1. Introduction
On 11 March 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a global pandemic, resulting in substantial worldwide mortality. On 5 May 2023, WHO announced that COVID-19 no longer constituted a public health emergency of international concern. Parallel to the COVID-19 pandemic, Europe has faced a “silent” but equally serious pandemic of antimicrobial resistance (AMR), largely driven by excessive and inappropriate antibiotic use. Most antibiotics in Europe are consumed in the community, particularly in primary care. The convergence of COVID-19 and AMR intensified existing weaknesses in infection control and antimicrobial stewardship. Despite the viral etiology of COVID-19, antibiotic prescribing increased in the United States, often motivated by concerns about bacterial coinfections. By contrast, data from the European Union (EU) suggest the opposite trend, with outpatient antibiotic prescribing declining in 2019–2020. Factors such as altered transmission dynamics, changes in healthcare-seeking behavior, modified prescribing practices, and reduced incidence of non-COVID-19 respiratory infections likely contributed. In hospitals, however, overall antibiotic consumption decreased in 2020–2021, while the use of broad-spectrum and last-line agents markedly increased. More than 60% of COVID-19 patients with confirmed bacterial infections harbored resistant isolates [
1,
2].
The Centers for Disease Control and Prevention (CDC) analyzed the pandemic’s impact on AMR in the United States. Between 2012 and 2017, AMR-related deaths declined by 18%. This trend reversed with the pandemic: in 2020, nosocomial AMR infections and associated deaths rose by 15% compared with 2019. Over 29,400 individuals died from AMR infections in the first pandemic year, nearly 40% acquired during hospitalization. Approximately 80% of hospitalized COVID-19 patients received antibiotics between March and October 2020, despite the absence of bacterial infection. The pandemic disrupted AMR surveillance, with CDC lacking data for 9 of 18 priority pathogens, likely underestimating the true burden. Overcrowded hospitals, prolonged hospitalizations, and increased invasive procedures (e.g., ventilation, catheterization) elevated infection risk. Shortages of protective equipment, reduced staffing, and supply chain disruptions hindered infection prevention. Prioritization of COVID-19 testing and treatment delayed diagnosis of multi-drug resistant (MDR) infections. Notably, carbapenem-resistant Acinetobacter baumannii (CR-AB) infections increased by 78% in 2020 compared with 2019, Candida auris by 60%, and other Candida species by 26%. The pandemic compromised CDC strategies in three domains:
After 2020, the pandemic profoundly affected outpatient prescribing, infection control, and resource allocation, influencing AMR trends. Several studies suggest accelerated dissemination of extended-spectrum β-lactamase (ESBL)-producing
Enterobacterales and carbapenem-resistant
Enterobacterales (CRE) [
4]. Approximately 75% of COVID-19 patients received antibiotics, though <10% had confirmed bacterial co-infections [
5]. Such overuse exacerbates AMR. The absence of antimicrobial stewardship programs (ASPs) was linked to increased resistance in Gram-negative bacteria. CDC reported a 15% rise in resistant infections, including CR-AB, methicillin-resistant
Staphylococcus aureus (MRSA), and CRE, underscoring the need for improved monitoring and prevention [
6].
Trends in Gram-positive resistance remained relatively stable. Meta-analyses showed no significant change in MRSA or vancomycin-resistant
Enterococcus (VRE). In contrast, Gram-negative AMR rose sharply. The pooled incidence of resistant Gram-negative organisms –including ESBL-producing
Enterobacterales, CRE, carbapenem-resistant
P. aeruginosa (CR-PA), and CR-AB—was 1.64 (95% CI: 0.92–2.92), with a relative risk (RR) of 1.08 (95% CI: 0.91–1.29). Lack of ASPs was associated with further increases, with RR 1.11 (95% CI: 1.03–1.20), highlighting antibiotic selective pressure and nosocomial transmission [
4].
Several factors shaped AMR trends. Initial pandemic measures—hand hygiene, distancing, restricted facility access—may have temporarily reduced AMR, especially in 2020. However, disruption of infection control and ASPs likely offset these gains. Overuse of broad-spectrum antibiotics, particularly β-lactams, created selective pressure favoring resistant Gram-negative organisms [
7,
8].
Our study investigated the impact of the COVID-19 pandemic and ward repurposing on hospitalization dynamics, antibiotic consumption, and resistance trends of Klebsiella sp., Acinetobacter sp., and P. aeruginosa at the Louis Pasteur University Hospital in Košice between 2018 and 2024. By comparing COVID-19 and non-COVID-19 units across pre-pandemic, pandemic, and post-pandemic periods, we aimed to assess how healthcare restructuring and shifts in antibiotic use influenced resistance epidemiology in a tertiary care setting.
2. Results
2.1. Hospitalization Trends
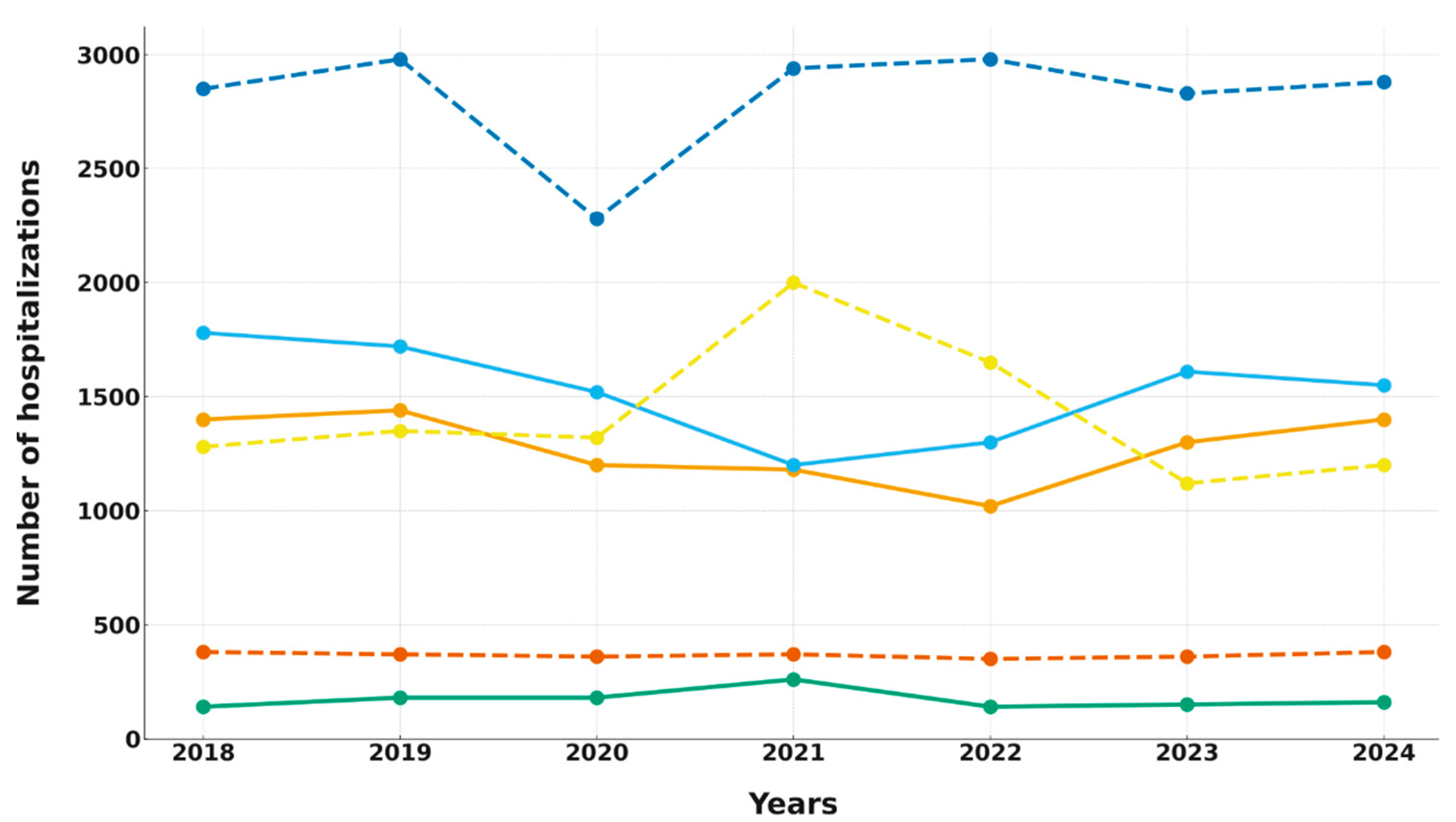
Hospitalization dynamics from 2018 to 2024 exhibited distinct patterns, reflecting the influence of the COVID-19 pandemic and the repurposing of bed capacity.
In the COVID-19 units (4th DIM and 2nd DS), hospitalization numbers remained stable during the pre-pandemic period (2018–2019). However, beginning in 2020, a notable decline occurred, reaching the lowest point in 2021 (approximately 1200 hospitalizations). This decrease was statistically significant according to both linear regression and correlation analyses (
Table 1). In the following years, hospitalization numbers gradually returned to pre-pandemic levels.
In CAIC, a temporary surge in hospitalizations was observed in 2021 during the Delta wave, with an increase of about 40% compared to previous years. This was followed by stabilization at pre-pandemic levels (around 140–150 hospitalizations annually), with no significant long-term trend detected (
Table 1 and
Figure 1).
The non-COVID-19 units displayed a different pattern. The 1st DIM experienced a temporary rise in hospitalizations in 2021 due to patient transfers from repurposed wards. The 1st DS showed a brief decline in 2020, followed by a recovery to approximately 2900 hospitalizations annually. DAIC maintained stable hospitalization numbers (342–379 annually), indicating minimal disruption related to the pandemic. Statistical analyses did not reveal significant long-term trends in these units (
Table 1).
In summary, only the COVID-19 units (4th DIM and 2nd DS) demonstrated a statistically significant decline in hospitalizations, while CAIC and the non-COVID-19 departments (1st DIM, 1st DS, DAIC) experienced only temporary, non-significant fluctuations. These findings highlight the heterogeneous effects of the pandemic and ward repurposing on hospitalization patterns.
2.2. Comparison of Pathogen Occurrence Across Departments and Trends over Time
The analysis of pathogen occurrence between 2018 and 2024 revealed clear contrasts between COVID-19 and non-COVID-19 units, although most interdepartmental differences did not reach statistical significance.
When comparing paired departments (4th DIM vs. 1st DIM; 2nd DS vs. 1st DS; CAIC vs. DAIC), no significant differences in pathogen occurrence were confirmed by the Wilcoxon test (all p = 0.25), likely due to the limited number of evaluated periods and high variability of data, particularly in the CAIC.
Nevertheless, numerical disparities were apparent. Among surgical departments, the 2nd DS consistently showed higher occurrence of all evaluated pathogens compared with the 1st DS (e.g., P. aeruginosa 10.7–6.8 vs. 2.1–3.3 isolates per 100 patients). Similarly, in intensive care departments, pathogen occurrence was markedly higher in the CAIC (Acinetobacter sp. 133.9–28.1/100 patients) than in the DAIC (17.6–10.4/100 patients), although without statistical significance.
Significant results were observed mainly in the time-series analysis. Decreasing trends were identified for
Acinetobacter sp. in the 4th DIM and CAIC, for
Klebsiella sp. in the 1st and 4th DIM, and for
P. aeruginosa in the 2nd DS (
Table 2).
In summary, despite evident numerical differences—particularly between the CAIC and DAIC, and between the 2nd DS and 1st DS—statistical testing did not confirm significant interdepartmental differences in pathogen occurrence. By contrast, time-series analysis revealed several significant decreasing trends, mainly in internal medicine and surgical COVID-19 units as well as in the CAIC.
2.3. Comparison of Pathogen Occurrence During the Pandemic (2020–2022) Between COVID-19 and Non-COVID-19 Units
The analysis of ward repurposing during the pandemic period (2020–2022) demonstrated that the occurrence of nosocomial pathogens was consistently and significantly higher in COVID-19 units compared with non-COVID-19 units. The most pronounced differences were observed for Acinetobacter sp., which showed a markedly higher proportion of positive clinical samples in COVID-19 units across all evaluated years. The same pattern was evident for Klebsiella sp., where the proportion of positive isolates was consistently almost twice as high in COVID-19 units compared with non-COVID-19 units. For P. aeruginosa, differences were less pronounced but remained consistent throughout the pandemic period, with higher rates in COVID-19 units across all three years analyzed.
Overall, the results confirmed a significantly greater occurrence of all three pathogens in COVID-19 units during 2020–2022 (
Table 3).
2.4. Resistance Trends of Klebsiella sp. in COVID-19 vs. Non-COVID-19 Units
The analysis of
Klebsiella sp. resistance across internal medicine, surgical, and intensive care units between 2018 and 2024 revealed marked differences between COVID-19 and non-COVID-19 units, along with dynamic changes during the pandemic (
Table 4).
In the 4th DIM, resistance to cephalosporins and fluoroquinolones showed a declining trend, while resistance to β-lactam/β-lactamase inhibitor combinations and carbapenems increased during the pandemic and remained elevated thereafter. The 1st DIM followed a similar pattern, with decreasing resistance to gentamicin and ciprofloxacin but rising resistance to ertapenem, which appeared during the pandemic and persisted in the post-pandemic years.
In the 2nd DS, the pandemic period was associated with a sharp increase in resistance across multiple antibiotic classes, particularly cephalosporins, β-lactam/β-lactamase inhibitor combinations, and carbapenems. Post-pandemic data indicated partial declines; however, resistance to ertapenem and cefoperazone/sulbactam combinations remained significantly higher than pre-pandemic levels. The 1st DS exhibited temporary reductions in cephalosporin and gentamicin resistance during the pandemic, followed by a rebound, thereafter, accompanied by a transient rise in amikacin resistance.
The CAIC displayed the highest resistance rates overall, with pre-pandemic values for cephalosporins and ciprofloxacin exceeding 70%. Although partial post-pandemic declines were observed, resistance remained high. A notable and consistent decrease was recorded for gentamicin. In contrast, the DAIC maintained lower baseline resistance levels but demonstrated increasing trends for piperacillin/tazobactam, cefoperazone/sulbactam, and carbapenems, while gentamicin resistance declined.
Overall,
Klebsiella sp. resistance to cephalosporins and fluoroquinolones was higher in COVID-19 units, whereas the pandemic period was characterized by a substantial rise in resistance to β-lactam/β-lactamase inhibitor combinations and carbapenems. These increases were only partially reversed post-pandemically, while gentamicin resistance declined consistently across all unit types (
Table 4).
2.5. Resistance Trends of Acinetobacter sp. in COVID-19 vs. Non-COVID-19 Units
The analysis of
Acinetobacter sp. resistance across internal medicine, surgical, and intensive care units between 2018 and 2024 demonstrated persistently high resistance rates across most departments, with clear differences between COVID-19 and non-COVID-19 units (
Table 5).
In the 4th DIM, resistance remained consistently high for most antibiotics, including piperacillin/tazobactam and ceftazidime, with no statistically significant trends identified. In contrast, the 1st DIM exhibited a significant increase in ampicillin/sulbactam resistance during and after the pandemic.
Among surgical units, the 2nd DS showed extremely high resistance levels across nearly all antibiotics, accompanied by a significant rise in ampicillin/sulbactam resistance during the pandemic period. The 1st DS displayed a variable pattern, with resistance decreasing before the pandemic, then rising and stabilizing at high levels thereafter. A statistically significant increase in ampicillin/sulbactam resistance was confirmed in this unit as well.
The highest resistance levels were observed in the intensive care units. The CAIC exhibited exceptionally high resistance across all antibiotics, often exceeding 90%, but significant post-pandemic decreases were observed for ceftazidime and gentamicin, while ciprofloxacin resistance showed a borderline decline. In contrast, the DAIC maintained high but relatively stable resistance rates, with significant upward trends in ampicillin/sulbactam, gentamicin, and amikacin resistance.
In summary,
Acinetobacter sp. demonstrated persistently high resistance across all departments, with partial post-pandemic improvements in the CAIC, but increasing ampicillin/sulbactam resistance across multiple units. Statistically significant trends included decreasing ceftazidime and gentamicin resistance in the CAIC, contrasted by rising ampicillin/sulbactam resistance in several other departments (
Table 5).
2.6. Resistance Trends of P. aeruginosa in COVID-19 vs. Non-COVID-19 Units
Across internal medicine, surgical, and intensive care units between 2018 and 2024,
P. aeruginosa resistance generally displayed a declining trend, particularly for β-lactams and ciprofloxacin, although the magnitude varied by department type (
Table 6).
In the 4th DIM, resistance remained largely stable without statistically significant changes, despite numerical decreases across most antibiotic classes. In the 1st DIM, significant reductions were observed for ciprofloxacin, cefepime, and gentamicin, indicating a gradual improvement in susceptibility during and after the pandemic.
Among surgical units, the 2nd DS exhibited significant decreases in resistance to multiple β-lactams, including cefepime, ceftazidime, and piperacillin/tazobactam, as well as to gentamicin and ciprofloxacin. In contrast, the 1st DS showed only non-significant numerical reductions across most antibiotics.
The most pronounced changes were recorded in intensive care. In the CAIC, marked and statistically significant declines were documented for piperacillin/tazobactam, cefepime, gentamicin, and ciprofloxacin, indicating a broad reduction in multidrug resistance. Similarly, the DAIC (non-COVID-19 unit) showed significant downward trends for cefepime, imipenem, gentamicin, and ciprofloxacin, confirming improved antimicrobial susceptibility patterns over time.
Across all departments, ciprofloxacin remained the most problematic agent, with resistance frequently exceeding 35–45%, although significant decreases were confirmed in several units. In contrast, amikacin consistently maintained the lowest resistance, while colistin resistance was virtually absent throughout the entire study period.
Overall,
P. aeruginosa resistance across the monitored departments demonstrated a consistent downward trend between 2018 and 2024, particularly for cephalosporins, carbapenems, and aminoglycosides. The most significant reductions were recorded in COVID-19 units (CAIC, 2nd DS) and, to a lesser extent, in non-COVID-19 units (1st DIM, DAIC). These findings indicate progressive improvements in the epidemiological situation, with intensive care units showing the most dynamic and statistically supported declines (
Table 6).
2.7. Trends in Pathogen-Specific Resistance Mechanisms
The evaluation of resistance mechanisms demonstrated distinct patterns between COVID-19 and non-COVID-19 units, characterized by several significant, pathogen-specific alterations observed throughout the pandemic period.
For Klebsiella sp., ESBL prevalence declined significantly in both settings, more markedly in COVID-19 units, while carbapenemase/MBL production increased in parallel, indicating a shift from ESBL towards more advanced resistance mechanisms. Inter-unit comparison confirmed significant differences: narrow-spectrum β-lactamase production was more prevalent in non-COVID-19 units, whereas carbapenemase/MBL production, aminoglycoside resistance, and multidrug resistance occurred more frequently in COVID-19 wards.
For Acinetobacter sp., there were no significant changes over time in the rates of carbapenem or multidrug resistance between 2018 and 2022. Nevertheless, both resistance mechanisms remained significantly more common in COVID-19 units, underscoring a more severe and persistent epidemiological challenge in these wards.
For P. aeruginosa, COVID-19 units exhibited significant downward trends across multiple mechanisms, including efflux-porin alterations, carbapenemase/MBL production, carbapenem resistance, and multidrug resistance. Non-COVID-19 units also showed significant reductions in carbapenem and multidrug resistance. Despite these improvements, the overall prevalence of all monitored mechanisms remained higher in COVID-19 units.
In summary, the pandemic period was associated with distinct pathogen-specific shifts:
Klebsiella sp. transitioned from ESBL to carbapenemase dominance,
P. aeruginosa demonstrated broad reductions across resistance mechanisms, and
Acinetobacter sp. maintained persistently high resistance levels with consistently greater prevalence in COVID-19 units (
Table 7).
2.8. Antibiotic Consumption Trends Between COVID-19 and Non-COVID-19 Units
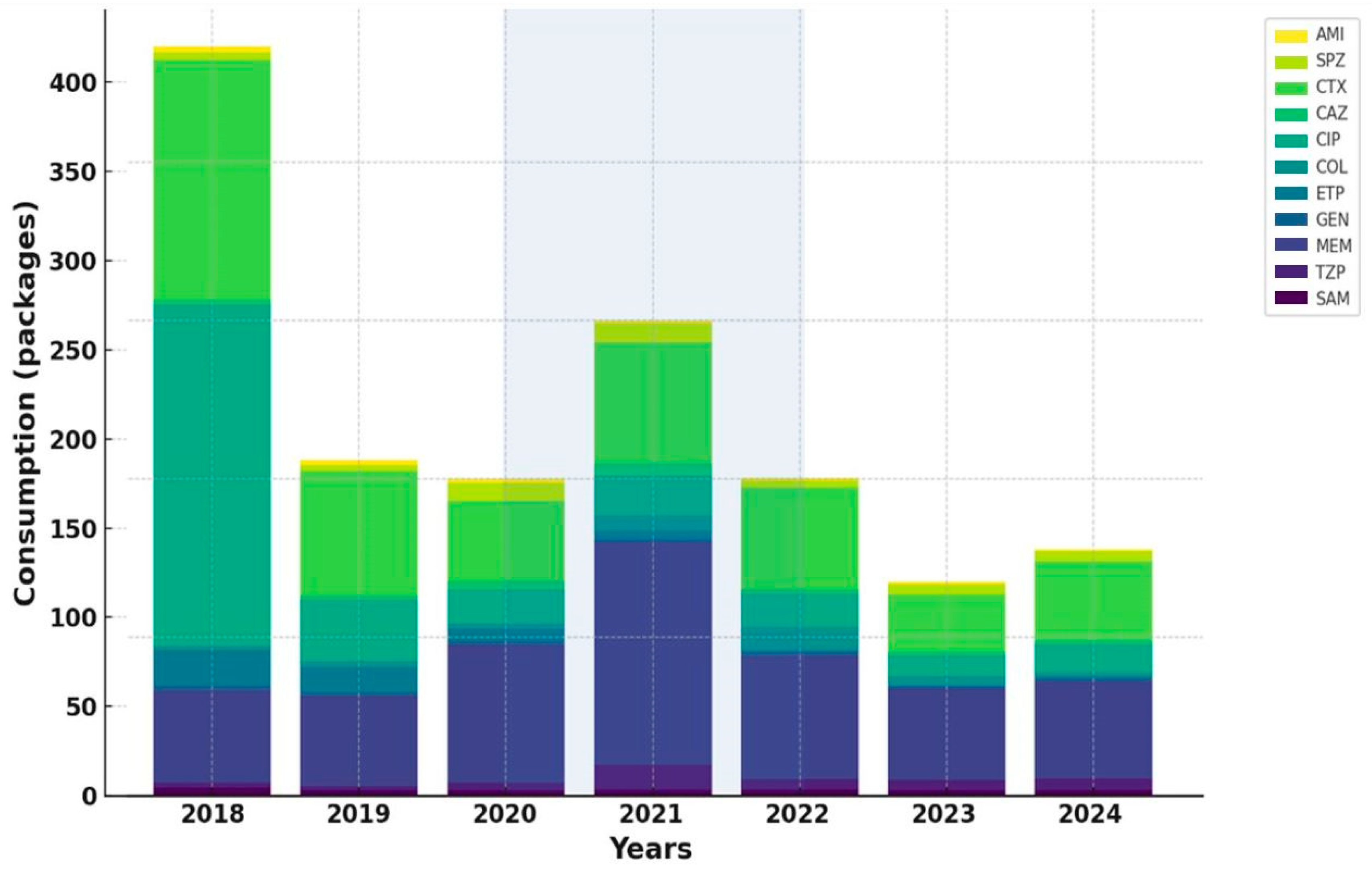
The analysis of standardized antibiotic consumption per 100 hospitalizations revealed substantial differences between COVID-19 and non-COVID-19 units, with overall use markedly higher in COVID-19 wards.
During the pandemic period, the most pronounced increases were recorded for broad-spectrum β-lactam/β-lactamase inhibitor combinations, particularly piperacillin/tazobactam and cefoperazone/sulbactam, both showing sharp surges in 2020–2021, especially in COVID-19 units.
In contrast, aminoglycoside consumption demonstrated a steady decline in both settings, most notably for amikacin, while gentamicin remained relatively stable but trended downward in COVID-19 units after 2020.
Among carbapenems, meropenem displayed the most striking pattern, with a dramatic surge during the pandemic in COVID-19 units, followed by a gradual post-pandemic decline. Imipenem and ertapenem both showed decreasing utilization over time, more pronounced in COVID-19 wards.
Within cephalosporins, ceftriaxone consumption remained consistently higher in COVID-19 units throughout the study period, exceeding levels observed in non-COVID-19 units more than twofold. Conversely, ciprofloxacin use decreased sharply across all units, reflecting a sustained decline in fluoroquinolone prescribing.
The most notable post-pandemic increase was observed for colistin, whose consumption rose substantially in 2022, particularly in COVID-19 units, indicating more frequent use as a last-line option against multidrug-resistant pathogens.
Overall, antibiotic consumption patterns mirrored the epidemiological dynamics observed during the pandemic, characterized by intensified use of broad-spectrum β-lactams and carbapenems in COVID-19 units, followed by gradual post-pandemic normalization and selective increase in last-resort agents (
Figure 2 and
Figure 3).
2.9. Correlation Between Antibiotic Consumption and Resistance Mechanisms
The analysis of correlations between antibiotic consumption and the prevalence of major resistance mechanisms in Klebsiella sp. demonstrated that changes in antibiotic use were directly associated with shifts in resistance, particularly during the pandemic period.
In both COVID-19 and non-COVID-19 units, declining use of ceftriaxone and ciprofloxacin was accompanied by a marked reduction in ESBL prevalence. A significant positive correlation was confirmed between ciprofloxacin consumption and ESBL occurrence, whereas no association was observed for ceftriaxone. In contrast, increased meropenem consumption coincided with a rise in carbapenemase-mediated resistance, showing a borderline-significant trend in COVID-19 units and a non-significant association in non-COVID-19 units.
For Acinetobacter sp., correlations were not assessed due to the absence of significant resistance mechanism trends, and no significant associations were identified between antibiotic consumption and resistance mechanisms in P. aeruginosa.
Overall, the most pronounced and statistically supported association was observed between declining ciprofloxacin consumption and the reduction of ESBL resistance in
Klebsiella sp. across both COVID-19 and non-COVID-19 units. Additionally, COVID-19 wards demonstrated a near-significant trend linking increased meropenem consumption with rising carbapenemase resistance (
Table 8).
2.10. Comparison of Clinical Applicability of Antibiotics Between COVID-19 and Non-COVID-19 Units
Non-COVID-19 departments retained a broader range of effective antibiotics against Klebsiella sp. and P. aeruginosa, whereas therapeutic options in COVID-19 units—particularly in the CAIC and 2nd DS—were markedly restricted.
For Klebsiella sp., non-COVID-19 units (1st DIM, 1st DS, DAIC) preserved up to seven effective antibiotics, while COVID-19 units CAIC and 2nd DS were limited to colistin as the only viable option. The 4th DIM maintained six active agents.
For Acinetobacter sp., the situation was critical across all units, with colistin being the sole effective antibiotic, highlighting extensive multidrug resistance.
For
P. aeruginosa, differences were most pronounced: non-COVID-19 units (1st DIM, 1st DS) retained up to ten antibiotics with resistance below 20%, whereas DAIC and COVID-19 units (CAIC, 2nd DS) were limited to four. The 4th DIM was an exception among COVID-19 wards, maintaining ten usable antibiotics—comparable to non-COVID-19 units (
Figure 4).
Among individual agents, ceftriaxone, ciprofloxacin, and gentamicin were clinically unusable in most settings, with resistance exceeding 20%. Piperacillin/tazobactam, cefoperazone/sulbactam, and meropenem remained effective mainly in non-COVID-19 units but had already lost reliability in CAIC and 2nd DS. Amikacin preserved activity against Klebsiella sp. and partly against P. aeruginosa in non-COVID-19 units, though it was ineffective against Acinetobacter sp. Ciprofloxacin showed resistance consistently above 20% across all pathogens and units, rendering it clinically obsolete.
Overall, COVID-19 units were disproportionately burdened with multidrug-resistant strains, leaving only limited therapeutic options, while non-COVID-19 departments preserved broader antibiotic efficacy and greater flexibility in empirical and targeted therapy.
3. Discussion
The pandemic unevenly affected hospital operations across COVID-19 and non-COVID-19 units (2018–2024). COVID-19 wards (4th DIM, 2nd DS) maintained stable admissions in 2018–2019, followed by a ≈30% decline in 2020–2021, consistent with international data showing a 20–50% drop in elective care and with nationwide restrictions on non-urgent procedures, such as those implemented in Canada from March 2020 [
9,
10,
11,
12]. Hospitalisations gradually recovered from 2022, approaching pre-pandemic levels by 2023–2024, though Canadian studies still noted a 10–15% deficit [
12]. In contrast, the CAIC reported a >40% surge in 2021, reflecting the global rise in intensive care demand, comparable to pandemic epicentres where ICU capacity expanded by >50%, and up to 80% of ICU beds in Italy were occupied by COVID-19 patients during the first wave [
13,
14].
Non-COVID-19 units were mainly influenced by patient-flow redistribution and compensatory transfers. The 1st DIM showed a 50% rise in 2021, consistent with the hub-and-spoke reallocation model [
11,
14]. The 1st DS rebounded from a transient 2020 decline, stabilising near 2900 annual admissions. The DAIC remained stable, indicating minimal disruption and a supporting role similar to other ICUs [
15]. Overall, COVID-19 units experienced marked but transient declines, whereas non-COVID-19 units were relatively stable. The convergence of long-term volumes between 4th and 1st DIM suggests these disparities were limited to the pandemic period, with remaining differences among surgical and intensive care units likely reflecting patient acuity, referral patterns, and capacity rather than the pandemic itself.
Comparative analysis of
Klebsiella sp.,
Acinetobacter sp., and
P. aeruginosa across departments revealed numerical differences, with higher isolation rates in the 2nd DS versus 1st DS, and greater values in the CAIC than in the DAIC, although none reached statistical significance. These findings correspond with the recognised epidemiological burden of surgical and intensive care settings, where mechanical ventilation, prolonged hospitalisation, and extensive broad-spectrum antibiotic exposure promote persistence and spread of multidrug-resistant organisms (MDROs) [
16,
17,
18].
Time-series analysis identified statistically significant declines in pathogen occurrence:
Acinetobacter sp. in the 4th DIM and CAIC,
Klebsiella sp. in both the 1st DIM and 4th DIM, and
P. aeruginosa in the 2nd DS. These trends mirror international data showing decreasing MDRO incidence over the past decade, attributed to reinforced infection prevention, antimicrobial stewardship, and greater awareness [
17,
19]. Despite this decline, MDROs remain a critical challenge in high-acuity environments, particularly in intensive care units.
During the pandemic, COVID-19 units exhibited a markedly higher MDRO burden, most notably for
Acinetobacter sp., which showed a more than sevenfold increase compared with non-COVID-19 units.
Klebsiella sp. and
P. aeruginosa also displayed two- to threefold higher rates across 2020–2022. These findings are consistent with global reports of increased MDRO prevalence in COVID-19 ICUs, where
Acinetobacter sp. predominated. Likely contributors included excessive patient load, frequent invasive ventilation, disruption of infection-prevention measures due to limited resources, and prolonged empirical broad-spectrum therapy for presumed bacterial co-infection [
17].
Before the pandemic,
Klebsiella sp. across departments displayed the expected multifactorial resistance profile. Internal medicine wards reported 40–50% resistance to third-generation cephalosporins (ceftriaxone, ceftazidime), consistent with ≈50% ESBL prevalence, with the 4th DIM trending higher but without significance. Surgical units differed, with 55% resistance in the 2nd DS versus 36% in the 1st DS, reflecting other hospital prevalences often >50% [
20]. During the pandemic, cephalosporin resistance on internal medicine wards fluctuated without significance: resistance in the 2nd DS remained high, whereas the 1st DS declined toward 20%. Literature reports both increases and up to 10% ESBL reductions in specific wards, underscoring local effects of policy and decreased elective activity [
21,
22]. This pattern likely reflects reduced third-generation cephalosporin use, consistent with known associations between lower consumption and attenuated resistance [
23].
According to 2023 ECDC–WHO surveillance,
Klebsiella sp. remains a key resistant pathogen in Europe. Invasive infections have increased since 2019, and carbapenem resistance now exceeds the EU 2030 reduction target. About half of the countries report rates > 50%, highest in southern and eastern Europe, while northern regions show relative stabilisation. Overall, EU/EEA trends indicate continued transmission of carbapenem-resistant
Klebsiella strains [
6].
Intensive care reflected surgical epidemiology: the repurposed CAIC reached ≈70% cephalosporin resistance versus 30% in the DAIC, likely driven by a pre-existing AMR burden and mixed surgical case profiles. Frequent transfers from the repurposed 2nd DS (55% resistance) plausibly maintained transmission, as shown in other studies [
24]. Despite reduced cephalosporin use, persistence via horizontal gene transfer and environmental reservoirs remains likely [
25]. Conversely, the non-repurposed DAIC, epidemiologically linked to the 1st DS (36% resistance), maintained lower rates, supported by steadier stewardship and a more homogeneous patient population [
25].
Carbapenem resistance remains a critical global issue [
26]. During the pandemic, ertapenem resistance rose sharply in the 2nd DS (meropenem stable), with smaller increases in the 1st DS, 4th DIM, and 1st DIM. The CAIC recorded the highest rates, while the DAIC remained lower but increased slightly. Similar surges were reported in Romania, Germany, and China, linked to intensified carbapenem use in COVID-19 wards [
20,
22,
27,
28]. Greater antibiotic pressure in repurposed units likely drove these patterns, as seen with meropenem spikes in Turkey and rising ertapenem resistance in Ireland [
29,
30].
Increasing resistance to β-lactam/β-lactamase inhibitors further limits empiric options [
31]. Piperacillin/tazobactam resistance increased in the 4th DIM, 2nd DS, 1st DIM, and DAIC, indicating that COVID-19 accelerated antimicrobial resistance and that ventilated ICU patients show high rates [
20,
32]. In contrast, Iranian data reported strong post-pandemic piperacillin/tazobactam activity against multidrug-resistant
Klebsiella sp. [
33]. Locally, resistance stabilised in internal medicine wards, decreased in the CAIC, and rose in the DAIC. Cefoperazone/sulbactam resistance also increased, notably in the 2nd DS and DAIC, though Taiwanese studies confirm its activity against ESBL-producing
Klebsiella sp. [
34]. These increases may encourage carbapenem overuse, reinforcing resistance; antibiotic rotation may mitigate this [
35].
Aminoglycosides remain essential for severe
Klebsiella sp. infections [
36]. Globally, resistance rose to ≈23% during the pandemic [
37]. In UNLP, gentamicin resistance averaged ≈40% on repurposed wards (up to ≈70% in the CAIC) versus ≈30% elsewhere, while amikacin resistance stayed low (≈3%). Gentamicin resistance declined significantly in the 4th DIM, CAIC, 1st DIM, and DAIC, opposite to trends in Jordan and Argentina, likely reflecting reduced use and nephrotoxicity concerns [
38,
39,
40]. Persistently low amikacin resistance reflects limited use and fewer enzyme-mediated changes [
41]. Pre-pandemic, resistance was higher in the 2nd DS (14.8%) and CAIC (45.6%), consistent with U.S. data, while non-repurposed units such as the DAIC stayed <10%, similar to Jordanian estimates (11%) [
42,
43]. Only the 1st DS showed a significant post-pandemic rise, possibly due to mobile
aac(6′)-Ib and co-selection with
blaKPC and
qnrB19 [
44].
Fluoroquinolone resistance further constrains therapy [
45]. Pre-pandemic ciprofloxacin resistance was higher in COVID-19 than non-COVID-19 units (46.2% vs. 38.9%). Iranian data show fluctuating
Klebsiella sp. resistance and declines in
P. aeruginosa, whereas other series reported increases peaking in 2020–2021 [
46]. These trends were not observed in our setting, likely reflecting effective local stewardship measures and substantial reductions in ciprofloxacin use [
47]. Persistently high rates in CAIC (~75% pre/in-pandemic) may be consistent with high-risk clones and biofilm-associated persistence [
48,
49,
50,
51]. Given hospital-wide resistance >20%, ciprofloxacin is unsuitable for empiric therapy of nosocomial infections.
Colistin, a last-line option, averaged 10.1% resistance in COVID-19 units vs. 2.4% in non-COVID-19 units pre-pandemic. Both rose during the pandemic (13.5% vs. 3.7%) and declined thereafter but remained higher in COVID-19 wards (8.4% vs. 2.6%). Our values mirror global averages (~3.1%) and the pandemic-era rise (~12.9%) [
52,
53]. Greater increases on repurposed wards likely reflect treatment of superinfections in critically ill patients and frequent isolation of highly resistant
Acinetobacter sp. [
54]. Carbapenemase producers often display higher colistin resistance; in our COVID-19 units, carbapenemase prevalence rose sharply during the pandemic [
55]. Notably, CAIC averaged 18.3%, approaching the 20% threshold at which use of last-line agent becomes uncertain; infections with concurrent carbapenem and colistin resistance are exceptionally challenging given limited alternatives [
56].
Acinetobacter sp. remains one of the most resistant nosocomial pathogens [
57]. Increasing resistance to last-line agents like meropenem and colistin is a critical global challenge [
58]. Ampicillin/sulbactam remains a cornerstone of combination regimens [
59].
According to the latest ECDC–WHO surveillance (2023 data),
Acinetobacter sp. continues to demonstrate the highest levels of antimicrobial resistance among all Gram-negative pathogens in Europe. Nearly half of all invasive isolates are resistant to carbapenems, with the highest rates reported in southern and eastern European countries. Although some western and northern regions have achieved partial declines since 2021, overall resistance remains above 40% across the EU/EEA [
6].
Before the pandemic, mean ampicillin/sulbactam resistance was comparable between COVID-19 and non-COVID-19 units (51.3% vs. 52.2%). Resistance increased in both during the pandemic, slightly higher in non-COVID-19 units, and persisted post-pandemically. These values exceed previous Slovak data, and were generally higher in intensive care settings, reaching 72.1% in CAIC during the pandemic [
60,
61].
Significant increases occurred across multiple departments (DAIC, CAIC, 1st DS, 2nd DS, 1st DIM), indicating a hospital-wide trend. Similar pandemic-era patterns have been described internationally [
62,
63]. Rising ampicillin/sulbactam resistance is concerning as it diminishes its role in synergistic therapy [
63].
The marked rise in ampicillin/sulbactam resistance from 2020 to 2022, without parallel consumption increases, suggests alternative drivers. Clonal analyses demonstrated
blaOXA-23 carriage in Brazilian carbapenem-resistant
Acinetobacter sp. with high genetic similarity [
63]. Similar mechanisms likely underlie concurrent increases in ampicillin/sulbactam and carbapenem resistance here. Pandemic-related ICU overload, weakened infection control, and suboptimal dosing (sulbactam ≥ 9 g/day rarely achieved) probably facilitated the spread of resistant clones independent of antibiotic pressure [
63].
Overall, ampicillin/sulbactam resistance increase appears driven more by clonal expansion, environmental persistence, and pharmacodynamic inadequacy than by overuse.
Regarding colistin, global studies report rising resistance due to lipopolysaccharide modification, membrane permeability changes, efflux activity, and hetero-resistance [
64]. Reports from Italy and Iran documented post-pandemic increases up to 44.2% [
62,
65]. In contrast, our data show persistently low colistin resistance despite increased use in COVID-19 units. The stability of susceptible clones lacking key resistance mutations (e.g.,
pmrAB,
lpxACD) likely explains this observation, suggesting that local clonal dynamics, rather than global selective trends, shaped resistance patterns [
66].
P. aeruginosa is a frequent nosocomial pathogen, accounting for ≈10–11% of infections and up to 23% in intensive care [
67]. Its resistance mechanisms mainly involve porin modification and efflux pump overexpression [
68]. According to the 2023 ECDC–WHO surveillance data,
P. aeruginosa remains a critical therapeutic concern across Europe. Carbapenem resistance exceeds 40% in parts of southern and eastern Europe, while the EU/EEA mean remains above 20%. Although some northern and western countries reported slight post-2021 improvements, resistance to key agents—including carbapenems, fluoroquinolones, and aminoglycosides—persists at clinically significant levels, especially in intensive care environments [
6].
In our study, resistance to cefepime declined across most departments, reaching statistical significance in both COVID-19 (CAIC, 2nd DS) and non-COVID-19 units (DAIC, 1st DIM). Baseline resistance exceeded 60% in CAIC and 40% in 1st DIM. Italian data reported lower baseline values (28%) with only a mild pandemic increase to 38%, contrasting with our findings [
69]. In our hospital, pre-pandemic cefepime use was minimal, suggesting that direct selective pressure was unlikely. The persistent post-pandemic decline across all sites likely reflects clinical omission. Comparable results from Serbia demonstrated that cefepime withdrawal reduced resistance not only to cefepime but also to meropenem, piperacillin/tazobactam, and ceftazidime [
70]. These effects are attributed to the attenuation of efflux-pump and porin-mediated mechanisms [
71].
Meropenem resistance showed complex dynamics. Before the pandemic, resistance was low in non-COVID-19 wards (1st DIM, 1st DS) and the 4th DIM but markedly higher in the CAIC (73.6%) and DAIC (31.5%). Rates remained largely stable during the pandemic, contrasting reports of doubling in other ICUs [
72]. This stability likely reflects effective stewardship that limited efflux-related carbapenem resistance [
71,
73].
Piperacillin/tazobactam resistance was initially highest in the CAIC (64%) and 2nd DS (38.9%) but declined during the pandemic to 36% and 30%, respectively, reaching statistical significance in the CAIC. This trend aligns with studies linking reductions to strict infection control despite increased antibiotic use [
69,
74]. Resistance stability, despite higher consumption, supports findings that extended-infusion dosing maintains efficacy and suppresses resistance [
40].
Ciprofloxacin resistance decreased across several units, paralleling reduced use. However, it remained the only antibiotic with resistance consistently > 20% in all sites and years, reflecting extensive prior fluoroquinolone use and the intrinsic adaptability of
P. aeruginosa [
75].
Gentamicin and amikacin resistance declined across multiple departments, with the CAIC maintaining the highest and the 1st DS the lowest levels. International patterns vary, showing stability in Kuwait but ICU increases in Mexico [
76,
77]. Our decrease likely reflects reduced aminoglycoside use during the pandemic, consistent with Taipei data linking lower consumption to reduced resistance [
40].
Analysis of resistance mechanisms showed that
Klebsiella sp. exhibited declining ESBL prevalence and rising carbapenemase-mediated resistance. Non-COVID-19 units had more narrow-spectrum β-lactamases, whereas COVID-19 units demonstrated greater carbapenemase production, aminoglycoside resistance, and multidrug resistance. The ESBL decline parallels global reports and is linked to strengthened infection control, reduced antibiotic use, and travel restrictions [
78]. Lower fluoroquinolone use likely contributed through the co-localisation of ESBL and fluoroquinolone resistance genes [
79]. The rise in carbapenem resistance mirrors global trends of increasing CRE incidence during the pandemic, driven by intensive carbapenem use, prolonged ICU stays, and widespread immunosuppressive therapy [
78,
80,
81].
The higher prevalence of narrow-spectrum β-lactamases in non-COVID-19 units is noteworthy. Literature suggests that enzymes such as TEM-1, SHV-1, and OXY-1, when combined with outer membrane protein mutations, can confer resistance to cefoperazone/sulbactam and piperacillin/tazobactam in otherwise carbapenem-susceptible
Enterobacteriaceae [
31]. Although Omp mutations were not evaluated in this study, the substantial increase in piperacillin/tazobactam and cefoperazone/sulbactam use during the pandemic—particularly in the DAIC—supports the hypothesis that these mechanisms underlie the observed rise in β-lactam resistance without a concurrent increase in carbapenem resistance.
For Acinetobacter sp., no major changes in carbapenem resistance were noted. For P. aeruginosa, we found significant decreasing trends in efflux + porin mechanisms, carbapenemase/MBL production, overall carbapenem resistance, and multidrug resistance within COVID-19 units.
The repurposing of hospitals significantly impacted antibiotic consumption. COVID-19 units showed markedly greater antibiotic consumption (e.g., meropenem use sharply increased during 2020–2021), indicating stronger selective pressure [
82,
83]. Trends in cephalosporin and fluoroquinolone use mirrored global patterns, with initial increases in some cephalosporins followed by stabilization or decline, and an overall reduction in fluoroquinolone use [
84,
85,
86]. Higher baseline consumption in COVID-19 units, reflecting patient complexity and prescribing habits, was amplified during repurposing. Decrease in ciprofloxacin use showed a significant positive correlation with ESBL prevalence, while meropenem use correlated with carbapenemase resistance (ρ = 0.750;
p = 0.052). Despite a marked decline in ceftriaxone use, no significant association with ESBL reduction was observed.
The comparison of clinically applicable antibiotics revealed substantial inter-unit disparities. Clinical applicability is increasingly limited by resistance, contributing to longer hospital stays, higher morbidity, mortality, and costs [
87]. Inappropriate prescribing remains a major driver, with a significant share of inpatient antibiotic use failing to meet standards for indication, dosage, or duration [
88]. The non-COVID-19 units had already implemented stricter ASP measures pre-pandemically, contributing to their more favourable resistance profiles.
Non-COVID-19 units (1st DIM, 1st DS, DAIC) retained a wider range of effective antibiotics, including piperacillin/tazobactam, cefoperazone/sulbactam, and meropenem against Klebsiella sp. and P. aeruginosa. For Acinetobacter sp., colistin remained the only effective option in both settings. COVID-19 units (4th DIM, 2nd DS, CAIC) were severely limited, with some wards having only one to four usable agents. High resistance rendered piperacillin/tazobactam, cefoperazone/sulbactam, meropenem, and aminoglycosides largely ineffective, while ceftriaxone and ciprofloxacin had lost all clinical value.
These discrepancies likely stem from differences in ASP enforcement, use of infection biomarkers, individualised PK/PD dosing, and infection-control standards [
89].
Our study provides a unique contribution to AMR–COVID-19 research through its seven-year longitudinal scope (2018–2024) and granular, unit-level evaluation of resistance and antibiotic consumption. By directly comparing COVID-19 and non-COVID-19 units within a single hospital, it captures real-world stewardship and epidemiological dynamics often overlooked in multicenter or surveillance-based studies. The integration of consumption and mechanistic data allows clearer identification of selective pressures, offering valuable guidance for future stewardship and infection-control strategies.
This study has several limitations. A key limitation is the retrospective, single-center design, which constrains external validity and precludes causal inference from ecological associations between antibiotic consumption and resistance. Temporal changes unrelated to the pandemic such as evolving case-mix, shifts in diagnostic intensity, and variable device utilization, may confound observed trends, and we lacked patient-level covariates to adjust for these factors. We did not perform molecular typing; hence, inferences about clonal spread or specific mechanisms remain indirect. Antibiotic use was standardized as packages per 100 hospitalizations rather than DDD per 1000 patient-days, which may bias comparisons across wards with different lengths of stay and acuity, and dosing/PK–PD adherence (including extended infusions or sulbactam dose optimization) could not be verified. We analyzed clinical isolates without systematically distinguishing colonization from infection across all sites and time periods, and changes in screening or sampling practices during surge phases could introduce bias. Several subgroup analyses had limited sample size, reducing statistical power. Finally, we did not link resistance patterns to clinical outcomes (e.g., time to effective therapy, mortality), which limits conclusions about the patient-level impact of the observed epidemiology.
Nevertheless, our study provides valuable insight into local antimicrobial epidemiology and resistance dynamics. Future multicenter prospective studies with molecular typing are warranted to validate these results and to clarify transmission pathways. Linking resistance data with antibiotic consumption and stewardship interventions would further enhance clinical practice and optimize empiric therapy.
4. Materials and Methods
4.1. Study Design
This research, aimed at evaluating the prevalence and trends of resistance in the three most epidemiologically and clinically significant Gram-negative pathogens—Klebsiella sp., Acinetobacter sp., and P. aeruginosa—across selected departments of Louis Pasteur University Hospital (UNLP), was conducted as a retrospective observational study. The primary data source consisted of microbiological records from the Institute of Medical and Clinical Microbiology (IMCM), including antibiogram results and resistance profile analyses.
The analyzed data, spanning the period from 1 January 2018, to 31 December 2024, were divided into three time intervals:
Pre-pandemic period (1 January 2018–31 December 2019);
Pandemic period (1 January 2020–31 December 2022);
Post-pandemic period (1 January 2023–31 December 2024).
Since data from the IMCM are evaluated on a calendar-year basis, they closely but not entirely reflect the pandemic timeframe. This division enabled monitoring of resistance dynamics in relation to prevailing epidemiological conditions, with an anticipated impact of the pandemic on antimicrobial resistance (AMR) trends.
4.2. Study Population
Two groups of hospital units were included in the analysis:
COVID-19 units: These were repurposed during the pandemic to admit and manage patients with COVID-19. Units were selected based on sufficient numbers of hospitalized patients, bacterial isolates, and a diverse patient population. The following were included: the 4th Department of Internal Medicine (4th DIM), the 2nd Department of Surgery (2nd DS), and the Department of Anesthesiology and Intensive Care Medicine (DAIC);
non-COVID-19 units: These departments, which had comparable patient numbers and case mix to the COVID-19 units, were not affected by the increased burden of COVID-19 hospitalizations. The following were included: the 1st Department of Internal Medicine (1st DIM), the 1st Department of Surgery (1st DS), and the Clinic of Anesthesiology and Intensive Care Medicine (CAIC).
Other departments were excluded primarily due to insufficient numbers of bacterial isolates. Patient counts in internal medicine and surgical units also encompassed individuals from their respective intensive care units.
The COVID-19 and non-COVID-19 units were located at separate hospital sites, which significantly limited patient transfers between them. This spatial separation minimized cross-unit patient mixing, thereby reducing the risk of direct microbial transmission. Consequently, the microbial environments of the respective sites were expected to exhibit distinct characteristics, shaped by differences in patient populations, antimicrobial exposure, and disinfection or sterilization practices. This factor plays a critical role in interpreting data on microbial ecology and the spectrum of nosocomial pathogens across hospital sites.
4.3. Methodology
The study was conducted as a retrospective analysis of epidemiological data, including evaluation of hospitalization numbers across departments using the Hospital Information System (HIS). Analyses were based on patient counts rather than hospital stays. Owing to HIS limitations, only so-called first admissions were assessed (patients with multiple admissions in a single year were counted once). Transfers between departments with subsequent returns were recorded as a single hospitalization. In collaboration with the hospital’s IT department, data were extracted under the technical constraints of the HIS, ensuring values were as close to reality as possible. The data were then systematically stratified by unit and year.
Microbiological data were obtained from the IMCM at UNLP. Analyses included total numbers of pathogens isolated from clinical samples, as well as resistance profiles. All clinical samples collected at the respective units were included, regardless of whether the isolated pathogen represented colonization or infection. This strategy was chosen to provide a comprehensive overview of the hospital microbiome.
Resistance to selected antibiotics was assessed using standard disk diffusion methods (Oxoid Ltd., Basingstoke, UK) and automated susceptibility testing using the VITEK 2 system (bioMérieux, Marcy-l’Étoile, France; software version 9.02). All procedures were carried out in accordance with the recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST, version 13.0, 2023). Resistance was reported as percentage values derived from antibiograms. Classification of pathogens as resistant or susceptible applied a 20% threshold, based on the average resistance value across the entire study period. Only resistance percentages were evaluated, not susceptibility. This approach enabled identification of clinically relevant resistance rates, evaluation of temporal dynamics, and comparison between COVID-19 and non-COVID-19 units.
The study focused on the following resistance mechanisms: production of narrow-spectrum β-lactamases, extended-spectrum β-lactamases (ESBL), AmpC, carbapenemases, aminoglycoside resistance, efflux pump activity, porin expression, and overall multidrug resistance. These mechanisms allowed for a comprehensive assessment of the type and dynamics of resistance during the study period.
Antibiotics included in resistance evaluation were as follows:
Acinetobacter sp.: ampicillin/sublactam (SAM), piperacillin/tazobactam (TZP), ceftazidime (CAZ), cefepime (FEP), imipenem (IMP), meropenem (MEM), gentamicin (GEN), amikacin (AMI), ciprofloxacin (CIP), and colistin (COL);
P. aeruginosa: TZP, CAZ, cefoperazone/sulbactam (SPZ), FEP, aztreonam (ATM), IMP, MEM, GEN, AMI, CIP, and COL;
Klebsiella sp.: TZP, cefotaxime (CTX), CAZ, SPZ, FEP, ertapenem (ETP), MEM, GEN, AMI, CIP, and COL.
Antibiotic consumption data were obtained from the hospital pharmacy. Because consumption data were unavailable in the format of Defined Daily Doses (DDD), as recommended by the WHO, this methodology could not be applied. The limitation was due to the unavailability of precise milligram-level dispensing records for each antibiotic. Instead, the number of packages of each antibiotic consumed per 100 hospitalizations was chosen as a surrogate indicator, enabling relative comparisons across units. Identical drug package formats were used across all years, ensuring data comparability. This approach allowed monitoring of antibiotic consumption trends in the hospital setting despite the lack of standardized DDD data.
4.4. Statistical Analysis
Trends in hospitalizations and antibiotic resistance were analyzed using linear regression and Spearman’s rank correlation. Linear regression was applied to quantify linear trends (increase or decrease) in continuous variables over time. To assess monotonic trends, Spearman’s correlation was used, as it does not assume normal data distribution and is robust to outliers and small sample sizes. Statistical analyses were conducted using IBM SPSS Statistics (version 29.0; IBM Corp., Armonk, NY, USA).
Comparisons of hospitalization numbers between COVID-19 and non-COVID-19 units of the same type were performed using the paired parametric t-test, selected for its suitability in analyzing paired datasets from comparable units under different conditions. To verify robustness and account for the limited number of years analyzed, the non-parametric Wilcoxon signed-rank test was also applied.
For comparing average annual numbers of pathogen isolates across different time periods, the two-sample t-test with Welch’s correction was used, ensuring reliable results in the presence of unequal variances. Differences in isolate occurrence normalized per number of hospitalizations were evaluated using the non-parametric Mann–Whitney U test, due to potential non-normality in smaller sample sets.
Differences in the occurrence of selected nosocomial pathogens between COVID-19 and non-COVID-19 units were analyzed using Fisher’s exact test, appropriate for categorical data (pathogen present/absent) and small sample sizes.
All statistical methods were selected with respect to the characteristics of the analyzed data, sample size, and test assumptions. Since normality could not always be guaranteed due to limited sample sizes, a combination of parametric and non-parametric methods was employed to ensure robust results. Statistical significance was set at p < 0.05.
The results are presented in structured tables and figures illustrating observed trends and comparisons. The study was approved by the UNLP Ethics Committee (approval no. 2025/EK/04034).