Abstract
Periapical surgery is a procedure indicated for the treatment of persistent apical periodontitis in an endodontically treated tooth and when retreatment has not been successful or not feasible. Various materials have been suggested and tested for this purpose: amalgam, MTA, and zinc-eugenol oxide cements, among others. The objective of the present study was to evaluate the results regarding the success of the periapical surgery and if the retrograde filling material used influences this success rate. A systematic review of the literature on the prognosis of periapical surgery was performed. The following PICO question was asked: “In patients who require periapical surgery (patient), is the retrograde filling (comparison) material used in apicoectomy (intervention) determining for the success of the treatment (outcome)?” Periapical surgery achieves successful results in 84% of cases. All the materials compared obtain satisfactory results. The results of the meta-analysis show that there are no statistically significant differences between MTA compared to SuperEBA (1.37 (95% CI: 0.87, 2.15)) or RRM (0.99 (95% CI: 0.51, 1.94)) but with MRI (1.93 (95% CI: 1.22, 3.05)), where the results favour MTA. In general, the most modern materials obtain better results than amalgam. Surgical techniques with magnification obtain better results (12.3% failure) than conventional techniques (22.93% failure). Periapical surgery is a procedure with a high success rate. The use of all the materials compared obtains satisfactory results. Magnification surgery techniques perform better than conventional techniques.
1. Introduction
Periapical surgery is a procedure indicated for the treatment of persistent apical periodontitis in an endodontically treated tooth when retreatment has not been successful or is not feasible [1]. The resection of the last 3 mm of the end of the root is carried out since the highest percentage of table accessory ducts are found in these 3 mm apical [2,3]. After apical preparation, a filling material is used to seal the cavity at the end of the root. Prevention of microfiltration, biocompatibility, and material stability in apical tissues are very important. The filling material must adhere to the walls of the cavity and resist resorption and moisture ingress. A good-quality apical root canal filler is essential for the success of periapical surgery [4]. Several materials have been suggested and tested for this purpose: silver amalgam, gutta-hanger, Cavit (3 M ESPE, St Paul, MN, USA), glass-ionomer cements, zinc-eugenol oxide-reinforced cements (IRM, SuperEBA), composite resin materials (Retroplast), compomers, polymers (Diaket, 3 M ESPE, St Paul, MN, USA), polycarboxylate cements, and bioceramic cements (MTA (Mineral Trioxide Aggregate), Biodentine or calcium phosphate silicate cements) [5,6].
Characteristics of the materials used in periapical surgery:
- -
- Silver amalgam
Amalgam has been the most widely used apical filler material for many years, mainly for its handling and radiopacity. In 1978, the composition of the alloy was standardized in the ISO 1559 standard, with the following composition: silver 64%, tin 29%, copper 6%, mercury 3% (prior to amalgamation; after this, the percentage of mercury is approximately 50%), and zinc 2%.
- -
- MTA
It is a refined hydrophilic powder derived from Portland cement (a basic component of concrete used in the construction industry) [6]. The main molecules present in MTA are calcium and phosphorus ions, derived mainly from tricalcium silicate, tricalcium aluminate, tricalcium oxide, and silicate oxide [7]. Bismuth is a heavy metal and is added to cement in the form of bismuth oxide (Bi2O3) in a ratio of 4:1 to provide radiopacity to the MTA for radiological diagnosis. MTA cement is prepared by mixing its powder with sterile water using a powder-to-liquid ratio of 3:1. After hydration, calcium hydroxide and a hydrated calcium silicate gel are formed, which solidify into a hard structure in about 165 min. Multiple versions of the MTA have been studied to improve its limitations, among which are the setting time and the difficulty of handling [6].
- -
- Zinc-oxide eugenol cementsTwo modifications of zinc-oxide eugenol cement have been recommended as root fillers:
- a.
- SuperEBA is a reinforced zinc-oxide eugenol cement. The powder contains 60% zinc oxide with 6% natural resin and 34% alumina. The liquid contains 62.5% orthohetoxybenzoic acid (EBA) and 37.5% eugenol [6].
- b.
- IRM is a zinc-oxide eugenol cement reinforced with 20% poly-methyl methacrylate in the powder. The eugenol fluid remains unchanged. Its composition would remain in IRM as 80% zinc oxide and 20% polymethylmethacrylate, and the liquid is 99% eugenol [6,7].
- -
- Guttapercha
Guttapercha is derived from the sap of trees, mainly from the genus Palaquium (Palaquium gutta). The guttapercha was introduced by Bowman in 1867 to fill the space of the root canal. Guttapercha for endodontic use contains 20% guttapercha as a matrix, 66% zinc oxide as a filler, 11% heavy metal sulfates as radiopacifiers, and 3% waxes or resins as a plasticizer [6].
- -
- Retroplast
It is a fluid–resin compound composed of aromatic or aliphatic dimethacrylate monomers, such as bisphenol-A-glycidyl methacrylate (BisGMA), triethyl glycol dimethacrylate (TEGDMA), and urethane dimethacrylate (UDMA). A technique using Retroplast bound with the dentin-binding agent GLUMA (Heraus Kulzer, Werheim, Germany) was introduced as a root end filler in 1984 [6].
- -
- RRM (root repair materials)
They are the latest generation of bioceramic cements. They are calcium phosphate silicate cements (CPSC) containing phosphate salts added to conventional calcium silicate cements. Examples of CPSCs are EndoSequence Root Repair Material Putty (ERRM Putty; Brasseler USA, Savannah, GA, USA), EndoSequence Root Repair Material Paste (ERRM Paste; Brasseler USA), iRoot BioAggregate (Innovative Bioceramix, Vancouver, BC, Canada), and TotalFill® BC RRM™ Putty (FKG, La Chaux-de-Fonds, Switzerland) [6].
Albrektsson et al. [8] have been indicating for years that peri-implant bone loss does not present a single causal factor but that it derives from a cluster of factors that have as their origin a reaction to the initial foreign body of the organism and that is affected by other types of elements such as poor clinical management, previous diseases of the patient, smoking, genetic disorders or patients with previous periodontitis, or adverse effects of pharmaceuticals. This makes it difficult to treat peri-implant pathology, for which there is still no effective consensual treatment [8].
According to some published studies, the prevalence of patients with peri-implantitis was 18.8%, while the prevalence of implants with peri-implantitis was 9.6%. There is a high incidence of peri-implantitis after 5 years of function in patients with a previous history of peri-implantitis and in smokers [9].
Due to the incidence and prevalence of peri-implant diseases, it is essential to extend the life of the tooth, with the placement of an implant being the last option. The problem that entails the maintenance of the tooth is the patient’s acceptance. This is due to the economic cost of the treatment for the conservation of the tooth and the difficulty for the patient to understand that this treatment will extend the useful life of the tooth but will not keep it in the mouth for a lifetime.
1.1. Prognosis of Periapical Surgery
Several studies have described the results of periapical surgery. Song et al. [2], in 2011, conducted a study to evaluate the success of periapical surgery, finding 92.9% success at 2 years. Later, in 2012, a study by Von Arx et al. [10] obtained an 84% success rate in periapical surgery at 12 months, and this success rate dropped to 76% at 5 years. In another study conducted in 2019 by Huang et al. [11], the success rate of surgical treatments was 95.2% with a follow-up of between 5 and 9 years.
1.2. Success Criteria for Periapical Surgery
The success criteria for periapical surgery were described by Molven et al. [12] in 1996 as:
- Complete healing: The periodontal space is normal or slightly increased, a uniform hard lamina or with a defect of less than 1 mm is observed, and the bone repair is complete [12].
- Incomplete healing (scar tissue): It is considered as incomplete healing when there is decreased rarefaction with an irregular contour that extends angularly into the periodontal space. Rarefaction can be located asymmetrically in relation to the apex of the root with or without visible internal bone structures [12].
- Uncertain healing: In cases of uncertain cure, reduced bone rarefaction with circular or semicircular periphery around the apex is found [12].
- Failure: Considered when bone rarefaction increases or does not change, and clinical signs and symptoms persist [12].
Cases of complete and incomplete healing were considered as success and cases that do not show signs of cure as failure. As for the cases of uncertain cure, the studies with a shorter review period considered them as failure, and those that follow-up more extensively re-evaluate them, considering them as success or failure depending on the new situation [12].
1.3. Prognostic Factors for Periapical Surgery
Variables that have been identified as affecting the outcome of surgical treatment include sex, age, tooth type, preoperative symptoms, postoperative complications, postoperative healing time, periapical lesion size, and root-filling material [13,14].
In a meta-analysis studying patient-related, tooth-related, and treatment-related prognostic factors related to the outcome of periapical surgery, von Arx et al. [10] found higher success rates in anterior teeth, teeth with radiographic lesions less than 5 mm in diameter, teeth with good radiographic density of existing root canal filling, surgeries done for the first time, addition of MTA as root end filling material, and when endoscope was used [10,13,15,16]. Lower cure rates were observed when patients had preoperative pain and if root end preparations were performed with burs [15,16].
1.4. Objectives
The main objective of this work was the evaluation of the prognosis of periapical surgery and its relationship with the material used for the sealing of the root preparation, comparing the results of each of them.
The secondary objective was the evaluation of the influence of the surgical technique, microsurgery, or conventional technique, on the prognosis of periapical surgery.
2. Materials and Methods
A systematic review of the literature on the prognosis of periapical surgery was conducted. Following the PICO (patients, intervention, comparison, outcome) criteria, the question was asked: “In patients requiring periapical surgery (patient), is the retrograde filling material (comparison) used in apicectomy (intervention) determinant for the success of the treatment (outcome)?”
- Patients: Patients requiring periapical surgery for the presence of periapical lesion.
- Intervention: Retrograde filling in apicectomy.
- Comparison: Different materials (or nothing) used for backsighting. The materials compared were MTA, SuperEBA, IRM, RRM, amalgam, and Retroplast. The following comparative groups were established:
- (1)
- MTA vs. MRI;
- (2)
- MTA vs. SuperEBA;
- (3)
- MTA vs. amalgam;
- (4)
- MTA vs. RRM;
- (5)
- MTA vs. Retroplast;
- (6)
- MRI vs. SuperEBA;
- (7)
- MRI vs. amalgam;
- (8)
- MRI vs. guttapercha;
- (9)
- Amalgam vs. SuperEBA;
- (10)
- SuperEBA vs. Retroplast.
- Outcome: Tooth survival.
In these comparative groups, the number of teeth whose treatment had failed was evaluated according to the material used. Cases of complete and incomplete healing were considered as success and cases of uncertain cure as failure [12].
2.1. Eligibility Criteria
The types of articles selected were meta-analyses, systematic reviews (SR), randomized controlled trials (RCTs), non-randomized controlled trials (ECNRs), and retrospective studies (RE).
Studies retrieved using the search strategy were included if they met the following inclusion criteria: studies had to be in humans and to assess the success of periapical surgery by comparing the use of several materials or nothing as a filling of apical preparation. Included studies had to follow-up for at least 6 months. The language of publication of the articles had to be in English or Spanish and be available in full text. The success or failure of the treatments evaluated in the studies had to be per tooth.
In vitro or animal studies and studies that did not compare retrograde filling materials were excluded. We also excluded studies that did not assess the success or failure of periapical surgery.
2.2. Sources of Information, Search, and Selection of Studies
A systematic review of the scientific literature was carried out aimed at evaluating the prognosis of periapical surgery and the influence of the material used in the apical preparation on the success of the treatment.
The studies were identified in a literature search in the PubMed database using the keywords: (apicoectomy) OR (periapical surgery) OR (endodontic microsurgery) AND (root end filling material). A total of 218 results were obtained in this search.
We screened the titles and abstracts of retrieved articles according to selection criteria. Figure 1 shows the PRISMA diagram [17]. Among 232 studies after deleting duplicates, finally 31 papers were selected to be read full text. Nine studies were excluded in this step because of these reasons: 2 studies did not compare different materials [18,19], 1 study did not provide the necessary data [20], the authors were unable to find the full text paper [21,22], 1 was excluded because the full text was nor available un English or Spanish [23], and 3 were animal studies [24,25,26].
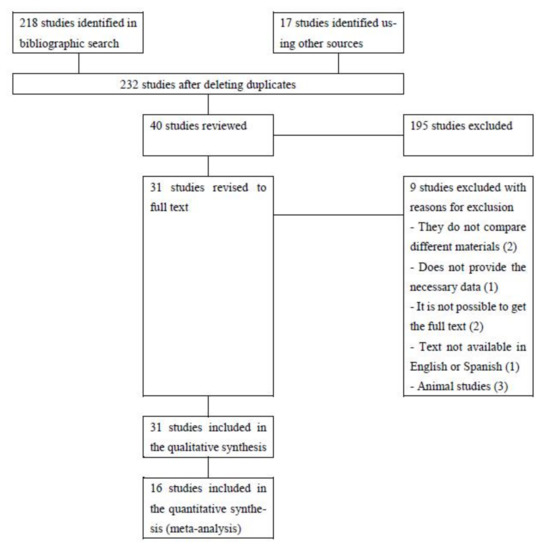
Figure 1.
Flowchart of included studies according to the PRISMA guidelines [17].
2.3. Data Extraction Process
Once the studies that met the selection criteria were selected, they were read independently. For the chosen studies, detailed information was recorded on the data for each of them. The data that were recorded are detailed below.
Data List
The information that was collected from each of the studies included in the selection process was as follows: the name of the author and the date of publication of the study, the type of study that had been carried out, the number of patients included in the study and their average age, the total number of teeth studied and the dental group to which it belonged, the previous pathology presented and for which the periapical surgery treatment had been performed, whether a root canal retreatment had been performed prior to the periapical surgery, the filling materials of the apical preparation used and the number of teeth in which each of them had been used, whether the treatment had been carried out with a conventional technique or had been performed under magnification (microsurgery), the follow-up time of the patients treated, the number of cases considered as success and the number of cases considered as failure of each study, and, finally, the conclusions reached by each of the authors.
2.4. Risk of Bias in Individual Studies and between Studies
For the analysis of the risks of bias, the CASPE guidelines adapted to each type of study were used [27,28,29]. The CASPe guideline for case-control studies [27] was used for retrospective studies [11,13,30,31,32,33], the CASPe guideline for clinical trials [29] was used for randomized [34,35,36,37,38,39] and nonrandomized clinical trials [2,40], and the CASPe guideline for cohort studies [28] was used for cohort studies [10,41]. We assessed the risk of bias between studies using an Excel (Microsoft Excel for Mac version 16.37, Microsoft Company, Washington, DC, USA) table in which we included all possible risks of bias and established risk based on all studies including: low risk (most studies showed low risk), medium (most studies showed unclear risk, or most studies showed low risk, but some of them were at high risk) or high (most studies showed high risk).
2.5. Synthesis of Results
All the data that were extracted from the jobs found by searching were entered into the Excel program (Microsoft Excel for Mac version 16.37). A series of tables were developed to compare the data collected in each of the studies.
2.6. Additional Analysis
Meta-analyses were performed in the groups comparing the use of MTA, SuperEBA, IRM, and RRM as retrograde filling material in periapical surgery. The comparative groups were as follows:
- MTA vs. SuperEBA;
- MTA vs. IRM;
- MTA vs. RRM;
- IRM vs. SuperEBA.
The software used to perform this meta-analysis was the Review Manager 5.3 program (Review Manager (RevMan) (computer program). Version 5.3.: The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark, 2014).
To prepare the meta-analysis, we performed the identification and measurement of the heterogeneity of the studies based on I2. Statistic I2 describes the percentage of variability in effect estimates that is due to heterogeneity rather than sampling error (chance). For this reason, if I2 was greater than 75%, the meta-analysis was performed for random effects and otherwise for fixed effects. A fixed-effect meta-analysis provides a result that can be considered a typical effect of the intervention of the studies included in the analysis. When there is heterogeneity in studies that cannot be easily explained, an analytical approach is to incorporate it into a random-effects model. A random-effects meta-analysis model includes the assumption that the effects calculated in the different studies are not identical but follow some distribution [42].
Regarding the analysis of the results of the meta-analysis, the forest plot was used. The global effect test (p) was also used. We judged the result to be statistically significant if the overall effect test (p), which measures the statistical significance of the meta-analysis result, was less than 0.05. In addition, a sensitivity analysis was carried out, eliminating one of the studies each time, to assess whether there was a significant modification of the results [42].
3. Results
3.1. Study Characteristics
Of the sixteen studies that were selected for quantitative synthesis, there were, depending on the type of study, six retrospective studies (RE) [11,13,30,31,32,33], six randomized controlled trials (RCT) [34,35,36,37,38,39], one cohort study (CS) [10], one retrospective cohort study (RCS) [41], and two non-randomized clinical trials (NRCT) [2,40]. The most important characteristics of these studies that were finally selected are summarized in Table 1.

Table 1.
Characteristics of the selected studies.
3.2. Outcome Measures of the Studies
All included articles used the same outcome measure (presence or absence of clinical symptoms/signs, radiographic assessment of bone reform, and hard lamina around the apical area of the tooth root) with an observation period from 6 months [40] to 9 years [13]. All characterized the results as “complete healing”, “incomplete healing”, “uncertain healing”, and “failure” [43].
3.3. Study Design
Overall, the designs of the included studies did not differ much. Mos of them performed a surgical intervention, the 3 mm apical of the root were removed, the preparation of the end of the root was carried out by burs or ultrasound, and subsequently, the experimental or control retrograde filling material was applied for each group.
In addition, the outcome measures were comparable. For each study, the existence of clinical symptoms or signs or the enlargement of bone radiolucency after surgery were defined as “failure”. When there was no presence of clinical symptoms/signs but no reduction in periapical radiolucency, they were defined as “uncertain cure”. No clinical symptoms/signs and elimination of bone radiolucency with or without complete reuptake of the hard lamina was defined as “complete healing” or “incomplete healing”, respectively [43].
3.4. Risk of Bias in Studies
The risk of bias was analyzed for each study individually. The results of this analysis for each study are in Appendix A (Table A1, Table A2 and Table A3).
3.4.1. Retrospective Studies
The study of Chan et al. [13] does not make it clear whether there was blinding of the evaluators. In the study by Dorn et al. [30], it is not clearly specified how to evaluate the results, whether there was more than one examiner, and whether there was blinding. In addition, they did not consider factors that can affect the result, such as type of tooth, type of restoration, or previous pathology. In the study of Huang et al. [11], it was not clear how the cases were assigned, and in the comparison of the material used, one of the samples was much larger than the other. In the case of the study by Tortorici et al. [33], it was not specified whether there was blinding in the outcome assessment or whether there was more than one assessor. It also did not consider some of the possible factors that may influence the results, such as the type of tooth restoration or previous pathology (Appendix A, Table A1).
3.4.2. Randomized and Non-Randomized Controlled Trials
In none of the included studies [2,34,35,36,37,38,39,40] was it possible to blind clinicians due to the characteristics of the procedure. In the study of Chong et al. [34], factors that may affect the outcome of the treatment, such as type of tooth, restoration, or previous pathology, were not considered. As for the work of Wälivara et al. [36] in 2011, some of the factors that can influence the treatment, such as the type of tooth restoration, were also not considered. It did specify the type of previous pathology but did not relate it to the results. Shin et al. [2] did not specify whether the assignment of the use of one backshoot material or another was randomized. Nor was it specified how many teeth of the total sample were treated with each of the materials or the results of each of the materials separately (Appendix A, Table A3).
3.4.3. Cohort Studies
Neither of the two included studies [10,41] specified whether there was blinding of the assessors (Appendix A, Table A3).
3.5. Results of Individual Studies
The results regarding the success and failure of each of the materials compared are detailed in Appendix B (Table A4).
3.6. Summary of Results
3.6.1. MTA vs. SuperEBA
Four studies compared results between MTA and SuperEBA [10,32,37,40]. One of them was a randomized controlled study (RCT) [37], another of the studies was a non-randomized controlled study (NRCT) [40], the third was a cohort study [10], and the fourth was a retrospective study [32].
In the Song, Jung et al. [32] study, there were no statistically significant differences between the outcomes of cases treated with MTA (85.6% success) and those treated with SuperEBA (85.5% success).
The study by Kim et al. [37] did not identify any significant difference in the 4-year success rates of MTA and Super EBA as retrograde filling materials in endodontic microsurgery. In addition, compared to short-term outcomes (1 year), long-term follow-up outcomes (4 years) were not significantly different.
In the study by Ögütlü et al. [40] also, no significant differences were found between the two materials. As for the MTA, 92.9% of success was obtained compared to 89.3% of the SuperEBA.
The study by Von Arx et al. [10] did find differences between the two materials. The success rate was higher in cases treated with MTA (86%) than with SuperEBA (67%).
Figure 2 shows the forest plot of the comparison between MTA and SuperEBA. In this case, the measurement of the heterogeneity of the studies using I2 resulted in 0%, so the meta-analysis was performed on a fixed-effect basis.
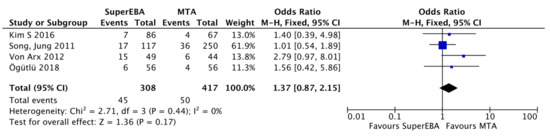
Figure 2.
Forest plot of comparison between the failure results between MTA and SuperEBA [10,32,37,40].
The overall result of the meta-analysis favoured the MTA. Based on these results, the use of MTA as a retrograde filling material in periapical surgery has less risk of failure than the use of SuperEBA. However, the overall effect test (p) was greater than 0.05 (p = 0.17), and if the diamond confidence interval is considered, it crosses the null value of the outcome variable (1.37 (95% CI: 0.87, 2.15)), and this indicates that the result is not statistically significant. When performing the sensitivity analysis by removing one of the studies, the result was not significantly modified.
3.6.2. MTA vs. IRM
Three made a comparison of results between the MTA and the IRM [11,32,34]. Two of them were retrospective studies (ER) [11,32], and one was a randomized controlled trial (RCT) [34].
The Song, Jung et al. [32] study did find significant differences between the results of cases treated with MRI and MTA as a filling material. The success results were 85.6% for the MTA and 75.5% for the IRM.
Huang et al. [11] resulted in high cure rates (78.3%) and long-term survival (95.2%) (5 to 9 years). They concluded that the type of retrograde filling material does influence the long-term outcome. The results obtained were 79.5% success in MTA treatments compared to 57.5% success in IRM treatments, but in the case of IRM, the sample was too small and not comparable with that of MTA.
Chong et al. [34] found that the use of MTA as a retrograde filling material obtained a higher success rate, although not statistically significant, than the use of IRM.
Figure 3 shows the forest plot of the comparison between MTA and IRM. The result of I2 for the measurement of the heterogeneity of the studies was 0%, and therefore, the meta-analysis was performed for fixed effects.
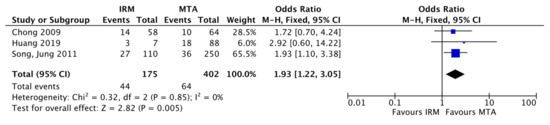
Figure 3.
Forest plot comparison. Failure results between MTA and IRM.
The overall result of the meta-analysis favoured, as in the previous case, the MTA. Therefore, it could be said that the use of MTA as a retrograde filling material in periapical surgery has less risk of failure than the use of MRI. In this case, the overall effect test (p) was less than 0.05 (p = 0.005), so the result is statistically significant. Regarding the confidence interval, the diamond did not cross the null value of the outcome variable (1.93 (95% CI: 1.22, 3.05)), which also indicates that there are significant differences. Sensitivity analysis performed by removing one of the studies showed similar results.
3.6.3. MTA vs. RRM
Three compared MTA to RRM as a sealing material [13,38,39]. Two of them were randomized controlled studies (RCT) [38,39], and the third was a retrospective study (RE) [13].
Chan et al. [13] concluded in their retrospective study that there was a high success rate in teeth treated with microsurgery with both materials. Both materials can be used as retrograde filling material with great predictability and favorable results.
Both the studies of Safi et al. [38] and Zhou et al. [39] did not find statistically significant differences in the outcomes of cases treated with MTA or RRM.
Figure 4 shows the forest plot of the comparison between MTA and RRM. Meta-analysis was performed on a fixed-effect basis, as measurement of study heterogeneity using I2 resulted in 0%.
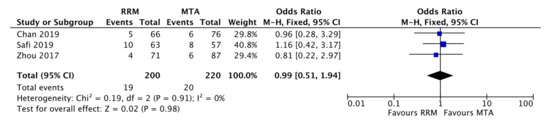
Figure 4.
Forest plot of comparison between the results of failure between MTA and RRM.
The overall result of the meta-analysis favoured the RRM slightly. The overall effect test (p) was greater than 0.05 (p = 0.98), and the diamond confidence interval in this case did cross the null value (0.99 (95% CI: 0.51, 1.94)), so the result is not statistically significant. The sensitivity analysis did not show a significant change in the results. Both MTA and RRM had similar results as retrograde filling materials in periapical surgery.
3.6.4. SuperEBA vs. IRM
Three studies compared the results obtained with SuperEBA and IRM [30,32,36]. Two of these studies were retrospective studies (RE) [30,32], and the other was a randomized controlled study (RCT) [36].
Dorn et al. [30] and Song, Jung et al. [32] found no significant differences in results between SuperEBA and IRM.
Wälivara et al. [36] concluded that both materials tested can serve as satisfactory retrograde filling material. A slight bias was found in favour of IRM, but the performance of Super-EBA could be improved by altering the powder/liquid mixing ratio to obtain greater plastic consistency.
In this case, meta-analysis was performed for random effects, as the measurement of study heterogeneity using I2 resulted in 77% (Figure 5).
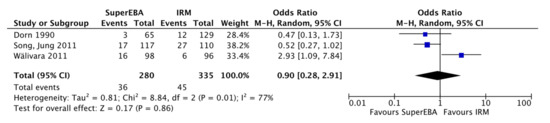
Figure 5.
Forest plot comparison failure results between SuperEBA and IRM.
The overall result of the meta-analysis favoured the SuperEBA slightly. The overall effect test (p) was greater than 0.05 (p = 0.86), and the diamond confidence interval crosses the null value (0.90 (95% CI: 0.28, 2.91)), thus indicating that there are no statistically significant differences in the use of SuperEBA versus IRM as a retrograde filling material in periapical surgery.
In addition, when performing the sensitivity analysis, the results changed significantly. We did not withdraw any studies, as relevant information was lost. By eliminating the study by Dorn et al. [30], the diamond moves to the right, favouring the MRI, leaving its confidence interval crossing the null value. By eliminating the Song, Jung et al. [32] study, the diamond increases its confidence interval significantly without changing position, slightly favouring the SuperEBA. Finally, by eliminating the study of Wälivara et al. [36], the diamond moves further to the left, leaving its confidence interval without crossing the null value, in favour of the SuperEBA.
As heterogeneity is too high, and the results change significantly in the sensitivity analysis, the results should be interpreted with caution.
3.6.5. Other Comparisons
Table 2 summarizes the results of studies conducted by other material comparisons not included in the meta-analysis.

Table 2.
Results of the studies carried out by other comparisons of materials.
Von Arx et al. [10] conducted a cohort study where they compared the results of MTA, SuperEBA, and Retroplast as retrograde filling material in periapical surgery, finding better results in treatments performed with MTA (86%) than with Retroplast (75%) or SuperEBA (67%).
Regarding the comparison between MTA and amalgam, the search only gave a single result: a retrospective study conducted by Tortorici et al. [33] that compared the results of periapical surgery at 12 months and 5 years comparing the use of amalgama and MTA as a backsighting material. They concluded that the use of microsurgery and MTA as a filling material gave results five times greater than with conventional surgery and amalgam as a retrograde filling material.
Dorn et al. [30] conducted a retrospective study comparing the results of the use of SuperEBA, amalgam, and IRM as retrograde filling materials in periapical surgery. The results obtained were better in treatments with retrograde filling materials with reinforced zinc-eugenol oxide, such as SuperEBA or IRM, than with amalgam.
Wälivara et al. [35] compared, in a randomized controlled study, the use of IRM and guttapercha in periapical surgery and concluded that both materials, guttapercha and IRM, are suitable as retrograde filling materials according to the results after 12 months of follow-up.
3.7. Conventional Technique vs. Microsurgery
Of the 16 studies that were included in the quantitative review, the comparison was made in terms of the number of failures according to the technique used, namely conventional technique or microsurgery. The results of this comparison are shown in Table 3.

Table 3.
Results of studies regarding the type of surgical technique.
Only one of the selected studies made a comparison between conventional technique and microsurgery [33]. In this study, results were found to be five times better with microsurgery techniques than with conventional technique.
Comparing the results of all the studies included in the quantitative review, out of a total of 3730 teeth treated, 1369 were treated by conventional surgery and 2215 by microsurgery. Of the 1369 teeth that were treated with conventional surgery, 22.9% failed (314 teeth). As for the teeth treated by microsurgery (2215), the failures were a total of 274 (12.37%).
Of the total of the studies included in this review, a total of 3730 teeth were studied and treated with periapical surgery with one of the techniques mentioned. Of these treated teeth, 3142 teeth obtained a successful treatment result (84.2%), and 588 resulted in failure (15.8%).
3.8. Risk of Bias between Studies
3.8.1. Cohort Studies
In both studies, the topic is clearly defined, cohorts were recruited in the most appropriate way, factors that could modify the results have been considered, the follow-up time is long enough, and the studies explain all the results and agree with other available studies. Neither study specifies whether blinding of assessors was performed [10,41]. The overall risk of bias of the cohort studies included in this review has been defined as low.
3.8.2. Case-Control Studies
In all of these studies [11,13,30,31,32,33], the topic was clearly defined, and an appropriate method was used to answer the question. The included cases were recruited acceptably in all cases except the study by Huang et al. [11], where the method was not fully specified but was classified globally as low risk. Regarding the measurement of results, half of the studies [11,31,32] made an accurate measurement of the results and were qualified as low risk, and the other half [13,30,33] did not specify some aspects of the measurement, so they were classified as medium risk. That is why all of them they were classified globally as medium risk. As for the confounding factors, most of the studies [11,13,31,32] took them into account, so the global has been classified as medium risk. Most studies [11,13,31,32] considered all the variables that could affect the outcome, so the studies have been classified as medium risk. In terms of results, we have classified studies as low risk, as most have credible results that correspond to the available evidence. The overall risk outcome is low for case-control studies.
3.8.3. Clinical Trials
In all studies [2,34,35,36,37,38,39,40], the question was clearly defined, so the overall risk of bias is low. Most studies [34,35,36,37,38,39] randomly assigned patients, and only two of the studies [2,40] did not perform randomization of allocation, so it was considered globally as low risk. In all cases, all patients included until the end of the follow-up period were considered, and the casualties were quantified. Due to the characteristics of the procedure under study, the blinding of personnel or operator is not possible. For this reason, this item was classified as high risk. In all studies, the groups were similar at the beginning of the trial; only in one case [2] was the exact number of patients assigned to each group not specified. They were rated globally as low risk. In all studies, all groups studied were treated with the same procedure, and the effect of the treatment has a high success rate, so both concepts were established as low risk. The accuracy of the effect in general corresponds to previous studies and can be applied to all media, so they have been rated as low risk. All studies except one [2] have taken into account all clinically important outcomes, so it was also defined as low risk. In all studies, the benefits justify the risks, so it was rated as low risk.
4. Discussion
4.1. Summary of the Evidence
4.1.1. Prognosis of Periapical Surgery
Many studies have been published on the outcome of endodontic surgery. However, their designs, treatment protocols, follow-up periods, and inclusion and exclusion criteria are extremely variable. Tsesis et al. [16] performed a meta-analysis of the literature, finding 91.6% of success of periapical surgery (95% CI, 85.9%–95.1%) and considering factors that may affect success (age, gender, type of tooth treated, retrograde filling material used, and use of magnification). Another meta-analysis by Kang et al. [44] found a 92% of success for periapical microsurgery versus 80% of success for non-surgical retreatment. Song et al. [45] obtained results of 93.3% success of long-term surgical treatments. This corresponds to the results obtained in this systematic review and meta-analysis, where the success results for periapical surgery treatments were 84.2%.
4.1.2. Comparison between Retrograde Filling Materials
The most common retrograde filling material in periapical surgery used in endodontic surgery treatments has been silver amalgam; nevertheless, in recent years, its use has been questioned for reasons such as microfiltration, biocompatibility, corrosion, stains, and poor overall performance [5,7], and some studies suggest better results when using IRM or SuperEBA over the use of amalgam [30]. Tortorici et al. [33] also obtained better results with MTA than with amalgam, with 37.5% failure of treatments in which amalgam was used compared to 10.4% failure of MTA. Regarding the results found in this review and meta-analysis, 32.5% of treatments in which amalgam was used ended up in failure, which gives a success rate of 67.5%.
Currently, materials such as IRM, SuperEBA, and MTA [34,36] have been replacing the use of amalgam as retrograde filling materials in periapical surgery. Several studies have been conducted comparing the results of treatments with these materials.
Regarding the comparison between MTA and SuperEBA, most of the studies included in this review found no significant differences between both materials [32,37,40]. However, Von Arx et al. [10] did find differences between the two materials, with a higher success rate in cases treated with MTA (86%) than with SuperEBA (67%). In this review, the results obtained in the meta-analysis comparing the use of MTA versus SuperEBA correspond to the results of most studies. The overall result of the meta-analysis favours the MTA (OR: 1.37 (95% CI: 0.87, 2.15)). According to these results, the use of MTA as a retrograde filling material in periapical surgery has less risk of failure than the use of SuperEBA, but the difference is not statistically significant.
In the comparison between MTA and IRM, Chong et al. [34] reported that MTA was not significantly better than IRM (84% and 76% success rates, respectively). Song, Jung et al. [32] and Huang et al. [11] found significant differences, with better results in treatments with MTA than with IRM. The result of the meta-analysis in this comparison also favours MTA (OR: 1.93 (95% CI: 1.22, 3.05)). Therefore, it could be said that the use of MTA as a retrograde filling material in periapical surgery has less risk of failure than the use of IRM, as most of the studies confirm.
Three of the included studies compared the use of MTA versus RRM [13,38,39]. None of these studies found significant differences in outcomes between the two materials. Chan et al. [13] concluded that both materials can be used with great predictability and favorable results. The result of this meta-analysis slightly favours RRM, but the difference is not statistically significant (OR: 0.99 (95% CI: 0.51, 1.94)). Therefore, both MTA and RRM have favorable results as retrograde filling materials in periapical surgery. More studies are needed to assess the results of the RRM.
There were three studies comparing the use of IRM and SuperEBA [30,32,36]. The study by Wälivara et al. [36] found certain differences, with slightly better results in IRM treatments. In the other two studies [30,31,32], no significant differences were found between the results of both materials. The result of the meta-analysis performed in this review slightly favours the SuperEBA, but the difference is not significant (OR: 0.90 (95% CI: 0.28, 2.91)). Further studies would be needed to arrive at conclusive results.
As for the rest of the materials compared, the use of Retroplast gave better results than SuperEBA but worse than with MTA in a study conducted by Von Arx et al. [10].
Wälivara et al. [35] compared the use of IRM and guttapercha in periapical surgery, finding no significant differences between the two materials.
In this review, only the type of material used when performing the retrograde filling of the root preparation was considered. However, it would be necessary to consider other factors that may affect the outcome of the treatment, such as the performance of orthograde retreatment prior to surgical treatment, the type of periapical lesion, the experience of the operator, and the presence of symptoms prior to periapical surgical treatment.
4.1.3. Conventional Surgery vs. Microsurgery
Between conventional surgery and microsurgery, only one of the included studies [33] compared the results obtained with both techniques, finding better results with microsurgery.
To compare the outcomes of conventional surgical treatment and microsurgery, the ideal systematic review should include randomized controlled studies that compare the two procedures. In this review, we grouped the results in order to compare conventional treatment and microsurgery of each study separately, as only one of the clinical studies directly compared the results of these two techniques.
Regarding the results found in this review, they were more favorable in the case of treatments performed by microsurgery, with 12% of cases failed compared to 22% of conventional surgery. This corresponds to previous studies where much better results have been found by microsurgery than with traditional techniques: in a retrospective study about the success of microsurgery, a 91% of success was found in microsurgery compared to 44.2% with conventional surgery [46]. In a two-part systematic review by Setzer et al. [47,48], a 94% of success of microsurgery was found compared to 59% of success of conventional surgery [47,48].
4.1.4. Follow-Up Time
In most cases, the results were limited to the one-year follow-up period. Although this allows comparison of the results of different studies after the same observation period, it does not consider the fact that, in surgical procedures, the risk of post-treatment emerging disease could increase over time. This fact was underlined by Kvist et al. [49], which reported relapses in four surgically treated participants between one and four years of follow-up. Therefore, the results per year may not reflect the longer-term results that researchers need to be aware of.
4.2. Limitations
The limitations of this review were the following: few studies are available, the included studies do not have the same methodological design, the evaluation criteria for success or failure of surgery are subjective, the follow-up time differs greatly between studies, and only the type of material is taken into account in many of the studies, but there are other factors that influence the success or failure of periapical surgery, such as the type of tooth restoration, the performance or not of duct retreatment prior to surgery, the type of tooth where the periapical surgery has been performed, surgical technique performed, and experience of the operator.
5. Conclusions
- In relation to the main objective, the conclusions are:
- (a)
- Periapical surgery obtains successful results in 84% of cases.
- (b)
- All the materials used as retrograde filling in periapical surgery obtain satisfactory results. More modern materials (MTA, RRM, SuperEBA, IRM) obtain better results than amalgam.
- (c)
- Among these more modern materials, MTA obtains better results than IRM, while the comparison of the rest of the materials did not yield conclusive results. In the comparison of MTA and SuperEBA, the results favour MTA. As for RRM, it obtains better results than MTA. Additionally, between IRM and SuperEBA, the results favour SuperEBA.
- As for the secondary objective, microsurgery techniques obtain better results than conventional techniques.
Special Comments
The maintenance of the teeth should be a priority for the dentist and for the patient above its replacement by prosthetic elements, especially in a world in which life expectancy is high, and durability must be given to the treatments that are performed on patients. It must be remembered that dental implants are not the definitive solution; they present complications and pathologies (fractures and loosening of screws, prosthesis fractures, infections, mucositis, or peri-implantitis) that can be difficult to treat or resolve and often end with the loss of the implant. On the other hand, there is not always adequate bone availability to place implants, which leads to costly bone regeneration treatments that do not always give the expected result. Tooth replacement using tooth-supported fixed prostheses is also an option, but it involves grinding adjacent teeth.
The perspective of the patient today is also important; in Spain, dentistry is private (the patient pays for the treatments out of pocket), so many times, faced with the prospect of possible future loss of the tooth, they decide on extraction and replacement using implants, tooth-supported fixed prostheses, or removable prostheses in order to avoid spending money that is not going to give them a 100% predictable result (which happens in all dental treatments, but the perception is different with respect to endodontic teeth). The fact that the results of a periapical surgery have to be evaluated after some time as well as the uncertainty discourages many patients from undergoing this type of treatment, betting on what they consider safer in the long term and investing their money in it.
Regarding the materials, in this work, it has been observed that the most innovative materials (MTA, RRM, SuperEBA, or IRM) offer better results in terms of success than amalgam. Being within these, MTA is the one that seems to have better results than the rest. Of course, the authors know that not only the type of material used will be decisive in the success of periapical surgery since there are multiple factors that can influence the result; however, it can be determined that one of the influential factors is the material used, so using materials that increase the success rate according to scientific evidence will increase the probability of success in the treatment.
On the other hand, the use of magnification techniques allows a better cleaning and obturation of the area, which also increases the probability of success of the treatment.
Based on the results obtained in this study, the authors consider that periapical surgery can and should be the treatment of choice for endodontic teeth in which maintenance in the mouth is feasible (lack of mobility, adequate crown-root ratio, sufficient remaining coronary structure, absence of active infection, position of the tooth, importance in the arch, feasibility of treatment, etc.). It is important in any case, as in all areas of dentistry, to make an appropriate selection of the case to reduce the risk of failure.
Author Contributions
Bibliographic search, analysis of results, preparation of the meta-analysis, and writing of the manuscript, A.A.-C. (data curation, formal analysis, investigation, methodology, resources, writing—original draft) and B.P.-P. (conceptualization, data curation, formal analysis, investigation, methodology, resources, visualization, writing—original draft); analysis of results and correction of the manuscript, N.Q.-L. (formal analysis, resources, writing—review and editing), M.L.-C. (formal analysis, writing—review and editing), and Á.S.-S. (formal analysis, writing—review and editing); study coordination, J.M. (project administration, supervision). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| BisGMA | Bisphenol-A-glycidyl methacrylate |
| CPSC | Calcium phosphate silicate cements |
| GLUMA | Dentin binding agent |
| IRM | Zinc-oxide eugenol cement |
| MTA | Mineral trioxide aggregate |
| RRM | Root repair materials |
| SuperEBA | Zinc-oxide eugenol cement with orthohetoxybenzoic acid (EBA) |
| TEGDMA | Triethyl glycol dimethacrylate |
| UDMA | Urethane dimethacrylate |
| CPSC | Calcium phosphate silicate cements |
Appendix A
Risk of bias assessment tables according to the CASPe guidelines.

Table A1.
Risk of bias analysis for case-control studies according to CASPe guidelines [27].
Table A1.
Risk of bias analysis for case-control studies according to CASPe guidelines [27].
| Cases and Controls | Chan et al. 2019 [13] | Dorn et al. 1990 [30] | Huang et al. 2019 [11] | Lui et al. 2014 [31] | Song, Jung et al. 2011 [32] | Tortorici et al. 2014 [33] |
|---|---|---|---|---|---|---|
| Do you focus on a clearly defined topic? | Yes | Yes | Yes | Yes | Yes | Yes |
| Have the authors used an appropriate method to answer the question? | Yes | Yes | Yes | Yes | Yes | Yes |
| Were the cases recruited in an acceptable way? | Yes | Yes | Ns | Yes | Yes | Yes |
| Were the controls selected in an acceptable manner? | Yes | Yes | Ns | Yes | Yes | Yes |
| Was exposure accurately measured in order to minimize potential bias? | Ns | Ns | Yes | Yes | Yes | Ns |
| Have the authors taken into account the potential of confounding factors in the design and/or analysis? | Yes | No | Yes | Yes | Yes | No |
| Results: Have you adjusted for possible confounding factors? | Yes | Ns | Yes | Yes | Yes | No |
| Are the results accurate? Have the authors considered all the variables? | Yes | No | Yes | Yes | Yes | No |
| Do you believe the results? | Yes | Yes | Ns | Yes | Yes | Yes |
| Are the results applicable to your medium? | Yes | Yes | Yes | Yes | Yes | Yes |
| Do the results of this study match other available evidence? | Yes | Yes | Ns | Yes | Yes | Yes |
NS, not specified in the article or not clear.

Table A2.
Risk of bias analysis for clinical trials according to CASPe guidelines [28].
Table A2.
Risk of bias analysis for clinical trials according to CASPe guidelines [28].
| Clinical Trial | Chong et al. 2003 [34] | Wälivara et al. 2011 [36] | Kim S. et al. 2016 [37] | Ögütlü et al. 2018 [40] | Safi et al. 2019 [38] | Song, Shin et al. 2011 [3] | Wälivara et al. 2009 [35] | Zhou et al. 2017 [39] |
|---|---|---|---|---|---|---|---|---|
| Is the essay oriented to a clearly defined question? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Was the allocation of patients to treatments random? | Yes | Yes | Yes | No | Yes | No | Yes | Yes |
| Were all patients who entered the study adequately considered until the end of the study? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Was blinding maintained to patients, clinicians, and staff? | No | No | No | No | No | No | No | No |
| Were the groups similar at the beginning of the trial? | Yes | Yes | Yes | Yes | Yes | Ns | Yes | Yes |
| Apart from the intervention under study, were the groups treated in the same way? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Is the effect of the treatment very large? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| What is the accuracy of this effect? | Ns | Ns | Yes | Yes | Yes | Yes | Yes | Yes |
| Can these results be applied to your environment or local population? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Were all clinically important outcomes taken into account? | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Do the benefits to be obtained justify the risks and costs? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
NS, not specified in the article or not clear.

Table A3.
Risk of bias analysis for cohort studies according to CASPe guidelines [29].
Table A3.
Risk of bias analysis for cohort studies according to CASPe guidelines [29].
| Cohort Study | Kim D. et al. 2019 [41] | Von Arx et al. 2012 [10] |
|---|---|---|
| Do you focus on a clearly defined topic? | Yes | Yes |
| Was the cohort recruited in the most appropriate way? | Yes | Yes |
| Was the outcome accurately measured in order to minimize potential bias? | Ns | Ns |
| Have the authors taken into account the potential of confounding factors in the design and/or analysis? | Yes | Yes |
| Was the follow-up of the subjects long and complete enough? | Yes | Yes |
| What are the results of this study? Have the authors given the rate or ratio between exposed/unexposed? | Yes | Yes |
| Are the results accurate? | Yes | Yes |
| Do you find the results credible? | Yes | Yes |
| Do the results of this study match other available evidence? | Yes | Yes |
| Can the results be applied to your environment? | Yes | Yes |
| Can this change the clinical decision? | Yes | Yes |
NS, not specified in the article or not clear.
Appendix B

Table A4.
Results of success and failure of each of the materials compared.
Table A4.
Results of success and failure of each of the materials compared.
| Author and Date | Follow-Up | Sample | N Failures | % Failures | N Successes | % Successes | |
|---|---|---|---|---|---|---|---|
| MTA | Chan et al. 2019 [13] | >6 months | 76 | 6 | 7.8947 | 70 | 92,105 |
| Chong et al. 2003 [34] | 12 months | 64 | 10 | 15,625 | 54 | 84,375 | |
| Huang et al. 2019 [11] | 12 months | 88 | 18 | 20,455 | 70 | 79,545 | |
| Kim D. et al. 2019 [41] | 12–72 months | 244 | 26 | 10,656 | 218 | 89,344 | |
| Kim S. et al. 2016 [37] | 12 months | 67 | 4 | 5.9701 | 63 | 94.03 | |
| Ögütlü et al. 2018 [40] | 6 months | 56 | 4 | 7.1429 | 52 | 92,857 | |
| Safi et al. 2019 [38] | 12–24 m | 57 | 8 | 14,035 | 49 | 85,965 | |
| Song, Jung et al. 2011 [32] | 12 months | 250 | 36 | 14.4 | 214 | 85.6 | |
| Tortorici et al. 2014 [33] | 60 months | 479 | 50 | 10,438 | 429 | 89,562 | |
| Von Arx et al. 2012 [10] | 60 months | 44 | 6 | 13,636 | 38 | 86,364 | |
| Zhou et al. 2017 [39] | 12 months | 87 | 6 | 6.8966 | 81 | 93,103 | |
| TOTAL | 1512 | 174 | 1338 | ||||
| % | 11,508 | 89,153 | |||||
| SuperEBA | Dorn et al. 1990 [30] | > 6 months | 65 | 3 | 4.6154 | 62 | 95,385 |
| Kim S. et al. 2016 [37] | 12 months | 86 | 7 | 8.1395 | 79 | 91.86 | |
| Ögütlü et al. 2018 [40] | 6 months | 56 | 6 | 10,714 | 50 | 89,286 | |
| Song Jung et al. 2011 [32] | >12 months | 117 | 17 | 14.53 | 100 | 85.47 | |
| Von Arx et al. 2012 [10] | 60 months | 49 | 15 | 30,612 | 34 | 69,388 | |
| Wälivara et al. 2011 [36] | 12–21 months | 98 | 16 | 16,327 | 82 | 83,673 | |
| TOTAL | 471 | 64 | 407 | ||||
| % | 13,588 | 86,412 | |||||
| IRM | Chong et al. 2009 [34] | 12 months | 58 | 14 | 24,138 | 44 | 75,862 |
| Dorn et al. 1990 [30] | >6 months | 129 | 12 | 9.3023 | 117 | 90,698 | |
| Huang et al. 2019 [11] | 12 months | 7 | 3 | 42,857 | 4 | 57,143 | |
| Song, Jung et al. 2011 [32] | >12 months | 110 | 27 | 24,545 | 83 | 75,455 | |
| Wälivara et al. 2009 [35] | 12–38 months | 66 | 10 | 15,152 | 56 | 84,848 | |
| Wälivara et al. 2011 [36] | 12–21 months | 96 | 6 | 6.25 | 90 | 93.75 | |
| TOTAL | 466 | 72 | 394 | ||||
| % | 15,451 | 84,549 | |||||
| Amalgam | Dorn et al. 1990 [30] | > 6 months | 294 | 73 | 24.83 | 221 | 75.17 |
| Tortorici et al. 2014 [33] | 60 months | 458 | 172 | 37,555 | 286 | 62,445 | |
| TOTAL | 752 | 245 | 507 | ||||
| % | 32.58 | 67.42 | |||||
| RRM | Chan et al. 2019 [13] | 6–110 months | 66 | 5 | 7.5758 | 61 | 92,424 |
| Safi et al. 2019 [38] | 6–12–24 months | 63 | 10 | 15,873 | 53 | 84,127 | |
| Zhou et al. 2017 [39] | 1 week, 3, 6 and 12 months | 71 | 4 | 5.6338 | 67 | 94,366 | |
| TOTAL | 200 | 19 | 181 | ||||
| % | 9.5 | 90.5 | |||||
| Guttapercha | Wälivara et al. 2009 [35] | 12–38 months | 77 | 8 | 10.39 | 69 | 89.61 |
| TOTAL | 77 | 8 | 69 | ||||
| % | 10.39 | 89.61 | |||||
| Retroplast | Von Arx et al. 2012 [10] | 60 months | 77 | 19 | 24,675 | 58 | 75,325 |
| Total | 77 | 19 | 58 | ||||
| % | 24,675 | 75,325 |
References
- Kohli, M.R.; Berenji, H.; Setzer, F.C.; Lee, S.-M.; Karabucak, B. Outcome of Endodontic Surgery: A Meta-analysis of the Literature—Part 3: Comparison of Endodontic Microsurgical Techniques with 2 Different Root-end Filling Materials. J. Endod. 2018, 44, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Shin, S.-J.; Kim, E. Outcomes of Endodontic Micro-resurgery: A Prospective Clinical Study. J. Endod. 2011, 37, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Carr, G.B. Ultrasonic root end preparation. Dent. Clin. North Am. 1997, 41, 541–554. [Google Scholar] [CrossRef]
- Bodrumlu, E. Biocompatibility of retrograde root filling materials: A review. Aust. Endod. J. 2008, 34, 30–35. [Google Scholar] [CrossRef]
- Hauman, C.H.; Love, R. Biocompatibility of dental materials used in contemporary endodontic therapy: A review. Part 2. Root-canal-filling materials. Int. Endod. J. 2003, 36, 147–160. [Google Scholar] [CrossRef]
- Seedat, H.; Van Der Vyver, P.; De Wet, F. Micro-endodontic surgery Part 2: Root-end filling materials-A literature review. South Afr. Dent. J. 2018, 73. [Google Scholar] [CrossRef]
- Borisova-Papancheva, T.; Panov, V.; Peev, S.; Papanchev, G. Root-end filling materials-review. Scr. Sci. Med. Dent. 2015, 1, 7. [Google Scholar] [CrossRef][Green Version]
- Albrektsson, T.; Canullo, L.; Cochran, D.; De Bruyn, H. “Peri-Implantitis”: A Complication of a Foreign Body or a Man-Made “Disease”. Facts and Fiction. Clin. Implant Dent. Relat. Res. 2016, 18, 840–849. [Google Scholar] [CrossRef]
- Ting, M.; Craig, J.; Balkin, B.E.; Suzuki, J.B. Peri-implantitis: A Comprehensive Overview of Systematic Reviews. J. Oral Implant. 2018, 44, 225–247. [Google Scholar] [CrossRef]
- Von Arx, T.; Jensen, S.S.; Hänni, S.; Friedman, S. Five-Year Longitudinal Assessment of the Prognosis of Apical Microsurgery. J. Endod. 2012, 38, 570–579. [Google Scholar] [CrossRef]
- Huang, S.; Chen, N.-N.; Yu, V.S.; Lim, H.A.; Lui, J.-N. Long-term Success and Survival of Endodontic Microsurgery. J. Endod. 2019, 46, 149–157.e4. [Google Scholar] [CrossRef]
- Molven, O.; Halse, A.; Grung, B. Incomplete healing (scar tissue) after periapical surgery—radiographic findings 8 to 12 years after treatment. J. Endod. 1996, 22, 264–268. [Google Scholar] [CrossRef]
- Chan, S.; Glickman, G.N.; Woodmansey, K.F.; He, J. Retrospective Analysis of Root-end Microsurgery Outcomes in a Postgraduate Program in Endodontics Using Calcium Silicate–based Cements as Root-end Filling Materials. J. Endod. 2020, 46, 345–351. [Google Scholar] [CrossRef]
- Allen, R.K.; Newton, C.W.; Brown, C.E. A statistical analysis of surgical and nonsurgical endodontic retreatment cases. J. Endod. 1989, 15, 261–266. [Google Scholar] [CrossRef]
- Friedman, S. The prognosis and expected outcome of apical surgery. Endod. Top. 2005, 11, 219–262. [Google Scholar] [CrossRef]
- Tsesis, I.; Faivishevsky, V.; Kfir, A.; Rosen, E. Outcome of Surgical Endodontic Treatment Performed by a Modern Technique: A Meta-analysis of Literature. J. Endod. 2009, 35, 1505–1511. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Corbella, S.; Sequeira-Byron, P.; Tsesis, I.; Rosen, E.; Lolato, A.; Taschieri, S. Endodontic procedures for retreatment of periapical lesions. Cochrane Database Syst. Rev. 2016, 2016, CD005511. [Google Scholar] [CrossRef]
- Karan, N.B.; Aricioğlu, B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin. Oral Investig. 2020, 24, 1065–1072. [Google Scholar] [CrossRef]
- Da Silva, S.R.; Neto, J.D.D.S.; Schnaider, T.B.; Veiga, D.F.; Novo, N.F.; Filho, M.M.; Ferreira, L.M. The use of a biocompatible cement in endodontic surgery. A randomized clinical trial 1. Acta Cir. Bras. 2016, 31, 422–427. [Google Scholar] [CrossRef][Green Version]
- Jou, Y.T.; Pertl, C. Is there a best retrograde filling material? Dent. Clin. North Am. 1997, 41, 555–561. [Google Scholar] [CrossRef]
- Tang, Y.; Li, X.; Yin, S. Outcomes of MTA as root-end filling in endodontic surgery: A systematic review. Quintessence Int. 2010, 41, 557–566. [Google Scholar]
- Grossman, I.; Abu El Naag, A.; Peled, M. Root-end filling materials in apicoectomy—A review. Refuat Ha-Peh Eha-Shinayim 2003, 20, 49–80. [Google Scholar]
- Economides, N.; Pantelidou, O.; Kokkas, A.; Tziafas, D. Short-term periradicular tissue response to mineral trioxide aggregate (MTA) as root-end filling material. Int. Endod. J. 2003, 36, 44–48. [Google Scholar] [CrossRef]
- Baek, S.-H.; Lee, W.C.; Setzer, F.C.; Kim, S. Periapical Bone Regeneration after Endodontic Microsurgery with Three Different Root-end Filling Materials: Amalgam, SuperEBA, and Mineral Trioxide Aggregate. J. Endod. 2010, 36, 1323–1325. [Google Scholar] [CrossRef]
- Witherspoon, D.E.; Gutmann, J.L. Analysis of the healing response to gutta-percha and Diaket when used as root-end filling materials in periradicular surgery. Int. Endod. J. 2000, 33, 37–45. [Google Scholar] [CrossRef]
- Cabello, J.B. Plantilla para ayudarte a entender un Estudio de Casos y Controles. In Guías CASPe de Lectura Crítica de la Literatura Médica; Elsevier: Barcelona, Spain, 2005; pp. 13–19. Available online: https://redcaspe.org/casos_y_controles.pdf (accessed on 27 June 2022).
- Cabello, J.B. Plantilla Para Ayudarte a Entender Estudios de Cohortes. In Guías CASPe de Lectura Crítica de la Literatura Médica; Cuaderno II; Elsevier: Barcelona, Spain, 2005; pp. 23–27. Available online: https://redcaspe.org/cohortes11.pdf (accessed on 27 June 2022).
- Cabello, J.B. Plantilla Para Ayudarte a Entender un Ensayo Clínico. In Guías CASPe de Lectura Crítica de la Literatura Médica; Cuaderno I; Elsevier: Barcelona, Spain, 2005; pp. 5–8. Available online: https://redcaspe.org/plantilla_ensayo_clinico_v1_0.pdf (accessed on 27 June 2022).
- Dorn, S.O.; Gartner, A.H. Retrograde filling materials: A retrospective success-failure study of amalgam, EBA, and IRM. J. Endod. 1990, 16, 391–393. [Google Scholar] [CrossRef]
- Lui, J.-N.; Khin, M.-M.; Krishnaswamy, G.; Chen, N.-N. Prognostic Factors Relating to the Outcome of Endodontic Microsurgery. J. Endod. 2014, 40, 1071–1076. [Google Scholar] [CrossRef]
- Song, M.; Jung, I.-Y.; Lee, S.-J.; Lee, C.-Y.; Kim, E. Prognostic Factors for Clinical Outcomes in Endodontic Microsurgery: A Retrospective Study. J. Endod. 2011, 37, 927–933. [Google Scholar] [CrossRef]
- Tortorici, S.; Difalco, P.; Caradonna, L.; Tetè, S. Traditional Endodontic Surgery Versus Modern Technique: A 5-year controlled clinical trial. J. Craniofacial Surg. 2014, 25, 804–807. [Google Scholar] [CrossRef]
- Chong, B.S.; Ford, T.R.P.; Hudson, M.B. A prospective clinical study of Mineral Trioxide Aggregate and IRM when used as root-end filling materials in endodontic surgery. Int. Endod. J. 2003, 36, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Wälivaara, D.; Abrahamsson, P.; Sämfors, K.-A.; Isaksson, S. Periapical surgery using ultrasonic preparation and thermoplasticized gutta-percha with AH Plus sealer or IRM as retrograde root-end fillings in 160 consecutive teeth: A prospective randomized clinical study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2009, 108, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Wälivaara, D.; Abrahamsson, P.; Fogelin, M.; Isaksson, S. Super-EBA and IRM as root-end fillings in periapical surgery with ultrasonic preparation: A prospective randomized clinical study of 206 consecutive teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2011, 112, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Song, M.; Shin, S.-J.; Kim, E. A Randomized Controlled Study of Mineral Trioxide Aggregate and Super Ethoxybenzoic Acid as Root-end Filling Materials in Endodontic Microsurgery: Long-term Outcomes. J. Endod. 2016, 42, 997–1002. [Google Scholar] [CrossRef]
- Safi, C.; Kohli, M.R.; Kratchman, S.I.; Setzer, F.; Karabucak, B. Outcome of Endodontic Microsurgery Using Mineral Trioxide Aggregate or Root Repair Material as Root-end Filling Material: A Randomized Controlled Trial with Cone-beam Computed Tomographic Evaluation. J. Endod. 2019, 45, 831–839. [Google Scholar] [CrossRef]
- Zhou, W.; Zheng, Q.; Tan, X.; Song, D.; Zhang, L.; Huang, D. Comparison of Mineral Trioxide Aggregate and iRoot BP Plus Root Repair Material as Root-end Filling Materials in Endodontic Microsurgery: A Prospective Randomized Controlled Study. J. Endod. 2017, 43, 1–6. [Google Scholar] [CrossRef]
- Öğütlü, F.; Karaca, I. Clinical and Radiographic Outcomes of Apical Surgery: A Clinical Study. J. Maxillofac. Oral Surg. 2018, 17, 75–83. [Google Scholar] [CrossRef]
- Kim, D.; Lee, H.; Chung, M.; Kim, S.; Song, M.; Kim, E. Effects of fast- and slow-setting calcium silicate–based root-end filling materials on the outcome of endodontic microsurgery: A retrospective study up to 6 years. Clin. Oral Investig. 2020, 24, 247–255. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; (Version 5.1.0); John Wiley & Sons: Hoboken, NJ, USA, 2011; pp. 1–639. [Google Scholar]
- Niederman, R.; Theodosopoulou, J.N. A systematic review of in vivo retrograde obturation materials. Int. Endod. J. 2003, 36, 577–585. [Google Scholar] [CrossRef]
- Kang, M.; Jung, H.I.; Song, M.; Kim, S.Y.; Kim, H.-C.; Kim, E. Outcome of nonsurgical retreatment and endodontic microsurgery: A meta-analysis. Clin. Oral Investig. 2015, 19, 569–582. [Google Scholar] [CrossRef]
- Song, M.; Chung, W.; Lee, S.-J.; Kim, E. Long-term Outcome of the Cases Classified as Successes Based on Short-term Follow-up in Endodontic Microsurgery. J. Endod. 2012, 38, 1192–1196. [Google Scholar] [CrossRef]
- Tsesis, I.; Rosen, E.; Schwartz-Arad, D.; Fuss, Z. Retrospective Evaluation of Surgical Endodontic Treatment: Traditional versus Modern Technique. J. Endod. 2006, 32, 412–416. [Google Scholar] [CrossRef]
- Setzer, F.C.; Shah, S.B.; Kohli, M.R.; Karabucak, B.; Kim, S. Outcome of Endodontic Surgery: A Meta-analysis of the Literature—Part 1: Comparison of Traditional Root-end Surgery and Endodontic Microsurgery. J. Endod. 2010, 36, 1757–1765. [Google Scholar] [CrossRef]
- Setzer, F.C.; Kohli, M.R.; Shah, S.B.; Karabucak, B.; Kim, S. Outcome of Endodontic Surgery: A Meta-analysis of the Literature—Part 2: Comparison of Endodontic Microsurgical Techniques with and without the Use of Higher Magnification. J. Endod. 2012, 38, 1–10. [Google Scholar] [CrossRef]
- Kvist, T.; Reit, C. Results of endodontic retreatment: A randomized clinical study comparing surgical and nonsurgical procedures. J. Endod. 1999, 25, 814–817. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).