Is Early Monitoring Better? Impact of Early Vancomycin Exposure on Treatment Outcomes and Nephrotoxicity in Patients with Methicillin-Resistant Staphylococcus aureus Infections
Abstract
1. Introduction
2. Results
2.1. Efficacy
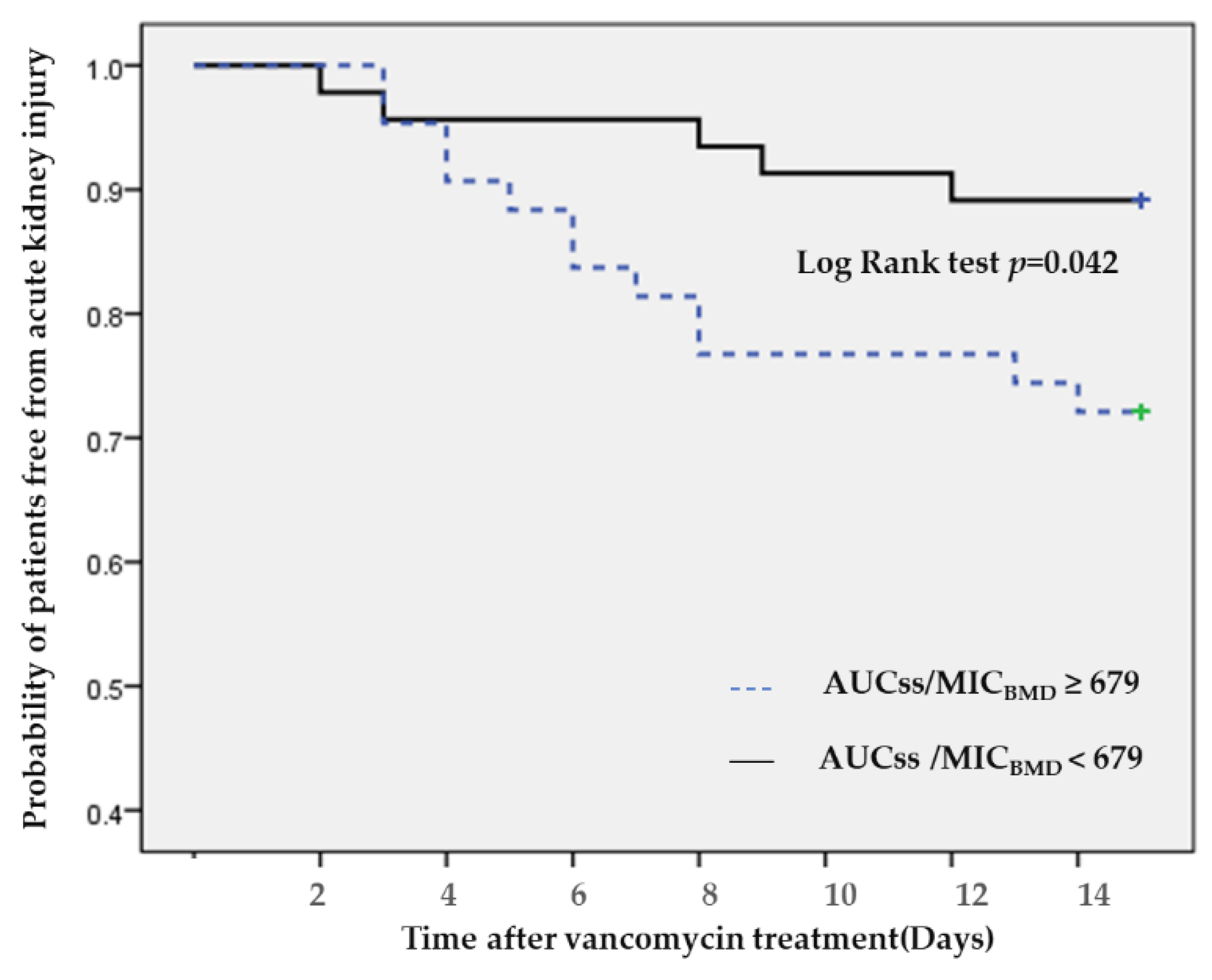
2.2. Nephrotoxicity
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Microbiological Data
4.3. Vancomycin Assay
4.4. Treatment Data and Outcomes
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Song, J.-H.; Hsueh, P.-R.; Chung, D.R.; Ko, K.S.; Kang, C.-I.; Peck, K.R.; Yeom, J.-S.; Kim, S.W.; Chang, H.-H.; Kim, Y.-S.; et al. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: An ANSORP study. J. Antimicrob. Chemother. 2011, 66, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Aziz, M.H.; Driver, E.; Lipman, J.; Roberts, J.A. New paradigm for rapid achievement of appropriate therapy in special populations: Coupling antibiotic dose optimization rapid microbiological methods. Expert Opin. Drug Metab. Toxicol. 2018, 14, 693–708. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.D.M.F.D.G.; Revilla, N.; Calvo, M.V.; Dominguez-Gil, A.; Navarro, A.S. Pharmacokinetic/pharmacodynamic analysis of vancomycin in ICU patients. Intensiv. Care Med. 2007, 33, 279–285. [Google Scholar]
- Baptista, J.P.; Sousa, E.; Martins, P.J.; Pimentel, J.M. Augmented renal clearance in septic patients and implications for vancomycin optimisation. Int. J. Antimicrob. Agents 2012, 39, 420–423. [Google Scholar] [CrossRef]
- Bakke, V.; Sporsem, H.; Von Der Lippe, E.; Nordøy, I.; Lao, Y.; Nyrerød, H.C.; Sandvik, L.; Hårvig, K.R.; Bugge, J.F.; Helset, E. Vancomycin levels are frequently subtherapeutic in critically ill patients: A prospective observational study. Acta Anaesthesiol. Scand. 2017, 61, 627–635. [Google Scholar] [CrossRef]
- Rybak, M.J.; Le, J.; Lodise, T.P.; Levine, D.P.; Bradley, J.S.; Liu, C.; Mueller, B.A.; Pai, M.P.; Wong-Beringer, A.; Rotschafer, J.C.; et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: A revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am. J. Health Syst. Pharm. 2020, 77, 835–864. [Google Scholar]
- Lodise, T.P.; McKinnon, P.S.; Swiderski, L.; Rybak, M.J. Outcomes Analysis of Delayed Antibiotic Treatment for Hospital-Acquired Staphylococcus aureus Bacteremia. Clin. Infect. Dis. 2003, 36, 1418–1423. [Google Scholar] [CrossRef]
- Holmes, N.E.; Turnidge, J.D.; Munckhof, W.J.; Robinson, J.O.; Korman, T.M.; O’Sullivan, M.V.; Anderson, T.L.; Roberts, S.A.; Warren, S.J.C.; Gao, W.; et al. Vancomycin AUC/MIC Ratio and 30-Day Mortality in Patients with Staphylococcus aureus Bacteremia. Antimicrob. Agents Chemother. 2013, 57, 1654–1663. [Google Scholar] [CrossRef]
- Lodise, T.P.; Drusano, G.L.; Zasowski, E.; Dihmess, A.; Lazariu, V.; Cosler, L.; McNutt, L.-A. Vancomycin Exposure in Patients With Methicillin-Resistant Staphylococcus aureus Bloodstream Infections: How Much Is Enough? Clin. Infect. Dis. 2014, 59, 666–675. [Google Scholar] [CrossRef]
- Lodise, T.P.; Rosenkranz, S.L.; Finnemeyer, M.; Evans, S.; Sims, M.; Zervos, M.J.; Creech, C.B.; Patel, P.C.; Keefer, M.; Riska, P.; et al. The Emperor’s New Clothes: PRospective Observational Evaluation of the Association Between Initial VancomycIn Exposure and Failure Rates Among ADult HospitalizEd Patients With Methicillin-resistant Staphylococcus aureus Bloodstream Infections (PROVIDE). Clin. Infect. Dis. 2019, 70, 1536–1545. [Google Scholar] [CrossRef]
- Chavada, R.; Ghosh, N.; Sandaradura, I.; Maley, M.; Van Hal, S.J. Establishment of an AUC0–24 Threshold for Nephrotoxicity Is a Step towards Individualized Vancomycin Dosing for Methicillin-Resistant Staphylococcus aureus Bacteremia. Antimicrob. Agents Chemother. 2017, 61, e02535-16. [Google Scholar] [CrossRef] [PubMed]
- Dalton, B.R.; Rajakumar, I.; Langevin, A.; Ondro, C.; Sabuda, D.; Griener, T.P.; Dersch-Mills, D.; Rennert-May, E. Vancomycin area under the curve to minimum inhibitory concentration ratio predicting clinical outcome: A systematic review and meta-analysis with pooled sensitivity and specificity. Clin. Microbiol. Infect. 2020, 26, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Brown, K.; Forrest, A. Vancomycin AUC24/MIC Ratio in Patients with Complicated Bacteremia and Infective Endocarditis Due to Methicillin-Resistant Staphylococcus aureus and Its Association with Attributable Mortality during Hospitalization. Antimicrob. Agents Chemother. 2012, 56, 634. [Google Scholar] [CrossRef] [PubMed]
- Moise-Broder, P.A.; Forrest, A.; Birmingham, M.C.; Schentag, J.J. Pharmacodynamics of Vancomycin and Other Antimicrobials in Patients with Staphylococcus aureus Lower Respiratory Tract Infections. Clin. Pharmacokinet. 2004, 43, 925–942. [Google Scholar] [CrossRef] [PubMed]
- Kullar, R.; Davis, S.L.; Levine, D.P.; Rybak, M.J. Impact of Vancomycin Exposure on Outcomes in Patients With Methicillin-Resistant Staphylococcus aureus Bacteremia: Support for Consensus Guidelines Suggested Targets. Clin. Infect. Dis. 2011, 52, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Pai, M.P.; Neely, M.; Rodvold, K.A.; Lodise, T.P. Innovative approaches to optimizing the delivery of vancomycin in individual patients. Adv. Drug Deliv. Rev. 2014, 77, 50–57. [Google Scholar] [CrossRef]
- Pea, F.; Bertolissi, M.; Di Silvestre, A.; Poz, D.; Giordano, F.; Furlanut, M. TDM coupled with Bayesian forecasting should be considered an invaluable tool for optimizing vancomycin daily exposure in unstable critically ill patients. Int. J. Antimicrob. Agents 2002, 20, 326–332. [Google Scholar] [CrossRef]
- Al-Sulaiti, F.K.; Nader, A.M.; Saad, M.O.; Shaukat, A.; Parakadavathu, R.; Elzubair, A.; Al-Badriyeh, D.; Elewa, H.; Awaisu, A. Clinical and Pharmacokinetic Outcomes of Peak–Trough-Based Versus Trough-Based Vancomycin Therapeutic Drug Monitoring Approaches: A Pragmatic Randomized Controlled Trial. Eur. J. Drug Metab. Pharmacokinet. 2019, 44, 639–652. [Google Scholar] [CrossRef]
- Song, K.-H.; Bin Kim, H.; Kim, H.-S.; Lee, M.J.; Jung, Y.; Kim, G.; Hwang, J.-H.; Kim, N.-H.; Kim, M.; Kim, C.J.; et al. Impact of area under the concentration–time curve to minimum inhibitory concentration ratio on vancomycin treatment outcomes in methicillin-resistant Staphylococcus aureus bacteraemia. Int. J. Antimicrob. Agents 2015, 46, 689–695. [Google Scholar] [CrossRef]
- Chan, M.; Ostermann, M. Outcomes of Chronic Hemodialysis Patients in the Intensive Care Unit. Crit. Care Res. Pract. 2013, 2013, 1–7. [Google Scholar] [CrossRef]
- Cho, K.C.; Himmelfarb, J.; Paganini, E.; Ikizler, T.A.; Soroko, S.H.; Mehta, R.L.; Chertow, G.M. Survival by Dialysis Modality in Critically Ill Patients with Acute Kidney Injury. J. Am. Soc. Nephrol. 2006, 17, 3132–3138. [Google Scholar] [CrossRef]
- Zasowski, E.J.; Murray, K.P.; Trinh, T.D.; Finch, N.A.; Pogue, J.M.; Mynatt, R.P.; Rybak, M.J. Identification of Vancomycin Exposure-Toxicity Thresholds in Hospitalized Patients Receiving Intravenous Vancomycin. Antimicrob. Agents Chemother. 2018, 62, e01684-17. [Google Scholar] [CrossRef] [PubMed]
- Mogle, B.T.; Steele, J.M.; Seabury, R.W.; Dang, U.J.; Kufel, W.D. Implementation of a two-point pharmacokinetic AUC-based vancomycin therapeutic drug monitoring approach in patients with methicillin-resistant Staphylococcus aureus bacteraemia. Int. J. Antimicrob. Agents 2018, 52, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Kawasaki, K.; Sato, Y.; Tokimatsu, I.; Itoh, H.; Hiramatsu, K.; Takeyama, M.; Kadota, J.-I. Is Peak Concentration Needed in Therapeutic Drug Monitoring of Vancomycin? A Pharmacokinetic-Pharmacodynamic Analysis in Patients with Methicillin-Resistant Staphylococcus aureus Pneumonia. Chemotherapy 2012, 58, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Lodise, T.P.; Patel, N.; Lomaestro, B.M.; Rodvold, K.A.; Drusano, G.L. Relationship between Initial Vancomycin Concentration-Time Profile and Nephrotoxicity among Hospitalized Patients. Clin. Infect. Dis. 2009, 49, 507–514. [Google Scholar] [CrossRef]
- Aljefri, D.M.; Avedissian, S.N.; Rhodes, N.J.; Postelnick, M.J.; Nguyen, K.; Scheetz, M.H. Vancomycin Area Under the Curve and Acute Kidney Injury: A Meta-analysis. Clin. Infect. Dis. 2019, 69, 1881–1887. [Google Scholar] [CrossRef]
- Ray, A.S.; Haikal, A.; Hammoud, K.A.; Yu, A.S.L. Vancomycin and the Risk of AKI: A Systematic Review and Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2016, 11, 2132–2140. [Google Scholar]
- Zhang, Y.; Wang, T.; Zhang, D.; You, H.; Dong, Y.; Liu, Y.; Du, Q.; Sun, D.; Zhang, T.; Dong, Y. Therapeutic Drug Monitoring Coupled With Bayesian Forecasting Could Prevent Vancomycin-Associated Nephrotoxicity in Renal Insufficiency Patients: A Prospective Study and Pharmacoeconomic Analysis. Ther. Drug Monit. 2020, 42, 600–609. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- Rybak, M.J.; Lomaestro, B.M.; Rotschafer, J.C.; Moellering, J.R.C.; Craig, W.A.; Billeter, M.; Dalovisio, J.R.; Levine, D.P. Vancomycin Therapeutic Guidelines: A Summary of Consensus Recommendations from the Infectious Diseases Society of America, the American Society of Health-System Pharmacists, and the Society of Infectious Diseases Pharmacists. Clin. Infect. Dis. 2009, 49, 325–327. [Google Scholar] [CrossRef]

| Characteristics | Values |
|---|---|
| Gender, male, n (%) | 88 (67.2) |
| Age, years, mean (SD) | 70.1 (15.8) |
| Weight, kg, mean (SD) | 61.5 (14.9) |
| Creatinine clearance, mL/min, mean (SD) | 30.9 (29.5) |
| Critically ill*, n (%) | 82 (62.6) |
| Indication, n (%) | |
| Pneumonia | 56 (42.7) |
| Bacteremia | 39 (29.8) |
| Urinary tract infection | 5 (3.8) |
| Skin and soft tissue infections | 18 (13.7) |
| Catheter-related bloodstream infection | 3 (2.3) |
| Central nervous system infection | 2 (1.5) |
| Septic joint infection | 4 (3.1) |
| Others | 4 (3.1) |
| Microbiological phenotypes | |
| MICBMD range (µg/mL) | 0.5–2 |
| 0.5, n (%) | 39 (29.8) |
| 1, n (%) | 84 (64.1) |
| 2, n (%) | 8 (6.1) |
| MICBMD50/90 | 1/1 |
| Vancomycin exposure variables, mean (SD) | |
| AUC0–24h | 561.1 (182.9) |
| AUC0–24h/MICBMD | 706.6 (365.3) |
| AUC24–48h | 646.7 (311.2) |
| AUC24–48h/MICBMD | 802.7 (492.3) |
| AUCss | 666.8 (360.1) |
| AUCss/MICBMD | 838.9 (446.6) |
| Outcomes | n (%) |
|---|---|
| Treatment failure | 40 (30.5) |
| 30-day mortality | 38 (29) |
| Microbiological failure | 6 (4.6) |
| Acute kidney injury | 17 (19.1) |
| Vancomycin Exposure | n | Treatment Failure | 30-Day Mortality | Microbiological Failure | ||||
|---|---|---|---|---|---|---|---|---|
| n (%) | p-value | n (%) | p-value | n (%) | p-value | |||
| AUC0–24h/MICBMD | ≥626 | 67 | 22 (32.8) | 0.558 | 20 (29.9) | 0.828 | 3 (4.5) | 0.954 |
| <626 | 64 | 18 (28.1) | 18 (28.1) | 3 (4.7) | ||||
| AUC24–48h/MICBMD | ≥698 | 68 | 19 (27.9) | 0.503 | 18 (26.5) | 0.506 | 3 (4.4) | 0.924 |
| <698 | 63 | 21 (33.3) | 21 (31.7) | 3 (4.8) | ||||
| AUCss /MICBMD | ≥679 | 65 | 20 (30.8) | 0.954 | 18 (27.7) | 0.742 | 3 (4.6) | 0.985 |
| <679 | 66 | 20 (30.3) | 20 (30.3) | 3 (4.5) | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chattaweelarp, T.; Changpradub, D.; Punyawudho, B.; Thunyaharn, S.; Santimaleeworagun, W. Is Early Monitoring Better? Impact of Early Vancomycin Exposure on Treatment Outcomes and Nephrotoxicity in Patients with Methicillin-Resistant Staphylococcus aureus Infections. Antibiotics 2020, 9, 672. https://doi.org/10.3390/antibiotics9100672
Chattaweelarp T, Changpradub D, Punyawudho B, Thunyaharn S, Santimaleeworagun W. Is Early Monitoring Better? Impact of Early Vancomycin Exposure on Treatment Outcomes and Nephrotoxicity in Patients with Methicillin-Resistant Staphylococcus aureus Infections. Antibiotics. 2020; 9(10):672. https://doi.org/10.3390/antibiotics9100672
Chicago/Turabian StyleChattaweelarp, Thanawat, Dhitiwat Changpradub, Baralee Punyawudho, Sudaluck Thunyaharn, and Wichai Santimaleeworagun. 2020. "Is Early Monitoring Better? Impact of Early Vancomycin Exposure on Treatment Outcomes and Nephrotoxicity in Patients with Methicillin-Resistant Staphylococcus aureus Infections" Antibiotics 9, no. 10: 672. https://doi.org/10.3390/antibiotics9100672
APA StyleChattaweelarp, T., Changpradub, D., Punyawudho, B., Thunyaharn, S., & Santimaleeworagun, W. (2020). Is Early Monitoring Better? Impact of Early Vancomycin Exposure on Treatment Outcomes and Nephrotoxicity in Patients with Methicillin-Resistant Staphylococcus aureus Infections. Antibiotics, 9(10), 672. https://doi.org/10.3390/antibiotics9100672





