Since the first reports of a contagious pneumonia such as the disease in China in December 2019, the world has witnessed a situation that very few people have ever seen in their lifetimes. With staggering numbers of deaths and infected cases, crashing economies, overburdened healthcare facilities, and severe restrictions on movement and human contact, the pandemic has changed the lives of millions worldwide. This infectious disease, referred to as COVID-19, is caused by a novel coronavirus that originated in Wuhan, China, with reports of being spread from animals to humans at a live food market in the vicinity where the first case was reported. The SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) virus belongs to the family of coronaviruses and, like MERS-CoV (Middle East Respiratory Syndrome) and SARS-CoV (Severe Acute Respiratory Syndrome), is a betacoronavirus. Reports propose a zoonotic origin for the virus, originating in bats and spreading to humans through an animal–human transmission mode. Like other viruses, including the influenza virus and H5N1, this virus easily spreads between humans through contact and airborne and droplet modes. A staggering number of 53 million cases with 1.3 million deaths have been reported thus far. The World Health Organization (WHO) designated COVID-19 as a global pandemic in early 2020. Efforts have been underway to establish early and effective screening methods and the tracing of infected individuals in order to mitigate the spread of the virus, and to develop an effective vaccine that is easily accessible to the entire world.
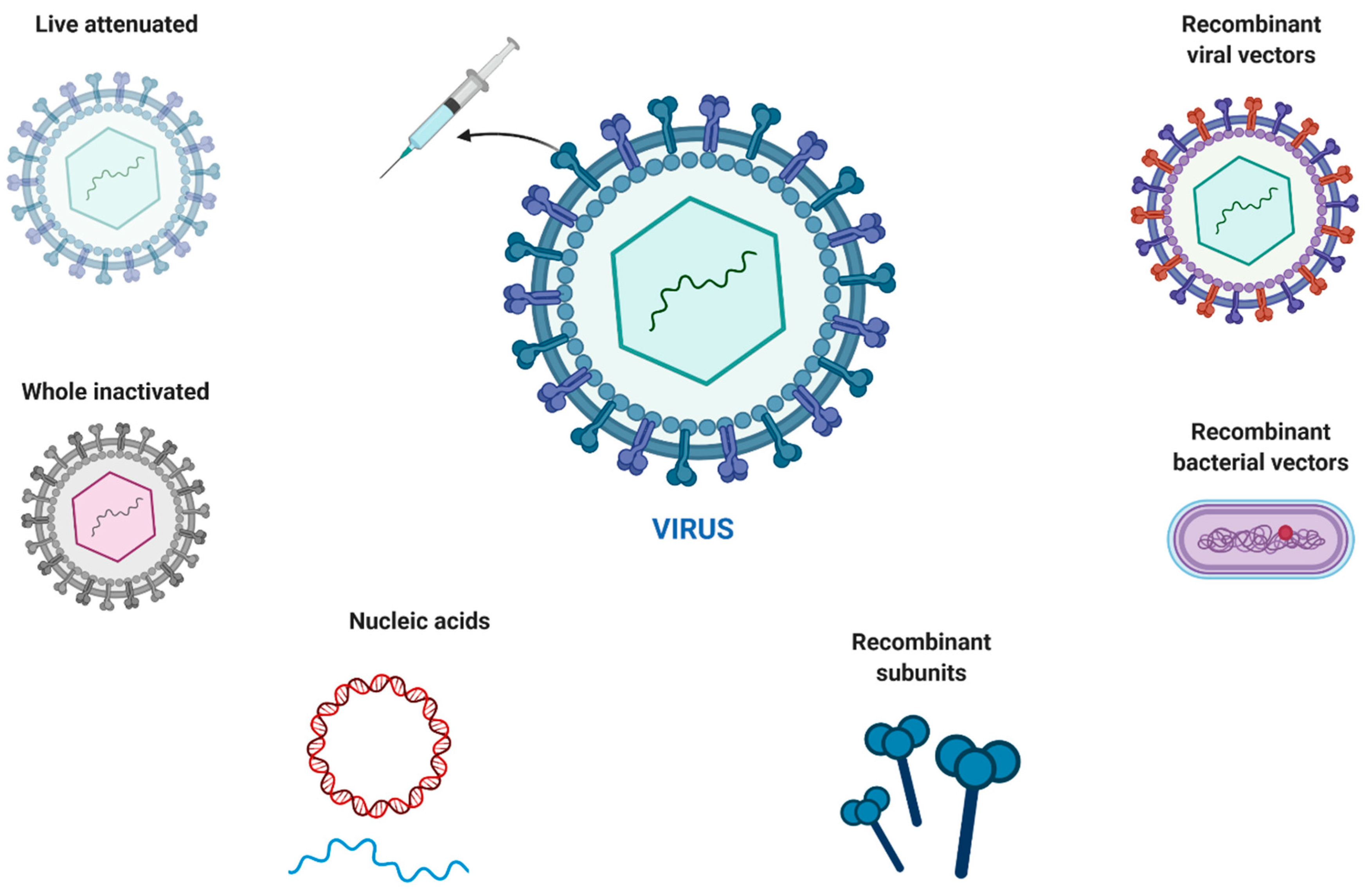
Figure 1 presents an overview of the various strategies commonly employed for vaccine development.
The use of nanomaterial-based technology has been extensively researched for the development of therapeutic carriers for a host of diseases, as well as for vaccine development [
1,
2]. Due to their tunable structural and functional features, these materials can either mimic virus particles or interact with them, thereby blocking their entry into the host cells via competitive binding. Certain characteristic features of the virus can be harnessed to the nanoparticle surface in order to generate complementary interaction sites. In this regard, a spiky morphology has been shown to greatly enhance the number of binding sites for various anti-viral drugs. Variations in the surfaces and material properties of nanomaterials can be tailored to meet the desired effects. The immunogenic fate of nanomaterials has generated considerable interest, and the targeting of immune cells for therapeutic purposes using these platforms has emerged as a popular strategy [
3]. Following the success of the Moderna SARS CoV-2 and Johnson & Johnson’s influenza vaccines based on lipid nanoparticles, several researchers have explored the scope of nanocarriers to be used for the development of a SARS CoV-2 vaccine. The advantages of a nanocarrier-based system include the size- and shape-dependent lymphatic trafficking and uptake by APCs, the possibility of delivering multiple therapeutics on a single platform (antigen/adjuvant), the facilitation of antigen cross-presentation through CD8 and T cell activation, and a prolonged immune memory.
Vaccine adjuvant nanoparticles (VANs) have also been reported to increase the efficiency and safety of the elicited immune response. They have been particularly useful when using reduced doses, thus enabling activation using only a small amount and, subsequently, permitting higher production numbers. Dose-sparing is achieved through lymph node targeting and the targeting of VANs, in turn, by dendritic cells, thereby increasing their adjuvanticity [
2,
4]. Currently, five protein subunit vaccine candidates use an antigen and adjuvant, such as NVX-CoV2373, which is a nanoparticle-based combination of the SARS-CoV-2 glycoprotein and the matrix M. These particles either function as carriers of the molecular adjuvants or are designed with specific inbuilt functions capable of stimulating anti-immunity reactions. As compared to the traditional delivery systems, VANs address the shortcomings of the small molecules and demonstrate the benefits of using nanocarriers, which include but are not limited to their systemic distribution, fast clearance, and targeting and uptake properties. These nanocarriers can also deliver adjuvants to inhibit autoimmune responses; thus, they are safe for immune-compromised individuals.
Various attractive and tunable features of nanomaterials, including their surface chemistry, can trigger adjuvanticity. Modifications of the functional groups, such as the introduction of hydroxyl groups, can activate the complement system and increase the immune response. The use of nanomaterials for vaccine formulations opens up new avenues for investigation and therapeutics. The mimicking of various cell functions has also been investigated using various liposomes, lipoproteins, and cell-membrane nanostructures. Surface-targeting using ligands and antibodies also remains a popular strategy for the inhibition of the pathogen’s entry into the host cells. Polymeric nanoparticles using a “topology-matching design” have also been reported to inhibit hemagglutinin and neuraminidase, thus blocking the entry of the virus into the host cells [
5].
In view of the numerous technologies available for developing a vaccine, it is rather impossible to identify a “one-size-fits-all” approach. The major challenge in the development of a vaccine to combat the deadly coronavirus is sustaining their half-life without deep-freezing them. Future endeavors should aim at prolonging the shelf life of the vaccines and reducing the costs associated with their storage, without compromising their efficacy or safety profiles. This is a global challenge for researchers, clinicians, and healthcare officials and workers alike. The success of a mass-produced vaccine, however, heavily relies on these factors.