Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
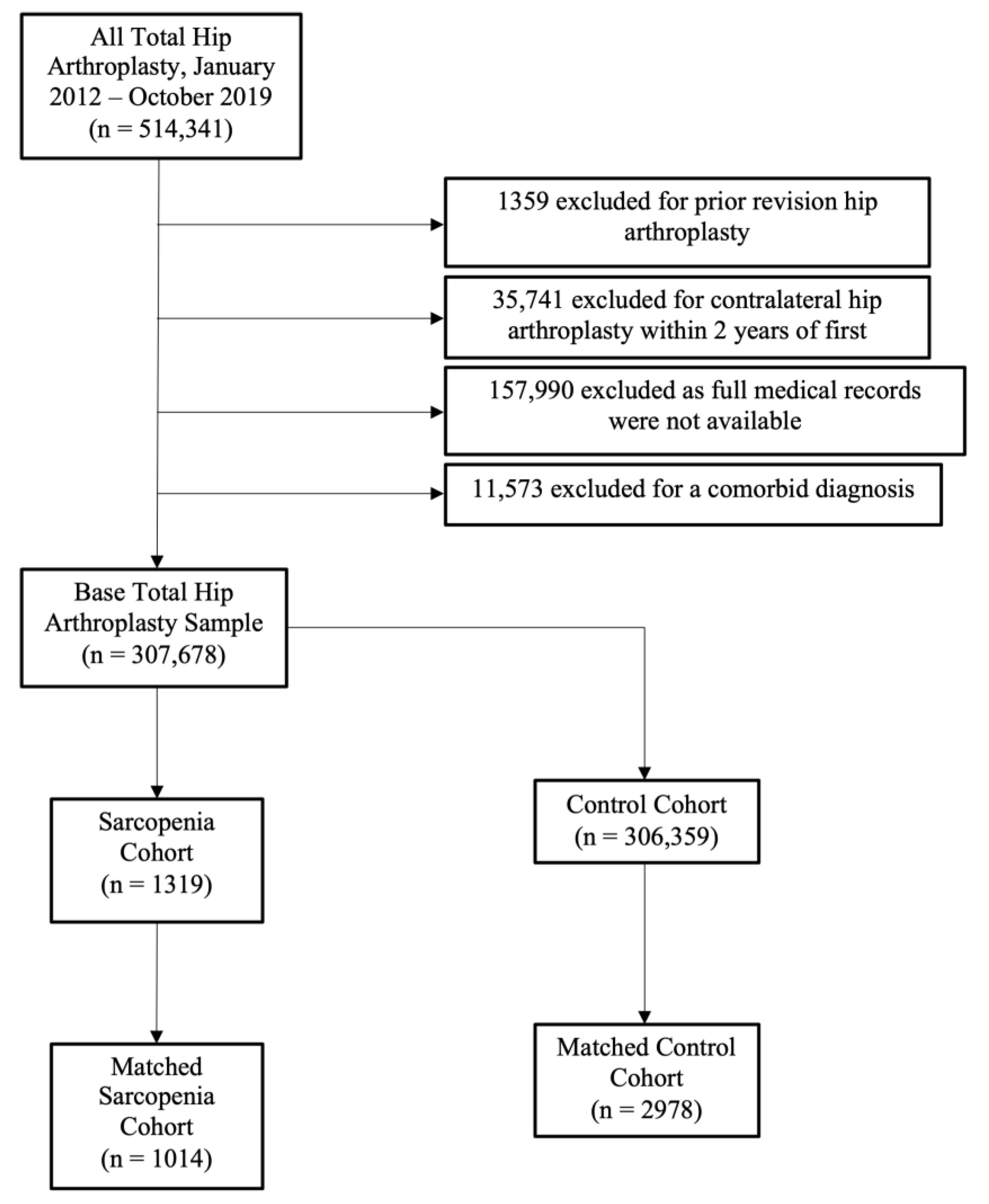
2.2. Creating the Experimental Cohort
2.3. Determining and Comparing the Rates of Postoperative Complications
2.4. Statistical Analysis
3. Results
3.1. Implant-Related Complications
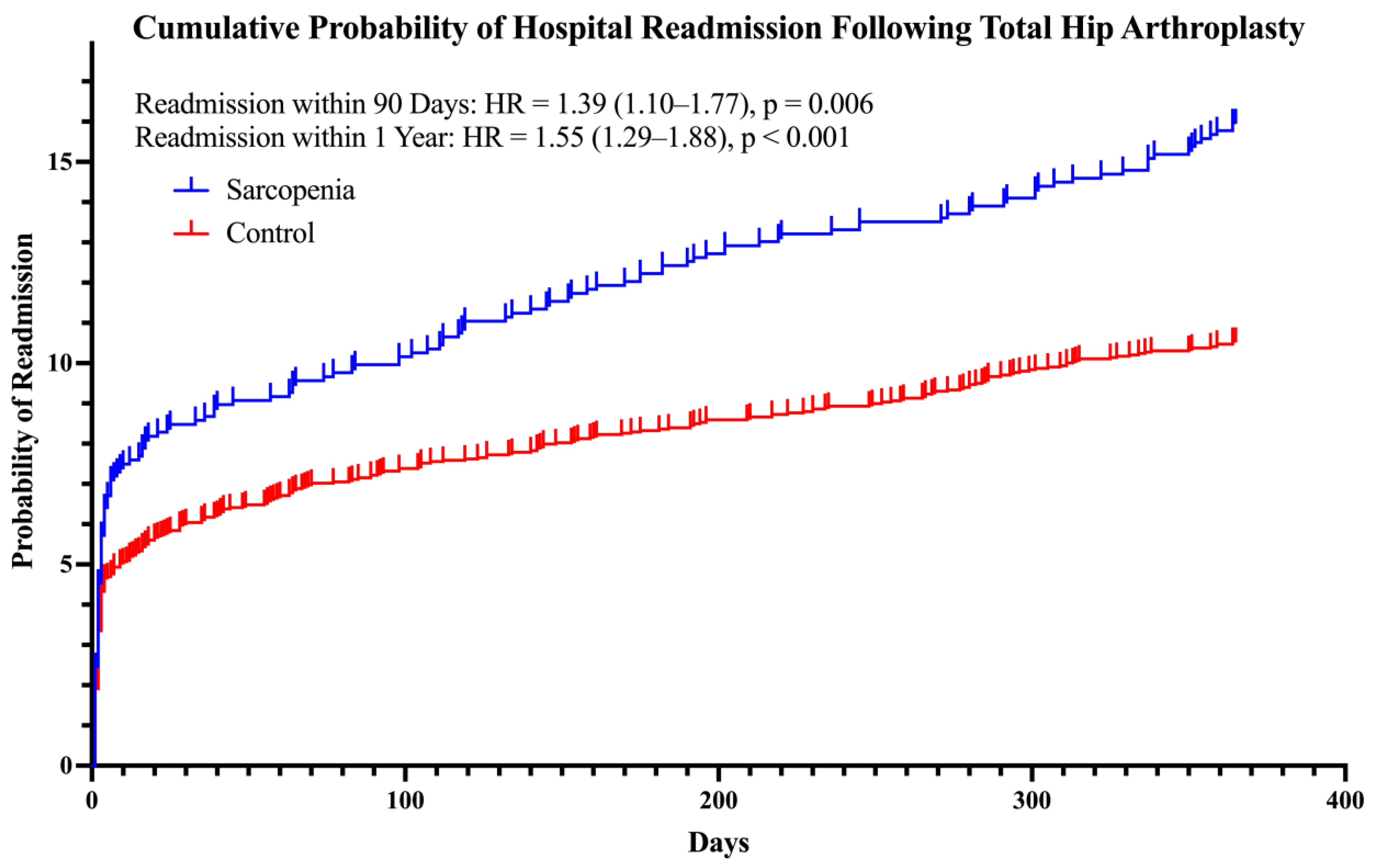
3.2. Ninety-Day Medical Complications and Readmission
3.3. Total Costs of Care
3.4. Fall and Fragility Fracture Risks
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Papadopoulou, S.K. Sarcopenia: A Contemporary Health Problem among Older Adult Populations. Nutrients 2020, 12, 1293. [Google Scholar] [CrossRef]
- Anker, S.D.; Morley, J.E.; von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle 2016, 7, 512–514. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Sobestiansky, S.; Michaelsson, K.; Cederholm, T. Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: A report from the ULSAM study. BMC Geriatr. 2019, 19, 318. [Google Scholar] [CrossRef]
- Dhillon, R.J.; Hasni, S. Pathogenesis and Management of Sarcopenia. Clin. Geriatr. Med. 2017, 33, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Okamura, H.; Kimura, N.; Tanno, K.; Mieno, M.; Matsumoto, H.; Yamaguchi, A.; Adachi, H. The impact of preoperative sarcopenia, defined based on psoas muscle area, on long-term outcomes of heart valve surgery. J. Thorac. Cardiovasc. Surg. 2019, 157, 1071–1079.e1073. [Google Scholar] [CrossRef]
- Pipek, L.Z.; Baptista, C.G.; Nascimento, R.F.V.; Taba, J.V.; Suzuki, M.O.; do Nascimento, F.S.; Martines, D.R.; Nii, F.; Iuamoto, L.R.; Carneiro-D’Albuquerque, L.A.; et al. The impact of properly diagnosed sarcopenia on postoperative outcomes after gastrointestinal surgery: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0237740. [Google Scholar] [CrossRef]
- Olson, B.; Edwards, J.; Stone, L.; Jiang, A.; Zhu, X.; Holland, J.; Li, R.; Andersen, P.; Krasnow, S.; Marks, D.L.; et al. Association of Sarcopenia With Oncologic Outcomes of Primary Surgery or Definitive Radiotherapy Among Patients with Localized Oropharyngeal Squamous Cell Carcinoma. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 714–722. [Google Scholar] [CrossRef]
- Arslan, I.G.; Damen, J.; de Wilde, M.; van den Driest, J.J.; Bindels, P.J.E.; van der Lei, J.; Bierma-Zeinstra, S.M.A.; Schiphof, D. Estimating incidence and prevalence of hip osteoarthritis using electronic health records: A population-based cohort study. Osteoarthr. Cartil. 2022, 30, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Karachalios, T.; Komnos, G.; Koutalos, A. Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev. 2018, 3, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Dargel, J.; Oppermann, J.; Bruggemann, G.P.; Eysel, P. Dislocation following total hip replacement. Dtsch. Arztebl. Int. 2014, 111, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, M.S.; Vidal, E.A.; Drtil, A.A.; Goytia, R.N.; Mathews, V.; Patel, A.R. Mortality After Revision Total Hip Arthroplasty. J. Arthroplast. 2021, 36, 2353–2358. [Google Scholar] [CrossRef] [PubMed]
- Rietbergen, L.; Kuiper, J.W.; Walgrave, S.; Hak, L.; Colen, S. Quality of life after staged revision for infected total hip arthroplasty: A systematic review. Hip Int. 2016, 26, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Mowat, F.S.; Chan, N.; Lau, E.; Halpern, M.T.; Kurtz, S.M. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin. Orthop. Relat. Res. 2006, 446, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, N.; Wang, Y.; Li, H. Association between sarcopenia and osteoarthritis: A protocol for meta-analysis. PLoS ONE 2022, 17, e0272284. [Google Scholar] [CrossRef] [PubMed]
- Babu, J.M.; Kalagara, S.; Durand, W.; Antoci, V.; Deren, M.E.; Cohen, E. Sarcopenia as a Risk Factor for Prosthetic Infection After Total Hip or Knee Arthroplasty. J. Arthroplast. 2019, 34, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Ardeljan, A.D.; Polisetty, T.S.; Palmer, J.; Vakharia, R.M.; Roche, M.W. Comparative Analysis on the Effects of Sarcopenia following Primary Total Knee Arthroplasty: A Retrospective Matched-Control Analysis. J. Knee Surg. 2022, 35, 128–134. [Google Scholar] [CrossRef]
- Albright, J.A.; Chang, K.; Alsoof, D.; McDonald, C.L.; Diebo, B.G.; Daniels, A.H. Sarcopenia and Postoperative Complications, Cost of Care, and All-Cause Hospital Readmission Following Lumbar Spine Arthrodesis: A Propensity Matched Cohort Study. World Neurosurg. 2022, 169, e131–e140. [Google Scholar] [CrossRef] [PubMed]
- Ueoka, K.; Kabata, T.; Kajino, Y.; Inoue, D.; Ohmori, T.; Ueno, T.; Yoshitani, J.; Yamamuro, Y.; Taninaka, A.; Kato, S.; et al. The prevalence and impact of sarcopenia in females undergoing total hip arthroplasty: A prospective study. Mod. Rheumatol. 2022, 32, 193–198. [Google Scholar] [CrossRef]
- Koto, S.; Ikeda, T.; Inoue, S.; Inoue, H.; Watanabe, M. Differences in preoperative function and outcome of patients with versus without sarcopenia after total hip arthroplasty. J. Phys. Ther. Sci. 2022, 34, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.D.; Chen, H.C.; Liou, T.H.; Lin, C.L.; Huang, S.W. Impact of Sarcopenia and Obesity on Gait Speed After Total Knee Replacement. J. Am. Med. Dir. Assoc. 2022, 23, 631–637. [Google Scholar] [CrossRef]
- Bokshan, S.L.; Han, A.L.; DePasse, J.M.; Eltorai, A.E.; Marcaccio, S.E.; Palumbo, M.A.; Daniels, A.H. Effect of Sarcopenia on Postoperative Morbidity and Mortality After Thoracolumbar Spine Surgery. Orthopedics 2016, 39, e1159–e1164. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, L.; Grabo, D.J.; Shashaty, M.; Dua, R.; Sonnad, S.S.; Sims, C.A.; Pascual, J.L.; Schwab, C.W.; Holena, D.N. Psoas:lumbar vertebra index: Central sarcopenia independently predicts morbidity in elderly trauma patients. Eur. J. Trauma Emerg. Surg. 2014, 40, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.H.; Lee, S.H.; Kim, J.W.; Koh, W.U.; Kim, H.T.; Ro, Y.J.; Kim, H.J. Low Psoas Lumbar Vertebral Index Is Associated with Mortality after Hip Fracture Surgery in Elderly Patients: A Retrospective Analysis. J. Pers. Med. 2021, 11, 673. [Google Scholar] [CrossRef] [PubMed]
- Soong, M.; Rubash, H.E.; Macaulay, W. Dislocation after total hip arthroplasty. J. Am. Acad. Orthop. Surg. 2004, 12, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Werner, B.C.; Brown, T.E. Instability after total hip arthroplasty. World J. Orthop. 2012, 3, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Takao, M.; Hamada, H.; Sakai, T.; Sugano, N. Soft tissue tension is four times lower in the unstable primary total hip arthroplasty. Int. Orthop. 2018, 42, 2059–2065. [Google Scholar] [CrossRef] [PubMed]
- Takao, M.; Nishii, T.; Sakai, T.; Sugano, N. Postoperative Limb-Offset Discrepancy Notably Affects Soft-Tissue Tension in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2016, 98, 1548–1554. [Google Scholar] [CrossRef]
- Woerner, M.; Weber, M.; Sendtner, E.; Springorum, R.; Worlicek, M.; Craiovan, B.; Grifka, J.; Renkawitz, T. Soft tissue restricts impingement-free mobility in total hip arthroplasty. Int. Orthop. 2017, 41, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Inacio, M.; Ryan, A.S.; Bair, W.N.; Prettyman, M.; Beamer, B.A.; Rogers, M.W. Gluteal muscle composition differentiates fallers from non-fallers in community dwelling older adults. BMC Geriatr. 2014, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Vadala, A.P.; Mazza, D.; Desideri, D.; Iorio, R.; Fedeli, G.; Scrivano, M.; Serlorenzi, P.; Ferretti, A. Could the tendon degeneration and the fatty infiltration of the gluteus medius affect clinical outcome in total hip arthroplasty? Int. Orthop. 2020, 44, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Sotelo, J.; Haidukewych, G.J.; Boberg, C.J. Hospital cost of dislocation after primary total hip arthroplasty. J. Bone Jt. Surg. Am. 2006, 88, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Hermansen, L.L.; Viberg, B.; Overgaard, S. Patient-reported outcome after dislocation of primary total hip arthroplasties: A cross-sectional study derived from the Danish Hip Arthroplasty Register. Acta Orthop. 2022, 93, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.K.; Beom, J.; Lee, S.Y.; Kim, B.R.; Chun, S.W.; Lim, J.Y.; Shin Lee, E. Association between sarcopenia and fall characteristics in older adults with fragility hip fracture. Injury 2020, 51, 2640–2647. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Wong, H.; Zhang, N.; Chow, S.K.H.; Chau, W.W.; Wang, J.; Chim, Y.N.; Leung, K.S.; Cheung, W.H. The relationship between sarcopenia and fragility fracture-a systematic review. Osteoporos. Int. 2019, 30, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.P.; Adachi, J.D.; Schemitsch, E.; Tarride, J.E.; Brown, V.; Bell, A.; Reiner, M.; Oliveira, T.; Motsepe-Ditshego, P.; Burke, N.; et al. Mortality in older adults following a fragility fracture: Real-world retrospective matched-cohort study in Ontario. BMC Musculoskelet. Disord. 2021, 22, 105. [Google Scholar] [CrossRef]
- Han, A.; Bokshan, S.L.; Marcaccio, S.E.; DePasse, J.M.; Daniels, A.H. Diagnostic Criteria and Clinical Outcomes in Sarcopenia Research: A Literature Review. J. Clin. Med. 2018, 7, 70. [Google Scholar] [CrossRef]
- Garbarino, L.J.; Gold, P.A.; Anis, H.; Sodhi, N.; Burshtein, J.; Burshtein, A.; Danoff, J.R.; Boraiah, S.; Rasquinha, V.J.; Mont, M.A. The Effect of Bladder Catheterization Technique on Postoperative Urinary Tract Infections After Primary Total Hip Arthroplasty. J. Arthroplast. 2020, 35, S325–S329. [Google Scholar] [CrossRef] [PubMed]
- Kostakopoulos, N.A.; Karakousis, N.D.; Moschotzopoulos, D. Frailty associated urinary tract infections (FaUTIs). J. Frailty Sarcopenia Falls 2021, 6, 9–13. [Google Scholar] [CrossRef]
- Majima, T.; Funahashi, Y.; Matsukawa, Y.; Inoue, S.; Sassa, N.; Kato, M.; Yamamoto, T.; Gotoh, M. Investigation of the relationship between bladder function and sarcopenia using pressure flow studies in elderly male patients. Neurourol. Urodyn. 2019, 38, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Song, I.K.; Nam, J.S.; Lee, S.W.; Lee, E.H.; Choi, I.C. Sarcopenia as a prognostic factor for outcomes after isolated tricuspid valve surgery. J. Cardiol. 2020, 76, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Zhao, R.; Wan, Q.; Wu, Y.; Zhou, Y.; Wang, Y.; Cui, Y.; Shen, X.; Wu, X. Sarcopenia and adverse health-related outcomes: An umbrella review of meta-analyses of observational studies. Cancer Med. 2020, 9, 7964–7978. [Google Scholar] [CrossRef]
- Janssen, I.; Shepard, D.S.; Katzmarzyk, P.T.; Roubenoff, R. The healthcare costs of sarcopenia in the United States. J. Am. Geriatr. Soc. 2004, 52, 80–85. [Google Scholar] [CrossRef]
- Glassou, E.N.; Hansen, T.B.; Pedersen, A.B. Risk of pneumonia and urinary tract infection within the first week after total hip arthroplasty and the impact on survival. Clin. Epidemiol. 2017, 9, 31–39. [Google Scholar] [CrossRef]
- Liao, C.D.; Wu, Y.T.; Tsauo, J.Y.; Chen, P.R.; Tu, Y.K.; Chen, H.C.; Liou, T.H. Effects of Protein Supplementation Combined with Exercise Training on Muscle Mass and Function in Older Adults with Lower-Extremity Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Trials. Nutrients 2020, 12, 2422. [Google Scholar] [CrossRef] [PubMed]
- Lo, J.H.; U, K.P.; Yiu, T.; Ong, M.T.; Lee, W.Y. Sarcopenia: Current treatments and new regenerative therapeutic approaches. J. Orthop. Translat. 2020, 23, 38–52. [Google Scholar] [CrossRef]
- Yanai, H. Nutrition for Sarcopenia. J. Clin. Med. Res. 2015, 7, 926–931. [Google Scholar] [CrossRef]
- Daly, R.M.; O’Connell, S.L.; Mundell, N.L.; Grimes, C.A.; Dunstan, D.W.; Nowson, C.A. Protein-enriched diet, with the use of lean red meat, combined with progressive resistance training enhances lean tissue mass and muscle strength and reduces circulating IL-6 concentrations in elderly women: A cluster randomized controlled trial. Am. J. Clin. Nutr. 2014, 99, 899–910. [Google Scholar] [CrossRef]
- Lin, C.C.; Shih, M.H.; Chen, C.D.; Yeh, S.L. Effects of adequate dietary protein with whey protein, leucine, and vitamin D supplementation on sarcopenia in older adults: An open-label, parallel-group study. Clin. Nutr. 2021, 40, 1323–1329. [Google Scholar] [CrossRef]
- Voyvodic, L.C.; Khan, N.Z.; Lam, A.W.; Horn, A.R.; Mont, M.A.; Razi, A.E. Crohn’s Disease is Associated with Longer In-Hospital Lengths of Stay and Higher Rates of Complications and Costs after Primary Total Hip Arthroplasty. J. Arthroplast. 2021, 36, 2110–2115. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, N.M.; Vakharia, R.M.; Mont, M.A.; Jiranek, W.A.; Bolognesi, M.P.; Seyler, T.M. Paget’s Disease in Primary Total Hip Arthroplasty Is Associated With Greater In-Hospital Lengths of Stay, Costs, and Complications. J. Arthroplast. 2021, 36, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Cnudde, P.H.J.; Nemes, S.; Bulow, E.; Timperley, A.J.; Whitehouse, S.L.; Karrholm, J.; Rolfson, O. Risk of further surgery on the same or opposite side and mortality after primary total hip arthroplasty: A multi-state analysis of 133,654 patients from the Swedish Hip Arthroplasty Register. Acta Orthop. 2018, 89, 386–393. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Unmatched | Matched | ||||
|---|---|---|---|---|---|---|
| Sarcopenia (n = 1319) | Control (n = 306,359) | p-Value | Sarcopenia (n = 1014) | Control (n = 2978) | p-Value | |
| Sex, female, n (%) | 803 (60.9) | 173,763 (56.7) | 0.003 | 634 (62.5) | 1862 (62.5) | 1.000 |
| Age, mean ± SD | 65.4 ± 10.0 | 65.0 ± 10.0 | 0.086 | 66.4 ± 8.9 | 66.3 ± 8.9 | 0.935 |
| CCI, mean ± SD | 2.4 ± 2.7 | 1.5 ± 1.9 | <0.001 | 1.6 ± 1.6 | 1.6 ± 1.6 | 0.472 |
| Comorbidities, n (%) | ||||||
| Osteoporosis | 386 (29.3) | 59,892(19.5) | <0.001 | 237 (23.4) | 684 (23.0) | 0.825 |
| Osteoarthritis | 1278 (96.9) | 262,582(85.7) | <0.001 | 999 (98.5) | 2933 (98.5) | 1.000 |
| Diabetes mellitus | 667 (50.6) | 121,346(39.6) | <0.001 | 482 (47.5) | 1403 (47.1) | 0.844 |
| Tobacco use | 744 (56.4) | 119,292(38.9) | <0.001 | 415 (40.9) | 1214 (40.8) | 0.958 |
| Obesity or overweight (BMI > 25) | 626 (47.5) | 125,541(41.0) | <0.001 | 442 (43.6) | 1286 (43.2) | 0.850 |
| Morbid obesity (BMI > 40) | 285 (21.6) | 51,458(16.8) | <0.001 | 183 (18.0) | 530 (17.8) | 0.895 |
| Vitamin D deficiency | 507 (38.4) | 91,886(30.0) | <0.001 | 346 (34.1) | 995 (33.4) | 0.707 |
| Hyperparathyroidism | 85 (6.4) | 10,313(3.4) | <0.001 | 14 (1.4) | 37 (1.2) | 0.860 |
| Orthopedic-Related Complications, n (%) | Sarcopenia (n = 1014) | Control (n = 2978) | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Total orthopedic-related complications | ||||
| 1 year | 48 (4.73) | 90 (3.02) | 1.70 (0.78–3.54) | 0.012 |
| 2 years | 51 (5.03) | 106 (3.56) | 1.67 (0.79–3.37) | 0.042 |
| Periprosthetic fracture (%) | ||||
| 1 year | 11 (1.08) | 19 (0.64) | 1.70 (0.78–3.54) | 0.167 |
| 2 years | 12 (1.18) | 21 (0.71) | 1.67 (0.79–3.37) | 0.159 |
| All-cause revision (%) | ||||
| 1 year | 32 (3.16) | 63 (2.12) | 1.51 (0.97–2.31) | 0.063 |
| 2 years | 35 (3.45) | 77 (2.59) | 1.34 (0.89–2.00) | 0.154 |
| Instability (%) | ||||
| 1 year | 20 (1.97) | 27 (0.91) | 2.19 (1.21–3.91) | 0.009 |
| 2 years | 21 (2.07) | 31 (1.04) | 2.00 (1.13–3.48) | 0.015 |
| Loosening (%) | ||||
| 1 year | <11 (N/A) | 12 (0.40) | 2.20 (0.90–5.23) | 0.075 |
| 2 years | 11 (1.08) | 16 (0.54) | 2.01 (0.90–4.32) | 0.076 |
| Dislocation (%) | ||||
| 1 year | 20 (1.97) | 27 (0.91) | 2.19 (1.21–3.91) | 0.008 |
| 2 years | 20 (1.97) | 30 (1.01) | 1.97 (1.10–3.46) | 0.020 |
| Deep periprosthetic infection (%) | ||||
| 6 months | 16 (1.58) | 29 (0.97) | 1.63 (0.86–2.98) | 0.122 |
| 1 year | 19 (1.87) | 32 (1.07) | 1.75 (0.99–3.11) | 0.055 |
| Experienced a fall (%) | ||||
| 1 year | 42 (4.14) | 77 (2.59) | 1.62 (1.10–2.39) | 0.014 |
| 2 years | 68 (6.71) | 121 (4.06) | 1.70 (1.24–2.30) | <0.001 |
| Fragility fracture (%) | ||||
| 1 year | 95 (9.37) | 168 (5.64) | 1.77 (1.34–2.31) | <0.001 |
| 2 years | 105 (10.36) | 206 (6.92) | 1.58 (1.22–2.03) | <0.001 |
| Medical Complications, n (%) | Sarcopenia (n = 1014) | Control (n = 2978) | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Total 90-day medical complications | 156 (15.38) | 349 (11.72) | 1.37 (1.11–1.69) | 0.003 |
| Acute kidney injury | 22 (2.17) | 67 (2.25) | 0.94 (0.56–1.51) | 0.790 |
| Cardiac arrest | 0 (0) | <11 (N/A) | N/A | 0.994 |
| Deep vein thrombosis | <11 (N/A) | <11 (N/A) | 1.17 (0.37–3.75) | 0.79 |
| Wound disruption | <11 (N/A) | 21 (0.71) | 0.97 (0.39–2.17) | 0.935 |
| Hematoma | 15 (1.47) | 23 (0.77) | 1.91 (0.97–3.65) | 0.053 |
| Nerve injury | <11 (N/A) | 0 (0) | N/A | 0.996 |
| Pneumonia | 16 (1.58) | 50 (1.68) | 0.92 (0.50–1.59) | 0.768 |
| Pulmonary embolism | 11 (1.08) | 21 (0.71) | 1.54 (0.71–3.14) | 0.249 |
| Required transfusion | 45 (4.44) | 105 (3.53) | 1.25 (0.87–1.79) | 0.217 |
| Urinary tract infection | 74 (7.30) | 127 (4.26) | 1.79 (1.32–2.42) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, K.; Albright, J.A.; Testa, E.J.; Balboni, A.B.; Daniels, A.H.; Cohen, E. Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis. Biology 2023, 12, 295. https://doi.org/10.3390/biology12020295
Chang K, Albright JA, Testa EJ, Balboni AB, Daniels AH, Cohen E. Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis. Biology. 2023; 12(2):295. https://doi.org/10.3390/biology12020295
Chicago/Turabian StyleChang, Kenny, J. Alex Albright, Edward J. Testa, Alanna B. Balboni, Alan H. Daniels, and Eric Cohen. 2023. "Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis" Biology 12, no. 2: 295. https://doi.org/10.3390/biology12020295
APA StyleChang, K., Albright, J. A., Testa, E. J., Balboni, A. B., Daniels, A. H., & Cohen, E. (2023). Sarcopenia Is Associated with an Increased Risk of Postoperative Complications Following Total Hip Arthroplasty for Osteoarthritis. Biology, 12(2), 295. https://doi.org/10.3390/biology12020295







