Performance of Early Sepsis Screening Tools for Timely Diagnosis and Antibiotic Stewardship in a Resource-Limited Thai Community Hospital
Abstract
1. Introduction
2. Results
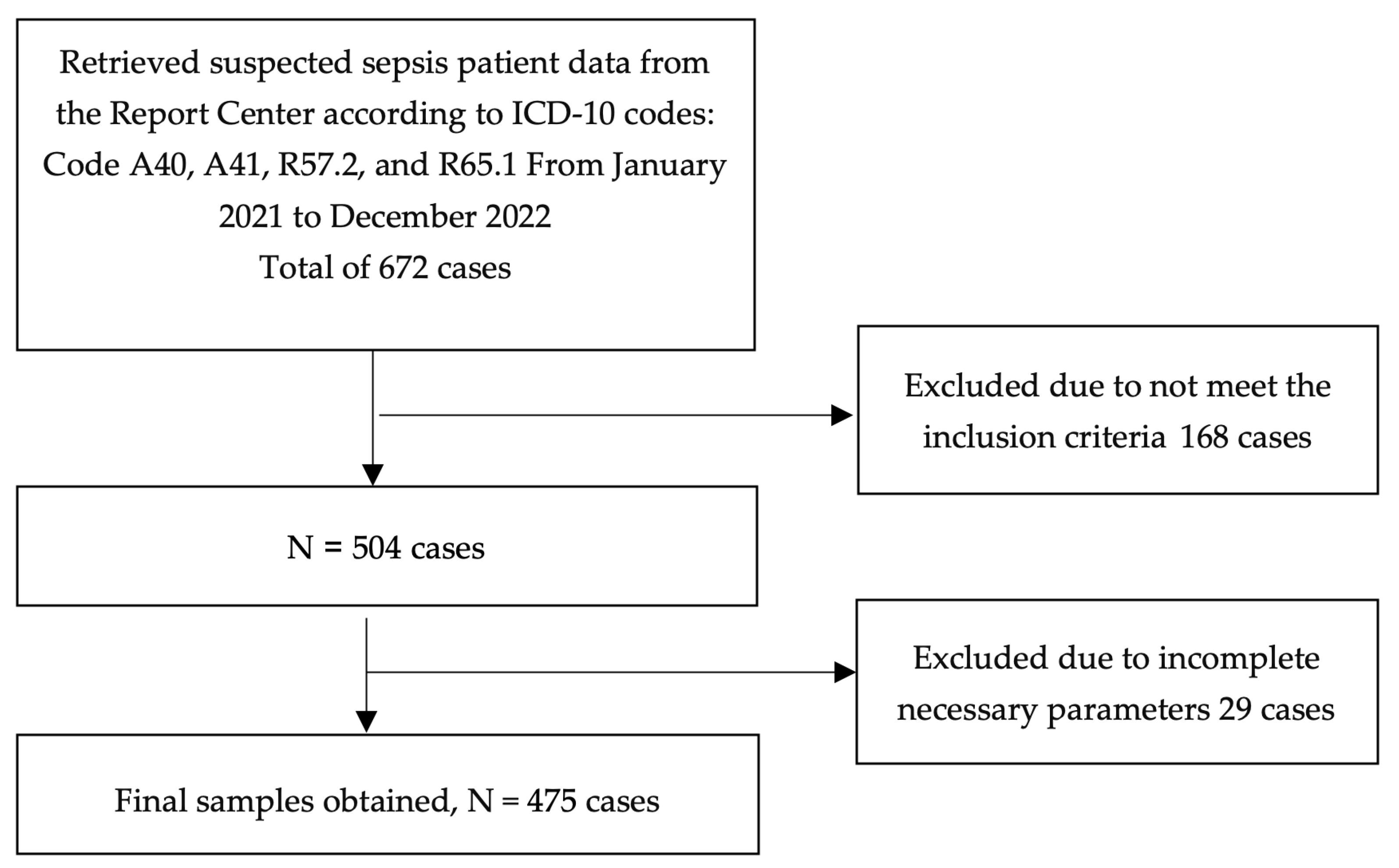
2.1. Patient Selection and Demographic Characteristics
2.2. Diagnostic Accuracy of Early Warning Scores
2.3. Summary of Findings
3. Discussion
3.1. Rationale for Two-Step Screening Approach: SIRS Followed by NEWS2
3.2. Strengths, Limitations, and Practical Considerations
4. Materials and Methods
4.1. Study Design and Setting
4.2. Population and Sampling
4.3. Data Collection and Instruments
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACVPU | alert, confusion, voice, pain, unresponsive |
| AMR | antimicrobial resistance |
| AUROC | area under receiver operating characteristic |
| AVPU | alert, voice, pain, unresponsive |
| COPD | chronic obstructive pulmonary disease |
| CI | confidence interval |
| ED | emergency department |
| EMT | emergency medical technician |
| HR | heart rate |
| ICD-10 | International Classification of Diseases, Tenth Revision |
| LMICs | low- and middle-income countries |
| LR+ | positive likelihood ratio |
| LR− | negative likelihood ratio |
| LRS | low-resource settings |
| MEWS | Modified Early Warning Score |
| NEWS | National Early Warning Score |
| NEWS2 | National Early Warning Score version 2 |
| NPV | negative predictive value |
| O2 | oxygen |
| PPV | positive predictive value |
| qSOFA | Quick Sequential Organ Failure Assessment |
| RR | respiratory rate |
| ROC | receiver operating characteristic |
| SBP | systolic blood pressure |
| SIRS | Systemic Inflammatory Response Syndrome |
| SpO2 | peripheral oxygen saturation |
| SOS | Search Out Severity |
| UTI | urinary tract infection |
References
- La Via, L.; Sangiorgio, G.; Stefani, S.; Marino, A.; Nunnari, G.; Cocuzza, S.; La Mantia, I.; Cacopardo, B.; Stracquadanio, S.; Spampinato, S.; et al. The global burden of sepsis and septic shock. Epidemiologia 2024, 5, 456–478. [Google Scholar] [CrossRef] [PubMed]
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Sepsis; World Health Organization: Geneva, Switzerland, 2023.
- Ministry of Public Health. KPI of Ministry of Public Health 2023; Nonthaburi (Thailand) Ministry of Public Health: Nonthaburi, Thailand, 2023. [Google Scholar]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef]
- Levy, M.M.; Evans, L.E.; Rhodes, A. The surviving sepsis campaign bundle: 2018 Update. Crit. Care Med. 2018, 46, 997–1000. [Google Scholar] [CrossRef]
- Champunot, R.; Permpikul, C.; Pajanasoontorn, B. (Eds.) Clinical Practice Guidelines for the Management of Patients with Severe Sepsis and Septic Shock (Draft). 2015. Available online: https://externinternguide.wordpress.com/wp-content/uploads/2017/12/52-septic-shock-draft-2015exin.pdf (accessed on 1 June 2025).
- Thwaites, L.; Nasa, P.; Abbenbroek, B.; Dat, V.Q.; Finfer, S.; Kwizera, A.; Ling, L.; Lobo, S.M.; Sinto, R.; Aditianingsih, D.; et al. Management of adult sepsis in resource-limited settings: Global expert consensus statements using a Delphi method. Intensive Care Med. 2024, 51, 21–38. [Google Scholar] [CrossRef]
- Pairattanakorn, P.; Angkasekwinai, N.; Sirijatuphat, R.; Wangchinda, W.; Tancharoen, L.; Thamlikitkul, V. Diagnostic and prognostic utility compared among different sepsis scoring systems in adult patients with sepsis in Thailand: A prospective cohort study. Open Forum Infect. Dis. 2020, 8, ofaa573. [Google Scholar] [CrossRef]
- Royal College of Physicians. National Early Warning Score 2 (NEWS2): Standardizing the Assessment of Acute Illness Severity in the NHS; Royal College of Physicians: London, UK, 2017. [Google Scholar]
- Royal College of Physicians. National Early Warning Score (NEWS): Standardizing the Assessment of Acute Illness Severity in the NHS; Royal College of Physicians: London, UK, 2012. [Google Scholar]
- Levy, M.M.; Fink, M.P.; Marshall, J.C.; Abraham, E.; Angus, D.; Cook, D.; Cohen, J.; Opal, S.M.; Vincent, J.-L.; Ramsay, G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit. Care Med. 2003, 31, 1250–1256. [Google Scholar] [CrossRef]
- Lam, T.; Mak, P.; Siu, W.; Lam, M.; Cheung, T.; Rainer, T. Validation of a Modified Early Warning Score (Mews) in Emergency Department Observation Ward Patients. Hong Kong J. Emerg. Med. 2006, 13, 24–30. [Google Scholar] [CrossRef]
- Chuworachet, N. Diagnostic performance of qSOFA score and SOS score for sepsis in Udon Thani Hospital. Mahasarakham Hosp. J. 2022, 19, 67–75. Available online: https://he02.tci-thaijo.org/index.php/MKHJ/article/view/259013/177846 (accessed on 1 June 2025). (In Thai).
- Thuakta, P. Compared SIRS, qSOFA and NEWS as screening tools for diagnosis sepsis in emergency department. Chiangrai Med. J. 2022, 14, 45–55. Available online: https://he01.tci-thaijo.org/index.php/crmjournal/article/view/252885/174406 (accessed on 1 June 2025). (In Thai).
- Svendsen, M.; Steindal, S.A.; Larsen, M.H.; Solberg, M.T. Comparison of the systematic Inflammatory response syndrome and the quick sequential organ failure assessment for prognostic accuracy in detecting sepsis in the emergency department: A systematic review. Int. Emerg. Nurs. 2023, 66, 101242. [Google Scholar] [CrossRef] [PubMed]
- Chua, W.L.; Bin Rusli, K.D.; Aitken, L.M. Early warning scores for sepsis identification and prediction of in-hospital mortality in adults with sepsis: A systematic review and meta-analysis. J. Clin. Nurs. 2024, 33, 2005–2018. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.; Reddy, H.; Gemnani, R.; Kumar, S.; Acharya, S. Navigating the Complexity of Scoring Systems in Sepsis Management: A Comprehensive Review. Cureus 2024, 16, e54030. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Finkelsztein, E.J.; Jones, D.S.; Ma, K.C.; Pabón, M.A.; Delgado, T.; Nakahira, K.; Arbo, J.E.; Berlin, D.A.; Schenck, E.J.; Choi, A.M.K.; et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit. Care 2017, 21, 73. [Google Scholar] [CrossRef]
- Elie-Turenne, M.-C.; Seethala, R.R.; Aisiku, I.P.; Bihorac, A.; Ozrazgat-Baslanti, T.; Mark, K.; George, N.R.; Allen, B.R.; Bozorgmehri, S.; Meurer, D.; et al. A large multicenter evaluation of quick Sequential Organ Failure Assessment (qSOFA) and Systemic Inflammatory Response Syndrome (SIRS) performance among hospitalized US Emergency Department patients with suspected infection. J. Emerg. Crit. Care Med. 2021, 5, 32. [Google Scholar] [CrossRef]
- Wallgren, U.M.; Sjölin, J.; Järnbert-Pettersson, H.; Kurland, L. Performance of NEWS2, RETTS, clinical judgment and the Predict Sepsis screening tools with respect to identification of sepsis among ambulance patients with suspected infection: A prospective cohort study. Scand. J. Trauma, Resusc. Emerg. Med. 2021, 29, 144. [Google Scholar] [CrossRef]
- Wongtida, C. Efficiency of National Early Warning Score (NEWS) for early detection of sepsis in a community hospital. J. Prim. Care Fam. Med. 2020, 3, 39–50. (In Thai) [Google Scholar]
- Wattanasit, P.; Khwannimit, B. Comparison the accuracy of early warning scores with qSOFA and SIRS for predicting sepsis in the emergency department. Am. J. Emerg. Med. 2021, 46, 284–288. [Google Scholar] [CrossRef]
- Jaruwatthanasunthon, J.; Worapratya, P.; Piyasuwankul, T. Comparison accuracy in mSIRS, NEWS and qSOFA score to triage sepsis patients in the emergency department at a hospital in Thailand. J. Health Sci. Med. Res. 2022, 40, 377–388. (In Thai) [Google Scholar] [CrossRef]
- Suttapanit, K.; Satiracharoenkul, S.; Sanguanwit, P.; Prachanukool, T. The Accuracy of Sepsis Screening Score for Mortality Prediction at Emergency Department Triage. West. J. Emerg. Med. 2022, 23, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Thodphetch, M.; Chenthanakij, B.; Wittayachamnankul, B.; Sruamsiri, K.; Tangsuwanaruk, T. A comparison of scoring systems for predicting mortality and sepsis in the emergency department patients with a suspected infection. Clin. Exp. Emerg. Med. 2021, 8, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Lo, R.S.L.; Lyngholm, L.E.; Brabrand, M.; Leung, L.Y.; Hung, K.K.C.; Laugesen, S.; Posth, S.; Cooksley, T.; A Graham, C.; Nickel, C.H. A tale of two continents: The performance of six early warning scores in two emergency departments. Hong Kong J. Emerg. Med. 2023, 30, 374–380. [Google Scholar] [CrossRef]
- Piedmont, S.; Goldhahn, L.; Swart, E.; Robra, B.-P.; Fleischmann-Struzek, C.; Somasundaram, R.; Bauer, W. Sepsis incidence, suspicion, prediction and mortality in emergency medical services: A cohort study related to the current international sepsis guideline. Infection 2024, 52, 1325–1335. [Google Scholar] [CrossRef]
- Iyer, V.; Castro, D.; Malla, B.; Panda, B.; Rabson, A.R.; Horowitz, G.; Heger, N.; Gupta, K.; Singer, A.; Norwitz, E.R. Culture-independent identification of bloodstream infections from whole blood: Prospective evaluation in specimens of known infection status. J. Clin. Microbiol. 2024, 62, e0149823. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensiv. Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- McCaffery, M.; Onikoyi, O.; Rodrigopulle, D.; Syed, A.; Jones, S.; Mansfield, L.; Krishna, M.G. Sepsis-review of screening for sepsis by nursing, nurse driven sepsis protocols and development of sepsis hospital policy/protocols. Nurs. Palliat. Care 2016, 1, 33–37. [Google Scholar] [CrossRef]
- Duncan, C.F.; Youngstein, T.; Kirrane, M.D.; Lonsdale, D.O. Diagnostic challenges in sepsis. Curr. Infect. Dis. Rep. 2021, 23, 22. [Google Scholar] [CrossRef]
- Gul, F.; Arslantas, M.K.; Cinel, I.; Kumar, A. Changing definitions of sepsis. Turk. J. Anesth. Reanim. 2017, 45, 129–138. [Google Scholar] [CrossRef]
- Diao, S.-T.; Dong, R.; Peng, J.-M.; Chen, Y.; Li, S.; He, S.-H.; Wang, Y.-F.; Du, B.; Weng, L. Validation of an ICD-based algorithm to identify sepsis: A retrospective study. Risk Manag. Healthc. Policy 2023, 16, 2249–2257. [Google Scholar] [CrossRef]
- Stephen, A.H.; Montoya, R.L.; Aluisio, A.R. Sepsis and septic shock in low- and middle-income countries. Surg. Infect. 2020, 21, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Usman, O.A.; Usman, A.A.; Ward, M.A. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am. J. Emerg. Med. 2019, 37, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Tusgul, S.; Carron, P.-N.; Yersin, B.; Calandra, T.; Dami, F. Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage. Scand. J. Trauma, Resusc. Emerg. Med. 2017, 25, 108. [Google Scholar] [CrossRef]
- Mellhammar, L.; Linder, A.; Tverring, J.; Christensson, B.; Boyd, J.H.; Sendi, P.; Åkesson, P.; Kahn, F. NEWS2 is superior to qSOFA in detecting Sepsis with Organ Dysfunction in the emergency department. J. Clin. Med. 2019, 8, 1128. [Google Scholar] [CrossRef]
- Brink, A.; Alsma, J.; Verdonschot, R.J.C.G.; Rood, P.P.M.; Zietse, R.; Lingsma, H.F.; Schuit, S.C.E.; Lopez-Delgado, J.C. Predicting mortality in patients with suspected sepsis at the Emergency Department; A retrospective cohort study comparing qSOFA, SIRS and National Early Warning Score. PLoS ONE 2019, 14, e0211133. [Google Scholar] [CrossRef]
- Kovacevic, P.; Jandric, M.; Kovacevic, T.; Momcicevic, D.; Zlojutro, B.; Baric, G.; Dragic, S. Impact of Checklist for Early Recognition and Treatment of Acute Illness on Treatment of Critically Ill Septic Patients in a Low-Resource Medical Intensive Care Unit. Microb. Drug Resist. 2021, 27, 1203–1206. [Google Scholar] [CrossRef]
- Inada-Kim, M. NEWS2 and improving outcomes from sepsis. Clin. Med. 2022, 22, 514–517. [Google Scholar] [CrossRef]
- Baker, K.F.; Hanrath, A.T.; van der Loeff, I.S.; Kay, L.J.; Back, J.; Duncan, C.J. National Early Warning Score 2 (NEWS2) to identify inpatient COVID-19 deterioration: A retrospective analysis. Clin. Med. 2021, 21, 84–89. [Google Scholar] [CrossRef]
- Tajarernmuang, P.; Sanwirat, P.; Inchai, J.; Phinyo, P.; Limsukon, A. The National Early Warning Score 2(NEWS2) to predict early progression to severe community-acquired pneumonia. Trop. Med. Infect. Dis. 2023, 8, 68. [Google Scholar] [CrossRef]
- Trongtrakul, K.; Tajarernmuang, P.; Limsukon, A.; Theerakittikul, T.; Niyatiwatchanchai, N.; Surasit, K.; Glunriangsang, P.; Liwsrisakun, C.; Bumroongkit, C.; Pothirat, C.; et al. The National Early Warning Score 2 with age and body mass index (NEWS2 Plus) to determine patients with severe COVID-19 pneumonia. J. Clin. Med. 2024, 13, 298. [Google Scholar] [CrossRef]
- Hsieh, M.-S.; Chiu, K.-C.; Chattopadhyay, A.; Lu, T.-P.; Liao, S.-H.; Chang, C.-M.; Lee, Y.-C.; Lo, W.-E.; Hsieh, V.C.-R.; Hu, S.-Y.; et al. Utilizing the National Early Warning Score 2 (NEWS2) to confirm the impact of emergency department management in sepsis patients: A cohort study from taiwan 1998–2020. Int. J. Emerg. Med. 2024, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Suntornsut, P.; Asadinia, K.S.; Limato, R.; Tamara, A.; A Rotty, L.W.; Bramanti, R.; Nusantara, D.U.; Nelwan, E.J.; Khusuwan, S.; Suphamongkholchaikul, W.; et al. Barriers and enablers to blood culture sampling in Indonesia, Thailand and Viet Nam: A Theoretical Domains Framework-based survey. BMJ Open 2024, 14, e075526. [Google Scholar] [CrossRef] [PubMed]
- Hantrakun, V.; Somayaji, R.; Teparrukkul, P.; Boonsri, C.; Rudd, K.; Day, N.P.J.; West, T.E.; Limmathurotsakul, D.; Mayr, F. Clinical epidemiology and outcomes of community acquired infection and sepsis among hospitalized patients in a resource limited setting in Northeast Thailand: A prospective observational study (Ubon-sepsis). PLoS ONE 2018, 13, e0204509. [Google Scholar] [CrossRef]
- Li, F.; Wang, S.; Gao, Z.; Qing, M.; Pan, S.; Liu, Y.; Hu, C. Harnessing artificial intelligence in sepsis care: Advances in early detection, personalized treatment, and real-time monitoring. Front. Med. 2025, 11, 1510792. [Google Scholar] [CrossRef]

| Criteria | NEWS | NEWS2 | qSOFA | SIRS | MEWS | SOS |
|---|---|---|---|---|---|---|
| Parameters | RR, O2 saturation and supplement SBP, HR, Level of consciousness, (AVPU) Temperature, | RR, O2 saturation and supplement SBP, HR, Level of consciousness, (ACVPU) Temperature | RR, SBP, Altered mental status | RR, HR, Temperature, WBC count | RR, SBP, HR, Level of consciousness (AVPU), Temperature, | RR, SBP, HR, Level of consciousness (ACVPU), Temperature, Urine output |
| Score Range | 0–20 | 0–20 | 0–3 | ≥2 out of 4 | 0–14 | 0–16 |
| Thresholds | ≥5 | ≥5 | ≥2 out of 3 | ≥2 out of 4 | ≥4 | ≥4 Varies by institution |
| Pros | Incorporates oxygen use, validated for diverse settings | Widely used, straightforward, SpO2 Scale 2 for COPD | Easy to calculate, identify sepsis risk for pre-hospital setting | Long-standing use, well understood | Simple, widely used | Specific to sepsis-related organ failure |
| Cons | More complex than qSOFA or SIRS | More complex than qSOFA or SIRS | Less sensitive than SIRS | Can be non-specific, many false positives | May not be specific to sepsis | More complex than qSOFA and SIRS |
| Advantages over Others | Includes oxygen saturation adjustments | Established benchmarks, broad applicability | Rapid, quick assessment | Captures early signs of systemic response | Early identification of deterioration | Focused on sepsis-related organ dysfunction |
| Characteristic | Number of Patients | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 246 | 51.79 |
| Female | 229 | 48.21 |
| End of Treatment | ||
| Alive | 456 | 96.00 |
| Dead | 19 | 4.00 |
| Age (years) | ||
| 18–30 | 17 | 3.58 |
| 31–45 | 56 | 11.79 |
| 46–60 | 86 | 18.10 |
| 61–75 | 174 | 36.63 |
| >75 | 142 | 29.90 |
| Comorbidity Diseases | ||
| No | 95 | 20.00 |
| Yes | 380 | 80.00 |
| 1 comorbidity | 99 | 20.84 |
| 2 comorbidities | 106 | 22.32 |
| 3 comorbidities | 94 | 19.79 |
| 4 comorbidities | 58 | 12.21 |
| 5 comorbidities | 18 | 3.79 |
| 6 comorbidities | 5 | 1.05 |
| Chronic Diseases | ||
| Hypertension | 237 | 49.89 |
| Dyslipidemia | 182 | 38.32 |
| Diabetes mellitus | 122 | 25.68 |
| Heart disease | 62 | 13.05 |
| Chronic kidney disease | 50 | 10.53 |
| Gout | 45 | 9.47 |
| Chronic obstructive pulmonary disease/ | 43 | 9.05 |
| Asthma | ||
| Benign prostatic hyperplasia | 39 | 8.21 |
| Cerebrovascular disease | 33 | 6.95 |
| Liver disease | 26 | 5.47 |
| Cancer | 26 | 5.47 |
| Tuberculosis | 20 | 4.21 |
| Human Immunodeficiency Virus | 14 | 2.95 |
| Epilepsy | 10 | 2.11 |
| Anemia | 8 | 1.68 |
| Others | 31 | 6.53 |
| Diagnosis | ||
| Sepsis | 242 | 50.95 |
| Pneumonia | 77 | 16.21 |
| UTI | 44 | 9.26 |
| Cellulitis | 27 | 5.68 |
| Fever unspecified | 19 | 4.00 |
| Infection diarrhea | 17 | 3.58 |
| Bronchitis | 8 | 1.69 |
| Cutaneous abscess | 8 | 1.69 |
| Dengue | 7 | 1.47 |
| Bacterial infection | 6 | 1.26 |
| Others | 20 | 4.21 |
| Blood Culture Results | ||
| Positive | 123 | 25.89 |
| Negative or no growth | 352 | 74.11 |
| Type of Bacteria from Hemoculture (n = 102) * | ||
| Escherichia coli | 47 | 46.08 |
| Staphylococcus aureus | 10 | 9.80 |
| Klebsiella pneumoniae | 8 | 7.85 |
| Streptococcus group A | 8 | 7.85 |
| Streptococcus viridans group | 7 | 6.86 |
| Burkhoderia pseudomallei | 3 | 2.94 |
| Aeromonas caviae | 2 | 1.96 |
| Kocuria marina | 2 | 1.96 |
| Staphylococcus saprophyticus | 2 | 1.96 |
| Streptococcus pneumoniae | 2 | 1.96 |
| Streptococcus group D | 2 | 1.96 |
| Enterobacter cloacae | 1 | 0.98 |
| Morganella morganii (CRE) | 1 | 0.98 |
| Paenibacillus spp. | 1 | 0.98 |
| Proteus mirabilis | 1 | 0.98 |
| Pseudomonas aeruginosa | 1 | 0.98 |
| Salmonella spp. | 1 | 0.98 |
| Streptococcus mutans | 1 | 0.98 |
| Streptococcus suis | 1 | 0.98 |
| Streptococus group B | 1 | 0.98 |
| Sepsis Screening Tools | %Sensitivity (95%CI) | %Specificity (95%CI) | %Positive Predictive Value (95%CI) | %Negative Predictive Value (95%CI) | Positive Likelihood Ratio | Negative Likelihood Ratio | Area Under ROC Curve (95%CI) |
|---|---|---|---|---|---|---|---|
| SIRS | 84 (80–89) | 25 (20–31) | 54 (49–59) | 61 (51–71) | 1.12 | 0.64 | 0.578 (0.527–0.630) |
| qSOFA | 16 (11–20) | 91 (88–95) | 66 (53–78) | 51 (46–56) | 1.78 | 0.92 | 0.577 (0.525–0.628) |
| MEWS | 69 (63–75) | 48 (42–55) | 58 (52–64) | 60 (53–67) | 1.33 | 0.65 | 0.623 (0.573–0.673) |
| NEWS2 | 68 (62–74) | 52 (62–74) | 60 (54–65) | 61 (54–68) | 1.42 | 0.62 | 0.625 (0.575–0.675) |
| NEWS | 67 (61–73) | 53 (46–59) | 59 (54–65) | 60 (54–67) | 1.43 | 0.62 | 0.624 (0.574–0.674) |
| SOS | 51 (45–58) | 67 (61–73) | 62 (55–68) | 57 (51–63) | 1.55 | 0.73 | 0.619 (0.569–0.670) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wanlumkhao, W.; Rattanamongkolgul, D.; Ekpanyaskul, C. Performance of Early Sepsis Screening Tools for Timely Diagnosis and Antibiotic Stewardship in a Resource-Limited Thai Community Hospital. Antibiotics 2025, 14, 708. https://doi.org/10.3390/antibiotics14070708
Wanlumkhao W, Rattanamongkolgul D, Ekpanyaskul C. Performance of Early Sepsis Screening Tools for Timely Diagnosis and Antibiotic Stewardship in a Resource-Limited Thai Community Hospital. Antibiotics. 2025; 14(7):708. https://doi.org/10.3390/antibiotics14070708
Chicago/Turabian StyleWanlumkhao, Wisanu, Duangduan Rattanamongkolgul, and Chatchai Ekpanyaskul. 2025. "Performance of Early Sepsis Screening Tools for Timely Diagnosis and Antibiotic Stewardship in a Resource-Limited Thai Community Hospital" Antibiotics 14, no. 7: 708. https://doi.org/10.3390/antibiotics14070708
APA StyleWanlumkhao, W., Rattanamongkolgul, D., & Ekpanyaskul, C. (2025). Performance of Early Sepsis Screening Tools for Timely Diagnosis and Antibiotic Stewardship in a Resource-Limited Thai Community Hospital. Antibiotics, 14(7), 708. https://doi.org/10.3390/antibiotics14070708






