Comparative Analysis of the Shear Bond Strength of Flowable Self-Adhering Resin-Composites Adhesive to Dentin with a Conventional Adhesive
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
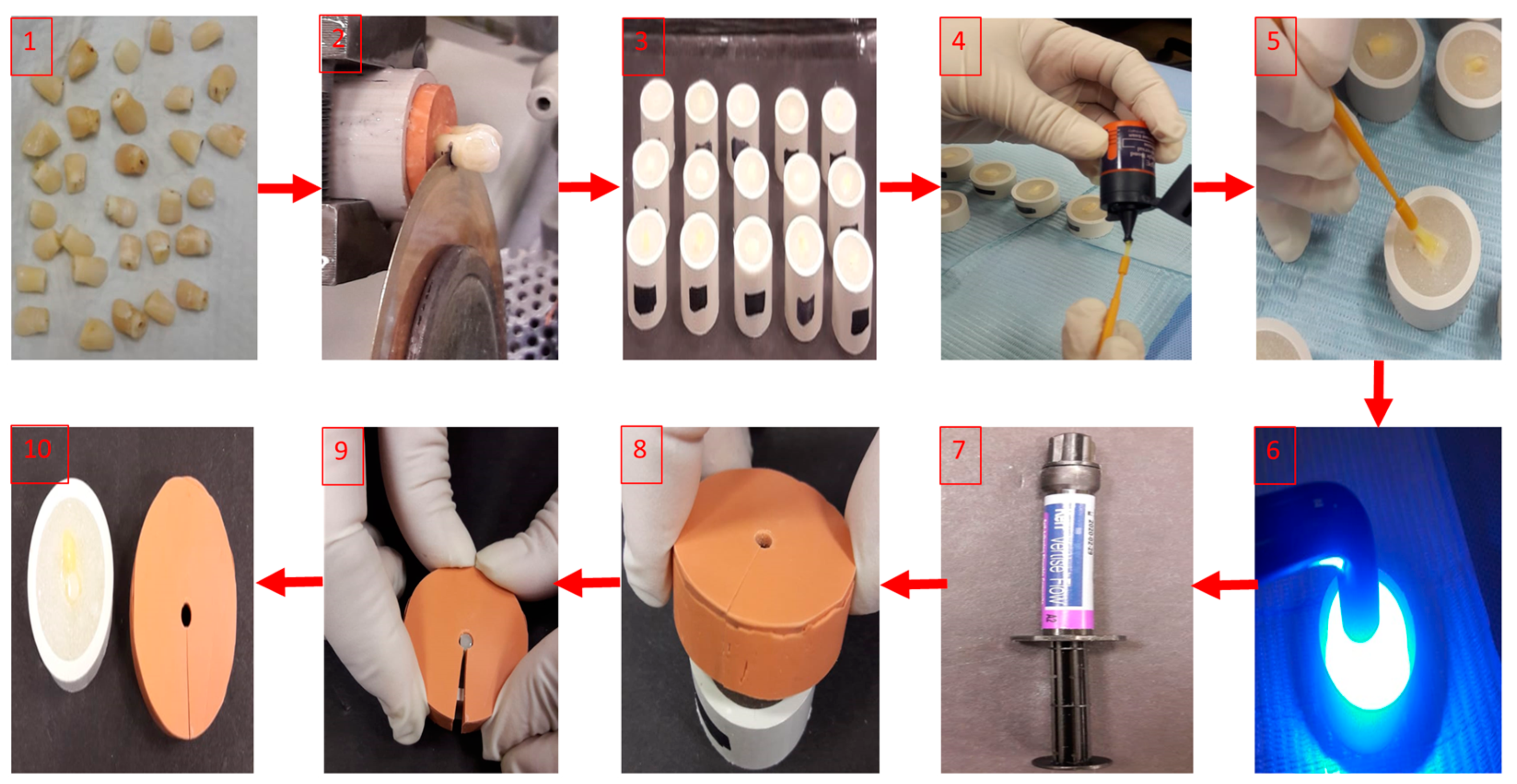
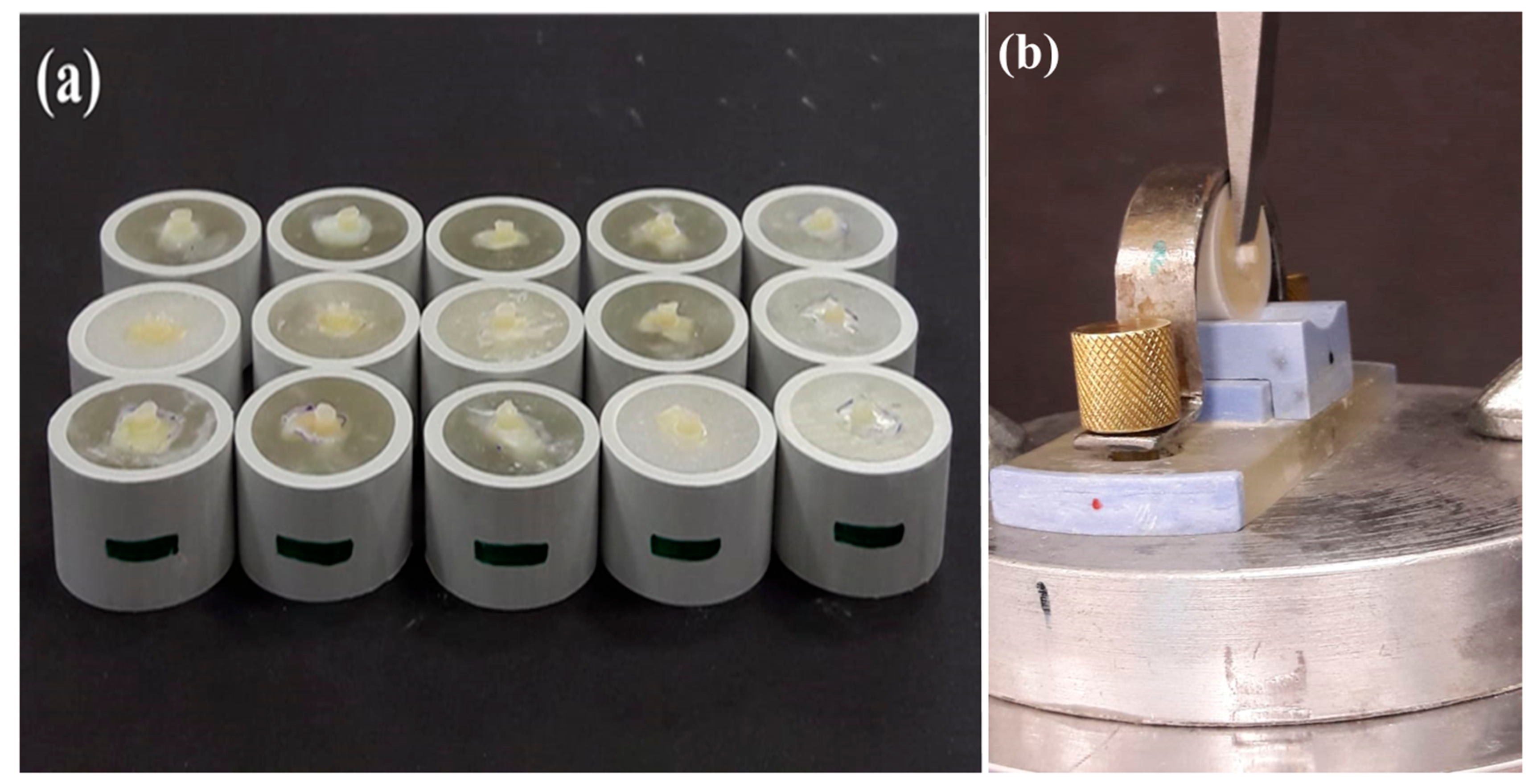
2.2. Methods
2.3. Shear Bond Testing
3. Results
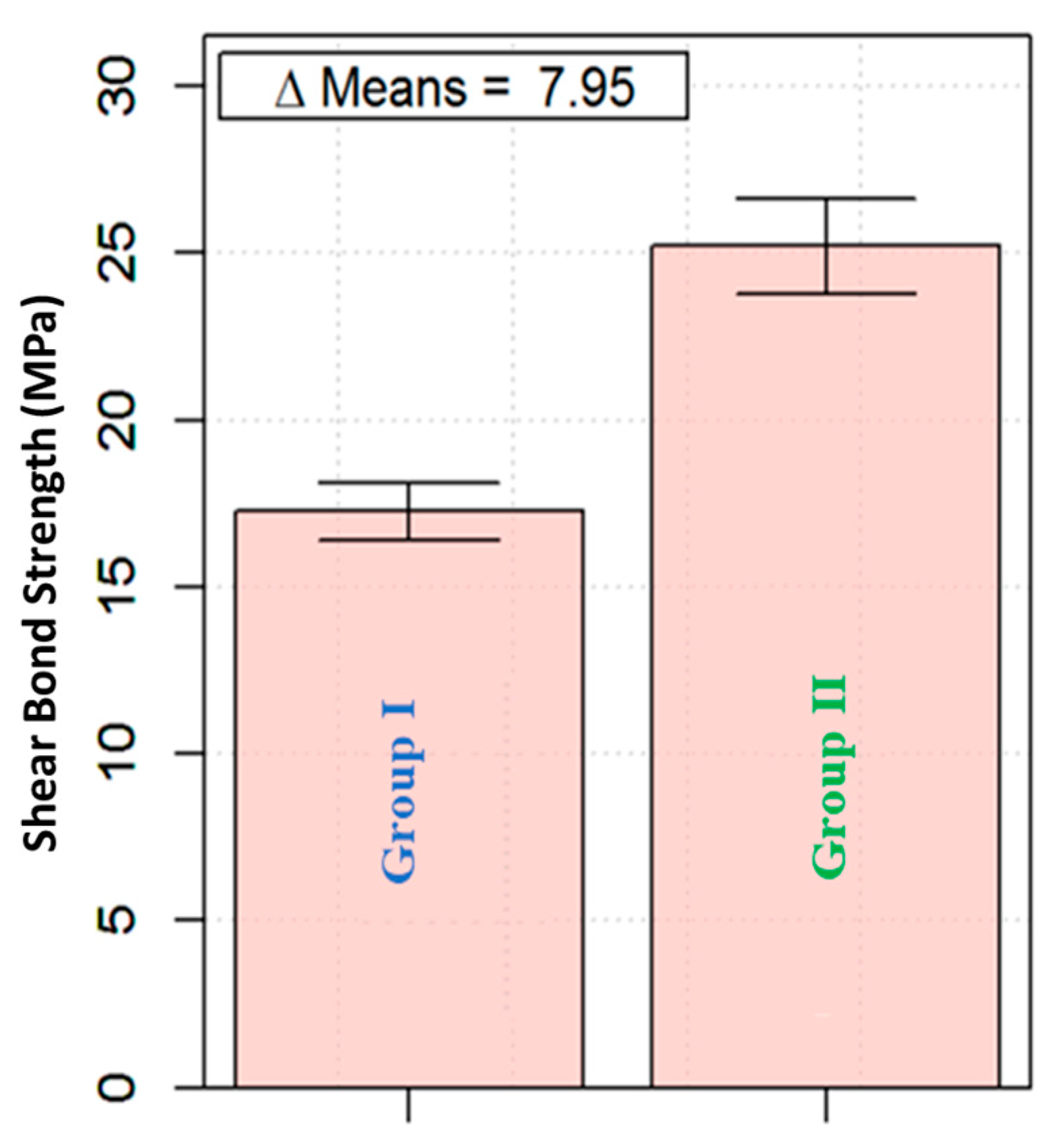
3.1. Shear Bond Strength Group I and Group II
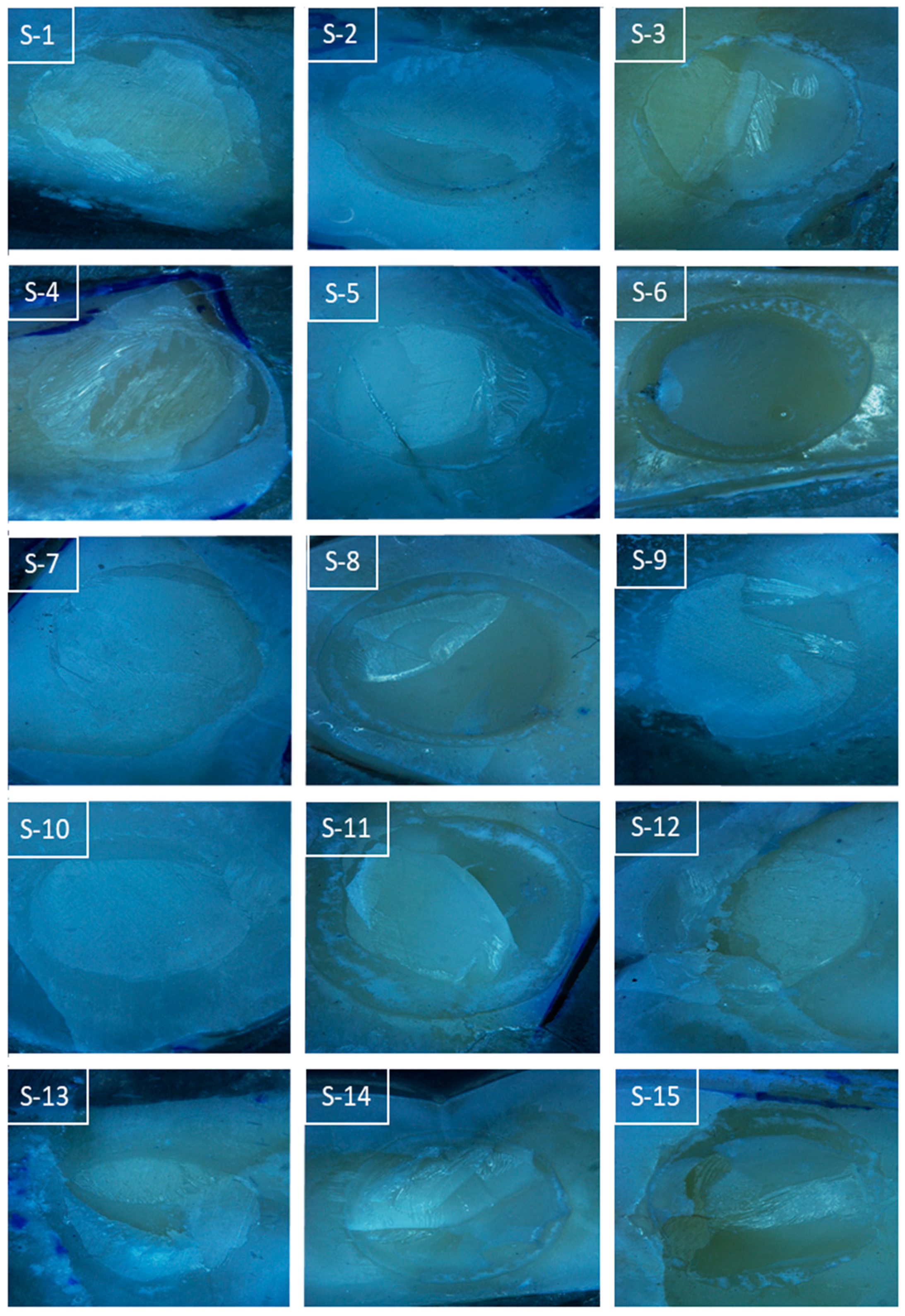
3.2. Modes of Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ben-Amar, A.; Kaffe, I.; Gorfil, C. Marginal leakage in amalgam restorations and its prevention. Refu’at Ha-Peh Veha-Shinayim (Tel Aviv Isr. 1969) 1978, 27, 25–29. [Google Scholar]
- Swift, E.J. Dentin/enamel adhesives: Review of the literature. Pediatr. Dent. 2002, 24, 456–461. [Google Scholar]
- Swift, E.J.; Perdigão, J.; Heymann, H.O. Bonding to enamel and dentin: A brief history and state of the art, 1995. Quintessence Int. Engl. Ed. 1995, 26, 95–110. [Google Scholar]
- Salerno, M.; Loria, P.; Matarazzo, G.; Tomè, F.; Diaspro, A.; Eggenhöffner, R. Surface morphology and tooth adhesion of a novel nanostructured dental restorative composite. Materials 2016, 9, 203. [Google Scholar] [CrossRef]
- Bektas, O.O.; Eren, D.; Akin, E.G.; Akin, H. Evaluation of a self-adhering flowable composite in terms of micro-shear bond strength and microleakage. Acta Odontol. Scand. 2012, 71, 541–546. [Google Scholar] [CrossRef]
- Labella, R.; Lambrechts, P.; Van Meerbeek, B.; Vanherle, G. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent. Mater. 1999, 15, 128–137. [Google Scholar] [CrossRef]
- Sofan, E.; Sofan, A.; Palaia, G.; Tenore, G.; Romeo, U.; Migliau, G. Classification review of dental adhesive systems: From the IV generation to the universal type. Ann. Stomatol. 2017, 8, 1. [Google Scholar]
- Vasconcelos e Cruz, J.; Polido, M.; Brito, J.; Gonçalves, L.L. Dentin bonding and SEM analysis of a new experimental universal adhesive system containing a dendrimer. Polymers 2020, 12, 461. [Google Scholar] [CrossRef]
- Kaptan A, K.V.; Hürmüzlü, F.; Serper, A.; Kaptan, A. Effect of chemical irrigants on the bond strength of a universal adhesive system to dentin-enamel junction and different dentin regions. Clin. Med. Rev. Case Rep. 2019, 6, 285. [Google Scholar]
- Nagarkar, S.; Theis-Mahon, N.; Perdigão, J. Universal dental adhesives: Current status, laboratory testing, and clinical performance. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 2121–2131. [Google Scholar] [CrossRef]
- Unterbrink, G.L.; Liebenberg, W.H. Flowable resin composites as “filled adhesives”: Literature review and clinical recommendations. Quintessence Int. 1999, 30, 249–257. [Google Scholar]
- Korkmaz, Y.; Gurgan, S.; Firat, E.; Nathanson, D. Shear bond strength of three different nano-restorative materials to dentin. Oper. Dent. 2010, 35, 50–57. [Google Scholar] [CrossRef]
- Goracci, C.; Cadenaro, M.; Fontanive, L.; Giangrosso, G.; Juloski, J.; Vichi, A.; Ferrari, M. Polymerization efficiency and flexural strength of low-stress restorative composites. Dent. Mater. 2014, 30, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Sudsangiam, S.; Van Noort, R. Do dentin bond strength tests serve a useful purpose? J. Adhes Dent. 1999, 1, 57–67. [Google Scholar] [PubMed]
- Ferdianakis, K. Microleakage reduction from newer esthetic restorative materials in permanent molars. J. Clin. Pediatr. Dent. 1998, 22, 221–229. [Google Scholar] [PubMed]
- Ikeda, M.; Tsubota, K.; Takamizawa, T.; Yoshida, T.; Miyazaki, M.; Platt, J.A. Bonding durability of single-step adhesives to previously acid-etched dentin. Oper. Dent. 2008, 33, 702–709. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Van Landuyt, K.; De Munck, J.; Hashimoto, M.; Peumans, M.; Lambrechts, P.; Yoshida, Y.; Inoue, S.; Suzuki, K. Technique-sensitivity of contemporary adhesives. Dent. Mater. J. 2005, 24, 1–13. [Google Scholar] [CrossRef]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2012, 17, 1497–1506. [Google Scholar] [CrossRef] [PubMed]
- Naughton, W.T.; Latta, M.A. Bond strength of composite to dentin using self-etching adhesive systems. Quintessence Int. 2005, 36, 259–262. [Google Scholar]
- Singh, K.; Naik, R.; Hegde, S.; Damda, A. Shear bond strength of superficial, intermediate and deep dentin in vitro with recent generation self-etching primers and single nano composite resin. J. Int. Oral Health 2015, 7, 28–32. [Google Scholar]
- Poitevin, A.; De Munck, J.; Van Ende, A.; Suyama, Y.; Mine, A.; Peumans, M.; Van Meerbeek, B. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent. Mater. 2013, 29, 221–230. [Google Scholar] [CrossRef]
- Wajdowicz, M.N.; Vandewalle, K.S.; Means, M.T. Shear bond strength of new self-adhesive flowable composite resins. Gen. Dent. 2012, 60, 104–108. [Google Scholar]
- Giannini, M.; Makishi, P.; Ayres, A.P.A.; Vermelho, P.M.; Fronza, B.M.; Nikaido, T.; Tagami, J. Self-etch adhesive systems: A literature review. Braz. Dent. J. 2015, 26, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Altunsoy, M.; Tanrıver, M.; Ok, E.; Kucukyilmaz, E. Shear bond strength of a self-adhering flowable composite and a flowable base composite to mineral trioxide aggregate, calcium-enriched mixture cement, and biodentine. J. Endod. 2015, 41, 1691–1695. [Google Scholar] [CrossRef] [PubMed]
- Yousef, M.K.; El Naga, A.A.; Ramadan, R.; Fayez, C.; Alshawwa, L.; Bahgat, S.F. Does the use of a novel self-adhesive flowable composite reduce nanoleakage? Clin. Cosmet. Investig. Dent. 2015, 7, 55–64. [Google Scholar] [CrossRef][Green Version]
- Makishi, P.; Pacheco, R.R.; Sadr, A.; Shimada, Y.; Sumi, Y.; Tagami, J.; Giannini, M. Assessment of self-adhesive resin composites: Nondestructive imaging of resin–dentin interfacial adaptation and shear bond strength. Microsc. Microanal. 2015, 21, 1523–1529. [Google Scholar] [CrossRef]
- Salerno, M.; Derchi, G.; Thorat, S.; Ceseracciu, L.; Ruffilli, R.; Barone, A.C. Surface morphology and mechanical properties of new-generation flowable resin composites for dental restoration. Dent. Mater. 2011, 27, 1221–1228. [Google Scholar] [CrossRef]
- Arlin, K.; Filiz, Y.; Saadet, G. Bonding to enamel and dentin using self-etching adhesive systems. Quintessence Int. 2004, 35, 367–370. [Google Scholar]
- Bhandary, S.; Hegde, M.N. An evaluation and comparison of shear bond strength of composite resin to dentin, using newer dentin bonding agents. J. Conserv. Dent. 2008, 11, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Thorat, S.B.; Diaspro, A.; Salerno, M. In vitro investigation of coupling-agent-free dental restorative composite based on nano-porous alumina fillers. J. Dent. 2014, 42, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Margvelashvili, M.; Giovannetti, A.; Vichi, A.; Ferrari, M. Shear bond strength of orthodontic brackets bonded with a new self-adhering flowable resin composite. Clin. Oral Investig. 2012, 17, 609–617. [Google Scholar] [CrossRef]
- Viotti, R.G.; Kasaz, A.; Peña, C.E.; Alexandre, R.S.; Arrais, C.A.; Reis, A.F. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J. Prosthet. Dent. 2009, 102, 306–312. [Google Scholar] [CrossRef]
- Goracci, C.; Sadek, F.; Fabianelli, A.; Tay, F.; Ferrari, M. Evaluation of the adhesion of fiber posts to intraradicular dentin. Oper. Dent.-Univ. Wash. 2005, 30, 627. [Google Scholar]
- Monticelli, F.; Osorio, R.; Mazzitelli, C.; Ferrari, M.; Toledano, M. Limited decalcification/diffusion of self-adhesive cements into dentin. J. Dent. Res. 2008, 87, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Gerth, H.U.; Dammaschke, T.; Züchner, H.; Schäfer, E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites—a comparative study. Dent. Mater. 2006, 22, 934–941. [Google Scholar] [CrossRef]
- Tuloglu, N.; Tunç, E.S.; Ozer, S.; Bayrak, S. Shear bond strength of self-adhering flowable composite on dentin with and without application of an adhesive system. J. Appl. Biomater. Funct. Mater. 2013, 12, 97–101. [Google Scholar] [CrossRef]
- Asmussen, E.; Uno, S. Solubility parameters, fractional polarities, and bond strengths of some intermediary resins used in dentin bonding. J. Dent. Res. 1993, 72, 558–565. [Google Scholar] [CrossRef]
- Miller, R.G.; Bowles, C.Q.; Chappelow, C.C.; Eick, J.D. Application of solubility parameter theory to dentin-bonding systems and adhesive strength correlations. J. Biomed. Mater. Res. 1998, 41, 237–243. [Google Scholar] [CrossRef]
- Pacifici, E.; Chazine, M.; Vichi, A.; Grandini, S.; Goracci, C.; Ferrari, M. Shear-bond strength of a new self-adhering flowable restorative material to dentin of primary molars. J. Clin. Pediatr. Dent. 2013, 38, 149–154. [Google Scholar] [CrossRef]
- Juloski, J.; Goracci, C.; Rengo, C.; Giovannetti, A.; Vichi, A.; Vulicevic, Z.R.; Ferrari, M. Enamel and dentin bond strength of new simplified adhesive materials with and without preliminary phosphoric acid-etching. Am. J. Dent. 2012, 25, 239–243. [Google Scholar]
- Titley, K.C.; Chernecky, R.; Rossouw, P.E.; Kulkarni, G.V. The effect of various storage methods and media on shear-bond strengths of dental composite resin to bovine dentine. Arch. Oral Biol. 1998, 43, 305–311. [Google Scholar] [CrossRef]
- Al-Salehi, S.K.; Burke, F.J. Methods used in dentin bonding tests: An analysis of 50 investigations on bond strength. Quintessence Int. 1997, 28, 717–723. [Google Scholar] [PubMed]
- Sakaguchi, R.L.; Powers, J.M. Chapter 5—Testing of Dental Materials and Biomechanics. In Craig’s Restorative Dental Materials, 13th ed.; Mosby: Saint Louis, MI, USA, 2012; pp. 83–107. [Google Scholar]

| Group Name | Product Name | Manufacturer | Composition | Instructions for Use |
|---|---|---|---|---|
| Group I | Vertise Flow | Kerr, Orange, CA, USA | GPDM adhesive and methacrylate co-monomers, monomer, prepolymerized filler containing barium glass filler, nano-sized colloidal silica, nano-sized Ybf3 (70 wt.%) | Brush a thin layer (<0.5 mm) of Vertise Flow for 15–20 s, light cure for 20 s. Build additional layers (2 mm or less) then light cure for 20 s |
| Group II | Filtek Ultimate Flow | 3M ESPE, St. Paul, MN, USA | Bis-GMA, TEGDMA, and procrylat resins, Ybf3 filler, zirconia/silica cluster filler, silica filler | Place the composite into the cavity (2 mm) Light cure for 20 s |
| Single Bond Universal | 3M ESPE, St. Paul, MN, USA | MDP phosphate monomer, dimethacrylate resins vitrebond copolymer, HEMA, filler, ethanol, water, initiators, silane | Apply a single coat of the adhesive to the required area on tooth by rubbing for 20 s; direct a gentle stream of air over the material for 5 s then LED light cure |
| Sample No. | Maximum Load (N) | Shear Bond Stress at Maximum Load (MPa) |
|---|---|---|
| 1 | 139.9 | 19.8 |
| 2 | 123.9 | 17.5 |
| 3 | 137.2 | 19.4 |
| 4 | 117.1 | 16.6 |
| 5 | 136.9 | 19.4 |
| 6 | 120.5 | 17.0 |
| 7 | 114.1 | 16.1 |
| 8 | 125.3 | 17.7 |
| 9 | 133.9 | 18.9 |
| 10 | 120.8 | 17.1 |
| 11 | 111.9 | 15.8 |
| 12 | 112.6 | 15.9 |
| 13 | 111.5 | 15.8 |
| 14 | 105.4 | 14.9 |
| 15 | 119.1 | 16.8 |
| Mean | 122.0 | 17.3 |
| Standard Deviation (SD) | 10.7 | 1.5 |
| Sample No. | Maximum Load (N) | Shear Bond Stress at Maximum Load (MPa) |
|---|---|---|
| 1 | 168.7 | 23.9 |
| 2 | 167.1 | 23.6 |
| 3 | 191.5 | 27.1 |
| 4 | 194.6 | 27.5 |
| 5 | 149.5 | 21.2 |
| 6 | 197.2 | 27.9 |
| 7 | 205.1 | 29.0 |
| 8 | 143.5 | 20.3 |
| 9 | 191.1 | 27.0 |
| 10 | 177.1 | 25.0 |
| 11 | 177.8 | 25.1 |
| 12 | 170.2 | 24.1 |
| 13 | 192.7 | 27.3 |
| 14 | 188.4 | 26.7 |
| 15 | 158.9 | 22.5 |
| Mean | 178.2 | 25.2 |
| Standard Deviation | 18.3 | 2.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asiri, A.A.; Khan, R.; Alzahrani, S.S.; Haider, S.; Khan, S.U.-D.; Asiri, E.A.M.; Alamri, M.F.; Ahmad, A.; Mubushar, M. Comparative Analysis of the Shear Bond Strength of Flowable Self-Adhering Resin-Composites Adhesive to Dentin with a Conventional Adhesive. Coatings 2021, 11, 273. https://doi.org/10.3390/coatings11030273
Asiri AA, Khan R, Alzahrani SS, Haider S, Khan SU-D, Asiri EAM, Alamri MF, Ahmad A, Mubushar M. Comparative Analysis of the Shear Bond Strength of Flowable Self-Adhering Resin-Composites Adhesive to Dentin with a Conventional Adhesive. Coatings. 2021; 11(3):273. https://doi.org/10.3390/coatings11030273
Chicago/Turabian StyleAsiri, Abdulmajeed Ali, Rawaiz Khan, Sultan Saeed Alzahrani, Sajjad Haider, Salah Ud-Din Khan, Essa Ali Mousa Asiri, Maha Fayez Alamri, Ashfaq Ahmad, and Muhammad Mubushar. 2021. "Comparative Analysis of the Shear Bond Strength of Flowable Self-Adhering Resin-Composites Adhesive to Dentin with a Conventional Adhesive" Coatings 11, no. 3: 273. https://doi.org/10.3390/coatings11030273
APA StyleAsiri, A. A., Khan, R., Alzahrani, S. S., Haider, S., Khan, S. U.-D., Asiri, E. A. M., Alamri, M. F., Ahmad, A., & Mubushar, M. (2021). Comparative Analysis of the Shear Bond Strength of Flowable Self-Adhering Resin-Composites Adhesive to Dentin with a Conventional Adhesive. Coatings, 11(3), 273. https://doi.org/10.3390/coatings11030273








