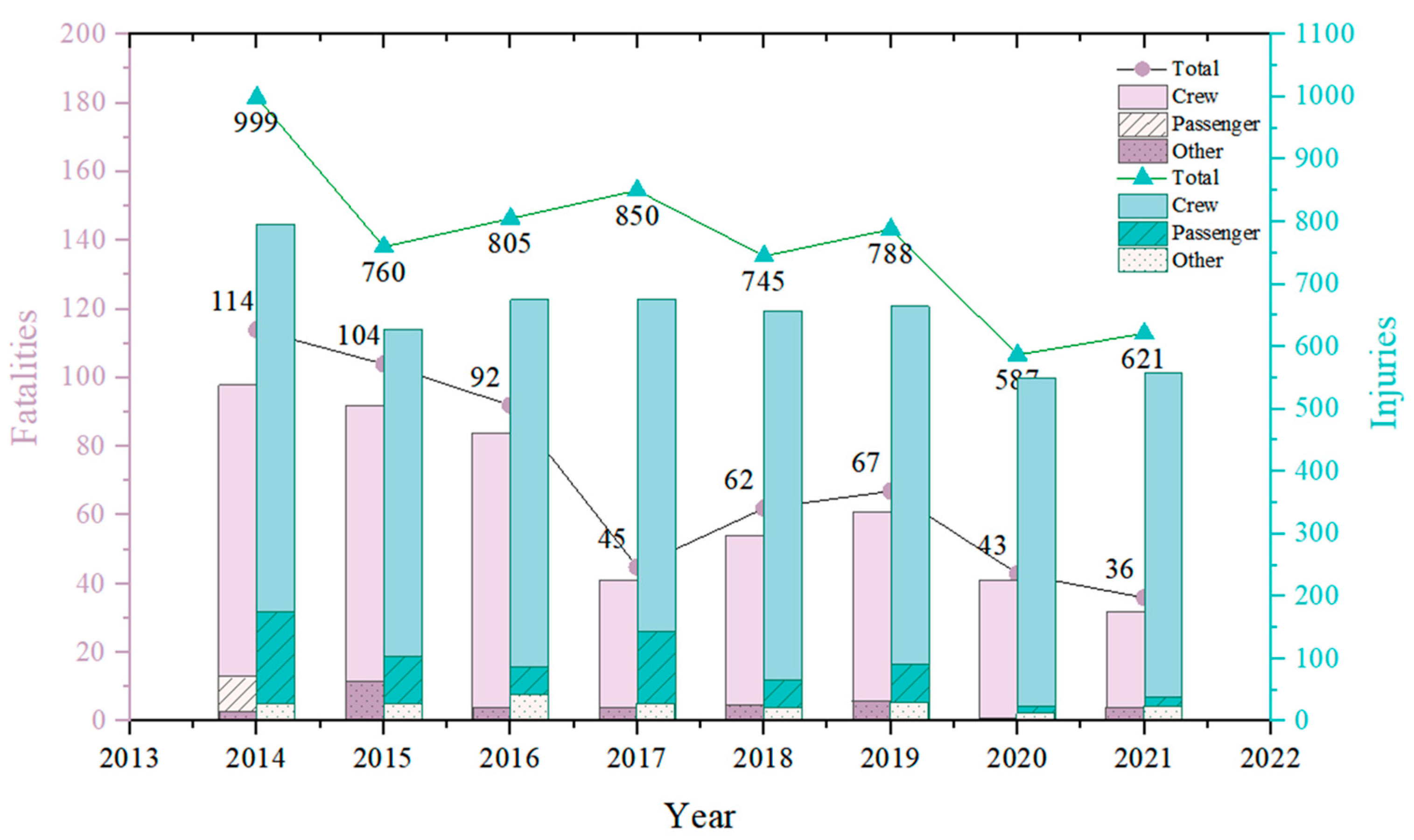
1. Introduction
- Why should DHE systems be introduced to ensure the safety of seafarers?
- What technical support is needed to build a DHE system, and what are the latest advancements in these technologies?
- What are the existing challenges in deploying DHE systems, and what is their potential?
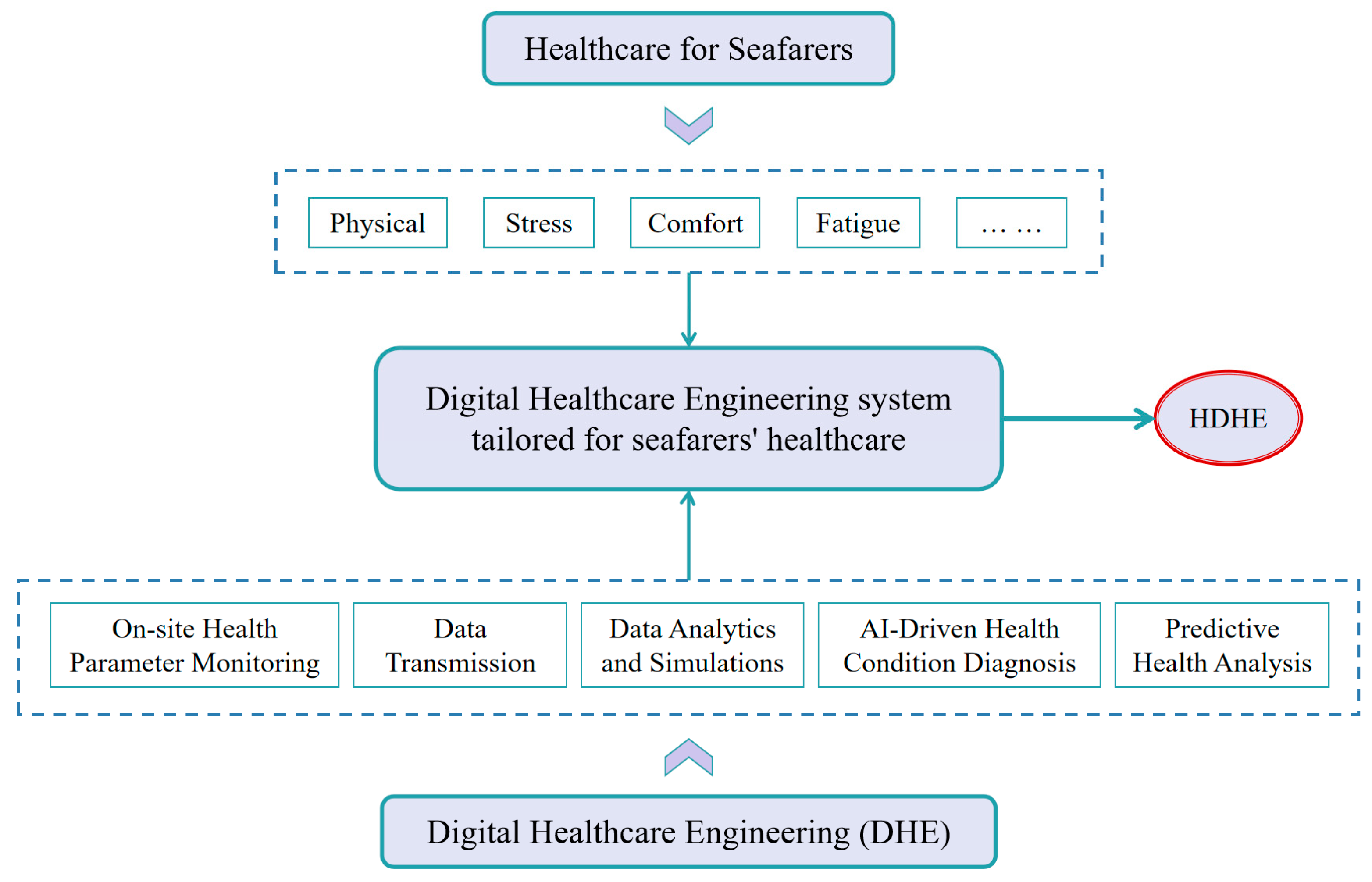
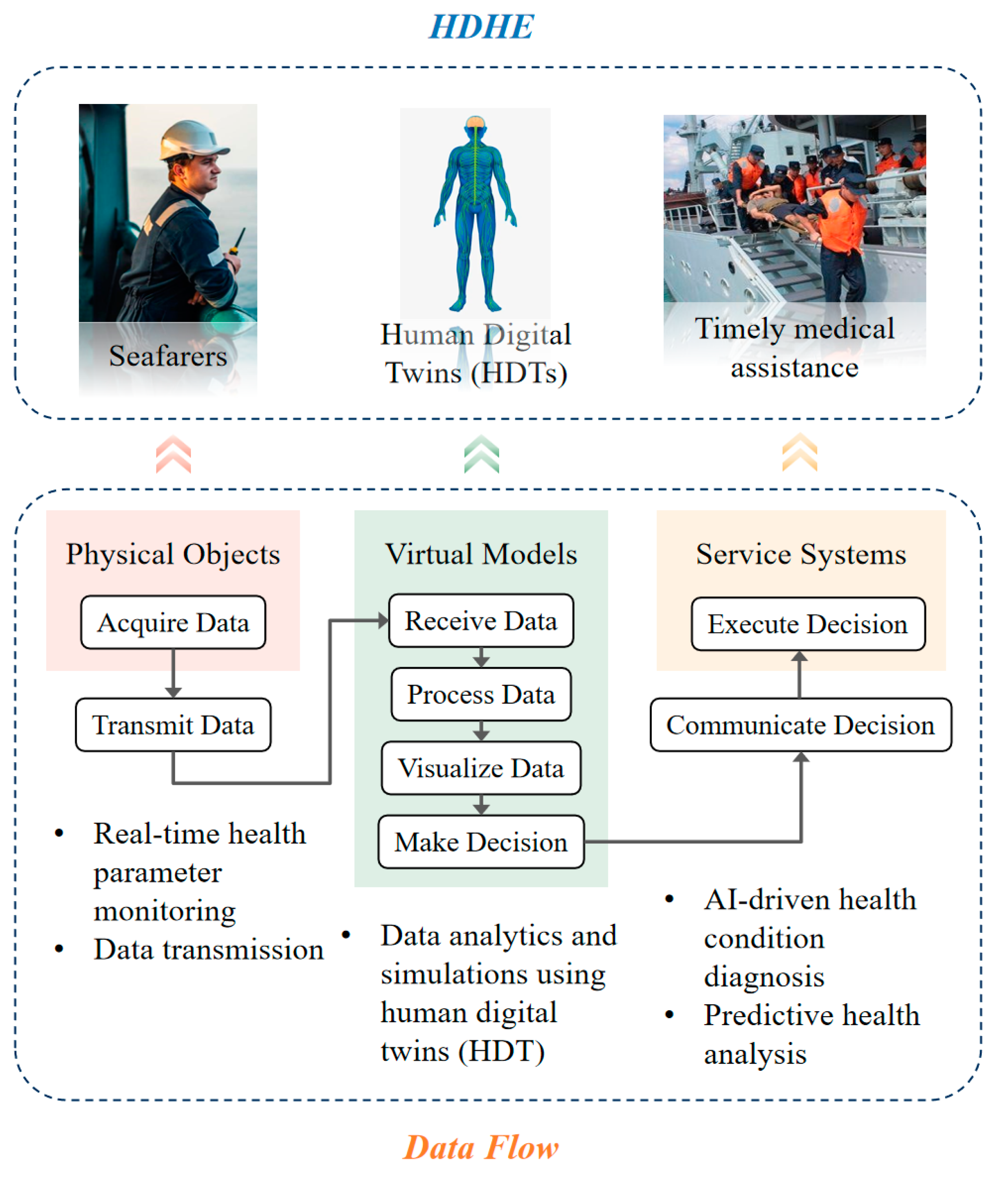
2. Human Digital Healthcare Engineering (HDHE) Framework
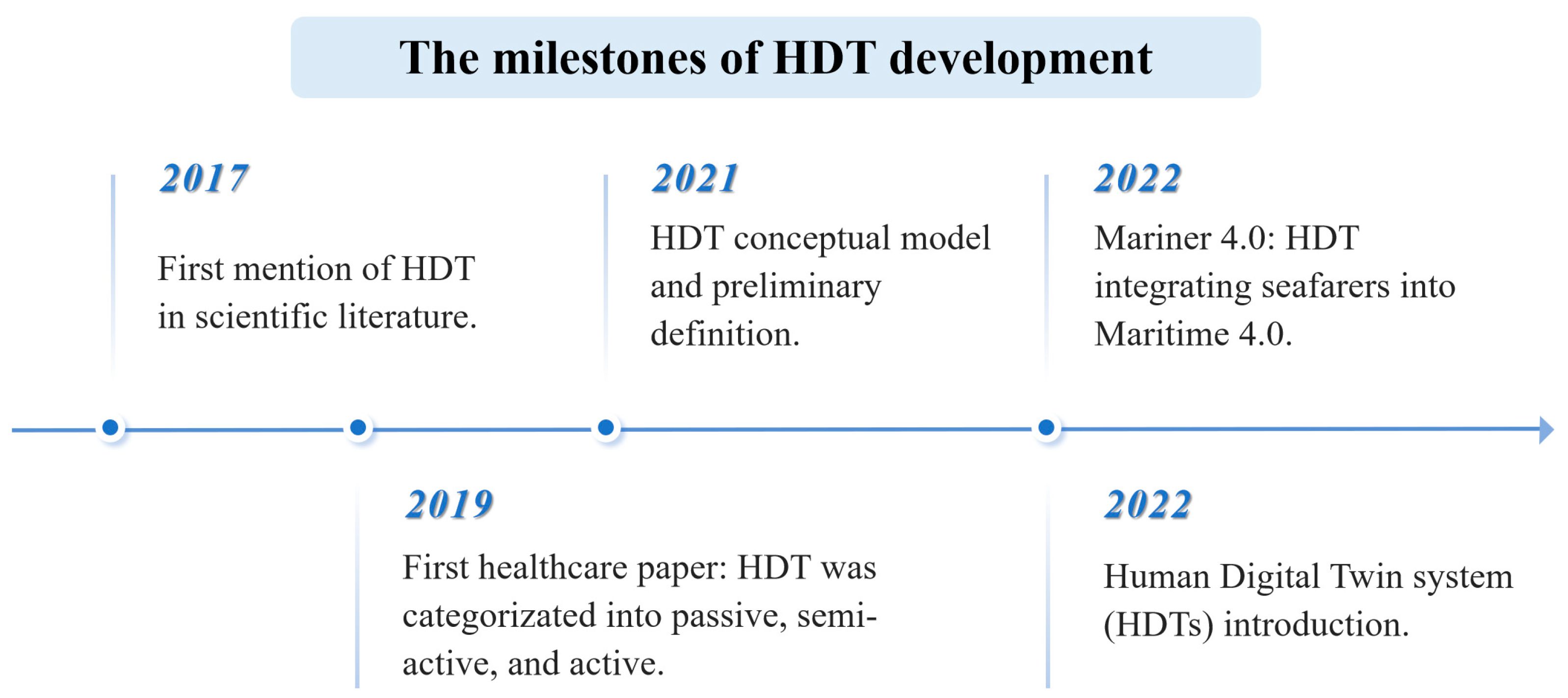
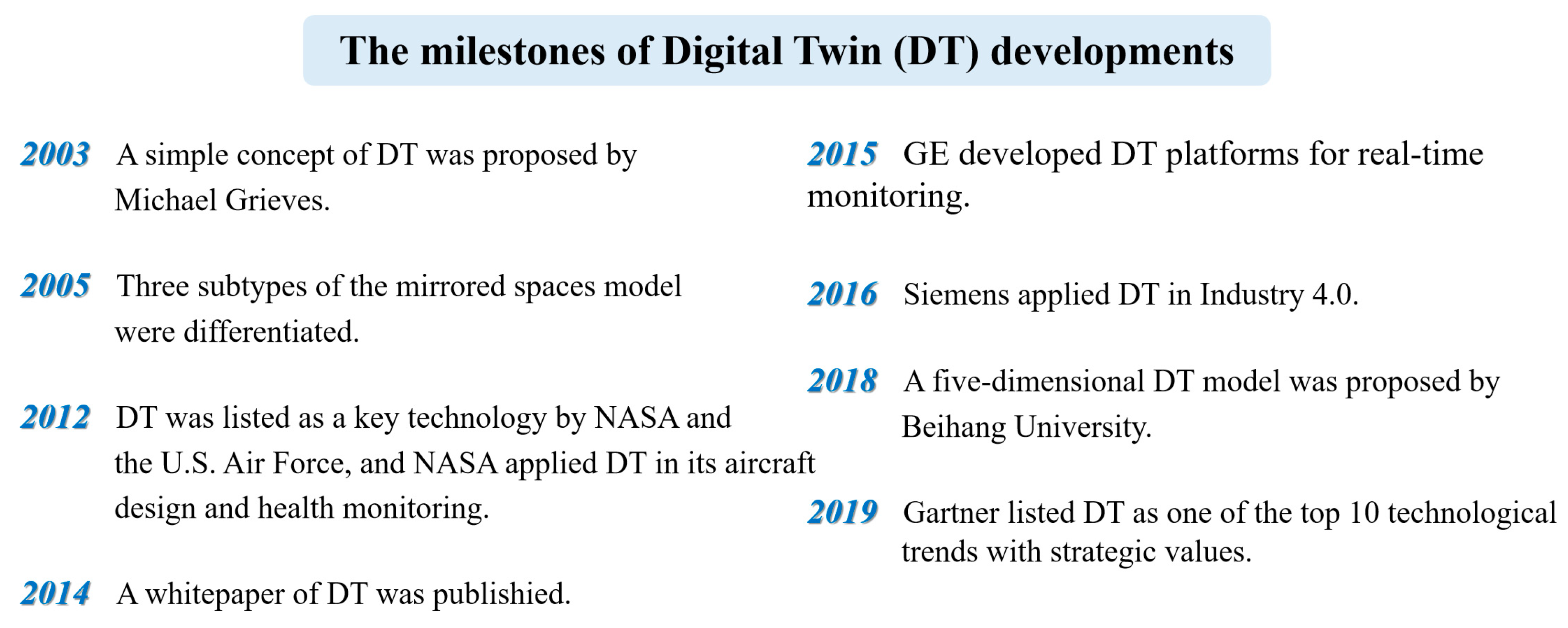
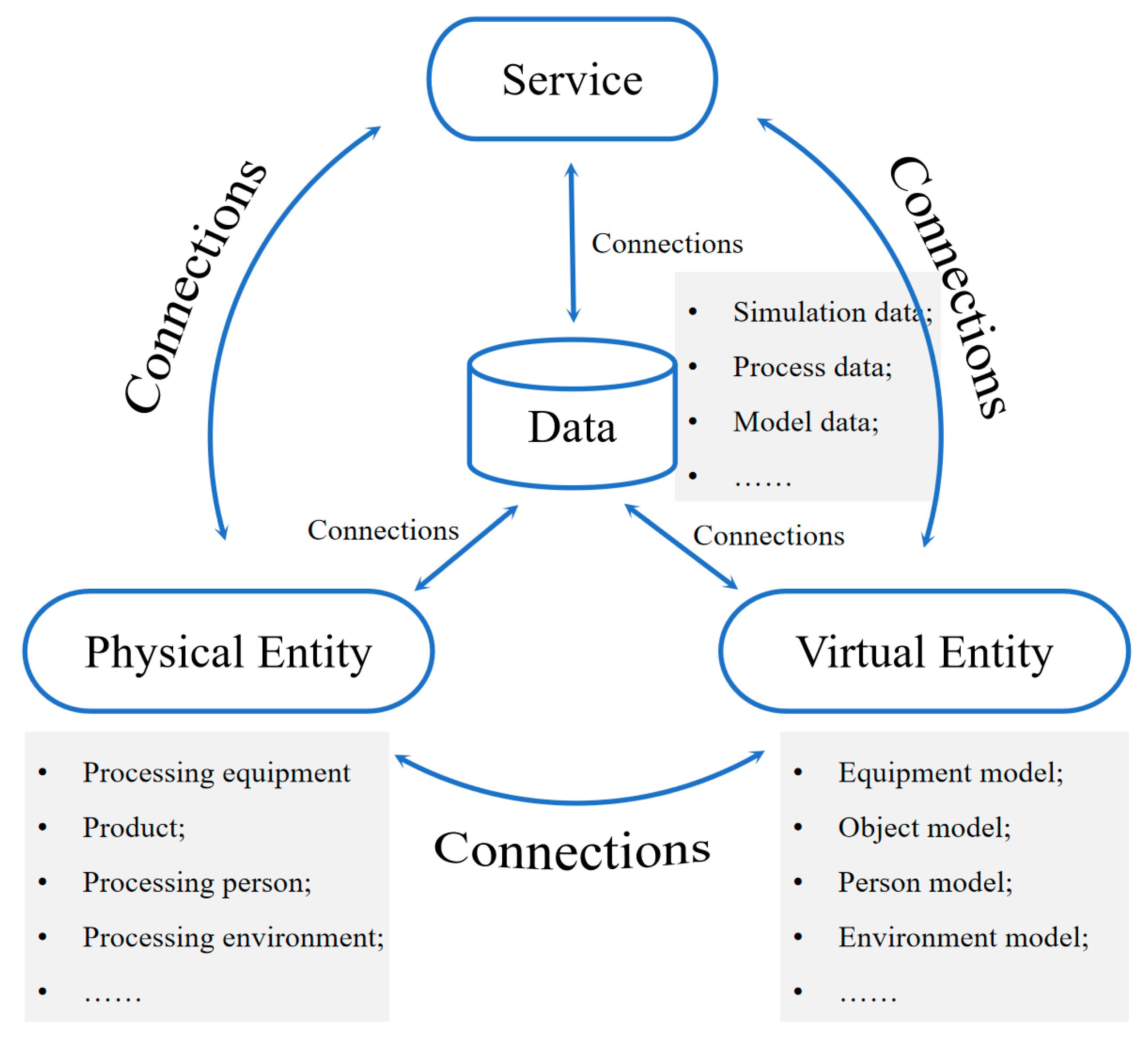
2.1. Research Progress in DTs and HDTs
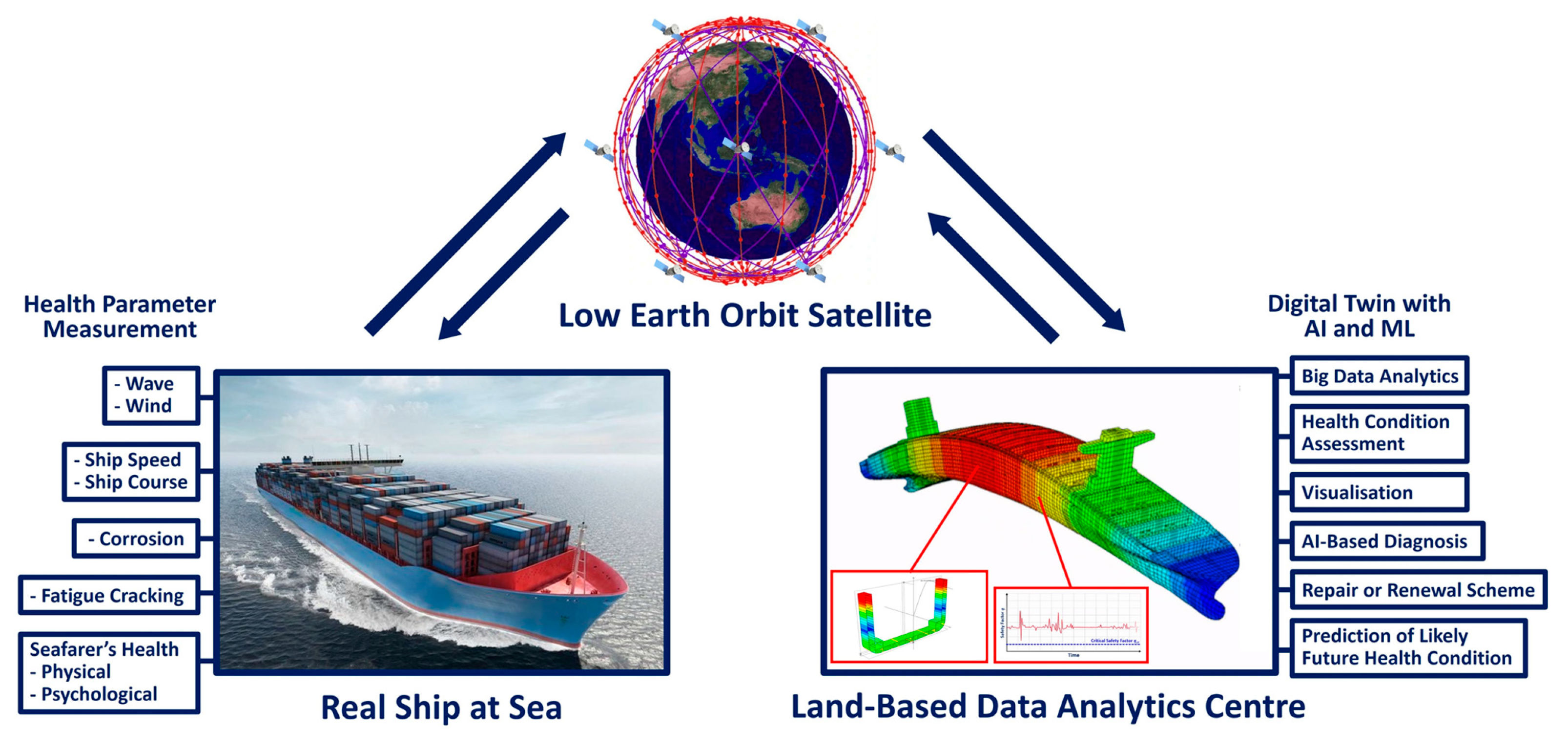
2.2. Research Progress in DHE
- Real-time on-site monitoring and digitalization of health parameters.
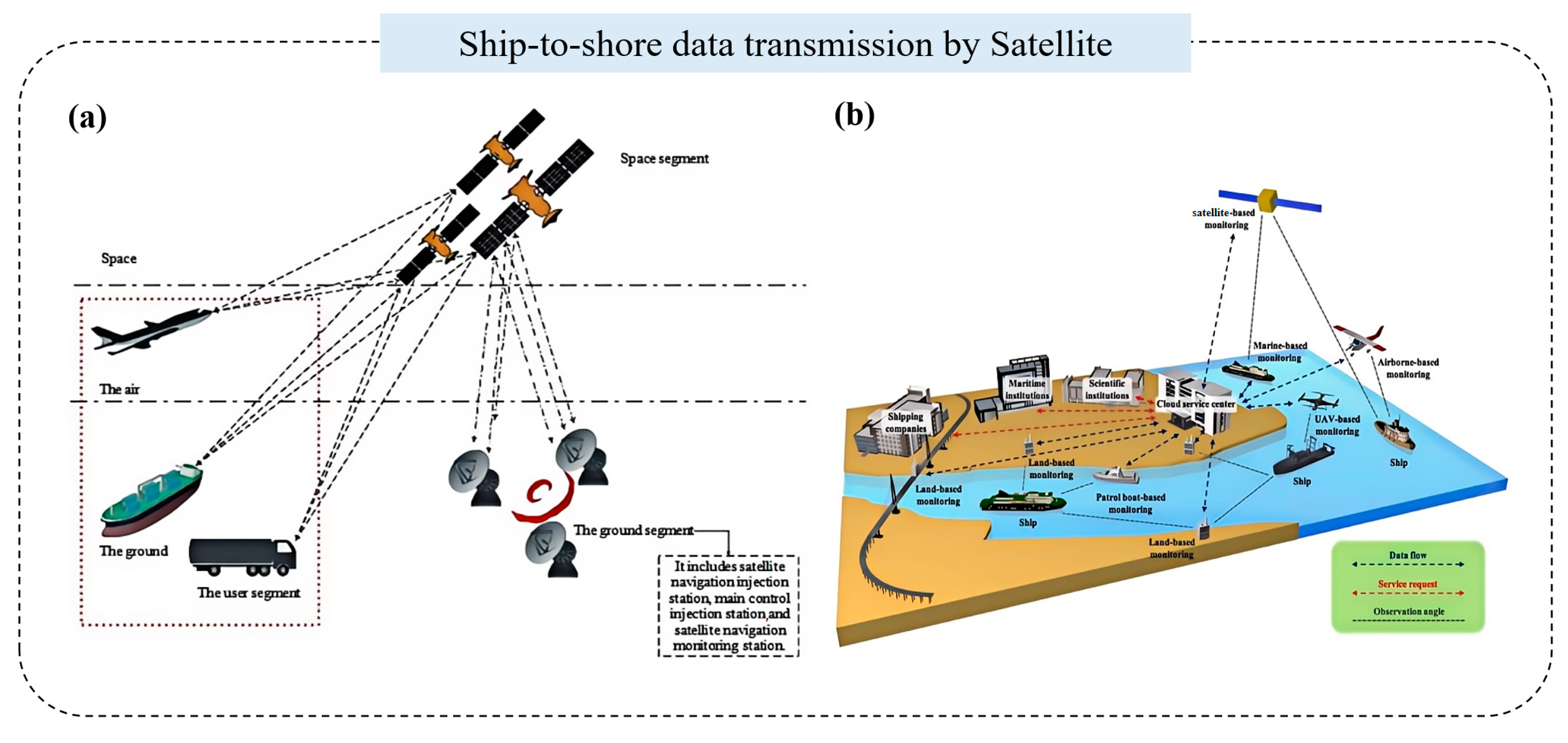
- Data transmission to land-based analytics centers via low Earth orbit (LEO) satellites.
- Advanced data analytics and simulations using digital twins.
- AI-driven diagnostics and automated treatment recommendations.
- Predictive health analysis for proactive care planning.
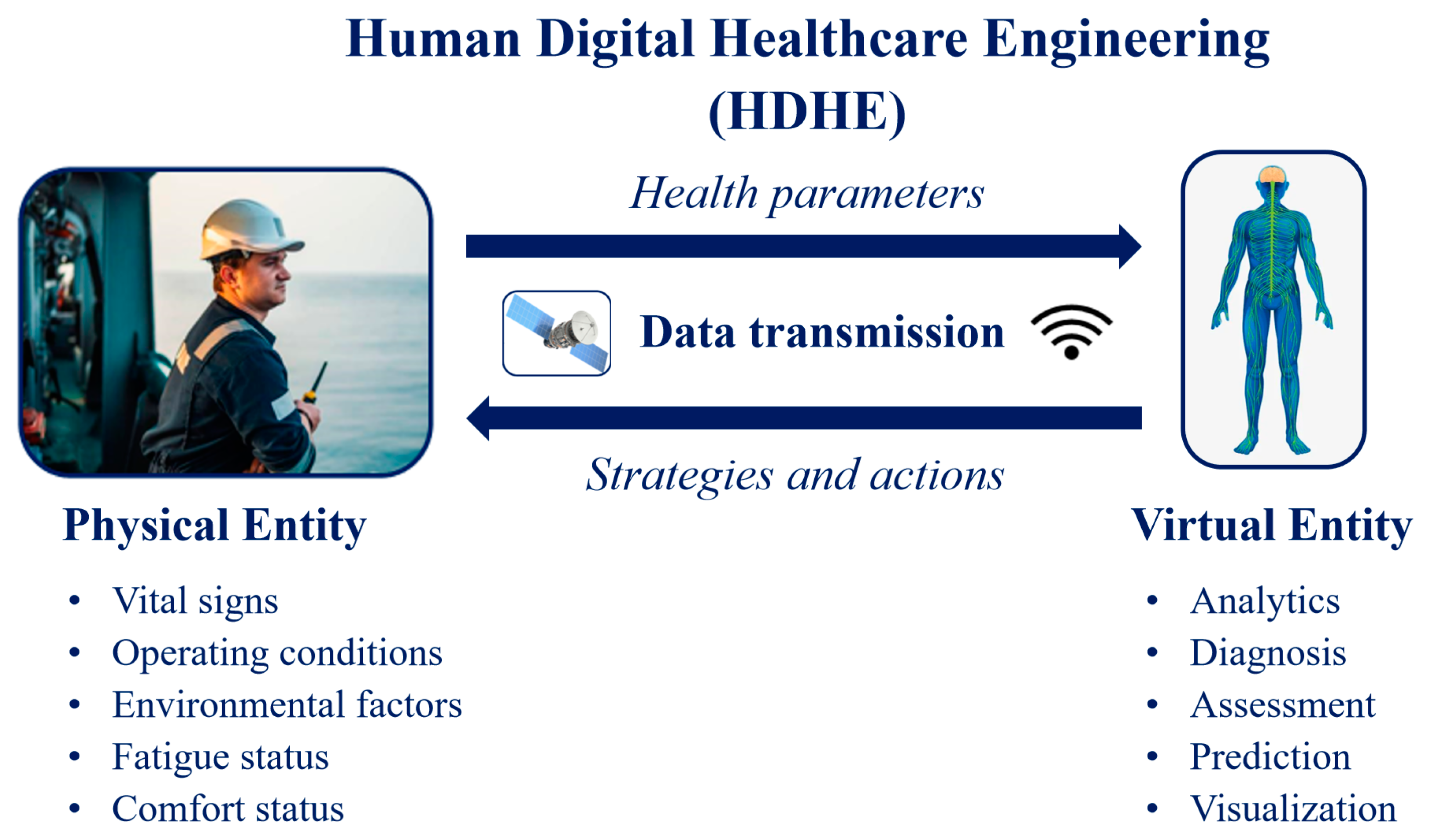
2.3. Concept of HDHE
3. Key Technologies for HDHE Systems
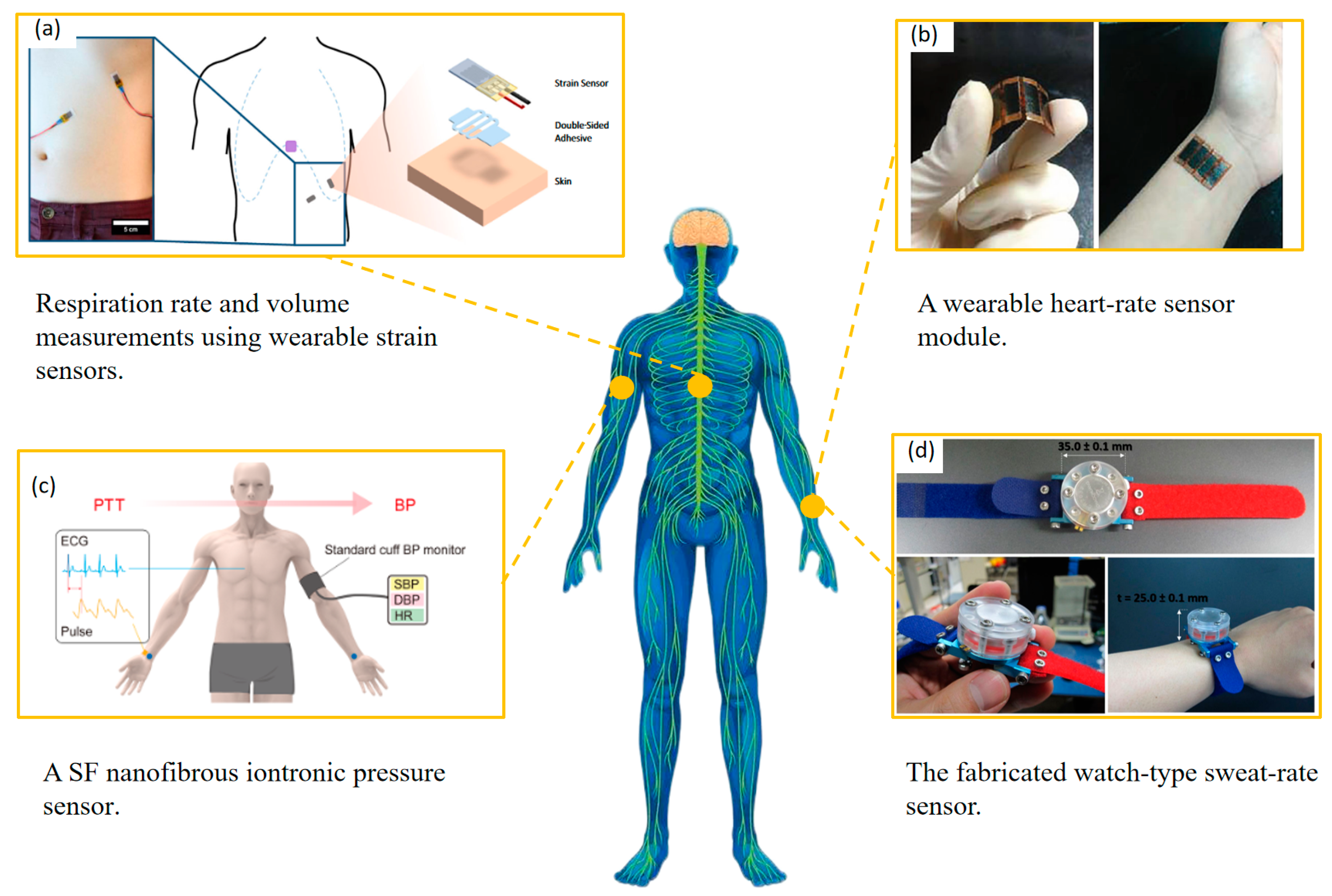
3.1. Real-Time Health Parameter Monitoring
- Miniaturization: reducing device size to micron or nanometer scales without compromising performance.
- Low energy consumption: minimizing energy use, ideally powered by solar energy or body heat.
- Interconnectivity: enabling integration with other smart technologies.
- Eco-friendliness: using sustainable materials to ensure environmental conservation.
3.2. Data Transmission
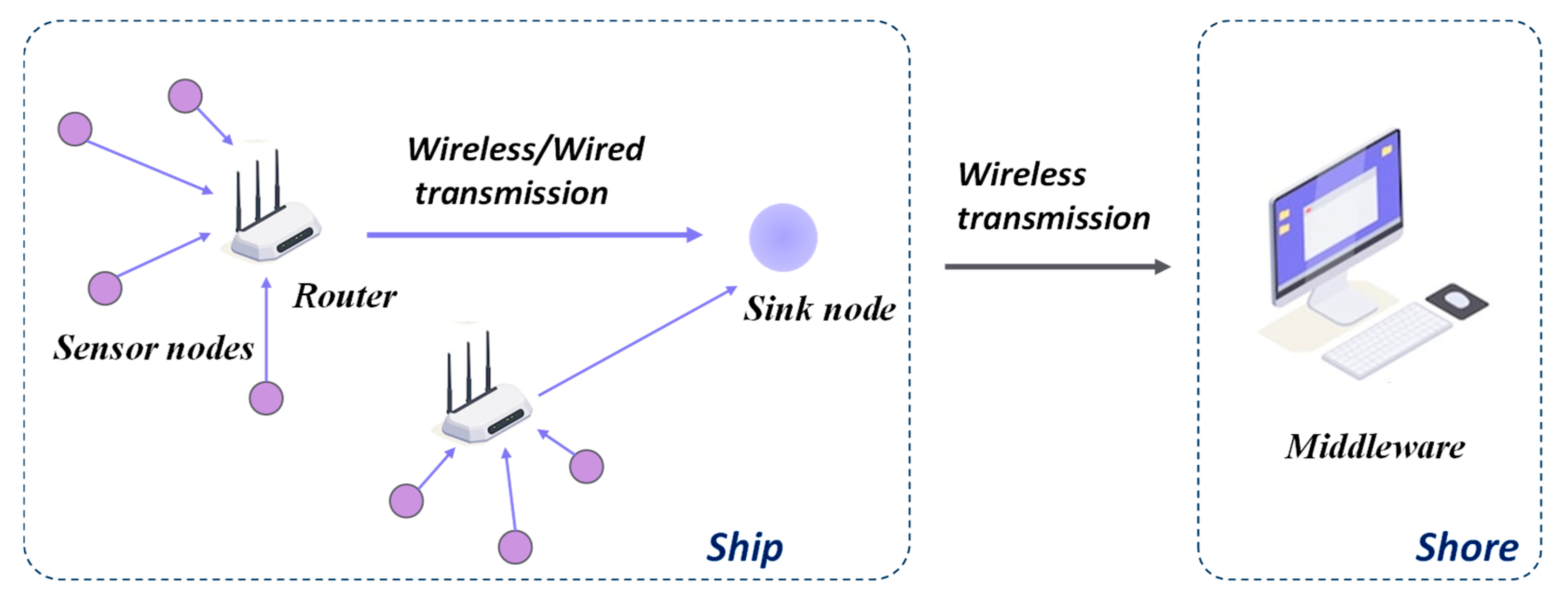
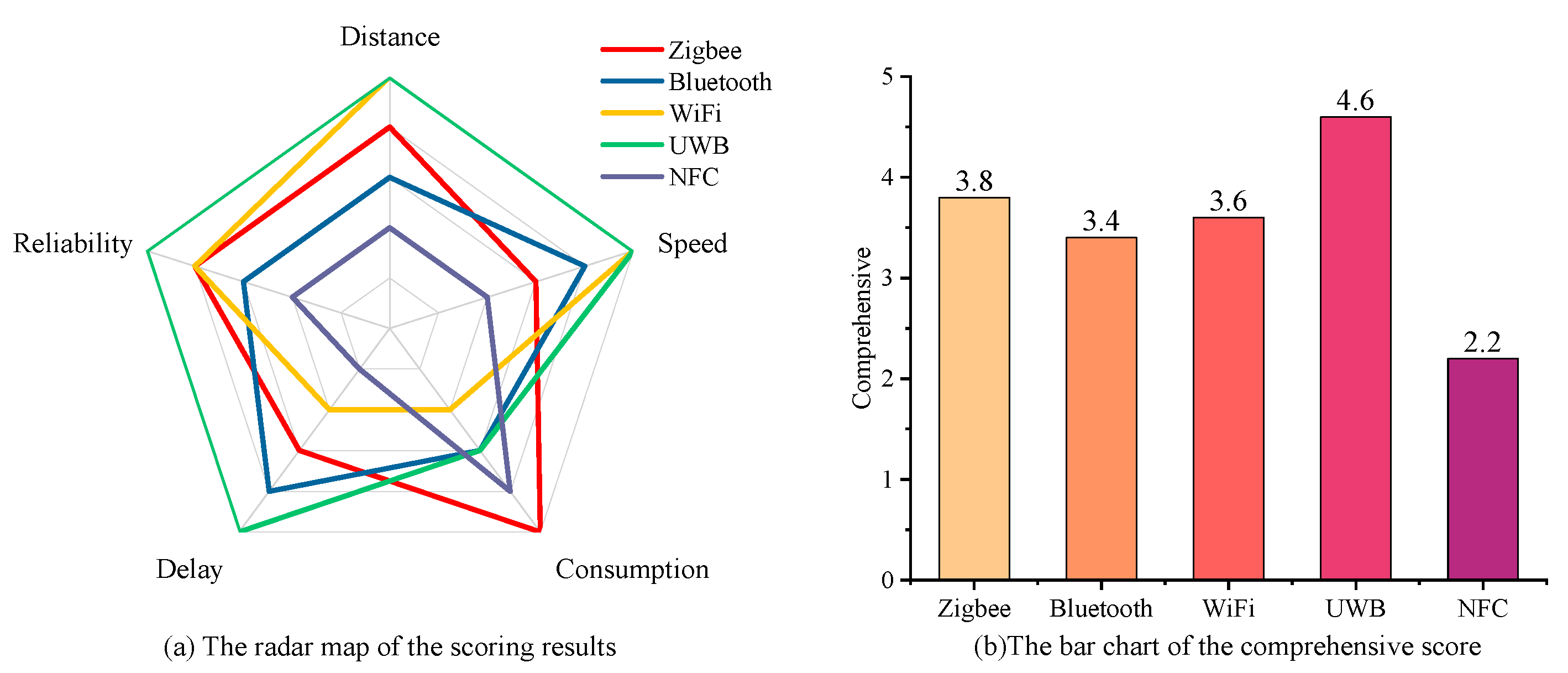
3.2.1. Onboard Data Transmission
- Zigbee and Bluetooth are ideal for short-distance, low-power communication, suitable for sensor integration.
- Wi-Fi excels in medium-distance, high-speed data transmission, making it ideal for transferring large datasets.
- UWB is particularly suited for long-distance communication requiring high-speed data transfer, making it a promising choice for HDHE systems.
3.2.2. Ship-to-Shore Data Transmission
3.3. Data Analytics and Simulations Using Human Digital Twins (HDTs)
3.4. AI-Driven Health Condition Diagnosis and Predictive Health Analysis
3.4.1. Machine Learning (ML)
- Ferreira et al. established a KNN prototyping scheme for embedded human activity recognition with online learning [62].
- Subramanian et al. developed a real-time emotion-recognition system using GB for healthcare applications [63].
- Moztarzadeh et al. employed ML methods including LR, DTr, RF, and GB to evaluate treatment progress and disease severity using DTs [64].
3.4.2. Deep Learning (DL)
- Ahmed et al. integrated DL with DTs to detect COVID-19 in X-ray images, achieving 94% accuracy [65].
- Wang et al. proposed a CNN-based framework for cognitive fatigue classification with 88.85% accuracy [66].
- Su et al. proposed an automated human activity recognition network HDL with smartphone motion sensor units, which combines DBLSTM (deep bidirectional long short-term memory) and a CNN. Its accuracy and F1 score are as high as 97.95% and 97.27% [67].
4. Discussion
4.1. Challenges and Practical Solutions
4.1.1. Resource Constraints
4.1.2. Privacy Concerns
4.1.3. Additional Stress
4.2. Implications and Economic Benefits
- Cost reduction for ship owners: HDHE can provide early prevention of health problems, reduce the frequency of accidents caused by human factors, and reduce the downtime of ships. At the same time, it can reduce the need for medical personnel on board and reduce medical costs.
- Improving diagnostic accuracy for healthcare providers: HDHE systems enable the accumulation and analysis of large amounts of seafarers’ health data and medical history so that physicians can recommend the appropriate treatment for each individual [97]. This reduces the possibility of misdiagnosis or inappropriate treatment and improves diagnostic accuracy and efficacy.
- Increase revenue for technology providers and training institutions: HDHE systems create new revenue generation opportunities for technology vendors and training institutions. As more companies invest in this system, they will benefit from the need for monitoring equipment, data analysis tools, and specialized project training.
5. Conclusions
- Unique Health Challenges: Seafarers and offshore workers face distinctive health risks due to long periods away from medical facilities and exposure to extreme weather, physical labor, and isolation.
- Role of Digital Twins: HDT is central to HDHE systems, enabling continuous real-time monitoring of seafarers’ health, predictive diagnostics, and personalized medical care. They integrate physical and digital data to allow ongoing health assessments and interventions.
- Enabling Technologies: Successful implementation of HDHE systems hinges on advanced technologies, including sensing technology, wearable devices, satellite communication, wireless networks, and AI-driven data analysis.
- Operational Workflow: HDHE systems involve several stages, including data collection via sensors and wearables, data transmission to onshore facilities, processing through AI algorithms, and providing real-time feedback for medical interventions.
- Challenges and Barriers: Implementation of HDHE systems faces technical complexities, organizational challenges, ethical issues related to privacy and security, and practical limitations like cost and resource constraints.
- Potential Impact: HDHE systems have the potential to transform healthcare for seafarers by enabling remote monitoring, accurate diagnostics, timely medical interventions, and personalized healthcare services, thereby improving their overall well-being, productivity, and safety onboard.
- Rapid Development: Though HDHE technology is still in its early stages and currently expensive, rapid advancements are underway. Ongoing research and development are expected to make these systems more accessible, affordable, and efficient in the near future.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DHE | Digital Healthcare Engineering |
| HDHE | Human Digital Healthcare Engineering |
| EMSA | European Maritime Safety Agency |
| DT | Digital Twin |
| HDT | Human Digital Twin |
| LEO | Low Earth Orbit |
| UWB | Ultra-Wideband |
| NFC | Near-Field Communication |
| BDS | BeiDou Satellite |
| SEMSW | Ship Emission Monitoring Sensor Web |
| FEM | Finite Element Method |
| CAD | Computer-Aided Design |
| VR | Virtual Reality |
| AR | Augmented Reality |
| AI | Artificial Intelligence |
| ML | Machine Learning |
| DL | Deep Learning |
| LR | Linear Regression |
| KNN | K-nearest Neighborhood |
| SVM | Support Vector Machine |
| DTr | Decision Tree |
| RF | Random Forest |
| GB | Gradient Boosting |
| NB | Naive Bayes |
| CNN | Convolutional Neural Network |
| RNN | Recurrent Neural Network |
| GAN | Generative Adversarial Network |
| DNN | Deep Neural Network |
| LSTM | Long Short-Term Memory |
References
- Bye, R.J.; Holmen, I.M.; Størkersen, K.V. Safety in Marine and Maritime Operations: Uniting Systems and Practice. Saf. Sci. 2021, 139, 105249. [Google Scholar] [CrossRef]
- Nurduhan, M.; Kuleyin, B. Cluster-Based Visualization of Human Element Interactions in Marine Accidents. Ocean Eng. 2024, 298, 117153. [Google Scholar] [CrossRef]
- Chen, J.; Bian, W.; Wan, Z.; Wang, S.; Zheng, H.; Cheng, C. Factor Assessment of Marine Casualties Caused by Total Loss. Int. J. Disaster Risk Reduct. 2020, 47, 101560. [Google Scholar] [CrossRef]
- Sánchez-Beaskoetxea, J.; Basterretxea-Iribar, I.; Sotés, I.; Machado, M. de las M.M. Human Error in Marine Accidents: Is the Crew Normally to Blame? Marit. Transp. Res. 2021, 2, 100016. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, W.J.; Lyu, H.G.; Zhou, X.Y.; Wang, Q.W.; Ramezani, R. Hybrid Early-Warning Framework for Unsafe Crew Acts Detection and Prediction. Ocean. Coast. Manag. 2023, 231, 106383. [Google Scholar] [CrossRef]
- Sullivan, B.P.; Desai, S.; Sole, J.; Rossi, M.; Ramundo, L.; Terzi, S. Maritime 4.0—Opportunities in Digitalization and Advanced Manufacturing for Vessel Development. Procedia Manuf. 2020, 42, 246–253. [Google Scholar] [CrossRef]
- De la Peña Zarzuelo, I.; Freire Soeane, M.J.; López Bermúdez, B. Industry 4.0 in the Port and Maritime Industry: A Literature Review. J. Ind. Inf. Integr. 2020, 20, 100173. [Google Scholar] [CrossRef]
- Öztürk, Ü.; Boz, H.A.; Balcisoy, S. Visual Analytic Based Ship Collision Probability Modeling for Ship Navigation Safety. Expert. Syst. Appl. 2021, 175, 114755. [Google Scholar] [CrossRef]
- Paik, J.K. Ship-Shaped Offshore Installations: Design, Construction, Operation, Healthcare and Decommissioning; Cambridge University Press: Cambridge, UK, 2022; ISBN 9781316519608. [Google Scholar]
- Paik, J.K. Digital Healthcare Engineering for Marine Applications. In Proceedings of the International Conference on Marine Equipment & Technology and Sustainable Development, Beijing, China, 1 April 2023. [Google Scholar]
- Paik, J.K. Enhancing Safety and Sustainability through Digital Healthcare Engineering. In Marine Technology; The Society ofNaval Architects and Marine Engineers: Alexandria, VA, USA, 2024; pp. 34–40. [Google Scholar]
- Sindi, A.; Kim, H.J.; Yang, Y.J.; Thomas, G.; Paik, J.K. Advancing Digital Healthcare Engineering for Aging Ships and Offshore Structures: An in-Depth Review and Feasibility Analysis. Data-Centric Eng. 2024, 5, e18. [Google Scholar] [CrossRef]
- Mohammad Fadzil, N.; Muda, M.F.; Abdul Shahid, M.D.; Mustafa, W.A.; Hairil Mohd, M.; Paik, J.K.; Mohd Hashim, M.H. Digital Healthcare Engineering for Aging Offshore Pipelines: A State-of-the-Art Review. Ships Offshore Struct. 2024, 1–14. [Google Scholar] [CrossRef]
- Mauro, F.; Kana, A.A. Digital Twin for Ship Life-Cycle: A Critical Systematic Review. Ocean. Eng. 2023, 269, 113479. [Google Scholar] [CrossRef]
- Han, S.; Li, F.; Lee, C.H.; Wang, T.; Diaconeasa, M.A. Mirror the Mind of Crew: Maritime Risk Analysis with Explicit Cognitive Processes in a Human Digital Twin. Adv. Eng. Inform. 2024, 62, 102746. [Google Scholar] [CrossRef]
- Grieves, M. Digital Twin: Manufacturing Excellence through Virtual Factory Replication. White Pap. 2015, 1, 1–7. [Google Scholar]
- Hu, W.; Zhang, T.; Deng, X.; Liu, Z.; Tan, J. Digital Twin: A State-of-the-Art Review of Its Enabling Technologies, Applications and Challenges. J. Intell. Manuf. Spec. Equip. 2021, 2, 1–34. [Google Scholar] [CrossRef]
- Söderberg, R.; Wärmefjord, K.; Carlson, J.S.; Lindkvist, L. Toward a Digital Twin for Real-Time Geometry Assurance in Individualized Production. CIRP Ann. Manuf. Technol. 2017, 66, 137–140. [Google Scholar] [CrossRef]
- Qi, Q.; Tao, F.; Hu, T.; Anwer, N.; Liu, A.; Wei, Y.; Wang, L.; Nee, A.Y.C. Enabling Technologies and Tools for Digital Twin. J. Manuf. Syst. 2021, 58, 3–21. [Google Scholar] [CrossRef]
- Cai, Y.; Starly, B.; Cohen, P.; Lee, Y.S. Sensor Data and Information Fusion to Construct Digital-Twins Virtual Machine Tools for Cyber-Physical Manufacturing. Procedia Manuf. 2017, 10, 1031–1042. [Google Scholar] [CrossRef]
- Zaccaria, V.; Stenfelt, M.; Aslanidou, I.; Kyprianidis, K.G. Fleet Monitoring and Diagnostics Framework Based on Digital Twin of Aero-Engines. In Proceedings of the ASME Turbo Expo, Oslo, Norway, 11–15 June 2018; Volume 6, pp. 1–10. [Google Scholar]
- Goossens, P. Industry 4.0 and the Power of the Digital Twin. Maplesoft 2017, 5, 1–17. [Google Scholar]
- Graessler, I.; Poehler, A. Integration of a Digital Twin as Human Representation in a Scheduling Procedure of a Cyber-Physical Production System. In Proceedings of the IEEE International Conference on Industrial Engineering and Engineering Management, Singapore, 10–13 December 2017; pp. 289–293. [Google Scholar]
- Chakshu, N.K.; Carson, J.; Sazonov, I.; Nithiarasu, P. A Semi-Active Human Digital Twin Model for Detecting Severity of Carotid Stenoses from Head Vibration—A Coupled Computational Mechanics and Computer Vision Method. Int. J. Numer. Method. Biomed. Eng. 2019, 35, 1–17. [Google Scholar] [CrossRef]
- Shengli, W. Is Human Digital Twin Possible? Comput. Methods Programs Biomed. Update 2021, 1, 100014. [Google Scholar] [CrossRef]
- Naudet, Y.; Baudet, A.; Risse, M. Human Digital Twin in Industry 4.0: Concept and Preliminary Model. In Proceedings of the IN4PL—Proceedings of the International Conference on Innovative Intelligent Industrial Production and Logistics, Online, 25–27 October 2021; pp. 137–144. [Google Scholar]
- Miller, M.E.; Spatz, E. A Unified View of a Human Digital Twin. Hum.-Intell. Syst. Integr. 2022, 4, 23–33. [Google Scholar] [CrossRef]
- Taylor, N.C.; Bekker, A.; Kruger, K. Mariner 4.0: Intergrating Seafarers into a Maritime 4.0 Emvironment. Int. J. Marit. Eng. 2023, 164, 373–384. [Google Scholar] [CrossRef]
- Stephenson, A.C.; Willis, R.; Alford, C. Using In-Seat Electrical Potential Sensors for Non-Contact Monitoring of Heart Rate, Heart Rate Variability, and Heart Rate Recovery. Int. J. Psychophysiol. 2021, 169, 1–10. [Google Scholar] [CrossRef]
- Tang, X.; Yang, A.; Li, L. Optimization of Nanofiber Wearable Heart Rate Sensor Module for Human Motion Detection. Comput. Math. Methods Med. 2022, 2022, 1747822. [Google Scholar] [CrossRef]
- Su, Y.; Ma, C.; Chen, J.; Wu, H.; Luo, W.; Peng, Y.; Luo, Z.; Li, L.; Tan, Y.; Omisore, O.M.; et al. Printable, Highly Sensitive Flexible Temperature Sensors for Human Body Temperature Monitoring: A Review. Nanoscale Res. Lett. 2020, 15, 1–34. [Google Scholar] [CrossRef]
- Luo, N.; Dai, W.; Li, C.; Zhou, Z.; Lu, L.; Poon, C.C.Y.; Chen, S.C.; Zhang, Y.; Zhao, N. Flexible Piezoresistive Sensor Patch Enabling Ultralow Power Cuffless Blood Pressure Measurement. Adv. Funct. Mater. 2016, 26, 1178–1187. [Google Scholar] [CrossRef]
- Wang, S.; Xiao, J.; Liu, H.; Zhang, L. Silk Nanofibrous Iontronic Sensors for Accurate Blood Pressure Monitoring. Chem. Eng. J. 2023, 453, 139815. [Google Scholar] [CrossRef]
- Chu, M.; Nguyen, T.; Pandey, V.; Zhou, Y.; Pham, H.N.; Bar-Yoseph, R.; Radom-Aizik, S.; Jain, R.; Cooper, D.M.; Khine, M. Respiration Rate and Volume Measurements Using Wearable Strain Sensors. NPJ Digit. Med. 2019, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.K.; Yoon, S.; Cho, Y.H. Wearable Sweat Rate Sensors for Human Thermal Comfort Monitoring. Sci Rep 2018, 8, 1181. [Google Scholar] [CrossRef]
- Kun, H.; Bin, L.; Orban, M.; Donghai, Q.; Hongbo, Y. Accurate Flexible Temperature Sensor Based on Laser-Induced Graphene Material. Shock. Vib. 2021, 2021, 9938010. [Google Scholar] [CrossRef]
- Yu, Y.; Peng, S.; Islam, M.; Wu, S.; Wang, C.H. Wearable Supercapacitive Temperature Sensors with High Accuracy Based on Ionically Conductive Organogel and Macro-Kirigami Electrode. Adv. Mater. Technol. 2023, 8, 2201020. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, J.; Jang, B.; Kim, S.; Sharma, B.K.; Kim, J.H.; Ahn, J.H. Graphene-Based Stretchable/Wearable Self-Powered Touch Sensor. Nano Energy 2019, 62, 259–267. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, Y.; Gu, H.; Zhu, P.; Jiang, W.; Zhang, G.; Sun, R.; Wong, C.P. A Highly Sensitive and Cost-Effective Flexible Pressure Sensor with Micropillar Arrays Fabricated by Novel Metal-Assisted Chemical Etching for Wearable Electronics. Adv. Mater. Technol. 2019, 4, 1900367. [Google Scholar] [CrossRef]
- Yao, D.J.; Tang, Z.; Zhang, L.; Liu, Z.G.; Sun, Q.J.; Hu, S.C.; Liu, Q.X.; Tang, X.G.; Ouyang, J. A Highly Sensitive, Foldable and Wearable Pressure Sensor Based on MXene-Coated Airlaid Paper for Electronic Skin. J. Mater. Chem. C Mater. 2021, 9, 12642–12649. [Google Scholar] [CrossRef]
- Li, X.; Chen, S.; Peng, Y.; Zheng, Z.; Li, J.; Zhong, F. Materials, Preparation Strategies, and Wearable Sensor Applications of Conductive Fibers: A Review. Sensors 2022, 22, 3028. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Lin, Z.; Dong, S.; Chen, M. Review of Wearable Optical Fiber Sensors: Drawing a Blueprint for Human Health Monitoring. Opt. Laser Technol. 2023, 161, 109227. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, F.; Hu, Z.; Li, M.; Ouyang, S.; Wu, Y.; Wang, S.; Li, Z.; Qian, J.; Wang, L.; et al. Applications of Cellulose-Based Flexible Self-Healing Sensors for Human Health Monitoring. Nano Energy 2024, 127, 109790. [Google Scholar] [CrossRef]
- Malode, S.J.; Alshehri, M.A.; Shetti, N.P. Revolutionizing Human Healthcare with Wearable Sensors for Monitoring Human Strain. Colloids Surf. B Biointerfaces 2025, 246, 114384. [Google Scholar] [CrossRef]
- Xie, J.; Pan, S.; Zhang, Y.; Wang, H.; He, J.; Guo, R. Knitted Fabric-Based Flexible Piezoresistive Pressure Sensors for Human Monitoring and Underwater Emergency Rescue. Sens. Actuators A Phys. 2025, 382, 116183. [Google Scholar] [CrossRef]
- Liu, X. Evolution of Fiber-Optic Transmission and Networking toward the 5G Era. iScience 2019, 22, 489–506. [Google Scholar] [CrossRef]
- Zhuang, X.; Xu, Y.; Gao, Y.; Sun, G.; Lin, T.; Chan, C.C.K. Remote Data Transmission Technology Based on BeiDou Satellite Navigation Sensor System Onboard Ship. Sens. Mater. 2021, 33, 715–726. [Google Scholar] [CrossRef]
- Zhou, F.; Fan, Y.; Zou, J.; An, B. Ship Emission Monitoring Sensor Web for Research and Application. Ocean Eng. 2022, 249, 110980. [Google Scholar] [CrossRef]
- Bilberg, A.; Malik, A.A. Digital Twin Driven Human–Robot Collaborative Assembly. CIRP Ann. 2019, 68, 499–502. [Google Scholar] [CrossRef]
- Roupa, I.; da Silva, M.R.; Marques, F.; Gonçalves, S.B.; Flores, P.; da Silva, M.T. On the Modeling of Biomechanical Systems for Human Movement Analysis: A Narrative Review. Arch. Comput. Methods Eng. 2022, 29, 4915–4958. [Google Scholar] [CrossRef]
- Wakabayashi, K.; Oda, T.; Okage, K.; Barolli, L. A Simulation System for Decision of Camera Position and Angle: Human Motion Analysis in Case of Dangerous Posture Scenarios. Internet Things 2025, 30, 101471. [Google Scholar] [CrossRef]
- Moingeon, P.; Chenel, M.; Rousseau, C.; Voisin, E.; Guedj, M. Virtual Patients, Digital Twins and Causal Disease Models: Paving the Ground for in Silico Clinical Trials. Drug Discov. Today 2023, 28, 103605. [Google Scholar] [CrossRef]
- Wang, H.; Arulraj, T.; Ippolito, A.; Popel, A.S. From Virtual Patients to Digital Twins in Immuno-Oncology: Lessons Learned from Mechanistic Quantitative Systems Pharmacology Modeling. NPJ Digit Med 2024, 7, 189. [Google Scholar] [CrossRef]
- Laubenbacher, R.; Mehrad, B.; Shmulevich, I.; Trayanova, N. Digital Twins in Medicine. Nat. Comput. Sci. 2024, 4, 184–191. [Google Scholar] [CrossRef]
- Vallée, A. Envisioning the Future of Personalized Medicine: Role and Realities of Digital Twins. J. Med. Internet Res. 2024, 26, e50204. [Google Scholar] [CrossRef]
- Kan Yeung, A.W.; Tosevska, A.; Klager, E.; Eibensteiner, F.; Laxar, D.; Stoyanov, J.; Glisic, M.; Zeiner, S.; Kulnik, S.T.; Crutzen, R.; et al. Virtual and Augmented Reality Applications in Medicine: Analysis of the Scientific Literature. J. Med. Internet Res. 2021, 23, 1–36. [Google Scholar]
- Prajapati, M.; Kumar, S. Virtual Reality Revolution in Healthcare: A Systematic Review. Health Technol. 2025, 15, 231–242. [Google Scholar] [CrossRef]
- Xuan, D.T.; Van Huynh, T.; Hung, N.T.; Thang, V.T. Applying Digital Twin and Multi-Adaptive Genetic Algorithms in Human–Robot Cooperative Assembly Optimization. Appl. Sci. 2023, 13, 4229. [Google Scholar] [CrossRef]
- Nguyen, B.; Coelho, Y.; Bastos, T.; Krishnan, S. Trends in Human Activity Recognition with Focus on Machine Learning and Power Requirements. Mach. Learn. Appl. 2021, 5, 100072. [Google Scholar] [CrossRef]
- Lambay, A.; Liu, Y.; Morgan, P.L.; Ji, Z. Machine Learning Assisted Human Fatigue Detection, Monitoring, and Recovery: A Review. Digit. Eng. 2024, 1, 100004. [Google Scholar] [CrossRef]
- Razavi, M.; Ziyadidegan, S.; Jahromi, R.; Kazeminasab, S.; Baharlouei, E.; Janfaza, V.; Mahmoudzadeh, A.; Sasangohar, F. Machine Learning, Deep Learning and Data Preprocessing Techniques for Detection, Prediction, and Monitoring of Stress and Stress-Related Mental Disorders: A Scoping Review. JMIR Ment. Heal. 2023, 11, e53714. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.J.S.; Cardoso, J.M.P.; Mendes-Moreira, J. KNN Prototyping Schemes for Embedded Human Activity Recognition with Online Learning. Computers 2020, 9, 96. [Google Scholar] [CrossRef]
- Subramanian, B.; Kim, J.; Maray, M.; Paul, A. Digital Twin Model: A Real-Time Emotion Recognition System for Personalized Healthcare. IEEE Access 2022, 10, 81155–81165. [Google Scholar] [CrossRef]
- Moztarzadeh, O.; Jamshidi, M.; Sargolzaei, S.; Jamshidi, A.; Baghalipour, N.; Malekzadeh Moghani, M.; Hauer, L. Metaverse and Healthcare: Machine Learning-Enabled Digital Twins of Cancer. Bioengineering 2023, 10, 455. [Google Scholar] [CrossRef]
- Ahmed, I.; Ahmad, M.; Jeon, G. Integrating Digital Twins and Deep Learning for Medical Image Analysis in the Era of COVID-19. Virtual Real. Intell. Hardw. 2022, 4, 292–305. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, Y.; Gu, B.; Cao, S.; Fang, D. Identifying Mental Fatigue of Construction Workers Using EEG and Deep Learning. Autom. Constr. 2023, 151, 104887. [Google Scholar] [CrossRef]
- Su, T.; Sun, H.; Ma, C.; Jiang, L.; Xu, T. HDL: Hierarchical Deep Learning Model Based Human Activity Recognition Using Smartphone Sensors. In Proceedings of the International Joint Conference on Neural Networks 2019, Budapest, Hungary, 14–19 July 2019. [Google Scholar] [CrossRef]
- Irfan, S.; Anjum, N.; Masood, N.; Khattak, A.S.; Ramzan, N. A Novel Hybrid Deep Learning Model for Human Activity Recognition Based on Transitional Activities. Sensors 2021, 21, 8227. [Google Scholar] [CrossRef] [PubMed]
- Aryal, A.; Ghahramani, A.; Becerik-Gerber, B. Monitoring Fatigue in Construction Workers Using Physiological Measurements. Autom. Constr. 2017, 82, 154–165. [Google Scholar] [CrossRef]
- Jebelli, H.; Mahdi Khalili, M.; Lee, S. A Continuously Updated, Computationally Efficient Stress Recognition Framework Using Electroencephalogram (EEG) by Applying Online Multitask Learning Algorithms (OMTL). IEEE J. Biomed. Health Inf. 2019, 23, 1928–1939. [Google Scholar] [CrossRef] [PubMed]
- Priya, A.; Garg, S.; Tigga, N.P. Predicting Anxiety, Depression and Stress in Modern Life Using Machine Learning Algorithms. Procedia Comput. Sci. 2020, 167, 1258–1267. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, X.; Zhao, L.; Jones, K. A Case for the Use of Deep Learning Algorithms for Individual and Population Level Assessments of Mental Health Disorders: Predicting Depression among China’s Elderly. J. Affect. Disord. 2025, 369, 329–337. [Google Scholar] [CrossRef]
- Li, C.; Zhang, Z.; Lee, W.S.; Lee, G.H. Convolutional Sequence to Sequence Model for Human Dynamics. In Proceedings of the IEEE Computer Society Conference on Computer Vision and Pattern Recognition; IEEE Computer Society, Salt Lake City, UT, USA, 18–23 June 2018; pp. 5226–5234. [Google Scholar]
- Mehmood, I.; Li, H.; Qarout, Y.; Umer, W.; Anwer, S.; Wu, H.; Hussain, M.; Fordjour Antwi-Afari, M. Deep Learning-Based Construction Equipment Operators’ Mental Fatigue Classification Using Wearable EEG Sensor Data. Adv. Eng. Inform. 2023, 56, 101978. [Google Scholar] [CrossRef]
- Manalu, H.V.; Rifai, A.P. Detection of Human Emotions through Facial Expressions Using Hybrid Convolutional Neural Network-Recurrent Neural Network Algorithm. Intell. Syst. Appl. 2024, 21, 200339. [Google Scholar] [CrossRef]
- Islam, R.; Layek, M.A. StackEnsembleMind: Enhancing Well-Being through Accurate Identification of Human Mental States Using Stack-Based Ensemble Machine Learning. Inf. Med. Unlocked 2023, 43, 101405. [Google Scholar] [CrossRef]
- Sagaro, G.G.; Amenta, F. Past, Present, and Future Perspectives of Telemedical Assistance at Sea: A Systematic Review. Int. Marit. Health 2020, 71, 97–104. [Google Scholar] [CrossRef]
- Hickey, B.A.; Chalmers, T.; Newton, P.; Lin, C.T.; Sibbritt, D.; McLachlan, C.S.; Clifton-Bligh, R.; Morley, J.; Lal, S. Smart Devices and Wearable Technologies to Detect and Monitor Mental Health Conditions and Stress: A Systematic Review. Sensors 2021, 21, 3461. [Google Scholar] [CrossRef]
- Mohammadzadeh, N.; Gholamzadeh, M. Equirements, Challenges, and Key Components to Improve Onboard Medical Care Using Maritime Telemedicine: Narrative Review. Int. J. Telemed. Appl. 2023, 2023, 9389286. [Google Scholar] [CrossRef] [PubMed]
- Seng, K.P.; Ang, L.M.; Peter, E.; Mmonyi, A. Machine Learning and AI Technologies for Smart Wearables. Electronics 2023, 12, 1509. [Google Scholar] [CrossRef]
- Health and Safety Executive. Accident Statistics for Floating Offshore Units on the UK Continental Shelf; Health and Safety Executive: London, UK, 2022. [Google Scholar]
- Supporting Seafarers: Resources and General Information. Available online: https://www.imo.org/en/MediaCentre/HotTopics (accessed on 25 April 2025).
- Yeung, K. Recommendation of the Council on Artificial Intelligence (OECD). Int. Leg. Mater. 2020, 59, 27–34. [Google Scholar] [CrossRef]
- Abila, S.; Kitada, M.; Malecosio, S.; Tang, L.; Subong-Espina, R. Empowering Seafarers as Agents of Their Mental Health: The Role of Information and Communication Technology in Seafarers’ Well-Being. Inquiry 2023, 60, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Battineni, G.; Amenta, F. Designing of an Expert System for the Management of Seafarer’s Health. Digit. Health 2020, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Battineni, G.; Chintalapudi, N.; Gagliardi, G.; Amenta, F. The Use of Radio and Telemedicine by TMAS Centers in Provision of Medical Care to Seafarers: A Systematic Review. J. Pers. Med. 2023, 13, 1171. [Google Scholar] [CrossRef]
- Ara, G. Deciphering the Digital Healthscape: Unveiling the Intricacies of the Internet of Medical Things (IoMT). Technoarete Trans. Adv. Data Sci. Anal. 2024, 3, 1–8. [Google Scholar] [CrossRef]
- Lodha, L.; Baghela, V.S.; Bhuvana, J.; Bhatt, R. A Blockchain-Based Secured System Using the Internet of Medical Things (IOMT) Network for e-Healthcare Monitoring. Meas. Sens. 2023, 30, 100904. [Google Scholar] [CrossRef]
- Singh, A.; Singh, M.; Singh, D. Blockchain Approach to Non-Invasive Gastro-Intestinal Diagnosis System. In Intelligent Human Computer Interaction—Proceedings of the International Conference on Intelligent Human Computer Interaction; Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer: Cham, Switzerland, 2024; Volume 14531, pp. 417–434. [Google Scholar]
- Shyam Mohan, J.S.; Kumaran, N. An Approach for Accessing Patients Records Using Medical Suite Blickchain. In Handbook of Research on Artificial Intelligence and Soft Computing Techniques in Personalized Healthcare Services; Apple Academic Press: New York, NY, USA, 2024; pp. 73–90. ISBN 9781000844276. [Google Scholar]
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth 2020, 8, 18907. [Google Scholar] [CrossRef]
- Choudhury, A.; Asan, O. Impact of Using Wearable Devices on Psychological Distress: Analysis of the Health Information National Trends Survey. Int. J. Med. Inf. 2021, 156, 104612. [Google Scholar] [CrossRef]
- Jonglertmontree, W.; Kaewboonchoo, O.; Morioka, I.; Boonyamalik, P. Mental Health Problems and Their Related Factors among Seafarers: A Scoping Review. BMC Public. Health 2022, 22, 282. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.H.S. Human Digital Twin—A Systematic Review of Business Applications and Future Directions. Master’s Thesis, Lahti University of Technology, Lappeenranta, Finland, 2024. [Google Scholar]
- Paganelli, A.I.; Mondéjar, A.G.; da Silva, A.C.; Silva-Calpa, G.; Teixeira, M.F.; Carvalho, F.; Raposo, A.; Endler, M. Real-Time Data Analysis in Health Monitoring Systems: A Comprehensive Systematic Literature Review. J. Biomed. Inf. 2022, 127, 104009. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, Y.; Yuen, K.F. A Systematic Review on Seafarer Health: Conditions, Antecedents and Interventions. Transp. Policy 2022, 122, 11–25. [Google Scholar] [CrossRef]
- Transforming Industry Using Digital Twin Technology; Mishra, A., El Barachi, M., Kumar, M., Eds.; Springer Nature: Cham, Switzerland, 2024; ISBN 9783031585234. [Google Scholar]
- Wagenhals, L.W.; Zaidi, A.K.; Levis, A.H. Scalable Adaptive Architectures for Maritime Operations Center Command and Control. Office of Naval Research. 2011. [Google Scholar]
- Papachristou, K.; Katsakiori, P.F.; Papadimitroulas, P.; Strigari, L.; Kagadis, G.C. Digital Twins’ Advancements and Applications in Healthcare, Towards Precision Medicine. J. Pers. Med. 2024, 14, 1101. [Google Scholar] [CrossRef]
- Mayer, A.; Greif, L.; Häußermann, T.M.; Otto, S.; Kastner, K.; El Bobbou, S.; Chardonnet, J.-R.; Reichwald, J.; Fleischer, J.; Ovtcharova, J. Digital Twins, Extended Reality, and Artificial Intelligence in Manufacturing Reconfiguration: A Systematic Literature Review. Sustainability 2025, 17, 2318. [Google Scholar] [CrossRef]
- Atienza-Barba, M.; del Río-Rama, M.d.l.C.; Meseguer-Martínez, Á.; Barba-Sánchez, V. Artificial Intelligence and Organizational Agility: An Analysis of Scientific Production and Future Trends. Eur. Res. Manag. Bus. Econ. 2024, 30, 100253. [Google Scholar] [CrossRef]


| Type | Model | Accuracy | Detection | Ref. |
|---|---|---|---|---|
| ML | DTr | 82.6% | Fatigue | [69] |
| KNN | 78.4% | Motions | [62] | |
| SVM | 80.3% | Stress | [70] | |
| NB | 85.5% | Stress | [71] | |
| RF | 73% | Stress | [72] | |
| DL | CNN | \ | Motions | [73] |
| BiLSTM | 99.9% | Fatigue | [74] | |
| CNN | 88.85% | Fatigue | [66] | |
| Hybrid | CNN + LSTM + BiLSTM | 98.38% | Motions | [68] |
| CNN + RNN | 85.71% | Stress | [75] | |
| RF + SVM | 98% | Stress | [76] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, M.-X.; He, K.-H.; Wang, F.; Paik, J.-K. Human Digital Healthcare Engineering for Enhancing the Health and Well-Being of Seafarers and Offshore Workers: A Comprehensive Review. Systems 2025, 13, 335. https://doi.org/10.3390/systems13050335
Cui M-X, He K-H, Wang F, Paik J-K. Human Digital Healthcare Engineering for Enhancing the Health and Well-Being of Seafarers and Offshore Workers: A Comprehensive Review. Systems. 2025; 13(5):335. https://doi.org/10.3390/systems13050335
Chicago/Turabian StyleCui, Meng-Xuan, Kun-Hou He, Fang Wang, and Jeom-Kee Paik. 2025. "Human Digital Healthcare Engineering for Enhancing the Health and Well-Being of Seafarers and Offshore Workers: A Comprehensive Review" Systems 13, no. 5: 335. https://doi.org/10.3390/systems13050335
APA StyleCui, M.-X., He, K.-H., Wang, F., & Paik, J.-K. (2025). Human Digital Healthcare Engineering for Enhancing the Health and Well-Being of Seafarers and Offshore Workers: A Comprehensive Review. Systems, 13(5), 335. https://doi.org/10.3390/systems13050335