Pet Owners’ Knowledge of Antibiotic Use and Antimicrobial Resistance and Their Antibiotic Practices: Comparison Between Contexts of Self and Pet
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics
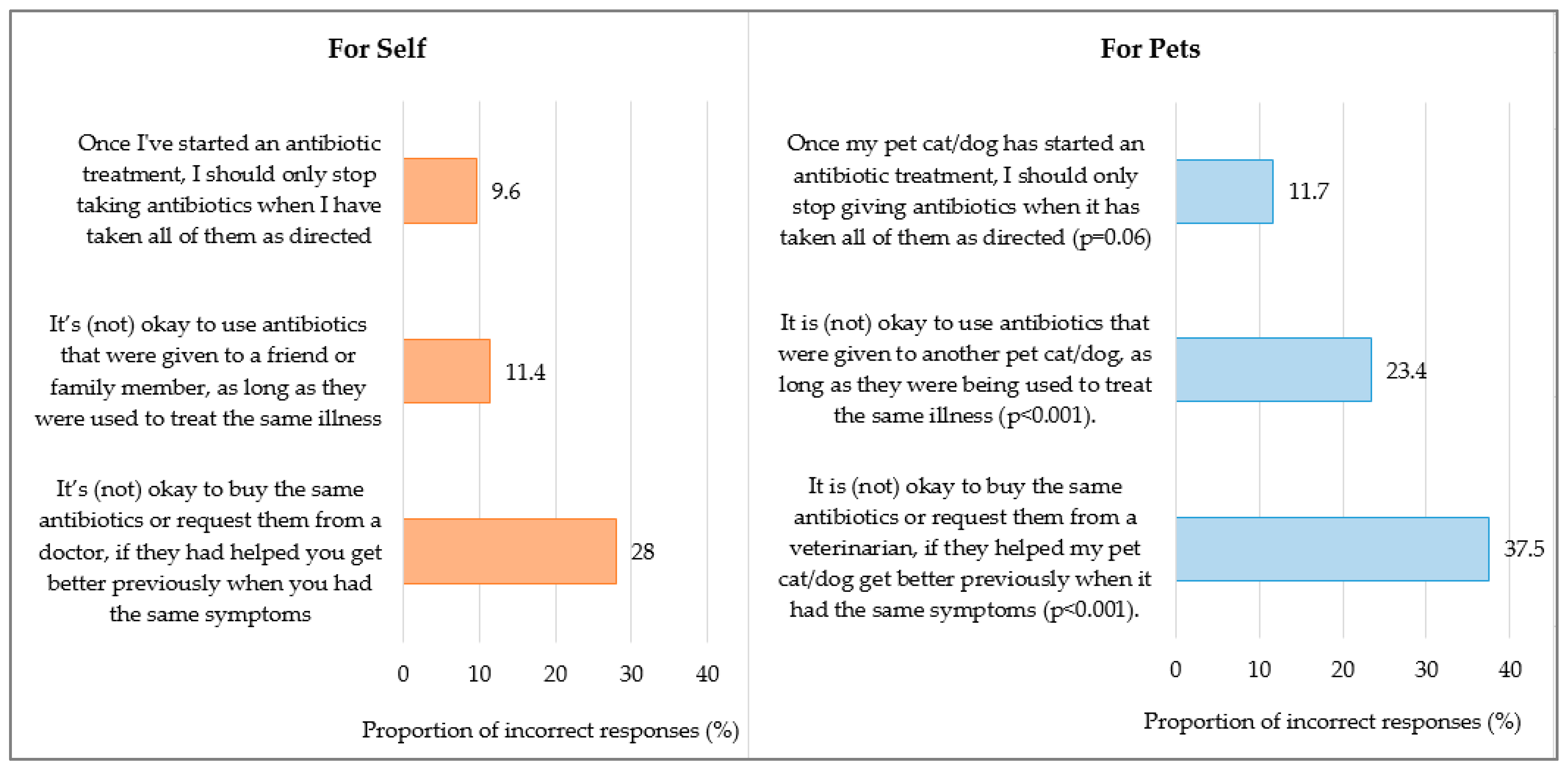
2.2. Knowledge of Antibiotic Use
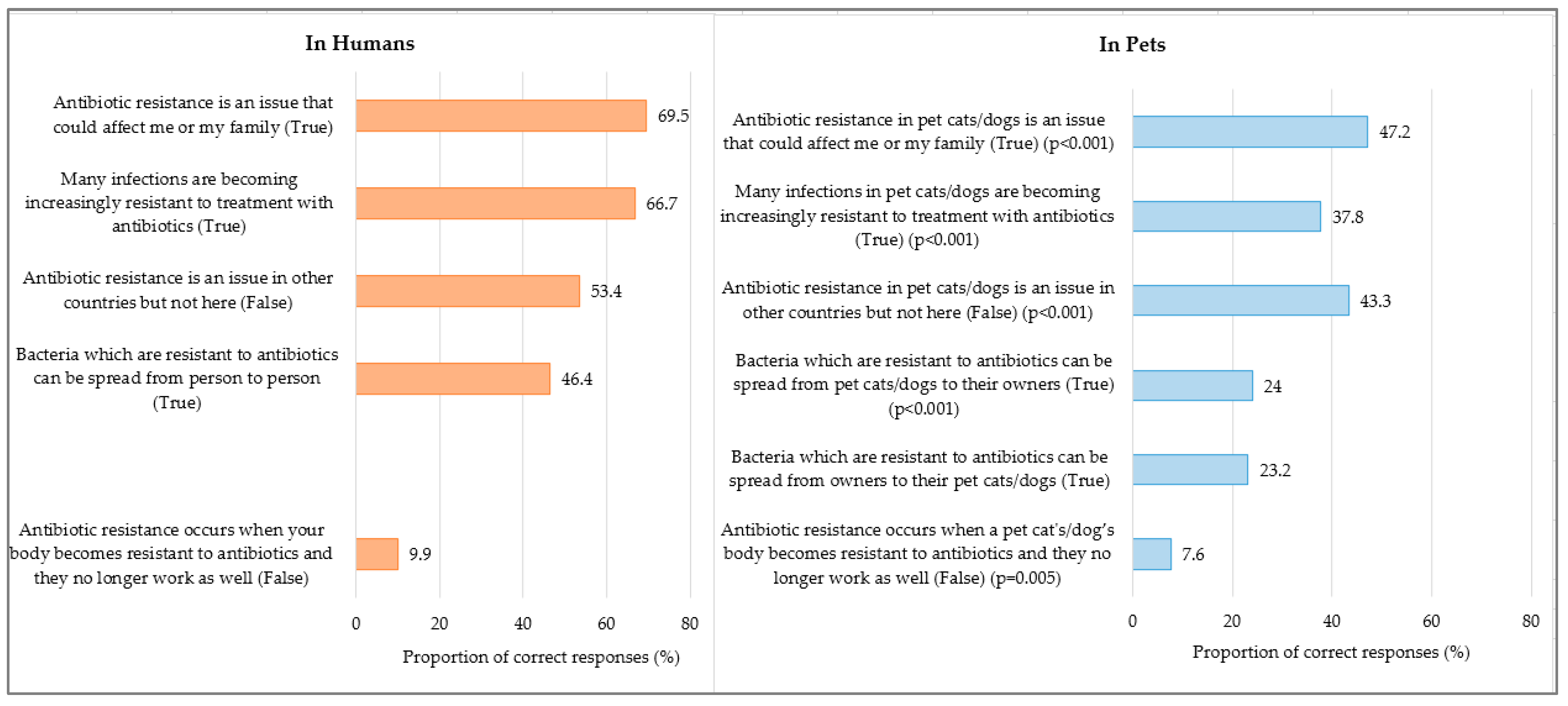
2.3. Knowledge of Antimicrobial Resistance
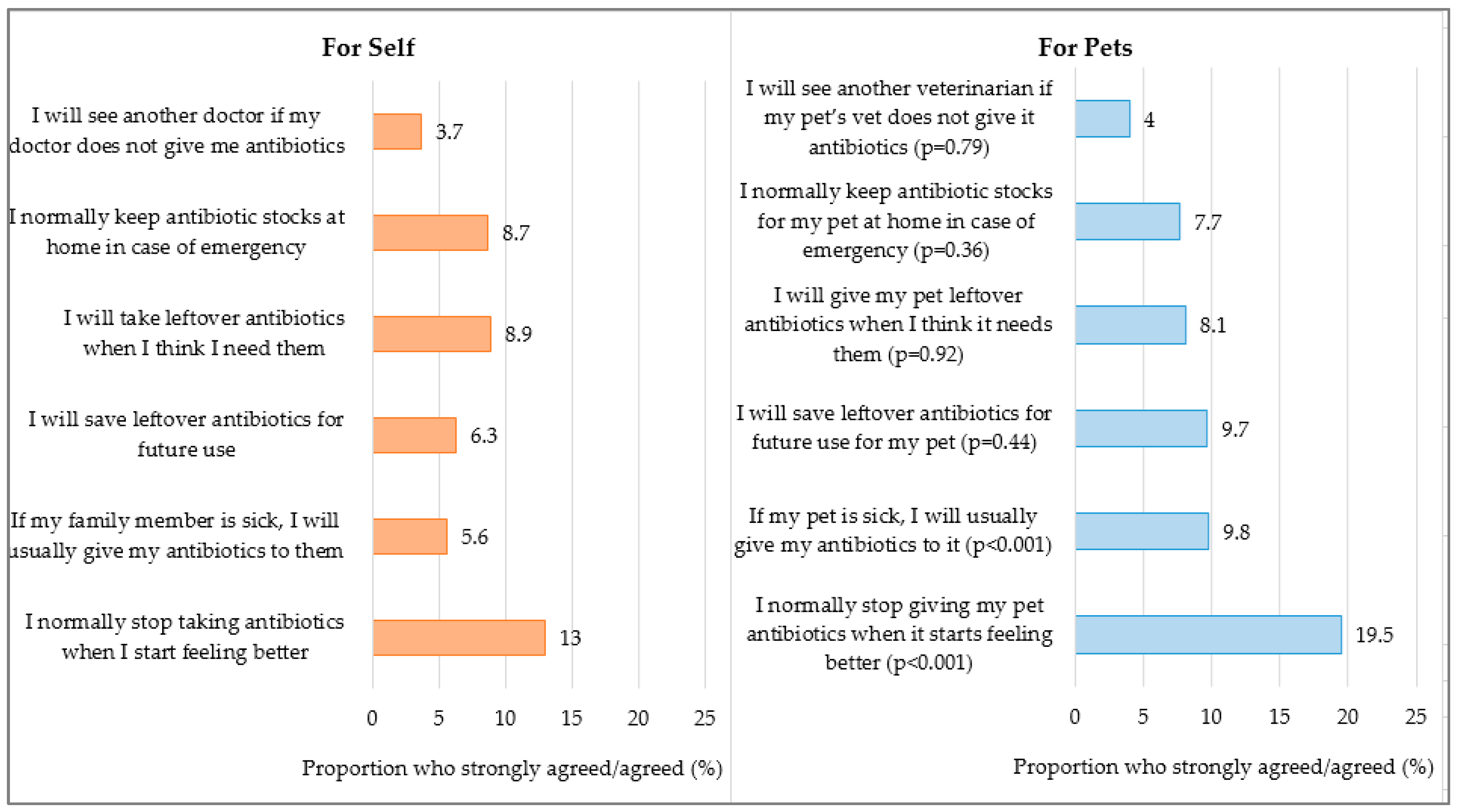
2.4. Antibiotic Practices
3. Discussion
4. Methods
4.1. Study Design and Settings
4.2. Survey Instrument
4.3. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; Wool, E.E.; Aguilar, G.R.; Mestrovic, T.; Smith, G.; Han, C.; et al. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Sobkowich, K.E.; Weese, J.S.; Poljak, Z.; Plum, A.; Szlosek, D.; Bernardo, T.M. Epidemiology of companion animal AMR in the United States of America: Filling a gap in the one health approach. Front. Public Health 2023, 11, 1161950. [Google Scholar] [CrossRef]
- Guardabassi, L.; Schwarz, S.; Lloyd, D.H. Pet animals as reservoirs of antimicrobial-resistant bacteria. J. Antimicrob. Chemother. 2004, 54, 321–332. [Google Scholar] [CrossRef]
- Jin, M.; Osman, M.; Green, B.A.; Yang, Y.; Ahuja, A.; Lu, Z.; Cazer, C.L. Evidence for the transmission of antimicrobial resistant bacteria between humans and companion animals: A scoping review. One Health 2023, 17, 100593. [Google Scholar] [CrossRef] [PubMed]
- Pomba, C.; Rantala, M.; Greko, C.; Baptiste, K.E.; Catry, B.; van Duijkeren, E.; Mateus, A.; Moreno, M.A.; Pyörälä, S.; Ružauskas, M.; et al. Public health risk of antimicrobial resistance transfer from companion animals. J. Antimicrob. Chemother. 2017, 72, 957–968. [Google Scholar] [CrossRef] [PubMed]
- Overgaauw, P.A.M.; Vinke, C.M.; van Hagen, M.A.E.; Lipman, L.J.A. A One Health Perspective on the Human–Companion Animal Relationship with Emphasis on Zoonotic Aspects. Int. J. Environ. Res. Public Health 2020, 17, 3789. [Google Scholar] [CrossRef]
- World Health Organization WHO List of Medically Important Antimicrobials—A Risk Management Tool for Mitigating Antimicrobial Resistance Due to Non-Human Use. 2024. Available online: https://cdn.who.int/media/docs/default-source/gcp/who-mia-list-2024-lv.pdf (accessed on 28 May 2024).
- American Veterinary Medical Association. Pet Ownership and Demographic Sourcebook—Animals Kept as Companions. AVMA 2022. Available online: https://www.avma.org/resources-tools/reports-statistics/us-pet-ownership-statistics (accessed on 27 May 2024).
- European Pet Food Industry (FEDIAF). European Statistics—Facts and Figures 2022 Report. Available online: https://europeanpetfood.org/about/statistics (accessed on 3 June 2024).
- McEwen, S.A.; Collignon, P.J. Antimicrobial resistance: A one health perspective. Microbiol. Spectr. 2018, 6, ARBA-0009-2017. [Google Scholar] [CrossRef] [PubMed]
- Dickson, A.; Smith, M.; Smith, F.; Park, J.; King, C.; Currie, K.; Langdridge, D.; Davis, M.; Flowers, P. Understanding the relationship between pet owners and their companion animals as a key context for antimicrobial resistance-related behaviours: An interpretative phenomenological analysis. Health Psychol. Behav. Med. 2019, 7, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Frey, E.; Kedrowicz, A.; Hedgpeth, M.W. Decision making on antimicrobial use: Cat and dog owners' knowledge and preferences for veterinary communication. Vet. Rec. 2024, 194, e3411. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.D.; Scallan Walter, E.J. Colorado pet owners’ perceptions of and attitudes towards antimicrobial drug use and resistance. Vet. Rec. 2023, 192, e2583. [Google Scholar] [CrossRef] [PubMed]
- Stallwood, J.; Shirlow, A.; Hibbert, A. A UK-based survey of cat owners’ perceptions and experiences of antibiotic usage. J. Feline Med. Surg. 2020, 22, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.R.; Weese, J.S.; Stull, J.W.; McClure, J.T.; Evason, M. Knowledge, attitudes and influencers of cat owners in North America around antimicrobials and antimicrobial stewardship. J. Feline Med. Surg. 2022, 24, e90–e97. [Google Scholar] [CrossRef]
- Smith, M.; King, C.; Davis, M.; Dickson, A.; Park, J.; Smith, F.; Currie, K.; Flowers, P. Pet Owner and Vet Interactions: Exploring the Drivers of AMR. Antimicrob. Resist. Infect. Control. 2018, 7, 46. [Google Scholar] [CrossRef] [PubMed]
- Redding, L.E.; Cole, S.D. Pet owners’ knowledge of and attitudes toward the judicious use of antimicrobials for companion animals. J. Am. Vet. Med. Assoc. 2019, 254, 626–635. [Google Scholar] [CrossRef]
- Scarborough, R.; Hardefeldt, L.; Browning, G.; Bailey, K. Pet owners and antibiotics: Knowledge, opinions, expectations, and communication preferences. Antibiotics 2021, 10, 1326. [Google Scholar] [CrossRef]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655, Erratum in Lancet 2022, 400, 1102. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zellweger, R.M.; Carrique-Mas, J.; Limmathurotsakul, D.; Day, N.P.J.; Thwaites, G.E.; Baker, S.; Southeast Asia Antimicrobial Resistance Network. A current perspective on antimicrobial resistance in Southeast Asia. J. Antimicrob. Chemother. 2017, 72, 2963–2972. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Euromonitor International. Asia Pacific Pet Care Market Projected to Reach USD $29-Billion in 2024. 2024. Available online: https://www.euromonitor.com/press/press-releases (accessed on 27 May 2024).
- Hartantyo, S.H.P.; Chau, M.L.; Fillon, L.; Ariff, A.Z.B.M.; Kang, J.S.L.; Aung, K.T.; Gutiérrez, R.A. Sick pets as potential reservoirs of antibiotic-resistant bacteria in Singapore. Antimicrob. Resist. Infect. Control 2018, 7, 106. [Google Scholar] [CrossRef]
- Buranasinsup, S.; Wiratsudakul, A.; Chantong, B.; Maklon, K.; Suwanpakdee, S.; Jiemtaweeboon, S.; Sakcamduang, W. Prevalence and characterization of antimicrobial-resistant Escherichia coli isolated from veterinary staff, pets, and pet owners in Thailand. J. Infect. Public Health 2023, 16 (Suppl. 1), 194–202. [Google Scholar] [CrossRef] [PubMed]
- Tsuyuki, Y.; Kurita, G.; Murata, Y.; Goto, M.; Takahashi, T. Identification of Group G Streptococcal Isolates from Companion Animals in Japan and Their Antimicrobial Resistance Patterns. Jpn. J. Infect. Dis. 2017, 70, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Wang, X.; He, J.; Zhou, K.; Xie, M.; Ding, H. Serovar and sequence type distribution and phenotypic and genotypic antimicrobial resistance of Salmonella originating from pet animals in Chongqing, China. Microbiol. Spectr. 2024, 12, e0354223. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kyung, S.M.; Lee, J.H.; Lee, E.-S.; Xiang, X.-R.; Yoo, H.S. Emergence and genomic characterization of Proteus mirabilis harboring blaNDM-1 in Korean companion dogs. Vet. Res. 2024, 55, 50. [Google Scholar] [CrossRef]
- Afshar, M.F.; Zakaria, Z.; Cheng, C.H.; Ahmad, N.I. Prevalence and multidrug-resistant profile of methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus pseudintermedius in dogs, cats, and pet owners in Malaysia. Vet. World. 2023, 16, 536–545. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scarborough, R.; Sri, A.E.; Browning, G.F.; Hardefeldt, L.Y.; Bailey, K.E. ‘Brave Enough’: A Qualitative Study of Veterinary Decisions to Withhold or Delay Antimicrobial Treatment in Pets. Antibiotics 2023, 12, 540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chadborn, T.; Williams, S.; Jorgensen, T.; Price, C.; Buckel, A.; Altieri, E. An approach for embedding behavioural science in antimicrobial resistance One Health research. J. Infect. Public Health 2023, 16 (Suppl. 1), 134–140. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Food and Agriculture Organization of the United Nations; United Nations Environment Programme and World Organisation for Animal Health. A One Health Priority Research Agenda for Antimicrobial Resistance. Geneva; 2023. Licence: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/handle/10665/370279 (accessed on 3 June 2024).
- One Health Antimicrobial Resistance Workgroup. One Health Report on Antimicrobial Utilisation and Resistance. National Centre for Infectious Diseases. 2019. Available online: https://www.ncid.sg/Health-Professionals/Documents/One%20Health%20Report%20on%20Antimicrobial%20Utilisation%20and%20Resistance%202019.pdf (accessed on 3 June 2024).
- Euromonitor International. Pet Care in Asia Pacific—Market Research Report. 2023. Available online: https://www.euromonitor.com/pet-care-in-asia-pacific/report (accessed on 27 May 2024).
- Price, L.; Gozdzielewska, L.; Young, M.; Smith, F.; MacDonald, J.; McParland, J.; Williams, L.; Langdridge, D.; Davis, M.; Flowers, P. Effectiveness of interventions to improve the public’s antimicrobial resistance awareness and behaviours associated with prudent use of antimicrobials: A systematic review. J. Antimicrob. Chemother. 2018, 73, 1464–1478. [Google Scholar] [CrossRef]
- Courtenay, M.; Castro-Sanchez, E.; Fitzpatrick, M.; Gallagher, R.; Lim, R.; Morris, G. Tackling antimicrobial resistance 2019–2024—The UK’s five-year national action plan. J. Hosp. Infect. 2019, 101, 426–427. [Google Scholar] [CrossRef]
- Wright, E.; Jessen, L.R.; Tompson, A.; Rutland, C.; Singleton, D.; Battersby, I.; Gajanayake, I.; Mosher, M.; Pfleger, S.; Gemmill, T.; et al. Influencing attitudes towards antimicrobial use and resistance in companion animals-the impact on pet owners of a short animation in a randomized controlled trial. JAC Antimicrob. Resist. 2024, 6, dlae065. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Quigley, M.; McKenna, C.; Webb, T.L. Best practices for recruitment in veterinary clinical trials. Front. Vet. Sci. 2024, 11, 1418747. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brøgger-Mikkelsen, M.; Ali, Z.; Zibert, J.R.; Andersen, A.D.; Thomsen, S.F. Online patient recruitment in clinical trials: Systematic review and meta-analysis. J. Med. Internet Res. 2020, 22, e22179. [Google Scholar] [CrossRef]
- Candellone, A.; Badino, P.; Girolami, F.; Ala, U.; Mina, F.; Odore, R. Dog owners’ attitude toward veterinary antibiotic use and antibiotic resistance with a focus on canine diarrhea management. Animals 2023, 13, 1061. [Google Scholar] [CrossRef]
- Rocholl, C.; Zablotski, Y.; Schulz, B. Online-Assisted Survey on Antibiotic Use by Pet Owners in Dogs and Cats. Antibiotics 2024, 13, 382. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Antibiotic Do’s & Don’ts: Take Antibiotics Exactly as Prescribed If You Need Them. 2021. Available online: https://www.cdc.gov/antibiotic-use/about/index.html (accessed on 8 April 2024).
| Demographics | Total (N = 1080) | Own Dogs (N = 754) | Do Not Own Dogs (N = 326) |
|---|---|---|---|
| Age group, in years, N(%) | |||
| 21–34 | 399 (36.9) | 262 (34.8) | 137 (42.0) |
| 35–49 | 382 (35.4) | 264 (35.0) | 118 (36.2) |
| 50 and above | 299 (27.7) | 228 (30.2) | 71 (21.8) |
| Gender, N(%) | |||
| Male | 390 (36.1) | 280 (37.1) | 110 (33.7) |
| Female | 690 (63.9) | 474 (62.9) | 216 (66.3) |
| Ethnicity, N(%) | |||
| Chinese | 798 (73.9) | 621 (82.4) | 177 (54.3) |
| Malay | 91 (8.4) | 3 (0.4) | 88 (27.0) |
| Indian | 70 (6.5) | 55 (7.3) | 15 (4.6) |
| Others | 121 (11.2) | 75 (10.0) | 46 (14.1) |
| Highest education level, N(%) | |||
| Lower educated (GCE-A level & below) | 141 (13.1) | 99 (13.1) | 42 (12.9) |
| Higher educated (Diploma & above) | 939 (86.9) | 655 (86.9) | 284 (87.1) |
| Marital status, N(%) | |||
| Married | 607 (56.2) | 426 (56.5) | 181 (55.5) |
| Never married/widowed/divorced/separated | 473 (43.8) | 328 (43.5) | 145 (44.5) |
| Housing type, N(%) | |||
| 1- to 4-room HDB apartments | 378 (35.0) | 226 (30) | 152 (46.6) |
| 5-room HDB; Privately-owned apartments, condominiums, and houses | 702 (65.0) | 528 (70) | 174 (53.4) |
| Employment status, N(%) | |||
| Currently working | 825 (76.4) | 574 (76.1) | 251 (77.0) |
| Retired/not working | 255 (23.6) | 180 (23.9) | 75 (23.0) |
| Occupation, N(%) | |||
| Not related to human or animal health | 833 (77.1) | 590 (78.3) | 243 (74.5) |
| Related to human or animal health | 247 (22.9) | 164 (21.8) | 83 (25.5) |
| Duration of pet ownership, N(%) | |||
| ≤10 years | 605 (56.0) | 393 (52.1) | 212 (65.0) |
| >10 years | 475 (44.0) | 361 (47.9) | 114 (35.0) |
| Knowledge of antibiotic use for pets, N(%) | |||
| Not poor | 580 (53.7) | 434 (57.6) | 146 (44.8) |
| Poor | 500 (46.3) | 320 (42.4) | 180 (55.2) |
| Knowledge of AMR in pets, N(%) | |||
| Not poor | 355 (32.9) | 258 (34.2) | 97 (29.8) |
| Poor | 725 (67.1) | 496 (65.8) | 229 (70.3) |
| Use of antibiotics for pets, N(%) | |||
| Appropriate | 714 (66.1) | 493 (65.4) | 221 (67.8) |
| Inappropriate | 366 (33.9) | 261 (34.6) | 105 (32.2) |
| Knowledge of antibiotic use for self, N(%) | |||
| Not poor | 722 (66.9) | 521 (69.1) | 201 (61.7) |
| Poor | 358 (33.2) | 233 (30.9) | 125 (38.3) |
| Knowledge of AMR in humans, N(%) | |||
| Not poor | 379 (35.1) | 269 (35.7) | 110 (33.7) |
| Poor | 701 (64.9) | 485 (64.3) | 216 (66.3) |
| Use of antibiotics for self, N(%) | |||
| Appropriate | 826 (76.5) | 579 (76.8) | 247 (75.8) |
| Inappropriate | 254 (23.5) | 175 (23.2) | 79 (24.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aithal, S.; Guo, H.; Teo, B.H.; Chua, T.; Hildon, Z.J.-L.; Chow, A. Pet Owners’ Knowledge of Antibiotic Use and Antimicrobial Resistance and Their Antibiotic Practices: Comparison Between Contexts of Self and Pet. Antibiotics 2025, 14, 158. https://doi.org/10.3390/antibiotics14020158
Aithal S, Guo H, Teo BH, Chua T, Hildon ZJ-L, Chow A. Pet Owners’ Knowledge of Antibiotic Use and Antimicrobial Resistance and Their Antibiotic Practices: Comparison Between Contexts of Self and Pet. Antibiotics. 2025; 14(2):158. https://doi.org/10.3390/antibiotics14020158
Chicago/Turabian StyleAithal, Seema, Huiling Guo, Boon Han Teo, Timothy Chua, Zoe Jane-Lara Hildon, and Angela Chow. 2025. "Pet Owners’ Knowledge of Antibiotic Use and Antimicrobial Resistance and Their Antibiotic Practices: Comparison Between Contexts of Self and Pet" Antibiotics 14, no. 2: 158. https://doi.org/10.3390/antibiotics14020158
APA StyleAithal, S., Guo, H., Teo, B. H., Chua, T., Hildon, Z. J.-L., & Chow, A. (2025). Pet Owners’ Knowledge of Antibiotic Use and Antimicrobial Resistance and Their Antibiotic Practices: Comparison Between Contexts of Self and Pet. Antibiotics, 14(2), 158. https://doi.org/10.3390/antibiotics14020158





