The Burden of Hospitalization and Rehospitalization Among Patients Hospitalized with Severe Community-Acquired Bacterial Pneumonia in the United States, 2018–2022
Abstract
1. Introduction
2. Results
3. Discussion
4. Methods
4.1. Ethics Statement
4.2. Study Design and Patient Population
4.3. Data Source and Time Frame
4.4. Baseline Measures
4.5. Outcome Variables
4.6. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAP | Community-acquired pneumonia |
| HAC | Hospital-acquired complication |
| CDI | Clostridioides difficile infection |
| CMS | Centers for Medicare and Medicaid Services |
| sCAP | Severe community-acquired pneumonia |
| HRU | Hospital resource utilization |
| CABP | Bacterial community-acquired pneumonia |
| sCABP | Severe bacterial community-acquired pneumonia |
| ICD-10 | International Classification of Diseases-10 |
| ICU | Intensive care unit |
| CDM | Charge Data Master |
| LOS | Length of stay |
| AHRQ | Agency for Healthcare Research and Quality |
| SD | Standard deviation |
References
- Musher, D.M.; Thorner, A.R. Community-acquired pneumonia. N. Engl. J. Med. 2014, 371, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Rozenbaum, M.H.; Mangen, M.J.; Huijts, S.M.; van der Werf, T.S.; Postma, M.J. Incidence, direct costs and duration of hospitalization of patients hospitalized with community acquired pneumonia: A nationwide retrospective claims database analysis. Vaccine 2015, 33, 3193–3199. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, J.A.; Wiemken, T.L.; Peyrani, P.; Arnold, F.W.; Kelley, R.; Mattingly, W.A.; Nakamatsu, R.; Pena, S.; Guinn, B.E.; Furmanek, S.P.; et al. Adults hospitalized with pneumonia in the United States: Incidence, epidemiology, and mortality. Clin. Infect. Dis. 2017, 65, 1806–1812. [Google Scholar] [CrossRef] [PubMed]
- Hayes, B.H.; Haberling, D.L.; Kennedy, J.L.; Varma, J.K.; Fry, A.M.; Vora, N.M. Burden of pneumonia-associated hospitalizations: United States, 2001–2014. Chest 2018, 153, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, M.; et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, J.D.; Akram, A.R.; Singanayagam, A.; Wilcox, M.H.; Hill, A.T. Risk factors for Clostridium difficile infection in hospitalized patients with community-acquired pneumonia. J. Infect. 2016, 73, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Deshpande, A.; Yu, P.C.; Imrey, P.B.; Lindenauer, P.K.; Zilberberg, M.D.; Haessler, S.; Rothberg, M.B. Association of fluoroquinolones or cephalosporin plus macrolide with Clostridioides difficile infection (CDI) after treatment for community-acquired pneumonia. Infect. Control Hosp. Epidemiol. 2023, 44, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Hospital-Acquired Condition Reduction Program. Centers for Medicare and Medicaid Services. Available online: https://www.cms.gov/medicare/quality/value-based-programs/hospital-acquired-conditions (accessed on 15 April 2025).
- Weiss, A.J.; Jiang, H.J. Overview of Clinical Conditions with Frequent and Costly Hospital Readmissions by Payer, 2018. July 2021. Agency for Healthcare Research and Quality. Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb278-Conditions-Frequent-Readmissions-By-Payer-2018.pdf (accessed on 15 April 2025).
- Averin, A.; Shaff, M.; Weycker, D.; Lonshteyn, A.; Sato, R.; Pelton, S.I. Mortality and readmission in the year following hospitalization for pneumonia among US adults. Respir. Med. 2021, 185, 106476. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Eldridge, N.; Metersky, M.L.; Rodrick, D.; Faniel, C.; Eckenrode, S.; Mathew, J.; Galusha, D.H.; Tasimi, A.; Ho, S.-Y.; et al. Analysis of hospital-level readmission rates and variation in adverse events among patients with pneumonia in the United States. JAMA Netw. Open 2022, 5, e2214586. [Google Scholar] [CrossRef] [PubMed]
- Patient Protection and Affordable Care Act, HR 3590, 111th Congress (2010). PUB L No. 111–148. Available online: https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf (accessed on 15 April 2025).
- Zuckerman, R.B.; Sheingold, S.H.; Orav, E.J.; Ruhter, J.; Epstein, A.M. Readmissions, observation, and the hospital readmissions reduction program. N. Engl. J. Med. 2016, 374, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- Wasfy, J.H.; Zigler, C.M.; Choirat, C.; Wang, Y.; Dominici, F.; Yeh, R.W. Readmission rates after passage of the Hospital Readmissions Reduction Program: A pre-post analysis. Ann. Intern. Med. 2017, 166, 324–331. [Google Scholar] [CrossRef] [PubMed]
- McIlvennan, C.K.; Eapen, Z.J.; Allen, L.A. Hospital readmissions reduction program. Circulation 2015, 131, 1796–1803. [Google Scholar] [CrossRef] [PubMed]
- Cavallazzi, R.; Furmanek, S.; Arnold, F.W.; Beavin, L.A.; Wunderink, R.G.; Niederman, M.S.; Ramirez, J.A. The burden of community-acquired pneumonia requiring admission to ICU in the United States. Chest 2020, 158, 1008–1016. [Google Scholar] [CrossRef] [PubMed]
- Haessler, S.; Guo, N.; Deshpande, A.; Zilberberg, M.D.; Lagu, T.; Lindenauer, P.K.; Imrey, P.B.; Rothberg, M.B. Etiology, treatments, and outcomes of patients with severe community-acquired pneumonia in a large U.S. sample. Crit. Care Med. 2022, 50, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Klompas, M.; Yu, P.C.; Imrey, P.B.; Pallotta, A.M.; Higgins, T.; Haessler, S.; Zilberberg, M.D.; Lindenauer, P.K.; Rothberg, M.B. Influenza testing and treatment among patients hospitalized with community-acquired pneumonia. Chest 2022, 162, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Lopez, E.; Neuman, T.; Jacobson, G.; Levitt, L. How Much More Than Medicare Do Private Insurers Pay? A Review of the Literature. Kaiser Family Foundation, 15 April 2020. Available online: https://www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature/ (accessed on 15 April 2025).
- Malone, D.C.; Armstrong, E.P.; Gratie, D.; Pham, S.V.; Amin, A. A systematic review of real-world healthcare resource use and costs of Clostridioides difficile infections. Antimicrob. Steward. Healthc. Epidemiol. 2023, 3, e17. [Google Scholar] [CrossRef] [PubMed]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 2007, 44 (Suppl. S2), S27–S72. [Google Scholar] [CrossRef] [PubMed]
- Human Subject Regulations Decision Charts. US Department of Health and Human Services Office for Human Research Protections. Available online: https://www.hhs.gov/ohrp/regulations-and-policy/decision-charts/index.html (accessed on 15 April 2025).
- Available IQVIA Data. IQVIA. Available online: https://www.iqvia.com/insights/the-iqvia-institute/available-iqvia-data (accessed on 15 April 2025).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Cost-to-Charge (CCR) Files. Agency for Healthcare Research and Quality. Available online: https://hcup-us.ahrq.gov/db/ccr/costtocharge.jsp (accessed on 15 April 2025).
| Total N = 24,422 | ||
|---|---|---|
| Characteristic | n | % |
| Age (years) | ||
| Mean | 65.4 | NA |
| SD | 14.6 | NA |
| Median | 67 | NA |
| Age Group | ||
| 2–17 years | 0 | 0.00% |
| 18–34 years | 1104 | 4.52% |
| 35–44 years | 1301 | 5.33% |
| 45–54 years | 2381 | 9.75% |
| 55–64 years | 5370 | 21.99% |
| ≥65 years | 14,266 | 58.41% |
| Gender | ||
| Male | 13,486 | 55.22% |
| Female | 10,936 | 44.78% |
| Geographic region | ||
| Northeast | 2791 | 11.43% |
| Midwest | 1838 | 7.53% |
| South | 12,762 | 52.26% |
| West | 7031 | 28.79% |
| Payer | ||
| Cash | 74 | 0.30% |
| Medicaid | 1084 | 4.44% |
| Medicare Risk | 8600 | 35.21% |
| Third Party | 10,399 | 42.58% |
| Other/Unknown | 4265 | 17.46% |
| Year of the index hospitalization | ||
| 2018 | 5743 | 23.52% |
| 2019 | 6531 | 26.74% |
| 2020 | 7502 | 30.72% |
| 2021 | 4646 | 19.02% |
| Number of hospital beds | ||
| 1–99 beds | 2137 | 8.75% |
| 100–199 beds | 5218 | 21.37% |
| 200–299 beds | 4665 | 19.10% |
| 300–499 beds | 7140 | 29.24% |
| 500+ beds | 5255 | 21.52% |
| Unknown | 7 | 0.03% |
| Hospital urbanicity | ||
| Urban | 22,437 | 91.87% |
| Rural | 1985 | 8.13% |
| Hospital teaching status | ||
| Teaching | 6373 | 26.10% |
| Non-Teaching | 15,451 | 63.27% |
| Unknown | 2598 | 10.64% |
| Admitting source | ||
| Emergency department | 20,934 | 85.72% |
| Referral and transfer | 246 | 1.01% |
| Routine admission | 2590 | 10.61% |
| Other | 286 | 1.17% |
| Unspecified | 366 | 1.50% |
| Charlson Comorbidity Index (CCI) | ||
| 0 | 15,596 | 63.86% |
| 1 | 1816 | 7.44% |
| 2 | 1797 | 7.36% |
| 3+ | 5213 | 21.35% |
| Mean | 1.35 | NA |
| SD | 2.33 | NA |
| Median | 0 | NA |
| Total N = 24,422 | ||
|---|---|---|
| n | % | |
| Index treatment antimicrobial class (not mutually exclusive) | ||
| Aminoglycosides | 272 | 1.11% |
| Antifungals | 428 | 1.75% |
| Carbapenems | 1436 | 5.88% |
| Cephalosporins | 13,124 | 53.74% |
| Fluoroquinolones | 3695 | 15.13% |
| Folate pathway inhibitors | 3 | 0.01% |
| Glycopeptide | 10,520 | 43.08% |
| Macrolides | 7925 | 32.45% |
| Monobactams | 450 | 1.84% |
| Monoclonal antibodies | 0 | 0.00% |
| Other antibiotics | 1630 | 6.67% |
| Oxazolidinone | 354 | 1.45% |
| Penicillin | 161 | 0.66% |
| Penicillin with beta-lactamase inhibitors | 7919 | 32.43% |
| Polymyxins | 11 | 0.05% |
| Tetracyclines | 1014 | 4.15% |
| Treatment type (mutually exclusive) | ||
| Monotherapy | ||
| Aminoglycosides | 162 | 0.66% |
| Antifungals | 736 | 3.01% |
| Carbapenems | 2448 | 10.02% |
| Cephalosporins | 8841 | 36.20% |
| Fluoroquinolones | 3039 | 12.44% |
| Folate pathway inhibitors | 1 | 0.00% |
| Glycopeptides | 2512 | 10.29% |
| Macrolides | 1433 | 5.87% |
| Monobactams | 179 | 0.73% |
| Monoclonal antibodies | 0 | 0.00% |
| Other antibiotics | 893 | 3.66% |
| Oxazolidinones | 503 | 2.06% |
| Penicillin | 482 | 1.97% |
| Penicillin with beta-lactamase inhibitors | 6044 | 24.75% |
| Polymyxins | 39 | 0.16% |
| Tetracyclines | 811 | 3.32% |
| Combination therapy (Top 5 most frequent combinations) | ||
| Cephalosporins and macrolides | 5591 | 22.89% |
| Glycopeptides and penicillin with beta-lactamase inhibitors | 4742 | 19.42% |
| Cephalosporins and glycopeptides | 4360 | 17.85% |
| Cephalosporins, glycopeptides, and macrolides | 1794 | 7.35% |
| Cephalosporins with other antibiotics | 1596 | 6.54% |
| Total N = 24,422 | |||||
|---|---|---|---|---|---|
| n | % | Mean | SD | Median | |
| Index hospitalization outcomes | |||||
| Hospital mortality | 3881 | 15.89% | |||
| Clostridioides difficile infection | 271 | 1.19% | |||
| Total cost (USD) | |||||
| Hospital | USD 91,965 | USD 133,734 | USD 54,806 | ||
| ICU | USD 23,847 | USD 36,760 | USD 12,063 | ||
| LOS (days) | |||||
| Hospital | 13.6 | 12.1 | 10.0 | ||
| ICU | 8.7 | 9.6 | 6.0 | ||
| Daily cost (USD) | |||||
| Hospital | USD 6605 | USD 18,371 | USD 5412 | ||
| ICU | USD 2684 | USD 2247 | USD 2120 | ||
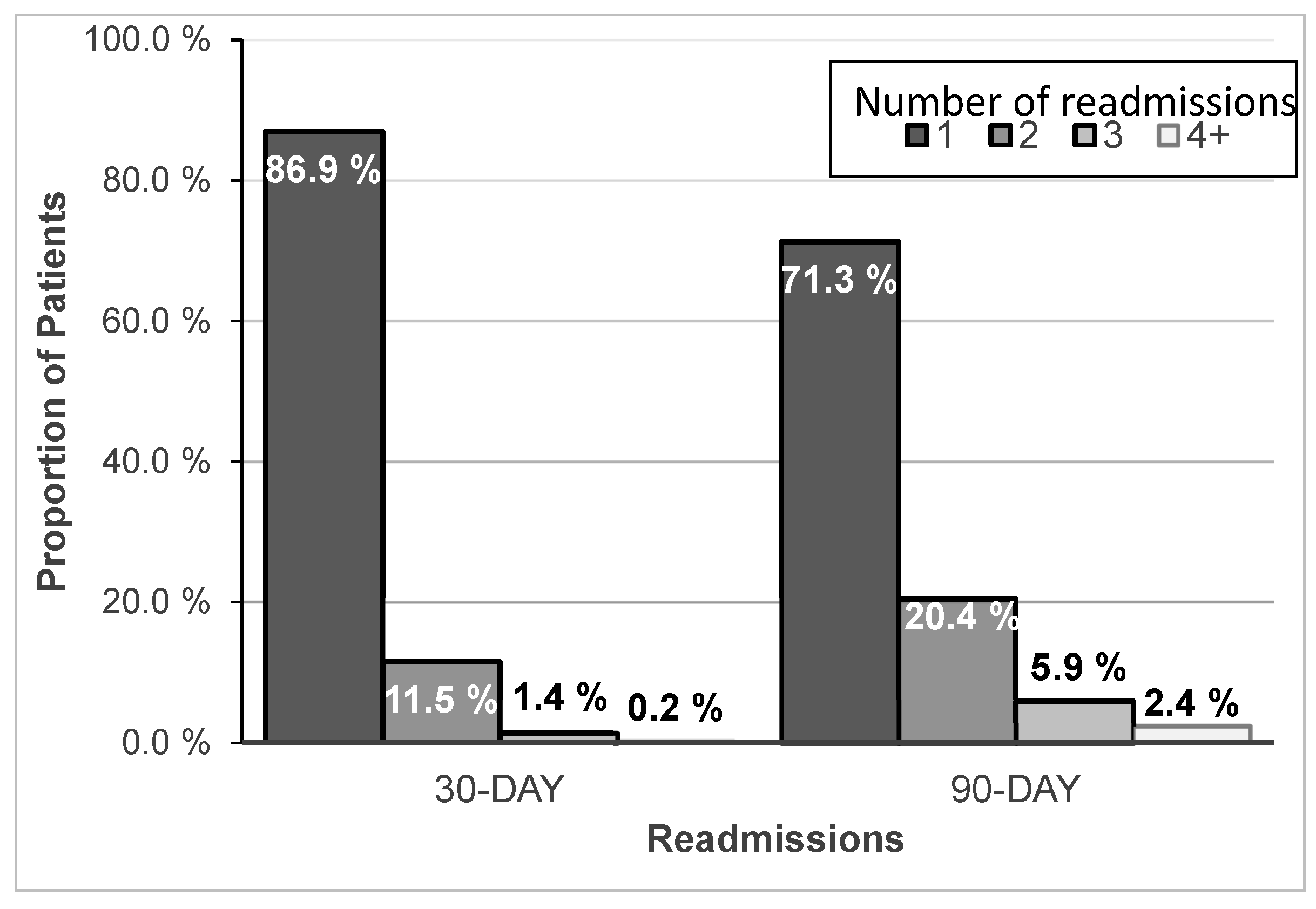
| Readmission outcomes | |||||
| 30-day readmission | |||||
| Incidence | 4082 | 19.87% | |||
| CABP admission diagnosis | 57 | 1.40% | |||
| Cost, first readmission (USD) | USD 50,667 | USD 83,279 | USD 26,112 | ||
| Length of stay, first readmission (days) | 10.03 | 10.88 | 7 | ||
| Cost, all readmissions (USD) | USD 61,072 | USD 102,604 | USD 30,851 | ||
| LOS, all readmissions (days) | 11.49 | 12.15 | 8 | ||
| 90-day readmission | |||||
| Incidence | 6148 | 29.93% | |||
| CABP admission diagnosis | 67 | 1.09% | |||
| Cost, first readmission (USD) | USD 48,927 | USD 77,243 | USD 25,932 | ||
| Length of stay, first readmission (days) | 9.49 | 10.16 | 7 | ||
| Cost, all readmissions (USD) | USD 72,117 | USD 113,421 | $35,447 | ||
| LOS, all readmissions (days) | 13.25 | 14.16 | 9 | ||
| 30-Day Readmissions | 90-Day Readmissions | |||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |||
| Lower Limit | Upper Limit | Lower Limit | Upper Limit | |||
| Age (reference: 18–34 years) | ||||||
| 35–44 years | 1.161 | 0.917 | 1.470 | 1.224 | 1.000 | 1.498 |
| 45–54 years | 1.430 | 1.161 | 1.760 | 1.472 | 1.231 | 1.760 |
| 55–64 years | 1.309 | 1.079 | 1.588 | 1.391 | 1.180 | 1.641 |
| ≥65 years | 1.362 | 1.132 | 1.637 | 1.431 | 1.223 | 1.675 |
| Female gender | 1.041 | 0.971 | 1.116 | 1.028 | 0.967 | 1.093 |
| Region (reference: Northeast) | ||||||
| Midwest | 1.073 | 0.918 | 1.254 | 1.007 | 0.875 | 1.159 |
| South | 0.825 | 0.739 | 0.922 | 0.840 | 0.762 | 0.926 |
| West | 0.823 | 0.731 | 0.927 | 0.865 | 0.779 | 0.960 |
| Admission year (reference: 2018) | ||||||
| 2019 | 0.981 | 0.891 | 1.081 | 0.958 | 0.880 | 1.042 |
| 2020 | 0.980 | 0.891 | 1.078 | 0.955 | 0.878 | 1.037 |
| 2021 | 0.984 | 0.883 | 1.095 | 0.928 | 0.845 | 1.020 |
| Diabetes mellitus | 1.447 | 1.315 | 1.593 | 1.533 | 1.407 | 1.671 |
| Chronic heart failure | 1.441 | 1.288 | 1.613 | 1.517 | 1.369 | 1.680 |
| Chronic obstructive pulmonary disease | 1.427 | 1.288 | 1.581 | 1.471 | 1.340 | 1.613 |
| ICU length of stay (per 1 day) | 1.013 | 1.009 | 1.016 | 1.009 | 1.006 | 1.012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zilberberg, M.D.; Greenberg, M.; Curt, V.; Shorr, A.F. The Burden of Hospitalization and Rehospitalization Among Patients Hospitalized with Severe Community-Acquired Bacterial Pneumonia in the United States, 2018–2022. Antibiotics 2025, 14, 642. https://doi.org/10.3390/antibiotics14070642
Zilberberg MD, Greenberg M, Curt V, Shorr AF. The Burden of Hospitalization and Rehospitalization Among Patients Hospitalized with Severe Community-Acquired Bacterial Pneumonia in the United States, 2018–2022. Antibiotics. 2025; 14(7):642. https://doi.org/10.3390/antibiotics14070642
Chicago/Turabian StyleZilberberg, Marya D., Mike Greenberg, Valentin Curt, and Andrew F. Shorr. 2025. "The Burden of Hospitalization and Rehospitalization Among Patients Hospitalized with Severe Community-Acquired Bacterial Pneumonia in the United States, 2018–2022" Antibiotics 14, no. 7: 642. https://doi.org/10.3390/antibiotics14070642
APA StyleZilberberg, M. D., Greenberg, M., Curt, V., & Shorr, A. F. (2025). The Burden of Hospitalization and Rehospitalization Among Patients Hospitalized with Severe Community-Acquired Bacterial Pneumonia in the United States, 2018–2022. Antibiotics, 14(7), 642. https://doi.org/10.3390/antibiotics14070642







