Drug Repurposing Approach against Novel Coronavirus Disease (COVID-19) through Virtual Screening Targeting SARS-CoV-2 Main Protease
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Sequence Comparison
2.2. Protein Preparation
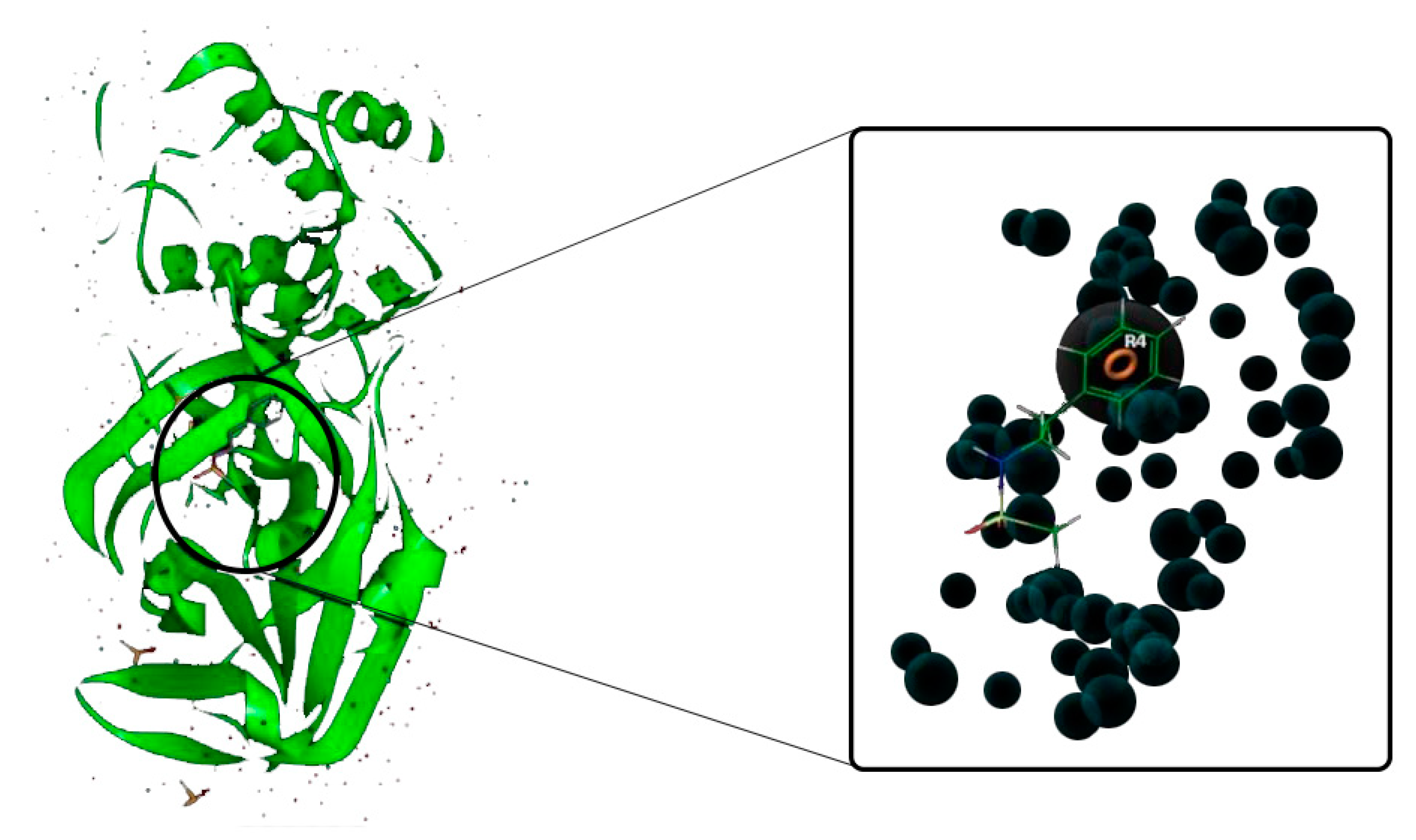
2.3. Generation of E-Pharmacophore Hypothesis
2.4. Virtual Screening using E-Pharmacophore Hypothesis
2.5. Ligand Preparation
2.6. Virtual Screening Based on Molecular Docking
2.7. MM/GBSA and Interaction Analysis
2.8. Molecular Dynamics Simulations
3. Results and Discussion
3.1. Sequence Comparison
3.2. The E-Pharmacophore Hypothesis
3.3. Virtual Screening Using E-Pharmacophore Hypothesis
3.4. Virtual Screening Based on Molecular Docking
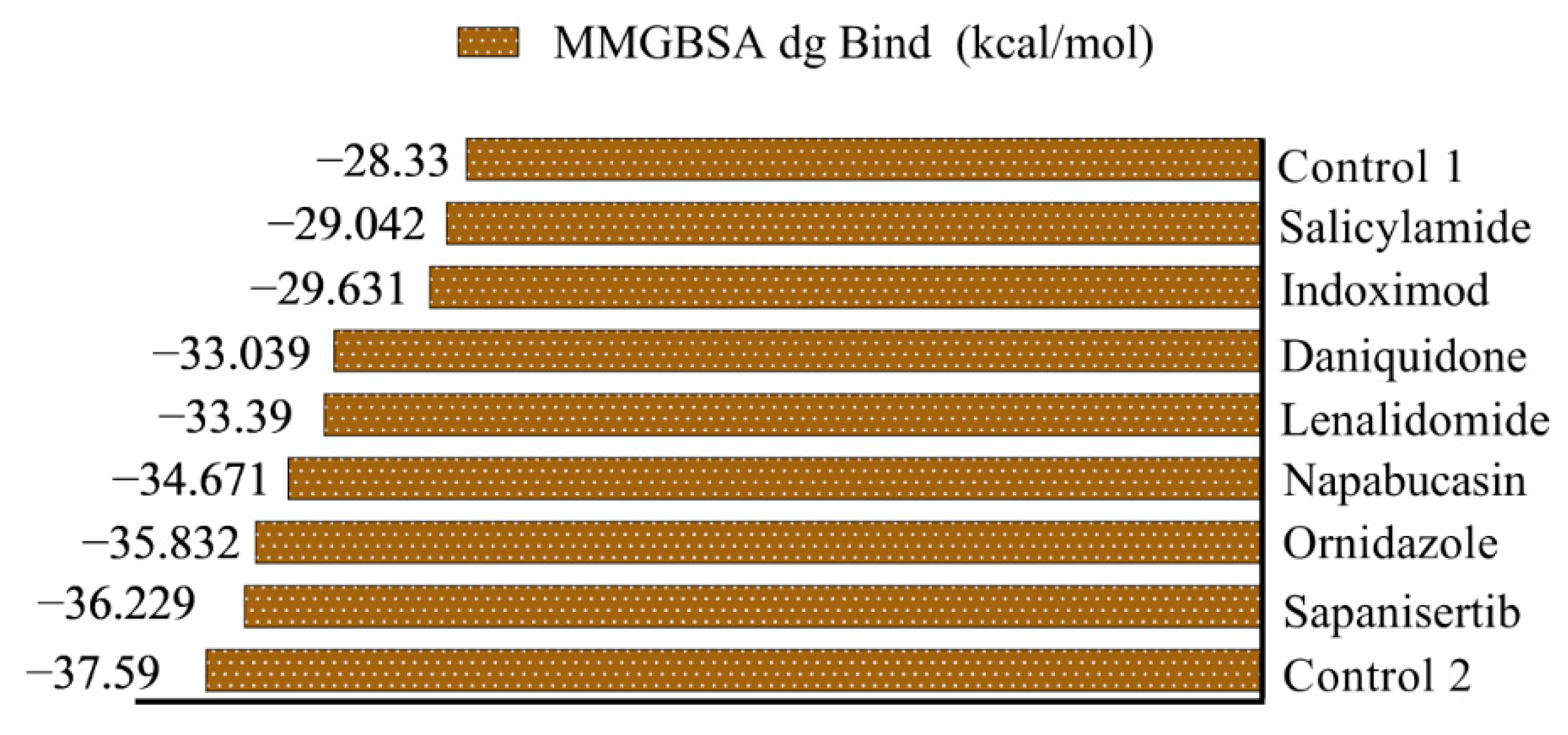
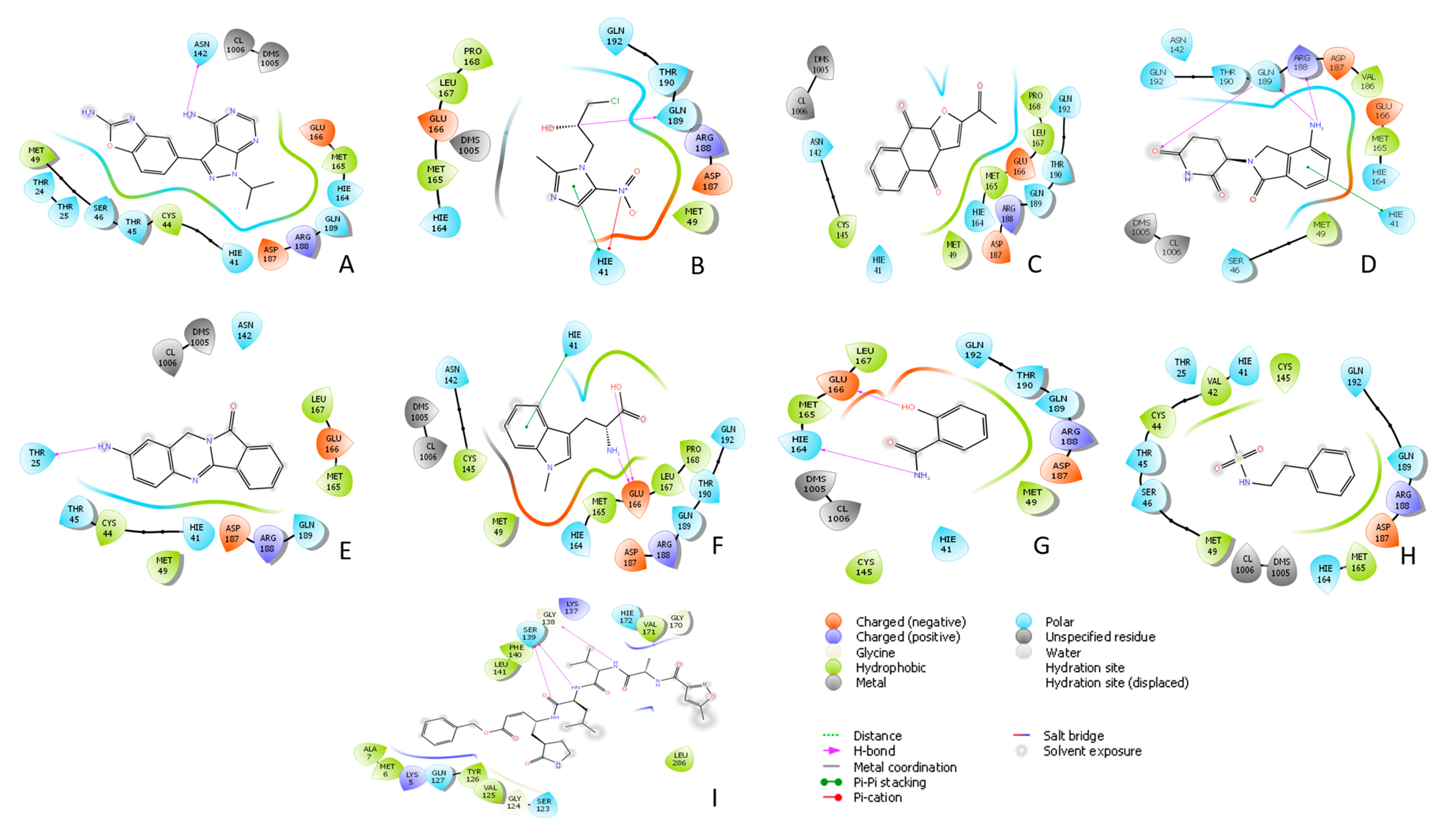
3.5. MM/GBSA and Interaction Analysis
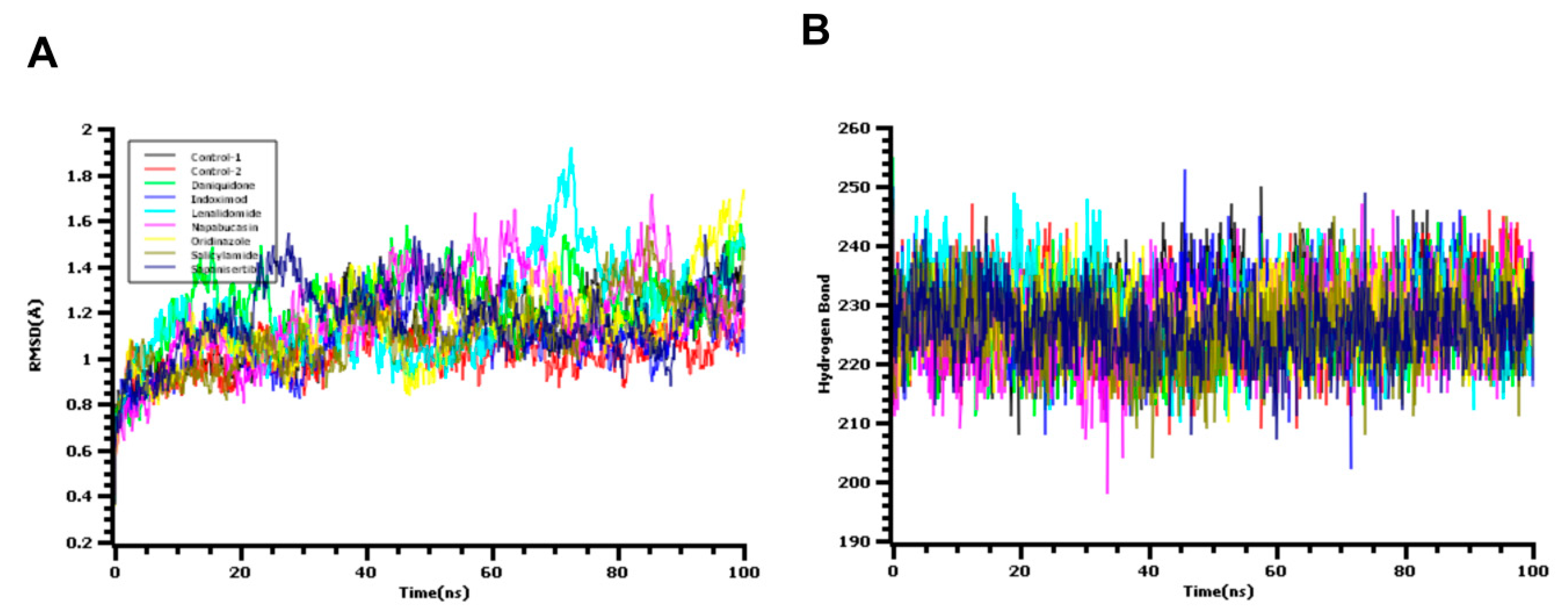
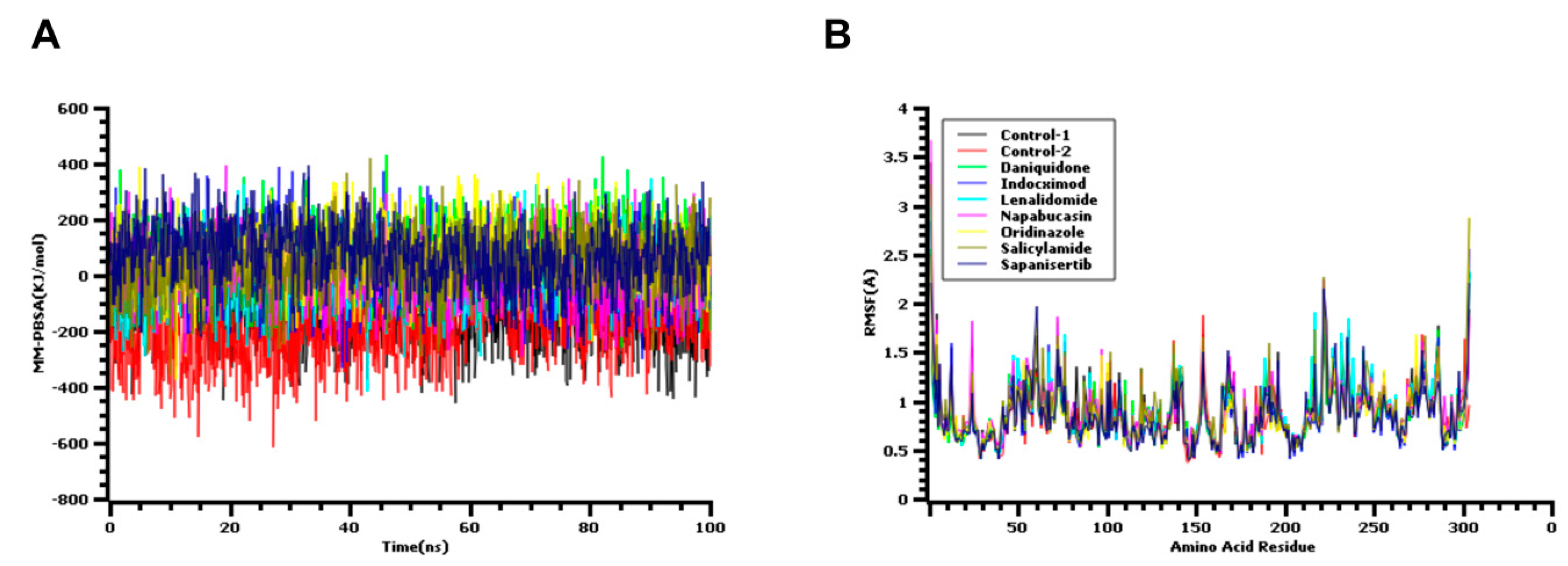
3.6. Molecular Dynamics Simulations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jin, Y.; Yang, H.; Ji, W.; Wu, W.; Chen, S.; Zhang, W.; Duan, G. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses 2020, 12, 372. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Update (Live): 12,250,111 Cases and 553,972 Deaths from COVID-19 Virus Pandemic-Worldometer. Available online: https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1 (accessed on 9 August 2020).
- Júnior, J.A.C.N.; Santos, A.M.; Quintans-Júnior, L.J.; Walker, C.I.B.; Borges, L.P.; Serafini, M.R. SARS, MERS and SARS-CoV-2 (COVID-19) treatment: A patent review. Expert Opin. Ther. Pat. 2020, 30, 567–579. [Google Scholar] [CrossRef]
- Xu, J.; Zhao, S.; Teng, T.; Abdalla, A.E.; Zhu, W.; Xie, L.; Wang, Y.; Guo, X. Systematic Comparison of Two Animal-to-Human Transmitted Human Coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses 2020, 12, 244. [Google Scholar] [CrossRef] [PubMed]
- Shamsi, A.; Mohammad, T.; Anwar, S.; Alajmi, M.F.; Hussain, A.; Rehman, T.; Islam, A.; Hassan, I. Glecaprevir and Maraviroc are high-affinity inhibitors of SARS-CoV-2 main protease: Possible implication in COVID-19 therapy. Biosci. Rep. 2020, 40. [Google Scholar] [CrossRef] [PubMed]
- Singhal, T. A Review of Coronavirus Disease-2019 (COVID-19), Indian. J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef]
- Mittal, L.; Kumari, A.; Srivastava, M.; Singh, M.; Asthana, S. Identification of potential molecules against COVID-19 main protease through structure-guided virtual screening approach. J. Biomol. Struct. Dyn. 2020, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Kandeel, M.; Al-Nazawi, M. Virtual screening and repurposing of FDA approved drugs against COVID-19 main protease. Life Sci. 2020, 251, 117627. [Google Scholar] [CrossRef] [PubMed]
- Rakib, A.; Sami, S.A.; Islam, M.A.; Ahmed, S.; Faiz, F.B.; Khanam, B.H.; Marma, K.K.S.; Rahman, M.; Uddin, M.M.N.; Nainu, F.; et al. Epitope-Based Immunoinformatics Approach on Nucleocapsid Protein of Severe Acute Respiratory Syndrome-Coronavirus-2. Molecules 2020, 25, 5088. [Google Scholar] [CrossRef]
- Fearon, D.; Powell, A.; Douangamath, A.; Owen, C.; Wild, C.; Krojer, T.; Lukacik, P.; Strain-Damerell, C.; Walsh, M.; Von Delft, F. PanDDA Analysis of COVID-19 Main Protease against the DSI-Poised Fragment Library. PDB ID: 5R7Y. Available online: https://www.wwpdb.org/pdb?id=pdb_00005r82 (accessed on 24 February 2020).
- Xu, T.; Ooi, A.; Lee, H.C.; Wilmouth, R.; Liu, D.X.; Lescar, J. Structure of the SARS coronavirus main proteinase as an active C 2 crystallographic dimer, Acta Crystallogr. Sect. F Struct. Biol. Cryst. Commun. 2005, 61, 964–966. [Google Scholar] [CrossRef]
- Ho, B.-L.; Cheng, S.-C.; Shi, L.; Wang, T.-Y.; Ho, K.-I.; Chou, C.-Y. Critical Assessment of the Important Residues Involved in the Dimerization and Catalysis of MERS Coronavirus Main Protease. PLoS ONE 2015, 10, e0144865. [Google Scholar] [CrossRef]
- Kemmish, H.; Fasnacht, M.; Yan, L. Fully automated antibody structure prediction using BIOVIA tools: Validation study. PLoS ONE 2017, 12, e0177923. [Google Scholar] [CrossRef] [PubMed]
- Harder, E.; Damm, W.; Maple, J.R.; Wu, C.; Reboul, M.; Xiang, J.Y.; Wang, L.; Lupyan, D.; Dahlgren, M.K.; Knight, J.L.; et al. OPLS3: A Force Field Providing Broad Coverage of Drug-like Small Molecules and Proteins. J. Chem. Theory Comput. 2016, 12, 281–296. [Google Scholar] [CrossRef] [PubMed]
- Sastry, G.M.; Adzhigirey, M.; Day, T.; Annabhimoju, R.; Sherman, W. Protein and ligand preparation: Parameters, protocols, and influence on virtual screening enrichments. J. Comput. Aid. Mol. Des. 2013, 27, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Dixon, S.L.; Smondyrev, A.M.; Knoll, E.H.; Rao, S.N.; Shaw, D.E.; Friesner, R.A. PHASE: A new engine for pharmacophore perception, 3D QSAR model development, and 3D database screening: 1. Methodology and preliminary results. J. Comput. Aided. Mol. Des. 2006, 20, 647–671. [Google Scholar] [CrossRef]
- Wishart, D.S.; Feunang, Y.D.; Guo, A.C.; Lo, E.J.; Marcu, A.; Grant, J.R.; Assempour, N. DrugBank 5.0: A major update to the DrugBank database for 2018. Nucleic Acids Res. 2018, 46, 1077–1082. [Google Scholar] [CrossRef]
- Shelley, J.C.; Cholleti, A.; Frye, L.L.; Greenwood, J.R.; Timlin, M.R.; Uchimaya, M. Epik: A software program for pK(a) prediction and protonation state generation for drug-like molecules. J. Comput. Aided. Mol. Des. 2007, 21, 681–691. [Google Scholar] [CrossRef]
- Friesner, R.A.; Murphy, R.B.; Repasky, M.P.; Frye, L.L.; Greenwood, J.R.; Halgren, T.A.; Sanschagrin, P.C.; Mainz, D.T. Extra Precision Glide: Docking and Scoring Incorporating a Model of Hydrophobic Enclosure for Protein−Ligand Complexes. J. Med. Chem. 2006, 49, 6177–6196. [Google Scholar] [CrossRef]
- Rakib, A.; Paul, A.; Chy, M.N.U.; Sami, S.A.; Baral, S.K.; Majumder, M.; Tareq, A.M.; Amin, M.N.; Shahriar, A.; Uddin, M.Z.; et al. Biochemical and Computational Approach of Selected Phytocompounds from Tinospora crispa in the Management of COVID-19. Molecules 2020, 25, 3936. [Google Scholar] [CrossRef]
- Verma, P.; Tiwari, M.; Tiwari, V. In silico high-throughput virtual screening and molecular dynamics simulation study to identify inhibitor for AdeABC efflux pump of Acinetobacter baumannii. J. Biomol. Struct. Dyn. 2018, 36, 1182–1194. [Google Scholar] [CrossRef]
- Krieger, E.; Darden, T.; Nabuurs, S.B.; Finkelstein, A.; Vriend, G. Making optimal use of empirical energy functions: Force-field parameterization in crystal space. Proteins 2004, 57, 678–683. [Google Scholar] [CrossRef]
- Dickson, C.J.; Madej, B.D.; Åge, A.S.; Betz, R.M.; Teigen, K.; Gould, I.R.; Walker, R.C. Lipid14: The amber lipid force field. J. Chem. Theory Comput. 2014, 10, 865–879. [Google Scholar] [CrossRef] [PubMed]
- Krieger, E.; Vriend, G.; Spronk, C. YASARA–Yet Another Scientific Artificial Reality Application. 2013. Available online: http://yasara.org/ (accessed on 24 February 2020).
- Oany, A.R.; Mia, M.; Pervin, T.; Junaid, M.; Hosen, S.; Moni, M.A. Design of novel viral attachment inhibitors of the spike glycoprotein (S) of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) through virtual screening and dynamics. Int. J. Antimicrob. Agents. 2020, 56, 106177. [Google Scholar] [CrossRef] [PubMed]
- Rakib, A.; Sami, S.A.; Mimi, N.J.; Chowdhury, M.M.; Eva, T.A.; Nainu, F.; Paul, A.; Shahriar, A.; Tareq, A.M.; Emon, N.U.; et al. Immunoinformatics-guided design of an epitope-based vaccine against severe acute respiratory syndrome coronavirus 2 spike glycoprotein. Comput. Biol. Med. 2020, 124, 103967. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Mahmud, S.; Sultana, R.; Dong, W. Identification and in silico molecular modelling study of newly isolated Bacillus subtilis SI-18 strain against S9 protein of Rhizoctonia solani. Arab. J. Chem. 2020, 13, 8600–8612. [Google Scholar] [CrossRef]
- Kumar, Y.; Singh, H.; Patel, C.N. In silico prediction of potential inhibitors for the main protease of SARS-CoV-2 using molecular docking and dynamics simulation based drug-repurposing. J. Infect. Public Health 2020, 13, 1210–1223. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, D.; Sun, X.; Curth, U.; Drosten, C.; Sauerhering, L.; Becker, S.; Rox, K.; Hilgenfeld, R. Crystal structure of SARS-CoV-2 main protease provides a basis for design of improved a-ketoamide inhibitors. Science 2020, 368, 409–412. [Google Scholar] [CrossRef]
- Ganser, L.R.; Lee, J.; Rangadurai, A.; Merriman, D.K.; Kelly, M.L.; Kansal, A.D.; Sathyamoorthy, B.; Al-Hashimi, H.M. High-performance virtual screening by targeting a high-resolution RNA dynamic ensemble. Nat. Struct. Mol. Biol. 2018, 25, 425–434. [Google Scholar] [CrossRef]
- Perez-Sanchez, H.; Lightstone, F.C. A Comprehensive Docking and MM/GBSA Rescoring Study of Ligand Recognition upon Binding Antithrombin. Curr. Top. Med. Chem. 2017, 17, 1631–1639. [Google Scholar] [CrossRef]
- Guo, N.; Azadniv, M.; Coppage, M.; Nemer, M.; Mendler, J.; Becker, M.; Liesveld, J. Effects of Neddylation and mTOR Inhibition in Acute Myelogenous Leukemia. Transl. Oncol. 2019, 12, 602–613. [Google Scholar] [CrossRef]
- Hubbard, J.M.; Grothey, A. Napabucasin: An Update on the First-in-Class Cancer Stemness Inhibitor. Drugs 2017, 77, 1091–1103. [Google Scholar] [CrossRef]
- NCI Thesaurus. National Cancer Institute. Available online: https://datascience.cancer.gov/ (accessed on 21 August 2020).
- Zeldis, J.B.; Knight, R.; Hussein, M.; Chopra, R.; Muller, G. A review of the history, properties, and use of the immunomodulatory compound lenalidomide. Ann. N. Y. Acad. Sci. 2011, 1222, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Choudhuri, G.; Rangan, M. Amebic infection in humans. Indian J. Gastroenterol. 2012, 31, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Fox, E.; Oliver, T.; Rowe, M.; Thomas, S.; Zakharia, Y.; Gilman, P.B.; Muller, A.J.; Prendergast, G.C. Indoximod: An immunometabolic adjuvant that empowers T cell activity in cancer. Front. Oncol. 2018, 8, 370. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, C.J.; Ciolino, H.P.; Yeh, G.C. The Drug Salicylamide Is an Antagonist of the Aryl Hydrocarbon Receptor That Inhibits Signal Transduction Induced by 2,3,7,8-Tetrachlorodibenzo-p-dioxin. Cancer Res. 2004, 64, 429–434. [Google Scholar] [CrossRef]
- Dror, R.O.; Dirks, R.M.; Grossman, J.; Xu, H.; Shaw, D.E. Biomolecular simulation: A computational microscope for molecular biology. Annu. Rev. Biophys. 2012, 41, 429–452. [Google Scholar] [CrossRef]
- Salmaso, V.; Moro, S. Bridging molecular docking to molecular dynamics in exploring ligand-protein recognition process: An overview. Front. Pharmacol. 2018, 9, 923. [Google Scholar] [CrossRef]
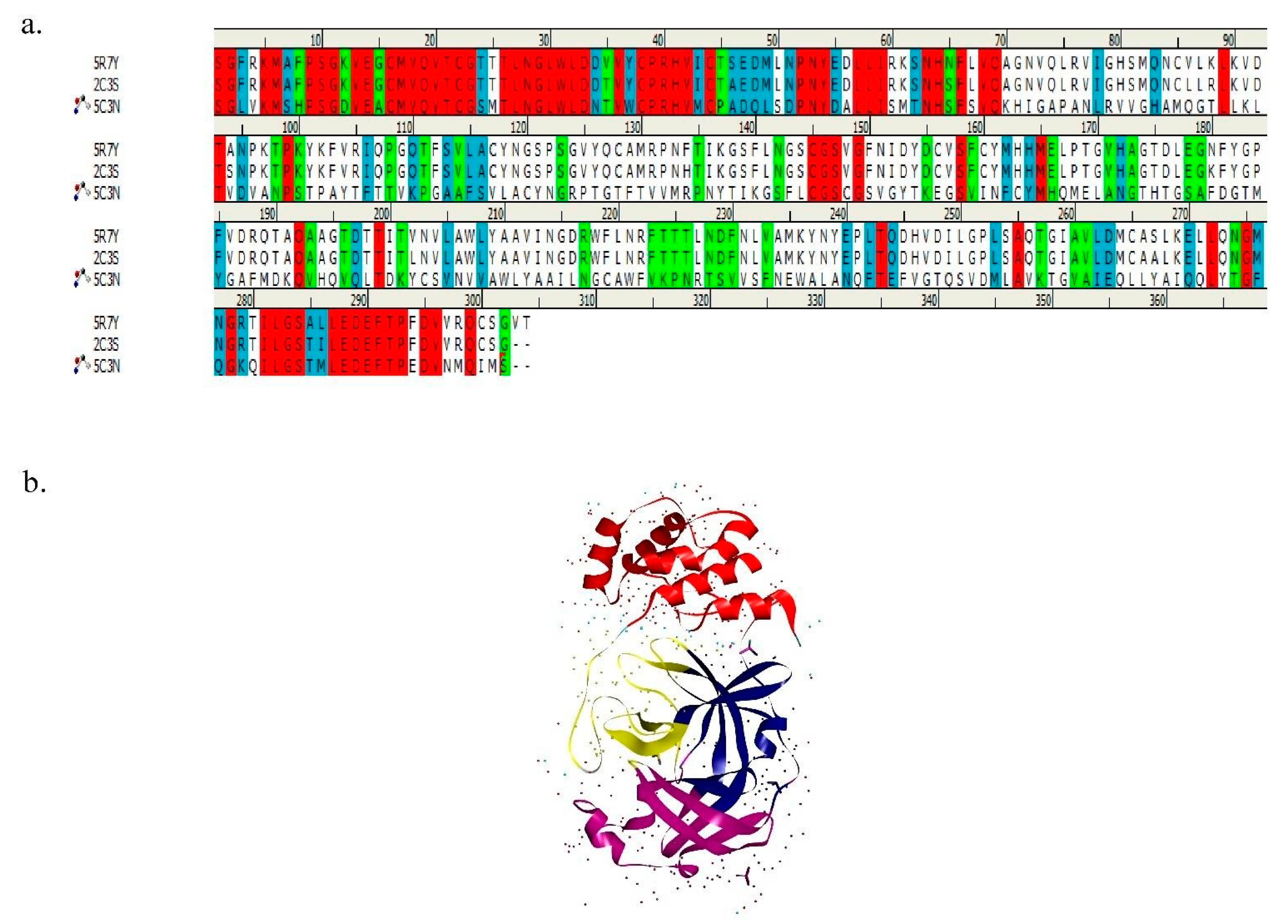
| Sequence Name | 5R7Y | 2C3S | 5C3N |
|---|---|---|---|
| 5R7Y | 100 | 96 | 24.2 |
| 2C3S | 96 | 100 | 25.5 |
| 5C3N | 24.2 | 25.5 | 100 |
| Drug Bank ID | Drug Name | Group | Category | Docking Score (kcal/mol) |
|---|---|---|---|---|
| DB08797 | Salicylamide | Approved | Analgesic | −7.10 |
| DB13026 | Ornidazole | Investigational | Antibiotic | −6.67 |
| DB14575 | Eslicarbazepine | Approved | Anticonvulsants. | −6.56 |
| DB14855 | 2-(aminomethyl)phenol | Investigational | Benzene Derivatives | −6.52 |
| DB13136 | Fluindione | Approved | Anticoagulants | −6.34 |
| DB04571 | Trioxsalen | Approved | Vitiligo | −6.34 |
| DB02262 | Orotic acid | Investigational | Pyrimidines | −6.29 |
| DB12155 | Napabucasin | Investigational | Anticancer | −6.25 |
| DB11836 | Sapanisertib | Investigational | Anticancer | −6.24 |
| DB12804 | Daniquidone | Investigational | Anticancer | −6.13 |
| DB00368 | Norepinephrine bitartrate | Approved | Cardiovascular agent | −6.12 |
| DB01424 | Aminophenazone | Approved; withdrawn | Analgesic | −6.10 |
| DB12827 | Indoximod | Investigational | Immunometabolic | −6.05 |
| DB06408 | Taribavirin Hydrochloride | Investigational | Antiviral | −6.03 |
| DB00480 | Lenalidomide | Approved | Anticancer | −5.99 |
| DB01033 | Mercaptopurine monohydrate | Approved | Anticancer | −5.99 |
| - | Z45617795 | - | Control 1 | −5.367 |
| - | Inhibitor N3 | - | Control 2 | −4.561 |
| Drug Bank ID | Drug Name | Docking Score (kcal/mol) |
|---|---|---|
| DB02502 | 8-hydroxy-2′-deoxyguanosine | −7.29 |
| DB02309 | 5-monophosphate-9-beta-D-ribofuranosyl xanthine | −7.20 |
| DB02690 | 8-hydroxy-2-methyl-3,4-dihydroquinazolin-4-one | −7.09 |
| DB03730 | 3,9-Dimethyladenine | −6.97 |
| DB04446 | Benzo[B]Thiophene-2-Carboxamidine | −6.93 |
| DB02599 | 2,6-Diamino-8-Propylsulfanylmethyl-3h-Quinazoline-4- One | −6.79 |
| DB15622 | Triazavirin | −6.76 |
| DB04103 | 3-methylcytosine | −6.63 |
| DB02187 | Equilin | −6.61 |
| DB04312 | (2,3-difluorophenyl)methanol | −6.47 |
| DB13549 | 4-dimethylaminophenol | −6.46 |
| DB07206 | 6-[2-(1H-indol-6-yl)ethyl]pyridin-2-amine | −6.41 |
| DB04448 | (2,4-difluorophenyl)methanol | −6.13 |
| DB02586 | 4,7-dimethyl-1,10-phenanthroline | −6.10 |
| DB04586 | 2-bromophenol | −6.05 |
| DB03763 | 5-methyl-2′-deoxypseudouridine | −6.00 |
| DB04440 | Purine nucleoside | −5.99 |
| Compounds | Amino Acid Residue | |
|---|---|---|
| Hydrogen Bond Interactions | Hydrophobic Interactions | |
| Sapanisertib | ASN-142 | HIS-41, MET-49, MET-165 |
| Ornidazole | ARG-188, GLN-189 | HIS-41, MET-165 |
| Napabucasin | PRO-168 | MET-165 |
| Lenalidomide | LYS-5, ARG-4 | ALA-7 |
| Daniquidone | THR-25 | HIS-41, MET-49, MET-165, |
| Indoximod | THR-129, GlU-166 | MET-165 |
| Salicylamide | CYS-145, HIS-164, GLU-166 | MET-165 |
| Control 1 | - | MET-165, MET-49, HIS-41 |
| Control 2 | SER-139, GLY138 | LYS-137, LYS-5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, K.H.; Chowdhury, M.R.; Mahmud, S.; Tareq, A.M.; Hanif, N.B.; Banu, N.; Reza, A.S.M.A.; Emran, T.B.; Simal-Gandara, J. Drug Repurposing Approach against Novel Coronavirus Disease (COVID-19) through Virtual Screening Targeting SARS-CoV-2 Main Protease. Biology 2021, 10, 2. https://doi.org/10.3390/biology10010002
Chowdhury KH, Chowdhury MR, Mahmud S, Tareq AM, Hanif NB, Banu N, Reza ASMA, Emran TB, Simal-Gandara J. Drug Repurposing Approach against Novel Coronavirus Disease (COVID-19) through Virtual Screening Targeting SARS-CoV-2 Main Protease. Biology. 2021; 10(1):2. https://doi.org/10.3390/biology10010002
Chicago/Turabian StyleChowdhury, Kamrul Hasan, Md. Riad Chowdhury, Shafi Mahmud, Abu Montakim Tareq, Nujhat Binte Hanif, Naureen Banu, A. S. M. Ali Reza, Talha Bin Emran, and Jesus Simal-Gandara. 2021. "Drug Repurposing Approach against Novel Coronavirus Disease (COVID-19) through Virtual Screening Targeting SARS-CoV-2 Main Protease" Biology 10, no. 1: 2. https://doi.org/10.3390/biology10010002
APA StyleChowdhury, K. H., Chowdhury, M. R., Mahmud, S., Tareq, A. M., Hanif, N. B., Banu, N., Reza, A. S. M. A., Emran, T. B., & Simal-Gandara, J. (2021). Drug Repurposing Approach against Novel Coronavirus Disease (COVID-19) through Virtual Screening Targeting SARS-CoV-2 Main Protease. Biology, 10(1), 2. https://doi.org/10.3390/biology10010002











