Marine Antimicrobial Peptides: Emerging Strategies Against Multidrug-Resistant and Biofilm-Forming Bacteria
Abstract
1. Introduction
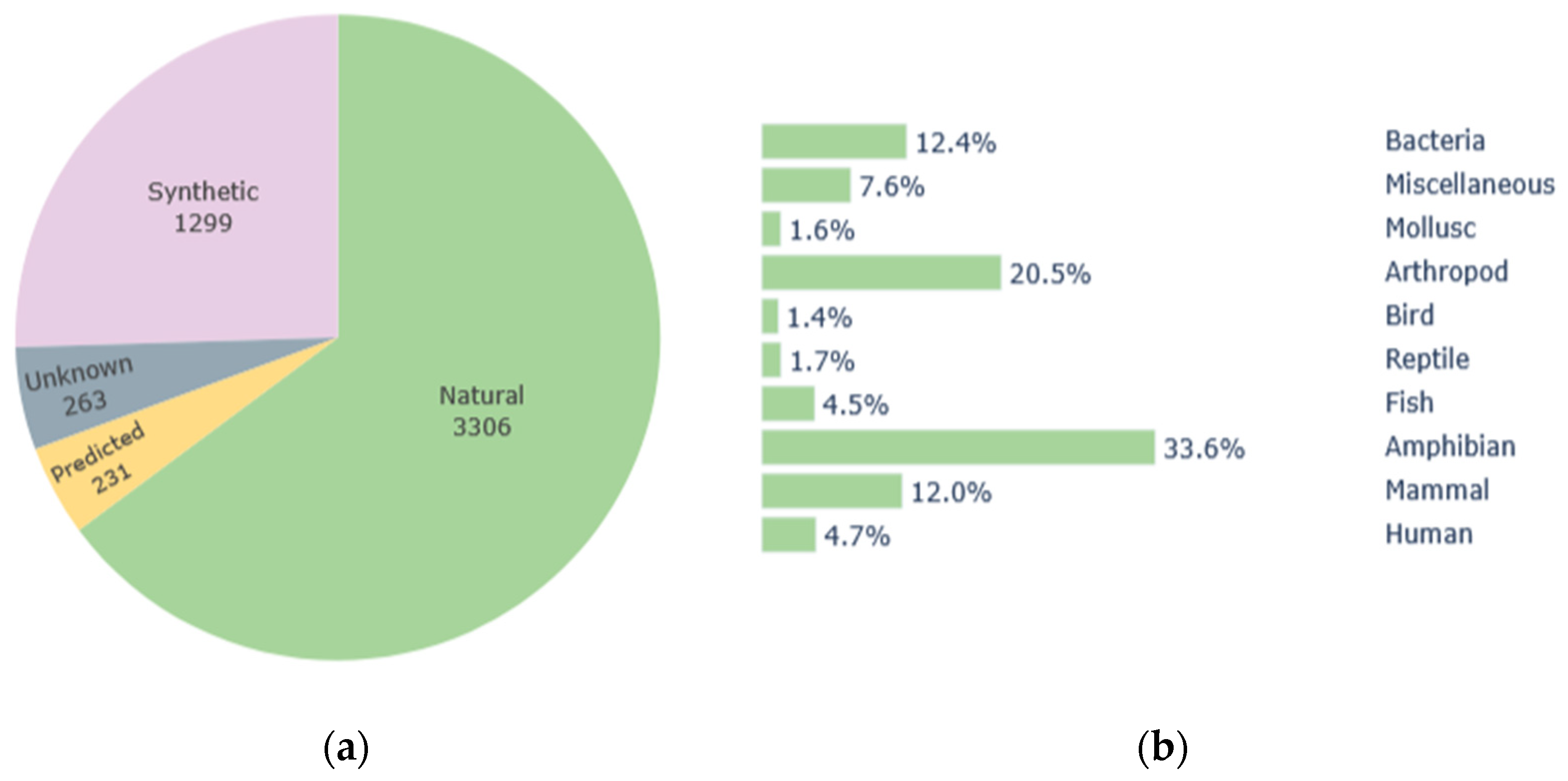
2. Antimicrobial Peptides
3. Marine AMPs Against Antibiotic Resistance
4. Marine AMPs Against Biofilm
| Compound | Source | Mechanism of Action | Antibiofilm Activity | References |
|---|---|---|---|---|
| Pleurocidin | Winter flounder (Pleuronectes americanus) | Membrane permeation and metabolic inhibition | S treptococcus mutans (75% reduction at 64 µg/mL); S. aureus (MBIC of 4 µM) | [42,45,73] |
| Tachyplesin III | Horseshoe crabs (Tachypleus gigas and Carcinoscorpius rotundicauda) | Disruption of the cell membrane structure and ROS production | Pseudomonas aeruginosa ATCC 27853 (MIC and MBC values of 4 and 32 µg/mL alone and 2 µg/mL and 8 µg/mL when associated with piperacillin-tazobactam) | [74,91] |
| Gaduscidin-1 | Atlantic codfish (Gadus morhua) | Reducing biofilm adhesion and ROS production | P. aeruginosa PAO1 biofilms show less 15 to 27% adhesion values (0.5 μM) | [75] |
| Cm-CATH2 | Green sea turtle (Chlonia mydas) | Membrane permeation and cell disruption | Vibrio vulnificus (73.68% reduction), Staphylococcus aureus CMCC26003 (77.77% reduction), Enterococcus faecium (93% reduction) and S. aureus (96% reduction) | [76,77] |
| Hc-CATH | Sea snake (Hydrophis cyanocinctus) | Membrane permeation and cell disruption | V. vulnificus (74.55% reduction) and S. aureus CMCC26003 (71.64% reduction) | [76] |
| Holothuroidin 1 | Sea-cucumber (Holothuria tubulosa) | Interference with the initial bacterial adhesion, elimination of early bacterial colonizers and inhibition of QS | S. aureus ATCC 25923 (51.8% reduction at 3.2 3200 mg/mL; 37.9% reduction at 1500 3.2 mg/mL), Staphylococcus epidermidis ATCC 35984 (68.5% reduction at 3200 3.2 mg/mL; 58.2% reduction at 1500 3.2 mg/mL) and P. aeruginosa ATCC 15442 (69.9% reduction at 6200 3.2 mg/mL; 62.7% reduction at 3100 3.2 mg/mL) | [19,80] |
| Holothuroidin 2 | Sea-cucumber (Holothuria tubulosa) | Interference with the initial bacterial adhesion, elimination of early bacterial colonizers and inhibition of QS | S. aureus ATCC 25923 (57.7% reduction at 3200 μg/mL; 40.5% reduction at 1500 μg/mL), S. epidermidis ATCC 35984 (73.8% reduction at 3200 μg/mL; 59.7% reduction at 1500 μg/mL) and P. aeruginosa ATCC 15442 (64.3% reduction at 6200 μg/mL; 43.8% reduction at 3100 μg/mL) | [19,80] |
| Paracentrin 1 | Sea-urchin (Paracentrotus lividus) | Unknown | S. aureus 25923, S. aureus 29213, S. aureus 6538, S. epidermidis RP62A and P. aeruginosa 15442 (~80% at 6200 μg/mL) | [12,19,79] |
| Rpdef1α | Manila clam (Ruditapes philippinarum) | Reduction in the initial attachment or stimulation of bacteria motility | Escherichia coli MG1655 | [82] |
| Phibilin | Two-striped slug Philomycus bilineatus | Prevention of the development of hyphae by destruction of the budding sites | Action against biofilm formation but also mature Candida albicans biofilms | [81] |
| Capitellacin | Polychaeta (Capitella teleta) | Membrane accumulation and consequent conductivity fluctuations. Membrane destruction when the threshold is reached | Action against biofilm formation but also E scherichia coli SBS 1936 mature biofilms | [92] |
| LFX01 | Lactiplantibacillus plantarum strain LF-8 | Unknown | Shigella flexneri 14 | [93] |
| Pontifactin | Pontibacter korlensis SBK-47 | Inhibition of microbial adhesion | Bacillus subtilis MRCC 619, S. aureus MTCC 96 and Vibrio cholerae MTCC3906 (99% reduction at 2000 μg/mL) | [94] |
| Pumilacidin-like cyclopeptide | Bacillus sp. 176 | Inhibition of microbial motility and adhesion | P. aeruginosa and B. subtilis (>50% reduction at 300 μg/mL) | [95] |
| Cyclo (Trp-Ser) | Rheinheimera aquimaris QS102 | Inhibition of QS | P. aeruginosa PAO1 (59.9% reduction at 200 μg/mL) | [70] |
| Cyclo (L-Trp-L-Pro) | Penicillium chruso genum DXY-1 | Inhibition of QS | P. aeruginosa PAO1 (48% reduction at 500 μg/mL) | [71] |
| Nesfactin | Nesterenkonia sp. MSA31 | Inhibition of QS | P. aeruginosa FSPA09 (90% reduction at 75,000 μg/mL) | [96] |
| Epicotripeptin | Epicoccum nigrum M13 | Unknown | B. subtilis ATCC6633, S. aureus NRRLB-767 (100 µg/mL) | [97] |
| Crustin (Pp-Cru) | Blue swimmer crab (Portunus pelagicus) | Membrane permeation and cell disruption | S. aureus, E. faecalis, P. aeruginosa, E. coli (100 μg/mL) | [98] |
| Crustin (Ps-cr) | Green tiger shrimp (Peaneaus semisulcatus) | Inhibition of bacterial adherence | Bacillus thuringiensis, B. pumilis, V. parahaemolyticus, and V. alginolyticuls (40 μg/mL) | [99] |
5. Current Challenges
6. Conclusions
7. Future Directions
8. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMP | Antimicrobial Peptide |
| MDR | Multidrug Resistant |
| APD3 | Antimicrobial Peptide Database 3 |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| MIC | Minimal Inhibitory Concentration |
| MBIC | Minimum Biofilm Inhibitory Concentration |
| ROS | Reactive Oxygen Species |
| VRE | Vancomycin-Resistant Enterococci |
| ESBL | Extended-Spectrum Beta-Lactamase |
| QS | Quorum Sensing |
| PAMPs | Pathogen-associated molecular patterns |
| QSI | Quorum sensing inhibitors |
| DKP | Diketopiperazine |
References
- Ho, C.S.; Wong, C.T.H.; Aung, T.T.; Lakshminarayanan, R.; Mehta, J.S.; Rauz, S.; McNally, A.; Kintses, B.; Peacock, S.J.; de la Fuente-Nunez, C.; et al. Antimicrobial Resistance: A Concise Update. Lancet Microbe 2025, 6, 100947. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- World Health Organization. Seventy-Eighth World Health Assembly-Daily Update: 27 May 2025. Available online: https://www.who.int/news/item/27-05-2025-seventy-eighth-world-health-assembly---daily-update--27-may-2025 (accessed on 27 July 2025).
- Xuan, J.; Feng, W.; Wang, J.; Wang, R.; Zhang, B.; Bo, L.; Chen, Z.-S.; Yang, H.; Sun, L. Antimicrobial Peptides for Combating Drug-Resistant Bacterial Infections. Drug Resist. Updat. 2023, 68, 100954. [Google Scholar] [CrossRef]
- Díaz-Puertas, R.; Adamek, M.; Mallavia, R.; Falco, A. Fish Skin Mucus Extracts: An Underexplored Source of Antimicrobial Agents. Mar. Drugs 2023, 21, 350. [Google Scholar] [CrossRef]
- Shahidi, F.; Saeid, A. Bioactivity of Marine-Derived Peptides and Proteins: A Review. Mar. Drugs 2025, 23, 157. [Google Scholar] [CrossRef]
- Santhiravel, S.; Dave, D.; Shahidi, F. Bioactives from Marine Resources as Natural Health Products: A Review. Pharmacol. Rev. 2025, 77, 100009. [Google Scholar] [CrossRef]
- Shahidi, F.; Santhiravel, S. Novel Marine Bioactives: Application in Functional Foods, Nutraceuticals, and Pharmaceuticals. J. Food Bioact. 2022, 19, 4–96. [Google Scholar] [CrossRef]
- Saucedo-Vázquez, J.P.; Gushque, F.; Vispo, N.S.; Rodriguez, J.; Gudiño-Gomezjurado, M.E.; Albericio, F.; Tellkamp, M.P.; Alexis, F. Marine Arthropods as a Source of Antimicrobial Peptides. Mar. Drugs 2022, 20, 501. [Google Scholar] [CrossRef]
- Wang, G.; Li, X.; Wang, Z. APD3: The Antimicrobial Peptide Database as a Tool for Research and Education. Nucleic Acids Res. 2016, 44, D1087–D1093. [Google Scholar] [CrossRef]
- Masso-Silva, J.; Diamond, G. Antimicrobial Peptides from Fish. Pharmaceuticals 2014, 7, 265–310. [Google Scholar] [CrossRef]
- Thomas, A.M.; Antony, S.P. Marine Antimicrobial Peptides: An Emerging Nightmare to the Life-Threatening Pathogens. Probiotics Antimicrob. Proteins 2024, 16, 552–578. [Google Scholar] [CrossRef]
- García, F.A.; Fuentes, T.F.; Alonso, I.P.; Bosch, R.A.; Brunetti, A.E.; Lopes, N.P. A Comprehensive Review of Patented Antimicrobial Peptides from Amphibian Anurans. J. Nat. Prod. 2024, 87, 600–616. [Google Scholar] [CrossRef]
- Van Hoek, M. Antimicrobial Peptides in Reptiles. Pharmaceuticals 2014, 7, 723–753. [Google Scholar] [CrossRef]
- Chen, P.; Ye, T.; Li, C.; Praveen, P.; Hu, Z.; Li, W.; Shang, C. Embracing the Era of Antimicrobial Peptides with Marine Organisms. Nat. Prod. Rep. 2024, 41, 331–346. [Google Scholar] [CrossRef]
- Lu, S.; Lin, J.; Jin, J.; Zhang, L.; Guan, Y.; Chen, H.; Wu, Y.; Zhang, W.; Luan, X. Tachyplesin I and Its Derivatives: A Pharmaco-Chemical Perspective on Their Antimicrobial and Antitumor Potential. Expert Opin. Drug Discov. 2022, 17, 1407–1423. [Google Scholar] [CrossRef]
- Kanaujia, K.A.; Wagh, S.; Pandey, G.; Phatale, V.; Khairnar, P.; Kolipaka, T.; Rajinikanth, P.S.; Saraf, S.A.; Srivastava, S.; Kumar, S. Harnessing Marine Antimicrobial Peptides for Novel Therapeutics: A Deep Dive into Ocean-Derived Bioactives. Int. J. Biol. Macromol. 2025, 307, 142158. [Google Scholar] [CrossRef]
- Sarkar, T.; Chetia, M.; Chatterjee, S. Antimicrobial Peptides and Proteins: From Nature’s Reservoir to the Laboratory and Beyond. Front. Chem. 2021, 9, 691532. [Google Scholar] [CrossRef]
- Guryanova, S.V.; Balandin, S.V.; Belogurova-Ovchinnikova, O.Y.; Ovchinnikova, T.V. Marine Invertebrate Antimicrobial Peptides and Their Potential as Novel Peptide Antibiotics. Mar. Drugs 2023, 21, 503. [Google Scholar] [CrossRef]
- Macedo, M.W.F.S.; Cunha, N.B.D.; Carneiro, J.A.; Costa, R.A.D.; Alencar, S.A.D.; Cardoso, M.H.; Franco, O.L.; Dias, S.C. Marine Organisms as a Rich Source of Biologically Active Peptides. Front. Mar. Sci. 2021, 8, 667764. [Google Scholar] [CrossRef]
- Wu, R.; Patocka, J.; Nepovimova, E.; Oleksak, P.; Valis, M.; Wu, W.; Kuca, K. Marine Invertebrate Peptides: Antimicrobial Peptides. Front. Microbiol. 2021, 12, 785085. [Google Scholar] [CrossRef]
- Yin, Z.-X.; He, W.; Chen, W.-J.; Yan, J.-H.; Yang, J.-N.; Chan, S.-M.; He, J.-G. Cloning, Expression and Antimicrobial Activity of an Antimicrobial Peptide, Epinecidin-1, from the Orange-Spotted Grouper, Epinephelus coioides. Aquaculture 2006, 253, 204–211. [Google Scholar] [CrossRef]
- Asensio-Calavia, P.; González-Acosta, S.; Otazo-Pérez, A.; López, M.R.; Morales-delaNuez, A.; Pérez De La Lastra, J.M. Teleost Piscidins—In Silico Perspective of Natural Peptide Antibiotics from Marine Sources. Antibiotics 2023, 12, 855. [Google Scholar] [CrossRef]
- Patra, A.; Das, J.; Agrawal, N.R.; Kushwaha, G.S.; Ghosh, M.; Son, Y.-O. Marine Antimicrobial Peptides-Based Strategies for Tackling Bacterial Biofilm and Biofouling Challenges. Molecules 2022, 27, 7546. [Google Scholar] [CrossRef]
- Hancock, R.E.W.; Sahl, H.-G. Antimicrobial and Host-Defense Peptides as New Anti-Infective Therapeutic Strategies. Nat. Biotechnol. 2006, 24, 1551–1557. [Google Scholar] [CrossRef]
- Semreen, M.H.; El-Gamal, M.I.; Abdin, S.; Alkhazraji, H.; Kamal, L.; Hammad, S.; El-Awady, F.; Waleed, D.; Kourbaj, L. Recent Updates of Marine Antimicrobial Peptides. Saudi Pharm. J. 2018, 26, 396–409. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, J.; Chen, Y. Alpha-helical Cationic Antimicrobial Peptides: Relationships of Structure and Function. Protein Cell 2010, 1, 143–152. [Google Scholar] [CrossRef]
- Mura, M.; Wang, J.; Zhou, Y.; Pinna, M.; Zvelindovsky, A.V.; Dennison, S.R.; Phoenix, D.A. The Effect of Amidation on the Behaviour of Antimicrobial Peptides. Eur. Biophys. J. 2016, 45, 195–207. [Google Scholar] [CrossRef]
- Sengupta, D.; Leontiadou, H.; Mark, A.E.; Marrink, S.-J. Toroidal Pores Formed by Antimicrobial Peptides Show Significant Disorder. Biochim. Biophys. Acta (BBA)-Biomembr. 2008, 1778, 2308–2317. [Google Scholar] [CrossRef]
- Joo, H.-S.; Fu, C.-I.; Otto, M. Bacterial Strategies of Resistance to Antimicrobial Peptides. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150292. [Google Scholar] [CrossRef]
- Sperstad, S.V.; Haug, T.; Blencke, H.-M.; Styrvold, O.B.; Li, C.; Stensvåg, K. Antimicrobial Peptides from Marine Invertebrates: Challenges and Perspectives in Marine Antimicrobial Peptide Discovery. Biotechnol. Adv. 2011, 29, 519–530. [Google Scholar] [CrossRef]
- Powers, J.-P.S.; Hancock, R.E.W. The Relationship between Peptide Structure and Antibacterial Activity. Peptides 2003, 24, 1681–1691. [Google Scholar] [CrossRef]
- Zhang, Y.; Bao, C.; Shen, L.; Tian, C.; Zang, X.; Chen, G.; Zhang, S. Microbial Cold Shock Proteins: Overview of Their Function and Mechanism of Action. Protein Pept. Lett. 2022, 29, 133–142. [Google Scholar] [CrossRef]
- Falanga, A.; Lombardi, L.; Franci, G.; Vitiello, M.; Iovene, M.; Morelli, G.; Galdiero, M.; Galdiero, S. Marine Antimicrobial Peptides: Nature Provides Templates for the Design of Novel Compounds against Pathogenic Bacteria. Int. J. Mol. Sci. 2016, 17, 785. [Google Scholar] [CrossRef]
- Lei, Y.; He, D.; Zhao, X.; Miao, L.; Cao, Z. Structure, Function, and Therapeutic Potential of Defensins from Marine Animals. Fish Shellfish Immunol. 2025, 163, 110365. [Google Scholar] [CrossRef]
- Inguglia, L.; Chiaramonte, M.; Arizza, V.; Turiák, L.; Vékey, K.; Drahos, L.; Pitonzo, R.; Avellone, G.; Di Stefano, V. Changes in the Proteome of Sea Urchin Paracentrotus Lividus Coelomocytes in Response to LPS Injection into the Body Cavity. PLoS ONE 2020, 15, e0228893. [Google Scholar] [CrossRef]
- Fraune, S.; Augustin, R.; Anton-Erxleben, F.; Wittlieb, J.; Gelhaus, C.; Klimovich, V.B.; Samoilovich, M.P.; Bosch, T.C.G. In an Early Branching Metazoan, Bacterial Colonization of the Embryo Is Controlled by Maternal Antimicrobial Peptides. Proc. Natl. Acad. Sci. USA 2010, 107, 18067–18072. [Google Scholar] [CrossRef]
- Khalifa, S.A.M.; Elias, N.; Farag, M.A.; Chen, L.; Saeed, A.; Hegazy, M.-E.F.; Moustafa, M.S.; Abd El-Wahed, A.; Al-Mousawi, S.M.; Musharraf, S.G.; et al. Marine Natural Products: A Source of Novel Anticancer Drugs. Mar. Drugs 2019, 17, 491. [Google Scholar] [CrossRef]
- Zhang, G.; Li, L.; Meng, J.; Qi, H.; Qu, T.; Xu, F.; Zhang, L. Molecular Basis for Adaptation of Oysters to Stressful Marine Intertidal Environments. Annu. Rev. Anim. Biosci. 2016, 4, 357–381. [Google Scholar] [CrossRef]
- Okeke, E.S.; Okagu, I.U.; Chukwudozie, K.; Ezike, T.C.; Ezeorba, T.P.C. Marine-Derived Bioactive Proteins and Peptides: A Review of Current Knowledge on Anticancer Potentials, Clinical Trials, and Future Prospects. Nat. Prod. Commun. 2024, 19, 1–19. [Google Scholar] [CrossRef]
- Barbosa, F.; Pinto, E.; Kijjoa, A.; Pinto, M.; Sousa, E. Targeting Antimicrobial Drug Resistance with Marine Natural Products. Int. J. Antimicrob. Agents 2020, 56, 106005. [Google Scholar] [CrossRef]
- Ko, S.J.; Kang, N.H.; Kim, M.K.; Park, J.; Park, E.; Park, G.H.; Kang, T.W.; Na, D.E.; Park, J.B.; Yi, Y.E.; et al. Antibacterial and Anti-Biofilm Activity, and Mechanism of Action of Pleurocidin against Drug Resistant Staphylococcus aureus. Microb. Pathog. 2019, 127, 70–78. [Google Scholar] [CrossRef]
- Hsu, H.-C.; Chen, M.-H.; Yeh, M.-L.; Chen, W.-J. Antibacterial and Anticancer Activities of Pleurocidin-Amide, a Potent Marine Antimicrobial Peptide Derived from Winter Flounder, Pleuronectes americanus. Mar. Drugs 2022, 20, 519. [Google Scholar] [CrossRef]
- Ramos, C.; Lorenz, K.; Putrinš, M.; Hind, C.K.; Meos, A.; Laidmäe, I.; Tenson, T.; Sutton, J.M.; Mason, A.J.; Kogermann, K. Fibrous Matrices Facilitate Pleurocidin Killing of Wound Associated Bacterial Pathogens. Eur. J. Pharm. Sci. 2024, 192, 106648. [Google Scholar] [CrossRef]
- McMillan, K.A.M.; Coombs, M.R.P. Investigating Potential Applications of the Fish Anti-Microbial Peptide Pleurocidin: A Systematic Review. Pharmaceuticals 2021, 14, 687. [Google Scholar] [CrossRef]
- Talandashti, R.; Mahdiuni, H.; Jafari, M.; Mehrnejad, F. Molecular Basis for Membrane Selectivity of Antimicrobial Peptide Pleurocidin in the Presence of Different Eukaryotic and Prokaryotic Model Membranes. J. Chem. Inf. Model. 2019, 59, 3262–3276. [Google Scholar] [CrossRef]
- Patrzykat, A.; Gallant, J.W.; Seo, J.-K.; Pytyck, J.; Douglas, S.E. Novel Antimicrobial Peptides Derived from Flatfish Genes. Antimicrob. Agents Chemother. 2003, 47, 2464–2470. [Google Scholar] [CrossRef]
- Juliano, S.A.; Serafim, L.F.; Duay, S.S.; Heredia Chavez, M.; Sharma, G.; Rooney, M.; Comert, F.; Pierce, S.; Radulescu, A.; Cotten, M.L.; et al. A Potent Host Defense Peptide Triggers DNA Damage and Is Active against Multidrug-Resistant Gram-Negative Pathogens. ACS Infect. Dis. 2020, 6, 1250–1263. [Google Scholar] [CrossRef]
- Miller, A.; Matera-Witkiewicz, A.; Mikołajczyk, A.; Wieczorek, R.; Rowińska-Żyrek, M. Chemical “Butterfly Effect” Explaining the Coordination Chemistry and Antimicrobial Properties of Clavanin Complexes. Inorg. Chem. 2021, 60, 12730–12734. [Google Scholar] [CrossRef]
- Naing, M.D.; Juliano, S.A.; Angeles-Boza, A.M. Synergy between the Clavanins as a Weapon against Multidrug-Resistant Enterobacter cloacae. RSC Med. Chem. 2024, 15, 2160–2164. [Google Scholar] [CrossRef]
- Juliano, S.A.; Pierce, S.; deMayo, J.A.; Balunas, M.J.; Angeles-Boza, A.M. Exploration of the Innate Immune System of Styela clava: Zn2+ Binding Enhances the Antimicrobial Activity of the Tunicate Peptide Clavanin A. Biochemistry 2017, 56, 1403–1414. [Google Scholar] [CrossRef]
- Duay, S.S.; Sharma, G.; Prabhakar, R.; Angeles-Boza, A.M.; May, E.R. Molecular Dynamics Investigation into the Effect of Zinc(II) on the Structure and Membrane Interactions of the Antimicrobial Peptide Clavanin A. J. Phys. Chem. B 2019, 123, 3163–3176. [Google Scholar] [CrossRef]
- Salimnejhad, Z.; Hassanzadazar, H.; Aminzare, M. Epinecidin-1 (an Active Marine Antimicrobial Peptide): Effects on the Survival of Inoculated Escherichia coli O157:H7 and Staphylococcus aureus Bacteria, Antioxidant, and Sensory Attributes in Raw Milk. Food Sci. Nutr. 2023, 11, 5573–5581. [Google Scholar] [CrossRef]
- Bolatchiev, A. Antimicrobial Peptides Epinecidin-1 and Beta-Defesin-3 Are Effective against a Broad Spectrum of Antibiotic-Resistant Bacterial Isolates and Increase Survival Rate in Experimental Sepsis. Antibiotics 2022, 11, 76. [Google Scholar] [CrossRef]
- Huang, H.-N.; Pan, C.-Y.; Su, B.-C.; Wu, H.-Y.; Chen, J.-Y. Epinecidin-1 Protects against Methicillin Resistant Staphylococcus aureus Infection and Sepsis in Pyemia Pigs. Mar. Drugs 2019, 17, 693. [Google Scholar] [CrossRef]
- Narayana, J.L.; Huang, H.-N.; Wu, C.-J.; Chen, J.-Y. Epinecidin-1 Antimicrobial Activity: In Vitro Membrane Lysis and In Vivo Efficacy against Helicobacter Pylori Infection in a Mouse Model. Biomaterials 2015, 61, 41–51. [Google Scholar] [CrossRef]
- Lee, S.-C.; Pan, C.-Y.; Chen, J.-Y. The Antimicrobial Peptide, Epinecidin-1, Mediates Secretion of Cytokines in the Immune Response to Bacterial Infection in Mice. Peptides 2012, 36, 100–108. [Google Scholar] [CrossRef]
- Pan, C.-Y.; Chen, J.-C.; Chen, T.-L.; Wu, J.-L.; Hui, C.-F.; Chen, J.-Y. Piscidin Is Highly Active against Carbapenem-Resistant Acinetobacter baumannii and NDM-1-Producing Klebsiella pneumonia in a Systemic Septicaemia Infection Mouse Model. Mar. Drugs 2015, 13, 2287–2305. [Google Scholar] [CrossRef]
- Huang, H.-N.; Chan, Y.-L.; Hui, C.-F.; Wu, J.-L.; Wu, C.-J.; Chen, J.-Y. Use of Tilapia Piscidin 3 (TP3) to Protect against MRSA Infection in Mice with Skin Injuries. Oncotarget 2015, 6, 12955–12969. [Google Scholar] [CrossRef]
- Peng, K.-C.; Lee, S.-H.; Hour, A.-L.; Pan, C.-Y.; Lee, L.-H.; Chen, J.-Y. Five Different Piscidins from Nile Tilapia, Oreochromis niloticus: Analysis of Their Expressions and Biological Functions. PLoS ONE 2012, 7, e50263. [Google Scholar] [CrossRef]
- Huang, H.-N.; Chan, Y.-L.; Wu, C.-J.; Chen, J.-Y. Tilapia Piscidin 4 (TP4) Stimulates Cell Proliferation and Wound Closure in MRSA-Infected Wounds in Mice. Mar. Drugs 2015, 13, 2813–2833. [Google Scholar] [CrossRef]
- Oliveira, M.; Cunha, E.; Tavares, L.; Serrano, I. P. aeruginosa Interactions with Other Microbes in Biofilms during Co-Infection. AIMS Microbiol. 2023, 9, 612–646. [Google Scholar] [CrossRef]
- Jamal, M.; Ahmad, W.; Andleeb, S.; Jalil, F.; Imran, M.; Nawaz, M.A.; Hussain, T.; Ali, M.; Rafiq, M.; Kamil, M.A. Bacterial Biofilm and Associated Infections. J. Chin. Med. Assoc. 2018, 81, 7–11. [Google Scholar] [CrossRef]
- Sukmarini, L.; Atikana, A.; Hertiani, T. Antibiofilm Activity of Marine Microbial Natural Products: Potential Peptide- and Polyketide-Derived Molecules from Marine Microbes toward Targeting Biofilm-Forming Pathogens. J. Nat. Med. 2024, 78, 1–20. [Google Scholar] [CrossRef]
- Ciofu, O.; Moser, C.; Jensen, P.Ø.; Høiby, N. Tolerance and Resistance of Microbial Biofilms. Nat. Rev. Microbiol. 2022, 20, 621–635. [Google Scholar] [CrossRef]
- Hall, C.W.; Mah, T.-F. Molecular Mechanisms of Biofilm-Based Antibiotic Resistance and Tolerance in Pathogenic Bacteria. FEMS Microbiol. Rev. 2017, 41, 276–301. [Google Scholar] [CrossRef]
- Stewart, P.S. Antimicrobial Tolerance in Biofilms. In Microbial Biofilms; Ghannoum, M., Parsek, M., Whiteley, M., Mukherjee, P.K., Eds.; ASM Press: Washington, DC, USA, 2015; pp. 269–285. ISBN 978-1-68367-091-9. [Google Scholar]
- Olsen, I. Biofilm-Specific Antibiotic Tolerance and Resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 877–886. [Google Scholar] [CrossRef]
- Ciofu, O.; Rojo-Molinero, E.; Macià, M.D.; Oliver, A. Antibiotic Treatment of Biofilm Infections. APMIS 2017, 125, 304–319. [Google Scholar] [CrossRef]
- Sun, S.; Dai, X.; Sun, J.; Bu, X.; Weng, C.; Li, H.; Zhu, H. A Diketopiperazine Factor from Rheinheimera aquimaris QSI02 Exhibits Anti-Quorum Sensing Activity. Sci. Rep. 2016, 6, 39637. [Google Scholar] [CrossRef]
- Yu, X.; Li, L.; Sun, S.; Chang, A.; Dai, X.; Li, H.; Wang, Y.; Zhu, H. A Cyclic Dipeptide from Marine Fungus Penicillium chrysogenum DXY-1 Exhibits Anti-Quorum Sensing Activity. ACS Omega 2021, 6, 7693–7700. [Google Scholar] [CrossRef]
- Cole, A.M.; Weis, P.; Diamond, G. Isolation and Characterization of Pleurocidin, an Antimicrobial Peptide in the Skin Secretions of Winter Flounder. J. Biol. Chem. 1997, 272, 12008–12013. [Google Scholar] [CrossRef]
- Tao, R.; Tong, Z.; Lin, Y.; Xue, Y.; Wang, W.; Kuang, R.; Wang, P.; Tian, Y.; Ni, L. Antimicrobial and Antibiofilm Activity of Pleurocidin against Cariogenic Microorganisms. Peptides 2011, 32, 1748–1754. [Google Scholar] [CrossRef]
- Minardi, D.; Ghiselli, R.; Cirioni, O.; Giacometti, A.; Kamysz, W.; Orlando, F.; Silvestri, C.; Parri, G.; Kamysz, E.; Scalise, G.; et al. The Antimicrobial Peptide Tachyplesin III Coated Alone and in Combination with Intraperitoneal Piperacillin-Tazobactam Prevents Ureteral Stent Pseudomonas Infection in a Rat Subcutaneous Pouch Model. Peptides 2007, 28, 2293–2298. [Google Scholar] [CrossRef]
- Portelinha, J.; Angeles-Boza, A.M. The Antimicrobial Peptide Gad-1 Clears Pseudomonas aeruginosa Biofilms under Cystic Fibrosis Conditions. ChemBioChem 2021, 22, 1646–1655. [Google Scholar] [CrossRef]
- Ouyang, J.; Zhu, Y.; Hao, W.; Wang, X.; Yang, H.; Deng, X.; Feng, T.; Huang, Y.; Yu, H.; Wang, Y. Three Naturally Occurring Host Defense Peptides Protect Largemouth Bass (Micropterus salmoides) against Bacterial Infections. Aquaculture 2022, 546, 737383. [Google Scholar] [CrossRef]
- Qiao, X.; Yang, H.; Gao, J.; Zhang, F.; Chu, P.; Yang, Y.; Zhang, M.; Wang, Y.; Yu, H. Diversity, Immunoregulatory Action and Structure-Activity Relationship of Green Sea Turtle Cathelicidins. Dev. Comp. Immunol. 2019, 98, 189–204. [Google Scholar] [CrossRef]
- Carlile, S.R.; Shiels, J.; Kerrigan, L.; Delaney, R.; Megaw, J.; Gilmore, B.F.; Weldon, S.; Dalton, J.P.; Taggart, C.C. Sea Snake Cathelicidin (Hc-Cath) Exerts a Protective Effect in Mouse Models of Lung Inflammation and Infection. Sci. Rep. 2019, 9, 6071. [Google Scholar] [CrossRef]
- Schillaci, D.; Cusimano, M.G.; Spinello, A.; Barone, G.; Russo, D.; Vitale, M.; Parrinello, D.; Arizza, V. Paracentrin 1, a Synthetic Antimicrobial Peptide from the Sea-Urchin Paracentrotus lividus, Interferes with Staphylococcal and Pseudomonas aeruginosa Biofilm Formation. AMB Express 2014, 4, 78. [Google Scholar] [CrossRef]
- Schillaci, D.; Cusimano, M.; Cunsolo, V.; Saletti, R.; Russo, D.; Vazzana, M.; Vitale, M.; Arizza, V. Immune Mediators of Sea-Cucumber Holothuria tubulosa (Echinodermata) as Source of Novel Antimicrobial and Anti-Staphylococcal Biofilm Agents. AMB Express 2013, 3, 35. [Google Scholar] [CrossRef]
- Li, Z.; Jing, X.; Yuan, Y.; Shui, Y.; Li, S.; Zhao, Z.; Deng, B.; Zhang, W. In Vitro and In Vivo Activity of Phibilin Against Candida Albicans. Front. Microbiol. 2022, 13, 862834. [Google Scholar] [CrossRef]
- Lv, C.; Han, Y.; Yang, D.; Zhao, J.; Wang, C.; Mu, C. Antibacterial Activities and Mechanisms of Action of a Defensin from Manila Clam Ruditapes philippinarum. Fish Shellfish Immunol. 2020, 103, 266–276. [Google Scholar] [CrossRef]
- Van Den Bergh, B.; Fauvart, M.; Michiels, J. Formation, Physiology, Ecology, Evolution and Clinical Importance of Bacterial Persisters. FEMS Microbiol. Rev. 2017, 41, 219–251. [Google Scholar] [CrossRef]
- Yang, S.; Hay, I.D.; Cameron, D.R.; Speir, M.; Cui, B.; Su, F.; Peleg, A.Y.; Lithgow, T.; Deighton, M.A.; Qu, Y. Antibiotic Regimen Based on Population Analysis of Residing Persister Cells Eradicates Staphylococcus epidermidis Biofilms. Sci. Rep. 2015, 5, 18578. [Google Scholar] [CrossRef]
- Kester, J.C.; Fortune, S.M. Persisters and beyond: Mechanisms of Phenotypic Drug Resistance and Drug Tolerance in Bacteria. Crit. Rev. Biochem. Mol. Biol. 2014, 49, 91–101. [Google Scholar] [CrossRef]
- Wood, T.K.; Knabel, S.J.; Kwan, B.W. Bacterial Persister Cell Formation and Dormancy. Appl. Environ. Microbiol. 2013, 79, 7116–7121. [Google Scholar] [CrossRef]
- Wainwright, J.; Hobbs, G.; Nakouti, I. Persister Cells: Formation, Resuscitation and Combative Therapies. Arch. Microbiol. 2021, 203, 5899–5906. [Google Scholar] [CrossRef]
- Barman, S.; Kurnaz, L.B.; Leighton, R.; Hossain, M.W.; Decho, A.W.; Tang, C. Intrinsic Antimicrobial Resistance: Molecular Biomaterials to Combat Microbial Biofilms and Bacterial Persisters. Biomaterials 2024, 311, 122690. [Google Scholar] [CrossRef]
- Liu, S.; Brul, S.; Zaat, S.A.J. Bacterial Persister-Cells and Spores in the Food Chain: Their Potential Inactivation by Antimicrobial Peptides (AMPs). Int. J. Mol. Sci. 2020, 21, 8967. [Google Scholar] [CrossRef]
- Libardo, M.D.J.; Bahar, A.A.; Ma, B.; Fu, R.; McCormick, L.E.; Zhao, J.; McCallum, S.A.; Nussinov, R.; Ren, D.; Angeles-Boza, A.M.; et al. Nuclease Activity Gives an Edge to Host-defense Peptide Piscidin 3 over Piscidin 1, Rendering It More Effective against Persisters and Biofilms. FEBS J. 2017, 284, 3662–3683. [Google Scholar] [CrossRef]
- Miao, F.; Tai, Z.; Wang, Y.; Zhu, Q.; Fang, J.K.-H.; Hu, M. Tachyplesin I Analogue Peptide as an Effective Antimicrobial Agent against Candida albicans—Staphylococcus aureus Poly-Biofilm Formation and Mixed Infection. ACS Infect. Dis. 2022, 8, 1839–1850. [Google Scholar] [CrossRef]
- Safronova, V.N.; Panteleev, P.V.; Sukhanov, S.V.; Toropygin, I.Y.; Bolosov, I.A.; Ovchinnikova, T.V. Mechanism of Action and Therapeutic Potential of the β-Hairpin Antimicrobial Peptide Capitellacin from the Marine Polychaeta Capitella Teleta. Mar. Drugs 2022, 20, 167. [Google Scholar] [CrossRef]
- Jiang, Y.-H.; Xin, W.-G.; Zhang, Q.-L.; Lin, L.-B.; Deng, X.-Y. A Novel Bacteriocin Against Shigella flexneri from Lactiplantibacillus plantarum Isolated from Tilapia Intestine: Purification, Antibacterial Properties and Antibiofilm Activity. Front. Microbiol. 2022, 12, 779315. [Google Scholar] [CrossRef]
- Balan, S.S.; Kumar, C.G.; Jayalakshmi, S. Pontifactin, a New Lipopeptide Biosurfactant Produced by a Marine Pontibacter korlensis Strain SBK-47: Purification, Characterization and Its Biological Evaluation. Process Biochem. 2016, 51, 2198–2207. [Google Scholar] [CrossRef]
- Xiu, P.; Liu, R.; Zhang, D.; Sun, C. Pumilacidin-Like Lipopeptides Derived from Marine Bacterium Bacillus sp. Strain 176 Suppress the Motility of Vibrio Alginolyticus. Appl. Environ. Microbiol. 2017, 83, e00450-17. [Google Scholar] [CrossRef]
- Kiran, G.S.; Priyadharsini, S.; Sajayan, A.; Priyadharsini, G.B.; Poulose, N.; Selvin, J. Production of Lipopeptide Biosurfactant by a Marine Nesterenkonia sp. and Its Application in Food Industry. Front. Microbiol. 2017, 8, 1138. [Google Scholar] [CrossRef]
- Qader, M.M.; Hamed, A.A.; Soldatou, S.; Abdelraof, M.; Elawady, M.E.; Hassane, A.S.I.; Belbahri, L.; Ebel, R.; Rateb, M.E. Antimicrobial and Antibiofilm Activities of the Fungal Metabolites Isolated from the Marine Endophytes Epicoccum nigrum M13 and Alternaria alternata 13A. Mar. Drugs 2021, 19, 232. [Google Scholar] [CrossRef]
- Rekha, R.; Vaseeharan, B.; Ishwarya, R.; Anjugam, M.; Alharbi, N.S.; Kadaikunnan, S.; Khaled, J.M.; Al-anbr, M.N.; Govindarajan, M. Searching for Crab-Borne Antimicrobial Peptides: Crustin from Portunus pelagicus Triggers Biofilm Inhibition and Immune responses of Artemia salina against GFP Tagged Vibrio parahaemolyticus Dahv2. Mol. Immunol. 2018, 101, 396–408. [Google Scholar] [CrossRef]
- Sivakamavalli, J.; Arthur James, R.; Park, K.; Kwak, I.-S.; Vaseeharan, B. Purification of WAP Domain-Containing Antimicrobial Peptides from Green Tiger Shrimp Peaneaus semisulcatus. Microb. Pathog. 2020, 140, 103920. [Google Scholar] [CrossRef]
- Sable, R.; Parajuli, P.; Jois, S. Peptides, Peptidomimetics, and Polypeptides from Marine Sources: A Wealth of Natural Sources for Pharmaceutical Applications. Mar. Drugs 2017, 15, 124. [Google Scholar] [CrossRef]
- Torres, M.D.T.; Cao, J.; Franco, O.L.; Lu, T.K.; De La Fuente-Nunez, C. Synthetic Biology and Computer-Based Frameworks for Antimicrobial Peptide Discovery. ACS Nano 2021, 15, 2143–2164. [Google Scholar] [CrossRef]
- Taheri-Araghi, S. Synergistic Action of Antimicrobial Peptides and Antibiotics: Current Understanding and Future Directions. Front. Microbiol. 2024, 15, 1390765. [Google Scholar] [CrossRef]
- Bolosov, I.A.; Kalashnikov, A.A.; Panteleev, P.V.; Ovchinnikova, T.V. Analysis of Synergistic Effects of Antimicrobial Peptide Arenicin-1 and Conventional Antibiotics. Bull. Exp. Biol. Med. 2017, 162, 765–768. [Google Scholar] [CrossRef]
- Choi, H.; Lee, D.G. Synergistic Effect of Antimicrobial Peptide Arenicin-1 in Combination with Antibiotics against Pathogenic Bacteria. Res. Microbiol. 2012, 163, 479–486. [Google Scholar] [CrossRef]
- Shi, W.; Chen, F.; Zou, X.; Jiao, S.; Wang, S.; Hu, Y.; Lan, L.; Tang, F.; Huang, W. Design, Synthesis, and Antibacterial Evaluation of Vancomycin-LPS Binding Peptide Conjugates. Bioorganic Med. Chem. Lett. 2021, 45, 128122. [Google Scholar] [CrossRef]
- Chu, H.; Pazgier, M.; Jung, G.; Nuccio, S.-P.; Castillo, P.A.; De Jong, M.F.; Winter, M.G.; Winter, S.E.; Wehkamp, J.; Shen, B.; et al. Human α-Defensin 6 Promotes Mucosal Innate Immunity Through Self-Assembled Peptide Nanonets. Science 2012, 337, 477–481. [Google Scholar] [CrossRef]
- González, R.; Brokordt, K.; Cárcamo, C.B.; Coba De La Peña, T.; Oyanedel, D.; Mercado, L.; Schmitt, P. Molecular Characterization and Protein Localization of the Antimicrobial Peptide Big Defensin from the Scallop Argopecten purpuratus after Vibrio splendidus Challenge. Fish Shellfish Immunol. 2017, 68, 173–179. [Google Scholar] [CrossRef]
- Luo, G.; Sun, Y.; Zhang, J.; Xu, Z.; Lu, W.; Wang, H.; Zhang, Y.; Li, H.; Mao, Z.; Ye, S.; et al. Nanodefensin-Encased Hydrogel with Dual Bactericidal and pro-Regenerative Functions for Advanced Wound Therapy. Theranostics 2021, 11, 3642–3660. [Google Scholar] [CrossRef]
- Ribeiro, K.L.; Frías, I.A.M.; Franco, O.L.; Dias, S.C.; Sousa-Junior, A.A.; Silva, O.N.; Bakuzis, A.F.; Oliveira, M.D.L.; Andrade, C.A.S. Clavanin A-Bioconjugated Fe 3 O 4/Silane Core-Shell Nanoparticles for Thermal Ablation of Bacterial Biofilms. Colloids Surf. B Biointerfaces 2018, 169, 72–81. [Google Scholar] [CrossRef]
- Mygind, P.H.; Fischer, R.L.; Schnorr, K.M.; Hansen, M.T.; Sönksen, C.P.; Ludvigsen, S.; Raventós, D.; Buskov, S.; Christensen, B.; De Maria, L.; et al. Plectasin Is a Peptide Antibiotic with Therapeutic Potential from a Saprophytic Fungus. Nature 2005, 437, 975–980. [Google Scholar] [CrossRef]
- Ahmed, I.; Asgher, M.; Sher, F.; Hussain, S.; Nazish, N.; Joshi, N.; Sharma, A.; Parra-Saldívar, R.; Bilal, M.; Iqbal, H. Exploring Marine as a Rich Source of Bioactive Peptides: Challenges and Opportunities from Marine Pharmacology. Mar. Drugs 2022, 20, 208. [Google Scholar] [CrossRef]
- Papon, N.; Copp, B.R.; Courdavault, V. Marine Drugs: Biology, Pipelines, Current and Future Prospects for Production. Biotechnol. Adv. 2022, 54, 107871. [Google Scholar] [CrossRef]
- Zhang, B.; Zhao, M.; Tian, J.; Lei, L.; Huang, R. Novel Antimicrobial Agents Targeting the Streptococcus mutans Biofilms Discovery through Computer Technology. Front. Cell. Infect. Microbiol. 2022, 12, 1065235. [Google Scholar] [CrossRef]
- Torres, M.D.T.; De La Fuente-Nunez, C. Toward Computer-Made Artificial Antibiotics. Curr. Opin. Microbiol. 2019, 51, 30–38. [Google Scholar] [CrossRef]
- Zhang, Q.-T.; Liu, Z.-D.; Wang, Z.; Wang, T.; Wang, N.; Wang, N.; Zhang, B.; Zhao, Y.-F. Recent Advances in Small Peptides of Marine Origin in Cancer Therapy. Mar. Drugs 2021, 19, 115. [Google Scholar] [CrossRef]
- Ucak, I.; Afreen, M.; Montesano, D.; Carrillo, C.; Tomasevic, I.; Simal-Gandara, J.; Barba, F.J. Functional and Bioactive Properties of Peptides Derived from Marine Side Streams. Mar. Drugs 2021, 19, 71. [Google Scholar] [CrossRef]
- Cappello, E.; Nieri, P. From Life in the Sea to the Clinic: The Marine Drugs Approved and under Clinical Trial. Life 2021, 11, 1390. [Google Scholar] [CrossRef]
- Ghareeb, M.A.; Tammam, M.A.; El-Demerdash, A.; Atanasov, A.G. Insights about Clinically Approved and Preclinically Investigated Marine Natural Products. Curr. Res. Biotechnol. 2020, 2, 88–102. [Google Scholar] [CrossRef]
- Alves, C.; Silva, J.; Pinteus, S.; Gaspar, H.; Alpoim, M.C.; Botana, L.M.; Pedrosa, R. From Marine Origin to Therapeutics: The Antitumor Potential of Marine Algae-Derived Compounds. Front. Pharmacol. 2018, 9, 777. [Google Scholar] [CrossRef]
- Anjum, K.; Abbas, S.Q.; Akhter, N.; Shagufta, B.I.; Shah, S.A.A.; Hassan, S.S.U. Emerging Biopharmaceuticals from Bioactive Peptides Derived from Marine Organisms. Chem. Biol. Drug Des. 2017, 90, 12–30. [Google Scholar] [CrossRef]
- Cheung, R.; Ng, T.; Wong, J. Marine Peptides: Bioactivities and Applications. Mar. Drugs 2015, 13, 4006–4043. [Google Scholar] [CrossRef]
- Martins, A.; Vieira, H.; Gaspar, H.; Santos, S. Marketed Marine Natural Products in the Pharmaceutical and Cosmeceutical Industries: Tips for Success. Mar. Drugs 2014, 12, 1066–1101. [Google Scholar] [CrossRef]

| Compound | Source | Mechanism of Action | Antibacterial Activity | References |
|---|---|---|---|---|
| Pleurocidin | Winter flounder (Pleuronectes americanus) | Membrane disruption, alteration of bacterial metabolic pathways and interference with quorum sensing | Active against multi-drug-resistant Enterococcus faecium, Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter baumannii (MIC values of 8–256 μg/mL) | [42,43,44,45,46,47] |
| Clavanins | Leathery sea squirt (Styelaclava) | When paired with Zn2+ ions there is an increased positive charge and membrane affinity, and therefore in membrane disruption ability | Active against MRSA ATCC 43300; MIC values of 16 μg/mL for clavanin C and 64 μg/mL for clavanin E | [48,49,50,51,52] |
| Clavanin D and Clavaspirin can translocate inside the cells without damaging the membrane suggesting that they can interfere with processes inside the bacterial cell | Active against multi-drug-resistant Enterobacter cloacae when clavanin D is paired with clavaspirin | |||
| Epinecidin-1 | Grouper (Epinephelus coioides) | Membrane disruption and immunomodulation | Active against MRSA in mouse and pig models, Helicobacter pylori, and P. aeruginosa | [53,54,55,56,57] |
| Tilapia piscidin-3 | Nile tilapia (Oreochromis niloticus) | Membrane disruption | Active against MRSA in mouse peritonitis models (≤40 μg/mL) | [58,59,60] |
| Tilapia piscidin-4 | Nile tilapia (Oreochromis niloticus) | Membrane disruption and immunomodulation | Active against MRSA, carbapenem-resistant A. baumannii and resistant K. pneumoniae in vitro and MRSA in wound and peritonitis models (≤6.25 μg/mL) | [58,60,61] |
| Strategy | Mode of Action | Examples | References |
|---|---|---|---|
| AMP-antibiotic conjugates | Combination of antibiotics with membrane-interfering AMPs | Colistin and Bacteriocin Ampicilin and Arenin-I Vancomycin and LPS binding peptides | [34] [17,102,103,104] [105] |
| Nanonetworks | Net-like meshwork of fibrils that entangled the bacteria | Human α-defensin 6 ApBD1 | [106] [107] |
| Nanoparticle-based drug delivery systems | Nanomaterials and hydrogels that can amplify the antibacterial spectrum and antimicrobial capacity of AMPs | Nanodefensin-encased hydrogel (NDEFgel) | [108,109] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magalhães, R.; Mil-Homens, D.; Cruz, S.; Oliveira, M. Marine Antimicrobial Peptides: Emerging Strategies Against Multidrug-Resistant and Biofilm-Forming Bacteria. Antibiotics 2025, 14, 808. https://doi.org/10.3390/antibiotics14080808
Magalhães R, Mil-Homens D, Cruz S, Oliveira M. Marine Antimicrobial Peptides: Emerging Strategies Against Multidrug-Resistant and Biofilm-Forming Bacteria. Antibiotics. 2025; 14(8):808. https://doi.org/10.3390/antibiotics14080808
Chicago/Turabian StyleMagalhães, Rita, Dalila Mil-Homens, Sónia Cruz, and Manuela Oliveira. 2025. "Marine Antimicrobial Peptides: Emerging Strategies Against Multidrug-Resistant and Biofilm-Forming Bacteria" Antibiotics 14, no. 8: 808. https://doi.org/10.3390/antibiotics14080808
APA StyleMagalhães, R., Mil-Homens, D., Cruz, S., & Oliveira, M. (2025). Marine Antimicrobial Peptides: Emerging Strategies Against Multidrug-Resistant and Biofilm-Forming Bacteria. Antibiotics, 14(8), 808. https://doi.org/10.3390/antibiotics14080808






