Telehealth as a Sociotechnical System: A Systems Analysis of Adoption and Efficacy Among Older Adults Post-COVID-19
Abstract
1. Introduction and Background
2. Materials and Methods
2.1. Information Sources
Preparation for the Review
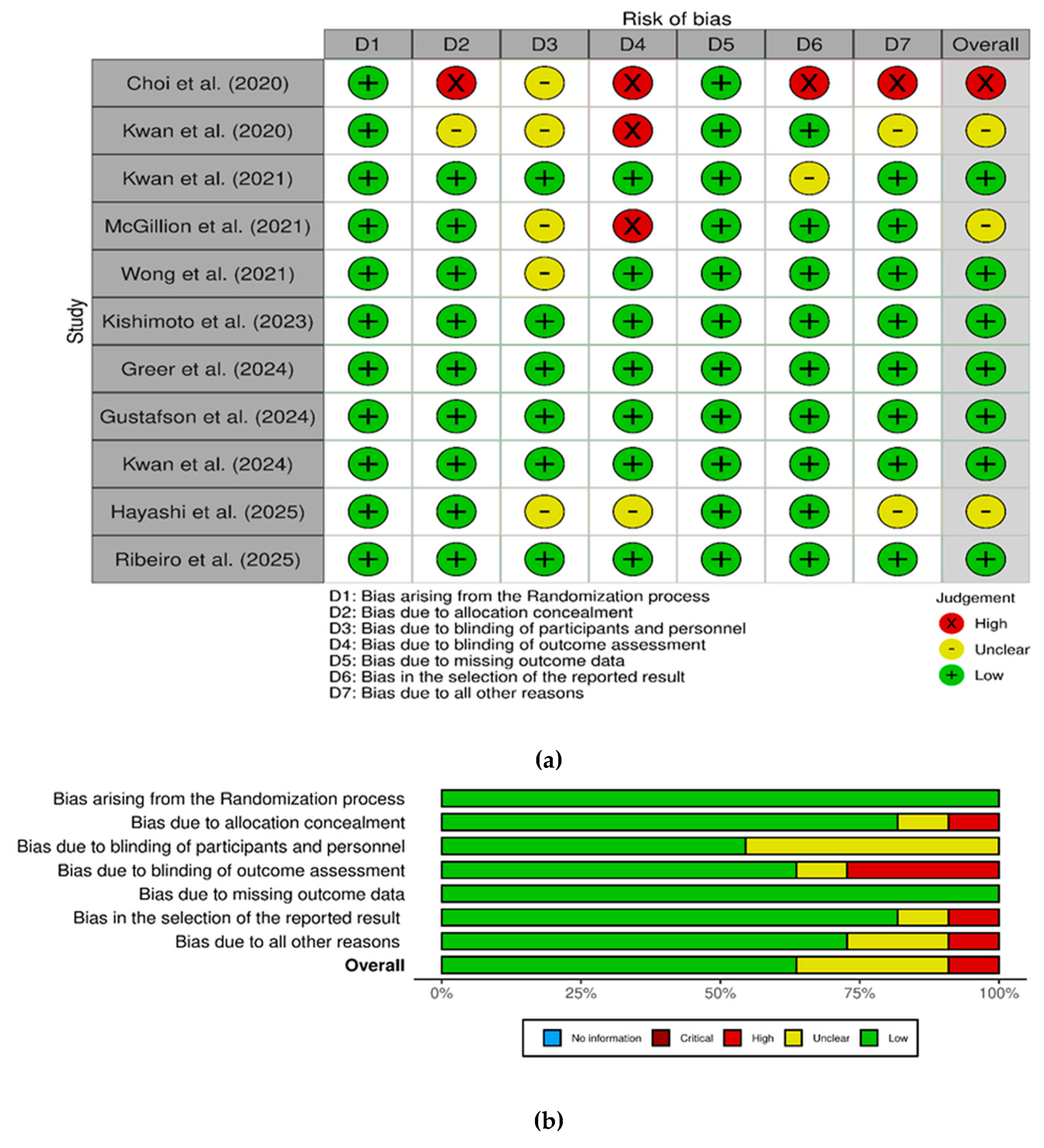
2.2. Quality Assessment (Risk of Bias)
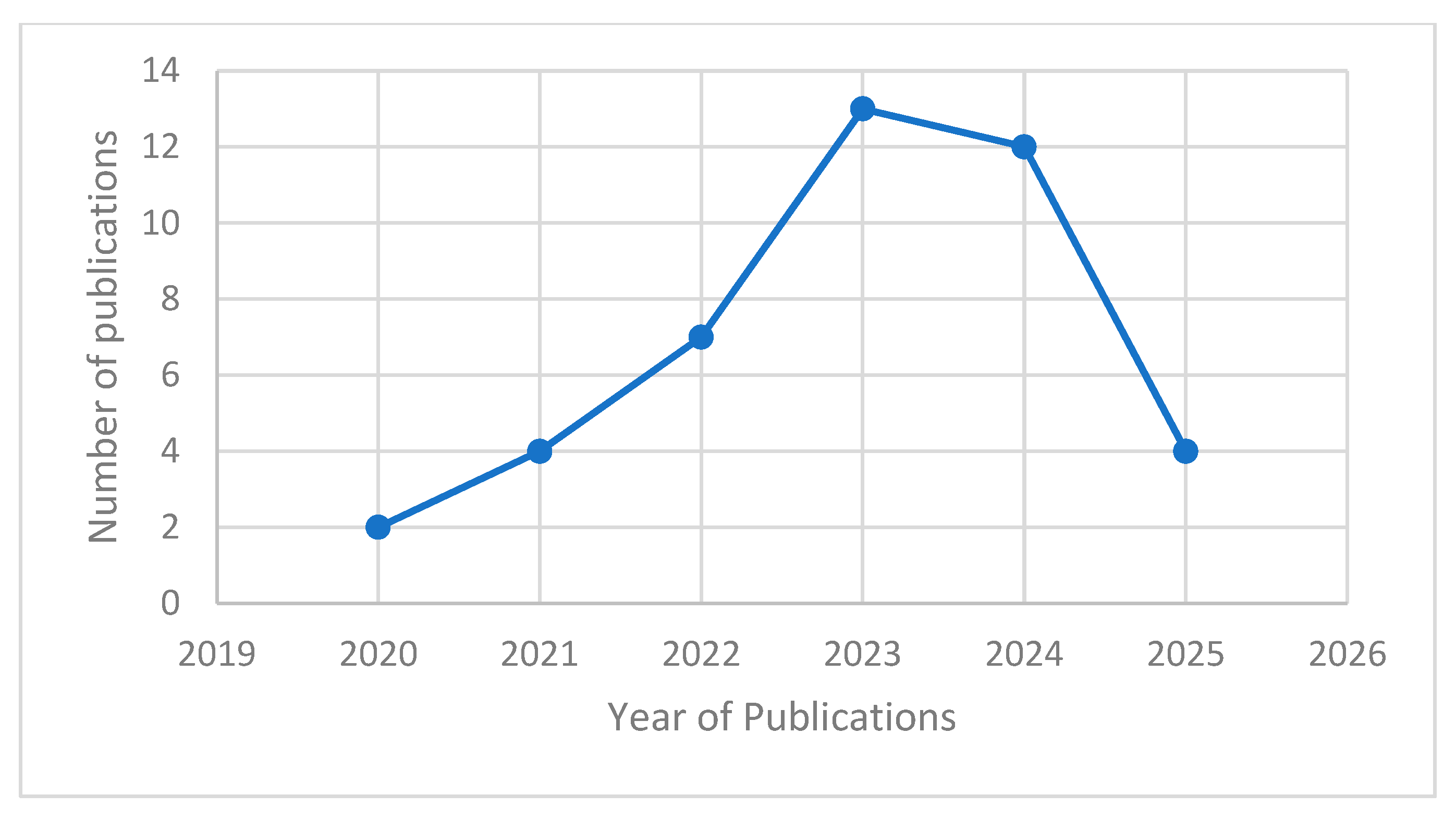
3. Results
3.1. Study Selection and Characteristics
3.2. Study Designs
3.3. Populations and Settings
3.4. Telehealth Modalities
3.5. System Components to Telehealth Adoption in Older Adults
3.5.1. Digital Literacy and Skills
3.5.2. Internet and Device Access
3.5.3. Complexity of Telehealth Platforms
3.5.4. Attitudinal and Trust System Components
3.5.5. Health and Cognitive Limitations
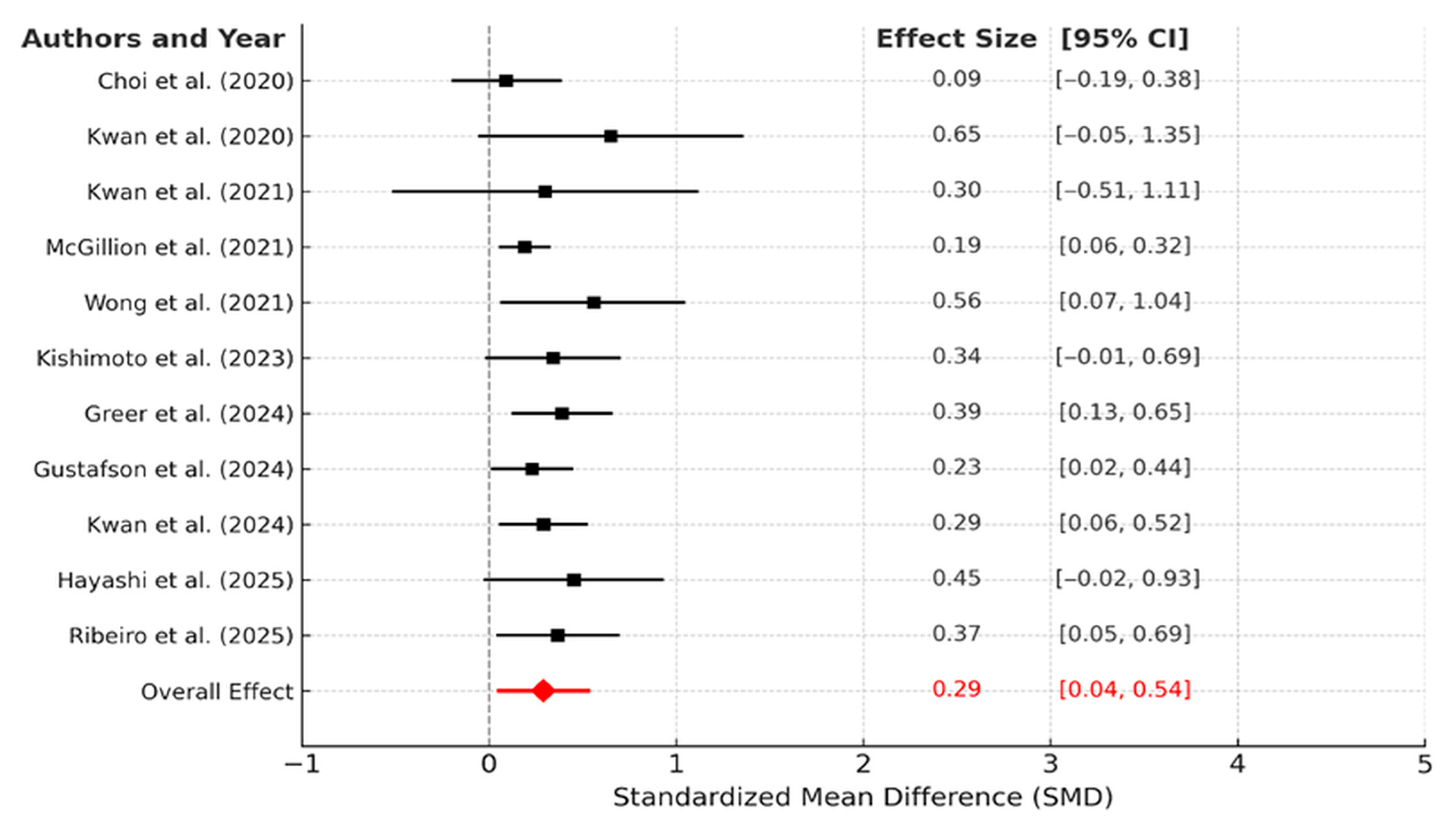
4. Effectiveness of Information and Communication Technology (ICT)-Based Interventions on Cognitive Emergent Properties
4.1. Publication Bias Assessment for ICT-Based Interventions on Cognitive Emergent Properties
4.2. Interpretation of Heterogeneity (I2)
4.3. System-Level Disparities: Emergent Properties of Sociotechnical Interactions
4.3.1. Age (Oldest-Old vs. Young-Old)
4.3.2. Health Literacy and eHealth Literacy
4.3.3. Telehealth Utilization Patterns and Emergent Properties (Pandemic vs. Post-Pandemic Utilization)
4.4. Healthcare Emergent Properties
4.4.1. Access to Care
4.4.2. Patient Satisfaction
4.4.3. Health Emergent Properties
4.4.4. Economic and Convenience Emergent Properties
4.4.5. Quality of Care
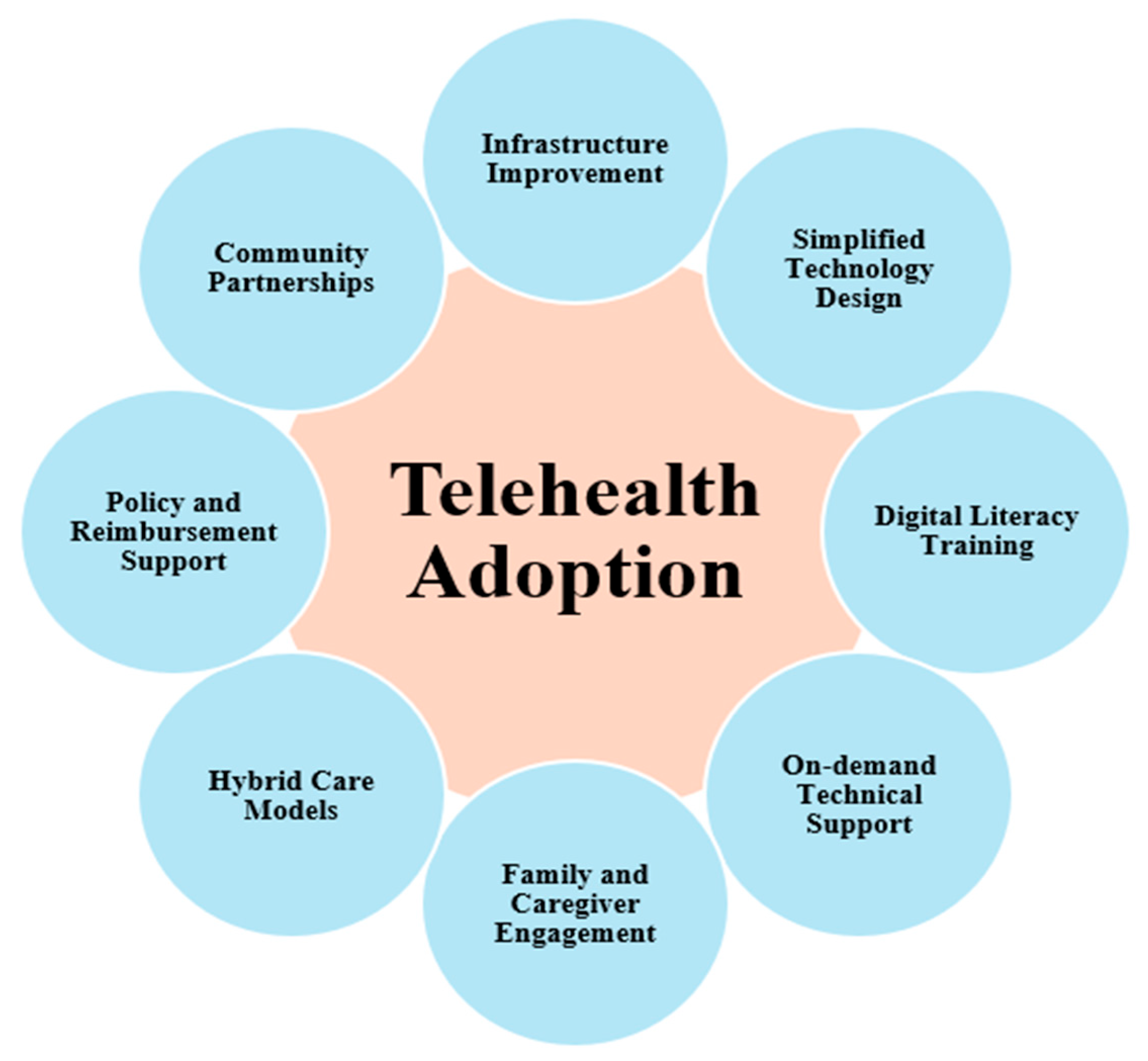
4.5. System Intervention Points and Leverage Strategies
4.5.1. Digital Literacy Training
4.5.2. On-Demand Technical Support
4.5.3. Family and Caregiver Engagement
4.5.4. Simplified Technology and User-Centered Design
4.5.5. Infrastructure and Broadband Expansion
4.5.6. Hybrid Care Models
4.5.7. Policy and Reimbursement Support
4.5.8. Community Partnerships
5. Systems-Level Understanding and Implications
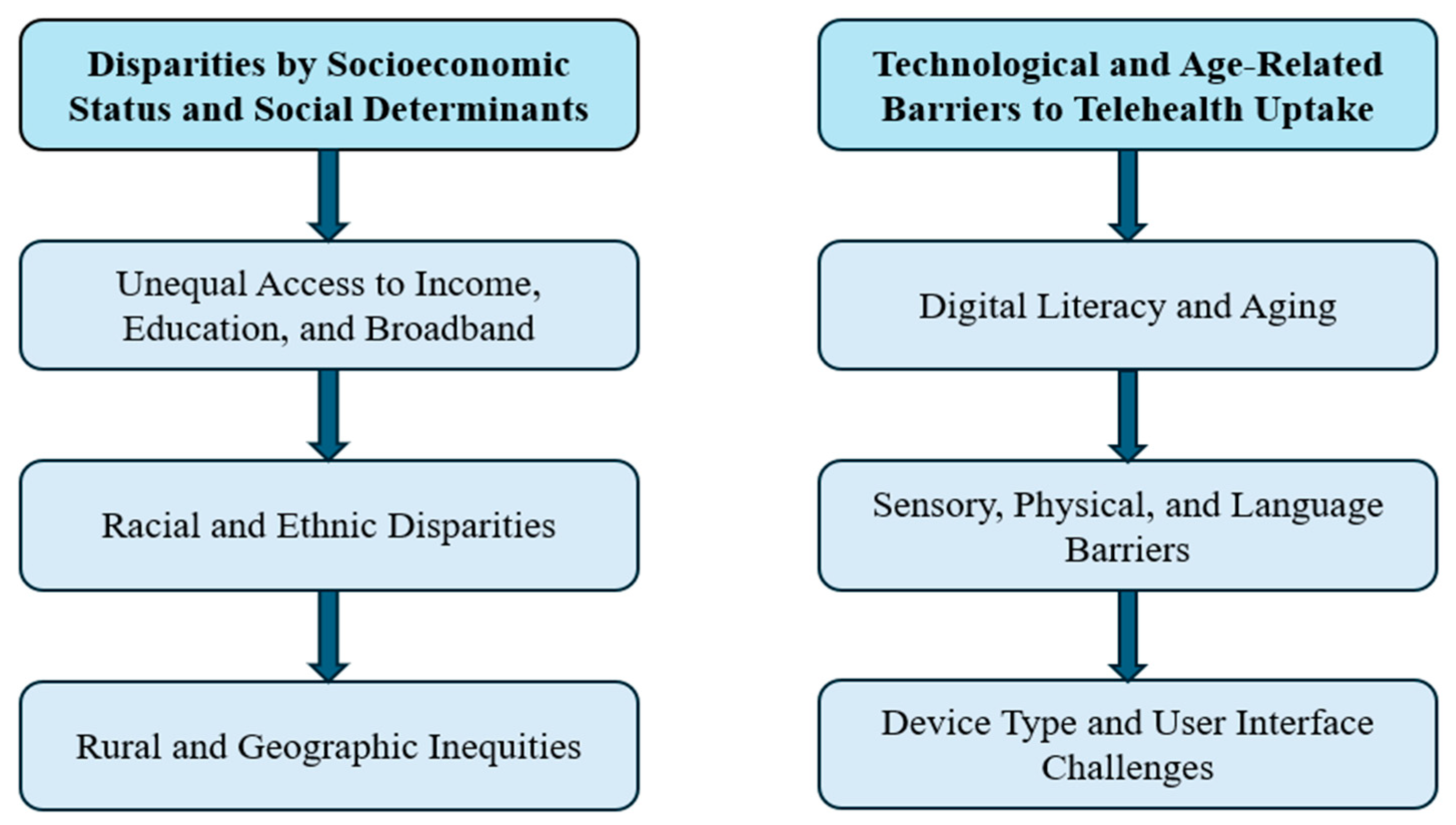
5.1. Disparities by Socioeconomic Status and Social Determinants
5.1.1. Unequal Access to Income, Education, and Broadband
5.1.2. Racial and Ethnic Disparities
5.1.3. Rural and Geographic Inequities
5.2. Technological and Age-Related System Components to Telehealth Uptake
5.2.1. Digital Literacy and Aging
5.2.2. Sensory, Physical, and Language System Components
5.2.3. Device Type and User Interface Challenges
5.3. Necessity for Support and Training
6. Limitations
- Firstly, most of the included studies were observational or cross-sectional in design and conducted during the acute phase of the COVID-19 pandemic (2020–2021), under emergency telehealth policies and conditions that may not reflect long-term patterns of use [47,69]. As a result, causality cannot be inferred from the associations reported, and the findings may be influenced by unmeasured confounders such as pandemic-related anxiety or restricted in-person services [61,62].
- Secondly, there was considerable heterogeneity across studies in terms of populations (e.g., Medicare beneficiaries, veterans, rural residents, racial/ethnic minorities), telehealth modalities (telephone vs. video vs. hybrid models), and emergent properties measured (access, satisfaction, clinical results), which complicates direct comparison and synthesis [49,52,54,70,71,75]. Populations ranged from community-dwelling seniors to veterans in both urban and rural settings, and telehealth was defined [52].
- Another limitation is that most of the included studies were conducted in the United States, with fewer from international settings. Consequently, the findings may reflect U.S.-specific healthcare systems and policies and might not be directly applicable to countries with different health infrastructures or digital systems. Including more international studies in future reviews would help confirm the conclusions across diverse global contexts.
- Only eleven studies provided quantitative data, which limits subgroup analyses and may underestimate variability across interventions. Possible biases include selective reporting and differences in outcome measures. While the random-effects model was suitable given the diversity of studies, the small dataset makes it challenging to fully evaluate model assumptions. Future meta-analyses with more extensive evidence are needed to validate these findings. Moreover, certain vulnerable groups were underrepresented across the dataset, particularly the oldest-old (≥85), those with cognitive impairments, sensory disabilities, or severe frailty, who are likely to face unique system components to telehealth but were often excluded or insufficiently stratified in the analyses [64].
- Although the review included international data (e.g., from Brazil and Malaysia), most of the evidence came from high-income countries, especially the United States, which limits how applicable the findings are to lower-resource settings with limited internet infrastructure or different healthcare systems.
- Finally, potential publication bias cannot be dismissed, as studies showing positive telehealth emergent properties or significant disparities might have been more likely to be published during the COVID-19 digital health surge, possibly leading to an overrepresentation of favorable results.
7. Implications and Policy Recommendations
8. Future Research
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A. JBI Quality Assessment
| Study Type | Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total | JBI Quality Rating | Total Overall Appraisal |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Randomized Control Trial | 27 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | 12 | High | include |
| 28 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 | High | include | |
| 29 | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12 | High | include | |
| 30 | Y | Y | Y | N | Y | Y | Y | Y | N | Y | Y | U | N | 9 | Moderate | include | |
| 31 | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | 11 | High | include | |
| 32 | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | Y | N | 9 | Moderate | include | |
| 33 | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 12 | High | include | |
| 34 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 | High | include | |
| 35 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 | High | include | |
| 36 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 11 | High | include | |
| 37 | Y | U | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 9 | Moderate | include | |
| 38 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 | High | include | |
| Cross-Sectional Survey | 39 | Y | Y | N | Y | Y | U | Y | N | 5 | Moderate | include | |||||
| 40 | Y | Y | Y | Y | N | Y | Y | Y | 7 | High | include | ||||||
| 41 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 43 | Y | Y | Y | N | Y | Y | Y | Y | 7 | High | include | ||||||
| 44 | Y | Y | Y | Y | Y | N | Y | Y | 7 | High | include | ||||||
| 45 | Y | Y | Y | Y | Y | Y | N | Y | 7 | High | include | ||||||
| 46 | Y | Y | Y | Y | Y | N | N | Y | 6 | High | include | ||||||
| 47 | Y | Y | N | Y | U | Y | N | Y | 5 | Moderate | include | ||||||
| 48 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 48 | Y | Y | Y | N | Y | Y | Y | Y | 7 | High | include | ||||||
| 51 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 52 | Y | Y | Y | N | N | Y | Y | Y | 6 | High | include | ||||||
| 54 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 55 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 56 | N | Y | N | Y | Y | Y | U | Y | 5 | Moderate | include | ||||||
| 57 | Y | Y | Y | Y | N | Y | Y | Y | 7 | High | include | ||||||
| 60 | Y | Y | Y | Y | Y | N | Y | Y | 7 | High | include | ||||||
| 61 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 62 | Y | U | Y | Y | N | N | Y | Y | 5 | Moderate | include | ||||||
| 63 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 64 | Y | Y | Y | N | Y | Y | Y | Y | 7 | High | include | ||||||
| 65 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 66 | Y | Y | Y | Y | Y | Y | U | N | 6 | High | include | ||||||
| 67 | Y | Y | Y | Y | N | Y | Y | Y | 7 | High | Include | ||||||
| 68 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 69 | Y | Y | Y | N | N | Y | U | Y | 5 | Moderate | include | ||||||
| 70 | Y | Y | Y | Y | Y | Y | Y | Y | 8 | High | include | ||||||
| 72 | Y | Y | Y | Y | Y | Y | U | Y | 7 | High | include | ||||||
| 73 | Y | Y | Y | Y | N | N | Y | Y | 6 | High | include | ||||||
| 74 | Y | Y | Y | Y | Y | Y | Y | U | 7 | High | include |
Appendix B. Details of the Selected Papers
| Author and Year | Study Topic | Aim of the Study | Key Emergent Properties | Future Direction | |
|---|---|---|---|---|---|
| 1 | Crowe et al. (2024) [39] | Telehealth adoption | 1. Examine the influence of race and rural areas on the adoption of telehealth in Southern Illinois. 2. To find variations in telehealth adoption based on better broadband access. | 1. Urban people have better access to the internet than rural areas. 2. Use of telehealth varies depending on geographic location and race. | 1. Analyze trust-building initiatives between the medical community and skeptical groups. 2. Assess the impact of affordable, high-speed broadband in poor rural areas. |
| 2 | Gmunder et al. (2024) [40] | Telemedicine surge | 1. Identify the key factors most likely to lead to a successful telemedicine visit. 2. To identify which groups of people are unable to use telemedicine during COVID-19. | 1. Identified demographic factors that can predict the duration of a video visit. 2. Older Hispanic people have lower odds of completing telemedicine. | 1. Address broadband restrictions and promote inclusive telemedicine policies. 2. Fix limits on broadband and push for policies that make telemedicine available to everyone. |
| 3 | Haimi and Sergienko (2024) [41] | Telemedicine adoption | The study aims to investigate the use and adoption of three different types of telehealth services by older people in Israel before, during, and after the COVID-19 outbreak. | 1. The older population significantly increased usage of all telehealth services. 2. Women utilized telehealth services more than men. | 1. Measure the impact of user-friendly telehealth system interventions on healthcare utilization and patient satisfaction. |
| 4 | Marcondes et al. (2024) [54] | Telemedicine Use | Determine the racial and ethnic differences in telemedicine utilization and total visits, taking into account geographic, demographic, and clinical factors. | 1. Based on clinical, demographic, and geographic factors, white people had larger telehealth visits than other groups. | 1. Make telehealth easier for minorities to access and use. 2. Implement targeted interventions in areas where telemedicine is not as prevalent. |
| 5 | Kohli et al. (2024) [44] | Telemedicine adoption | 1. Integrate high-speed internet into mental health services 2. Find out how social factors in the U.S. affect high-speed internet access. | 1. Telemedicine makes it easier for people to get mental health care. 2. Linking high-speed internet to mental health tools is crucial. | 1. Investigating the effects of broadband availability outside of homes, such as schools and libraries. 2. Using new data to show how the internet spreads before and after the pandemic. |
| 6 | Falvey et al. (2024) [45] | Telemedicine readiness | 1. Estimate the readiness of older rehabilitation users in the US for video-based telerehabilitation. 2. Assess disparities in readiness among racial and ethnic minority populations. 3. Evaluate disparities in readiness among socioeconomically disadvantaged populations. | 1. Significant disparities in readiness for video-based telerehabilitation. 2. Recommendations include focusing interventions on improving broadband access, technology ownership, and training to ensure equitable adoption in populations with lower readiness. | 1. Conduct longitudinal studies to track changes in telerehabilitation readiness over time. 2. Look at programs that try to help people who are not as ready, like those who live in rural areas or are poor, get better internet access. |
| 7 | Foglia et al. (2024) [65] | Telemedicine adoption | 1. Investigate the feasibility and advantages of the T-CUBE telehealth ecosystem. 2. Assess the T-CUBE’s organizational sustainability in healthcare settings. 3. Measure healthcare professionals’ acceptance and utilization of digital technology. | 1. Exploring the possible benefits of T-CUBE, such as using digital technologies for telemonitoring, telerehabilitation, and tele-supporting. | 1. Explore perceptions of digital technologies among elderly and chronic patients. 2. Implement local support centers for patient assistance and education. 3. Improve sensor options and technologies to ensure scalability and adaptability. |
| 8 | Chandrasekaran (2024) [68] | Telemedicine adoption | 1. Telemedicine usage and trends during the early post-pandemic phase. 2. Patient Health Factors and Telemedicine Disparities | 1. Urban residents used more telemedicine. 2. Better speed internet satisfaction leads to increased usage. | 1. Raise public consciousness and provide education regarding the advantages of telemedicine. 2. Promote policy reforms and research to remove system components and expand telemedicine access. |
| 9 | Jezewski et al. (2022) [48] | Telehealth adoption | 1. To lower telehealth system components in vulnerable individuals through education. 2. To enhance older adults’ access to healthcare, thereby increasing health promotion and proactive service use. | Enhanced trust in using and accessing telehealth services increases the likelihood that health promotion will be implemented among older individuals. | To assess long-term telehealth use and address demographic imbalances to generalize the results. |
| 10 | Ryskina et al. (2021) [67] | Telemedicine adoption | Identify factors of older adults’ telemedicine vs. in-person primary care use among older adults. | 1. Older patients were less likely to use telemedicine. 2. Disparities in access to telemedicine due to age or race. | Evaluating telemedicine for lower-risk visits and avoiding a strict comparison between telemedicine-only and in-person-only visits |
| 11 | Nakayama et al. (2023) [43] | Telehealth adoption | Examine the first-level digital divide in Brazil, assess the variable relationships, and identify challenges and opportunities for implementing digital healthcare. | 1. Older individuals with lower socioeconomic status and rural residents face significant challenges in bridging the digital divide. 2. The digital divide underscores the need to ensure equitable digital healthcare services | To understand how to improve digital healthcare access and evaluate internet access variation during the period, and to conduct prospective analyses. |
| 12 | Tan et al. (2025) [69] | Telehealth adoption | To explore the key determinants influencing the adoption of telehealth among older adults in Malaysia, including transition costs and subjective well-being. | 1. Subjective well-being was the strongest determinant influencing older adults’ intention to use telehealth. 2. Positive attitudes and perceived usefulness significantly influenced telehealth adoption. | 1. To better understand sustained telehealth use and investigate additional influential factors 2. Expanding research into different types of telehealth services and exploring their unique impacts on older adults. |
| 13 | Ganguli et al. (2025) [66] | Telemedicine adoption | To quantify the relationship between telemedicine adoption and low-value testing and spending among fee-for-service Medicare beneficiaries in the US. | 1. Telemedicine adoption was associated with modestly lower usage of 7 out of 20 low-value medical tests. 2. There were slight decreases in spending on 2 of these tests and overall visit spending, despite a slight increase in the total number of visits. | 1. To explore mechanisms behind reduced low-value testing, evaluate telemedicine’s broader effects on healthcare quality, 2. To examine how the adoption of more extensive telemedicine could affect low-value care and associated spending on a larger scale. |
| 14 | Zoorob et al. (2022) [51] | Telemedicine adoption | 1. To identify factors affecting older adults’ use of patient portals and their preferences for future updates. 2. To identify specific, timely improvements to guide developers and healthcare systems in creating actionable plans. | 1. Fear of misuse and privacy issues regarding online personal information are notable concerns. 2. Ownership of technology does not equate to proficiency in use. | 1. Development of educational materials and technical support tailored to older patients. 2. Implement policies that ensure equitable access to technology and the Internet for older patients. |
| 15 | Choi and Lee (2022) [56] | Telehealth service | To mitigate potential risks for secure, error-free, and sustainable digital transformation by enhancing telehealth services for low-income older individuals through failure mode and effects analysis (FMEA). | 1. Lower-income older adults tend to have less experience with technology than other older adults. 2. Research shows that age and education substantially impact ICT use. | 1. Stabilizing the platform or system for easy and non-intrusive access. 2. Increasing the health care provider workforce through continuing education and teleconsultation. |
| 16 | Mao et al. (2022) [47] | Telemedicine adoption | 1. Improve telehealth for low-income older adults by enhancing the quality and reducing errors. 2. Ensure a safe user environment by using the Failure Mode and Effects Analysis (FMEA) tool to manage risks in digital transformation. | Socioeconomic disparities in digital access and telemedicine usage reveal distinct obstacles to telemedicine encountered by older individuals residing in the community. | Implement targeted initiatives to address specific requirements, enhance education about telemedicine, and emphasize its role as a supplement, rather than a substitute, for face-to-face medical attention. |
| 17 | Hunter et al. (2022) [46] | Telehealth services | Examine the factors that facilitate the use of telehealth services among underserved rural communities and enhance healthcare accessibility for older people residing in rural areas. | Telehealth services are made available through fixed community hubs or mobile units, accompanied by support, in conjunction with unrelated services such as Internet banking. | 1. Improving the support infrastructure for telehealth 2. Further integration of telehealth services with non-health-related services, such as online banking |
| 18 | Neumann et al. (2023) [62] | Telehealth adoption | 1. To mitigate technological inequalities among older individuals by improving their telehealth capacities. 2. To assess the efficacy of this method in mitigating inequalities such as inadequate education, income, or technological proficiency. | 1. Enhanced proficiency and self-assurance in participating in diverse telehealth endeavors. 2. Elderly individuals encounter system components such as limited knowledge and poor health while acquiring technical skills. | Exploring long-term impacts and integrating innovative, accessible training methods to enhance telehealth use among older adults. |
| 19 | Yoo et al. (2023) [70] | Telehealth uses | The quality of primary care delivered via telehealth is equitable for older adults across racial and ethnic boundaries. | 1. Blacks and Hispanics had many fewer records in Mobility compared to their counterparts. | In assessing racial and ethnic disparities, documentation is required for telehealth access and equal healthcare service. |
| 20 | Root and Grace (2023) [57] | eMental Health Services | Improving senior well-being and aging through access to online mental health information. | 1. Higher eMental health literacy did not reduce psychological distress as expected. 3. Stress and access to mental health care should be considered when studying the impact of e-mental health literacy. | 1. Examine how enhancing senior adults’ mental health literacy diminishes obstacles to their access to mental health care. 2. Determine whether eMental health literacy is associated with obstacles such as stigma or cost. |
| 21 | Karim et al. (2025) [63] | Telehealth adoption | 1. To examine factors influencing telehealth adoption among rural hospitals during COVID-19. 2. To evaluate its relationship with hospital financial performance. | 1. Many rural hospitals faced system components to telehealth adoption. 2. Telehealth adoption did not significantly impact the financial performance of rural hospitals | 1. To target financially constrained rural hospitals, address systemic components, improve reimbursement policies, and invest in telehealth infrastructure to enhance long-term sustainability. |
| 22 | Cheng et al. (2023) [74] | Telehealth uses | To evaluate video capabilities, eHealth literacy, and engagement with video telehealth among hospitalized patients. | 1. Telehealth use exhibits disparities, which may exacerbate health inequities. 2. Patients favored audio-only telehealth with low electronic health literacy (eHL). | 1. To improve the video capabilities and skills of patients who have difficulty accessing the internet and technology, including eHL. 2. Examine potential interventions to mitigate the digital divide, focusing on marginalized communities. |
| 23 | Dang et al. (2022). [52] | Telehealth adoption | To assess veterans’ disposition, availability, and capacity for high-need, high-risk (HNHR) adults to use telemedicine for their health care needs and access. | 1. A minority of older veterans are fully prepared for video visit-based health care. 2. There is a notable gap in willingness and ability to use video visits among those with poorer health and lower tech skills. | 1. Strategies to enhance the adoption of telehealth in older populations, focusing on age, health literacy, and socioeconomic system components. 2. Gender-specific variations in telehealth readiness and usage among older adults. |
| 24 | Okoye et al. (2021) [55] | Telehealth adoption | Neighborhood broadband internet subscriptions are associated with engagement in telehealth among older adults | The prevalence of neighborhood broadband internet subscription was correlated with telehealth use, whereas race, health, and metropolitan status. | 1. Explore strategies to mitigate telemedicine obstacles among HNHR patients, focusing on the system level. |
| 25 | Madabhushi et al. (2023) [73] | Telemedicine adoption | Patient access to the structural resources required for telehealth | 1. Growing age and Medicare insurance were the most consistent predictors of the absence of telehealth. 2. Telehealth can help decrease healthcare costs and address inequities in rural populations. | The potential for telehealth to be leveraged to overcome healthcare access system components in rural and marginalized populations for further exploration in healthcare policy and service provision. |
| 26 | Alhussein et al. (2023) [60] | Telehealth uses | Participation in telehealth | 1. Lower income and living in non-metro areas had lower odds of using technological devices. | Intersectional technology, health care accessibility, and socioeconomic aspects among older adults. |
| 27 | Adepoju et al. (2023) [61] | Telemedicine adoption | Factors connected with in-person visits compared with telemedicine and hybrid health care visits | 1. Hybrid opportunities can mitigate racial and ethnic disparities in healthcare access. 2. Older adults are more likely to use hybrid work than they were during the pandemic. | Factors affecting the adoption of telemedicine among older adults could lead to targeted interventions, such as promoting hybrid visits, to bridge access disparities. |
| 28 | Broffman et al. (2023) [49] | Telehealth services | 1. The role of wired broadband in telehealth adoption and determining whether smartphones are substitutes in the absence of wired access. 2. Investigate the impact of age, race, and income on telehealth use and ensure equitable access to equal healthcare services. | Elderly individuals exhibit a higher propensity to use computers for telehealth services, underscoring the importance of platform adaptability in catering to various age-related preferences and obstacles. | 1. To investigate improving cell data alongside regular internet, testing subsidies for data costs, and checking how well Wi-Fi spots work. 2. Studies focus on making telehealth easy for different groups of people and keep their information safe. |
| 29 | Bernocchi et al., (2024) [64] | Telehealth adoption | To investigate the effectiveness of telehealth in managing chronic diseases and reducing hospital readmissions among older adults. | Telehealth significantly improved chronic disease management, reduced hospital readmissions, and enhanced patient satisfaction. | Assess the cost-effectiveness and feasibility of integrating telehealth into broader healthcare systems. |
| 30 | Chan et al., (2023) [72] | Telehealth intervention | To evaluate the efficacy of a virtual multidisciplinary telehealth intervention in improving self-management in older adults with multimorbidity. | Virtual intervention significantly improved patients’ self-management skills and enhanced their quality of life. | Extending to larger and diverse populations, incorporating long-term follow-up to assess sustained efficacy. |
| 31 | Choi et al., (2020) [30] | Telehealth effectiveness | To evaluate the clinical effectiveness of behavioral activation treatment via telehealth for depressive symptoms among homebound older adults. | Behavioral activation via telehealth has been shown to reduce depressive symptoms, increase social engagement, and decrease disability. | Conduct studies to compare behavioral activation with other therapeutic interventions and evaluate the long-term emergent properties. |
| 32 | Gustafson et al., (2024) [32] | eHealth intervention | To determine the effectiveness of the Elder Tree eHealth intervention for older adults with multiple chronic conditions on socio-emotional and health emergent properties. | ElderTree significantly improved mental quality of life, with more potent effects for women, and reduced feelings of loneliness among participants. | Conduct further studies to test ElderTree’s targeting of older adults with chronic pain or a higher number of chronic conditions. |
| 33 | Kwan et al., (2020) [27] | mHealth intervention | To examine the feasibility and effects of an mHealth brisk walking intervention to increase physical activity among older adults with cognitive frailty. | mHealth brisk walking significantly improved cognitive function, physical frailty, and moderate-to-vigorous physical activity. | Implement a larger-scale randomized controlled trial to confirm the effectiveness and long-term sustainability of mHealth interventions. |
| 34 | Kwan et al., (2021) [34] | Virtual reality effectiveness | To evaluate the effectiveness of virtual reality motor-cognitive training in improving cognitive and physical function among older adults with cognitive frailty. | VR motor-cognitive training significantly improved cognitive function, reduced frailty, and improved walking speed. | Conduct larger trials to confirm the effects and assess long-term cognitive benefits, as well as patient adherence. |
| 35 | Kwan et al., (2024) [35] | Virtual reality effectiveness | To assess the effects of virtual reality motor-cognitive training compared with non-VR motor-cognitive training on cognitive function in older adults with cognitive frailty. | VR motor-cognitive training significantly enhanced cognitive functions, reduced frailty, and showed good acceptance and adherence among older adults. | Explore efficacy across different intervention intensities, comparing VR versus non-VR training modalities. |
| 36 | Lin et al., (2022) [38] | AIoT-based ergometer effectiveness | To evaluate the feasibility and effectiveness of an Artificial Intelligence Internet-of-Things (AIoT)-based ergometer for physical training in frail elderly with cognitive decline. | AIoT-based ergometers significantly improved muscle strength and physical function, showing high feasibility and acceptability in long-term care facilities. | Expand the AIoT-based system trial to multiple settings and examine long-term clinical and cost-effective emergent properties. |
| 37 | McGillion et al., (2021) [37] | eHealth intervention | To investigate whether combining ElderTree with primary care can improve quality of life, socio-emotional, and physical emergent properties in older adults with multiple chronic conditions. | ElderTree, when combined with primary care, improved mental quality of life, with more significant benefits for women, but a lesser impact on physical emergent properties. | Further trials should focus specifically on subsets of chronic conditions to enhance the physical quality of life, particularly its emergent properties. |
| 38 | Wong et al., (2021) [28] | Telecare management | To evaluate the effectiveness of a telecare case management program for improving self-efficacy, health emergent properties, quality of life, and health care utilization. | The telecare intervention showed significant improvements in medication adherence and physical quality of life. | Future research should involve a larger-scale study to validate the findings and assess the long-term sustainability and cost-effectiveness of telecare. |
| 39 | Ribeiro et al. (2025) [33] | Telemedicine intervention for heart failure | 1. To evaluate whether telemedicine interventions (TMI) added to usual care reduce heart failure (HF) rehospitalizations in Brazil. 2. To assess clinical outcomes, including rehospitalizations, deaths, and adherence. | 1. Nurse-led structured telephone support with cardiologist teleconsultations reduced HF-related rehospitalizations by 44%. 2. Improved self-care, medication adherence, and early detection of decompensation. | 1. Conduct cost-effectiveness evaluations in low- and middle-income countries. 2. Explore the scalability of telemedicine for chronic disease management in resource-limited settings. |
| 40 | Hayashi et al. (2025) [29] | Telemedicine with wearable devices for chronic musculoskeletal pain | 1. To examine whether home-based telemedicine plus wearable devices improves pain-related outcomes compared to usual care. 2. To evaluate changes in physical activity, disability, and quality of life. | 1. At 6 months, the telemedicine group showed significant improvements in pain, anxiety/depression, and disability. 2. Increased daily steps and distance confirmed by wearable devices. | 1. Investigate long-term sustainability of benefits. 2. Explore integration of wearable-based telemedicine into chronic pain management guidelines. |
| 41 | Kishimoto et al. (2024) [36] | Telepsychiatry (two-way video vs. face-to-face) | 1. To test the noninferiority of two-way video psychiatric treatment compared with face-to-face for depression, anxiety, and OCD. 2. To evaluate patient satisfaction, treatment alliance, and discontinuation rates. | 1. Two-way video treatment was noninferior to face-to-face regarding quality of life (SF-36 MCS). 2. No significant difference in treatment efficacy, satisfaction, or adverse events. | 1. Extend evaluation to other psychiatric disorders (e.g., schizophrenia, bipolar). 2. Assess long-term effectiveness and sustainability of telepsychiatry in diverse cultural contexts. |
| 42 | Greer et al. (2024) [31] | Telehealth vs. in-person early palliative care for advanced lung cancer | 1. To compare the effect of early palliative care delivered via secure video versus in-person visits on quality of life in advanced NSCLC patients. 2. To examine caregiver participation, satisfaction, and coping. | 1. Quality-of-life outcomes were equivalent between telehealth and in-person groups (FACT-L scores). 2. Caregiver participation rates were lower in the telehealth group, but patient and caregiver satisfaction did not differ. | 1. Inform policies for sustained telehealth reimbursement beyond COVID-19. 2. Address equity barriers (e.g., technology access, digital literacy) for telehealth palliative care. |
References
- Verma, J.; Mishra, A.S. COVID-19 infection: Disease detection and mobile technology. PeerJ 2020, 8, e10345. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.; Bal-Alvarado, M.; Guerra, F.S.; Ares-Rico, R.; Suárez-Gil, R.; Rodríguez-Álvarez, A.; Pérez-López, A.; Casariego-Vales, E.; on behalf of the TELEA-COVID-19 Joint Monitoring Team Lugo; TELEA COVID-19 Team (Lugo); et al. Monitoring of COVID-19 patients via telemedicine with telemonitoring. Rev. Clín. Esp. 2020, 220, 472–479. [Google Scholar] [CrossRef]
- Lipsitch, M.; Swerdlow, D.L.; Finelli, L. Defining the Epidemiology of COVID-19—Studies Needed. N. Engl. J. Med. 2020, 382, 1194–1196. [Google Scholar] [CrossRef]
- Little, M.O.; Morley, J.E. Healthcare for older adults in North America: Challenges, successes and opportunities. Age Ageing 2022, 51, afac216. [Google Scholar] [CrossRef]
- World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on EHealth; World Health Organization: Geneva, Switzerland, 2010; 93p. [Google Scholar]
- Samson, L.W.; Tarazi, W.; Turrini, G.; Sheingold, S. Medicare beneficiaries’ use of telehealth in 2020: Trends by beneficiary characteristics and location. Off. Assist. Secr. Plan. Eval. 2021, 3, 1–34. [Google Scholar]
- Centers for Medicare & Medicaid Services. Medicare Telehealth Trends Report Medicare FFS Part B Claims Data [Internet]. 2023. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4195038/ (accessed on 24 July 2025).
- Anderson, M.; Perrin, A. Tech Adoption Climbs Among Older Adults; Pew Research Center: Washington, DC, USA, 2017; Available online: https://www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/ (accessed on 20 September 2025).
- Hinton, E.; Guth, M.; Raphael, J.; Haldar, S.; Kff, R.R.; Gifford, K.; Lashbrook, A.; Nardone, M.; Health, M.W.; Associates, M. How the Pandemic Continues to Shape Medicaid Priorities—Results from an Annual Medicaid Budget Survey for State Fiscal Years 2022 and 2023. In Health Policy and Services Research; Kaiser Family Foundation: San Francisco, CA, USA; National Association of Medical Directors: Washington, DC, USA, 2022. [Google Scholar]
- Scott, A.J. The longevity economy. Lancet Healthy Longev. 2021, 2, e828–e835. [Google Scholar] [CrossRef]
- Auyeung, T.W.; Chan, F.H.W.; Chan, T.Y.; Kng, C.P.L.; Lee, J.S.W.; Luk, J.K.H.; Mok, W.Y.W.; Shum, C.K.; Wong, C.W. COVID-19 and older adults: Experience in Hong Kong. Asian J. Gerontol. Geriatr. 2020, 15, 54–59. [Google Scholar] [CrossRef]
- Patel, S.Y.; Mehrotra, A.; Huskamp, H.A.; Uscher-Pines, L.; Ganguli, I.; Barnett, M.L. Variation in telemedicine use and outpatient care during the covid-19 pandemic in the United States. Health Aff. 2021, 40, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Serper, M.; Nunes, F.; Ahmad, N.; Roberts, D.; Metz, D.C.; Mehta, S.J. Positive Early Patient and Clinician Experience with Telemedicine in an Academic Gastroenterology Practice During the COVID-19 Pandemic. Gastroenterology 2020, 159, 1589–1591.e4. [Google Scholar] [CrossRef]
- Van Iterson, E.H.; Laffin, L.J.; Cho, L. National, regional, and urban-rural patterns in fixed-terrestrial broadband internet access and cardiac rehabilitation utilization in the United States. Am. J. Prev. Cardiol. 2023, 13, 100454. [Google Scholar]
- Haimi, M.; Brammli-Greenberg, S.; Waisman, Y.; Baron-Epel, O. Physicians’ experiences, attitudes and challenges in a pediatric telemedicine service. Pediatr. Res. 2018, 84, 650–656. [Google Scholar] [CrossRef]
- Shaver, J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim. Care Clin. Off. Practice. 2022, 49, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Seifert, A.; Cotten, S.R.; Xie, B. A Double Burden of Exclusion? Digital and Social Exclusion of Older Adults in Times of COVID-19. J. Gerontol. Ser. B Psychol. Sci. Soc. Sciences. 2021, 76, E99–E103. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 372. [Google Scholar] [CrossRef]
- Kitchenham, B.; Charters, S. Guidelines for performing Systematic Literature Reviews in Software Engineering. EBSE Technical Report, EBSE-2007-01, Keele University and Durham University Joint Report. 2007. Available online: https://www.elsevier.com/__data/promis_misc/525444systematicreviewsguide.pdf (accessed on 20 September 2025).
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Xiao, Y.; Watson, M. Guidance on Conducting a Systematic Literature Review. J. Plan. Educ. Res. 2019, 39, 93–112. [Google Scholar] [CrossRef]
- Webster, J.; Watson, R.T. Analyzing the Past to Prepare for the Future: Writing a Literature Review. MIS Q. 2002, 26, 13–23. [Google Scholar]
- Okoli, C. A guide to conducting a standalone systematic literature review. Commun. Assoc. Inf. Syst. 2015, 37, 879–910. [Google Scholar] [CrossRef]
- Snyder, H. Literature review as a research methodology: An overview and guidelines. J. Bus. Res. 2019, 104, 333–339. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Kwan, R.Y.C.; Lee, D.; Lee, P.H.; Tse, M.; Cheung, D.S.K.; Thiamwong, L.; Choi, K.S. Effects of an mHealth brisk walking intervention on increasing physical activity in older people with cognitive frailty: Pilot randomized controlled trial. JMIR Mhealth Uhealth 2020, 8, e16596. [Google Scholar] [CrossRef]
- Wong, A.K.C.; Wong, F.K.Y.; Chow, K.K.S.; Wong, S.M.; Lee, P.H. Effect of a Telecare Case Management Program for Older Adults Who Are Homebound during the COVID-19 Pandemic: A Pilot Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2123453. [Google Scholar] [CrossRef]
- Hayashi, K.; Miki, K.; Shiro, Y.; Tetsunaga, T.; Takasusuki, T.; Hosoi, M.; Yukioka, M. Utilization of telemedicine in conjunction with wearable devices for patients with chronic musculoskeletal pain: A randomized controlled clinical trial. Sci. Rep. 2025, 15, 1396. [Google Scholar] [CrossRef]
- Choi, N.G.; Marti, C.N.; Wilson, N.L.; Chen, G.J.; Sirrianni, L.; Hegel, M.T.; Bruce, M.L.; Kunik, M.E. Effect of Telehealth Treatment by Lay Counselors vs by Clinicians on Depressive Symptoms among Older Adults Who Are Homebound: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, E2015648. [Google Scholar] [CrossRef]
- Greer, J.A.; Temel, J.S.; El-Jawahri, A.; Rinaldi, S.; Kamdar, M.; Park, E.R.; Horick, N.K.; Pintro, K.; Rabideau, D.J.; Schwamm, L.; et al. Telehealth vs in-person early palliative care for patients with advanced lung cancer: A multisite randomized clinical trial. JAMA 2024, 332, 1153–1164. [Google Scholar] [CrossRef]
- Gustafson, D.H.; Mares, M.L.; Johnston, D.C.; Mahoney, J.E.; Brown, R.T.; Landucci, G.; Pe-Romashko, K.; Cody, O.J.; Gustafson, D.H.; Shah, D.V. An eHealth Intervention to Improve Quality of Life, Socioemotional, and Health-Related Measures Among Older Adults with Multiple Chronic Conditions: Randomized Controlled Trial. JMIR Aging 2024, 10, e59588. [Google Scholar] [CrossRef]
- Ribeiro, E.G.; Brant, L.C.C.; Rezende, L.C.; Bernal, R.; Chequer, G.; Temponi, B.V.; Vilela, D.B.; Buback, J.B.; Lopes, R.D.; Franco, T.B.; et al. Effect of Telemedicine Interventions on Heart Failure Hospitalizations: A Randomized Trial. J. Am. Heart Assoc. 2025, 14, e036241. [Google Scholar] [CrossRef]
- Kwan, R.Y.C.; Liu, J.Y.W.; Fong, K.N.K.; Qin, J.; Leung, P.K.Y.; Sin, O.S.K.; Hon, P.Y.; Suen, L.W.; Tse, M.K.; Lai, C.K.Y. Feasibility and effects of virtual reality motor-cognitive training in community-dwelling older people with cognitive frailty: Pilot randomized controlled trial. JMIR Serious Games 2021, 9, e28400. [Google Scholar] [CrossRef]
- Kwan, R.Y.C.; Liu, J.; Sin, O.S.K.; Fong, K.N.K.; Qin, J.; Wong, J.C.Y.; Lai, C. Effects of Virtual Reality Motor-Cognitive Training for Older People with Cognitive Frailty: Multicentered Randomized Controlled Trial. J. Med. Internet Res. 2024, 26, e57809. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, T.; Kinoshita, S.; Kitazawa, M.; Hishimoto, A.; Asami, T.; Suda, A.; Bun, S.; Kikuchi, T.; Sado, M.; Takamiya, A.; et al. Live two-way video versus face-to-face treatment for depression, anxiety, and obsessive-compulsive disorder: A 24-week randomized controlled trial. Psychiatry Clin. Neurosci. 2024, 78, 220–228. [Google Scholar] [CrossRef] [PubMed]
- McGillion, M.H.; Parlow, J.; Borges, F.K.; Marcucci, M.; Jacka, M.; Adili, A.; Lalu, M.M.; Ouellette, C.; Bird, M.; Ofori, S.; et al. Post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: Randomised controlled trial. BMJ 2021, 374, n2209. [Google Scholar] [CrossRef]
- Lin, C.C.; Kuo, L.C.; Lin, Y.S.; Chang, C.M.; Hu, F.W.; Chen, Y.J.; Lin, C.T.; Su, F.C. AIoT-Based Ergometer for Physical Training in Frail Elderly with Cognitive Decline: A Pilot Randomized Control Trial. J. Med. Biol. Eng. 2022, 42, 909–921. [Google Scholar] [CrossRef]
- Crowe, J.; Nikolic-Khatatbeh, J.; Li, R. The digital health divide: Understanding telehealth adoption across racial lines in rural Illinois. SSM Popul. Health 2024, 26, 101665. [Google Scholar] [PubMed]
- Gmunder, K.N.; Ruiz, J.W.; Franceschi, D.; Suarez, M.M. Demographics associated with US healthcare disparities are exacerbated by the telemedicine surge during the COVID-19 pandemic. J. Telemed. Telecare 2024, 30, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Haimi, M.; Sergienko, R. Adoption and Use of Telemedicine and Digital Health Services among Older Adults in Light of the COVID-19 Pandemic: Repeated Cross-Sectional Analysis. JMIR Aging 2024, 7, e52317. [Google Scholar] [CrossRef]
- Kim, E.; Han, S. Investigating the digital health acceptance of Korean baby boomers: Comparative study of telemedicine and wearable healthcare devices. Health Policy Technol. 2023, 12, 100727. [Google Scholar] [CrossRef]
- Nakayama, L.F.; Binotti, W.W.; Woite, N.L.; Fernandes, C.O.; Alfonso, P.G.; Celi, L.A.; Regatieri, C.V. The Digital Divide in Brazil and Barriers to Telehealth and Equal Digital Health Care: Analysis of Internet Access Using Publicly Available Data. J. Med. Internet Res. 2023, 25, e42483. [Google Scholar] [CrossRef]
- Kohli, K.; Jain, B.; Patel, T.A.; Eken, H.N.; Dee, E.C.; Torous, J. The digital divide in access to broadband internet and mental healthcare. Nat. Ment. Health 2024, 2, 88–95. [Google Scholar] [CrossRef]
- Falvey, J.R.; Sun, N.; Miller, M.J.; Pravdo, A.; Mullins, C.D. Demystifying the Digital Divide: Disparities in Telerehabilitation Readiness Among Older Adults in the United States. Arch. Phys. Med. Rehabil. 2024, 105, 1255–1261. [Google Scholar] [CrossRef]
- Hunter, I.; Lockhart, C.; Rao, V.; Tootell, B.; Wong, S. Enabling Rural Telehealth for Older Adults in Underserved Rural Communities: Focus Group Study. JMIR Form. Res. 2022, 6, e35864. [Google Scholar] [CrossRef] [PubMed]
- Mao, A.; Tam, L.; Xu, A.; Osborn, K.; Sheffrin, M.; Gould, C.; Schillinger, E.; Martin, M.; Mesias, M. Barriers to Telemedicine Video Visits for Older Adults in Independent Living Facilities: Mixed Methods Cross-sectional Needs Assessment. JMIR Aging 2022, 5, e34326. [Google Scholar] [CrossRef] [PubMed]
- Jezewski, E.; Miller, A.; Eusebio, M.A.; Potter, J. Targeted Telehealth Education Increases Interest in Using Telehealth among a Diverse Group of Low-Income Older Adults. Int. J. Env. Res. Public Health 2022, 19, 13349. [Google Scholar] [CrossRef] [PubMed]
- Broffman, L.; Harrison, S.; Zhao, M.; Goldman, A.; Patnaik, I.; Zhou, M. The Relationship Between Broadband Speeds, Device Type, Demographic Characteristics, and Care-Seeking Via Telehealth. Telemed. E-Health 2023, 29, 425–431. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef]
- Zoorob, D.; Hasbini, Y.; Chen, K.; Wangia-Anderson, V.; Moussa, H.; Miller, B.; Brobst, D. Ageism in healthcare technology: The older patients’ aspirations for improved online accessibility. JAMIA Open 2022, 5, ooac061. [Google Scholar] [CrossRef]
- Dang, S.; Muralidhar, K.; Li, S.; Tang, F.; Mintzer, M.; Ruiz, J.; Valencia, W.M. Gap in Willingness and Access to Video Visit Use Among Older High-risk Veterans: Cross-sectional Study. J. Med. Internet Res. 2022, 24, e32570. [Google Scholar] [CrossRef]
- Le, T.V.; Galperin, H.; Traube, D. The impact of digital competence on telehealth utilization. Health Policy Technol. 2023, 12, 100724. [Google Scholar] [CrossRef]
- Marcondes, F.O.; Normand, S.L.T.; Le Cook, B.; Huskamp, H.A.; Rodriguez, J.A.; Barnett, M.L.; Uscher-Pines, L.; Busch, A.B.; Mehrotra, A. Racial and Ethnic Differences in Telemedicine Use. JAMA Health Forum. 2024, 5, E240131. [Google Scholar] [CrossRef]
- Okoye, S.M.; Mulcahy, J.F.; Fabius, C.D.; Burgdorf, J.G.; Wolff, J.L. Neighborhood broadband and use of telehealth among older adults: Cross-sectional study of national survey data linked with census data. J. Med. Internet Res. 2021, 23, e26242. [Google Scholar] [CrossRef]
- Choi, H.; Lee, S.K. Failure mode and effects analysis of telehealth service of minority elderly for sustainable digital transformation. Comput. Biol. Med. 2022, 148, 105950. [Google Scholar] [CrossRef]
- Root, E.Z.; Caskie, G.I.L. The Associations between eMental Health Literacy, Barriers to Mental Health Services, and Psychological Distress in Older Adults. J. Appl. Gerontol. 2023, 42, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Bajgain, B.; Rabi, S.; Ahmed, S.; Kiryanova, V.; Fairie, P.; Santana, M.J. Patient-Reported Experiences and Outcomes of Virtual Care during COVID-19: A Systematic Review. J. Patient-Rep. Outcomes 2023, 7, 126. [Google Scholar] [CrossRef] [PubMed]
- Kunonga, T.P.; Spiers, G.F.; Beyer, F.R.; Hanratty, B.; Boulton, E.; Hall, A.; Bower, P.; Todd, C.; Craig, D. Effects of digital technologies on older people’s access to health and social care: Umbrella review. J. Med. Internet Res. 2021, 23, e25887. [Google Scholar] [CrossRef]
- Alhussein, M.; Patel, B.; Liu, X. Closing the gap: Technology access and telehealth use among older adults in the US Medicare beneficiaries. Telemat. Inform. Rep. 2023, 12, 100103. [Google Scholar] [CrossRef]
- Adepoju, O.E.; Dang, P.; Valdez, M.R. Comparing In-Person Only, Telemedicine Only, and Hybrid Health Care Visits Among Older Adults in Safety-Net Clinics. In Telemedicine Reports; Mary Ann Liebert Inc.: New Rochelle, NY, USA, 2023; pp. 93–99. [Google Scholar]
- Neumann, A.V.; Gonzalez, A.; Walter, L.C.; Rivera, J. Improving older adults’ telehealth through a novel community–academic partnership: Preliminary data. J. Am. Geriatr. Soc. 2023, 71, 3886–3895. [Google Scholar] [CrossRef]
- Karim, S.A.; Tilford, J.M.; Bogulski, C.A.; Hayes, C.J.; Eswaran, H. Exploring telehealth adoption and financial outcomes for rural hospitals during the COVID-19 public health emergency. J. Rural Health 2025, 41, e70038. [Google Scholar] [CrossRef] [PubMed]
- Bernocchi, P.; Giudici, V.; Borghi, G.; Bertolaia, P.; D’Isa, S.; Trevisan, R.; Scalvini, S. Telemedicine home-based management in patients with chronic heart failure and diabetes type II: Study protocol for a randomized controlled trial. Trials 2024, 25, 333. [Google Scholar] [CrossRef]
- Foglia, E.; Garagiola, E.; Bellavia, D.; Rossetto, F.; Baglio, F. Digital technology and COVID-19 pandemic: Feasibility and acceptance of an innovative telemedicine platform. Technovation 2024, 130, 102941. [Google Scholar] [CrossRef]
- Ganguli, I.; Lim, C.; Daley, N.; Cutler, D.; Rosenthal, M.; Mehrotra, A. Telemedicine Adoption and Low-Value Care Use and Spending Among Fee-for-Service Medicare Beneficiaries. JAMA Intern. Med. 2025, 185, 440. [Google Scholar] [CrossRef]
- Ryskina, K.L.; Shultz, K.; Zhou, Y.; Lautenbach, G.; Brown, R.T. Older adults’ access to primary care: Gender, racial, and ethnic disparities in telemedicine. J. Am. Geriatr. Soc. 2021, 69, 2732–2740. [Google Scholar] [CrossRef]
- Chandrasekaran, R. Telemedicine in the Post-Pandemic Period: Understanding Patterns of Use and the Influence of Socioeconomic Demographics, Health Status, and Social Determinants. Telemed. E-Health 2024, 30, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.H.; Yap, Y.Y.; Tan, S.K.; Wong, C.K. Determinants of Telehealth Adoption Among Older Adults: Cross-Sectional Survey Study. JMIR Aging 2025, 8, e60936. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.W.; Kang, H.T.; Choe, I.; Kim, L.; Han, D.H.; Shen, J.J.; Kim, Y.; Reed, P.S.; Ioanitoaia-Chaudhry, I.; Chong, M.T.; et al. Racial and Ethnic Disparity in 4Ms among Older Adults Among Telehealth Users as Primary Care. Gerontol. Geriatr. Med. 2023, 9, 23337214231189053. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N.; Choi, B.Y. Telehealth use among older adults during COVID-19: Associations with sociodemographic and health characteristics, technology device ownership, and technology learning. J. Appl. Gerontol. 2022, 41, 600–609. [Google Scholar] [CrossRef]
- Chan, K.O.; Yuen, P.P.; Fong, B.Y.; Law, V.T.; Ng, F.S.; Fung, W.C.; Ng, T.K.; Cheung, I.S. Effectiveness of telehealth in preventive care: A study protocol for a randomised controlled trial of tele-exercise programme involving older people with possible sarcopenia or at risk of fall. BMC Geriatr. 2023, 23, 845. [Google Scholar] [CrossRef]
- Madabhushi, V.; McLouth, C.J.; King, R.; Bhakta, A.; Beck, S.; Patel, J.A. Age and Medicare Insurance are Barriers to Telemedicine Access—A Quality Improvement Project. Am. Surg. 2023, 89, 1643–1649. [Google Scholar] [CrossRef]
- Cheng, J.; Arora, V.M.; Kappel, N.; Vollbrecht, H.; Meltzer, D.O.; Press, V. Assessing Disparities in Video-Telehealth Use and eHealth Literacy among Hospitalized Patients: Cross-sectional Observational Study. JMIR Form. Res. 2023, 7, e44501. [Google Scholar] [CrossRef] [PubMed]
- Schifeling, C.H.; Shanbhag, P.; Johnson, A.; Atwater, R.C.; Koljack, C.; Parnes, B.L.; Vejar, M.M.; Farro, S.A.; Phimphasone-Brady, P.; Lum, H.D. Disparities in Video and Telephone Visits Among Older Adults During the COVID-19 Pandemic: Cross-Sectional Analysis. JMIR Aging 2020, 3, e23176. [Google Scholar] [CrossRef]
- Yoon, E. Patient-Reported Experiences with Telehealth During the COVID-19 Pandemic and Beyond. Ph.D. Thesis, Northwestern University, Evanston, IL, USA, 2023. [Google Scholar]
- Gustafson, D.H.; Mares, M.L.; Johnston, D.C.; Mahoney, J.E.; Brown, R.T.; Landucci, G.; Pe-Romashko, K.; Cody, O.J.; Gustafson, D.H.; Shah, D.V. A web-based ehealth intervention to improve the quality of life of older adults with multiple chronic conditions: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2021, 10, e25175. [Google Scholar] [CrossRef]
- Amouzadeh, E.; Dianat, I.; Faradmal, J.; Babamiri, M. Optimizing mobile app design for older adults: Systematic review of age-friendly design. Aging Clin. Exp. Res. 2025, 37, 248–260. [Google Scholar] [CrossRef] [PubMed]

| Time Duration | January 2020–June 2025 |
|---|---|
| Source selection | The following databases were systematically searched:
|
| Search strategy | Candidate studies were identified by screening document titles, abstracts, and keywords. Search terms included combinations of: “telehealth”, “telemedicine”, “virtual care”, “digital health”, “older adults”, “elderly”, “COVID-19”, “pandemic”, “health disparities”, “health equity”, and “socioeconomic factors”. |
| Study selection | The final collection of relevant studies will be excluded based on defined inclusion and exclusion criteria (Table 2). |
| Validation process | The entire screening and selection process was independently validated by two reviewers, with discrepancies resolved through discussion and consensus. |
| Databases | Total Article Retrieved | Search Term |
|---|---|---|
| MEDLINE | 127 | (“telehealth” OR “telemedicine” OR “e-health” OR “virtual care” OR “remote health” OR “digital health” OR “mHealth”) AND (“older adults” OR “elderly” OR “aged” OR “senior” OR “geriatric” OR “older people”) AND (“COVID-19” OR “post-COVID-19” OR pandemic OR “post-pandemic”) AND (“health disparities” OR inequities OR inequalities OR “socioeconomic factors” OR “social determinants of health” OR “economic factors” OR “income” OR “education level” OR “health equity”) |
| Web of Science | 318 | |
| EBSCOhost | 344 | |
| ACM Digital Library | 98 | |
| PsycINFO | 77 | |
| Scopus | 754 |
| Topic | Description | Keywords |
|---|---|---|
| Telehealth | Keywords related to telehealth services and remote healthcare |
|
| Older Adults | Keywords specifically targeting the older adult population |
|
| COVID-19/Pandemic | Keywords relevant to the COVID-19 pandemic and its aftermath |
|
| Health Disparities and Socioeconomic Factors | Keywords: capturing health disparities, socioeconomic determinants, and related inequalities |
|
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Year of publication | Article Published Between January 2020 and June 2025 | Year of publication: Before January 2020 |
| Databases | Studies identified from MEDLINE, Web of Science, EBSCOhost, ACM Digital Library, PsycINFO, and Scopus | Studies from databases not specified in the search |
| Publication type | Peer-reviewed journal articles and peer-reviewed conference papers with quantitative emergent properties | Non-peer-reviewed articles, editorials, commentaries, reviews without quantitative emergent properties, opinion pieces, theses, and dissertations |
| Language | Published in English | Published in languages other than English |
| Population | Focused explicitly on older adults aged 60 and above | Studies not focused on older adults (below 60 or unspecified age) |
| Intervention and Context | Studies evaluating telehealth adoption and/or efficacy specifically during or after the COVID-19 pandemic | Studies unrelated to telehealth, telemedicine, or studies outside the COVID-19 or post-pandemic period |
| Emergent properties and Scope | Studies addressing at least one of the following:
| Studies lack clear emergent properties related to telehealth adoption, efficacy, health disparities, socioeconomic dynamics, or quantitative data. |
| Availability | Full text available for quantitative and qualitative analyses | Full text not available or insufficient data for extraction |
| Egger’s Test | Estimate | 95% CI | p-Value |
|---|---|---|---|
| Intercept | 1.24 | [0.27, 2.21] | 0.018 |
| Slope | 0.11 | [−0.02, 0.24] | 0.081 |
| Q Statistic | Degrees of Freedom | I2 (%) | p-Value (Q) |
|---|---|---|---|
| 4.73 | 10 | 0 | 0.579 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabbani, M.G.; Alam, A.; Prybutok, V.R. Telehealth as a Sociotechnical System: A Systems Analysis of Adoption and Efficacy Among Older Adults Post-COVID-19. Systems 2025, 13, 843. https://doi.org/10.3390/systems13100843
Rabbani MG, Alam A, Prybutok VR. Telehealth as a Sociotechnical System: A Systems Analysis of Adoption and Efficacy Among Older Adults Post-COVID-19. Systems. 2025; 13(10):843. https://doi.org/10.3390/systems13100843
Chicago/Turabian StyleRabbani, Md Golam, Ashrafe Alam, and Victor R. Prybutok. 2025. "Telehealth as a Sociotechnical System: A Systems Analysis of Adoption and Efficacy Among Older Adults Post-COVID-19" Systems 13, no. 10: 843. https://doi.org/10.3390/systems13100843
APA StyleRabbani, M. G., Alam, A., & Prybutok, V. R. (2025). Telehealth as a Sociotechnical System: A Systems Analysis of Adoption and Efficacy Among Older Adults Post-COVID-19. Systems, 13(10), 843. https://doi.org/10.3390/systems13100843