Simple Summary
In physical training, it is common to perform preparatory activities to improve the performance of subsequent exercise. One of these activities is inspiratory exercise, which has been increasingly applied as a muscle-warm-up strategy due to the demands on the respiratory muscles in high-intensity effort. Generally, inspiratory exercise is performed by a device that works as an inspiratory exerciser, imposing resistance to the respiratory muscles in the inspiratory phase by restricting airflow. This resistance is based on the assessment of the individual’s global inspiratory-muscle strength (maximum inspiratory pressure). Our review aimed to systematically review the literature in order to examine the effects of inspiratory muscle warm-up on the inspiratory, metabolic, respiratory and performance parameters of a main exercise performed by athletes and healthy and active individuals, taking into account the protocols applied as well as the equipment used as the inspiratory exerciser. According to the results, the inspiratory-muscle warm-up was mostly performed in two series of thirty inspirations at 40% of the maximum inspiratory pressure, using POWERbreathe® (IMT Technologies Ltd., Birmingham, UK). Our review demonstrated that inspiratory-muscle warm-up can be a practical and simple additional resource to improve performance in high-intensity physical exercise, taking into account its individualized prescription.
Abstract
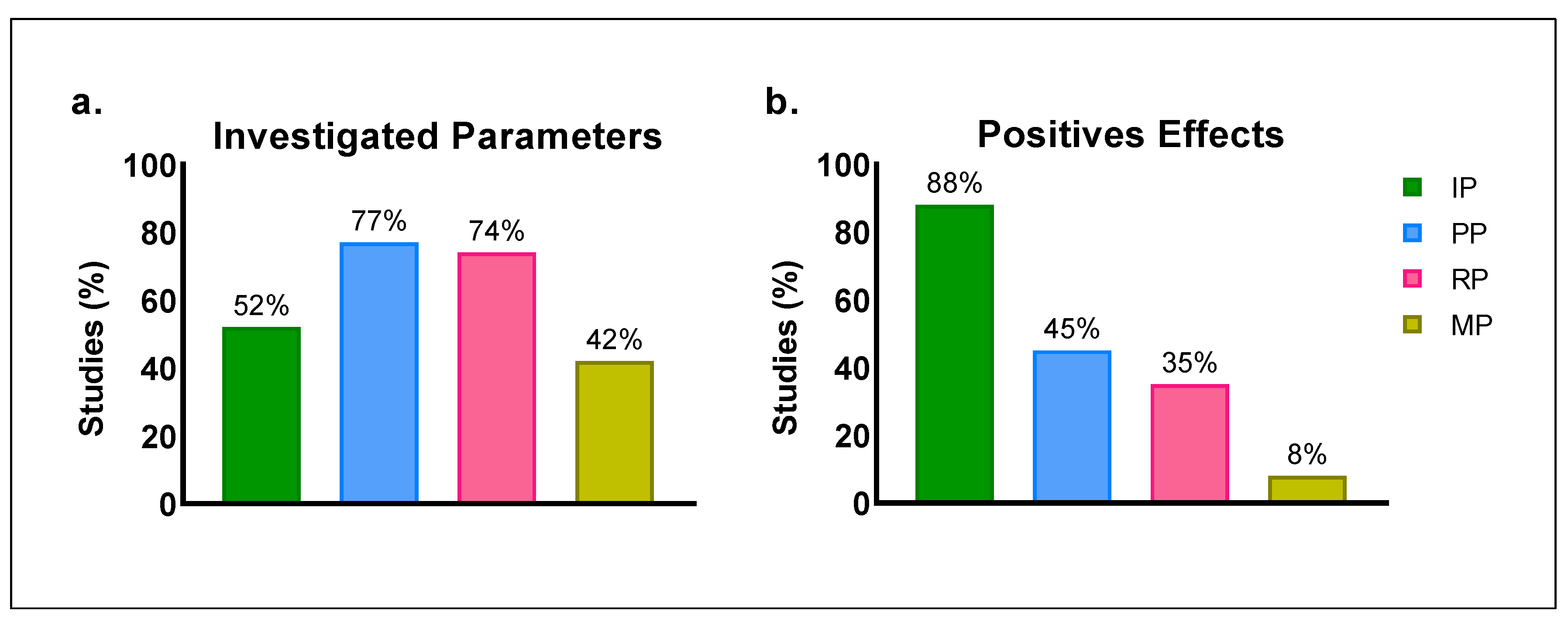
This study aimed to systematically review the literature to examine the effects of inspiratory-muscle warm-up (IMW) on the inspiratory, metabolic, respiratory and performance parameters of a main exercise performed by athletes and healthy and active individuals. Methods: This systematic review included randomized studies in English based on the criteria of the PICOS model. The exclusion criteria adopted were studies that applied inspiratory exercise to: i. promote long-term adaptations through inspiratory training (chronic responses); ii. obtain acute responses to inspiratory load (overload) during and in breaks from physical effort and in an inspiratory-exercise session (acute training effect); iii. evaluate the effects of IMW on participants with cardiorespiratory and/or metabolic disease. Data Sources: PubMed, Embase, MedLine, Scopus, SPORTDiscus and Google Scholar (until 17 January 2023). Results: Thirty-one studies were selected. The performance and respiratory parameters were the most investigated (77% and 74%, respectively). Positive effects of IMW were reported by 88% of the studies that investigated inspiratory parameters and 45% of those that evaluated performance parameters. Conclusions: The analyzed protocols mainly had positive effects on the inspiratory and performance parameters of the physical exercises. These positive effects of IMW are possibly associated with the contractile and biochemical properties of inspiratory muscles.
1. Introduction
The respiratory muscles are responsible for the flow of air into (inspiration) and out of (expiration) the lungs, while respiratory demand is associated with the metabolic rate to ensure homeostasis. In intense exercise, the cardiorespiratory and neuromuscular systems undergo several modulations to sustain the effort. Alveolar ventilation must increase proportionally to the consumption of oxygen (O2) and the production of carbon dioxide (CO2), consequently improving cardiac output. Furthermore, the higher respiratory rate intensifies the work of the respiratory muscles, requiring adjustments to the breathing pattern and increasing muscle recruitment so as to reduce the metabolic cost of breathing. As a consequence, these adjustments increase the demand for blood flow and O2 transport to these muscles during effort [1,2]. Due to these physiological challenges, the inspiratory muscles in particular become more intolerant of exercise when the energy demand exceeds the supply [2] since, in fatigue, these muscles consume 10–15% of the total O2 [3] and the blood flow corresponds to up to 16% of the cardiac output [4]. Of the muscles activated during inspiration, the main groups are the diaphragm and the external and parasternal intercostals, while the accessory muscles include the sternocleidomastoid, the scalene, the pectoralis major and minor, the serratus anterior and the iliocostalis cervicis [5,6,7], which perform functions related to inspiratory and motor tasks concomitantly. They are more prone to fatigue during main tasks of greater intensity.
In addition to being a type of training used in clinical practice, inspiratory exercise has become an interesting strategy in the sports field, given the importance of the participation of the respiratory muscles in high-intensity efforts [8]. Clinical trials have shown that this resource can reduce blood pressure, since breathing is a modulator of the autonomic nervous system and the baroreflex [9], as well as, helping in the prevention and rehabilitation of diseases that cause respiratory damage, such as dyspnea and exercise intolerance [10,11,12]. In athletes and active and healthy individuals, inspiratory exercise has brought benefits when used chronically in association with long-term training [8,13,14,15,16], or applied acutely to obtain exercise responses with inspiratory overload [17], in a single inspiratory training session [18] or to assist in the recovery from high-intensity efforts [19]. Moreover, inspiratory exercise has been widely used as a preparatory activity for physical exercise. This is known as the inspiratory-muscle warm-up (IMW) [20,21,22,23,24], which is the particular focus of this systematic review. The application of specific previous activities can provide positive effects for physical exercises by controlling the intensity and duration of previous stimuli, as well as recovery between tasks [25]. The exercise performed in the warm-up before a more intense effort can be a resource for post-activation potentiation, whose effects can improve physical performance [26,27].
The first investigation of IMW was based on the hypothesis that a specific warm-up would affect the global strength of this musculature [28]. After confirming this hypothesis, several studies sought to assess the effects of this intervention not only on the overall strength of the inspiratory muscles [29,30,31,32,33], but also on sports performance, especially in high-intensity efforts, taking into account metabolic and respiratory parameters [20,21,22,23,24,29,31,34,35,36,37,38].
Although the literature has reported the positive effects of IMW on athletes and healthy and active individuals while performing several tasks, there are still gaps regarding the protocols to be applied in relation to the prescription of inspiratory load, as well as the characteristics of the warm-up protocol, such as the number of repetitions (breaths), pauses between efforts and the equipment used as the inspiratory exerciser. Since IMW has been used as a strategy to improve performance, it seems pertinent to discuss the subject in a systematic review, providing robust information both for its proper prescription and for the indication of new paths for future investigations. Therefore, this study aimed to systematically review the literature in order to examine the effects of inspiratory-muscle warm-up on the inspiratory, metabolic, respiratory and performance parameters of a physical exercise performed by athletes and healthy and active individuals, taking into consideration the protocols applied as well as the equipment used as the inspiratory exerciser.
2. Methods
This systematic review was conducted according to the methodological guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [39]. This systematic review was not recorded.
2.1. Eligibility Criteria
This review addressed randomized studies that applied inspiratory exercise as a muscle -warm-up strategy with the aim of improving the performance of subsequent activity. Only English -language studies were considered for the analysis. The exclusion criteria adopted were associated with the types of studies published in the form of an editorials, letters to the editor, comments, reviews, abstracts, lectures or opinion articles. Regarding the types of intervention, we excluded studies that applied inspiratory exercise to: i. promotes long-term adaptations through inspiratory training (chronic responses); ii. obtain acute responses to inspiratory load (overload) during and in breaks from physical effort and in an inspiratory exercise session (acute training effect); and iii. investigate its effects on participants with cardiorespiratory and/or metabolic disease. The definition of the inclusion criteria was based on the PICOS structured-questions model (P—Population; I—Intervention; C—Comparison; O—Outcome; S—Study design; Table 1). Only studies conducted with athletes and healthy and active individuals aged over 18 years without any motor limitations were considered. No restriction was adopted as to the sex of the participants.

Table 1.
Inclusion criteria based on the PICOS method.
2.2. Data Sources and Search Strategy
The comprehensive literature search was performed on the following electronic databases PubMed, Embase, MedLine, Scopus and SPORTDiscus and Google Scholar (additional search). Database queries were restricted to the period between 1999 and 17 January 2023. On all electronic databases, the following combinations of terms were applied: “inspiratory” OR “respiratory” AND “warm-up” OR “pre-activation” AND “exercise” OR “performance.”
2.3. Quality Assessment
The PEDro (Physiotherapy Evidence Database) scale was used to assess the methodological quality of the studies included in this review [40]. This scale considers 11 items: 1. eligibility criteria specified; 2. random allocation; 3. concealed allocation; 4. groups similar at baseline; 5. subject blinding; 6. therapist blinding; 7. assessor blinding; 8. dropout rate lower than 15%; 9. intention-to-treat analysis; 10. between-group statistical comparisons; 11. point measures and variability data. The classifications of the methodological quality of the studies were determined as poor (scores ≤3), fair (scores 4–5), good (scores 6–8) and excellent (scores 9–10). The quality assessment was not applied as an inclusion criterion.
2.4. Risk of Bias Assessment
The risk of bias was assessed according to the Cochrane Collaboration guidelines (Review Manager software, version 5.4.1, Copenhagen, DK. The bias risk was analyzed in the selection, performance, attrition and reporting domains. The judgement was classified as high, low, or unclear risk of bias [41]. The risk-of-bias assessment was not applied as an inclusion criterion.
2.5. Data Extraction and Management
The literature search, screening and selection of articles were carried out by two authors independently (CC and ABM). After consulting the databases, the screening was conducted considering the title, abstract and keywords according to the eligibility criteria. Duplicate references were removed. At a different point in the study, the same authors analyzed the texts in full. In cases of divergence, decisions were taken by a third author (FBMG). The two authors used a customized data-extraction form, taking into account the criteria established based on the PICOS model. This form extracted information about the participants (characteristics, sex, age and sample size), IMW protocols (inspiratory load, number of sets and repetitions, interval between sets and between intervention and physical exercise), performance parameters analyzed and results obtained (IMW effects). Regarding the effects of the interventions, the parameters investigated were: inspiratory (variables related to inspiratory measurements), sports performance (variables provided by the tests to determine the sports performance), respiratory (physiological and psychophysiological variables related to ventilatory measurements) and metabolic (variables associated with the metabolic products of the exercise).
3. Results
3.1. Study Selection
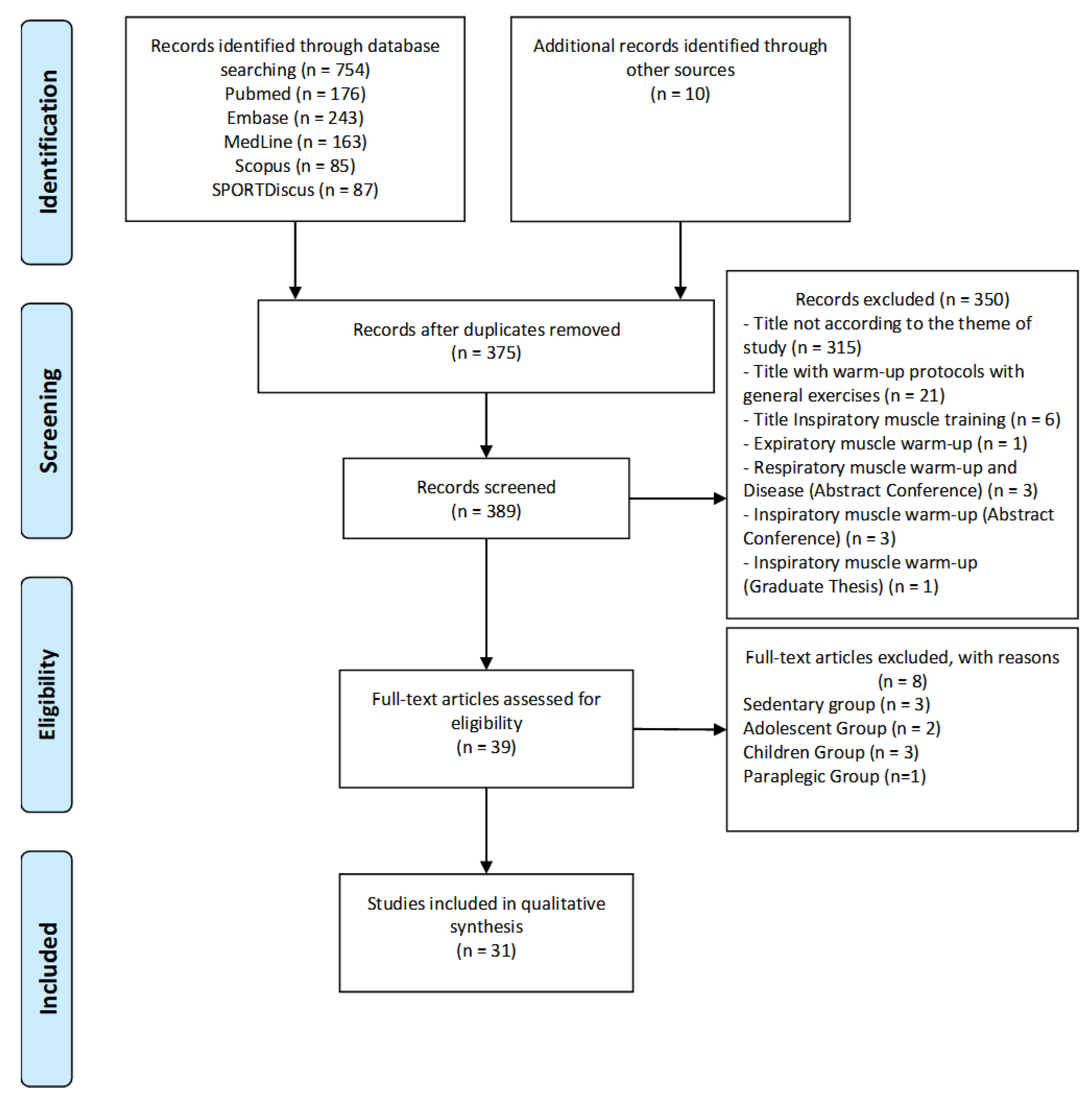
Initially, a total of 764 studies were selected, of which 176 were from PubMed, 243 were from Embase, 163 were from MedLine, 85 were from Scopus, 87 were from SPORTDiscus and 10 were from Google Scholar (additional database). Next, 375 duplicates were excluded, resulting in 389 studies. Of these, we excluded three-hundred and fifty titles for not being in accordance with the study topic, twenty-one titles with warm-up protocols applied to general exercises, six titles with inspiratory-muscle training, one title with expiratory-muscle warm-up, three titles with respiratory-muscle warm-up associated with disease (conference abstract), three titles with IMW (conference abstract) and one study published as a graduation thesis. From the remaining thirty-nine studies, we extracted three that were applied to sedentary groups, two that were applied to groups of adolescents (aged below 18 years), three that were applied to a group of children and one that was applied to a group of paraplegics. Finally, a total of 31 studies were included in this systematic review (Figure 1).
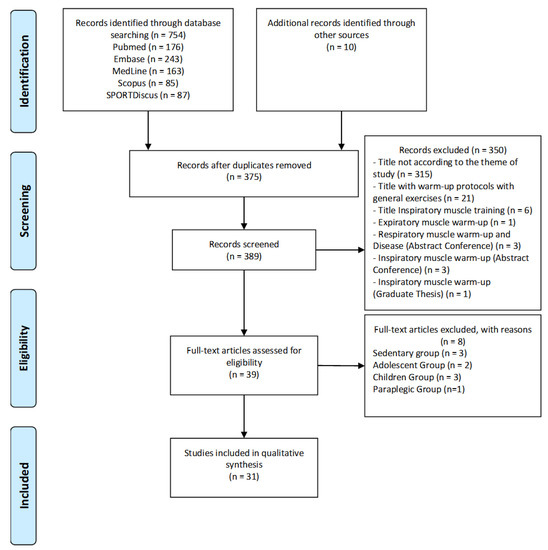
Figure 1.
Flow diagram of the study’s screening process.
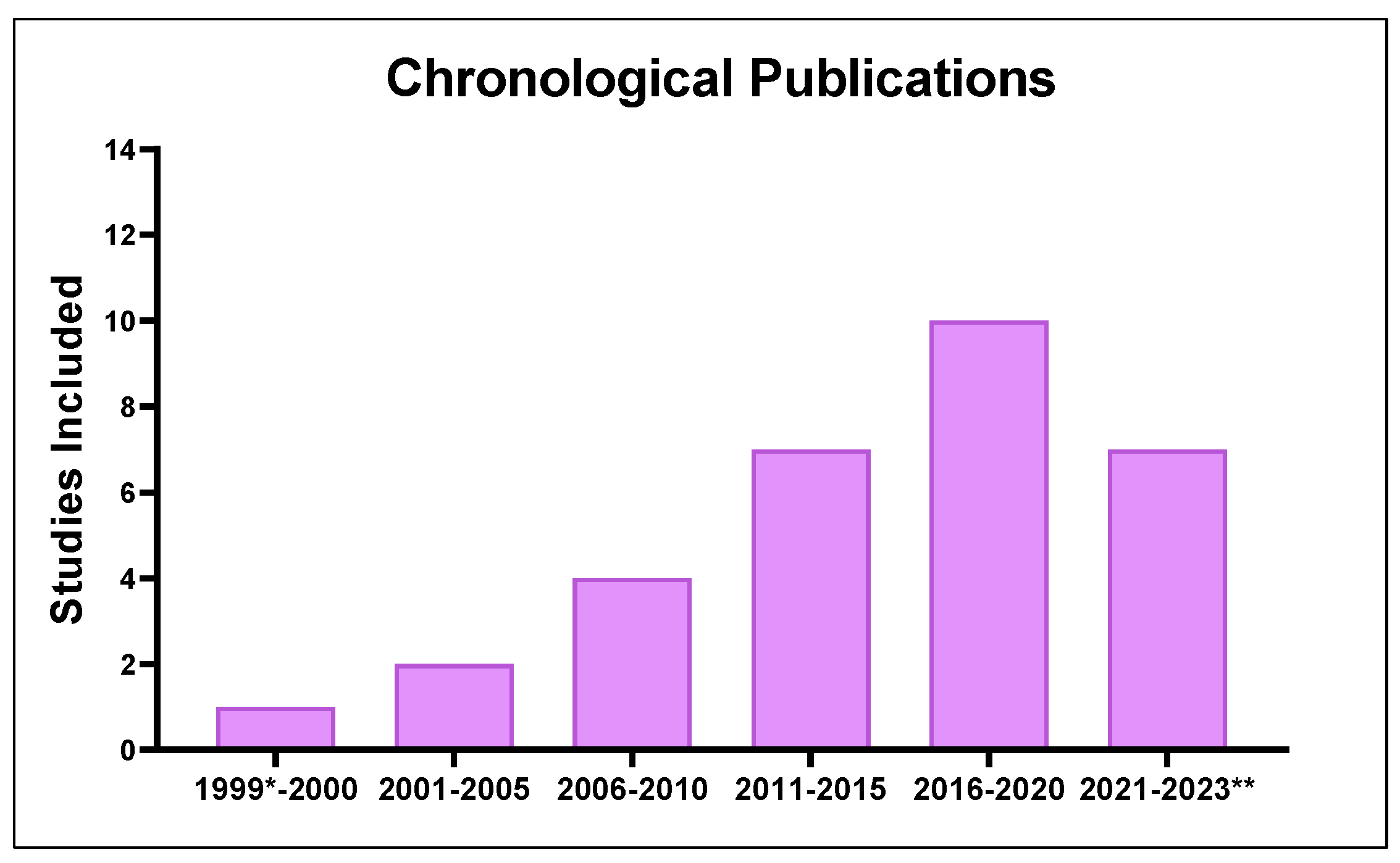
Among the selected studies, the chronological analysis of the publications (Figure 2) showed an exponential increase in investigations related to IMW from 1999 (the first study on the subject) to 2020. It should be noted that between 2021 and 2022, 7 studies were published prior to this review (17 January 2023).
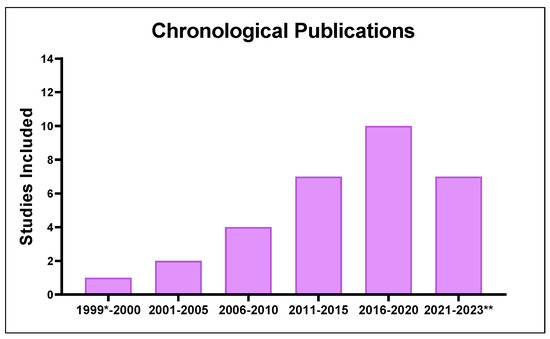
Figure 2.
Distribution of published studies on inspiratory muscle warm-up applied to athletes and healthy and active individuals (period analyzed: 1999 to 2023). * First publication. ** Reviewed until 17 January 2023.
3.2. Quality Assessment
Table 2 presents the assessment of the methodological quality of the studies. According to the PEDro scale, 77% of the studies had good methodological quality, while the others were classified as being of excellent quality. However, most of the studies did not score on items related to randomization and blinding.

Table 2.
Assessment of the methodological quality of studies (PEDro Scale).
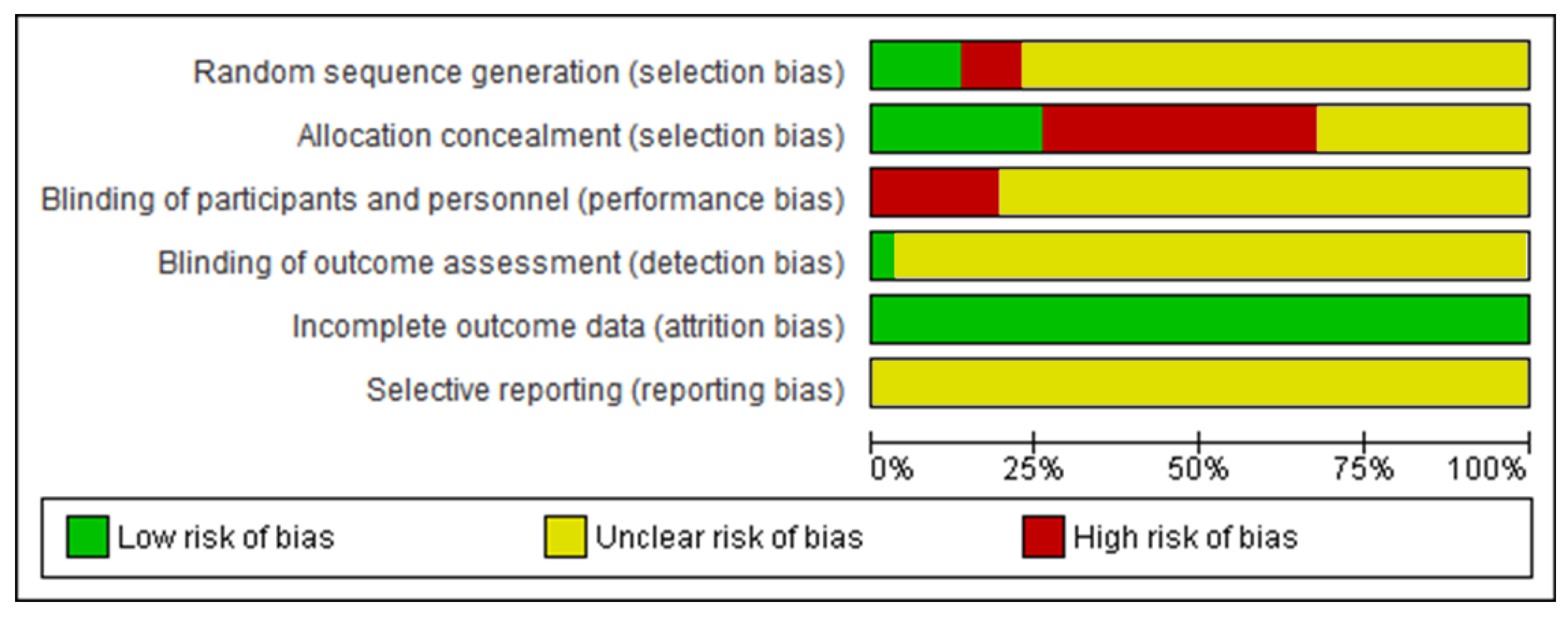
3.3. Risk-of-Bias Assessment
Figure 3 demonstrates the risk-of-bias analysis of the included studies on a percentage scale. In general, most of the studies omitted methodological information that indicated an unclear risk of bias for all domains, except for incomplete outcome data. This domain has a low risk of bias for all studies because it is used to investigate acute interventions, facilitating data collection. Some of the investigations showed a high risk of bias in domains related to randomization and blinding. Thus, the risk-of-bias analysis raised concerns, since the studies did not explicitly present methodological information.
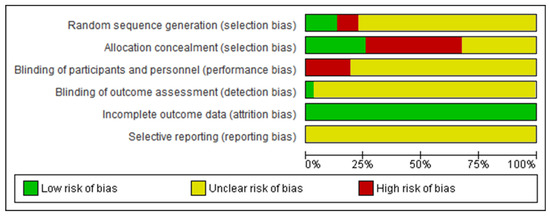
Figure 3.
Percentage risk of bias of the studies included in the review.
3.4. Study Characteristics
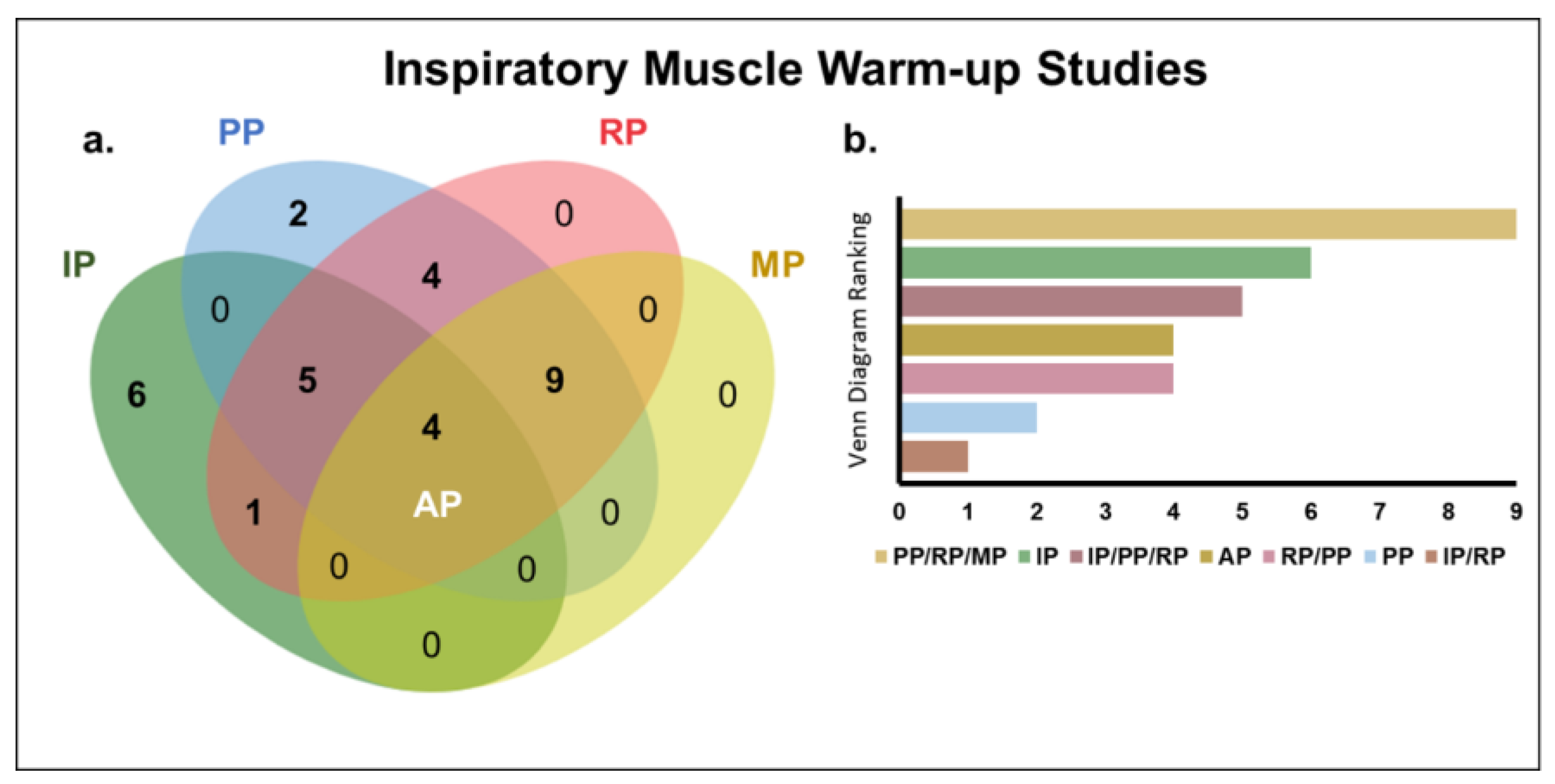
Table 3 presents the characteristics and effects of the IMW protocols applied prior to a physical exercise. The IMW protocols were characterized by the measure used to determine inspiratory load, the prescription of the volume and intensity of inspiratory exercises, the pause between efforts, the type of intervention and the equipment used. The effects of IMW on inspiratory, performance, respiratory and metabolic parameters were also evaluated. A Venn diagram (Figure 4a) was used to quantify the studies in relation to the parameters investigated. According to Figure 4b, of the thirty-one studies considered in this review, nine simultaneously investigated the effects of the intervention on the performance, respiratory and metabolic parameters, six analyzed only the inspiratory parameters, five addressed the inspiratory, performance and respiratory parameters in the same investigation, four quantified all the parameters investigated, four evaluated the effects of the intervention only on the performance and respiratory parameters, two considered only the performance parameters and one analyzed the inspiratory and respiratory parameters in the same investigation.

Table 3.
Description of the IMW protocols. a POWERbreathe®. b PowerLung®. c Flow-restriction device. d Not informed.
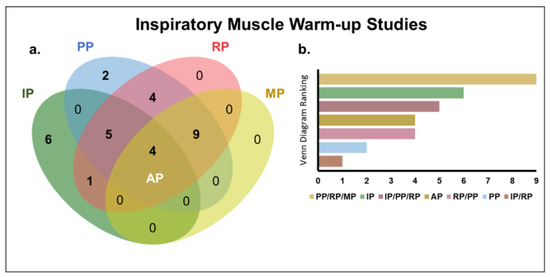
Figure 4.
Inspiratory-muscle-warm-up studies. (a) Venn diagram [57] of the intersection of studies on the effects of inspiratory-muscle warm-up in relation to the investigated parameters. (b) Ranking of the intersections of the Venn diagram (number of studies evaluating the investigated parameters). All parameters (AP); inspiratory parameters (IP); performance parameters (PP); respiratory parameters (RP); and metabolic parameters (MP).
Figure 5 shows that the performance and respiratory parameters were the most frequently investigated (77% and 74%, respectively). The positive effects of IMW were reported 88% of the studies that evaluated inspiratory parameters, followed by 45% of those that investigated performance parameters (Figure 5b).
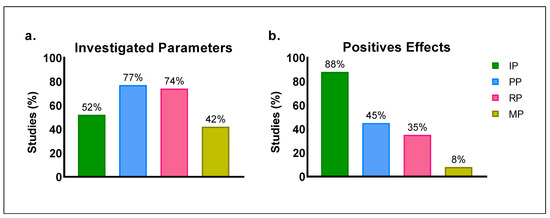
Figure 5.
Percentage of studies on the effects of inspiratory-muscle warm-up on inspiratory parameters (IP); performance parameters (PP); respiratory parameters (RP); and metabolic parameters (MP). (a) Investigated parameters. (b) Positive effects.
4. Discussion
This study investigated the effects of inspiratory exercise applied as a muscle-warm-up strategy prior to physical exercise performed by athletes and healthy and active individuals. According to our analysis, the most frequently investigated factors used to examine the effects of IMW were performance (77%) and respiratory (74%) parameters. The positive effects of IMW were reported in 88% of the studies that evaluated inspiratory parameters and 45% of those that investigated performance parameters. Of the selected studies, the majority concurrently analyzed the effects of IMW on performance, respiratory and metabolic parameters, followed by those that investigated the effects only on inspiratory parameters. Furthermore, most of the investigations that found positive effects of this intervention applied the traditional protocol, consisting of two sets of thirty deep breaths performed using POWERbreathe® (IMT Technologies Ltd., Birmingham, UK), at an inspiratory load of 40% MIP. The assessment of methodological quality and risk of bias was not used as an inclusion criterion. Therefore, all the studies on the subject were analyzed in this review.
Most of the studies covered in this systematic review used maximal inspiratory pressure (MIP) measures to determine effort intensity during IMW, given that these measures are a reference in the assessment of global inspiratory-muscle strength [20,21,22,23,28,29,30,31,32,33,34,35,36,37,38,42,43,44,46,47,48,49,50,51,52,53,54,55], enabling correct individual measurement and guidance on the inspiratory intervention load. The inspiratory-muscle-strength levels were obtained by measuring the maximal inspiratory pressures through the airways or diaphragm [58]. The pressure measurement followed Laplace’s law, which refers to the tension radius of the curvature ratio, which, in this case, was the curvature of the diaphragm dome [59]. In relation to diaphragm tension in particular, the measure used was trans-diaphragmatic pressure (Pdi), which corresponds to the difference between the gastric and esophageal pressures resulting from the passage of catheters via the nasal route to the distal esophagus and stomach [60]. Although this method is the most accurate for assessing the pressure exerted by the diaphragm [61], it is invasive and restricted, as it provides the pressure index of only one inspiratory muscle [60]. Thus, to determine pressure through the airways [56], the MIP is the most commonly used measure in clinical practice [60,62] and in inspiratory-muscle training, since it is a non-invasive method [8,13,14,15,16]. The measure that represents global inspiratory-muscle strength [60,62,63], is obtained using a manovacuometer, by the Mueller maneuver performed against an occluded valve that requires maximum contraction from residual volume to total lung capacity, eliciting maximal isometric effort from the inspiratory muscles [59,62].
Alternatively, more recent studies adopted the use of the S-index (strength-index) measure, which dynamically assesses global inspiratory-muscle strength through the airflow generated in an open system during an inspiratory maneuver [62,64,65]. It should be noted that even though this measure does not represent the MIP, it has proved to be a valid option, capable of providing the necessary measures for the prescription of inspiratory-muscle training [62,64]. In addition, the S-index can be advantageous due to its easy applicability, since the device used to obtain this measure (POWERbreathe®, K-Series) can also be employed to perform inspiratory exercises [62]. Although this measure is becoming increasingly popular [62], only the studies by Barnes and Ludge [24] and Silapabanleng et al. [54] adopted it for prescribing inspiratory exercise. While the former [24] applied the protocol before the S-index and 3200-m running tests, the latter [56] used IMW based on S-index prior to a 3-min all-out test on a cycle ergometer.
Regarding the IMW protocol, especially in relation to volume (the number of sets and repetitions) and intensity (the percentage of maximal inspiratory pressure), most studies applied the traditional protocol defined by Volianitis et al. [28], with two sets of thirty breaths at 40% MIP. The use of 40% MIP in the traditional protocol can be justified by the fact that this inspiratory load represents the highest intensity at which inspiratory-muscle fatigue is not induced [44,66]. An IMW protocol with an inspiratory load corresponding to 15% MIP was adopted in some investigations as a placebo, since it did not differ from the protocol without IMW intervention (control) [20,21,22,23,43,48,50,52]. However, other studies that applied two sets of fifteen breaths at 15% MIP showed positive changes, indicating that this inspiratory load can be used to prepare athletes for subsequent high-intensity efforts [36,38].
Of the studies that applied the traditional protocol (2 × 30), most of reported positive effects on MIP measures [28,29,31,32,33,42,44,46,49], in dynamic inspiratory function estimated using different inspiratory loads [20,43], and in improved lung-function parameters [46]. Barnes and Ludge [24] observed an increased S-index in an alternative protocol (1 × 30 breaths at 50% S-index). Regarding the performance parameters, the studies that adopted the traditional protocol found positive effects of IMW on rowing [29,55], badminton [20], intermittent running [31], swimming [22], anaerobic fitness test [23,37,38], maximal running (sprints) [53] and hockey [54]. In these studies, the performance improvement ranged between 2.1% and 34.4% when IMW was applied. However, other investigations that also assessed high-intensity efforts with the intervention of the traditional IMW protocol showed no changes in performance parameters [21,32,34,35,43,47,48,49,52,55]. Although all of these studies applied the same volume and intensity, with intervals between sets of 30 s up to 2 min [23,31,32,34,35,50,52], that is, similar stimuli, the different results found may have been associated with the time between the IMW stimulus and the physical exercise. While Tong and Fu [43] started the physical exercise immediately after the warm-up integrated with the IMW, Lomax et al. [31] waited for 3 min. The other studies did not provide this information in their experimental designs, which may have affected their understanding of the responses to the stimuli caused by the IMW. Other interventions that can provide the post-activation potentiation described in the literature reported short-duration effects of around a few minutes on muscle actions [67]. In this reasoning, it is safe to say that the duration of the IMW’s effects on high-intensity efforts is still unknown; therefore, the time taken to start the physical exercise can affect its effect on performance. Hawkes et al. [44] observed that the positive effects of the traditional protocol of IMW on MIP lost their effectiveness 15 min after the intervention. Moreover, unlike the effort caused by the MIP assessment, the high-intensity stimuli characteristic of sports practice may result in inspiratory-muscle fatigue [1,2], which can affect the duration of the IMW effects.
Other studies sought to assess IMW protocols with different volumes and intensities of inspiratory exercise. Arend et al. [33] assessed the effects of IMW on MIP by applying four different protocols. According to the authors, a protocol with a more intense inspiratory load (60% MIP) and a lower number of breaths (12 inspirations) led to positive effects on global inspiratory-muscle strength. Marostegan et al. [38] also tested IMW at 60% MIP (two sets with fifteen breaths) and observed an increase in mechanical parameters in 30-s all-out tethered running. Merola et al. [51] also applied a protocol at an inspiratory load of 60% MIP (two sets of fifteen breaths) as a preliminary activity to a specific judo test. However, this study did not show changes in performance or respiratory parameters.
It is worth mentioning that the most recent studies, such as those developed by Cirino et al. [36], who evaluated a judo match, and Manchado-Gobatto et al. [37], who evaluated performance in 30-s all-out tethered running, brought innovations to the analysis of the effects of inspiratory-muscle warm-up, demonstrating that the complex-networks model allows a more integrative analysis and highlighting the involvement of physiological parameters that are important for performance.
Regarding the type of equipment used as an inspiratory exerciser in the IMW included in the studies, Thurston et al. [45] used one that promotes inspiratory overload by restricting airflow through holes with diameters between 3 and 13 mm. Since the individualized intensity was not determined, this study found no changes in performance, metabolic or respiratory parameters. Although this equipment is low-cost and easy to apply, it has been used on a smaller scale due to the difficulty in controlling the inspiratory load, as it does not have a mechanism to regulate load during breathing [8]. The study by Lomax et al. [31] was based both on the MIP measure used to define the inspiratory load and on the use of PowerLung® (Sports, USA) to control the restriction of air flow through valves and provided the possibility of acting in the inspiratory and expiratory phases [8,68]. Nonetheless, McConnell and Romer [68] do not recommend the use of this equipment in the expiration phase, as the addition of an expiratory load may increase intrathoracic pressure, consequently increasing the potential risks during effort. It is important to highlight that Lomax et al. [31] observed positive effects of IMW both on sports-performance parameters and on MIP measures. The other studies also prescribed inspiratory exercise based on individualized MIP using POWERbreathe® (IMT Technologies Ltd., Birmingham, UK), a device that acts only in the inspiratory phase but has a regulation mechanism, involving a valve that is controlled electronically, which makes it able to maintain load intensity during inspiration [69].
The effects of IMW on MIP and sports-performance parameters [20,28,30,31,32,33,36,43,46] may be associated with the neural control of the inspiratory muscles, since this musculature exerts ventilatory and postural demands [70,71]. The IMW can help improve intra and intramuscular coordination [20,28,31], as the mechanical efficiency of these muscles requires coordinated muscle action [72], determined by the contractile and fatigue properties of the recruited motor units [73].
With a specific emphasis on metabolic and respiratory aspects, some investigations did not report positive effects on parameters related to responses after intense efforts [20,21,22,24,29,32,34,36,55], except for tissue-oxygenation rate in active muscles [21], respiratory rate [35] and dyspnea perception [20,24,43]. These results may be related to inspiratory-muscle fatigue, as previously discussed [74], since high-intensity efforts increase metabolites close to phrenic nerve endings, sensitizing type III and type IV afferent fibers that activate the metaboreflex [75]. This stimulates adrenergic vasoconstriction, redistributing blood flow from active to respiratory muscles [76]. Cheng et al. [21] suggested that the application of the traditional IMW protocol in submaximal exercise performed on a cycle ergometer may have delayed the metaboreflex, mitigating the drop in oxygen saturation. However, this positive effect was not associated with an improved cycling performance [21]. Furthermore, regarding submaximal exercise, Arend et al. [35] found that the effect of IMW at 40% MIP in rowers increased the respiratory rate during effort. The authors did not consider it a negative sign, but rather an opportunity to increase ventilation without causing dyspnea [35]. With respect to the decrease in dyspnea [20,24,43], which can be considered a limiting factor in maintaining effort, it was verified that the positive effects of IMW on high-intensity efforts helped improve performance [43]. It can therefore be concluded from the results that IMW facilitates chest stabilization, improving the mechanical efficiency of ventilation and reducing the sensation of dyspnea [77,78,79].
In our review, the assessment of the methodological quality and risk of bias of the studies indicated strengths and limitations that must be taken into account. The methodological quality of the studies was classified as good and excellent, according to the PEDro scale. This strengthens the description of the characteristics of the protocols and the possible applications of inspiratory exercises for enhancing the subsequent activity. However, most of the studies did not score items related to the randomization-and-blinding process (PEDro Scale). The main concerns raised by the risk-of-bias analysis reflect this judgment. It is noteworthy that this is the first exploratory review on IMW to select all the studies on the subject in order to indicate a direction for future investigations with more methodological details about inspiratory-muscle-warm-up effects.
5. Conclusions
Considering the above, the traditional IMW protocol (two sets of thirty inspirations at 40% MIP) was the most frequently applied to athletes and healthy and active individuals. According to the IMW protocols analyzed in this review, there was an improvement mainly in the inspiratory parameters related to MIP (4.0–21.2%) and in the performance of specific tasks (2.1–34.4%). Although the application of other protocols with control over the number of repetitions, inspiratory load and type of intervention also showed favorable effects on the improvement of physical exercise, further investigation is still required. In conclusion, the positive effects of IMW are associated with the efficiency of inspiratory muscles, possibly due to the contractile and biochemical properties of motor units and muscle fibers. We consider that the use of IMW can be a practical and simple additional resource to improve performance in high-intensity physical exercise, taking into account its individualized prescription.
Author Contributions
C.C., A.B.M. and F.B.M.-G. contributed to the proposal of ideas, conception and design of the work, and wrote the main manuscript text. C.C. and F.B.M.-G. prepared the figures and tables. C.C. and A.B.M. contributed to the development of the search strategy and conducted the systematic search. C.C. and A.B.M. performed the data acquisition. C.C., A.B.M., C.A.G. and F.B.M.-G. performed the data analysis. All authors assisted in the interpretation. C.S.H., M.A.M., C.A.G. and F.B.M.-G. provided critical intellectual input to the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Council for Scientific and Technological Development (CNPq) under grant nos. 307718/2018-2, 308117/2018-2 and 409521/2021-3 and the São Paulo Research Foundation (FAPESP) under grants nos. 2018/05821-6, 2019/20894-2 and 2020/11946-6. Furthermore, this study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES), finance code 001.
Acknowledgments
The authors thank Espaço da Escrita-Pró-Reitoria de Pesquisa—UNICAMP—for the language services provided and Mariana Devito Castro Avansi (technical translator and proofreader) for the revision of the English language.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article.
References
- Forster, H.V.; Haouzi, P.; Dempsey, J.A. Control of Breathing During Exercise. Compr. Physiol. 2012, 2, 743–777. [Google Scholar] [CrossRef]
- Welch, J.F.; Kipp, S.; Sheel, A.W. Respiratory muscles during exercise: Mechanics, energetics, and fatigue. Curr. Opin. Physiol. 2019, 10, 102–109. [Google Scholar] [CrossRef]
- Aaron, E.A.; Seow, K.C.; Johnson, B.D.; Dempsey, J.A. Oxygen cost of exercise hyperpnea: Implications for performance. J. Appl. Physiol. 1992, 72, 1818–1825. [Google Scholar] [CrossRef]
- Harms, C.A.; Wetter, T.J.; McClaran, S.R.; Pegelow, D.F.; Nickele, G.A.; Nelson, W.B.; Hanson, P.; Dempsey, J.A. Effects of respiratory muscle work on cardiac output and its distribution during maximal exercise. J. Appl. Physiol. 1998, 85, 609–618. [Google Scholar] [CrossRef]
- Ratnovsky, A.; Elad, D.; Halpern, P. Mechanics of respiratory muscles. Respir. Physiol. Neurobiol. 2008, 163, 82–89. [Google Scholar] [CrossRef]
- Hudson, A.L.; Butler, J.E.; Gandevia, S.C.; De Troyer, A. Interplay Between the Inspiratory and Postural Functions of the Human Parasternal Intercostal Muscles. J. Neurophysiol. 2010, 103, 1622–1629. [Google Scholar] [CrossRef]
- Saillant, N.N. Chest Wall Anatomy. In Rib Fracture Management; Moya, M., Mayberry, J., Eds.; Springer: Cham, Switzerland, 2018; pp. 25–33. [Google Scholar]
- Lorca-Santiago, J.; Jiménez, S.L.; Pareja-Galeano, H.; Lorenzo, A. Inspiratory Muscle Training in Intermittent Sports Modalities: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4448. [Google Scholar] [CrossRef]
- Silva, C.D.; Abreu, R.M.; Rehder-Santos, P.; De Noronha, M.; Catai, A.M. Can respiratory muscle training change the blood pressure levels in hypertension? A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2021, 31, 1384–1394. [Google Scholar] [CrossRef]
- Newall, C.; Stockley, R.A.; Hill, S.L. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax 2005, 60, 943–948. [Google Scholar] [CrossRef]
- Dall’Ago, P.; Chiappa, G.R.S.; Guths, H.; Stein, R.; Ribeiro, J.P. Inspiratory Muscle Training in Patients With Heart Failure and Inspiratory Muscle Weakness: A Randomized Trial. J. Am. Coll. Cardiol. 2006, 47, 757–763. [Google Scholar] [CrossRef]
- Palermo, A.E.; Cahalin, L.P.; Nash, M.S. A case for inspiratory muscle training in SCI: Potential role as a preventative tool in infectious respiratory diseases like COVID-19. Spinal Cord Ser. Cases 2020, 6, 87. [Google Scholar] [CrossRef]
- Witt, J.D.; Guenette, J.A.; Rupert, J.L.; McKenzie, D.C.; Sheel, A.W. Inspiratory muscle training attenuates the human respiratory muscle metaboreflex. J. Physiol. 2007, 584, 1019–1028. [Google Scholar] [CrossRef]
- Klusiewicz, A.; Borkowski, L.; Zdanowicz, R.; Boros, P.; Wesołowski, S. The inspiratory muscle training in elite rowers. J. Sports Med. Phys. Fit. 2008, 48, 279–284. [Google Scholar]
- Tong, T.K.; Fu, F.H.; Chung, P.K.; Eston, R.; Lu, K.; Quach, B.; Nie, J.; So, R. The effect of inspiratory muscle training on high-intensity, intermittent running performance to exhaustion. Appl. Physiol. Nutr. Metab. 2008, 33, 671–681. [Google Scholar] [CrossRef]
- Karsten, M.; Ribeiro, G.S.; Esquivel, M.S.; Matte, D.L. The effects of inspiratory muscle training with linear workload devices on the sports performance and cardiopulmonary function of athletes: A systematic review and meta-analysis. Phys. Ther. Sport 2018, 34, 92–104. [Google Scholar] [CrossRef]
- Caruso, F.R.; Archiza, B.; Andaku, D.K.; Trimer, R.; Bonjorno-Junior, J.C.; de Oliveira, C.R.; Libardi, C.A.; Phillips, S.A.; Arena, R.; Mendes, R.G.; et al. Effects of acute inspiratory loading during treadmill running on cerebral, locomotor and respiratory muscle oxygenation in women soccer players. Respir. Physiol. Neurobiol. 2020, 281, 103488. [Google Scholar] [CrossRef]
- Tanriverdi, A.; Kahraman, B.O.; Ozsoy, I.; Ozpelit, E.; Savci, S. Acute effects of inspiratory muscle training at different intensities in healthy young people. Ir. J. Med. Sci. 2020, 190, 577–585. [Google Scholar] [CrossRef]
- Cheng, C.-F.; Hsu, W.-C.; Kuo, Y.-H.; Chen, T.-W. Acute effect of inspiratory resistive loading on sprint interval exercise performance in team-sport athletes. Respir. Physiol. Neurobiol. 2020, 282, 103531. [Google Scholar] [CrossRef]
- Lin, H.; Tong, T.K.; Huang, C.; Nie, J.; Lu, K.; Quach, B. Specific inspiratory muscle warm-up enhances badminton footwork performance. Appl. Physiol. Nutr. Metab. 2007, 32, 1082–1088. [Google Scholar] [CrossRef]
- Cheng, C.-F.; Tong, T.K.; Kuo, Y.-C.; Chen, P.-H.; Huang, H.-W.; Lee, C.-L. Inspiratory muscle warm-up attenuates muscle deoxygenation during cycling exercise in women athletes. Respir. Physiol. Neurobiol. 2013, 186, 296–302. [Google Scholar] [CrossRef]
- Wilson, E.; McKeever, T.; Lobb, C.; Sherriff, T.; Gupta, L.; Hearson, G.; Martin, N.; Lindley, M.; Shaw, D. Respiratory muscle specific warm-up and elite swimming performance. Br. J. Sports Med. 2014, 48, 789–791. [Google Scholar] [CrossRef]
- Özdal, M.; Bostanci, Ö.; Dağlioğlu, Ö.; Ağaoğlu, S.A.; Kabadayi, M. Effect of respiratory warm-up on anaerobic power. J. Phys. Ther. Sci. 2016, 28, 2097–2098. [Google Scholar] [CrossRef]
- Barnes, K.R.; Ludge, A.R. Inspiratory Muscle Warm-up Improves 3200-m Running Performance in Distance Runners. J. Strength Cond. Res. 2021, 35, 1739–1747. [Google Scholar] [CrossRef]
- Bishop, D. Warm up II: Performance Changes Following Active Warm Up and How to Structure the Warm Up. Sports Med. 2003, 33, 483–498. [Google Scholar] [CrossRef]
- Hamada, T.; Sale, D.G.; MacDougall, J.D.; Tarnopolsky, M.A. Postactivation potentiation, fiber type, and twitch contraction time in human knee extensor muscles. J. Appl. Physiol. 2000, 88, 2131–2137. [Google Scholar] [CrossRef]
- Dallas, G.; Mavvidis, A.; Kosmathaki, I.; Tsoumani, I. The post activation potentiation effect of two different conditioning stimuli on drop jump parameters on young female artistic gymnasts. Sci. Gymnastics J. 2019, 11, 103–113. [Google Scholar] [CrossRef]
- Volianitis, S.; McConnell, A.K.; Koutedakis, Y.; Jones, D.A. The Influence of Prior Activity Upon Inspiratory Muscle Strength in Rowers and Non-Rowers. Int. J. Sports Med. 1999, 20, 542–547. [Google Scholar] [CrossRef]
- Volianitis, S.; McConnell, A.; Koutedakis, Y.; Jones, D.A. Specific respiratory warm-up improves rowing performance and exertional dyspnea. Med. Sci. Sports Exerc. 2001, 33, 1189–1193. [Google Scholar] [CrossRef]
- Lomax, M.; McConnell, A. Influence of Prior Activity (Warm-Up) and Inspiratory Muscle Training upon Between- and Within-Day Reliability of Maximal Inspiratory Pressure Measurement. Respiration 2009, 78, 197–202. [Google Scholar] [CrossRef]
- Lomax, M.; Grant, I.; Corbett, J. Inspiratory muscle warm-up and inspiratory muscle training: Separate and combined effects on intermittent running to exhaustion. J. Sports Sci. 2011, 29, 563–569. [Google Scholar] [CrossRef]
- Ohya, T.; Hagiwara, M.; Suzuki, Y. Inspiratory muscle warm-up has no impact on performance or locomotor muscle oxygenation during high-intensity intermittent sprint cycling exercise. Springerplus 2015, 4, 556. [Google Scholar] [CrossRef]
- Arend, M.; Kivastik, J.; Mäestu, J. Maximal inspiratory pressure is influenced by intensity of the warm-up protocol. Respir. Physiol. Neurobiol. 2016, 230, 11–15. [Google Scholar] [CrossRef]
- Johnson, M.A.; Gregson, I.R.; Mills, D.E.; Gonzalez, J.T.; Sharpe, G.R. Inspiratory muscle warm-up does not improve cycling time-trial performance. Eur. J. Appl. Physiol. 2014, 114, 1821–1830. [Google Scholar] [CrossRef]
- Arend, M.; Mäestu, J.; Kivastik, J.; Rämson, R.; Jürimäe, J. Effect of Inspiratory Muscle Warm-up on Submaximal Rowing Performance. J. Strength Cond. Res. 2015, 29, 213–218. [Google Scholar] [CrossRef]
- Cirino, C.; Gobatto, C.A.; Pinto, A.S.; Torres, R.S.; Hartz, C.S.; Azevedo, P.H.S.M.; Moreno, M.A.; Manchado-Gobatto, F.B. Complex network model indicates a positive effect of inspiratory muscles pre-activation on performance parameters in a judo match. Sci. Rep. 2021, 11, 11148. [Google Scholar] [CrossRef]
- Manchado-Gobatto, F.B.; Torres, R.S.; Marostegan, A.B.; Rasteiro, F.M.; Hartz, C.S.; Moreno, M.A.; Pinto, A.S.; Gobatto, C.A. Complex Network Model Reveals the Impact of Inspiratory Muscle Pre-Activation on Interactions among Physiological Responses and Muscle Oxygenation during Running and Passive Recovery. Biology 2022, 11, 963. [Google Scholar] [CrossRef]
- Marostegan, A.B.; Gobatto, C.A.; Rasteiro, F.M.; Hartz, C.S.; Moreno, M.A.; Manchado-Gobatto, F.B. Effects of different inspiratory muscle warm-up loads on mechanical, physiological and muscle oxygenation responses during high-intensity running and recovery. Sci. Rep. 2022, 12, 11223. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G. Assessing risk of bias in included studies. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Chichester, UK, 2018. [Google Scholar]
- Volianitis, S.; McConnell, A.K.; Jones, D.A. Assessment of Maximum Inspiratory Pressure. Respiration 2001, 68, 22–27. [Google Scholar] [CrossRef]
- Tong, T.K.; Fu, F.H. Effect of specific inspiratory muscle warm-up on intense intermittent run to exhaustion. Eur. J. Appl. Physiol. 2006, 97, 673–680. [Google Scholar] [CrossRef]
- Hawkes, E.Z.; Nowicky, A.; McConnell, A. Diaphragm and intercostal surface EMG and muscle performance after acute inspiratory muscle loading. Respir. Physiol. Neurobiol. 2007, 155, 213–219. [Google Scholar] [CrossRef]
- Thurston, T.S.; Coburn, J.W.; Brown, L.E.; Bartolini, A.; Beaudette, T.L.; Karg, P.; McLeland, K.A.; Arevalo, J.A.; Judelson, D.A.; Galpin, A.J. Effects of Respiratory Muscle Warm-up on High-Intensity Exercise Performance. Sports 2015, 3, 312–324. [Google Scholar] [CrossRef]
- Özdal, M. Acute effects of inspiratory muscle warm-up on pulmonary function in healthy subjects. Respir. Physiol. Neurobiol. 2016, 227, 23–26. [Google Scholar] [CrossRef]
- Faghy, M.A.; Brown, P.I. Whole-body active warm-up and inspiratory muscle warm-up do not improve running performance when carrying thoracic loads. Appl. Physiol. Nutr. Metab. 2017, 42, 810–815. [Google Scholar] [CrossRef]
- Hartz, C.S.; Ferreira, C.R.; Moreno, M.A. Effects of the Application of an Inspiratory Muscular Warm-Up Protocol in the Physical Performance of Handball Athletes. J. Exerc. Physiol. 2017, 20, 12–22. [Google Scholar]
- Özdal, M.; Bostanci, Ö. Influence of inspiratory muscle warm-up on aerobic performance during incremental exercise. Isokinet. Exerc. Sci. 2018, 26, 167–173. [Google Scholar] [CrossRef]
- Richard, P.; Billaut, F. Combining Chronic Ischemic Preconditioning and Inspiratory Muscle Warm-Up to Enhance On-Ice Time-Trial Performance in Elite Speed Skaters. Front. Physiol. 2018, 9, 1036. [Google Scholar] [CrossRef]
- Merola, P.K.; Zaccani, W.A.; Faria, C.C.; Berton, D.C.; Verges, S.; Franchini, E. High load inspiratory muscle warm-up has no impact on Special Judo Fitness Test performance. Ido Mov. Cult. 2019, 19, 66–74. [Google Scholar] [CrossRef]
- Richard, P.; Billaut, F. Effects of inspiratory muscle warm-up on locomotor muscle oxygenation in elite speed skaters during 3000 m time trials. Eur. J. Appl. Physiol. 2018, 119, 191–200. [Google Scholar] [CrossRef]
- Tong, T.K.; Baker, J.S.; Zhang, H.; Kong, Z.; Nie, J. Effects of Specific Core Re-Warm-Ups on Core Function, Leg Perfusion and Second-Half Team Sport-Specific Sprint Performance: A Randomized Crossover Study. J. Sports Sci. Med. 2019, 18, 479–489. [Google Scholar]
- Avci, N.; Özdal, M.; Vural, M. Influence of inspiratory muscle warm-up exercise on field hockey drag-flick and shooting performance. Eur. J. Phys. Educ. Sport Sci. 2021, 6, 92–104. [Google Scholar] [CrossRef]
- Arend, M.; Kivastik, J.; Talts, J.; Mäestu, J. The Effect of Inspiratory Muscle Warm-Up on VO2 Kinetics during Submaximal Rowing. Sports 2021, 9, 42. [Google Scholar] [CrossRef]
- Silapabanleng, S.; Boonkobkaew, N.; Singthongyam, T.; Phangjaem, M.; Puengtanom, V.; Nakpanom, W.; Suwondit, P. Effect of Inspiratory Muscle Warm-Up on Short-Distance Cycling Performance. Sci. Technol. Asia 2021, 26, 221–228. [Google Scholar]
- Bardou, P.; Mariette, J.; Escudié, F.; Djemiel, C.; Klopp, C. jvenn: An interactive Venn diagram viewer. BMC Bioinf. 2014, 15, 293. [Google Scholar] [CrossRef]
- McCool, F.D.; Conomos, P.; Benditt, J.O.; Cohn, D.; Sherman, C.B.; Hoppin, F.G. Maximal inspiratory pressures and dimensions of the diaphragm. Am. J. Respir. Crit. Care Med. 1997, 155, 1329–1334. [Google Scholar] [CrossRef]
- Silva, P.E.; Chiappa, G.R.; Vieira, P.J.C.; Roncada, C. Avaliação da função muscular ventilatória. In PROFISIO Programa de Atualização em Fisioterapia Cardiovascular e Respiratória: Ciclo 2; Martins, J.A., Karsten, M., Dal Corso, S., Associação Brasileira de Fisioterapia Cardiorrespiratória e Fisioterapia em Terapia Intensiva, Eds.; Artmed Panamericana: Porto Alegre, BR, 2016; pp. 9–46. (In Portuguese) [Google Scholar]
- Caruso, P.; Albuquerque, A.L.P.; Santana, P.V.; Cardenas, L.Z.; Ferreira, J.G.; Prina, E.; Trevizan, P.F.; Pereira, M.C.; Iamonti, V.; Pletsch, R.; et al. Métodos diagnósticos para avaliação da força muscular inspiratória e expiratória. J. Bras. Pneumol. 2015, 41, 110–123. [Google Scholar] [CrossRef]
- De Troyer, A.; Estenne, M. Limitations of measurement of transdiaphragmatic pressure in detecting diaphragmatic weakness. Thorax 1981, 36, 169–174. [Google Scholar] [CrossRef]
- Areias, G.D.S.; Santiago, L.R.; Teixeira, D.S.; Reis, M.S. Concurrent Validity of the Static and Dynamic Measures of Inspiratory Muscle Strength: Comparison between Maximal Inspiratory Pressure and S-Index. Rev. Bras. Cir. Cardiovasc. 2020, 35, 459–464. [Google Scholar] [CrossRef]
- Neder, J.; Andreoni, S.; Lerario, M.; Nery, L. Reference values for lung function tests: II. Maximal respiratory pressures and voluntary ventilation. Braz. J. Med. Biol. Res. 1999, 32, 719–727. [Google Scholar] [CrossRef]
- Minahan, C.; Sheehan, B.; Doutreband, R.; Kirkwood, T.; Reeves, D.; Cross, T. Repeated-sprint cycling does not induce respiratory muscle fatigue in active adults: Measurements from the powerbreathe® inspiratory muscle trainer. J. Sports Sci. Med. 2015, 14, 233–238. [Google Scholar]
- Silva, P.E.; De Carvalho, K.L.; Frazão, M.; Maldaner, V.; Daniel, C.R.; Gomes-Neto, M. Assessment of Maximum Dynamic Inspiratory Pressure. Respir. Care 2018, 63, 1231–1238. [Google Scholar] [CrossRef]
- Roussos, C.S.; Macklem, P.T. Diaphragmatic fatigue in man. J. Appl. Physiol. 1977, 43, 189–197. [Google Scholar] [CrossRef]
- Blazevich, A.J.; Babault, N. Post-activation potentiation (PAP) versus post-activation performance enhancement (PAPE) in humans: Historical perspective, underlying mechanisms, and current issues. Front. Physiol. 2019, 10, 1359. [Google Scholar] [CrossRef]
- McConnell, A.K.; Romer, L.M. Respiratory Muscle Training in Healthy Humans: Resolving the Controversy. Int. J. Sports Med. 2004, 25, 284–293. [Google Scholar] [CrossRef]
- McDonald, T.; Stiller, K. Inspiratory muscle training is feasible and safe for patients with acute spinal cord injury. J. Spinal Cord Med. 2018, 42, 220–227. [Google Scholar] [CrossRef]
- Hodges, P.W.; Heijnen, I.; Gandevia, S.C. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J. Physiol. 2001, 537, 999–1008. [Google Scholar] [CrossRef]
- Kolar, P.; Sulc, J.; Kyncl, M.; Sanda, J.; Neuwirth, J.; Bokarius, A.V.; Kriz, J.; Kobesova, A. Stabilizing function of the diaphragm: Dynamic MRI and synchronized spirometric assessment. J. Appl. Physiol. 2010, 109, 1064–1071. [Google Scholar] [CrossRef]
- Fogarty, M.J.; Mantilla, C.B.; Sieck, G.C. Breathing: Motor Control of Diaphragm Muscle. Physiology 2018, 33, 113–126. [Google Scholar] [CrossRef]
- Mantilla, C.B.; Seven, Y.B.; Sieck, G.C. Convergence of Pattern Generator Outputs on a Common Mechanism of Diaphragm Motor Unit Recruitment. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2014; pp. 309–329. [Google Scholar] [CrossRef]
- Croix, C.M.S.; Morgan, B.J.; Wetter, T.J.; Dempsey, J.A. Fatiguing inspiratory muscle work causes reflex sympathetic activation in humans. J. Physiol. 2000, 529, 493–504. [Google Scholar] [CrossRef]
- Hill, J.M. Discharge of group IV phrenic afferent fibers increases during diaphragmatic fatigue. Brain Res. 2000, 856, 240–244. [Google Scholar] [CrossRef]
- Dempsey, J.A.; Romer, L.; Rodman, J.; Miller, J.; Smith, C. Consequences of exercise-induced respiratory muscle work. Respir. Physiol. Neurobiol. 2006, 151, 242–250. [Google Scholar] [CrossRef]
- Luce, J.M.; Culver, B.H. Respiratory Muscle Function in Health and Disease. Chest 1982, 81, 82–90. [Google Scholar] [CrossRef]
- Green, M.; Moxham, J. The respiratory muscles. Clin. Sci. 1985, 68, 1–10. [Google Scholar] [CrossRef]
- Sieck, G.C.; Gransee, H.M. Respiratory Muscles: Structure, Function, and Regulation. In Colloquium Series on Integrated Systems Physiology: From Molecule to Function to Disease; Morgan & Claypool Life Sciences: San Rafael, CA, USA, 2012; pp. 1–96. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).