In Vitro Therapeutic Efficacy of Furazolidone for Antimicrobial Susceptibility Testing on Campylobacter
Abstract
1. Introduction
2. Results
2.1. First Study Phase (2012–2013)
2.2. Second Study Phase (2014–2015)
2.3. MIC and Inhibitory Quotient (IQ) Analysis
2.4. Multidrug Resistance Trends
3. Discussion
3.1. Strengths
3.2. Main Discussion
3.3. Limitations
4. Methods
4.1. Study Design and Ethical Approval
4.2. Sample Collection, Inclusion Criteria, and Variables
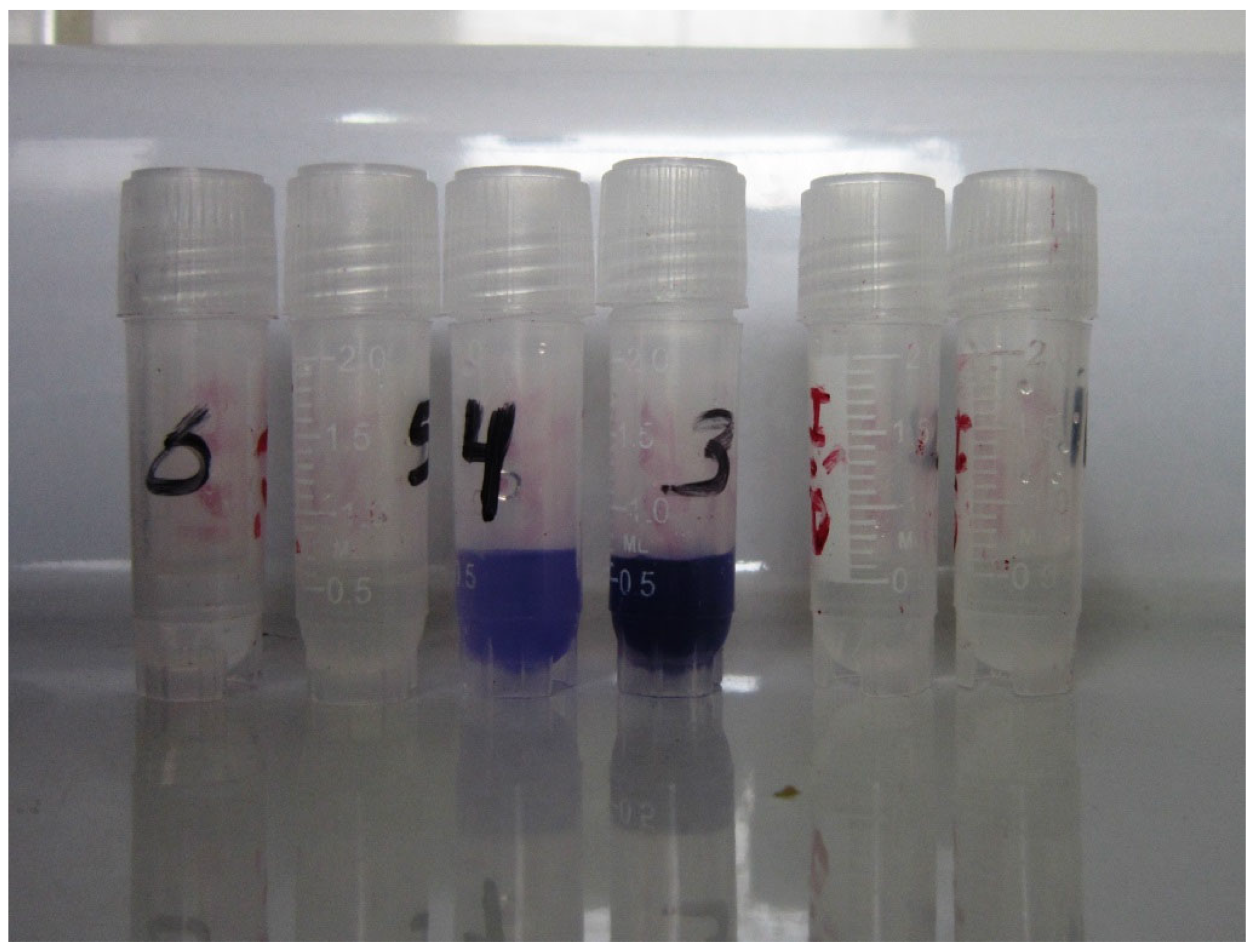
4.3. Bacterial Isolation and Culture
4.4. Bacterial Identification
4.5. Antibiotic Susceptibility Testing
4.6. Determination of Minimum Inhibitory Concentration (MIC)
4.7. Inhibitory Quotient (IQ) Determination
4.8. Statistical Analysis
4.9. Ethical Statement
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Kaakoush, N.O.; Castaño-Rodríguez, N.; Mitchell, H.M.; Man, S.M. Global epidemiology of Campylobacter infection. Clin. Microbiol. Rev. 2015, 28, 687–720. [Google Scholar] [CrossRef] [PubMed]
- Block, C.; Shainberg, B.; Valinsky, L.; Ken-Dror, S.; Agmon, V.; Lerner, L.; Peled, N.; Keller, N.; Keness, Y.; Rouach, T.; et al. Trends in the Epidemiology of Campylobacteriosis in Israel (1999–2012). Foodborne Pathog. Dis. 2016, 13, 448–455. [Google Scholar] [CrossRef]
- Allos, B.M.; Blaser, M.J. Mandell, Douglas & Bennett’s Principles and Practice of Infectious Diseases; Mandel, G.L., Ed.; Elsevier Publishing Co: Philadelphia, PA, USA, 2009; Chapter 2016. [Google Scholar]
- Szczepanska, B.; Andrzejewska, M.; Spica, D.; Klawe, J.J. Prevalence and antimicrobial resistance of Campylobacter jejuni and Campylobacter coli isolated from children and environmental sources in urban and suburban areas. BMC Microbiol. 2017, 17, 80. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Lindo, E.; Meza, R.; Kasper, M.; Rocha, C.; Gregory, M.; Perez, J.; Bernal, M.; Patiño, L.; Valencia, A.; Camiña, M.; et al. Campylobacter antimicrobial resistance in Peru: A ten-year observational study. BMC Infect. Dis. 2012, 12, 193. [Google Scholar] [CrossRef]
- World Health Organization. WHO Publishes List of Bacteria for Which New Antibiotics are Urgently Needed; WHO: Geneva, Switzerland, 2017; Available online: http://www.who.int/mediacentre/news/releases/2017/bacteria-antibiotics-needed/es/ (accessed on 27 February 2025).
- Urban-Chmiel, R.; Marek, A.; Stępień-Pyśniak, D.; Wieczorek, K.; Dec, M.; Nowaczek, A.; Osek, J. Antibiotic resistance in bacteria—A review. Antibiotics 2022, 11, 1079. [Google Scholar] [CrossRef]
- Ministerio de Salud. Centro de Atención Farmacéutica (CAF DIGEMID) Furazolidona. Available online: https://es.scribd.com/document/383859102/Furazolidona-pdf (accessed on 10 January 2018).
- Wang, S.-M.; Huang, F.-H.; Wu, C.-H.; Tang, K.-S.; Tiao, M.-M. Clinical significance of erythromycin-resistant Campylobacter jejuni in children. J. Microbiol. Immunol. Infect. 2011, 44, 63–66. [Google Scholar] [CrossRef]
- Li, Y.-Y.; Qu, J.-Y.; Guo, C.-G.; Ji, C.-R.; Liu, J.; Zhang, Y.; Zuo, X. Safety of furazolidone-containing regimen in Helicobacter pylori infection: A systematic review and meta-analysis. BMJ Open 2020, 10, e037375. [Google Scholar] [CrossRef]
- Rabbani, G.H.; Butler, T.; Shahrier, M.; Mazumdar, R.; Islam, M.R. Efficacy of a single dose of furazolidone for treatment of cholera in children. Antimicrob. Agents Chemother. 1991, 35, 1864–1867. [Google Scholar] [CrossRef]
- Safaralizadeh, R.; Siavoshi, F.; Malekzadeh, R.; Akbari, M.R.; Derakhshan, M.H.; Sohrabi, M.R.; Massarrat, S. Antimicrobial effectiveness of furazolidone against metronidazole-resistant strains of Helicobacter pylori. East Mediterr Health J. 2006, 12, 286–293. [Google Scholar] [PubMed]
- The Gastrointestinal Physiology Working Group of Cayetano Heredia; The Johns Hopkins Universities; Morgan, D.; Kraft, W.; Bender, M.; Pearson, A. Nitrofurans in the treatment of gastritis associated with Campylobacter pylori. Gastroenterology 1988, 95, 1178–1184. [Google Scholar] [CrossRef]
- Moya-Salazar, J.; Terán-Vásquez, A.; Salazar-Hernández, R. High-Antimicrobial Resistance to Fluoroquinolones by Campylobacter in Pediatric Patients in a Peruvian Hospital. Rev. Peru Med. Exp. Salud Publica 2018, 35, 156–158. [Google Scholar] [CrossRef] [PubMed]
- Adam, E.; Klein, P.; Graham, D.; Evans, D.; Opekun, A.; Smith, K.; Polasani, R.; Evans, D.; Alpert, L.; Michaletz, P.; et al. In vivo susceptibility of Campylobacter pylori. Am. J. Gastroenterol. 1989, 84, 233–238. [Google Scholar]
- Wu, S.; Wang, Y.; Zhuge, L.; Li, Z.; Zhao, R.; Xie, Y. Furazolidone treatment for Helicobacter Pylori infection: A systematic review and meta-analysis. Helicobacte 2018, 23, e12468. [Google Scholar] [CrossRef]
- Vanhoof, R.; Vanderlinden, M.P.; Dierickx, R.; Lauwers, S.; Yourassowsky, E.; Butzler, J.P. Susceptibility of Campylobacter fetus subsp. jejuni to Twenty-Nine Antimicrobial Agents. Antimicrob. Agents Chemother. 1978, 14, 553–556. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, 26th ed.; CLSI supplement M100S; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2016. [Google Scholar]
- The European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 7.1. 2017. Available online: https://www.megumed.de/wp-content/uploads/2024/02/v_14.0_Breakpoint_Tables.pdf (accessed on 21 June 2025).
- Aksomaitiene, J.; Ramonaite, S.; Olsen, J.E.; Malakauskas, M. Prevalence of Genetic Determinants and Phenotypic Resistance to Ciprofloxacin in Campylobacter jejuni from Lithuania. Front. Microbiol. 2018, 9, 203. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, X.; Liu, Y.; Jiang, J.; Shen, Z.; Chen, Q.; Ma, X. Tipos de secuencias de loci múltiples y resistencia antimicrobiana de aislamientos de Campylobacter jejuni y C. coli de pacientes humanos de Beijing, China, 2017–2018. Front. Microbiol. 2020, 11, 554784. [Google Scholar] [CrossRef]
- Smith, J.J.; Bulach, D.; Glass, K.; Kirk, M.D.; Polkinghorne, B.G.; Jennison, A.V.; Valcanis, M.; Wallace, R.L.; Varrone, L.; McLure, A. Antimicrobial Resistance of Campylobacter spp. Causing Human Infection in Australia: An International Comparison. Microb. Drug Resist. 2021, 27, 518–528. [Google Scholar] [CrossRef]
- Hanna, S.; Vugia, D.J.; Payne, D.C.; Ford, L.; Bruce, B.B.; Chen, J.; Ray, L.C.; Healy, J.M.; Cui, Z.; Ahart, L.; et al. Epidemiology and Antimicrobial Resistance of Campylobacter Infections in the United States, 2005–2018. Open Forum Infect. Dis. 2023, 10, ofad378. [Google Scholar] [CrossRef]
- Tang, M.; Zhou, Q.; Zhang, X.; Zhou, S.; Zhang, J.; Tang, X.; Lu, J.; Gao, Y. Antibiotic Resistance Profiles and Molecular Mechanisms of Campylobacter from Chicken and Pig in China. Front. Microbiol. 2020, 11, 592496. [Google Scholar] [CrossRef]
- Portes, A.B.; Panzenhagen, P.; Pereira dos Santos, A.M.; Junior, C.A.C. Antibiotic Resistance in Campylobacter: A Systematic Review of South American Isolates. Antibiotics 2023, 12, 548. [Google Scholar] [CrossRef]
- World Health Organizaton. Global Antimicrobial Resistance Surveillance System Report; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Hlashwayo, D.F.; Sigaúque, B.; Bila, C.G. Epidemiology and antimicrobial resistance of Campylobacter spp. in animals in Sub-Saharan Africa: A systematic review. Heliyon 2020, 6, e03537. [Google Scholar] [CrossRef] [PubMed]
- Same, R.G.; Tamma, P.D. Campylobacter Infections in Children. Pediatr. Rev. 2018, 39, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Benguigui, Y.; Bernal, C.; Figueroa, D. Manual de Tratamiento de la Diarrea en Niños Serie PALTEX para Ejecutores de Programas de Salud No. 48; OPS: Washington, DC, USA, 2008. [Google Scholar]
- Afazani, A.; Beltramino, D.; Bruno, M.E.; Cairoli, H.; Caro, M.B.; Cervetto, J.L.; Daniel, S.; De Rosa, S.; Escobal, N.; Turienzo, C.F.; et al. Diarrea aguda en la infancia. In Actualización Sobre Criterios de Diagnóstico y Tratamiento; Consenso Nacional, Ministerio de Salud Pública: Buenos Aires, Argentina, 2020. [Google Scholar]
- Ministerio de Salud. Guía de Práctica Clínica para el Diagnóstico y Tratamiento de Diarrea Aguda Infecciosa en Paciente Pediátrico; MINSA: Lima, Peru, 2022. [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria, 3rd ed.; CLSI guidelines M45; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2015. [Google Scholar]
- Fishbein, S.R.; Mahmud, B.; Dantas, G. Antibiotic perturbations to the gut microbiome. Nat. Rev. Microbiol. 2023, 21, 772–788. [Google Scholar] [CrossRef]
- Feitosa, I.B.; Mori, B.; Santos, A.P.D.A.D.; Villanova, J.C.O.; Teles, C.B.G.; Costa, A.G. What are the immunopharmacological effects of furazolidone? A systematic review. Immunopharmacol. Immunotoxicol. 2021, 43, 674–679. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Ruiz, A.P.; Perea, L.B. Indicaciones y valoración clínica del urocultivo y coprocultivo. Medicine 2010, 10, 3317–3320. [Google Scholar]
- Moya-Salazar, J.; Pio-Dávila, L.; Terán-Vásquez, A.; Olivo, L.J. Yield diagnosis of blood agar with filter against karmali agar for isolation of Campylobacter in stool culture. Horiz. Med. 2016, 16, 58–65. (In Spanish) [Google Scholar]
- CLSI. Publication M40-A2. In Quality Control of Microbiological Transport Systems; Approved Standard, 2nd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2014. [Google Scholar]
- de Baranda Camino, C.S.; Álvarez, J.B.; Señalada, J.B.; González, R.C.; Garaizábal, E.E.; Serra, J.L.; Padilla, T.P.; Bravo, E.R.; Domínguez, P.R.; Córdoba, M.E.S. Manual de Recogida, Transporte y Conservación de Muestras; Laboratorio de microbiología, Complejo Hospitalario de Albacete: Albacete, Spain, 2010. [Google Scholar]
- Engberg, J.; On, S.L.; Harrington, C.S.; Gerner-Smidt, P. Prevalence of Campylobacter, Arcobacter, Helicobacter, and Sutterella spp. in human fecal samples as estimated by a reevaluation of isolation methods for campylobacters. J. Clin. Microbiol. 2000, 38, 286–291. [Google Scholar] [CrossRef]
- Steele, T.W.; McDermott, S.N. Technical note: The use of membrane filters applied directly to the surface of agar plates for the isolation of Campylobacter jejuni from faeces. Pathology 1984, 16, 263–265. [Google Scholar] [CrossRef]
- Winn, W.; Allen, S.; Janda, W.; Koneman, E.; Procop, G.; Schreckenberger, P.; Woods, G. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; pp. 373–379. [Google Scholar]
- CLSI. Publication M35-A2. In Abbreviated Identification of Bacteria and Yeast; Approved Guideline, 2nd ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2008. [Google Scholar]
- Kahlmeter, G.; Brown, D.F.; Goldstein, F.W.; MacGowan, A.P.; Mouton, J.W.; Österlund, A.; Rodloff, A.; Steinbakk, M.; Urbaskova, P.; Vatopoulos, A. European harmonization of MIC breakpoints for antimicrobial susceptibility testing of bacteria. J. Antimicrob. Chemother. 2003, 52, 145–148. [Google Scholar] [CrossRef]
- Neu, H.C.; Ellner, P.D. The inhibitory quotient. Bull. N. Y. Acad Med. 1983, 59, 430–442. [Google Scholar] [PubMed]
- Drusano, G.L.; Goldastein, F.W. Relevance of the Alexander Project: Pharmacodynamic considerations. J. Antimicrob. Chemother. 1996, 38 (Suppl. A), 141–154. [Google Scholar] [CrossRef] [PubMed]
- Forrest, A.; Nix, D.; Ballow, D.; Goss, T.; Birmingham, B.; Schentag, J. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob. Agents Chemother. 1993, 37, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Turnidge, J.; Paterson, D.L. Setting and revising antibacterial susceptibility breakpoints. Clin. Microbiol. Rev. 2007, 20, 391–408. [Google Scholar] [CrossRef]
- Altman, D.; Machin, D.; Bryant, T.; Gardner, M. Statistics with Confidence: Confidence Intervals and Statistical Guidelines, 2nd ed.; BMJ Books: London, UK, 1989; p. 254. [Google Scholar]

| CLSI (mm) | EUCAST (mm) | MIC (μg/mL) § | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ERY | CIP | FZD | ERY * | CIP | FZD | ERY | CIP | FZD | ||||||||||||||||
| R | I | S | R | I | S | R | I | S | R | S | R | S | R | S | R | I | S | R | I | S | R | I | S | |
| C. jejuni | 2 | 0 | 28 | 26 | 0 | 4 | 0 | 4 | 26 | 4 | 26 | 28 | 2 | 0 | 30 | 2 | 0 | 28 | 26 | 0 | 4 | 0 | 4 | 26 |
| C.no-jejuni | 8 | 2 | 66 | 62 | 8 | 6 | 0 | 2 | 74 | 16 | 60 | 72 | 4 | 0 | 76 | 8 | 2 | 66 | 62 | 8 | 6 | 0 | 2 | 74 |
| C. spp. | 2 | 0 | 86 | 86 | 0 | 2 | 0 | 0 | 88 | 2 | 86 | 86 | 2 | 0 | 88 | 2 | 0 | 86 | 86 | 0 | 2 | 0 | 0 | 88 |
| Total | 12 | 2 | 180 | 174 | 8 | 12 | 0 | 6 | 188 | 22 | 172 | 186 | 8 | 0 | 194 | 12 | 2 | 180 | 174 | 8 | 12 | 0 | 6 | 188 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moya-Salazar, J.; Terán-Vásquez, A.; Salazar-Hernandez, R.; Rojas-Zumaran, V.; Goicochea-Palomino, E.A.; Moya-Salazar, M.M.; Contreras-Pulache, H. In Vitro Therapeutic Efficacy of Furazolidone for Antimicrobial Susceptibility Testing on Campylobacter. Antibiotics 2025, 14, 636. https://doi.org/10.3390/antibiotics14070636
Moya-Salazar J, Terán-Vásquez A, Salazar-Hernandez R, Rojas-Zumaran V, Goicochea-Palomino EA, Moya-Salazar MM, Contreras-Pulache H. In Vitro Therapeutic Efficacy of Furazolidone for Antimicrobial Susceptibility Testing on Campylobacter. Antibiotics. 2025; 14(7):636. https://doi.org/10.3390/antibiotics14070636
Chicago/Turabian StyleMoya-Salazar, Jeel, Alfonso Terán-Vásquez, Richard Salazar-Hernandez, Víctor Rojas-Zumaran, Eliane A. Goicochea-Palomino, Marcia M. Moya-Salazar, and Hans Contreras-Pulache. 2025. "In Vitro Therapeutic Efficacy of Furazolidone for Antimicrobial Susceptibility Testing on Campylobacter" Antibiotics 14, no. 7: 636. https://doi.org/10.3390/antibiotics14070636
APA StyleMoya-Salazar, J., Terán-Vásquez, A., Salazar-Hernandez, R., Rojas-Zumaran, V., Goicochea-Palomino, E. A., Moya-Salazar, M. M., & Contreras-Pulache, H. (2025). In Vitro Therapeutic Efficacy of Furazolidone for Antimicrobial Susceptibility Testing on Campylobacter. Antibiotics, 14(7), 636. https://doi.org/10.3390/antibiotics14070636






