Antimicrobial Stewardship Programs in Pediatric Intensive Care Units: A Systematic Scoping Review
Abstract
1. Introduction
2. Results
| Author, Year, Setting | Study Design | Population | Intervention | Outcome | Key Findings |
|---|---|---|---|---|---|
| Audit and Feedback, presence of PID at ward round or positive Feedback | |||||
| Haque et al., 2018 [15], LMIC | Retrospective study comparing pre-intervention (Jan–Mar 2016) with post-intervention period (Apr–Jun 2016). Short report | Cardiothoracic PICU | Prospective audit and feedback | Antibiotic consumption by measuring total DOT/1000 pd in the pre- and post-intervention periods. | There was a 64% reduction in antibiotic utilization in ASP period. The appropriate use of empirical antibiotic therapy for culture-negative infection-like symptoms increased from 6% to 45% |
| Aizawa et al., 2018 [16], HIC | Retrospective study between Apr 2010 and Dec 2015 | All patients admitted | Pediatric infectious disease physicians attended the PICU morning rounds every day | The primary outcome was the consumption of antipseudomonal agents, as measured by DOT/1000 pd. ITS performed. | Significant reduction in the level and trend of DOT/1000 pd for total antipseudomonal agents (−24%); significant change in trend but not in level of DOT/1000 pd for non-antipseudomonal agents |
| Adams, 2019 [17], HIC | Retrospective cohort study, pre- and postimplementation quality improvement study (Jul 2015–Mar 2016) | All patients admitted | Mandatory antimicrobial time-out 48–72 h after initiation of therapy | Primary outcome: DOT/1000 pd for vancomycin, meropenem and piperacillin/tazobactam and DOT for all antibiotics | Overall significant reduction for DOT/1000 pd for overall antibiotics, meropenem and vancomycin |
| Jones et al., 2019 [18], HIC | Prospective non-randomized study, Apr 2017–Mar 2018 | All patients admitted | Positive feedback for behaviors via reports and interviews | Antibiotic consumption measured by dispended doses/PICU bes-days | Overall reduction by 6.5%, meropenem reduction by 17.5% |
| Renk et al., 2020 [20], HIC | Prospective, pre- and post-implementation cohort study (Jan 2017–Jun 2017 and Jan 2018–Jun 2018) | All patients admitted | Weekly PID ward round, audit and feedback | Antibiotic consumption by DOT/1000 ppd and LOT/1000 pd, PICU LOS, mortality, costs | Significant reduction of DOT/1000 pd by 18%. LoT/1000 ppd decreased not significantly. Vancomycin significantly decreased |
| Aljassim et al., 2021 [21], HIC | Multicenter retrospective cohort study (2 PICUs), pre- and postimplementation quality improvement study (Jul 2015–Mar 2016 and Jul 2016–Mar 2017) | Patients with bronchiolitis | Audit and feedback implemented in 1 PICU out of 2 | Proportion of antimicrobials discontinued 72 h after hospital admission; anti-microbial treatment duration; antimicrobial prescriptions within 48 h of hospital admission | ASP is associated with increased odds of discontinuing antimicrobials but not with antimicrobial duration or antimicrobial prescriptions |
| Kit-Anan et al., 2022 [22], LMIC | Historical control study (Jul 2017–Dec 2018 and Apr 2019–Sep 2020) | All patients admitted | “Handshake” approach ASP, no pre-authorization | Carbapenem consumption rate, measured by DOT/1000 pd | Carbapenem consumption significantly decreased |
| Alfraij et al., 2023 [25], HIC | Retrospective cohort study (Oct 2018–Oct 2020) | Admitted patients who received antimicrobials | Tele-ASP: weekly prospective audit and feedback by the ASP team, with PID specialist joining remotely | Antimicrobial consumption by DOT/1000 pd | A decline in DOT was observed across most antibiotic classes, except for ceftriaxone. In the analysis based on admission diagnosis, the decrease in antimicrobial consumption was significant only for cardiac diseases. No effect on the length of PICU stay, length of hospitalization or mortality was observed. |
| Zombori et al., 2023 [26], HIC | Multicenter retrospective study (Apr 19–Apr 21) | All patients admitted | The antimicrobial stewardship pre-dates the beginning of the study: twice weekly virtual handshake stewardship rounds on all ICUs discussing patients receiving antibiotics | Evaluation of antibiotic consumption by comparing the antimicrobial spectrum index (ASI) with DOTs | Median ASI/antibiotic days: Immunocompromised patients received much broader-spectrum antibiotics than immunocompetent patients. Patients who had stewardship input had a higher ASI compared with those who did not throughout the whole period. ASI shows less variability than DOT. |
| Preauthorization plus guidelines and education | |||||
| Wassef et al., 2020 [19], LMIC | Prospective study (Apr 2016, Jun 2017) | All patients admitted | Guidelines, education, antibiotics time-out, pre-authorization | Clinical outcome of patients, LOS, DOT, LOT | No difference in mortality, reduced LOT and LOS, decrease in ceftriaxone and amikacin consumption, increase in gentamicin, levofloxacin, clindamycin |
| Guidelines and education | |||||
| Lee et al., 2016 [14], HIC | Retrospective chart review before and after intervention (Sep 2010–Aug 2011 and Sep 2012–Aug 2013) | Patients in pediatric, neonatal cardiac ICUs | Guidelines and education | Monthly change in overall antibiotic and broad-spectrum antibiotic prescriptions by DOT/1000 pd | The overall antibiotic days of therapy in PICU decreased by 21%, and targeted broad-spectrum antibiotic days of therapy decreased by 75% after guideline implementation |
| Fan et al., 2023 [24], HIC | Retrospective study (May 2016 to April 2020) | Patients admitted with severe bacterial pneumonia | Education, regular inspections on antibiotics use | Antimicrobial resistance rates, antimicrobial consumption by DDD/1000 pd, antibiotic consumption and clinical outcome | Reduced resistances for S.pneumoniae, S.aureus, K.pneumoniae, A.baumanii. Cephalosporins, carbapenems, macrolides, antifungal agents and linezolid showed a decreasing consumption trend |
| Other interventions | |||||
| Oliveira da Silva et al., 2022 [23], LMIC | Longitudinal study (2007–2018) | Patients with Healthcare Associated Infection (HAI) | Monitoring software that flags patients with antimicrobial “alert” | Antibiotic consumption measured by DOT/1000 pd and antimicrobial resistance | Decrease in total antibiotic consumption; decrease in some antimicrobial resistances (Enterobacterales, S.aureus, non-fermenting gram-negative bacilli) |
| Author, Year, Setting | Study Design | Population | Intervention | Outcome | Key Findings |
|---|---|---|---|---|---|
| Downes et al., 2017 [27], HIC | Prospective cohort study Jan 2012–Mar 2014 | Children with SIRS and suspected infection | Biomarker panel daily for 72 h at initiation of antibiotics | “Excess” days of therapy (days after 48 h in patients in which bacterial infection is excluded) | The best combination of biomarkers to identify patients at low risk of bacterial infection was CRP ≤ 5.0 mg/dL plus SAA ≤ 15 µg/mL. Patients without bacterial infection received a mean of 3.8 excess days of therapy |
| Katz et al., 2021 [28], HIC | Single center, randomized prospective clinical trial (Feb 2018–Apr 2019) | Critically ill children admitted to an ICU setting and started on intravenous antibiotics | Intervention: PCT testing protocol; comparison: usual care arm | Median antibiotic DOTs per patient in the first 14 days after enrollment | No difference in antibiotic DOT between study arms |
| Wagner et al., 2021 [29], HIC | Retrospective review (Dec 2018–Aug 2019) | Admitted children 1 month-18 year with SIRS, at least 1 PCT level and one blood culture. Excluded if immunocompromised, antibiotics administered for <48 h or antibiotics initiated at an outside hospital | PCT monitoring protocol to help guide antibiotic decision-making | Adherence to the protocol | Full adherence was observed in 34%. Reasons for non-adherence were excess PCT monitoring (54.5%), antibiotic continuation (30.3%) or both (15.2%) |
| Yoshida et al., 2021 [30], HIC | Single-center, pre-/post-study (Dec 2017–Nov 2018 and Mar 2019–Feb 2020) | Consecutive children with respiratory infections | Multiplex polymerase chain reaction testing panel (17 viruses and 3 bacteria) with following recommendations | Primary outcome: pathogen identification rate during pre- and post-intervention. Secondary outcome: use and duration of antibiotics within 14 days of admission to the PICU, before and after the implementation of mPCR testing | The panel increased the proportion of pathogen identification. No differences were observed in use and duration of broad-spectrum antibiotics |
| Brotons et al., 2022 [31], HIC | Prospective cohort study (Dec 2015–Feb 2017) | Patients aged < 18 years with clinical diagnosis of acute low respiratory tract infection | Rapid panel test of respiratory viral and atypical bacteria | Primary outcome: panel diagnostic performance compared to standard, antimicrobial changes consequence of panel results, days of antimicrobial saved that could be attributable to panel test use | The panel increased diagnostic yield of routine diagnostic assays. The main achievements were suspension of oseltamivir and macrolide use with early panel results |
2.1. Type of Intervention
2.2. Metrics Used for Outcome Evaluation
2.3. Outcomes
3. Discussion
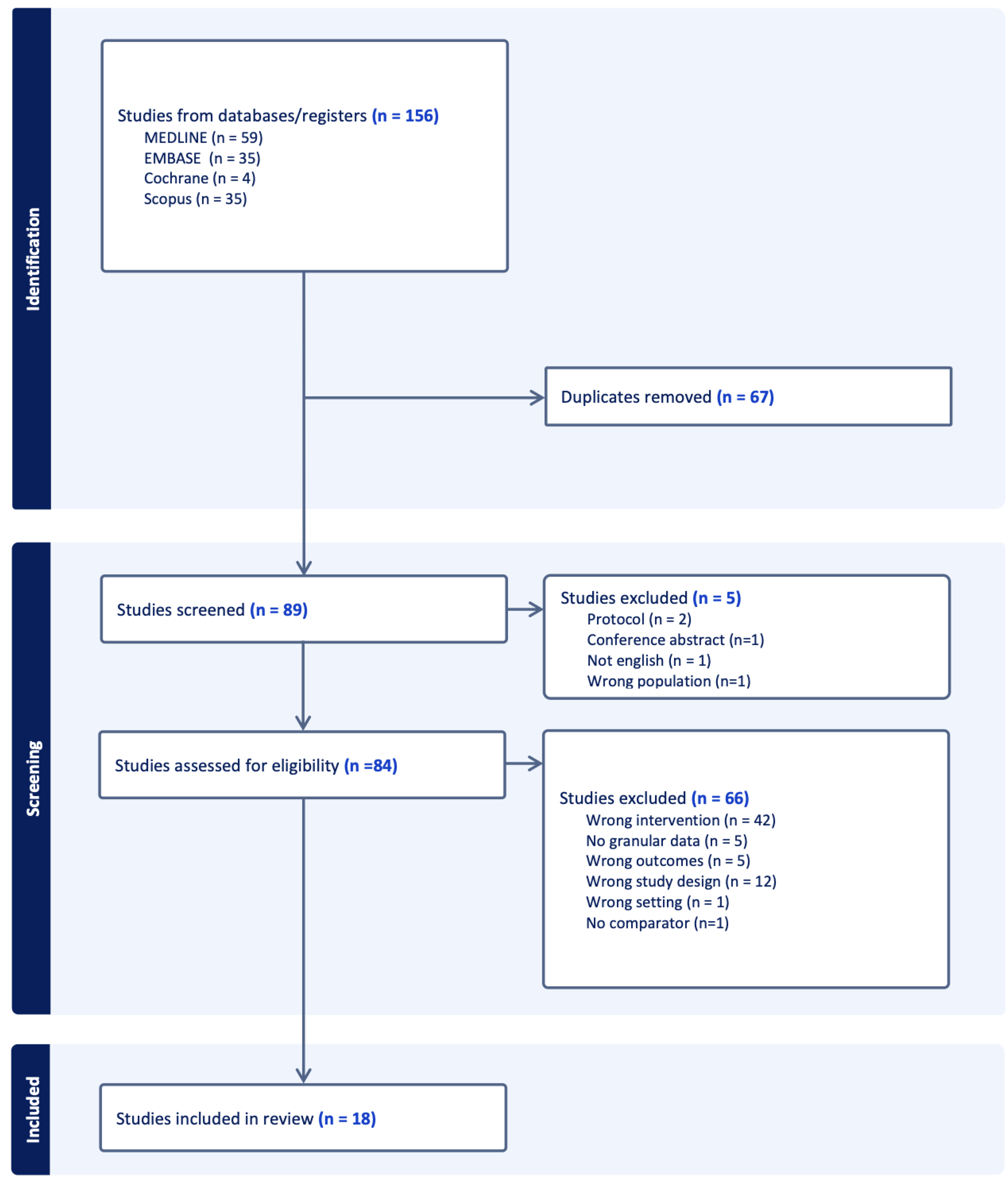
4. Materials and Methods
4.1. Study Design
4.2. Search Strategy and Data Extraction
4.3. Eligibility Criteria
4.4. Outcomes
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- EClinicalMedicine. Antimicrobial resistance: A top ten global public health threat. EClinicalMedicine 2021, 41, 101221. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Branstetter, J.W.; Barker, L.; Yarbrough, A.; Ross, S.; Stultz, J.S. Challenges of antibiotic stewardship in the pediatric and neonatal intensive care units. J. Pediatr. Pharmacol. Ther. 2021, 26, 659–668. [Google Scholar] [CrossRef]
- Majumdar, A.; Shah, M.R.; Park, J.J.; Narayanan, N.; Kaye, K.S.; Bhatt, P.J. Challenges and Opportunities in Antimicrobial Stewardship among Hematopoietic Stem Cell Transplant and Oncology Patients. Antibiotics 2023, 12, 592. [Google Scholar] [CrossRef]
- Wu, S.C.; Liang, C.X.; Zhang, Y.L.; Hu, W.P. Elevated serum procalcitonin level in patients with chronic kidney disease without infection: A case-control study. J. Clin. Lab. Anal. 2020, 34, e23065. [Google Scholar] [CrossRef]
- Dornbusch, H.J.; Strenger, V.; Sovinz, P.; Lackner, H.; Schwinger, W.; Kerbl, R.; Urban, C. Non-infectious causes of elevated procalcitonin and C-reactive protein serum levels in pediatric patients with hematologic and oncologic disorders. Support. Care Cancer 2008, 16, 1035–1040. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.B. Factors impacting on the problem of antibiotic resistance. J. Antimicrob. Chemother. 2002, 49, 25–30. [Google Scholar] [CrossRef]
- Dellit, T.H.; Owens, R.C.; McGowan, J.E.; Gerding, D.N.; Weinstein, R.A.; Burke, J.P.; Huskins, W.C.; Paterson, D.L.; Fishman, N.O.; Carpenter, C.F.; et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. CliClin. Infect. Dis. 2007, 44, 159–177. [Google Scholar] [CrossRef]
- Kopsidas, I.; Vergnano, S.; Spyridis, N.; Zaoutis, T.; Patel, S. A Survey on National Pediatric Antibiotic Stewardship Programs, Networks and Guidelines in 23 European Countries. Pediatr. Infect. Dis. J. 2020, 39, E359–E362. [Google Scholar] [CrossRef] [PubMed]
- Donà, D.; Barbieri, E.; Daverio, M.; Lundin, R.; Giaquinto, C.; Zaoutis, T.; Sharland, M. Implementation and impact of pediatric antimicrobial stewardship programs: A systematic scoping review. Antimicrob. Resist. Infect. Control. 2020, 9, 1–12. [Google Scholar] [CrossRef]
- Karanika, S.; Paudel, S.; Grigoras, C.; Kalbasi, A.; Mylonakis, E. Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital-based antimicrobial stewardship programs. Antimicrob. Agents Chemother. 2016, 60, 4840–4852. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.R.; Bagga, B.; Arnold, S.R. Reduction of broad-spectrum antimicrobial use in a tertiary children s hospital post antimicrobial stewardship program guideline implementation. Pediatr. Crit. Care Med. 2016, 17, 187–193. [Google Scholar] [CrossRef]
- Haque, A.; Hussain, K.; Ibrahim, R.; Abbas, Q.; Ahmed, S.A.; Jurair, H.; Ali, S.A. Impact of pharmacist-led antibiotic stewardship program in a PICU of low/ middle-income country. BMJ Open Qual. 2018, 7, 2017–2019. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, Y.; Suwa, J.; Higuchi, H.; Fukuoka, K.; Furuichi, M.; Kaneko, T.; Morikawa, Y.; Okazaki, K.; Shimizu, N.; Horikoshi, Y. Antimicrobial Stewardship Program in a Pediatric Intensive Care Unit. J. Pediatr. Infect Dis. Soc. 2018, 7, E156–E159. [Google Scholar] [CrossRef]
- Adams, S.M.; Ngo, L.; Morphew, T.; Babbitt, C.J. Does an Antimicrobial Time-Out Impact the Duration of Therapy of Antimicrobials in the PICU? Pediatr. Crit. Care Med. 2019, 20, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.S.; Isaac, R.E.; Price, K.L.; Plunkett, A.C. Impact of Positive Feedback on Antimicrobial Stewardship in a Pediatric Intensive Care Unit: A Quality Improvement Project. Pediatr. Qual. Saf. 2019, 4, E206. [Google Scholar] [CrossRef] [PubMed]
- Wassef, M.A.A.; Sayed, A.M.; Aziz, H.S.A.; Meligy, B.; Halim, M.M.A. Implementation and evaluation of antimicrobial stewardship program in medical icu in cairo university specialized pediatric hospital. Open Access Maced. J. Med. Sci. 2020, 8, 716–722. [Google Scholar] [CrossRef]
- Renk, H.; Sarmisak, E.; Spott, C.; Kumpf, M.; Hofbeck, M.; Hölzl, F. Antibiotic stewardship in the PICU: Impact of ward rounds led by paediatric infectious diseases specialists on antibiotic consumption. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Aljassim, N.A.; Noël, K.C.; Maratta, C.; Tam, I.M.; Almadani, A.; Papenburg, J.M.; Quach, C.M.; Thampi, N.M.; McNally, J.D.; Dendukuri, N.; et al. Antimicrobial Stewardship in Bronchiolitis: A Retrospective Cohort Study of Three PICUs in Canada. Pediatr. Crit. Care Med. 2022, 23, 160–170. [Google Scholar] [CrossRef]
- Kit-Anan, W.; Boonsathorn, S.; Anantasit, N.; Techasaensiri, C.; Chaisavaneeyakorn, S.; Apiwattanakul, N. Handshake stewardship reduces carbapenem prescription in a pediatric critical care setting. Pediatr. Int. 2022, 64, e15227. [Google Scholar] [CrossRef] [PubMed]
- da Silva, B.B.O.; de Menezes, F.G.; Silva, M.; Troster, E.J. The impact of monitoring software on antimicrobial management in a pediatric intensive care unit. Am. J. Infect. Control. 2022, 50, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.; Yang, M.; Mao, Y.; Fang, B.; He, Y.; Li, R.; Qian, S. Effect of Antimicrobial Stewardship 2018 on severe pneumonia with bacterial infection in paediatric intensive care units. J. Glob. Antimicrob. Resist. 2023, 36, 444–452. [Google Scholar] [CrossRef]
- Alfraij, A.; Abdelmoniem, A.; Elseadawy, M.; Surour, M.; Basuni, M.; Papenburg, J.; Alghounaim, M. The effect of Telehealth Antimicrobial Stewardship Program (Tele-ASP) on antimicrobial use in a pediatric intensive care unit: Pre- and post-implementation single center study. J. Infect. Public Health 2023, 16, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Zombori, L.; Paulus, S.; Shah, M.A.; McGarrity, O.; Hatcher, J. Antibiotic spectrum index as an antimicrobial stewardship tool in paediatric intensive care settings. Int. J. Antimicrob. Agents 2023, 61, 106710. [Google Scholar] [CrossRef] [PubMed]
- Downes, K.J.; Weiss, S.L.; Gerber, J.S.; Klieger, S.B.; Fitzgerald, J.C.; Balamuth, F.; Kubis, S.E.; Tolomeo, P.; Bilker, W.B.; Han, X.; et al. A pragmatic biomarker-driven algorithm to guide antibiotic use in the pediatric intensive care unit: The optimizing antibiotic strategies in sepsis (OASIS) study. J. Pediatr. Infect. Dis. Soc. 2017, 6, 134–141. [Google Scholar] [CrossRef][Green Version]
- Katz, S.E.; Crook, J.; Gillon, J.; Stanford, J.E.M.; Wang, L.; Colby, J.M.; Banerjee, R. Use of a Procalcitonin-guided Antibiotic Treatment Algorithm in the Pediatric Intensive Care Unit. Pediatr. Infect. Dis. J. 2021, 40, 333–337. [Google Scholar] [CrossRef]
- Wagner, M.E.; Hale, C.M.; Ericson, J.E.; Trout, L.C. Real-world application of a procalcitonin monitoring protocol in a pediatric intensive care unit. J. Pediatr. Pharmacol. Ther. 2021, 26, 603–607. [Google Scholar] [CrossRef]
- Yoshida, K.; Hatachi, T.; Okamoto, Y.; Aoki, Y.; Kyogoku, M.; Miyashita, K.M.; Inata, Y.; Shimizu, Y.; Fujiwara, F.B.; Takeuchi, M. Application of multiplex polymerase chain reaction for pathogen identification and antibiotic use in children with respiratory infections in a picu. Pediatr. Crit. Care Med. 2021, 22, E644–E648. [Google Scholar] [CrossRef]
- Brotons, P.; Villaronga, M.; Henares, D.; Armero, G.; Launes, C.; Jordan, I.; Muñoz-Almagro, C. Clinical impact of rapid viral respiratory panel testing on pediatric critical care of patients with acute lower respiratory infection. Enferm. Infecc. Microbiol. Clin. 2022, 40, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Northway, T.; Langley, J.M.; Skippen, P. Health Care–Associated Infection in the Pediatric Intensive Care Unit: Epidemiology and Control—Keeping Patients Safe. Pediatr. Crit. Care 2011, 29, 1349. [Google Scholar] [CrossRef]
- Ista, E.; van der Hoven, B.; Kornelisse, R.F.; van der Starre, C.; Vos, M.C.; Boersma, E.; Helder, O.K. Eff ectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: A systematic review and meta-analysis. Lancet Infect Dis. 2016, 16, 724–734. [Google Scholar] [CrossRef]
- Newland, J.G.; Hersh, A.L. Purpose and design of antimicrobial stewardship programs in pediatrics. Pediatr. Infect. Dis. J. 2010, 29, 862–863. [Google Scholar] [CrossRef] [PubMed]
- Boracchini, R.; Brigadoi, G.; Barbieri, E.; Liberati, C.; Rossin, S.; Tesser, F.; Chiusaroli, L.; Demarin, G.C.; Maestri, L.; Tirelli, F.; et al. Validation of Administrative Data and Timing of Point Prevalence Surveys for Antibiotic Monitoring. JAMA Netw. Open. 2024, 7, e2435127. [Google Scholar] [CrossRef]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Jandoc, R.; Burden, A.M.; Mamdani, M.; Lévesque, L.E.; Cadarette, S.M. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J. Clin. Epidemiol. 2015, 68, 950–956. [Google Scholar] [CrossRef]
- Mo, Y.; Oonsivilai, M.; Lim, C.; Niehus, R.; Cooper, B.S. Implications of reducing antibiotic treatment duration for antimicrobial resistance in hospital settings: A modelling study and meta-analysis. PLoS Med. 2023, 20, 1–20. [Google Scholar] [CrossRef]
- Baer, G.; Baumann, P.; Buettcher, M.; Heininger, U.; Berthet, G.; Schäfer, J.; Bucher, H.C.; Trachsel, D.; Schneider, J.; Gambon, M.; et al. Procalcitonin Guidance to Reduce Antibiotic Treatment of Lower Respiratory Tract Infection in Children and Adolescents (ProPAED): A Randomized Controlled Trial. PLoS ONE 2013, 8, e68419. [Google Scholar] [CrossRef]
- Brigadoi, G.; Gastaldi, A.; Moi, M.; Barbieri, E.; Rossin, S.; Biffi, A.; Cantarutti, A.; Giaquinto, C.; Da Dalt, L.; Donà, D. Point-of-Care and Rapid Tests for the Etiological Diagnosis of Respiratory Tract Infections in Children: A Systematic Review and Meta-Analysis. Antibiotics 2022, 11, 1192. [Google Scholar] [CrossRef] [PubMed]
- Sick-Samuels, A.C.; Woods-Hill, C. Diagnostic Stewardship in the Pediatric Intensive Care Unit. Infect. Dis. Clin. N. Am. 2022, 36, 203–218. [Google Scholar] [CrossRef] [PubMed]
- Woods-Hill, C.Z.; Koontz, D.W.; King, A.F.; Voskertchian, A.; Colantuoni, E.A.; Miller, M.R.; Fackler, J.C.; Bonafide, C.P.; Milstone, A.M.; Xie, A. Practices, Perceptions, and Attitudes in the Evaluation of Critically Ill Children for Bacteremia: A National Survey. Pediatr. Crit. Care Med. 2020, 21, E23–E29. [Google Scholar] [CrossRef]
- Woods-Hill, C.Z.; Lee, L.; Xie, A.; King, A.F.; Voskertchian, A.; Klaus, S.A.; Smith, M.M.; Miller, M.R.; Colantuoni, E.A.; Fackler, J.C.; et al. Dissemination of a Novel Framework to Improve Blood Culture Use in Pediatric Critical Care. Pediatr. Qual. Saf. 2018, 3, e112. [Google Scholar] [CrossRef]
- Ormsby, J.B.; Conrad, P.M.; Blumenthal, J.; Carpenter, J.; Jones, S.; Sandora, T.J.; Vaughan, A.; Vincuilla, J.B.; McAdam, A.J.; Fogg, L.F.; et al. Practice Improvement for Standardized Evaluation and Management of Acute Tracheitis in Mechanically Ventilated Children. Pediatr. Qual. Saf. 2020, 6, E368. [Google Scholar] [CrossRef]
- Sick-Samuels, A.C.; Linz, M.; Bergmann, J.; Fackler, J.C.; Berenholtz, S.M.; Ralston, S.L.; Hoops, K.; Dwyer, J.; Colantuoni, E.; Milstone, A.M. Diagnostic Stewardship of Endotracheal Aspirate Cultures in a PICU. Pediatrics 2021, 147, e20201634. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liberati, C.; Brigadoi, G.; Barbieri, E.; Giaquinto, C.; Donà, D. Antimicrobial Stewardship Programs in Pediatric Intensive Care Units: A Systematic Scoping Review. Antibiotics 2025, 14, 130. https://doi.org/10.3390/antibiotics14020130
Liberati C, Brigadoi G, Barbieri E, Giaquinto C, Donà D. Antimicrobial Stewardship Programs in Pediatric Intensive Care Units: A Systematic Scoping Review. Antibiotics. 2025; 14(2):130. https://doi.org/10.3390/antibiotics14020130
Chicago/Turabian StyleLiberati, Cecilia, Giulia Brigadoi, Elisa Barbieri, Carlo Giaquinto, and Daniele Donà. 2025. "Antimicrobial Stewardship Programs in Pediatric Intensive Care Units: A Systematic Scoping Review" Antibiotics 14, no. 2: 130. https://doi.org/10.3390/antibiotics14020130
APA StyleLiberati, C., Brigadoi, G., Barbieri, E., Giaquinto, C., & Donà, D. (2025). Antimicrobial Stewardship Programs in Pediatric Intensive Care Units: A Systematic Scoping Review. Antibiotics, 14(2), 130. https://doi.org/10.3390/antibiotics14020130






