Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength
Abstract
1. Introduction
2. Materials and Methods
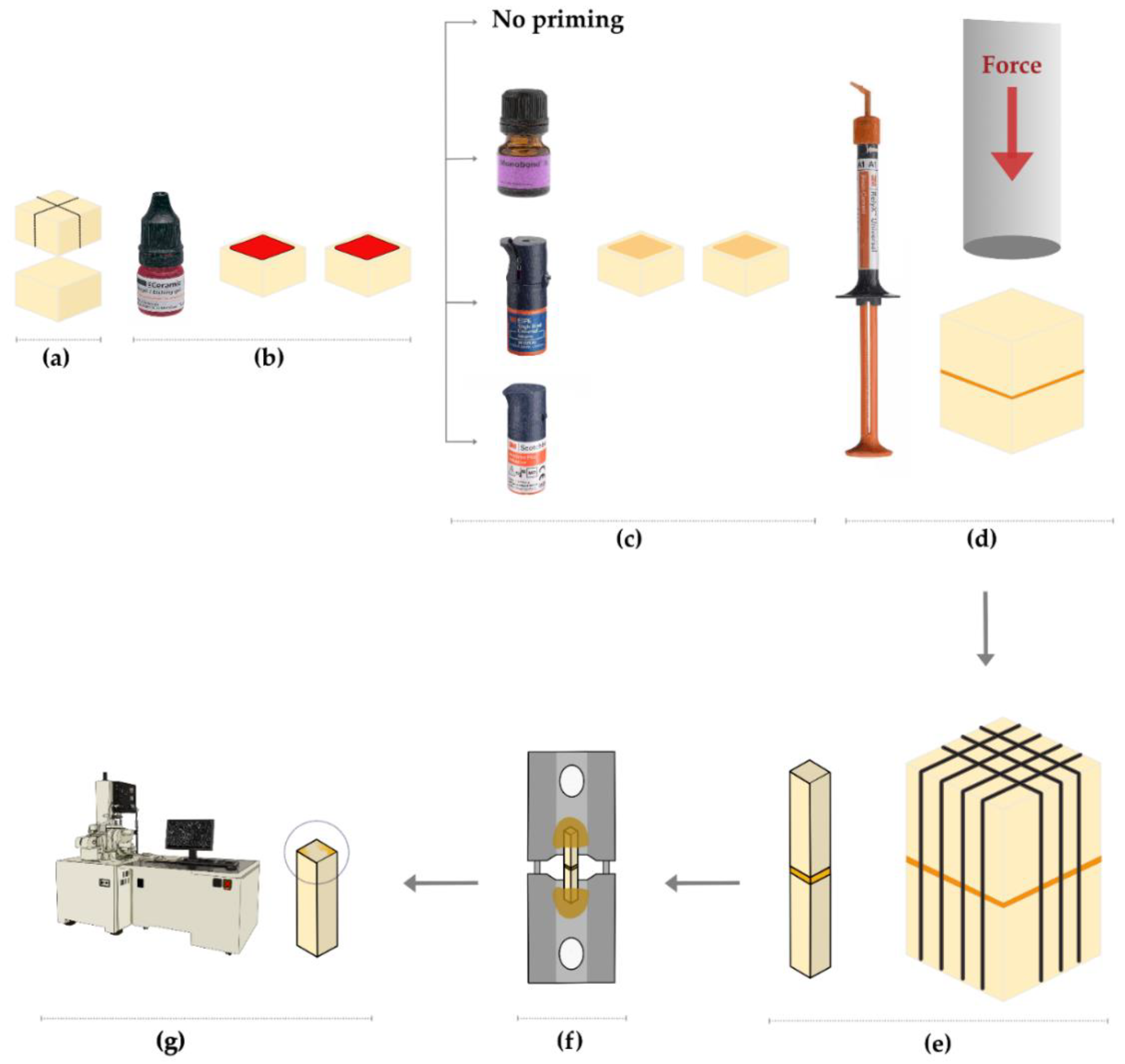
2.1. Specimens’ Preparation
2.2. μTBS
2.3. Failure/Fracture Mode Assessment
2.4. Statistical Analysis
3. Results
3.1. μTBS
3.2. Failure Mode Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van den Breemer, C.R.; Gresnigt, M.M.; Cune, M.S. Cementation of Glass-Ceramic Posterior Restorations: A Systematic Review. BioMed Res. Int. 2015, 2015, 148954. [Google Scholar] [CrossRef] [PubMed]
- Politano, G.; Van Meerbeek, B.; Peumans, M. Nonretentive Bonded Ceramic Partial Crowns: Concept and Simplified Protocol for Long-lasting Dental Restorations. J. Adhes. Dent. 2018, 20, 495–510. [Google Scholar] [CrossRef] [PubMed]
- Phark, J.-H.; Duarte, S., Jr. Microstructural considerations for novel lithium disilicate glass ceramics: A review. J. Esthet. Restor. Dent. 2022, 34, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.M.; Alqahtani, H.; Al-Mudahi, A.; Murayshed, M.S.; Alrahlah, A.; Bhandi, S.H. Adhesive Bonding to Computer-aided Design/ Computer-aided Manufacturing Esthetic Dental Materials: An Overview. J. Contemp. Dent. Pract. 2017, 18, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Malysa, A.; Wezgowiec, J.; Grzebieluch, W.; Danel, D.P.; Wieckiewicz, M. Effect of Thermocycling on the Bond Strength of Self-Adhesive Resin Cements Used for Luting CAD/CAM Ceramics to Human Dentin. Int. J. Mol. Sci. 2022, 23, 745. [Google Scholar] [CrossRef]
- Malysa, A.; Wezgowiec, J.; Orzeszek, S.; Florjanski, W.; Zietek, M.; Wieckiewicz, M. Effect of Different Surface Treatment Methods on Bond Strength of Dental Ceramics to Dental Hard Tissues: A Systematic Review. Molecules 2021, 26, 1223. [Google Scholar] [CrossRef]
- Akar, T.; Dündar, A.; Kırmalı, Ö.; Üstün, Ö.; Kapdan, A.; Er, H.; Kuştarcı, A.; Er, K.; Yılmaz, B. Evaluation of the shear bond strength of zirconia to a self-adhesive resin cement after different surface treatment. Dent. Med. Probl. 2021, 58, 463–472. [Google Scholar] [CrossRef]
- Lubauer, J.; Belli, R.; Peterlik, H.; Hurle, K.; Lohbauer, U. Grasping the Lithium hype: Insights into modern dental Lithium Silicate glass-ceramics. Dent. Mater. 2022, 38, 318–332. [Google Scholar] [CrossRef]
- Tian, T.; Tsoi, J.K.-H.; Matinlinna, J.P.; Burrow, M.F. Aspects of bonding between resin luting cements and glass ceramic materials. Dent. Mater. 2014, 30, e147–e162. [Google Scholar] [CrossRef]
- Della Bona, A.; Anusavice, K.J.; Mecholsky, J.J., Jr. Failure analysis of resin composite bonded to ceramic. Dent. Mater. 2003, 19, 693–699. [Google Scholar] [CrossRef]
- Matinlinna, J.P.; Lassila, L.V.; Özcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 155–164. [Google Scholar] [PubMed]
- Lung, C.Y.; Matinlinna, J.P. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent. Mater. 2012, 28, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Oh, W.S.; Williams, J.R. Effect of post-silanization drying on the bond strength of composite to ceramic. J. Prosthet. Dent. 2004, 91, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Nagarkar, S.; Theis-Mahon, N.; Perdigão, J. Universal dental adhesives: Current status, laboratory testing, and clinical performance. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 2121–2131. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Suárez, C.E.; de Oliveira da Rosa, W.L.; Vitti, R.P.; da Silva, A.F.; Piva, E. Bonding Strength of Universal Adhesives to Indirect Substrates: A Meta-Analysis of in Vitro Studies. J. Prosthodont. 2020, 29, 298–308. [Google Scholar] [CrossRef]
- Kalavacharla, V.K.; Lawson, N.C.; Ramp, L.C.; Burgess, J.O. Influence of Etching Protocol and Silane Treatment with a Universal Adhesive on Lithium Disilicate Bond Strength. Oper. Dent. 2015, 40, 372–378. [Google Scholar] [CrossRef]
- Makishi, P.; Andre, C.B.; Silva, J.L.; Bacelar-Sa, R.; Correr-Sobrinho, L.; Giannini, M. Effect of Storage Time on Bond Strength Performance of Multimode Adhesives to Indirect Resin Composite and Lithium Disilicate Glass Ceramic. Oper. Dent. 2016, 41, 541–551. [Google Scholar] [CrossRef]
- Yao, C.; Yang, H.; Yu, J.; Zhang, L.; Zhu, Y.; Huang, C. High Bond Durability of Universal Adhesives on Glass Ceramics Facilitated by Silane Pretreatment. Oper. Dent. 2018, 43, 602–612. [Google Scholar] [CrossRef]
- Yao, C.; Zhou, L.; Yang, H.; Wang, Y.; Sun, H.; Guo, J.; Huang, C. Effect of silane pretreatment on the immediate bonding of universal adhesives to computer-aided design/computer-aided manufacturing lithium disilicate glass ceramics. Eur. J. Oral Sci. 2017, 125, 173–180. [Google Scholar] [CrossRef]
- Awad, M.M.; Albedaiwi, L.; Almahdy, A.; Khan, R.; Silikas, N.; Hatamleh, M.M.; Alkhtani, F.M.; Alrahlah, A. Effect of universal adhesives on microtensile bond strength to hybrid ceramic. BMC Oral Health 2019, 19, 178. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Sonoda, A.; Maruo, Y.; Makita, Y.; Okihara, T.; Irie, M.; Yoshida, Y.; Van Meerbeek, B. Effectiveness and stability of silane coupling agent incorporated in ‘universal’ adhesives. Dent. Mater. 2016, 32, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Alrahlah, A.; Awad, M.M.; Vohra, F.; Al-Mudahi, A.; Al Jeaidi, Z.A.; Elsharawy, M. Effect of self etching ceramic primer and universal adhesive on bond strength of lithium disilicate ceramic. J. Adhes. Sci. Technol. 2017, 31, 2611–2619. [Google Scholar] [CrossRef]
- Yao, C.; Ahmed, M.H.; De Grave, L.; Yoshihara, K.; Mercelis, B.; Okazaki, Y.; Van Landuyt, K.L.; Huang, C.; Van Meerbeek, B. Optimizing glass-ceramic bonding incorporating new silane technology in an experimental universal adhesive formulation. Dent. Mater. 2021, 37, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Südbeck, J.M.; Jacker-Guhr, S.; Lührs, A.K. Do Different Pretreatment Methods Influence the Microtensile Bond Strength of Composite Cements to Silicate Ceramic? J. Adhes. Dent. 2021, 23, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, S.; Breschi, L.; Özcan, M.; Pfefferkorn, F.; Ferrari, M.; Van Meerbeek, B. Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent. Mater. 2017, 33, 133–143. [Google Scholar] [CrossRef]
- Eckert, G.J.; Platt, J.A. A statistical evaluation of microtensile bond strength methodology for dental adhesives. Dent. Mater. 2007, 23, 385–391. [Google Scholar] [CrossRef]
- El Zohairy, A.A.; De Gee, A.J.; Mohsen, M.M.; Feilzer, A.J. Microtensile bond strength testing of luting cements to prefabricated CAD/CAM ceramic and composite blocks. Dent. Mater. 2003, 19, 575–583. [Google Scholar] [CrossRef]
- De Munck, J.; Mine, A.; Poitevin, A.; Van Ende, A.; Cardoso, M.V.; Van Landuyt, K.L.; Peumans, M.; Van Meerbeek, B. Meta-analytical review of parameters involved in dentin bonding. J. Dent. Res. 2012, 91, 351–357. [Google Scholar] [CrossRef]
- Salz, U.; Bock, T. Testing adhesion of direct restoratives to dental hard tissue—A review. J. Adhes. Dent. 2010, 12, 343–371. [Google Scholar] [CrossRef]
- Huang, T.H.; Kao, C.T. The shear bond strength of composite brackets on porcelain teeth. Eur. J. Orthod. 2001, 23, 433–439. [Google Scholar] [CrossRef]
- Matinlinna, J.P.; Lung, C.Y.K.; Tsoi, J.K.H. Silane adhesion mechanism in dental applications and surface treatments: A review. Dent. Mater. 2018, 34, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Zakir, M.; Ashraf, U.; Tian, T.; Han, A.; Qiao, W.; Jin, X.; Zhang, M.; Tsoi, J.K.-H.; Matinlinna, J.P. The Role of Silane Coupling Agents and Universal Primers in Durable Adhesion to Dental Restorative Materials—A Review. Curr. Oral Health Rep. 2016, 3, 244–253. [Google Scholar] [CrossRef]
- Chen, C.; Niu, L.N.; Xie, H.; Zhang, Z.Y.; Zhou, L.Q.; Jiao, K.; Chen, J.H.; Pashley, D.H.; Tay, F.R. Bonding of universal adhesives to dentine--Old wine in new bottles? J. Dent. 2015, 43, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Papadogiannis, D.; Dimitriadi, M.; Zafiropoulou, M.; Gaintantzopoulou, M.D.; Eliades, G. Universal Adhesives: Setting Characteristics and Reactivity with Dentin. Materials 2019, 12, 1720. [Google Scholar] [CrossRef]
- Lima, R.B.W.; Muniz, I.A.F.; Campos, D.E.S.; Murillo-Gómez, F.; Andrade, A.K.M.; Duarte, R.M.; de Souza, G.M. Effect of universal adhesives and self-etch ceramic primers on bond strength to glass ceramics: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022. [Google Scholar] [CrossRef]
- Acres, R.G.; Ellis, A.V.; Alvino, J.; Lenahan, C.E.; Khodakov, D.A.; Metha, G.F.; Andersson, G.G. Molecular Structure of 3-Aminopropyltriethoxysilane Layers Formed on Silanol-Terminated Silicon Surfaces. J. Phys. Chem. C 2012, 116, 6289–6297. [Google Scholar] [CrossRef]
- Park, S.-J.; Jin, J.-S.; Lee, J.-R. Influence of silane coupling agents on the surface energetics of glass fibers and mechanical interfacial properties of glass fiber-reinforced composites. J. Adhes. Sci. Technol. 2000, 14, 1677–1689. [Google Scholar] [CrossRef]
- Xiong, M.; Zhang, K.; Chen, Y. ATRP of 3-(triethoxysilyl)propyl methacrylate and preparation of “stable” gelable block copolymers. Eur. Polym. J. 2008, 44, 3835–3841. [Google Scholar] [CrossRef]
- Roeder, L.; Pereira, P.N.; Yamamoto, T.; Ilie, N.; Armstrong, S.; Ferracane, J. Spotlight on bond strength testing--unraveling the complexities. Dent. Mater. 2011, 27, 1197–1203. [Google Scholar] [CrossRef]
- Comba, L.; Tichy, A.; Bradna, P. The Effect of Censoring on the Statistical Evaluation of Composite-to-Composite Bond Strength. J. Adhes. Dent. 2020, 22, 183–193. [Google Scholar] [CrossRef]
- Franz, A.; Lettner, S.; Watts, D.C.; Schedle, A. Should statistical analysis of bond-strength data include or exclude cohesive failures? Dent. Mater. 2022, 38, 1942–1946. [Google Scholar] [CrossRef] [PubMed]
- da Silva, S.E.G.; de Araújo, G.M.; Souza, K.B.; Moura, D.M.D.; Aurélio, I.L.; May, L.G.; Vila-Nova, T.E.L.; Zhang, Y.; de Assunção, E.S.R.O. Biaxial flexure strength and physicochemical characterization of a CAD/CAM lithium disilicate ceramic: Effect of etching time, silane, and adhesive applications. Clin. Oral Investig. 2022, 26, 6753–6763. [Google Scholar] [CrossRef] [PubMed]



| Material (LOT Number) | Code | Composition |
|---|---|---|
| Initial LiSi Block, GC, GC corporation, Tokyo, Japan. (LOT: 2201201C) | LDC | Silicon dioxide: 81%; phosphorus oxide 8.1%; potassium oxide 5.9%; aluminum oxide 3.8%; titanium oxide 0.5%; and cerium oxide 0.6%. |
| Single Bond Universal Adhesive, 3M Deutschland GmbH, Neuss, Germany. (LOT: 10608B) | SBU | 10-MDP phosphate monomer, Vitrebond, copolymer, HEMA, Bis-GMA, dimethacrylate resin, camphorquinone, silane (γMPTS), ethanol, and water. |
| Scotchbond Universal Plus Adhesive, 3M Deutschland GmbH, Neuss, Germany. (LOT: 7676509) | SBP | 10-MDP phosphate monomer, Vitrebond, copolymer, HEMA, dimethacrylate resin, crosslinking radiopaque monomer, dual-cure accelerator, camphorquinone, optimized silane (γMPTES/APTES), ethanol, and water. |
| Monobond N, Ivoclar Vivadent, Schaan, Liechtenstein. (LOT: Z02S7Z) | MBN | Alcohol, silane methacrylate, phosphoric acid methacrylate, disulfide methacrylate. |
| RelyX Universal Resin Cement, 3M Oral Care, St. Paul, USA. (LOT: 7756479) | - | Dimethacrylate monomers, phosphorylated dimethacrylate adhesion monomers, photoinitiator system, novel amphiphilic redox initiator system, radiopaque fillers, and rheological additives and pigments. |
| Pair-Wise Groups Comparisons | Mean Difference | Lower Bound | Upper Bound | p-Value | Significance |
|---|---|---|---|---|---|
| Control-MBN | 23.739 | 15.581 | 31.897 | <0.001 | * |
| Control-SBU | 2.181 | −5.977 | 10.339 | 0.869 | |
| Control-SBP | 11.942 | 3.784 | 20.100 | 0.003 | * |
| MBN-SBU | 21.557 | 13.399 | 29.715 | <0.001 | * |
| MBN-SBP | 11.797 | 3.639 | 19.955 | 0.004 | * |
| SBU-SBP | −9.761 | −17.919 | −1.603 | 0.017 | * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Awad, M.M.; Alhalabi, F.; Alshehri, A.; Salem, M.A.; Robaian, A.; Alghannam, S.; Alayad, A.S.; Almutairi, B.; Alrahlah, A. Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength. Coatings 2023, 13, 477. https://doi.org/10.3390/coatings13020477
Awad MM, Alhalabi F, Alshehri A, Salem MA, Robaian A, Alghannam S, Alayad AS, Almutairi B, Alrahlah A. Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength. Coatings. 2023; 13(2):477. https://doi.org/10.3390/coatings13020477
Chicago/Turabian StyleAwad, Mohamed M., Feras Alhalabi, Abdullah Alshehri, Mohammed Ali Salem, Ali Robaian, Shahad Alghannam, Abdullah S. Alayad, Basil Almutairi, and Ali Alrahlah. 2023. "Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength" Coatings 13, no. 2: 477. https://doi.org/10.3390/coatings13020477
APA StyleAwad, M. M., Alhalabi, F., Alshehri, A., Salem, M. A., Robaian, A., Alghannam, S., Alayad, A. S., Almutairi, B., & Alrahlah, A. (2023). Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength. Coatings, 13(2), 477. https://doi.org/10.3390/coatings13020477








