Redundant Anaerobic Antimicrobial Prescriptions in German Acute Care Hospitals: Data from a National Point Prevalence Survey
Abstract
1. Introduction
2. Materials and Methods
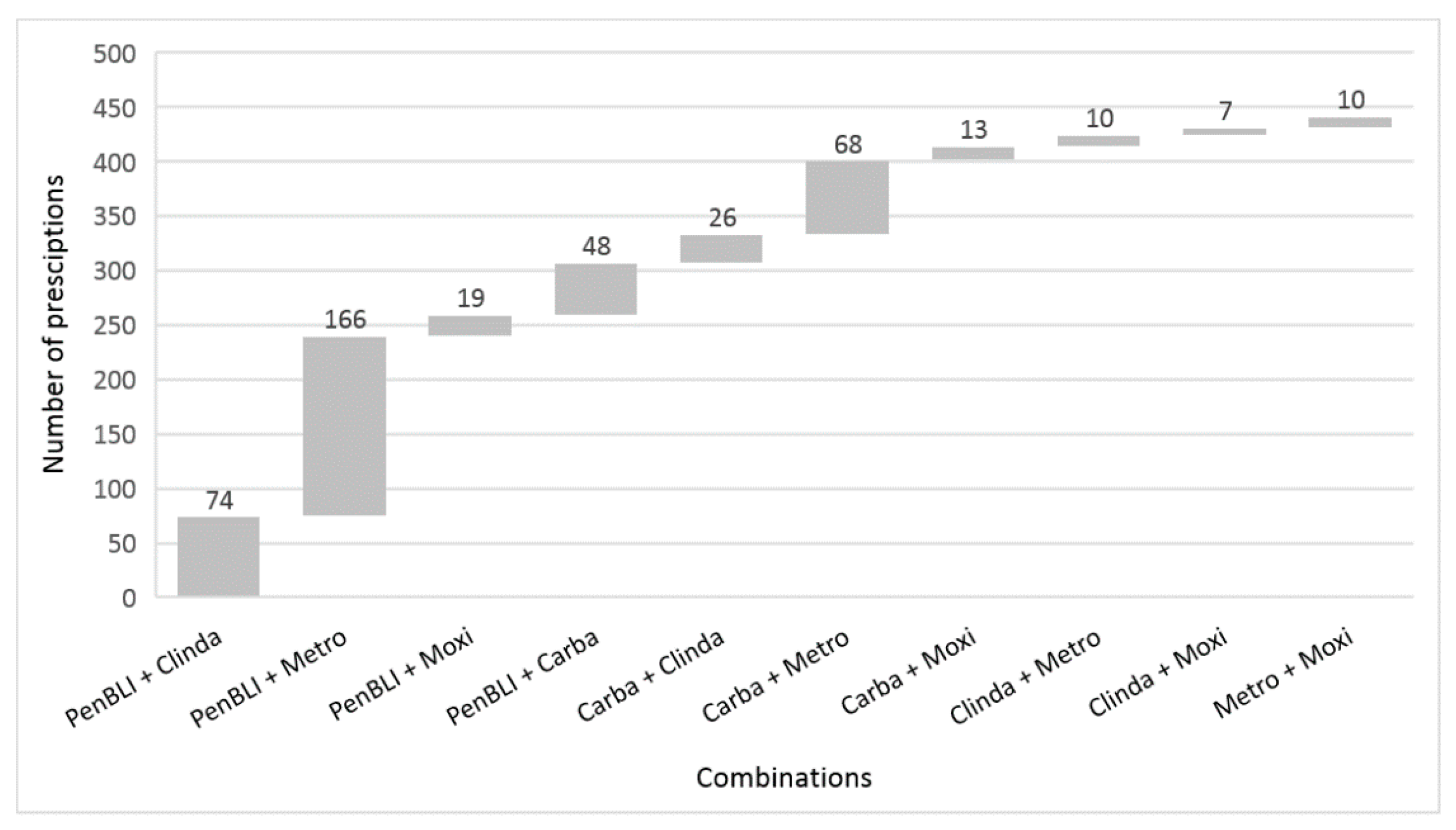
- PenBLI plus clindamycin;
- PenBLI plus metronidazole;
- PenBLI plus moxifloxacin;
- PenBLI plus carbapenem;
- Carbapenem plus clindamycin;
- Carbapenem plus metronidazole;
- Carbapenem plus moxifloxacin;
- Clindamycin plus metronidazole;
- Clindamycin plus moxifloxacin; and
- Metronidazole plus moxifloxacin.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Buffie, C.G.; Jarchum, I.; Equinda, M.; Lipuma, L.; Gobourne, A.; Viale, A.; Ubeda, C.; Xavier, J.; Pamer, E.G. Profound alterations of intestinal microbiota following a single dose of clindamycin results in sustained susceptibility to Clostridium difficile-induced colitis. Infect. Immun. 2012, 80, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Curtis, N. The effect of antibiotics on the composition of the intestinal microbiota—A systematic review. J. Infect. 2019, 76, 471–489. [Google Scholar] [CrossRef] [PubMed]
- Veloo, A.C.; van Winkelhoff, A.J. Antibiotic susceptibility profiles of anaerobic pathogens in The Netherlands. Anaerobe 2015, 31, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Cobo, F.; Rodríguez-Granger, J.; Pérez-Zapata, I.; Sampedro, A.; Aliaga, L.; Navarro-Marí, J.M. Antimicrobial susceptibility and clinical findings of significant anaerobic bacteria in southern Spain. Anaerobe 2019, 59, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Kioka, M.J.; DiGiovine, B.; Rezik, M.; Jennings, J.H. Anaerobic antibiotic usage for pneumonia in the medical intensive care unit. Respirology 2017, 22, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, M.; Roux, X.; Huttner, B.; Pugin, J. Streptococcal toxic shock syndrome in the intensive care unit. Ann. Intensive Care 2018, 8, 88. [Google Scholar] [CrossRef] [PubMed]
- Huttner, B.; Jones, M.; Rubin, M.A.; Madaras-Kelly, K.; Nielson, C.; Goetz, M.B.; Neuhauser, M.M.; Samore, M.H. Double trouble: How big a problem is redundant anaerobic antibiotic coverage in Veterans Affairs medical centres? J. Antimicrob. Chemother. 2012, 67, 1537–1539. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De With, K.; Allerberger, F.; Amann, S.; Apfalter, P.; Brodt, H.R.; Eckmanns, T.; Fellhauer, M.; Geiss, H.K.; Janata, O.; Krause, R.; et al. Strategies to enhance rational use of antibiotics in hospital: A guideline by the German Society for Infectious Diseases. Infection 2016, 44, 395–439. [Google Scholar] [CrossRef] [PubMed]
- Schultz, L.; Lowe, T.J.; Srinivasan, A.; Neilson, D.; Pugliese, G. Economic impact of redundant antimicrobial therapy in US hospitals. Infect. Control Hosp. Epidemiol. 2014, 35, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Rattanaumpawan, P.; Morales, K.H.; Binkley, S.; Synnestvedt, M.; Weiner, M.G.; Gasink, L.B.; Fishman, N.O.; Lautenbach, E. Impact of antimicrobial stewardship programme changes on unnecessary double anaerobic coverage therapy. J. Antimicrob. Chemother. 2011, 66, 2655–2658. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, H.S.; Song, Y.J.; Lee, E.; Song, K.H.; Choe, P.G.; Park, W.B.; Bang, J.H.; Kim, E.S.; Park, S.W.; et al. Redundant combinations of antianaerobic antimicrobials: Impact of pharmacist-based prospective audit and feedback and prescription characteristics. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Aghdassi, S.J.S.; Schwab, F.; Hansen, S.; Hansen, S.; Peña Diaz, L.A.; Behnke, M.; Gastmeier, P.; Kramer, T.S. The quality of antimicrobial prescribing in acute care hospitals: Results derived from a national point prevalence survey, Germany, 2016. Eurosurveillance 2019, 24, 1900281. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial use in European Acute Care Hospitals. Protocol Version 5.3. Stockholm: ECDC; 2016. Available online: https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/PPS-HAI-antimicrobial-use-EU-acute-care-hospitals-V5-3.pdf (accessed on 17 May 2020).
- Federal Office of Statistics. Anzahl der Krankenhäuser in Deutschland in den Jahren 2000 Bis 2018 [Number of Hospitals in Germany in the Years 2000 until 2018], 2020. Available online: https://de.statista.com/statistik/daten/studie/2617/umfrage/anzahl-der-krankenhaeuser-in-deutschland-seit-2000/ (accessed on 17 May 2020).
- WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC Classification and DDD Assignment 2013. Oslo, 2012. Available online: https://www.whocc.no/filearchive/publications/1_2013guidelines.pdf (accessed on 17 May 2020).
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 10.0, 2020. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_10.0_Breakpoint_Tables.pdf (accessed on 17 May 2020).
- Brook, I.; Wexler, H.M.; Goldstein, E.J. Antianaerobic antimicrobials: Spectrum and susceptibility testing. Clin. Microbiol. Rev. 2013, 26, 526–546. [Google Scholar] [CrossRef] [PubMed]
- Brook, I. Antimicrobials therapy of anaerobic infections. J. Chemother. 2016, 28, 143–150. [Google Scholar] [CrossRef] [PubMed]
- German Protection against Infection Act. Gesetze-im-Internet Website. Available online: http://www.gesetze-im-internet.de/ifsg/BJNR104510000.html (accessed on 17 May 2020).
- McDonald, L.C.; Gerding, D.N.; Johnson, S.; Bakken, J.S.; Carroll, K.C.; Coffin, S.E.; Dubberke, E.R.; Garey, K.W.; Gould, C.V.; Kelly, C.; et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 2018, 66, e1–e48. [Google Scholar] [CrossRef] [PubMed]
- Ooijevaar, R.E.; van Beurden, Y.H.; Terveer, E.M.; Goorhuis, A.; Bauer, M.P.; Keller, J.J.; Mulder, C.J.J.; Kuijper, E.J. Update of treatment algorithms for Clostridium difficile infection. Clin. Microbiol. Infect. 2018, 24, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Andreoni, F.; Zürcher, C.; Tarnutzer, A.; Schilcher, K.; Neff, A.; Keller, N.; Maggio, E.M.; Poyart, C.; Schuepbach, R.A. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J. Infect. Dis. 2016, 215, 269–277. [Google Scholar] [CrossRef][Green Version]
- Stevens, D.L.; Bisno, A.L.; Chambers, H.F.; Dellinger, E.P.; Goldstein, E.J.C.; Gorbach, S.L.; Hirschmann, J.; Kaplan, S.L.; Montoya, J.G.; Wade, J.C.; et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2014, 59, e10–e52. [Google Scholar] [CrossRef] [PubMed]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef] [PubMed]
- Glowacki, R.C.; Schwartz, D.N.; Itokazu, G.S.; Wisniewski, M.F.; Kieszkowski, P.; Weinstein, R.A. Antibiotic Combinations with Redundant Antimicrobial Spectra: Clinical Epidemiology and Pilot Intervention of Computer-Assisted Surveillance. Clin. Infect. Dis. 2003, 37, 59–64. [Google Scholar] [CrossRef] [PubMed]

| Variable | Group/Parameter | Number (Percentage) or Median (Interquartile Range) |
|---|---|---|
| Hospital type | Primary care | 118 (54.1) |
| Secondary care | 41 (18.8) | |
| Tertiary care | 36 (16.5) | |
| Specialized hospital | 23 (10.6) | |
| Hospital ownership | Public | 103 (47.2) |
| Private, not for profit | 63 (28.9) | |
| Private, for profit | 31 (14.2) | |
| Other/Unknown | 21 (9.6) | |
| Hospital size | Number of beds | 305 (185–541) |
| Antimicrobial/Antimicrobial Group | All Prescriptions | Redundant Prescriptions (Percentage) |
|---|---|---|
| Penicillin/beta-lactamase inhibitor | 5119 | 307 (6.0) |
| Carbapenems | 1369 | 155 (11.3) |
| Clindamycin | 695 | 117 (16.8) |
| Metronidazole | 1621 | 254 (15.7) |
| Moxifloxacin | 227 | 49 (21.6) |
| Type of Infection | Number (Percentage) | ||
|---|---|---|---|
| All Infections | Community-Acquired Infections | Hospital-Acquired Infections | |
| All | 378 (100) | 258 (100) | 120 (100) |
| Bacteremia | 21 (5.6) | 17 (6.6) | 4 (3.3) |
| Non-microbiologically confirmed systemic infection | 40 (10.6) | 21 (8.1) | 19 (15.8) |
| Bone/Joint infection | 19 (5.0) | 13 (5.0) | 6 (5) |
| Skin/Soft tissue infection | 76 (20.1) | 57 (22.1) | 19 (15.8) |
| Intra-abdominal infection | 32 (8.5) | 22 (8.5) | 10 (8.3) |
| Gastrointestinal infection | 50 (13.2) | 35 (13.6) | 15 (12.5) |
| Lower respiratory tract infection | 77 (20.4) | 43 (16.7) | 34 (28.3) |
| Urinary tract infection | 25 (6.6) | 14 (5.4) | 11 (9.2) |
| Other/Not specified | 38 (10.1) | 36 (14.0) | 2 (1.7) |
| Combination | Number (Percentage) | |||||
|---|---|---|---|---|---|---|
| All | Treatment of CAI | Treatment of HAI | Surgical Prophylaxis | Medical Prophylaxis | Other/Unknown | |
| All | 441 (100) | 258 (100) | 120 (100) | 23 (100) | 25 (100) | 15 (100) |
| PenBLI + Clinda | 74 (16.8) | 54 (20.9) | 11 (9.2) | 5 (21.7) | 2 (8) | 2 (13.3) |
| PenBLI + Metro | 166 (37.6) | 98 (38.0) | 40 (33.3) | 14 (60.9) | 8 (32) | 6 (40) |
| PenBLI + Moxi | 19 (4.3) | 9 (3.5) | 5 (4.2) | 0 (0) | 4 (16) | 1 (6.7) |
| PenBLI + Carba | 48 (10.9) | 28 (10.9) | 18 (15) | 0 (0) | 1 (4) | 1 (6.7) |
| Carba + Clinda | 26 (5.9) | 19 (7.4) | 4 (3.3) | 2 (8.7) | 1 (4) | 0 (0) |
| Carba + Metro | 68 (15.4) | 26 (10.1) | 30 (25) | 2 (8.7) | 7 (28) | 3 (20) |
| Carba + Moxi | 13 (2.9) | 7 (2.7) | 5 (4.2) | 0 (0) | 1 (4) | 0 (0) |
| Clinda + Metro | 10 (2.7) | 7 (2.7) | 2 (1.7) | 0 (0) | 0 (0) | 1 (6.7) |
| Clinda + Moxi | 7 (1.6) | 3 (1.2) | 3 (2.5) | 0 (0) | 0 (0) | 1 (6.7) |
| Metro + Moxi | 10 (2.7) | 7 (2.7) | 2 (1.7) | 0 (0) | 1 (4) | 0 (0) |
| Combination | Number (Percentage) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | BAC | SYS | BJI | SSTI | IA | GI | LRTI | UTI | O/NS | |
| All | 378 (100) | 21 (100) | 40 (100) | 19 (100) | 76 (100) | 32 (100) | 50 (100) | 77 (100) | 25 (100) | 38 (100) |
| PenBLI + Clinda | 65 (17.2) | 2 (9.5) | 3 (7.5) | 12 (63.2) | 31 (40.8) | 0 (0) | 1 (2) | 5 (6.5) | 3 (12) | 8 (21.1) |
| PenBLI + Metro | 138 (36.5) | 7 (33.3) | 12 (30) | 1 (5.3) | 19 (25) | 18 (56.3) | 34 (68) | 25 (32.5) | 11 (44) | 11 (28.9) |
| PenBLI + Moxi | 14 (3.7) | 3 (14.3) | 1 (2.5) | 0 (0) | 2 (2.6) | 0 (0) | 1 (2) | 6 (7.8) | 0 (0) | 1 (2.6) |
| PenBLI + Carba | 46 (12.2) | 1 (4.8) | 5 (12.5) | 1 (5.3) | 5 (6.6) | 6 (18.8) | 2 (4) | 19 (24.7) | 5 (20) | 2 (5.3) |
| Carba + Clinda | 23 (6.1) | 1 (4.8) | 4 (10) | 2 (10.5) | 8 (10.5) | 0 (0) | 0 (0) | 5 (6.5) | 0 (0) | 3 (7.9) |
| Carba + Metro | 56 (14.8) | 5 (23.8) | 13 (32.5) | 0 (0) | 2 (2.6) | 7 (21.9) | 8 (16) | 9 (11.7) | 4 (16) | 8 (21.1) |
| Carba + Moxi | 12 (3.2) | 0 (0) | 1 (2.5) | 0 (0) | 0 (0) | 1 (3.2) | 2 (4) | 4 (5.2) | 2 (8) | 2 (5.3) |
| Clinda + Metro | 9 (2.4) | 0 (0) | 1 (2.5) | 2 (10.5) | 3 (3.9) | 0 (0) | 1 (2) | 0 (0) | 0 (0) | 2 (5.3) |
| Clinda + Moxi | 6 (1.6) | 0 (0) | 0 (0) | 1 (5.3) | 3 (3.9) | 0 (0) | 0 (0) | 2 (2.6) | 0 (0) | 0 (0) |
| Metro + Moxi | 9 (2.4) | 2 (9.5) | 0 (0) | 0 (0) | 3 (3.9) | 0 (0) | 1 (2) | 2 (2.6) | 0 (0) | 1 (2.6) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aghdassi, S.J.S.; Gastmeier, P.; Behnke, M.; Hansen, S.; Kramer, T.S. Redundant Anaerobic Antimicrobial Prescriptions in German Acute Care Hospitals: Data from a National Point Prevalence Survey. Antibiotics 2020, 9, 288. https://doi.org/10.3390/antibiotics9060288
Aghdassi SJS, Gastmeier P, Behnke M, Hansen S, Kramer TS. Redundant Anaerobic Antimicrobial Prescriptions in German Acute Care Hospitals: Data from a National Point Prevalence Survey. Antibiotics. 2020; 9(6):288. https://doi.org/10.3390/antibiotics9060288
Chicago/Turabian StyleAghdassi, Seven Johannes Sam, Petra Gastmeier, Michael Behnke, Sonja Hansen, and Tobias Siegfried Kramer. 2020. "Redundant Anaerobic Antimicrobial Prescriptions in German Acute Care Hospitals: Data from a National Point Prevalence Survey" Antibiotics 9, no. 6: 288. https://doi.org/10.3390/antibiotics9060288
APA StyleAghdassi, S. J. S., Gastmeier, P., Behnke, M., Hansen, S., & Kramer, T. S. (2020). Redundant Anaerobic Antimicrobial Prescriptions in German Acute Care Hospitals: Data from a National Point Prevalence Survey. Antibiotics, 9(6), 288. https://doi.org/10.3390/antibiotics9060288





