Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol of the Study
2.3. Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, X.; Hu, F. Relationship Between Physical Fitness, Anthropometric Measurement, and Bone Health in Adult Men. Clin. Nurs. Res. 2021, 10547738211060937. [Google Scholar] [CrossRef] [PubMed]
- Więch, P.; Sałacińska, I.; Bączek, M.; Bazaliński, D. The nutritional status of healthy children using bioelectrical impedance and anthropometric measurement. J. Pediatr. 2022, 98, 161–167. [Google Scholar] [CrossRef] [PubMed]
- You, W.; Henneberg, M. Significantly different roles of economic affluence in sex-specific obesity prevalence rates: Understanding more modifications within female body weight management. Sci. Rep. 2022, 12, 15757. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.Y.; Bruyère, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef] [Green Version]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Norris, T.; Cole, T.J.; Bann, D.; Hamer, M.; Hardy, R.; Li, L.; Ong, K.K.; Ploubidis, G.B.; Viner, R.; Johnson, W. Duration of obesity exposure between ages 10 and 40 years and its relationship with cardiometabolic disease risk factors: A cohort study. PLoS Med. 2020, 17, e1003387. [Google Scholar] [CrossRef]
- Walsh, T.P.; Arnold, J.B.; Evans, A.M.; Yaxley, A.; Damarell, R.A.; Shanahan, E.M. The association between body fat and musculoskeletal pain: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2018, 19, 233. [Google Scholar] [CrossRef] [Green Version]
- Karimi, S.; Pasdar, Y.; Hamzeh, B.; Ayenehpour, A.; Heydarpour, F.; Goudarzi, F. Obesity phenotypes related to musculoskeletal disorders; a cross-sectional study from RaNCD cohort. Arch. Public Health 2022, 80, 185. [Google Scholar] [CrossRef]
- Tanishima, S.; Hagino, H.; Matsumoto, H.; Tanimura, C.; Nagashima, H. The Risk Factor of Worsening Low Back Pain in Older Adults Living in a Local Area of Japan: The GAINA Study. Yonago Acta Med. 2020, 63, 319–325. [Google Scholar] [CrossRef]
- Milewska, M.; Przekop, Z.; Szostak-Węgierek, D.; Chrzanowska, M.; Raciborski, F.; Traczyk, I.; Sińska, B.I.; Samoliński, B. Prevalence of Risk of Sarcopenia in Polish Elderly Population-A Population Study. Nutrients 2022, 14, 3466. [Google Scholar] [CrossRef]
- Borga, M.; West, J.; Bell, J.D.; Harvey, N.C.; Romu, T.; Heymsfield, S.B.; Dahlqvist Leinhard, O. Advanced body composition assessment: From body mass index to body composition profiling. J. Investing. Med. 2018, 66, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, E.L.; Frost, G.; Taylor-Robinson, S.D.; Bell, J.D. Excess body fat in obese and normal-weight subjects. Nut. Res. Rev. 2012, 25, 150–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laughton, G.E.; Buchholz, A.C.; Martin Ginis, K.A.; Goy, R.E.; SHAPE SCI Research Group. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal. Cord. 2009, 47, 757–762. [Google Scholar] [CrossRef] [Green Version]
- Gawlik, K.; Zwierzchowska, A.; Celebańska, D. Impact of physical activity on obesity and lipid profile of adults with intellectual disability. J. Appl. Res. Intellect. Disabil. 2018, 31, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Zwierzchowska, A.; Rosołek, B.; Sikora, M.; Celebańska, D. Forced Sedentariness and Sports Activity as Factors Differentiating Anthropometric Characteristics, Indices, and Body Composition in People with Disabilities. Biology 2022, 11, 906. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Bautista, L.; Franzosi, M.G.; Commerford, P.; Lang, C.C.; Rumboldt, Z.; Onen, C.L.; Lisheng, L.; et al. Obesity and the risk of myocardial infarction in 27, 000 participants from 52 countries: A case-control study. Lancet 2005, 366, 1640–1649. [Google Scholar] [CrossRef]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef]
- Compston, J.E.; Bhambhani, M.; Laskey, M.A.; Murphy, S.; Khaw, K.T. Body composition and bone mass in postmenopausal women. Clin. Endocrinol. 1992, 37, 426–431. [Google Scholar] [CrossRef]
- Rose Berlin Piodena-Aportadera, M.; Lau, S.; Chew, J.; Lim, J.P.; Ismail, N.H.; Ding, Y.Y.; Lim, W.S. Calf circumference measurement protocols for sarcopenia screening: Differences in agreement, convergent validity and diagnostic performance. Ann. Geriatr. Med. Res. 2022, 26, 215–224. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Topinková, E.; Michel, J.P. Understanding sarcopenia as a geriatric syndrome. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Toth, M.J.; Tchernof, A.; Sites, C.K.; Poehlman, E.T. Effect of menopausal status on body composition and abdominal fat distribution. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 226–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucas, R.; Nassif, P.; Tabushi, F.I.; Nassif, D.; Ariede, B.L.; Brites-Neto, J.; Malafaia, O. Can stature, abdominal perimeter and bmi index predict possible cardiometabolic risks in future obesity? Arq. Bras. Cir. Dig. 2000, 33, e1529. [Google Scholar] [CrossRef] [PubMed]
- Neeland, I.J.; Ross, R.; Després, J.P.; Matsuzawa, Y.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; et al. International Chair on Cardiometabolic Risk Working Group on Visceral Obesity Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 2019, 7, 715–725. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- WHO. Obesity: Preventing and Managing the Global Epidemic: Report on a WHO Consultation on Obesity; WHO: Geneva, Switzerland, 1998.
- Tosato, M.; Ciciarello, F.; Zazzara, M.B.; Pais, C.; Cacciatore, S.; Montenero, R.; Leone, M.S.; Chisci, E.; Picca, A.; Galluzzo, V.; et al. Lifestyle Changes and Psychological Well-Being in Older Adults During COVID-19 Pandemic. Clin. Geriatr Med. 2022, 38, 449–459. [Google Scholar] [CrossRef]
- WHO. WHO Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; WHO: Geneva, Switzerland, 2008.
- WHO. WHO European Regional Obesity Report 2022; WHO: Geneva, Switzerland, 2022.
- Djibo, D.A.; Araneta, M.R.; Kritz-Silverstein, D.; Barrett-Connor, E.; Wooten, W. Body adiposity index as a risk factor for the metabolic syndrome in postmenopausal Caucasian, African American, and Filipina women. Diabetes Metab. Syndr. 2015, 9, 108–113. [Google Scholar] [CrossRef] [Green Version]
- Zając-Gawlak, I.; Groffik, D. Ubytki wysokości ciała jako składowa inwolucyjnych zmian w budowie somatycznej kobiet i mężczyzn po 50. roku życia. Gerontol. Pol. 2010, 18, 183–193. [Google Scholar]
- Chmielewski, P.; Borysławski, K.; Chmielowiec, J.; Chmielowiec, K. Ubytki wysokości ciała a ryzyko zgonu u osób starszych. Gerontol. Współczesna 2016, 4, 73–80. [Google Scholar]
- Bosy-Westphal, A.; Müller, M.J. Identification of skeletal muscle mass depletion across age and BMI groups in health and disease--there is need for a unified definition. Int. J. Obes. 2015, 39, 379–386. [Google Scholar] [CrossRef]
- Gray, L.A.; Breeze, P.R.; Williams, E.A. BMI trajectories, morbidity, and mortality in England: A two-step approach to estimating consequences of changes in BMI. Obesity 2022, 30, 1898–1907. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.A.; Pagotto, V.; Barbosa, L.S.; Oliveira, C.; Pena, G.D.G.; Velasquez-Melendez, G. Accuracy of BMI and waist circumference cut-off points to predict obesity in older adults. Ciên. Saúde Colet. 2020, 25, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Swainson, M.G.; Batterham, A.M.; Tsakirides, C.; Rutherford, Z.H.; Hind, K. Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLoS ONE 2017, 12, e0177175. [Google Scholar] [CrossRef] [PubMed]
- Zwierzchowska, A.; Grabara, M.; Palica, D.; Zając, A. BMI and BAI as markers of obesity in a Caucasian population. Obes. Facts 2013, 6, 507–511. [Google Scholar] [CrossRef]
- Elisha, B.; Rabasa-Lhoret, R.; Messier, V.; Abdulnour, J.; Karelis, A.D. Relationship between the body adiposity index and cardiometabolic risk factors in obese postmenopausal women. Eur. J. Nutr. 2013, 52, 145–151. [Google Scholar] [CrossRef]
- Chang, H.; Simonsick, E.M.; Ferrucci, L.; Cooper, J.A. Validation study of the body adiposity index as a predictor of percent body fat in older individuals: Findings from the BLSA. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1069–1075. [Google Scholar] [CrossRef] [Green Version]
- Zwierzchowska, A.; Celebańska, D.; Rosołek, B.; Gawlik, K.; Żebrowska, A. Is body mass index (BMI) or body adiposity index (BAI) a better indicator to estimate body fat and selected cardiometabolic risk factors in adults with intellectual disabilities? BMC Cardiovasc. Disord. 2021, 21, 119. [Google Scholar] [CrossRef]
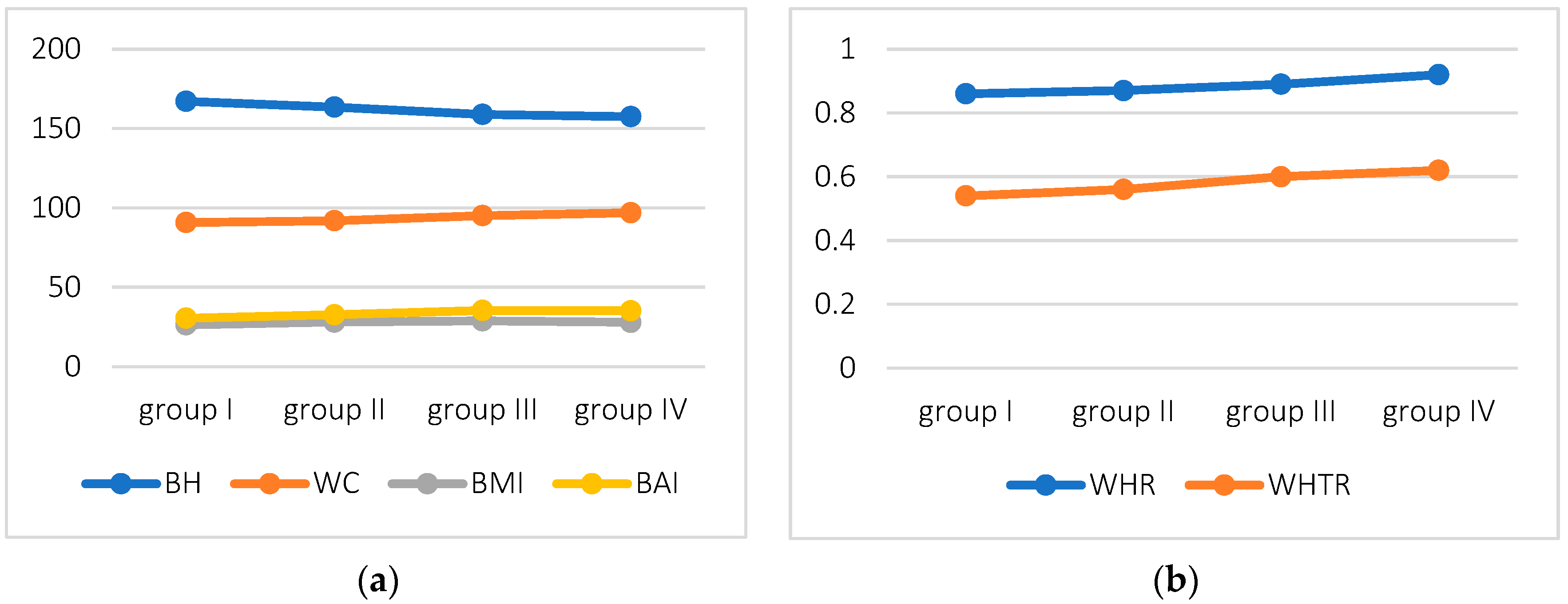

| Characteristics, Indices | Group I Age: 40–49 Years (n = 6) | Group II Age: 50–59 Years (n = 21) | Group III Age: 60–69 Years (n = 43) | Group IV Age: 70–79 Years (n = 17) |
|---|---|---|---|---|
| Age * | 45.5 ± 2.1 | 54.4 ± 2.8 | 64.3 ± 3.3 | 73.2 ± 2.5 |
| BH [cm] * | 167.2 ± 3.9 | 163.5 ± 8.1 | 158.9 ± 5.4 | 157.5 ± 4.4 |
| BM [kg] | 73.6 ± 9.7 | 75.3 ± 15.9 | 72.8 ± 13.7 | 69.3 ± 7.7 |
| WC [cm] | 90.8 ± 12.5 | 91.9 ± 13.8 | 95.1 ± 11.5 | 96.9 ± 8.9 |
| HC [cm] | 104.8 ± 6.4 | 105.8 ± 14.1 | 106.7 ± 10.6 | 105.0 ± 7.1 |
| BMI [kg/m2] | 26.4 ± 4.3 | 28.1 ± 5.1 | 28.9 ± 5.3 | 27.9 ± 3.1 |
| BAI [%] | 30.6 ± 4.4 | 32.7 ± 6.6 | 35.4 ± 5.7 | 35.2 ± 4.2 |
| WHR * | 0.86 ± 0.08 | 0.87 ± 0.09 | 0.89 ± 0.06 | 0.92 ± 0.05 |
| WHTR | 0.54 ± 0.08 | 0.56 ± 0.08 | 0.6 ± 0.08 | 0.62 ± 0.06 |
| FV [cm3] | 1107.3 ± 382.9 | 1113.2 ± 740.8 | 1389.9 ± 716.9 | 1272.3 ± 583.9 |
| FT [%] | 37.3 ± 5.6 | 38.7 ± 7.2 | 40.7 ± 6.7 | 40.4 ± 3.9 |
| WC | BMI | BAI | WHR | WHTR | |
|---|---|---|---|---|---|
| Total | |||||
| FT [%] | 0.81 *** | 0.83 *** | 0.76 *** | 0.19 | 0.79 *** |
| Group I, 40–49 years (n = 7) | |||||
| FT [%] | 0.89 ** | 0.94 ** | - | 0.54 | 0.89 * |
| Group II, 50–59 years (n = 21) | |||||
| FT [%] | 0.91 *** | 0.89 *** | 0.74 *** | 0.3 | 0.84 *** |
| Group III, 60–69 years (n = 43) | |||||
| FT [%] | 0.83 *** | 0.83 *** | 0.75 *** | 0.38 ** | 0.82 *** |
| Group IV, 70–79 years (n = 17) | |||||
| FT [%] | 0.65 ** | 0.75 ** | 0.56 ** | 0.28 | 0.66 ** |
| WC | BMI | BAI | WHR | WHTR | |
|---|---|---|---|---|---|
| Total | |||||
| FV (cm3) | 0.74 *** | 0.73 *** | 0.59 | 0.30 ** | 0.69 *** |
| Group I, 40–49 years (n = 7) | |||||
| FV (cm3) | −0.37 | −0.25 | −0.49 | −0.37 | −0.37 |
| Group II, 50–59 years (n = 21) | |||||
| FV (cm3) | 0.87 *** | 0.79 *** | 0.52 ** | 0.27 | 0.75 *** |
| Group III, 60–69 years (n = 43) | |||||
| FV (cm3) | 0.85 *** | 0.81 *** | 0.69 *** | 0.49 *** | 0.83 *** |
| Group IV, 70–79 years (n = 17) | |||||
| FV (cm3) | 0.65 *** | 0.53 | 0.29 ** | 0.58 ** | 0.73 *** |
| WC | BMI | BAI | WHTR | |
|---|---|---|---|---|
| Se [%] | 98.53 | 89.7 | 41.18 | 100 |
| Sp [%] | 57.89 | 73.68 | 94.74 | 84.21 |
| AUC | 0.935 p < 0.000 | 0.933 p < 0.000 | 0.906 p < 0.000 | 0.925 p < 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zwierzchowska, A.; Kantyka, J.; Rosołek, B.; Nawrat-Szołtysik, A.; Małecki, A. Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life. Biology 2022, 11, 1804. https://doi.org/10.3390/biology11121804
Zwierzchowska A, Kantyka J, Rosołek B, Nawrat-Szołtysik A, Małecki A. Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life. Biology. 2022; 11(12):1804. https://doi.org/10.3390/biology11121804
Chicago/Turabian StyleZwierzchowska, Anna, Joanna Kantyka, Barbara Rosołek, Agnieszka Nawrat-Szołtysik, and Andrzej Małecki. 2022. "Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life" Biology 11, no. 12: 1804. https://doi.org/10.3390/biology11121804
APA StyleZwierzchowska, A., Kantyka, J., Rosołek, B., Nawrat-Szołtysik, A., & Małecki, A. (2022). Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life. Biology, 11(12), 1804. https://doi.org/10.3390/biology11121804








