Subcutaneous Adipose Tissue Measured by B-Mode Ultrasound to Assess and Monitor Obesity and Cardio–Metabolic Risk in Children and Adolescents
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Anthropometry
2.3. Subcutaneous Adipose Tissue (SAT) Measurements
2.4. Blood Pressure Measurements
2.5. Statistical Analysis
3. Results
3.1. Sexual Dimorphism in Anthropometric Measures and Subcutaneous Adipose Tissue
3.2. SAT in Children and Adolescents
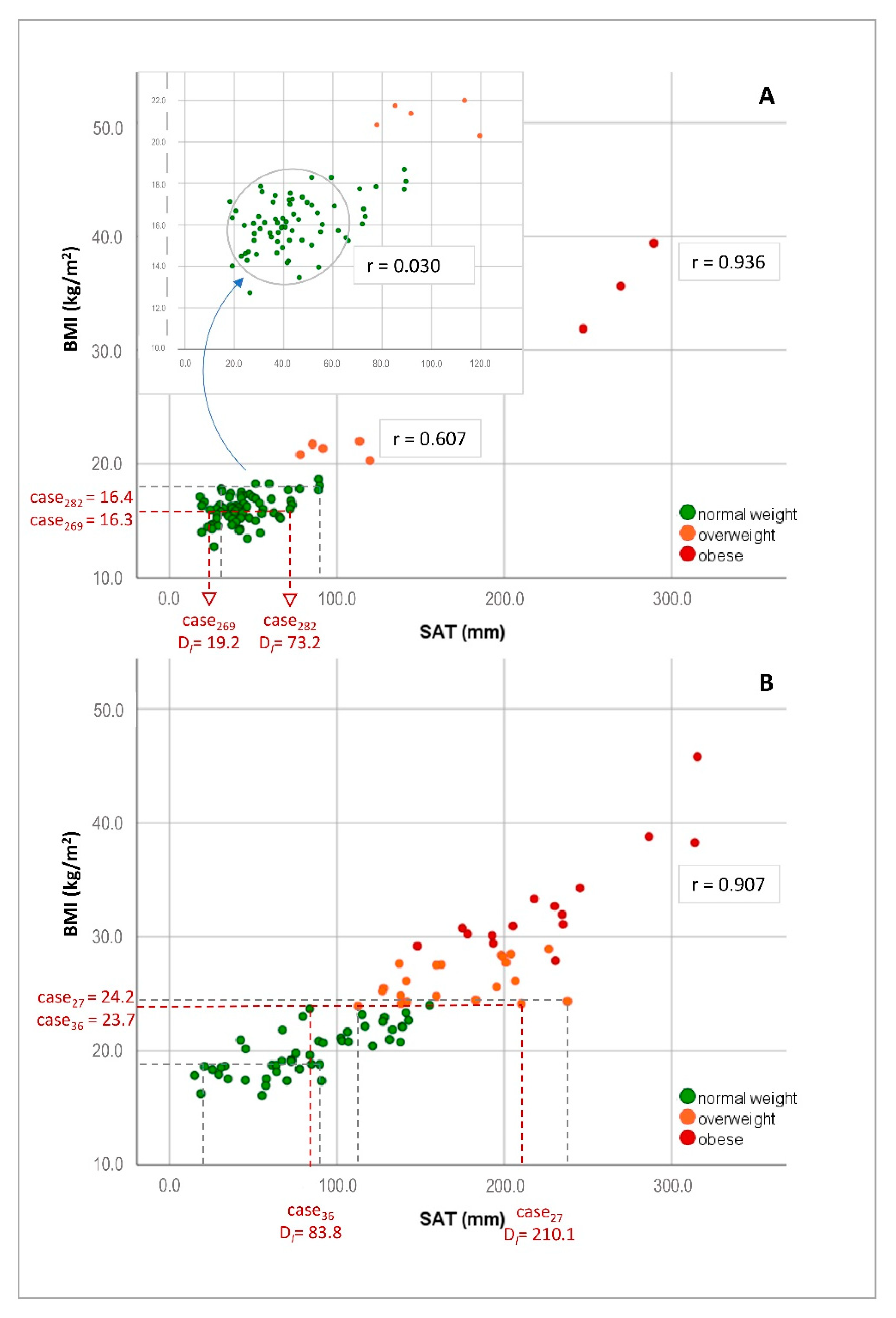
3.3. Correlation of Anthropometric Measures, Body Indices and SAT
3.4. Hemodynamic Measures and Subcutaneous Adipose Tissue
3.5. Estimation of SAT by Four- and Five-Site Measurements
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNIATF. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2017. [Google Scholar]
- UNICEF; WHO; The World Bank Group. Levels and Trends in Child Malnutrition: UNICEF-WHO-World Bank Joint Child Malnutrition Estimates. 2016. Available online: https://www.who.int/nutgrowthdb/jme_brochure2016.pdf?ua=1 (accessed on 1 September 2016).
- Farrag, N.S.; Cheskin, L.J.; Farag, M.K. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: Prevalence and risk factors meta-analysis. Adv. Pediatr. Res. 2017, 4, 4. [Google Scholar] [CrossRef]
- Rank, M.; Siegrist, M.; Wilks, D.C.; Langhof, H.; Wolfarth, B.; Haller, B.; Koenig, W.; Halle, M. The cardio-metabolic risk of moderate and severe obesity in children and adolescents. J. Pediatr. 2013, 163, 137–142. [Google Scholar] [CrossRef]
- Stabouli, S.; Kotsis, V.; Papamichael, C.; Constantopoulos, A.; Zakopoulos, N. Adolescent obesity is associated with high ambulatory blood pressure and increased carotid intimal-medial thickness. J. Pediatr. 2005, 147, 651–656. [Google Scholar] [CrossRef]
- Muthuri, S.K.; Francis, C.E.; Wachira, L.J.; Leblanc, A.G.; Sampson, M.; Onywera, V.O.; Tremblay, M.S. Evidence of an overweight/obesity transition among school-aged children and youth in Sub-Saharan Africa: A systematic review. PLoS ONE 2014, 9, e92846. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Shayo, F.K. Co-occurrence of risk factors for non-communicable diseases among in-school adolescents in Tanzania: An example of a low-income setting of sub-Saharan Africa for adolescence health policy actions. BMC Public Health 2019, 19, 972. [Google Scholar] [CrossRef] [PubMed]
- Okeyo, A.P.; Seekoe, E.; de Villiers, A.; Faber, M.; Nel, J.H.; Steyn, N.P. Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban-Rural and Gender Differences. Int. J. Environ. Res. Public Health 2020, 17, 5864. [Google Scholar] [CrossRef] [PubMed]
- Danquah, F.I.; Ansu-Mensah, M.; Bawontuo, V.; Yeboah, M.; Udoh, R.H.; Tahiru, M.; Kuupiel, D. Risk factors and morbidities associated with childhood obesity in sub-Saharan Africa: A systematic scoping review. BMC Nutr. 2020, 6, 37. [Google Scholar] [CrossRef]
- Wells, J.C.; Fewtrell, M.S. Measuring body composition. Arch. Dis. Child. 2006, 91, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Javed, A.; Jumean, M.; Murad, M.H.; Okorodudu, D.; Kumar, S.; Somers, V.K.; Sochor, O.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: A systematic review and meta-analysis. Pediatr. Obes. 2015, 10, 234–244. [Google Scholar] [CrossRef]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Jayawardena, R.; Gamage, N.; Pujitha Wickramasinghe, V.; Hills, A.P. The range of non-traditional anthropometric parameters to define obesity and obesity-related disease in children: A systematic review. Eur. J. Clin. Nutr. 2021, 75, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Vanderwall, C.; Randall Clark, R.; Eickhoff, J.; Carrel, A.L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 2017, 17, 135. [Google Scholar] [CrossRef] [PubMed]
- Adom, T.; Kengne, A.P.; De Villiers, A.; Boatin, R.; Puoane, T. Diagnostic Accuracy of Body Mass Index in Defining Childhood Obesity: Analysis of Cross-Sectional Data from Ghanaian Children. Int. J. Environ. Res. Public Health 2019, 17, 36. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008, 32, S56–S59. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, V.P.; Cleghorn, G.J.; Edmiston, K.A.; Murphy, A.J.; Abbott, R.A.; Davies, P.S. Validity of BMI as a measure of obesity in Australian white Caucasian and Australian Sri Lankan children. Ann. Hum. Biol. 2005, 32, 60–71. [Google Scholar] [CrossRef]
- Delisle Nyström, C.; Henriksson, P.; Ek, A.; Henriksson, H.; Ortega, F.B.; Ruiz, J.R.; Löf, M. Is BMI a relevant marker of fat mass in 4 year old children? Results from the MINISTOP trial. Eur. J. Clin. Nutr. 2018, 72, 1561–1566. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Committee. Physical Status: The Use and Interpretation of Anthropometry; WHO Technical Report Series; WHO: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Jensen, N.S.; Camargo, T.F.; Bergamaschi, D.P. Comparison of methods to measure body fat in 7-to-10-year-old children: A systematic review. Public Health 2016, 133, 3–13. [Google Scholar] [CrossRef]
- Fredriksen, P.M.; Hjelle, O.P.; Mamen, A.; Meza, T.J.; Westerberg, A.C. The health Oriented pedagogical project (HOPP)—A controlled longitudinal school-based physical activity intervention program. BMC Public Health 2017, 17, 370. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.R.; Leonard, M.B.; Zemel, B.S. Body composition analysis in the pediatric population. Pediatr. Endocrinol. Rev. 2012, 10, 130–139. [Google Scholar]
- Lichtenauer, M.; Wheatley, S.D.; Martyn-St James, M.; Duncan, M.J.; Cobayashi, F.; Berg, G.; Musso, C.; Graffigna, M.; Soutelo, J.; Bovet, P.; et al. Efficacy of anthropometric measures for identifying cardiovascular disease risk in adolescents: Review and meta-analysis. Minerva Pediatr. 2018, 70, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Wang, R.; Liu, Y.; Lu, Q.; Lu, N.; Tian, Y.; Liu, X.; Yin, F. Performance of obesity indices for screening elevated blood pressure in pediatric population: Systematic review and meta-analysis. Medicine 2016, 95, e4811. [Google Scholar] [CrossRef]
- Simoni, P.; Guglielmi, R.; Aparisi Gómez, M.P. Imaging of body composition in children. Quant. Imaging Med. Surg. 2020, 10, 1661–1671. [Google Scholar] [CrossRef]
- Kelso, A.; Vogel, K.; Steinacker, J.M. Ultrasound measurements of subcutaneous adipose tissue thickness show sexual dimorphism in children of three to five years of age. Acta Paediatr. 2019, 108, 514–521. [Google Scholar] [CrossRef]
- Müller, W.; Horn, M.; Fürhapter-Rieger, A.; Kainz, P.; Kröpfl, J.M.; Maughan, R.J.; Ahammer, H. Body composition in sport: A comparison of a novel ultrasound imaging technique to measure subcutaneous fat tissue compared with skinfold measurement. Br. J. Sports Med. 2013, 47, 1028–1035. [Google Scholar] [CrossRef]
- Müller, W.; Lohman, T.G.; Stewart, A.D.; Maughan, R.J.; Meyer, N.L.; Sardinha, L.B.; Kirihennedige, N.; Reguant-Closa, A.; Risoul-Salas, V.; Sundgot-Borgen, J.; et al. Subcutaneous fat patterning in athletes: Selection of appropriate sites and standardisation of a novel ultrasound measurement technique: Ad hoc working group on body composition, health and performance, under the auspices of the IOC Medical Commission. Br. J. Sports Med. 2016, 50, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Störchle, P.; Müller, W.; Sengeis, M.; Ahammer, H.; Fürhapter-Rieger, A.; Bachl, N.; Lackner, S.; Mörkl, S.; Holasek, S. Standardized Ultrasound Measurement of Subcutaneous Fat Patterning: High Reliability and Accuracy in Groups Ranging from Lean to Obese. Ultrasound Med. Biol. 2017, 43, 427–438. [Google Scholar] [CrossRef]
- Kelso, A.; Müller, W.; Fürhapter-Rieger, A.; Sengeis, M.; Ahammer, H.; Steinacker, J.M. High inter-observer reliability in standardized ultrasound measurements of subcutaneous adipose tissue in children aged three to six years. BMC Pediatr. 2020, 20, 145. [Google Scholar] [CrossRef]
- Müller, W.; Fürhapter-Rieger, A.; Ahammer, H.; Lohman, T.G.; Meyer, N.L.; Sardinha, L.B.; Stewart, A.D.; Maughan, R.J.; Sundgot-Borgen, J.; Müller, T.; et al. Relative Body Weight and Standardised Brightness-Mode Ultrasound Measurement of Subcutaneous Fat in Athletes: An International Multicentre Reliability Study, Under the Auspices of the IOC Medical Commission. Sports Med. 2020, 50, 597–614. [Google Scholar] [CrossRef] [PubMed]
- Wajchenberg, B.L. Subcutaneous and visceral adipose tissue: Their relation to the metabolic syndrome. Endocr. Rev. 2000, 21, 697–738. [Google Scholar] [CrossRef] [PubMed]
- Sengeis, M.; Müller, W.; Störchle, P.; Führhapter-Rieger, A. Body weight and subcutaneous fat patterning in elite judokas. Scand. J. Med. Sci. Sports 2019, 29, 1774–1788. [Google Scholar] [CrossRef]
- Ali, O.; Cerjak, D.; Kent, J.W.; James, R.; Blangero, J.; Zhang, Y. Obesity, central adiposity and cardiometabolic risk factors in children and adolescents: A family-based study. Pediatr. Obes. 2014, 9, e58–e62. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Fox, C.S.; Hickson, D.A.; May, W.D.; Hairston, K.G.; Carr, J.J.; Taylor, H.A. Impact of Abdominal Visceral and Subcutaneous Adipose Tissue on Cardiometabolic Risk Factors: The Jackson Heart Study. J. Clin. Endocrinol. Metab. 2010, 95, 5419–5426. [Google Scholar] [CrossRef]
- Kjellberg, E.; Roswall, J.; Andersson, J.; Bergman, S.; Karlsson, A.K.; Svensson, P.A.; Kullberg, J.; Dahlgren, J. Metabolic Risk Factors Associated with Visceral and Subcutaneous Adipose Tissue in a Sex-Specific Manner in Seven-Year-Olds. Obesity 2019, 27, 982–988. [Google Scholar] [CrossRef]
- Lee, J.J.; Pedley, A.; Therkelsen, K.E.; Hoffmann, U.; Massaro, J.M.; Levy, D.; Long, M.T. Upper Body Subcutaneous Fat Is Associated with Cardiometabolic Risk Factors. Am. J. Med. 2017, 130, 958–966.e1. [Google Scholar] [CrossRef]
- Yan, Y.; Liu, J.; Zhao, X.; Cheng, H.; Huang, G.; Mi, J. Abdominal visceral and subcutaneous adipose tissues in association with cardiometabolic risk in children and adolescents: The China Child and Adolescent Cardiovascular Health (CCACH) study. BMJ Open Diabetes Res. Care 2019, 7, e000824. [Google Scholar] [CrossRef]
- Kelly, A.S.; Dengel, D.R.; Hodges, J.; Zhang, L.; Moran, A.; Chow, L.; Sinaiko, A.R.; Steinberger, J. The relative contributions of the abdominal visceral and subcutaneous fat depots to cardiometabolic risk in youth. Clin. Obes. 2014, 4, 101–107. [Google Scholar] [CrossRef]
- González-Álvarez, C.; Ramos-Ibáñez, N.; Azprioz-Leehan, J.; Ortiz-Hernández, L. Intra-abdominal and subcutaneous abdominal fat as predictors of cardiometabolic risk in a sample of Mexican children. Eur. J. Clin. Nutr. 2017, 71, 1068–1073. [Google Scholar] [CrossRef]
- Matsha, T.E.; Ismail, S.; Speelman, A.; Hon, G.M.; Davids, S.; Erasmus, R.T.; Kengne, A.P. Visceral and subcutaneous adipose tissue association with metabolic syndrome and its components in a South African population. Clin. Nutr. ESPEN 2019, 32, 76–81. [Google Scholar] [CrossRef]
- Nazare, J.A.; Smith, J.D.; Borel, A.L.; Haffner, S.M.; Balkau, B.; Ross, R.; Massien, C.; Alméras, N.; Després, J.P. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: The International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am. J. Clin. Nutr. 2012, 96, 714–726. [Google Scholar] [CrossRef] [PubMed]
- Nkeh-Chungag, B.N.; Sekokotla, A.M.; Sewani-Rusike, C.; Namugowa, A.; Iputo, J.E. Prevalence of hypertension and pre-hypertension in 13–17 year old adolescents living in Mthatha—South Africa: A cross-sectional study. Cent. Eur. J. Public Health 2015, 23, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Letswalo, B.P.; Schmid-Zalaudek, K.; Brix, B.; Matjuda, E.N.; Klosz, F.; Obernhumer, N.; Gaisl, M.; Engwa, G.A.; Sewani-Rusike, C.; Fredriksen, P.M.; et al. Cardiometabolic risk factors and early indicators of vascular dysfunction: A cross-sectional cohort study in South African adolescents. BMJ Open 2021, 11, e042955. [Google Scholar] [CrossRef] [PubMed]
- Matjuda, E.N.; Engwa, G.A.; Anye, S.N.C.; Nkeh-Chungag, B.N.; Goswami, N. Cardiovascular Risk Factors and Their Relationship with Vascular Dysfunction in South African Children of African Ancestry. J. Clin. Med. 2021, 10, 354. [Google Scholar] [CrossRef] [PubMed]
- Noubiap, J.J.; Essouma, M.; Bigna, J.J.; Jingi, A.M.; Aminde, L.N.; Nansseu, J.R. Prevalence of elevated blood pressure in children and adolescents in Africa: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e375–e386. [Google Scholar] [CrossRef]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; De Ridder, J. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Wellington, New Zealand, 2011; Volume 137. [Google Scholar]
- Ryder, J.R.; Kaizer, A.M.; Rudser, K.D.; Daniels, S.R.; Kelly, A.S. Utility of Body Mass Index in Identifying Excess Adiposity in Youth Across the Obesity Spectrum. J. Pediatr. 2016, 177, 255–261.e2. [Google Scholar] [CrossRef]
- Melaku, Y.A.; Wassie, M.M.; Gill, T.K.; Zhou, S.J.; Tessema, G.A.; Amare, A.T.; Lakew, Y.; Hiruye, A.; Bekele, T.H.; Worku, A.; et al. Burden of disease attributable to suboptimal diet, metabolic risks and low physical activity in Ethiopia and comparison with Eastern sub-Saharan African countries, 1990–2015: Findings from the Global Burden of Disease Study 2015. BMC Public Health 2018, 18, 552. [Google Scholar] [CrossRef]
- Forkert, E.C.O.; Rendo-Urteaga, T.; Nascimento-Ferreira, M.V.; de Moraes, A.C.F.; Moreno, L.A.; de Carvalho, H.B. Abdominal obesity and cardiometabolic risk in children and adolescents, are we aware of their relevance? Nutrire 2016, 41, 15. [Google Scholar] [CrossRef]
- Micklesfield, L.K.; Hanson, S.K.; Lobelo, F.; Cunningham, S.A.; Hartman, T.J.; Norris, S.A.; Stein, A.D. Adolescent physical activity, sedentary behavior and sleep in relation to body composition at age 18 years in urban South Africa, Birth-to-Twenty+ Cohort. BMC Pediatr. 2021, 21, 30. [Google Scholar] [CrossRef]

| Girls (n = 50) | Boys (n = 23) | Total (n = 73) | |||
|---|---|---|---|---|---|
| mean ± SD | mean ± SD | mean ± SD (CI) | t (df) | p | |
| Age | 9.64 ± 0.94 | 9.78 ± 0.90 | 9.69 ± 0.93 (9.47, 9.01) | −0.609 (71) | 0.554 |
| Anthropometric measures | |||||
| body height (m) | 1.30 ± 0.07 | 1.31 ± 0.07 | 1.31 ± 0.07 (1.29, 1.33) | −0.704 (71) | 0.483 |
| body weight (kg) | 28.4 ± 5.1 | 28.2 ± 4.8 | 28.3 ± 5.02 (27.2, 29.5) | 0.181 (71) | 0.857 |
| sitting height (m) | 0.683 ± 0.03 | 0.683 ± 0.03 | 0.683 ± 0.03 (0.675, 0.690) | −0.022 (71) | 0.983 |
| leg length (m) | 0.726 ± 0.05 | 0.739 ± 0.04 | 0.729 ± 0.05 (0.719, 0.741) | −0.872 (71) | 0.386 |
| F (1) | p | ||||
| neck circumference (cm) | 26.4 ± 1.79 | 26.2 ± 1.75 | 26.3 ± 1.77 (25.9, 26.7) | 0.087 | 0.769 |
| chest circumference (cm) | 61.5 ± 4.38 | 60.4 ± 3.34 | 61.2 ± 4.11 (60.2, 62.2) | 1.073 | 0.304 |
| mid-upper arm circ. (cm) | 20.7 ± 2.37 | 19.2 ± 2.52 | 20.3 ± 2.50 (19.7, 20.9) | 5.739 | 0.019 |
| waist circumference (cm) | 58.1 ± 5.42 | 56.4 ± 3.49 | 57.6 ± 4.96 (56.4, 58.8) | 1.676 | 0.200 |
| hip circumference (cm) | 68.8 ± 5.07 | 66.3 ± 5.29 | 68.1 ± 5.23 (66.9, 69.3) | 3.517 | 0.065 |
| thigh circumference (cm) | 36.7 ± 3.33 | 33.9 ± 3.88 | 35.9 ± 3.71 (35.0, 36.7) | 9.899 | 0.002 |
| calf circumference (cm) | 26.3 ± 2.72 | 25.5 ± 2.26 | 26.1 ± 2.60 (25.5, 26.7) | 1.721 | 0.194 |
| ankle circumference (cm) | 20.5 ± 1.53 | 20.7 ± 1.90 | 20.5 ± 1.64 (20.2, 20.9) | 0.301 | 0.585 |
| Body indices | t (df) | p | |||
| BMI (kg/m2) | 16.55 ± 1.84 | 16.14 ± 1.71 | 16.42 ± 1.79 (16.0, 16.8) | 0.905 (71) | 0.369 |
| MI (0.53 m/(hs)) | 17.05 ± 1.95 | 16.88 ± 2.56 | 16.99 ± 2.15 (16.5, 17.5) | 0.313 (71) | 0.755 |
| Cormic index | 0.523 ± 0.016 | 0.518 ± 0.009 | 0.522 ± 0.014 (.519, 0.525) | 1.425 (71) | 0.158 |
| WHt ratio (m) | 0.423 ± 0.034 | 0.427 ± 0.024 | 0.424 ± 0.031 (.417, 0.431) | −0.582 (71) | 0.563 |
| SAT measures (in mm) | F (1, 73) | p | |||
| upper abdomen (UA) | 5.03 ± 4.03 | 2.83 ± 2.57 | 4.29 ± 3.73 (3.40, 5.18) | 5.782 | 0.019 |
| lower abdomen (LA) | 8.67 ± 5.07 | 5.67 ± 3.72 | 7.70 ± 4.87 (6.54, 8.64) | 6.441 | 0.013 |
| front thigh (FT) | 7.29 ± 2.21 | 5.21 ± 1.90 | 6.64 ± 2.30 (6.09, 7.19) | 15.269 | <0.001 |
| lateral thigh (LT) | 13.49 ± 4.94 | 7.71 ± 3.63 | 11.62 ± 5.28 (10.36, 12.88) | 25.180 | <0.001 |
| medial calf (MC) | 5.62 ± 2.22 | 3.72 ± 1.56 | 5.01 ± 2.19 (4.49, 5.54) | 13.726 | <0.001 |
| erector spinae (ES) | 3.81 ± 2.72 | 1.86 ± 1.33 | 3.13 ± 2.43 (2.55, 3.71) | 10.565 | 0.002 |
| distal triceps (DT) | 6.87 ± 2.12 | 5.27 ± 1.88 | 6.36 ± 2.16 (5.85, 6.88) | 9.624 | 0.003 |
| brachioradialis (BR) | 3.23 ± 1.38 | 2.15 ± 1.00 | 2.89 ± 1.37 (2.57, 3.22) | 11.338 | 0.001 |
| t (df) | p | ||||
| DI | 54.02 ± 21.71 | 34.42 ± 15.84 | 47.65 ± 21.7 (42.5, 52.8) | 3.875 (71) | <0.001 |
| DE | 49.54 ± 20.90 | 30.46 ± 15.13 | 43.30 ± 20.8 (38.3, 48.3) | 3.924 (71) | <0.001 |
| Fibers | 4.48 ± 1.53 | 3.96 ± 1.36 | 4.34 ± 1.5 (3.9, 4.7) | 1.393 (71) | 0.168 |
| SAT (kg) | 4.15 ± 1.56 | 2.96 ± 1.33 | 3.79 ± 1.59 (3.41, 4.17) | 3.045 (71) | 0.003 |
| SAT (%) | 14.44 ± 3.55 | 10.36 ± 2.89 | 13.21 ± 3.84 (12.3, 14.1) | 4.646 (71) | <0.001 |
| Girls (n = 66) | Boys (n = 19) | Total (n = 85) | |||
|---|---|---|---|---|---|
| mean ± SD | mean ± SD | mean ± SD (CI) | t (df) | p | |
| Age | 15.05 ± 0.92 | 14.58 ± 1.12 | 14.89 ± 0.97 (14.67, 15.10) | 1.854 (83) | 0.067 |
| Anthropometric measures | |||||
| body height (m) | 1.57 ± 0.05 | 1.60 ± 0.09 | 1.58 ± 0.06 (1.56, 1.59) | −2.012 (83) | 0.048 |
| body weight (kg) | 59.7 ± 13.1 | 55.6 ± 17.4 | 58.6 ± 14.0 (55.5, 61.7) | 1.111 (83) | 0.270 |
| sitting height (m) | 0.800 ± 0.04 | 0.801 ± 0.05 | 0.80 ± 0.04 (.792, 0.809) | −0.088 (83) | 0.930 |
| leg length (m) | 0.022 ± 0.05 | 0.912 ± 0.08 | 0.920 ± 0.05 (.908, 0.932) | 0.476 (83) | 0.4766 |
| F (1, 80) | p | ||||
| neck circumference (cm) | 31.0 ± 1.81 | 32.2 ± 3.08 | 31.3 ± 2.22 (30.8, 31.8) | 4.776 | 0.032 |
| chest circumference (cm) | 85.5 ± 9.59 | 79.3 ± 12.64 | 84.1 ± 10.6 (81.7, 86.4) | 5.131 | 0.026 |
| mid-upper arm circ. (cm) | 26.6 ± 3.97 | 25.4 ± 4.97 | 26.3 ± 4.22 (25.4, 27.3) | 1.138 | 0.289 |
| waist circumference (cm) | 73.2 ± 9.52 | 73.4 ± 16.01 | 73.2 ± 11.3 (70.7, 75.7) | 0.008 | 0.928 |
| hip circumference (cm) | 100.7 ± 9.99 | 91.0 ± 14.77 | 98.5 ± 11.9 (95.8, 101.1) | 10.866 | 0.001 |
| thigh circumference (cm) | 52.2 ± 6.92 | 51.1 ± 10.53 | 52.0 ± 7.84 (50.2, 53.7) | 0.319 | 0.574 |
| calf circumference (cm) | 35.6 ± 4.05 | 33.9 ± 5.05 | 35.2 ± 4.34 (34.3, 36.2) | 2.515 | 0.117 |
| ankle circumference (cm) | 23.3 ± 2.17 | 23.2 ± 2.63 | 23.3 ± 2.27 (22.8, 23.8) | 0.055 | 0.815 |
| Body indices | t (df) | p | |||
| BMI (kg/m2) | 24.11 ± 4.98 | 21.38 ± 5.12 | 23.41 ± 5.08 (22.3, 24.5) | 2.096 (83) | 0.039 |
| MI (0.53 m/(hs)) | 25.04 ± 5.13 | 22.64 ± 5.13 | 24.49 ± 5.19 (23.4, 25.6) | 1.795 (83) | 0.076 |
| Cormic index | 0.510 ± 0.023 | 0.500 ± 0.013 | 0.507 ± 0.021 (0.503, 0.512) | 1.840 (83) | 0.069 |
| WHt ratio (m) | 0.469 ± 0.067 | 0.458 ± 0.092 | 0.466 ± 0.073 (0.451, 0.482) | 0.602 (83) | 0.549 |
| SAT measures (in mm) | F (1, 73) | p | |||
| upper abdomen (UA) | 21.07 ± 13.68 | 9.69 ± 13.22 | 18.74 ± 14.3 (15.6, 21.9) | 9.483 | 0.003 |
| lower abdomen (LA) | 29.38 ± 15.66 | 14.58 ± 17.72 | 26.35 ± 17.1 (22.6, 30.1) | 11.433 | 0.001 |
| front thigh (FT) | 15.43 ± 5.52 | 8.41 ± 6.60 | 13.99 ± 6.39 (12.6, 15.4) | 20.134 | <0.001 |
| lateral thigh (LT) | 32.67 ± 12.84 | 15.97 ± 14.40 | 29.25 ± 14.7 (26.0, 32.5) | 21.734 | <0.001 |
| medial calf (MC) | 11.74 ± 4.58 | 5.96 ± 3.55 | 10.55 ± 4.96 (9.5, 11.6) | 23.364 | <0.001 |
| erector spinae (ES) | 13.19 ± 7.36 | 5.84 ± 3.55 | 11.68 ± 7.69 (10.0, 13.4) | 14.338 | <0.001 |
| distal triceps (DT) | 11.08 ± 4.57 | 6.43 ± 5.70 | 10.13 ± 5.14 (9.0, 11.3) | 12.608 | 0.001 |
| brachioradialis (BR) | 6.32 ± 2.48 | 3.26 ± 2.51 | 5.69 ± 2.76 (5.1, 6.3) | 20.363 | <0.001 |
| t (df) | p | ||||
| DI | 140.86 ± 59.4 | 79.48 ± 75.6 | 127.14 ± 67.2 (112.5, 141.8) | 3.727 (83) | <0.001 |
| DE | 134.19 ± 58.5 | 72.73 ± 72.4 | 119.84 ± 66.1 (105.4, 134.3) | 3.821 (83) | <0.001 |
| Fibers | 6.66 ± 2.3 | 6.75 ± 3.6 | 6.54 ± 2.4 (6.0, 7.1) | −0.135 (83) | 0.893 |
| SAT (kg) | 13.13 ± 5.31 | 8.17 ± 7.06 | 11.89 ± 5.86 (10.6, 13.2) | 3.317 (83) | 0.001 |
| SAT (%) | 21.25 ± 4.50 | 13.16 ± 739 | 19.43 ± 6.25 (18.1, 20.8) | 5.910 (83) | <0.001 |
| BMI Children | <85th pc | ≥85th < 95th pc | ≥95th | Total | |
|---|---|---|---|---|---|
| Girls | 46 (88.5%) | 4 (7.7%) | 2 (3.8%) | 52 (100%) | |
| Boys | 22 (91.7%) | 1 (4.2%) | 1 (4.2%) | 24 (100%) | |
| Total children | 68 (89.5%) | 5 (6.6%) | 3 (3.9%) | 76 (100%) | |
| mean ± SD | mean ± SD | t (df) | p | ||
| SBP | 111 ± 13.0 | 136 ± 25.6 | −2.725 (7.4) | 0.028 | |
| DBP | 69 ± 8.3 | 83 ± 17.1 | −2.271 (7.4) | 0.055 | |
| HR | 86 ± 11.2 | 85 ± 6.6 | 0.228 (71) | 0.820 | |
| DI | 44.2 ± 17.3 | 161.8 ± 90.3 | −3.674 (7.1) | 0.008 | |
| DE | 40.1 ± 16.9 | 154.5 ± 89.6 | −3.607 (7.1) | 0.009 | |
| Fibers | 4.12 ± 1.13 | 7.22 ± 2.5 | −3.530 (7.4) | 0.009 | |
| SAT kg | 3.48 ± 1.11 | 13.09 ±7.5 | −3.643 (7.0) | 0.008 | |
| SAT % | 12.7 ± 3.5 | 23.68 ± 6.4 | −4.737 (7.5) | 0.002 | |
| correlations | SBP | DBP | HR | ||
| DI | 0.550 ** | 0.402 ** | −0.013 | ||
| DE | 0.548 ** | 0.400 ** | −0.009 | ||
| Fibers | 0.380 ** | 0.298 ** | −0.129 | ||
| BMI Adolescents | <85th pc | ≥85th < 95th pc | ≥95th | Total | |
|---|---|---|---|---|---|
| Girls | 36 (54.5%) | 19 (28.8%) | 11 (16.7%) | 66 (100%) | |
| Boys | 14 (70.0%) | 2 (10.0%) | 4 (20.0%) | 20 (100%) | |
| Total adolescents | 50 (51.8%) | 21 (24.4%) | 15 (17.4%) | 86 (100%) | |
| mean ± SD | mean ± SD | mean ± SD | F (df) | p | |
| SBP | 113 ± 8.2 | 124 ± 14.1 | 126 ± 11.1 | 14.043 | <0.001 |
| DBP | 66 ± 6.9 | 68 ± 11.2 | 70 ± 8.1 | 1.533 | 0.222 |
| HR | 80 ± 11.7 | 77 ± 8.3 | 80 ± 7.9 | 0.929 | 0.399 |
| DI | 82.3 ± 38.2 | 171.7 ± 36.8 | 226.7 ±49.0 | 91.399 | <0.001 |
| DE | 76.7 ± 37.5 | 163.6 ± 36.7 | 217.6 ± 48.0 | 89.514 | <0.001 |
| Fibers | 5.5 ± 1.5 | 8.2 ± 2.9 | 9.1 ± 4.0 | 16.348 | <0.001 |
| SAT kg | 8.02 ± 3.1 | 15.6 ± 3.0 | 21.9 ± 5.5 | 96.301 | <0.001 |
| SAT % | 15.8 ± 5.1 | 23.8 ± 3.2 | 26.1 ± 2.8 | 45.10 | <0.001 |
| correlations | SBP | DBP | HR | ||
| DI | 0.534 ** | 0.262 * | 0.040 | ||
| DE | 0.525 ** | 0.252 * | 0.042 | ||
| Fibers | 0.528 ** | 0.371 ** | −0.020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmid-Zalaudek, K.; Brix, B.; Sengeis, M.; Jantscher, A.; Fürhapter-Rieger, A.; Müller, W.; Matjuda, E.N.; Mungamba, M.M.; Nkeh-Chungag, B.; Fredriksen, P.M.; et al. Subcutaneous Adipose Tissue Measured by B-Mode Ultrasound to Assess and Monitor Obesity and Cardio–Metabolic Risk in Children and Adolescents. Biology 2021, 10, 449. https://doi.org/10.3390/biology10050449
Schmid-Zalaudek K, Brix B, Sengeis M, Jantscher A, Fürhapter-Rieger A, Müller W, Matjuda EN, Mungamba MM, Nkeh-Chungag B, Fredriksen PM, et al. Subcutaneous Adipose Tissue Measured by B-Mode Ultrasound to Assess and Monitor Obesity and Cardio–Metabolic Risk in Children and Adolescents. Biology. 2021; 10(5):449. https://doi.org/10.3390/biology10050449
Chicago/Turabian StyleSchmid-Zalaudek, Karin, Bianca Brix, Marietta Sengeis, Andreas Jantscher, Alfred Fürhapter-Rieger, Wolfram Müller, Edna N. Matjuda, Muhau M. Mungamba, Benedicta Nkeh-Chungag, Per Morten Fredriksen, and et al. 2021. "Subcutaneous Adipose Tissue Measured by B-Mode Ultrasound to Assess and Monitor Obesity and Cardio–Metabolic Risk in Children and Adolescents" Biology 10, no. 5: 449. https://doi.org/10.3390/biology10050449
APA StyleSchmid-Zalaudek, K., Brix, B., Sengeis, M., Jantscher, A., Fürhapter-Rieger, A., Müller, W., Matjuda, E. N., Mungamba, M. M., Nkeh-Chungag, B., Fredriksen, P. M., & Goswami, N. (2021). Subcutaneous Adipose Tissue Measured by B-Mode Ultrasound to Assess and Monitor Obesity and Cardio–Metabolic Risk in Children and Adolescents. Biology, 10(5), 449. https://doi.org/10.3390/biology10050449






