Evaluation of Microleakage, Tensile Bond Strength, and Adhesive Interface of Bulk Fill, Ormocer, and Alkasite Against Conventional Composite in Caries-Affected Primary Molars
Abstract
1. Introduction
2. Materials and Methods
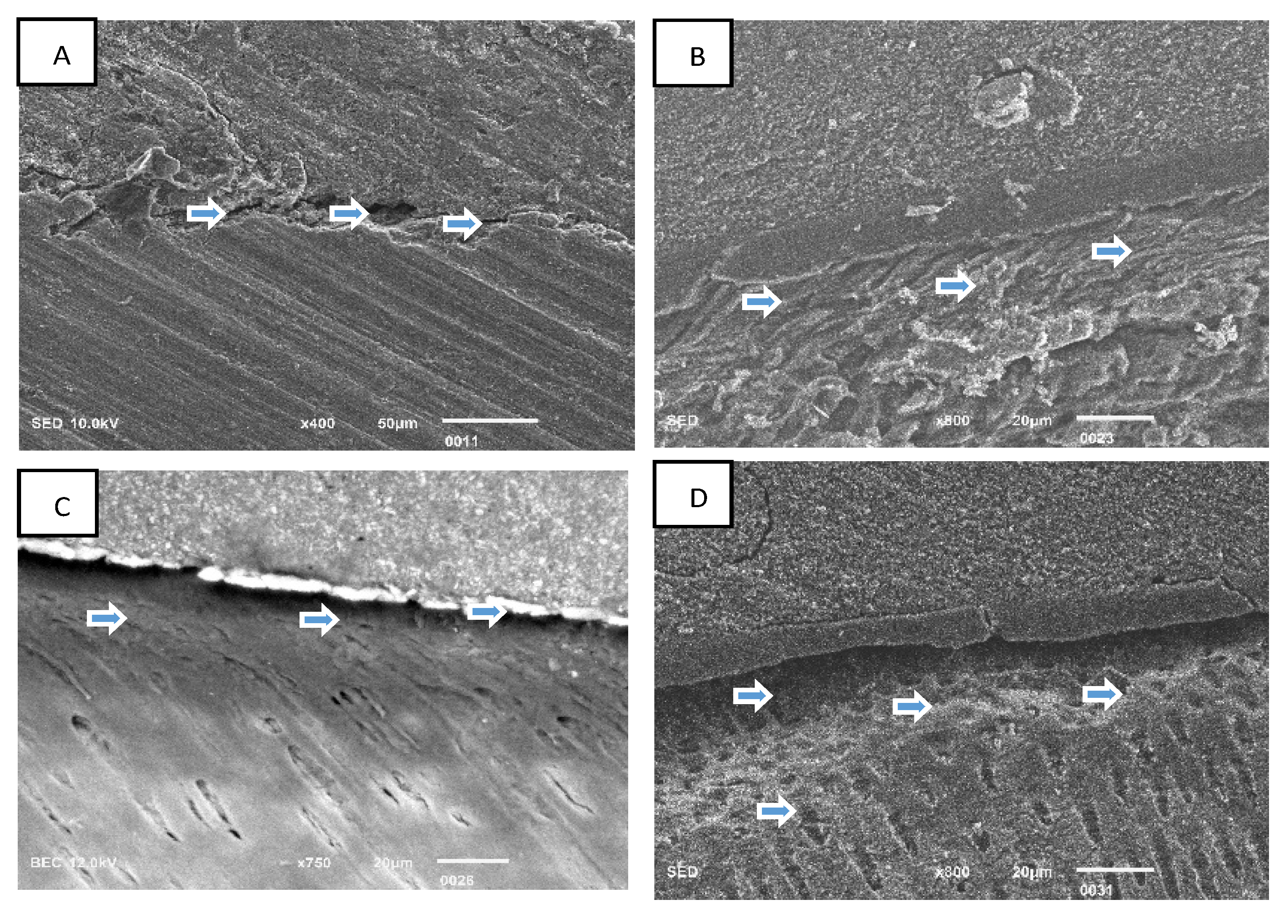
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carvalho, R.M.; Manso, A.P.; Geraldeli, S.; Tay, F.R.; Pashley, D.H. Durability of Bonds and Clinical Success of Adhesive Restorations. Dent. Mater. 2012, 28, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, S.R. Abrasive Finishing and Polishing in Restorative Dentistry: A State-of-the-Art Review. Dent. Clin. N. Am. 2007, 51, 379–397. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, A.Y.; Talaat, D.M.; Essawy, M.M.; Bakry, N. The Effectiveness of Carie-CareTM, Chemomechanical Caries Removal Technique in Primary Teeth: Randomized Controlled Clinical Trial. BMC Oral Health 2023, 23, 882. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, A.; Abrar, E.; Maawadh, A.M.; Al-Hamdan, R.S.; Almohareb, T.; AlFawaz, Y.; Naseem, M.; Vohra, F.; Abduljabbar, T. Management of Caries Affected Dentin (CAD) with Resin Modified Glass Ionomer Cement (RMGIC) in the Presence of Different Caries Disinfectants and Photosensitizers. Photodiagnosis Photodyn. Ther. 2020, 32, 101978. [Google Scholar] [CrossRef]
- Osiewicz, M.A.; Werner, A.; Roeters, F.J.M.; Kleverlaan, C.J. Wear of Bulk-Fill Resin Composites. Dent. Mater. 2022, 38, 549–553. [Google Scholar] [CrossRef]
- Mosharrafian, S.; Heidari, A.; Rahbar, P. Microleakage of Two Bulk Fill and One Conventional Composite in Class II Restorations of Primary Posterior Teeth. J. Dent. 2017, 14, 123–131. [Google Scholar]
- Paolone, G.; Mandurino, M.; Scotti, N.; Cantatore, G.; Blatz, M.B. Color Stability of Bulk-Fill Compared to Conventional Resin-Based Composites: A Scoping Review. J. Esthet. Restor. Dent. 2023, 35, 657–676. [Google Scholar] [CrossRef]
- Gupta, S.; Vellanki, V.K.; Shetty, V.K.; Kushwah, S.; Goyal, G.; Chandra, S.S. In Vitro Evaluation of Shear Bond Strength of Nanocomposites to Dentin. J. Clin. Diagn. Res. 2015, 9, ZC09–ZC11. [Google Scholar] [CrossRef]
- Mosharrafian, S.; Farahmand, N.; Poorzandpoush, K.; Hosseinipour, Z.S.; Kahforushan, M. In Vitro Microleakage at the Enamel and Dentin Margins of Class II Cavities of Primary Molars Restored with a Bulk-Fill and a Conventional Composite. Clin. Exp. Dent. Res. 2023, 9, 512–517. [Google Scholar] [CrossRef]
- AlQhtani, F.A.B.A.; Abdullah, A.M.; Sainudeen, S.; Batool, R.; Kamran, M.A. Comparison of Marginal Seal and Tensile Bond Strength of an Alkasite, Zircomer, and Bulk Fill Composite to Carious Affected Primary Molars. J. Biomater. Tissue Eng. 2024, 14, 38–44. [Google Scholar] [CrossRef]
- Pirmoradian, M.; Al-Bakhakh, B.A.J.; Behroozibakhsh, M.; Pedram, P. Repairability of Aged Dimethacrylate-Free ORMOCER-Based Dental Composite Resins with Different Surface Roughening Methods and Intermediate Materials. J. Prosthet. Dent. 2024, 131, 1238–1249. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, S.; Vinay, C.; Alla, R.K.; Uloopi, K.; Chaitanya, P.; Chandana, N. Physico-Mechanical Characteristics of Ormocer and Bulk Fill Composite Resin Restorative Materials: An in-Vitro Study. J. Clin. Diagn. Res. 2023, 17, ZC01–ZC04. [Google Scholar] [CrossRef]
- Bordina, G.E.; Lopina, N.P.; Andreev, A.A. Comparative Characteristics of the Chemical Structure of Ormokers and Traditional Composites. Russ. J. Dent. 2022, 26, 503–512. [Google Scholar] [CrossRef]
- Mulgaonkar, A.; de Ataide, I.; Fernandes, M.; Lambor, R. Shear Bond Strength Evaluation of an Alkasite Restorative Material to Three Different Liners with and without Using Adhesive System: An in Vitro Study. J. Conserv. Dent. 2021, 24, 278–282. [Google Scholar] [CrossRef]
- Meshram, P.; Meshram, V.; Palve, D.; Patil, S.; Gade, V.; Raut, A. Comparative Evaluation of Microleakage around Class V Cavities Restored with Alkasite Restorative Material with and without Bonding Agent and Flowable Composite Resin: An in Vitro Study. Indian J. Dent. Res. 2019, 30, 403–407. [Google Scholar] [CrossRef]
- Sulimany, A.M.; Aldowsari, M.K.; Bin Saleh, S.; Alotaibi, S.S.; Alhelal, B.M.; Hamdan, H.M. An In Vitro Assessment of the Shear Bond Strength of Alkasite Restorative Material in Primary Molars Compared with Glass Ionomer and Resin-Modified Glass Ionomer Restorations. Materials 2024, 17, 6230. [Google Scholar] [CrossRef]
- Gupta, M.; Gugnani, N.; Pandit, I. International Caries Detection and Assessment System (ICDAS): A New Concept. Int. J. Clin. Pediatr. Dent. 2011, 4, 93–100. [Google Scholar] [CrossRef]
- Naz, F.; Khan, A.S.; Kader, M.A.; Al Gelban, L.O.S.; Mousa, N.M.A.; Asiri, R.S.H.; Hakeem, A.S. Comparative Evaluation of Mechanical and Physical Properties of a New Bulk-Fill Alkasite with Conventional Restorative Materials. Saudi Dent. J. 2021, 33, 666–673. [Google Scholar] [CrossRef]
- Kalra, S.; Singh, A.; Gupta, M.; Chadha, V. Ormocer: An Aesthetic Direct Restorative Material; An in Vitro Study Comparing the Marginal Sealing Ability of Organically Modified Ceramics and a Hybrid Composite Using an Ormocer-Based Bonding Agent and a Conventional Fifth-Generation Bonding Agent. Contemp. Clin. Dent. 2012, 3, 48–53. [Google Scholar] [CrossRef]
- Alrahlah, A.; Naseem, M.; Tanveer, S.A.; Abrar, E.; Charania, A.; AlRifaiy, M.Q.; Vohra, F. Influence of Disinfection of Caries Effected Dentin with Different Concentration of Silver Diamine Fluoride, Curcumin and Er, Cr:YSGG on Adhesive Bond Strength to Resin Composite. Photodiagnosis Photodyn. Ther. 2020, 32, 102065. [Google Scholar] [CrossRef]
- Aljamhan, A.S.; Alrefeai, M.H.; Alhabdan, A.; Alzehiri, M.H.; Naseem, M.; Vohra, F.; Alkhudhairy, F. Interaction of Zirconium Oxide Nanoparticle Infiltrated Resin Adhesive with Dentin Conditioned by Phosphoric Acid and Er, Cr: YSGG Laser. J. Appl. Biomater. Funct. Mater. 2022, 20, 228080002210873. [Google Scholar] [CrossRef]
- ElBahrawy, E.M.S.; Shebl, E.; Attia, R. The Impact of Artificial Aging Using Chewing Simulator on Micro-Shear Bond Strength and Micro-Leakage of Alkasite and Bioactive Resin Based Composites: An in-Vitro Comparative Study. Tanta Dent. J. 2024, 21, 157–169. [Google Scholar] [CrossRef]
- Ebaya, M.M.; Ali, A.I.; El-Haliem, H.A.; Mahmoud, S.H. Color Stability and Surface Roughness of Ormocer- versus Methacrylate-Based Single Shade Composite in Anterior Restoration. BMC Oral Health 2022, 22, 208. [Google Scholar] [CrossRef]
- Çağırır Dindaroğlu, F.; Yılmaz, E. Two-Year Evaluation of a Nano-Hybrid and a Bulk-Fill Resin Composite: A Randomized, Double-Blind Split-Mouth Clinical Study. Clin. Oral Investig. 2024, 28, 208. [Google Scholar] [CrossRef]
- Awad, M.M.; Alshehri, T.; Alqarni, A.M.; Magdy, N.M.; Alhalabi, F.; Alotaibi, D.; Alrahlah, A. Evaluation of the Bond Strength and Cytotoxicity of Alkasite Restorative Material. Appl. Sci. 2020, 10, 6175. [Google Scholar] [CrossRef]
- Cruz, M.W.A.; Turssi, C.P.; Amaral, F.L.; Basting, R.T.; Junior, W.F.V.; Franca, F.M.G. Long-Term Bond Strength of Ormocer-Based Resin Composites Using a Universal Adhesive Used in Different Adhesive Strategies. Am. J. Dent. 2023, 36, 201–206. [Google Scholar]
- Boaro, L.C.C.; Lopes, D.P.; de Souza, A.S.C.; Nakano, E.L.; Perez, M.D.A.; Pfeifer, C.S.; Gonçalves, F. Clinical Performance and Chemical-Physical Properties of Bulk Fill Composites Resin —A Systematic Review and Meta-Analysis. Dent. Mater. 2019, 35, e249–e264. [Google Scholar] [CrossRef]
- Eltoum, N.A.; Bakry, N.S.; Talaat, D.M.; Elshabrawy, S.M. Microleakage evaluation of bulk-fill composite in Class II restorations of primary molars. Alex. Dent. J. 2019, 44, 111–116. [Google Scholar] [CrossRef]
- Chatra, A.; Nair, P.M.S.; D’costa, V.F.; Kukkila, J.; Mayya, A.; Chatra, L.; Mayya, S.S. Shear Bond Strength of Self-Adhesive Versus Conventional Flowable Composites: An In Vitro Study. J. Int. Soc. Prev. Community Dent. 2024, 14, 362–368. [Google Scholar] [CrossRef]
- Zanatta, C.T.I.; de Faveri Cardoso, P.M.; Camilotti, V.; Mendonça, M.J.; Ueda, J.K. Micro-Shear Bond Strength of Self-Adhesive Versus Conventional Low-Viscosity Composite Resins: In Vitro Study. J. Adv. Med. Med. Res. 2024, 36, 11–20. [Google Scholar] [CrossRef]
- Bilgrami, A.; Maqsood, A.; Alam, M.K.; Ahmed, N.; Mustafa, M.; Alqahtani, A.R.; Alshehri, A.; Alqahtani, A.A.; Alghannam, S. Evaluation of Shear Bond Strength between Resin Composites and Conventional Glass Ionomer Cement in Class II Restorative Technique—An In Vitro Study. Materials 2022, 15, 4293. [Google Scholar] [CrossRef] [PubMed]
- Prabakar, J.; Jeevanandan, G.; Kengadaran, S. In Vitro Evaluation of Viscosity, Depth of Penetration, Microleakage, and Shear Bond Strength of Conventional and Hydrophilic Sealants. Int. J. Clin. Pediatr. Dent. 2023, 16, 765–770. [Google Scholar] [CrossRef]
- Javed, F.; Siddiqui, F.; Majid, A. Beyond Traditional Fillings: Why Bulk-Fill Composites Are Changing the Game. Int. J. Res. Rev. 2024, 11, 198–203. [Google Scholar] [CrossRef]
- Alp, G.; Subaşı, M.G.; Johnston, W.M.; Yilmaz, B. Effect of Different Resin Cements and Surface Treatments on the Shear Bond Strength of Ceramic-Glass Polymer Materials. J. Prosthet. Dent. 2018, 120, 454–461. [Google Scholar] [CrossRef]
- Rayar, S.; Sadasiva, K.; Singh, P.; Thomas, P.; Senthilkumar, K.; Jayasimharaj, U. Effect of 2% Chlorhexidine on Resin Bond Strength and Mode of Failure Using Two Different Adhesives on Dentin: An in Vitro Study. J. Pharm. Bioallied Sci. 2019, 11, S325–S330. [Google Scholar] [CrossRef]
- Sauro, S.; Faus-Matoses, V.; Makeeva, I.; Martí, J.M.N.; Martínez, R.G.; Bautista, J.A.G.; Faus-Llácer, V. Effects of Polyacrylic Acid Pre-Treatment on Bonded-Dentine Interfaces Created with a Modern Bioactive Resin-Modified Glass Ionomer Cement and Subjected to Cycling Mechanical Stress. Materials 2018, 11, 1884. [Google Scholar] [CrossRef]
- Alsunbul, H.; Almutairi, B.; Aljanakh, M.; Abduljabbar, T. Hybrid Ceramic Repair Strength, Surface Roughness, and Bond Failure, Using Methylene Blue-Activated Low-Level Laser Therapy, Carbon Dioxide, and Ti: Al2O3 Laser. Photodiagnosis Photodyn. Ther. 2023, 43, 103693. [Google Scholar] [CrossRef]
- Takashino, N.; Nakashima, S.; Shimada, Y.; Tagami, J.; Sumi, Y. Effect of Thermal Cyclic Stress on Acid Resistance of Resin-Infiltrated Incipient Enamel Lesions in Vitro. Dent. Mater. J. 2016, 35, 425–431. [Google Scholar] [CrossRef]
| Materials | Composition |
|---|---|
| Bulk-fill Composite GrandioSO, Voco; GmbH Germany | Filler 89% w/w: Glass Ceramic Filler; Functionalized Silicon Dioxide Nanoparticles; Iron Oxide; Titanium Oxide.Resin: BisGMa; TEGDMA Camphorquinone Photocatalyst Butylated Hydroxytoluene Stabilizer |
| BF composite Tetric® N-Ceram BF composite (Ivoclar Vivadent, NY, USA) | Monomer Matrix: Mono-methacrylate and Di-methacrylate (28 wt.%) Fillers: Barium glass, Ytterbium trifluoride and Copolymers (71 wt.%). Additives, initiators, stabilizers and pigments are additional ingredients (<1.0 wt.%) |
| Alkasite (Cention N) (Ivoclar Vivadent Inc., NY, USA, A2 shade) | Liquid consists of Methacrylate and initiators, while the Powder includes a mixture of glass fillers, initiators, and pigments |
| Ormocer (Admira Fusion xtra, VOCO GmbH) | Pure silicate-based ORMOCER matrix, containing a high percentage of Nano-hybrid fillers (60% nano-particulate and 40% micro/macro-particulate). Free of traditional monomers like Bis-GMA or HEMA. |
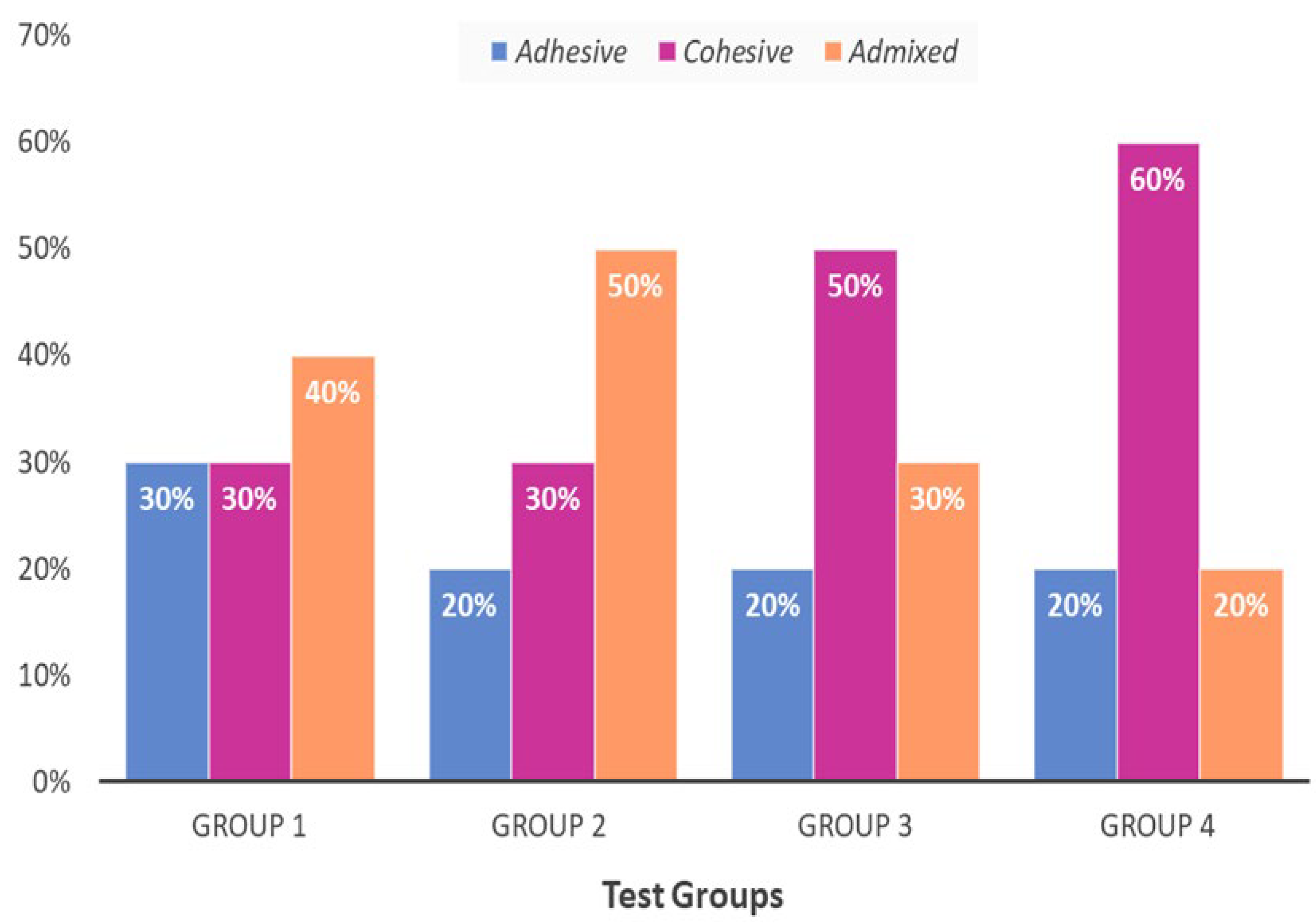
| Experimental Groups | Mean ± SD | p-Value ! |
|---|---|---|
| Group 1: Conventional Composite | 47.23 ± 0.10 c | ˂0.05 |
| Group 2: BF Composite | 27.11 ± 0.11 b | |
| Group 3: Alkasite | 15.24 ± 0.14 a | |
| Group 4: Ormocer | 13.22 ± 0.12 a |
| Experimental Groups | Mean± SD (MPa) | p-Value ! |
|---|---|---|
| Group 1: Conventional Composite | 9.92 ± 0.53 c | ˂0.05 |
| Group 2: BF Composite | 11.18 ± 0.22 b | |
| Group 3: Alkasite | 13.12 ± 0.16 a | |
| Group 4: Ormocer | 13.42 ± 0.19 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shono, N.N.; Alkhudhairy, F. Evaluation of Microleakage, Tensile Bond Strength, and Adhesive Interface of Bulk Fill, Ormocer, and Alkasite Against Conventional Composite in Caries-Affected Primary Molars. Coatings 2025, 15, 321. https://doi.org/10.3390/coatings15030321
Shono NN, Alkhudhairy F. Evaluation of Microleakage, Tensile Bond Strength, and Adhesive Interface of Bulk Fill, Ormocer, and Alkasite Against Conventional Composite in Caries-Affected Primary Molars. Coatings. 2025; 15(3):321. https://doi.org/10.3390/coatings15030321
Chicago/Turabian StyleShono, Nourah N., and Fahad Alkhudhairy. 2025. "Evaluation of Microleakage, Tensile Bond Strength, and Adhesive Interface of Bulk Fill, Ormocer, and Alkasite Against Conventional Composite in Caries-Affected Primary Molars" Coatings 15, no. 3: 321. https://doi.org/10.3390/coatings15030321
APA StyleShono, N. N., & Alkhudhairy, F. (2025). Evaluation of Microleakage, Tensile Bond Strength, and Adhesive Interface of Bulk Fill, Ormocer, and Alkasite Against Conventional Composite in Caries-Affected Primary Molars. Coatings, 15(3), 321. https://doi.org/10.3390/coatings15030321






